Professional Documents
Culture Documents
Kim 2006
Kim 2006
Uploaded by
pilarerasoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kim 2006
Kim 2006
Uploaded by
pilarerasoCopyright:
Available Formats
October 2006: (I)468 – 475
Brief Critical Review
Does a High Folate Intake Increase the Risk of Breast
Cancer?
Young-In Kim, MD, FRCP(C)
Although not uniformly consistent, epidemiologic play an important pathogenetic role in the development
studies generally suggest an inverse association be- of anemia, atherosclerosis, neural tube defects, adverse
tween dietary intake and blood measurements of folate pregnancy outcomes, and neuropsychiatric disorders.2
and breast cancer risk. However, the Prostate, Lung, Folate has generally been regarded as safe and has long
Colorectal, and Ovarian (PLCO) Cancer Screening been presumed to be purely beneficial3 and an ideal
trial has recently reported for the first time a potential functional food component for disease prevention.4 For
harmful effect of high folate intake on breast cancer example, an overwhelming body of evidence for a pro-
risk. In this study, the risk of developing breast cancer tective effect of periconceptional folic acid supplemen-
was significantly increased by 20% in women report- tation against neural tube defects led to mandatory folic
ing supplemental folic acid intake ⱖ 400 g/d com- acid fortification in the United States and in Canada in
pared with those reporting no supplemental intake. 1998.2 Preliminary reports suggest a significant reduc-
Furthermore, although food folate intake was not
tion (15%–50%) in the incidence of neural tube defects
significantly related to breast cancer risk, total folate
in the United States and Canada associated with this
intake, mainly from folic acid supplementation, signif-
mandatory fortification.2 In addition to the drastic in-
icantly increased breast cancer risk by 32%. The data
crease in dietary intake from mandatory folic acid forti-
from the PLCO trial support prior observations made
in epidemiologic, clinical, and animal studies suggest- fication,5-7 30% to 40% of the North American popula-
ing that folate possesses dual modulatory effects on tion consume supplemental folic acid for several possible
the development and progression of cancer depending but as yet unproven health benefits, including prevention
on the timing and dose of folate intervention. Based on of atherosclerosis, improvement in cognitive function,
the lack of compelling supportive evidence, routine and cancer prevention.8
folic acid supplementation should not be recom- Folate deficiency has also been linked to the risk of
mended as a chemopreventive measure against breast several malignancies in humans, including cancer of the
cancer at present. colorectum, oropharynx, esophagus, stomach, pancreas,
Key words: breast cancer, folate, folic acid lungs, cervix and ovary, and neuroblastoma and leuke-
© 2006 International Life Sciences Institute mia.9,10 Although not uniformly consistent, dietary in-
doi: 10.1301/nr.2006.oct.468 – 475 take and blood levels of folate have generally been
shown to be inversely related to the risk of these malig-
nancies in a large body of epidemiologic studies.9,10
Folate is a water-soluble B vitamin and important
However, the precise role of folate deficiency in cancer
cofactor in one-carbon metabolism.1 Folic acid is the
development and progression and of folate supplemen-
fully oxidized monoglutamyl form of this vitamin that is
tation in cancer prevention remain highly speculative and
used commercially in supplements and in fortified
provocative to date.
foods.1 The role of folate in human health and disease
has rapidly been expanding. Folate deficiency appears to
Folate and Breast Cancer: Epidemiologic
Evidence
Dr. Kim is with the Department of Medicine and
Nutritional Sciences, University of Toronto, Division of An accumulating number of epidemiologic studies
Gastroenterology, St. Michael’s Hospital, Toronto, have suggested an inverse association between folate
Canada.
status and the risk of breast cancer. However, epidemi-
Please address all correspondence to: Dr. Young-In
Kim, Room 7258, Medical Sciences Building, University ologic evidence available thus far has not been consis-
of Toronto, 1 King’s College Circle, Toronto, Ontario, tent, nor has it provided unequivocal support for the
Canada, M5S 1A8; Phone: 416-978-1183; Fax: 416- purported inverse relationship between folate status and
978-8765; E-mail: youngin.kim@utoronto.ca breast cancer risk. The majority of 13 published case-
468 Nutrition Reviews姞, Vol. 64, No. 10
control studies investigating the relationship between with low or no alcohol consumption. Furthermore, these
dietary folate intake and breast cancer risk showed either studies also suggest that the increased risk of breast
a significant or equivocal inverse relationship that was cancer associated with alcohol consumption is more
not statistically significant, became nonsignificant after pronounced in or limited to women with low folate
adjustment, or could not be distinguished from other intake. Two prospective studies have since shown that
factors in relation to risk.11-23 Overall, these studies the increased risk of breast cancer associated with low
suggested a 30% to 35% reduction in the risk of devel- folate and high alcohol intake is limited to estrogen
oping breast cancer in individuals with the highest di- receptor-negative breast cancer.38,39
etary intake of folate compared with those with the
lowest intake.11-23 Two of these studies also examined Folate-Gene Interactions in Breast Cancer Risk
the association between total folate intake (dietary plus Modifications
supplemental) and breast cancer risk and found no sig-
nificant relationship.14, 22 Recent molecular epidemiologic studies have also sug-
The interpretation of results from case-control stud- gested that the inverse association between folate status and
ies are often limited because of inherent problems asso- breast cancer risk, as well as the interaction between folate
ciated with retrospective analyses, including the accu- and alcohol in modifying this risk, are further modulated by
