Professional Documents
Culture Documents
Decompressive Craniectomy in Children With Severe Traumatic Brain Injury: A Multicenter Retrospective Study and Literature Review
Uploaded by
Sebastian SalvadorOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Decompressive Craniectomy in Children With Severe Traumatic Brain Injury: A Multicenter Retrospective Study and Literature Review
Uploaded by
Sebastian SalvadorCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/332796278
Decompressive Craniectomy in Children with Severe Traumatic Brain Injury: A
Multicenter Retrospective Study and Literature Review
Article in World Neurosurgery · May 2019
DOI: 10.1016/j.wneu.2019.04.215
CITATIONS READS
4 53
23 authors, including:
Manfiotto Marie Giovanna Paternoster
Centre Hospitalier Universitaire de Nice Catholic University of the Sacred Heart
4 PUBLICATIONS 30 CITATIONS 22 PUBLICATIONS 373 CITATIONS
SEE PROFILE SEE PROFILE
Matthieu Vinchon Carmine Mottolese
Université de Lille Hospices Civils de Lyon (Centre Hospitalier Universitaire de Lyon)
220 PUBLICATIONS 3,999 CITATIONS 269 PUBLICATIONS 4,007 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
pineal region tumors View project
rare craniomaxillofacial malformations View project
All content following this page was uploaded by Pierre-Aurélien Beuriat on 28 February 2020.
The user has requested enhancement of the downloaded file.
Original Article
Decompressive Craniectomy in Children with Severe Traumatic Brain Injury: A
Multicenter Retrospective Study and Literature Review
Marie Manfiotto1, Kevin Beccaria2, Alice Rolland3, Giovanna Paternoster2, Benjamin Plas4, Sergio Boetto4,
Mathieu Vinchon5, Carmine Mottolese6, Pierre-Aurélien Beuriat6, Alexandru Szathmari6, Federico Di Rocco6,
Didier Scavarda7, Eric Seigneuret8, Isabelle Wrobleski8, Olivier Klein9, Antony Joud9, Edouard Gimbert10,
Vincent Jecko10, Jean Rodolphe Vignes10, Thomas Roujeau3, Audrey Dupont11, Michel Zerah2, Michel Lonjon1
- BACKGROUND: Severe traumatic brain injury (TBI) is this surgery in the management of children with severe
the most common cause of disability in children. Refractory TBI.
increased intracranial pressure can be a therapeutic
challenge. Decompressive craniectomy can be proposed
when medical management is insufficient, but its place is
not clearly defined in guidelines. The aim of this study was
to identify prognostic factors in children with TBI. INTRODUCTION
- METHODS: We performed a retrospective, multicenter
study to analyze long-term outcomes of 150 children with
severe TBI treated by decompressive craniectomy and to
identify prognostic factors.
T raumatic brain injury (TBI) is the leading cause of
morbidity and mortality in children. In addition, survivors
of pediatric TBI may have cognitive and behavioral
dysfunction that impairs their ability to reintegrate into social
environments. Both the primary brain injury and the management
of secondary brain injury are important in determining outcomes
- RESULTS: A satisfactory neurologic evolution (repre-
of pediatric TBI. Many studies have demonstrated that high
sented by a King’s Outcome Scale for Childhood Head
intracranial pressure (ICP) is associated with increased mortality.
Injury score >3) was observed in 62% of children with a When pharmacologic management of ICP fails, it is unclear
mean follow-up of 3.5 years. Mortality rate was 17%. whether there is a benefit from decompressive craniectomy (DC).
Prognostic factors associated with outcome were age, In the adult population, DC may prove to be beneficial for pa-
initial Glasgow Coma Scale score, presence of mydriasis, tients with stroke; however, for adults with TBI, there is no proven
neuromonitoring values (maximal intracranial pressure >30 benefit compared with maximal medical management. In the
mm Hg), and radiologic findings (Rotterdam score ‡4). pediatric population, Taylor et al.1 conducted a randomized trial of
DC versus maximal medical management for medically refractory
- CONCLUSIONS: This study in a large population con- intracranial hypertension and reported a potential benefit of early
firms that children with severe TBI treated by decom- DC. This benefit is supported by 17 retrospective studies
pressive craniectomy can achieve a good neurologic (Table 1).1-17 Guidelines recommend consideration of DC in pe-
outcome. Further studies are needed to clarify the use of diatric patients showing early signs of neurologic deterioration,
Key words From the 1Service de Neurochirurgie, CHU de Nice, Nice; 2Service de Neurochirurgie
- Brain injuries Pédiatrique, Hôpital Necker, Paris; 3Service de Neurochirurgie, CHU de Montpellier,
- Child Montpellier; 4Service de Neurochirurgie, CHU de Toulouse, Toulouse; 5Service de
- Decompressive craniectomy Neurochirurgie, CHU de Lille, Lille; 6Service de Neurochirurgie Pédiatrique, Hôpital Femme
- Traumatic
Mère Enfant, Lyon; 7Service de Neurochirurgie Pédiatrique, Hôpital Timone, Marseille;
8
Service de Neurochirurgie Pédiatrique, CHU Grenoble, Grenoble; 9Service de Neurochirurgie
Abbreviations and Acronyms Pédiatrique, CHU Nancy, Nancy; 10Service de Neurochirurgie Pédiatrique, CHU Bordeaux,
Bordeaux; and 11Service de Réanimation Pédiatrique, Hôpital Lenval, Nice, France
DC: Decompressive craniectomy
GCS: Glasgow Coma Scale To whom correspondence should be addressed: Marie Manfiotto, M.D.
GOS: Glasgow Outcome Scale [E-mail: marie.manfiotto@hotmail.com]
ICH: Intracranial hypertension Citation: World Neurosurg. (2019) 129:e56-e62.