racy with which intake of dietary factors or polymorphisms of critical genes (e.g., C667T polymor-
supplementation can be established and the inability to phism of the methylenetetrahydrofolate reductase [MTHFR
adequately control or correct potential confounders. The C677T] gene) that are involved in the folate metabolic
relationship between dietary and total intake of folate pathway. A recent meta-analysis has shown that the
and breast cancer risk has also been examined in seven MTHFR C677T polymorphism may increase the risk of
prospective studies that avoid most of the methodologi- breast cancer in premenopausal women and in women with
cal problems of case-control studies and that can control low folate intake.40
and correct confounding factors more adequately than
can case-control studies.24-30 None of these prospective
Folate and Breast Cancer: Evidence from
studies found a significant association between either Animal Studies
dietary or total folate intake and breast cancer risk.24-30
With respect to actual blood (serum or plasma) levels of Although direct evidence from human intervention
folate and breast cancer risk, one case-control study trials is lacking at present, three animal studies41-43
reported a significant inverse association,31 two nested conducted in the well-established N-methyl-N-nitro-
case-control studies found a nonsignificant inverse asso- sourea (MNU) rat model of mammary tumorigenesis
ciation,32,33 and another nested case-control study ob- provide a vastly different picture of the role of folate in
served no association.34 breast carcinogenesis than that from human epidemio-
logic studies. These studies collectively suggest that
Folate-Alcohol Interactions in Breast Cancer dietary folate deficiency of a mild degree significantly
Risk Modifications inhibits, whereas folic acid supplementation (4 –20 times
above the basal dietary requirement) does not signifi-
Overall, the portfolio of epidemiologic evidence cantly modulate, the development and progression of
supporting the relationship between folate status and mammary tumors in this model.41-43 Although MNU-
breast cancer risk in women is tenuous at best. However, induced mammary tumorigenesis in rat is different from
a clearer picture emerges when studies examining the the human disease in several important aspects, this
joint effects of folate and alcohol are considered. Con- model is generally considered to be the best animal
sumption of alcohol, a well-established folate antago- model of breast cancer currently available because of
nist,35 has consistently been shown to increase the risk of histological, clinical, and certain molecular similarities
breast cancer in epidemiologic studies, and is accepted as to human breast cancer.44
a well-established risk factor for breast cancer develop-
ment.36,37 All prospective studies24-26,29,30 except one28 Prostate, Lung, Colorectal, and Ovarian Cancer
and three case-control studies16-18 that examined this Screening Trial
issue have found a significant interaction between alco-
hol and folate intake in modifying the risk of breast In contrast to the inverse association, albeit not
cancer. These studies collectively suggest that low folate uniformly consistent, between folate intake and breast
intake increases, whereas high intake decreases, breast cancer risk reported in epidemiologic studies thus far, a
cancer risk among women who regularly consume mod- recently published prospective study suggested for the
erate or high amounts of alcohol, but not among women first time a potential harmful effect of high folate intake
Nutrition Reviews姞, Vol. 64, No. 10 469
on breast cancer risk.45 The Prostate, Lung, Colorectal, strengths and weaknesses usually associated with the
and Ovarian (PLCO) Cancer Screening Trial is a pro- prospective epidemiologic design. One of the weak-
spective study that investigated the association between nesses associated with this study was that folate intake at
folate intake, alcohol consumption, and postmenopausal baseline was correlated to subsequent incidence of breast
breast cancer risk. Women 55 to 74 years of age between cancer. In other words, folate intake at baseline was
November 1993 and July 2001 were recruited in 10 US assumed to reflect past and subsequent consumption.
centers. Women with a personal history of one of the Therefore, whether the subjects in these studies changed
prostate, lung, colorectal, and ovarian cancers, with a their diet during the follow-up period and how this might
recent history of screening procedures for one of these have affected the study outcome could not be deduced. In
cancers, or with current treatment for any cancer except this regard, the most limiting factor in interpreting the
non-melanoma skin cancer were excluded from the trial. data in this study is mandatory folic acid fortification in
Women randomly assigned to the intervention arm un- the United States beginning in 1998.
derwent period cancer screening tests for these four The effectiveness of folic acid fortification in
cancers, where those assigned to the control were in- improving folate status has already been shown to be
structed to follow their usual medical practice. Of the quite striking, with a dramatic increase in blood mea-
77,376 women enrolled in the PLCO trial, only those in surements of folate concentrations in the United States
the intervention arm were given the food frequency and Canada.2 In these two countries, the average
questionnaire at baseline (n ⫽ 38,660), which was self- post-fortification total folate intake is estimated to be
administered and characterized usual dietary intake over approximately 400 g/d in supplement non-users,
the preceding 12 months prior to the study. After appro- with approximately 200 g/d consumed as naturally
priate exclusion, 25,400 women remained for analysis. occurring folate food and approximately 200 g/d as
Between September 1993 and June 2003, 691 incident folic acid provided in enriched products.2 For those
breast cancer cases were identified and confirmed. The taking multivitamins containing folic acid, the esti-
risk of developing breast cancer was adjusted for age, mated total folate intake is approximately 800 g/d.
education, age at menarche, parity, age at first birth, oral Several studies assessing food composition and di-
contraceptive use, age at menopause, hormonal replace- etary intakes have suggested that the increased post-
ment therapy, mammography screening history, history fortification folate intake in the US population may be
of benign breast disease, family history, and energy. about twice that originally anticipated.5-7 Further-
The main, and novel, finding of this study is that the more, these estimates of folate intake based on food
risk of developing breast cancer was significantly increased composition databases are likely to be low because of
by 20% (hazard ratio [HR] ⫽ 1.19; 95% confidence interval limitations in the analytic methods previously used to
[CI] ⫽ 1.01-1.41; P trend ⫽ 0.04) in women reporting analyze food folate.5-7 The PLCO Cancer Screening
supplemental folic acid intake ⱖ 400 g/d compared with Trial only estimated folate intake at baseline (most
those reporting no supplemental intake. Furthermore, al- subjects were recruited in the pre-fortification era) and
though food folate intake was not significantly related to did not measure any change in folate intake during the
breast cancer risk (HR for highest [⬎412 g/d] versus study period. Therefore, this study did not correct for
lowest [ⱕ261 g/d] intake ⫽ 1.04; 95% CI ⫽ 0.83–1.31; P possible confounding effects of folic acid fortification
trend ⫽ 0.56), total folate intake, mainly from folic acid in data analysis.
supplementation, significantly increased breast cancer risk Another shortcoming is that this study did not con-
by 32% (HR for highest [⬎853 g/d] versus lowest [ⱕ336 sider and incorporate interactions between folate and
g/d] ⫽ 1.32; 95% CI ⫽ 1.04 –1.68; P trend ⫽ 0.03). several genetic polymorphisms in the folate metabolic
Consistent with previous findings, alcohol consumption pathway in the study design and data analysis. Advances
was positively associated with breast cancer risk and the in molecular epidemiology have added another dimen-
risk was greatest in women with lower total folate intake. sion to the already complex field of nutrition and cancer.
This study is therefore the first to suggest that high folate Recently identified and characterized single nucleotide
intake, generally attributable to supplemental folic acid, polymorphisms and other genetic and epigenetic variants
may increase the risk of breast cancer in postmenopausal of genes that are involved in the absorption, transport,
women. metabolism, and excretion of nutrients have been shown
not only to modify cancer risk but also to significantly
Commentary on the PLCO Cancer Screening modulate the effect of nutrients and related compounds
Trial on cancer risk.46 In this regard, there is an emerging body
of evidence suggesting that several genetic polymor-
The PLCO Cancer Screening Trial is a well-de- phisms in the folate metabolic pathway (e.g., MTHFR
signed and conducted prospective study with obvious C677T) interact with folate and other related nutrients
470 Nutrition Reviews姞, Vol. 64, No. 10
(e.g., alcohol) in modulating the risk of cancers including DUAL MODULATORY ROLE OF FOLATE IN
breast cancer.40,47 This emerging important topic in the CARCINOGENESIS
field of nutrition and cancer, termed “gene-nutrient in-
teractions” in carcinogenesis, has significant implications Folate appears to possess dual modulatory effects on
in designing and interpreting data from observational carcinogenesis depending on the timing and dose of
epidemiologic and intervention studies. Although indi- folate intervention.2,9,48 Folate deficiency has an inhibi-
viduals are subjected to the same level of nutritional tory effect, whereas folate supplementation has a pro-
exposure, systemic and target tissue bioavailability of moting effect, on the progression of established neo-
nutrients and their metabolites, as well as their functional plasms.2,9,48 In contrast, folate deficiency in normal
effects in the target tissue, might be vastly different tissues appears to predispose them to neoplastic transfor-
because of genetic and epigenetic variations. mation, and modest supplemental levels suppress,
whereas supraphysiologic doses of supplementation en-
Folate and Colorectal Cancer: A Complex Role hance, the development of tumors in normal tissues.2,9,48
of Folate in Cancer Risk Modification Are there biologically plausible explanations for these
seemingly paradoxical and contradictory epidemiologic,
The puzzling role of folate in breast tumorigenesis is animal, and clinical observations concerning the role of
closely mirrored in colorectal carcinogenesis. An over- folate in cancer development and progression?