ICP: Intracranial pressure https://doi.org/10.1016/j.wneu.2019.04.215
KOSCHI: King’s Outcome Scale for Childhood Head Injury Journal homepage: www.journals.elsevier.com/world-neurosurgery
TBI: Traumatic brain injury
Available online: www.sciencedirect.com
1878-8750/$ - see front matter ª 2019 Elsevier Inc. All rights reserved.
e56 www.SCIENCEDIRECT.com WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2019.04.215
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
Table 1. Literature Review
No DC/ Mean Age Mean Follow-Up Favorable Mortality
Reference Control (years) Study Type (months)* Evaluation Criteria Outcome (%) Rate (%)
Dam Hieu et al., 19962 2 8 Case report 8 Recovery of autonomy 100 0
Polin et al., 19973 18 ND Retrospective controlled ND Good recovery 44 ND
study
Taylor et al., 20011 14/27 10 Prospective randomized 7.5 GOS and HUS at 6 54 23
study months
Simma et al., 20024 8 10 Case report ND GOS score >3 75 25
5
Figaji et al. 2003 5 8 Case report 28.4 (14e42) GOS score >3 100 0
6
Ruf et al., 2003 6 7.8 Case report 6 Normal neurologic status 50 0
Josan and Sgouros, 6 13 Case report >1 year GOS score >3 100 0
20067
Kan et al., 20068 6/45 6.6 Retrospective controlled 18.6 KOSCHI score >3 17 83
study
Rutigliano et al., 20069 6 14.5 Case report ND FIM ambulation and 83 0
feeding
Jagannathan et al., 23 11.9 Prospective study 62 (11e126) GOS score >3 65 30
200710
Adamo et al., 200911 7 1.15 Case report (1.5e24) KOSCHI score >3 57 0
Thomale et al., 201012 14/39 8.41 Prospective study 62.4 (12e126) GOS score >3 86 20
Guresir et al., 201213 34 13 Retrospective study ND Rankin Scale score 44 ND
14
Oluigbo et al., 2012 37 6 Prospective study ND KOSCHI score >3 60 16
Khan et al., 201415 25 6 Retrospective study 5 GOS score >3 64 36
Mhanna et al., 201416 7/17 10.2 Retrospective study 48 GOS score >3 42 29
Beuriat et al., 201517 55 7.4 Retrospective study 54 Independent daily life 80 18
ND, not determined; GOS, Glasgow Outcome Scale; HUS, health state utility index; KOSCHI, King’s Outcome Scale for Childhood Head Injury; FIM, Functional Independence Measurement.
*Ranges in parentheses.
herniation, or developing intracranial hypertension (ICH) re- a score !3 were the bad prognosis group (group B). Afterward, we
fractory to medical management. However, long-term clinical compared initial clinical and radiologic data between both groups
outcomes after DC have not been widely studied. In this study, we to identify prognostic factors. Computed tomography scans were
analyzed the long-term neurologic outcomes of children with analyzed by a single radiologist to avoid interpretation bias. We
severe TBI treated by DC in France to identify prognosis factors. used the Rotterdam score19 to summarize the different lesions for
its reproducibility and because we believe that the radiologic score
best takes in account cerebral edema, which is a common lesion in
MATERIALS AND METHODS children with severe TBI.20
Our local ethics committee approved this study, and we obtained The Shapiro-Wilk test was used to analyze data distribution.
consent of the families of the patients to be part of the study.We Normally distributed data were compared using the Student t test,
retrospectively analyzed 150 records of children (<18 years old) and nonenormally distributed data were compared using the
with severe TBI treated by DC at 10 French neuropediatric centers Mann-Whitney test. Qualitative data were compared using the c2
between January 2006 and December 2016. We excluded non- test and Fisher exact test. The significance level was set at 5%.
accidental trauma, rupture of an arteriovenous malformation, and Statistical analyses were performed using XLSTAT software
vascular dissection previous to or concomitant with the trauma. (Addinsoft Inc., Long Island City, New York, USA).
The primary endpoint was the neurologic outcome at last follow-
up as evaluated by the King’s Outcome Scale for Childhood Head RESULTS
Injury (KOSCHI) score (Figure 1).18
We separated patients into 2 groups according to their long- Epidemiologic Data
term neurologic status. Patients with KOSCHI score >3 were We included 150 patients from 10 centers. There were 103 boys and
considered the good prognosis group (group A), and patients with 47 girls (male/female ratio: 2.1/1). The mean age was 10.75 years
WORLD NEUROSURGERY 129: e56-e62, SEPTEMBER 2019 www.journals.elsevier.com/world-neurosurgery e57
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
Figure 1. King’s Outcome Scale for Childhood Head Rossiter L, Colaco T, Forsyth R. A practical outcome
Injury score categories. KOSCHI, King’s Outcome scale for paediatric head injury. Arch Dis Child.
Scale for Childhood Head Injury; PTSD, posttraumatic 2001;84:120-124.18)
stress disorder. (Reprinted from Crouchman M,
e58 www.SCIENCEDIRECT.com WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2019.04.215
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
(range, 0.63e17.94 years) with significantly younger patients in
group B (9.6 years vs. 11.4 years in group A) (P ¼ 0.0456).
KOSCHI Categories
Neurologic Outcome 3%
During the initial hospitalization (0e49 days), 23 patients died, 13% 17% KOSCHI 1
mostly during the first week after trauma. One more patient died 5 4% KOSCHI 2
KOSCHI 3a
years after trauma during surgery for splenorenal anastomosis. Eleven 6%
KOSCHI 3b
patients were lost to follow-up. The total mortality rate was 17.2%. 27%
10% KOSCHI 4a
Among the 115 survivors available for follow-up (mean 3.55 years KOSCHI 4b
[range, 0.09e12.96 years]), 87 patients (75.6%) had a KOSCHI 20% KOSCHI 5a
score >3 and were included in group A, and 28 patients (24.4%) KOSCHI 5b
had a KOSCHI score between 2 and 3 and were included in group
B. Deceased patients were also included in group B (Figure 2).
Figure 2. King’s Outcome Scale for Childhood Head Injury score
distribution. KOSCHI, King’s Outcome Scale for Childhood Head Injury.