whelming body of epidemiologic evidence from case- As an essential cofactor for the de novo biosynthesis
control and prospective studies, including recent meta- of purines and thymidylate, folate plays an important role
analyses, suggests an inverse association between folate in DNA synthesis, stability, integrity, and repair, aberra-
status and the risk of colorectal cancer.47,48 Furthermore, tions of which have been implicated in carcinogene-
small clinical trials have demonstrated that folic acid sis.9,50,51 Folate may also modulate DNA methylation,
supplementation can improve or reverse surrogate end- which is an important epigenetic determinant in gene
point biomarkers of colorectal cancer.9,48 Animal studies expression, in the maintenance of DNA integrity and
generally support a causal relationship between folate stability, in chromosomal modifications, and in the de-
depletion and colorectal cancer risk and an inhibitory velopment of mutations.9,10 The potential for a dual
effect of modest levels of folate supplementation on modulatory role for folate on carcinogenesis is illustrated
colorectal carcinogenesis.9,48 However, these animal in Figure 1. In normal tissues, folate deficiency is asso-
studies have also shown that the dose and timing of ciated with DNA strand breaks, impaired DNA repair,
folate intervention are critical in providing safe and increased mutations, and aberrant DNA methylation,
effective chemoprevention; exceptionally high supple- thereby predisposing them to neoplastic transformation,
mental folate levels and folate intervention after micro- and folate supplementation can correct some of these
scopic neoplastic foci are established in the colorectal
defects induced by folate deficiency, thereby preventing
mucosa promote, rather than suppress, colorectal carci-
or suppressing neoplastic transformation.9,10,50,51 In con-
nogenesis.9,48
trast, in neoplastic cells, where DNA replication and cell
The Aspirin-Folate Polyp Prevention Study (N ⫽
division are occurring at an accelerated rate, folate de-
1021) reported that folic acid supplementation (1 mg/d)
pletion causes ineffective DNA synthesis, resulting in
for up to 6 years in subjects with previous colorectal
inhibition of tumor growth and progression, which is the
adenomas (well-established precursor of colorectal ade-
basis for antifolate-based cancer chemotherapy.9,10,50,51
nocarcinoma) did not significantly prevent the recurrence
of colorectal adenomas (rate ratio [RR] ⫽ 1.04).49 How- Folic acid supplementation promotes the progres-
ever, folic acid supplementation significantly increased sion of rapidly replicating preneoplastic and neoplastic
the number of adenomas by 44% (RR ⫽ 1.44; 95% CI ⫽ cells by providing nucleotide precursors for an acceler-
1.03–2.02) and nonsignificantly increased the incidence ated proliferation and growth.9,10,50,51 Another mecha-
of advanced adenomas with a high malignant potential nism of the folic acid supplementation-associated tumor
compared with placebo.49 One explanation for this un- promoting effect may be de novo methylation of pro-
expected observation is that folic acid supplementation moter CpG islands of tumor suppressor genes with con-
might have promoted the progression of already existing, sequent gene inactivation leading to tumor progres-
undiagnosed preneopalstic lesions (e.g., aberrant crypt sion.2,10 This potential epigenetic mechanism of tumor
foci, the probable earliest precursor of colorectal adeno- progression is supported by recent animal studies using
carcinoma or microscopic adenomas) or adenomas viable yellow agouti mice that unequivocally have dem-
missed on initial colonoscopy in these genetically pre- onstrated that maternal dietary methyl group supplemen-
disposed subjects at high risk of developing colorectal tation with a modest amount of folic acid permanently
cancer. alters phenotypic coat color of the offspring via in-
Nutrition Reviews姞, Vol. 64, No. 10 471
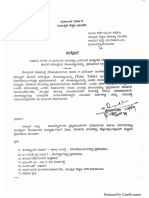
Tumor promoting mechanisms: Tumor inhibitory mechanism:
1. DNA strand breaks Ineffective DNA synthesis leading to
2. Impaired DNA repair inhibition of tumor growth and progression
3. Increased mutagenesis
4. Genomic DNA hypomethylation Folate deficiency
risk of neoplatic
transformation
? progression of
early IEN
progression of
late IEN to cancer
progression of
cancer
Normal Intraepithelial Neoplasia Cancer
risk of neoplatic progression of progression of progression of
transformation ? early IEN late IEN to cancer cancer
Folate supplementation
Tumor inhibitory mechanisms: Tumor promoting mechanisms
1. DNA stability and integrity 1. Provision of nucleotide precursors for
2. Optimal DNA repair proliferation and growth of neoplastic cells
3. Decreased mutagenesis 2. De novo methylation of promoter CpG islands of
4. Prevention of aberrant DNA methylation tumor suppressor genes leading to gene inactivation
Figure 1. Dual modulatory role of folate in carcinogenesis. Cancer develops over decades, if not a lifetime, through different stages
of premalignant lesions (intraepithelial neoplasia, IEN) in the target organ. Folate deficiency in normal tissues predisposes them to
neoplastic transformation and modest supplemental levels suppress, whereas supraphysiologic doses of supplementation enhances,
the development of tumors in normal tissues. In contrast, folate deficiency has an inhibitory effect, whereas folate supplementation
has a promoting effect, on the progression of established neoplasms. The effect of folate deficiency and supplementation on the
progression of early precursor or preneoplastic IEN lesions to more advanced stages of IEN and to frank cancer is unknown at present.
The mechanisms by which folate exerts dual modulatory effects on carcinogenesis depending on the timing and dose of folate
intervention relate to its essential role in one-carbon transfer reactions involved in DNA synthesis and biological methylation
reactions.
creased methylation at the promoter CpG site of the total cancer (RR ⫽ 1.22; 95% CI ⫽ 0.88 –1.70) in the
agouti gene.52,53 Norwegian Vitamin Trials (N ⫽ 3749; 800 g folic
acid/d for 40 months)54 and of colon cancer (RR ⫽ 1.36;
Effects of Folate Supplementation and 95% CI ⫽ 0.89 –2.08) in the Heart Outcomes Prevention
Fortification on Cancer Risk in Humans Evaluation II Trial (N ⫽ 5522; 2.5 mg folic acid/d for 5
years).55
In addition to the Aspirin-Folate Polyp Prevention Among participants in a large (N ⫽ 2928) trial of
Study,49 which observed a possible tumor-promoting folic acid supplementation during pregnancy, women
effect of folic acid supplementation, several uncontrolled who received 5 mg folic acid/d had a 70% increased risk
or randomized studies have investigated the effect of of total cancer mortality compared with those not on
folic acid supplementation on cancer risk as either the supplementation (HR ⫽ 1.70; 95% CI ⫽ 1.06 –2.72; P ⫽
primary or secondary endpoint. Two recently published 0.02).56 The risk of death from breast cancer in women
large, randomized, placebo-controlled intervention trials taking 5 mg folic acid/d was twice that of women taking
designed to test the effect of folic acid supplementation no supplementation in this study, albeit nonsignificant
in conjunction with other B vitamins on primary and (HR ⫽ 2.02; 95% CI ⫽ 0.88 – 4.72; P ⫽ 0.10).56 The
secondary prevention of cardiovascular events have re- tumor-promoting effect of folate supplementation on
ported a nonsignificant trend toward an increased risk of established neoplasm is actually not a new observation;
472 Nutrition Reviews姞, Vol. 64, No. 10
in the 1940s, children with acute leukemia treated with plastic or neoplastic foci in the breast and other target
folate supplementation experienced an accelerated pro- organs. Given the incidence and mortality of breast
gression of the disease.57 cancer in the United States, determining the overall
In contrast, a recent Canadian study reported the benefits of folic acid fortification and supplementation
effect of folic acid fortification on the incidence of has significant public health implications. As such, the
neuroblastoma among children ⱕ 17 years of age using role of folate in the development and progression of
the database of the Pediatric Oncology Group of Ontario, breast cancer needs to be clarified with additional future
which captures 95% of all pediatric cancers in Ontario.58 studies.