Initial Clinical Data
The median initial Glasgow Coma Scale (GCS) score was 6 (range,
3e15) and was significantly lower in group B (median score ¼ 4 Surgical Complications
[range, 3e15]) compared with group A (median score ¼ 7 [range, Apart from conditions commonly observed in patients admitted to
3e15]) (P ¼ 0.003). As expected, the initial GCS score strongly the intensive care unit (e.g., urinary tract infection, pneumonia),
impacted the prognosis. Initial GCS score !6 was significantly 21% of patients had a surgical complication. Six (4%) patients had
associated with a poor neurologic outcome (P ¼ 0.009). Pre- meningitis, and 14 (9.3%) patients developed a wound infection.
hospital pupillary abnormalities were found in 47 patients (31.4%): Empyema was found in 3 (2%) patients. One patient with an
26 with anisocoria and 21 with bilateral mydriasis. This finding external ventricular drain developed a cerebral abscess. Meningitis
was significantly associated with bad prognosis (P ¼ 0.027). On was the only complication significantly related to bad prognosis
admission to the intensive care unit, 36 patients had a pupillary (P ¼ 0.03). Ten patients presented with hemorrhagic complica-
abnormality (24%): 24 with anisocoria and 12 with bilateral tions (4 epidural hematomas, 4 subdural hematomas, 1 intra-
mydriasis. Pupillary abnormality at admission was also associated parenchymal hematoma, and 1 intraventricular hemorrhage after
with bad prognosis (P ¼ 0.002). ventriculoperitoneal shunt placement).
ICP Monitoring
DISCUSSION
ICP was monitored in 70 patients. The mean initial ICP value (i.e.,
the first value recorded after placement of the monitor) was 31 mm In this series, we demonstrate good long-term outcome (mean
Hg (range, 2e90 mm). The mean maximal ICP value (i.e., the follow-up 3.5 years) in 62% of children with severe TBI treated
highest value recorded before surgery) was 41 mm Hg (range, 5e100 with DC and a mortality rate of 17%. These results are similar to
mm Hg). Maximal ICP >30 mm Hg was associated with a bad results observed in previous series. Mortality rates varied between
prognosis (P ¼ 0.0280), especially if the threshold was 40 mm Hg 0% and 36% in different publications.5,7,8,11 Most of these studies
(P ¼ 0.006). Finally, the best ICP value related to the long-term describe good neurologic outcomes in >50% of children with
outcome was postoperative ICP. The mean postoperative ICP severe TBI who underwent DC.1-17,21-25 However, the low numbers
decreased to 10 mm Hg in group A but remained high at 30 mm Hg of subjects (range, 2e55) as well as the single-center and retro-
in group B (P ¼ 0.0000012). We considered the threshold of post- spective nature of most of these studies do not allow statistically
operative ICP >15 mm Hg as a bad prognostic factor (P ¼ 0.0003). significant results. They are mostly case studies or series. Beuriat
et al.17 reported good neurologic outcomes for 65% of patients.
The main assessment criterion also varies among studies. It is
Radiologic Data often subjective (i.e., not based on a formal evaluation or using
There were 81 preoperative computed tomography scans available a reproducible and validated tool). In the study by Polin et al.,3
for analysis. The radiologic parameters that statistically correlated the evaluation criterion was a favorable neurologic progression,
with bad prognosis were Rotterdam score (P ¼ 0.001), absence of which was reported to be the case for 47% of children.
cisterns (P ¼ 0.0002), and median shift >5 mm (P ¼ 0.019). According to Ruf et al.,6 the neurologic condition is considered
normal for 50% of children who sustained a severe TBI that
Surgical Data required a DC.
The mean elapsed time between trauma and surgery was 1.45 days More recent series are based on the Glasgow Outcome Scale
(range, 0e9 days). There was no evident correlation between the delay (GOS)1,4,5,7,10,12,15,16 or KOSCHI score.8,11,14 We decided to use the
of surgery and prognosis (P ¼ 0.2857). Hemicraniectomy was per- KOSCHI score to evaluate long-term functional neurologic out-
formed in 124 patients (83%), mostly in cases of unilateral lesions comes, as we consider it more suitable for the pediatric population
with median shift, and bifrontal craniectomy was performed in the 26 and more discriminatory.26 Five studies compared outcomes with
(17%) remaining patients who presented with diffuse edema without a control group.3,8,11,12,15 Josan and Sgouros7 reported satisfactory
median shift. The technique did not impact the prognosis. neurologic outcomes (1-year GOS score #4) in 100% of children
WORLD NEUROSURGERY 129: e56-e62, SEPTEMBER 2019 www.journals.elsevier.com/world-neurosurgery e59
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
with craniectomy compared with 50% in the control group; the There were 80 computed tomography scans available for the
mortality rates were 0% and 33%, respectively. Thomale et al.12 analysis. Only a few pediatric series have studied the impact of DC
used the same assessment criteria and noted that only 50% of in children after assessing radiologic lesions with a validated
the patients had a 1-year GOS score #4, with a mortality rate of score. Cerebral edema, which is the most frequent lesion in
21% in the craniectomy group. In a retrospective case-controlled children with TBI (2e5 times more common in children compared
study of 34 patients, Mhanna et al.16 concluded that although with adults), used to be associated with bad prognosis.19,33
DC does not impact the survival of patients with TBI, it does However, in patients treated with DC, children seem to have a
considerably change the neurologic progression, with 42% of more favorable outcome than adults, even with diffuse post-
patients achieving a GOS score of 5 in the surgical group traumatic brain edema. Therefore, we think that DC is particularly
compared with 0% in the control group. Only one study was effective in this situation, and indications for this surgery must be
carried out in a prospective and randomized manner.1 The considered after analyzing the degree of brain edema.
authors showed that patients who underwent a DC had a Not all studies described DC surgical protocols, and none of the
favorable neurologic progression in 54% of cases compared with studies compared different techniques. In the prospective ran-
14% in the control group (P ¼ 0.046). However, the statistical domized study of Taylor et al.,1 a temporal craniectomy was
significance of this study can be questioned because the performed without opening the dura mater. In other pediatric
threshold was lowered to 0.0022 to account for multiple series, the technique and size of the craniectomy depended on
analyses. Moreover, although the study was prospective and the lesion side and presence of cerebral edema.
randomized, it was only a pilot study with no calculation of the Our emphasis was on identifying the optimal timing for
required number of participants carried out a priori. Although it decompression. According to the different studies, the time frame
yielded encouraging results, it does not provide sufficient varies from a few hours to several days. Nevertheless, all pediatric
evidence to make formal conclusions about the indications for DC. series evaluating the benefit of DC in children with cranial trauma
Studies have suggested that children with TBI treated by DC agree on early surgery (within 48 hours after the trauma) to avoid the
have better outcomes than adults owing to greater cerebral plas- adverse effects of ICH.1,12,22 Few groups have been able to demon-
ticity and a lack of systemic comorbidities.3 Controversy remains, strate a significant effect of surgical delay on neurologic outcome.
however, and results within the pediatric population are Josan and Sgouros7 showed that DC surgery within 24 hours of
contradictory. Some authors report worse results, especially trauma was associated with better outcomes compared with the
among older children, whereas others claim that the high control group. Figaji et al.5 also reported better results in children
vulnerability of the developing brain leads to irreversible damage with early decompression. For Polin et al.,3 DC performed after
in infants.27 Güresir et al.13 found no obvious difference in the second day after trauma was a poor prognostic factor.
terms of long-term outcomes in children according to their age Our surgical complication rate was 21%. In previous series, the
group (!2 years, 2e6 years, 6e12 years, and 12e18 years). In our complication rate ranged from 0% to 47%. The difference in
series, patients with bad prognosis (group B) were significantly complication rates could be due to definition differences. We
younger (P ¼ 0.0456), but we failed to define an age that would be analyzed the specific complications associated with surgery rather
a suitable threshold. We had only a few patients <2 years (n ¼ 12) than the overall complications. We observed hemorrhagic compli-
because we excluded nonaccidental trauma, which accounts for cations in 10 patients. Whether extradural or subdural, approxi-
most of the etiologies in this age group. mately 75% were contralateral to the craniectomy. Based on this, we
A low initial GCS score in TBI is known to be a poor prognostic propose that DC can decompensate contralateral lesions. Other
factor. In our series, the GCS score was statistically correlated with complications were predominantly infectious and were reported in
neurologic outcomes (P ¼ 0.0003). Other pediatric series on DCs 25 (17%) patients. Meningitis occurred in 6 (4%) patients. Cere-
concluded that low GCS score was significantly associated with poor brospinal fluid leakage from the scar was observed in 4 patients, but
outcomes.15 In other series, GCS score was not correlated with none of them had meningitis. In contrast, 14 (9.3%) patients had
outcome.12,13 The GCS score is difficult to assess in pediatric pa- scar infections, 3 of whom developed meningitis. Three patients
tients, especially if the GCS is not administered by a specialized developed empyema. A patient with an external ventricular drain
pediatric team.28-30 This is why our series did not include numerical developed a cerebral abscess. Only the occurrence of meningitis was
GCS scores for 8 patients; rather, the state of consciousness of the associated with neurologic outcome (P ¼ 0.03). Few series describe
patient was described as coma or agitated coma. infectious complications. Kan et al.8 reported an 8.6% rate of
Several studies reported that pupillary anomaly in TBI is asso- infectious complications. This was similar to the 9% rate
ciated with poor prognosis.31,32 We confirmed that the presence of described by Beuriat et al.17 Jagannathan et al.10 described only 1
a unilateral or bilateral mydriasis was strongly associated with case of meningitis in their series of 23 patients.
poor prognosis, especially if it persisted after resuscitation ma- Among frequently described complications, the persistence of a
neuvers. However, in 16 patients with initial mydriasis, 6 (37.5%) cerebrospinal fluid resorption disorder (hydrocephalus or
had a favorable neurologic outcome with a KOSCHI score of 4a or hygroma) was reported in 40% of cases in the series by Khan
4b. In the series by Güresir et al.,13 60% of patients with unilateral et al.15 Beuriat et al.17 reported a 16% rate of subdural collections
mydriasis and 45% of patients with bilateral mydriasis had a requiring subduroperitoneal shunting, and 10% of patients
favorable neurologic outcome. required ventriculoperitoneal derivation. The presence of an
e60 www.SCIENCEDIRECT.com WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2019.04.215
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
external ventricular drain increases the risk of developing this having good neurologic progression) and low rates of compli-
complication, especially in patients with TBI treated with DC. It cations in the medium term, despite serious pathology. The
was discussed that DC, all the more so when associated with a overall risk/benefit ratio indicates that this surgical intervention
duraplasty, could alter cerebrospinal fluid hydrodynamics. is often warranted. Managing refractory ICH remains contro-
versial and varies by center and surgeon training and experience.