This study showed that folic acid fortification was asso-
ciated with a significant 60% reduction in the incidence
of neuroblastoma (from 1.57 cases per 10,000 births in REFERENCES
1996 to 0.62 cases per 10,000 births after 1997, when 1. Shane B. Folate chemistry and metabolism. In:
folic acid fortification of food became mandatory in Bailey LB, ed. Folate in Health and Disease. New
Canada).58 The incidence of infant acute lymphoblastic York: Marcel Dekker; 1995:1–22.
2. Kim YI. Will mandatory folic acid fortification prevent
leukemia and hepatoblastoma, however, remained al-
or promote cancer? Am J Clin Nutr. 2004;80:1123–
most the same in this study.58 1128.
3. Campbell NR. How safe are folic acid supplements?
Arch Intern Med. 1996;156:1638 –1644.
HIGH FOLATE INTAKES: BENEFICIAL OR 4. Lucock M. Is folic acid the ultimate functional food
HARMFUL? component for disease prevention? BMJ. 2004;328:
211–214.
Whether possible deleterious effects of folic acid 5. Choumenkovitch SF, Selhub J, Wilson PW, Rader
fortification and supplementation outweigh the known JI, Rosenberg IH, Jacques PF. Folic acid intake from
and potential health benefits is essentially unknown at fortification in United States exceeds predictions. J
Nutr. 2002;132:2792–2798.
present. In addition to masking of vitamin B12, especially
6. Pfeiffer CM, Caudill SP, Gunter EW, Osterloh J,
in the elderly, an emerging body of evidence suggests Sampson EJ. Biochemical indicators of B vitamin
that folate supplementation may possess potentially se- status in the US population after folic acid fortifica-
rious adverse effects, including resistance or tolerance to tion: results from the National Health and Nutrition
anti-folate-based chemotherapy and anti-inflammatory Examination Survey 1999 –2000. Am J Clin Nutr.
drugs; epigenetic instability; decreased natural killer cell 2005;82:442– 450.
7. Quinlivan EP, Gregory JF 3rd. Effect of food fortifi-
cytotoxicity; and genetic selection of disease alleles (e.g.,
cation on folic acid intake in the United States. Am J
MTHFR C677T).2,4,59,60 Furthermore, recent epidemio- Clin Nutr. 2003;77:221–225.
logic, animal, and intervention studies suggest that folate 8. Radimer K, Bindewald B, Hughes J, Ervin B, Swan-
supplementation may promote the progression of estab- son C, Picciano MF. Dietary supplement use by US
lished preneoplastic and neoplastic lesions.2,48,49,61,62 adults: data from the National Health and Nutrition
The potential adverse effects, including the cancer-pro- Examination Survey, 1999-2000. Am J Epidemiol.
2004;160:339 –349.
moting effect, from a drastic increase in folate intake
9. Kim YI. Folate and carcinogenesis: evidence, mech-
from mandatory fortification and supplementation in the anisms, and implications. J Nutr Biochem. 1999;10:
vast majority of the North American population need to 66 – 88.
be determined in long-term longitudinal studies as well 10. Kim YI. Folate and DNA methylation: a mechanistic
as in appropriate animal studies. link between folate deficiency and colorectal can-
cer? Cancer Epidemiol Biomarkers Prev. 2004;13:
511–519.
CONCLUSION 11. Graham S, Hellmann R, Marshall J, et al. Nutritional
epidemiology of postmenopausal breast cancer in
What can we conclude about the role of folate in western New York. Am J Epidemiol. 1991;134:552–
566.
breast cancer development and progression? Based on
12. Freudenheim JL, Marshall JR, Vena JE, et al. Pre-
the lack of compelling supportive evidence, routine folic menopausal breast cancer risk and intake of vege-
acid supplementation should not be recommended as a tables, fruits, and related nutrients. J Natl Cancer
chemopreventive measure against breast cancer at Inst. 1996;88:340 –348.
present. In fact, folate supplementation may promote the 13. Thorand B, Kohlmeier L, Simonsen N, Croghan C,
progression of already existing, undiagnosed pre-malig- Thamm M. Intake of fruits, vegetables, folic acid and
related nutrients and risk of breast cancer in post-
nant lesions in the breast. However, women consuming
menopausal women. Public Health Nutr. 1998;1:
moderate to high amounts of alcohol and women with 147–156.
the MTHFR C677T genotype may benefit from folate 14. Potischman N, Swanson CA, Coates RJ, et al. In-
supplementation, provided that they are free of preneo- take of food groups and associated micronutrients
Nutrition Reviews姞, Vol. 64, No. 10 473
in relation to risk of early-stage breast cancer. Int J postmenopausal women in Denmark. Eur J Clin
Cancer. 1999;82:315–321. Nutr. 2006;60:280 –286.