CONCLUSIONS Children have a long life expectancy, making it important to
No study has been able to adequately demonstrate the benefit of provide them with suitable and intensive treatment. The benefit
DC in children with severe TBI. Our study did not include a of including DC in the therapeutic arsenal for refractory ICH
comparison group, which precludes us from reaching a warrants a thorough investigation. A prospective randomized
conclusion about the effectiveness of this intervention. Several study with univariate and multivariate analyses may allow iden-
authors have reported good outcomes with children (50%e60% tification of better candidates for DC.
11. Adamo MA, Drazin D, Waldman JB. Decom- 20. Bruce DA, Alavi A, Bilaniuk L, Dolinskas C,
REFERENCES pressive craniectomy and postoperative complica- Obrist W, Uzzell B. Diffuse cerebral swelling
tion management in infants and toddlers with following head injuries in children: the syndrome
1. Taylor A, Butt W, Rosenfeld J, et al. A randomized
severe traumatic brain injuries. J Neurosurg Pediatr. of “malignant brain edema”. J Neurosurg. 1981;54:
trial of very early decompressive craniectomy in
2009;3:334-339. 170-178.
children with traumatic brain injury and sustained
intracranial hypertension. Childs Nerv Syst. 2001;17:
12. Thomale UW, Graetz D, Vajkoczy P, 21. Cambra FJ, Palomeque A, Muñoz-Santanach D,
154-162.
Sarrafzadeh AS. Severe traumatic brain injury in Segura Matute S, Navarro Balbuena R, García
children—a single center experience regarding Fructuoso G. Use of decompressive craniectomy
2. Dam Hieu P, Sizun J, Person H, Besson G. The
therapy and long-term outcome. Childs Nerv Syst. in the management of refractory intracranial hy-
place of decompressive surgery in the treatment of
2010;26:1563-1573. pertension in paediatric patients [in Spanish] An
uncontrollable post-traumatic intracranial hyper-
tension in children. Childs Nerv Syst. 1996;12: Pediatr (Barc). 2010;73:12-18.
13. Güresir E, Schuss P, Seifert V, Vatter H. Decom-
270-275.
pressive craniectomy in children: single-center 22. Skoglund TS, Eriksson-Ritzén C, Jensen C,
3. Polin RS, Ayad M, Jane JA. Decompressive cra- series and systematic review. Neurosurgery. 2012; Rydenhag B. Aspects on decompressive craniec-
niectomy in pediatric patients. Crit Care. 2003;7: 70:881-888 [discussion: 888-889]. tomy in patients with traumatic head injuries.
409-410. J Neurotrauma. 2006;23:1502-1509.
14. Oluigbo CO, Wilkinson CC, Stence NV, Fenton LZ,
4. Simma B, Tscharre A, Hejazi N, Krasznai L, Fae P. McNatt SA, Handler MH. Comparison of outcomes 23. Jacob AT, Heuer GG, Grant R, et al. Decom-
Neurologic outcome after decompressive cra- following decompressive craniectomy in children pressive hemicraniectomy for pediatric traumatic
niectomy in children. Intensive Care Med. 2002;28: with accidental and nonaccidental blunt cranial brain injury: long-term outcome based on quality
1000. trauma. J Neurosurg Pediatr. 2012;9:125-132. of life. Pediatr Neurosurg. 2011;47:81-86.
5. Figaji AA, Fieggen AG, Peter JC. Early decom- 15. Khan SA, Shallwani H, Shamim MS, et al. Pre-
24. Hejazi N, Witzmann A, Fae P. Unilateral decom-
pressive craniotomy in children with severe trau- dictors of poor outcome of decompressive cra-
pressive craniectomy for children with severe
matic brain injury. Childs Nerv Syst. 2003;19: niectomy in pediatric patients with severe
brain injury. Report of seven cases and review of
666-673. traumatic brain injury: a retrospective single cen-
the relevant literature. Eur J Pediatr. 2002;161:
ter study from Pakistan. Childs Nerv Syst. 2014;30:
99-104.
6. Ruf B, Heckmann M, Schroth I, et al. Early 277-281.
decompressive craniectomy and duraplasty for 25. Appelboom G, Zoller SD, Piazza MA, et al. Trau-
refractory intracranial hypertension in children: 16. Mhanna MJ, Mallah WE, Verrees M, Shah R,
Super DM. Outcome of children with severe matic brain injury in pediatric patients: evidence
results of a pilot study. Crit Care. 2003;7:R133-R138. for the effectiveness of decompressive surgery.
traumatic brain injury who are treated with
decompressive craniectomy. J Neurosurg Pediatr. Neurosurg Focus. 2011;31:E5.
7. Josan VA, Sgouros S. Early decompressive cra-
niectomy may be effective in the treatment of re- 2015;16:508-514.
26. Calvert S, Miller HE, Curran A, et al. The King’s
fractory intracranial hypertension after traumatic
17. Beuriat PA, Javouhey E, Szathmari A, et al. Outcome Scale for Childhood Head Injury and
brain injury. Childs Nerv Syst. 2006;22:1268-1274.
Decompressive craniectomy in the treatment of injury severity and outcome measures in children
8. Kan P, Amini A, Hansen K, et al. Outcomes after post-traumatic intracranial hypertension in chil- with traumatic brain injury. Dev Med Child Neurol.
decompressive craniectomy for severe traumatic dren: our philosophy and indications. J Neurosurg 2008;50:426-431.
brain injury in children. J Neurosurg. 2006;105(5 Sci. 2015;59:405-428.
Suppl):337-342. 27. Anderson V, Catroppa C, Morse S, Haritou F,
18. Crouchman M, Rossiter L, Colaco T, Forsyth R. Rosenfeld J. Functional plasticity or vulnerability
9. Rutigliano D, Egnor MR, Priebe CJ, et al. A practical outcome scale for paediatric head after early brain injury? Pediatrics. 2005;116:
Decompressive craniectomy in pediatric patients injury. Arch Dis Child. 2001;84:120-124. 1374-1382.
with traumatic brain injury with intractable
elevated intracranial pressure. J Pediatr Surg. 2006; 19. Maas AI, Hukkelhoven CW, Marshall LF, 28. Balestreri M, Czosnyka M, Chatfield DA, et al.
41:83-87 [discussion: 83-87]. Steyerberg EW. Prediction of outcome in trau- Predictive value of Glasgow Coma Scale after
matic brain injury with computed tomographic brain trauma: change in trend over the past ten
10. Jagannathan J, Okonkwo DO, Dumont AS, et al. characteristics: a comparison between the years. J Neurol Neurosurg Psychiatr. 2004;75:161-162.
Outcome following decompressive craniectomy in computed tomographic classification and combi-
children with severe traumatic brain injury: a 10- nations of computed tomographic predictors. 29. Buechler CM, Blostein PA, Koestner A, Hurt K,
year single-center experience with long-term Neurosurgery. 2005;57:1173-1182 [discussion: 1173- Schaars M, McKernan J. Variation among trauma
follow up. J Neurosurg. 2007;106(4 Suppl):268-275. 1182]. centers’ calculation of Glasgow Coma Scale score:
WORLD NEUROSURGERY 129: e56-e62, SEPTEMBER 2019 www.journals.elsevier.com/world-neurosurgery e61
ORIGINAL ARTICLE
MARIE MANFIOTTO ET AL. DECOMPRESSIVE CRANIECTOMY IN CHILDREN
results of a national survey. J Trauma. 1998;45: 32. Andrews BT, Pitts LH. Functional recovery after commercial or financial relationships that could be construed
429-432. traumatic transtentorial herniation. Neurosurgery. as a potential conflict of interest.
1991;29:227-231.
Received 7 March 2019; accepted 24 April 2019
30. Moskopp D, Stähle C, Wassmann H. Problems of 33. Liesemer K, Riva-Cambrin J, Bennett KS, et al. Citation: World Neurosurg. (2019) 129:e56-e62.
the Glasgow Coma Scale with early intubated Use of Rotterdam CT scores for mortality risk https://doi.org/10.1016/j.wneu.2019.04.215
patients. Neurosurg Rev. 1995;18:253-257. stratification in children with traumatic brain
Journal homepage: www.journals.elsevier.com/world-
injury. Pediatr Crit Care Med. 2014;15:554-562.
neurosurgery
31. Prasad MR, Ewing-Cobbs L, Swank PR, Kramer L.
Available online: www.sciencedirect.com
Predictors of outcome following traumatic brain
injury in young children. Pediatr Neurosurg. 2002;36: Conflict of interest statement: The authors declare that the 1878-8750/$ - see front matter ª 2019 Elsevier Inc. All
64-74. article content was composed in the absence of any rights reserved.
e62 www.SCIENCEDIRECT.com WORLD NEUROSURGERY, https://doi.org/10.1016/j.wneu.2019.04.215
View publication stats
You might also like
- Cisternostomy: A Timely Intervention in Moderate To Severe Traumatic Brain Injuries: Rationale, Indications, and ProspectsDocument6 pagesCisternostomy: A Timely Intervention in Moderate To Severe Traumatic Brain Injuries: Rationale, Indications, and ProspectsAtul JainNo ratings yet
- (10920684 - Neurosurgical Focus) Traumatic Brain Injury in Pediatric Patients - Evidence For The Effectiveness of Decompressive SurgeryDocument8 pages(10920684 - Neurosurgical Focus) Traumatic Brain Injury in Pediatric Patients - Evidence For The Effectiveness of Decompressive SurgerySebastian SalvadorNo ratings yet
- NeuroblastomaDocument9 pagesNeuroblastomasamantha mccoyNo ratings yet
- Fneur 08 00685Document15 pagesFneur 08 00685AZZAHRA KARYA BULAN IRIANDANo ratings yet
- Echography and Doppler of the BrainFrom EverandEchography and Doppler of the BrainChiara RobbaNo ratings yet
- Assessing The Severity of Traumatic Brain Injury-Time For A Change?Document12 pagesAssessing The Severity of Traumatic Brain Injury-Time For A Change?Anonymous R6ex8BM0No ratings yet
- DIandbright SpotDocument10 pagesDIandbright SpotJamaluddin HaikhahNo ratings yet
- Clinical Trials For Pediatric Traumatic Brain Injury:: Definition of Insanity?Document9 pagesClinical Trials For Pediatric Traumatic Brain Injury:: Definition of Insanity?Genesis VelasteguiNo ratings yet
- Management of Concussion and Mild Traumatic Brain Injury: A Synthesis of Practice GuidelinesDocument12 pagesManagement of Concussion and Mild Traumatic Brain Injury: A Synthesis of Practice GuidelinesKomangNo ratings yet
- Traumatic Brain Injury 1: SeriesDocument13 pagesTraumatic Brain Injury 1: SeriesIntan HaddadNo ratings yet
- Severe Traumatic Brain Injury Targeted Management in The Intensive Care UnitDocument24 pagesSevere Traumatic Brain Injury Targeted Management in The Intensive Care UnitJuan Sebastian Rodriguez GarciaNo ratings yet
- Coppetal 2015 Nat Revs Disease Primers 20157Document67 pagesCoppetal 2015 Nat Revs Disease Primers 20157Nexi anessaNo ratings yet
- Ten Rules For The Management of Moderate and Severe Traumatic Brain Injury During Pregnancy: An Expert ViewpointDocument11 pagesTen Rules For The Management of Moderate and Severe Traumatic Brain Injury During Pregnancy: An Expert ViewpointKaren Campos GonzalezNo ratings yet
- Perioperative Management of The Pediatric Patient With Traumatic Brain InjuryDocument14 pagesPerioperative Management of The Pediatric Patient With Traumatic Brain InjuryBaha MirzaeifarNo ratings yet