15. Ronco A, De Stefani E, Boffetta P, Deneo-Pellegrini 31. Beilby J, Ingram D, Hahnel R, Rossi E. Reduced
H, Mendilaharsu M, Leborgne F. Vegetables, fruits, breast cancer risk with increasing serum folate in a
and related nutrients and risk of breast cancer: a case-control study of the C677T genotype of the
case-control study in Uruguay. Nutr Cancer. 1999; methylenetetrahydrofolate reductase gene. Eur J
35:111–119. Cancer. 2004;40:1250 –1254.
16. Negri E, La Vecchia C, Franceschi S. Re: dietary 32. Zhang SM, Willett WC, Selhub J, et al. Plasma
folate consumption and breast cancer risk. J Natl folate, vitamin B6, vitamin B12, homocysteine, and
Cancer Inst. 2000;92:1270 –1271. risk of breast cancer. J Natl Cancer Inst. 2003;95:
17. Levi F, Pasche C, Lucchini F, La Vecchia C. Dietary 373–380.
intake of selected micronutrients and breast-cancer 33. Rossi E, Hung J, Beilby JP, Knuiman MW, Divitini
risk. Int J Cancer. 2001;91:260 –263. ML, Bartholomew H. Folate levels and cancer mor-
18. Shrubsole MJ, Jin F, Dai Q, et al. Dietary folate bidity and mortality: prospective cohort study from
intake and breast cancer risk: results from the Busselton, Western Australia. Ann Epidemiol. 2006;
Shanghai Breast Cancer Study. Cancer Res. 2001; 16:206 –212.
61:7136 –7141. 34. Wu K, Helzlsouer KJ, Comstock GW, Hoffman SC,
19. Sharp L, Little J, Schofield AC, et al. Folate and Nadeau MR, Selhub J. A prospective study on fo-
breast cancer: the role of polymorphisms in meth- late, B12, and pyridoxal 5’-phosphate (B6) and
ylenetetrahydrofolate reductase (MTHFR). Cancer breast cancer. Cancer Epidemiol Biomarkers Prev.
Lett. 2002;181:65–71. 1999;8:209 –217.
20. Zhu K, Davidson NE, Hunter S, et al. Methyl-group 35. Hillman RS, Steinberg SE. The effects of alcohol on
dietary intake and risk of breast cancer among folate metabolism. Annu Rev Med. 1982;33:345–
African-American women: a case-control study by 354.
methylation status of the estrogen receptor alpha 36. Smith-Warner SA, Spiegelman D, Yaun SS, et al.
genes. Cancer Causes Control. 2003;14:827– 836. Alcohol and breast cancer in women: a pooled
21. Adzersen KH, Jess P, Freivogel KW, Gerhard I, analysis of cohort studies. JAMA. 1998;279:535–
Bastert G. Raw and cooked vegetables, fruits, se- 540.
lected micronutrients, and breast cancer risk: a 37. Singletary KW, Gapstur SM. Alcohol and breast
case-control study in Germany. Nutr Cancer. 2003; cancer: review of epidemiologic and experimental
46:131–137. evidence and potential mechanisms. JAMA. 2001;
22. Chen J, Gammon MD, Chan W, et al. One-carbon 286:2143–2151.
metabolism, MTHFR polymorphisms, and risk of 38. Sellers TA, Vierkant RA, Cerhan JR, et al. Interaction
breast cancer. Cancer Res. 2005;65:1606 –1614. of dietary folate intake, alcohol, and risk of hormone
23. Lajous M, Lazcano-Ponce E, Hernandez-Avila M, receptor-defined breast cancer in a prospective
Willett W, Romieu I. Folate, vitamin B(6), and vitamin study of postmenopausal women. Cancer Epide-
B(12) intake and the risk of breast cancer among miol Biomarkers Prev. 2002;11:1104 –1107.
Mexican women. Cancer Epidemiol Biomarkers 39. Zhang SM, Hankinson SE, Hunter DJ, Giovannucci
Prev. 2006;15:443– 448. EL, Colditz GA, Willett WC. Folate intake and risk of
24. Zhang S, Hunter DJ, Hankinson SE, et al. A pro- breast cancer characterized by hormone receptor
spective study of folate intake and the risk of breast status. Cancer Epidemiol Biomarkers Prev. 2005;
cancer. JAMA. 1999;281:1632–1637. 14:2004 –2008.
25. Rohan TE, Jain MG, Howe GR, Miller AB. Dietary 40. Zintzaras E. Methylenetetrahydrofolate reductase
folate consumption and breast cancer risk. J Natl gene and susceptibility to breast cancer: a meta-
Cancer Inst. 2000;92:266 –269. analysis. Clin Genet. 2006;69:327–336.