- Handbook of Outpatient MedicineFrom EverandHandbook of Outpatient MedicineElana SydneyRating: 5 out of 5 stars5/5 (1)
- Pediatric Head Trauma: A Review and Update: Practice GapsDocument16 pagesPediatric Head Trauma: A Review and Update: Practice GapsnadiaNo ratings yet
- Tich Cepeda EtalDocument9 pagesTich Cepeda EtalIkki DongNo ratings yet
- Operative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesFrom EverandOperative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesAlexander Y. ShinNo ratings yet
- Clinical Cases in Psychiatry: Integrating Translational Neuroscience ApproachesFrom EverandClinical Cases in Psychiatry: Integrating Translational Neuroscience ApproachesAlfredo Carlo AltamuraNo ratings yet
- TBI ChildrenDocument21 pagesTBI ChildrenSayed AdelNo ratings yet
- Neurometabolic Hereditary Diseases of AdultsFrom EverandNeurometabolic Hereditary Diseases of AdultsAlessandro P. BurlinaNo ratings yet
- Nihms 1598170Document3 pagesNihms 1598170Mario SerranoNo ratings yet
- Central Nervous System MetastasesFrom EverandCentral Nervous System MetastasesManmeet AhluwaliaNo ratings yet
- Variation in Guideline Implementation and Adherence Regarding Severe Traumatic Brain Injury Treatment: A CENTER-TBI Survey Study in EuropeDocument6 pagesVariation in Guideline Implementation and Adherence Regarding Severe Traumatic Brain Injury Treatment: A CENTER-TBI Survey Study in EuropefinaNo ratings yet
- Trauma CraneoencefalicoDocument18 pagesTrauma CraneoencefalicoUCIADULTO UPEDNo ratings yet
- Abnormal Structural Connectivity in The Brain Networks of Children With HydrocephalusDocument11 pagesAbnormal Structural Connectivity in The Brain Networks of Children With HydrocephalusQuang NguyễnNo ratings yet
- Minimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachFrom EverandMinimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachGiorgio PietramaggioriNo ratings yet
- Personalization and Pragmatism - Pediatric Intracranial Pressure and Cerebral Perfusion Pressure Treatment ThresholdsDocument4 pagesPersonalization and Pragmatism - Pediatric Intracranial Pressure and Cerebral Perfusion Pressure Treatment ThresholdsdrdivyapukNo ratings yet
- Bayley ScalesDocument4 pagesBayley ScalesPame SniezhkinNo ratings yet
- Tirado-Bsn 4d-Journal Summary and ReflectionDocument3 pagesTirado-Bsn 4d-Journal Summary and ReflectionJeniper Marie Cute29No ratings yet
- Critical Care Nephrology and Renal Replacement Therapy in ChildrenFrom EverandCritical Care Nephrology and Renal Replacement Therapy in ChildrenAkash DeepNo ratings yet
- AranedaDocument10 pagesAranedafonoaudiologaclaudiafigueroaNo ratings yet
- Understanding The Relationship Between Cognitive Performance and Function in Daily Life After Traumatic Brain InjuryDocument11 pagesUnderstanding The Relationship Between Cognitive Performance and Function in Daily Life After Traumatic Brain InjuryKatia DjerroudNo ratings yet
- Consultation in Neurourology: A Practical Evidence-Based GuideFrom EverandConsultation in Neurourology: A Practical Evidence-Based GuideNo ratings yet
- 14 DipinoDocument13 pages14 Dipinosaad hassanNo ratings yet
- Biomedical Journal: SciencedirectDocument11 pagesBiomedical Journal: SciencedirectTahir AlyasNo ratings yet
- Paediatric Traumatic Brain InjuryDocument6 pagesPaediatric Traumatic Brain InjuryJuan Fernando Méndez RamírezNo ratings yet
- Global Neurosurgery The Current Capacity and DeficDocument11 pagesGlobal Neurosurgery The Current Capacity and DeficathathathNo ratings yet
- Frozen Section Pathology: Diagnostic ChallengesFrom EverandFrozen Section Pathology: Diagnostic ChallengesAlain C. BorczukNo ratings yet
- Faktor Resiko PisDocument9 pagesFaktor Resiko PisRahmasitaNo ratings yet
- Fneur 12 598777Document8 pagesFneur 12 598777Miguel HuangNo ratings yet
- Neuropathology Simplified: A Guide for Clinicians and NeuroscientistsFrom EverandNeuropathology Simplified: A Guide for Clinicians and NeuroscientistsNo ratings yet
- Management of Traumatic Brain Injury (TBI) - A Clinical Neuroscience-Led Pathway For The NHSDocument8 pagesManagement of Traumatic Brain Injury (TBI) - A Clinical Neuroscience-Led Pathway For The NHS彭金辉 KIVINo ratings yet
- Experimental NeurologyDocument14 pagesExperimental NeurologyMontserratNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- Neurologia MeningiteDocument10 pagesNeurologia MeningitesuzanaNo ratings yet
- Traumatic Brain Injury Advances Since 2017: What Has Changed?Document2 pagesTraumatic Brain Injury Advances Since 2017: What Has Changed?Stavya DubeyNo ratings yet
- Citicoline For Traumatic Brain Injury: A Systematic Review & Meta-AnalysisDocument10 pagesCiticoline For Traumatic Brain Injury: A Systematic Review & Meta-AnalysisAdria Putra FarhandikaNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- A Quick Guide to Pediatric RetinaFrom EverandA Quick Guide to Pediatric RetinaWei-Chi WuNo ratings yet