26. Sellers TA, Kushi LH, Cerhan JR, et al. Dietary folate 41. Baggott JE, Vaughn WH, Juliana MM, Eto I, Krum-
intake, alcohol, and risk of breast cancer in a pro- dieck CL, Grubbs CJ. Effects of folate deficiency
spective study of postmenopausal women. Epide- and supplementation on methylnitrosourea-induced
miology. 2001;12:420 – 428. rat mammary tumors. J Natl Cancer Inst. 1992;84:
27. Cho E, Spiegelman D, Hunter DJ, et al. Premeno- 1740 –1744.
pausal intakes of vitamins A, C, and E, folate, and 42. Kotsopoulos J, Sohn KJ, Martin R, et al. Dietary
carotenoids, and risk of breast cancer. Cancer Epi- folate deficiency suppresses N-methyl-N-nitro-
demiol Biomarkers Prev. 2003;12:713–720. sourea-induced mammary tumorigenesis in rats.
28. Feigelson HS, Jonas CR, Robertson AS, McCul- Carcinogenesis. 2003;24:937–944.
lough ML, Thun MJ, Calle EE. Alcohol, folate, me- 43. Kotsopoulos J, Medline A, Renlund R, et al. Effects
thionine, and risk of incident breast cancer in the of dietary folate on the development and progres-
American Cancer Society Cancer Prevention Study sion of mammary tumors in rats. Carcinogenesis.
II Nutrition Cohort. Cancer Epidemiol Biomarkers 2005;26:1603–1612.
Prev. 2003;12:161–164. 44. Mehta RG. Experimental basis for the prevention of
29. Baglietto L, English DR, Gertig DM, Hopper JL, breast cancer. Eur J Cancer. 2000;36:1275–1282.
Giles GG. Does dietary folate intake modify effect of 45. Stolzenberg-Solomon RZ, Chang SC, Leitzmann
alcohol consumption on breast cancer risk? Pro- MF, et al. Folate intake, alcohol use, and postmeno-
spective cohort study. BMJ. 2005;331:807. pausal breast cancer risk in the Prostate, Lung,
30. Tjonneland A, Christensen J, Olsen A, et al. Folate Colorectal, and Ovarian Cancer Screening Trial.
intake, alcohol and risk of breast cancer among Am J Clin Nutr. 2006;83:895–904.
474 Nutrition Reviews姞, Vol. 64, No. 10
46. Rebbeck TR, Ambrosone CB, Bell DA, et al. SNPs, acute myocardial infarction. N Engl J Med. 2006;
haplotypes, and cancer: applications in molecular 354:1578 –1588.
epidemiology. Cancer Epidemiol Biomarkers Prev. 55. Lonn E, Yusuf S, Arnold MJ, et al. Homocysteine
2004;13:681– 687. lowering with folic acid and B vitamins in vascular
47. Giovannucci E. Epidemiologic studies of folate and disease. N Engl J Med. 2006;354:1567–1577.
colorectal neoplasia: a review. J Nutr. 2002;132: 56. Charles D, Ness AR, Campbell D, Davey Smith G,
2350S–2355S. Hall MH. Taking folate in pregnancy and risk of
48. Kim YI. Role of folate in colon cancer development maternal breast cancer. BMJ. 2004;329:1375–1376.
and progression. J Nutr. 2003;133:3731S–3739S. 57. Farber S. Some observations on the effect of folic
49. Cole BF, Baron JA, Sandler RS, et al. A randomized acid antagonists on acute leukemia and other forms
trial of folic acid to prevent colorectal adenomas. of incurable cancer. Blood. 1949;4:160 –167.
Proc Am Assoc Cancer Res. 2005;46:4399. 58. French AE, Grant R, Weitzman S, et al. Folic acid food
fortification is associated with a decline in neuroblas-
50. Choi SW, Mason JB. Folate status: effects on path-
toma. Clin Pharmacol Ther. 2003;74:288 –294.
ways of colorectal carcinogenesis. J Nutr. 2002;
59. Lucock M, Yates Z. Folic acid - vitamin and pana-
132:2413S–2418S.
cea or genetic time bomb? Nat Rev Genet. 2005;6:
51. Lamprecht SA, Lipkin M. Chemoprevention of colon 235–240.
cancer by calcium, vitamin D and folate: molecular 60. Ulrich CM, Potter JD. Folate supplementation: too
mechanisms. Nat Rev Cancer. 2003;3:601– 614. much of a good thing? Cancer Epidemiol Biomark-
52. Waterland RA, Jirtle RL. Transposable elements: ers Prev. 2006;15:189 –193.
targets for early nutritional effects on epigenetic 61. Song J, Medline A, Mason JB, Gallinger S, Kim YI.
gene regulation. Mol Cell Biol. 2003;23:5293–5300. Effects of dietary folate on intestinal tumorigenesis
53. Cooney CA, Dave AA, Wolff GL. Maternal methyl in the apcMin mouse. Cancer Res. 2000;60:5434 –
supplements in mice affect epigenetic variation and 5440.
DNA methylation of offspring. J Nutr. 2002;132: 62. Song J, Sohn KJ, Medline A, Ash C, Gallinger S, Kim
2393S–2400S. YI. Chemopreventive effects of dietary folate on
54. Bonaa KH, Njolstad I, Ueland PM, et al. Homo- intestinal polyps in Apc⫹/-Msh2-/- mice. Cancer
cysteine lowering and cardiovascular events after Res. 2000;60:3191–3199.
Nutrition Reviews姞, Vol. 64, No. 10 475
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Treating Emotional TraumaDocument556 pagesTreating Emotional TraumaPaco Ladera100% (3)
- Path Endocrine OutlineDocument46 pagesPath Endocrine Outlineaya derweshNo ratings yet
- Food Technology IiDocument212 pagesFood Technology IiKhaled Abu-Alruz100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Advantage of Ecological System TheoryDocument2 pagesAdvantage of Ecological System TheoryRonnie Serrano Pueda100% (2)
- Summative Test - FROM CELL TO ORGANISMDocument2 pagesSummative Test - FROM CELL TO ORGANISMroelpabelonia50% (2)
- EMSC5103 Assignment - Sustainable ConstructionDocument156 pagesEMSC5103 Assignment - Sustainable ConstructionIzam Muhammad100% (2)
- (PPT) Environmental Impacts of DamDocument17 pages(PPT) Environmental Impacts of DamKristine May Maturan100% (1)
- PermeabilidadDocument6 pagesPermeabilidadpilarerasoNo ratings yet
- Dietary Supplement Use in Ambulatory Cancer Patients: A Survey On Prevalence, Motivation and AttitudesDocument9 pagesDietary Supplement Use in Ambulatory Cancer Patients: A Survey On Prevalence, Motivation and AttitudespilarerasoNo ratings yet
- Regulationofimmune Functionbyvitamindand ItsuseindiseasesofimmunityDocument34 pagesRegulationofimmune Functionbyvitamindand ItsuseindiseasesofimmunitypilarerasoNo ratings yet
- Hutchinson 2010Document10 pagesHutchinson 2010pilarerasoNo ratings yet
- Mali Hi 2018Document7 pagesMali Hi 2018pilarerasoNo ratings yet
- Intelligence PDFDocument8 pagesIntelligence PDFab2409348No ratings yet
- GCE AS/A Level 1071/01 Biology/Human Biology - By1: A.M. MONDAY, 16 May 2011 1 HoursDocument12 pagesGCE AS/A Level 1071/01 Biology/Human Biology - By1: A.M. MONDAY, 16 May 2011 1 Hoursramloghun veerNo ratings yet
- Virus Resistant Papaya in Hawaii PDFDocument28 pagesVirus Resistant Papaya in Hawaii PDFRobert WagnerNo ratings yet
- Nutrition FSMDocument45 pagesNutrition FSMHema DeepikaNo ratings yet
- DocDocument43 pagesDocSachin Ranganath (RNK)No ratings yet
- Nobel Laureates in Chemistry: by Prof. Pahup Singh Department of Chemistry University of Rajasthan Jaipur-302004Document118 pagesNobel Laureates in Chemistry: by Prof. Pahup Singh Department of Chemistry University of Rajasthan Jaipur-302004Deepak PainulyNo ratings yet
- No. 167, Vol.2, No.4, 9720980, RJC-499Document9 pagesNo. 167, Vol.2, No.4, 9720980, RJC-499Salih OzerNo ratings yet
- Photosynthesis Post-Lab WorksheetDocument6 pagesPhotosynthesis Post-Lab WorksheetharrisonNo ratings yet
- Pharmacology NotesDocument4 pagesPharmacology NotesKristoffer VelezNo ratings yet
- Freelesson1endhairloss EulastversionDocument7 pagesFreelesson1endhairloss EulastversionDezant MiradzNo ratings yet
- 1-Dialysis Activity 2021Document4 pages1-Dialysis Activity 2021Marwa AliNo ratings yet
- Filtration Rate of The Blue Mussel, Mytilus Edulis, During Exposure To Various Diet TreatmentsDocument30 pagesFiltration Rate of The Blue Mussel, Mytilus Edulis, During Exposure To Various Diet TreatmentsMarissa McNallyNo ratings yet
- Respiration in ArthropodaDocument36 pagesRespiration in Arthropodadark.phoenix91124No ratings yet
- Medical Physics - Pulsed Short Wave DiathermyDocument25 pagesMedical Physics - Pulsed Short Wave DiathermyMuhammad AmmazNo ratings yet
- Animal Tissue Concept Map: Epithelial Tissue Connective TissueDocument1 pageAnimal Tissue Concept Map: Epithelial Tissue Connective TissueRowan LoveriaNo ratings yet
- Springer, Royal Swedish Academy of Sciences AmbioDocument4 pagesSpringer, Royal Swedish Academy of Sciences AmbioKlaus RiedeNo ratings yet
- Oil Pulling As An Adjunct To Scaling and Root Planing: A Clinico-Microbial StudyDocument7 pagesOil Pulling As An Adjunct To Scaling and Root Planing: A Clinico-Microbial StudyinventionjournalsNo ratings yet
- COVID-19 Information: Ncbi S Kip To Main Content S Kip To Navigation Resources How To A Bout NCBI AccesskeysDocument5 pagesCOVID-19 Information: Ncbi S Kip To Main Content S Kip To Navigation Resources How To A Bout NCBI AccesskeyscatheirneNo ratings yet
- Soc - Sci - Med 1998 Barkre 1067 1076 PDFDocument10 pagesSoc - Sci - Med 1998 Barkre 1067 1076 PDFWaoNo ratings yet
- BC-6800 BrochureDocument17 pagesBC-6800 BrochureDwiyan FitraNo ratings yet
- Types of FracturesDocument50 pagesTypes of FracturesMariah Rosette Sison HandomonNo ratings yet
- Introduccion LRmix StudioDocument21 pagesIntroduccion LRmix StudiofutbolizadoNo ratings yet
- Adolescence Adolescence (From Latin Adolescere, Meaning 'To Grow Up') Is A Transitional StageDocument8 pagesAdolescence Adolescence (From Latin Adolescere, Meaning 'To Grow Up') Is A Transitional StageLawalNo ratings yet