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- 2012 Rehabilitation of Brachial Plexus Injuries in Adults and ChildrenDocument24 pages2012 Rehabilitation of Brachial Plexus Injuries in Adults and ChildrenchayankkuNo ratings yet
- Congenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeDocument7 pagesCongenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeIbrahim Abdul KareemNo ratings yet
- Traumatic Brain Injury: Integrated Approaches To Improve Prevention, Clinical Care, and ResearchDocument63 pagesTraumatic Brain Injury: Integrated Approaches To Improve Prevention, Clinical Care, and Researchakish4uNo ratings yet
- Fped 07 00163Document7 pagesFped 07 00163TanFransisca DianNo ratings yet
- Case Study Secon EditDocument42 pagesCase Study Secon EditAbegail PolicarpioNo ratings yet
- National Clinical Guideline For Stroke in Secondary CareDocument25 pagesNational Clinical Guideline For Stroke in Secondary CareSebastian SalvadorNo ratings yet
- Endoscopic Surgical Management of Intracranial SymDocument15 pagesEndoscopic Surgical Management of Intracranial SymSebastian SalvadorNo ratings yet
- Cancers: New Developments in The Pathogenesis, Therapeutic Targeting, and Treatment of Pediatric MedulloblastomaDocument15 pagesCancers: New Developments in The Pathogenesis, Therapeutic Targeting, and Treatment of Pediatric MedulloblastomaSebastian SalvadorNo ratings yet
- Endoscopic Third Ventriculostomy in The Treatment of Hydrocephalus in Pediatric PatientsDocument101 pagesEndoscopic Third Ventriculostomy in The Treatment of Hydrocephalus in Pediatric PatientsSebastian SalvadorNo ratings yet
- Journal Pre-Proof: European Journal of Paediatric NeurologyDocument31 pagesJournal Pre-Proof: European Journal of Paediatric NeurologySebastian SalvadorNo ratings yet
- Opab 314Document7 pagesOpab 314Sebastian SalvadorNo ratings yet
- Clasificacion de Tumores Cerebreales de La OMS 2016 Articulo de RevisionDocument17 pagesClasificacion de Tumores Cerebreales de La OMS 2016 Articulo de RevisionSebastian SalvadorNo ratings yet
- Glioma Invasion: Mechanisms and Therapeutic Challenges: Mariano S. Viapiano Sean E. LawlerDocument35 pagesGlioma Invasion: Mechanisms and Therapeutic Challenges: Mariano S. Viapiano Sean E. LawlerSebastian SalvadorNo ratings yet
- Raindrop Technique SeminarDocument1 pageRaindrop Technique SeminaromshantidevaNo ratings yet
- Food Safety PosterDocument1 pageFood Safety PosterMP CariappaNo ratings yet
- A Community-Based Mothers and Infants CenterDocument10 pagesA Community-Based Mothers and Infants CenterRazonable Morales RommelNo ratings yet
- This Study Resource WasDocument2 pagesThis Study Resource WasAbhishek SachdevaNo ratings yet
- Yenepoya Medical CollegeDocument11 pagesYenepoya Medical CollegepentagoneducationNo ratings yet
- Chapter 003 Geriatric Pharmacology: Multiple Choice QuestionsDocument15 pagesChapter 003 Geriatric Pharmacology: Multiple Choice QuestionsgoldfishxNo ratings yet
- Mental Health-Case Study GDocument14 pagesMental Health-Case Study Gapi-545670336No ratings yet
- National Human Resources For Health Master Plan 2020-2040 (Updated As of 12 Nov 2021)Document318 pagesNational Human Resources For Health Master Plan 2020-2040 (Updated As of 12 Nov 2021)Renard JaenNo ratings yet
- Do The Benefits of Medical Marijuana Justify Its LegalityDocument4 pagesDo The Benefits of Medical Marijuana Justify Its LegalityAlexander MasakuNo ratings yet
- Optimalisasi Nutrisi Enteral Dan Parenteral (New Version)Document25 pagesOptimalisasi Nutrisi Enteral Dan Parenteral (New Version)Titik sukamtiNo ratings yet
- True MedicineDocument52 pagesTrue MedicineMoga RazvanNo ratings yet
- NURS4060 - AshleyVigne - Assessment 4 - Attempt1Document7 pagesNURS4060 - AshleyVigne - Assessment 4 - Attempt1ashleyNo ratings yet
- Life After Oracle Support PDFDocument20 pagesLife After Oracle Support PDFgs2s42419No ratings yet
- MAKE YOUR PRACTICE FLOURISH WITH FERTILITY NUTRITION - Workbook PDFDocument8 pagesMAKE YOUR PRACTICE FLOURISH WITH FERTILITY NUTRITION - Workbook PDFHershey AngelesNo ratings yet
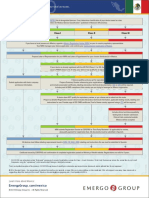
- Low Risk Class I Class II Class IIIDocument2 pagesLow Risk Class I Class II Class IIImd edaNo ratings yet
- Caries Indices PDFDocument6 pagesCaries Indices PDFTamara Nitya ArianiNo ratings yet
- MSC Nursing Induction Programme - 14th-18th September 2020 (Final) PDFDocument8 pagesMSC Nursing Induction Programme - 14th-18th September 2020 (Final) PDFEno ObongNo ratings yet
- Recognized Nursing Colleges in Tamil NaduDocument31 pagesRecognized Nursing Colleges in Tamil Naduprasadden100% (1)
- C RAD Field Service Engineer HoustonDocument2 pagesC RAD Field Service Engineer HoustonSargunan SabNo ratings yet
- Forensic NursingDocument3 pagesForensic NursingJoras Joy Yu Gregorio-AntojadoNo ratings yet
- Vanderbilt Rating Scale Scoring InstructionsDocument2 pagesVanderbilt Rating Scale Scoring InstructionsYeon Ae Narita100% (2)
- Katayani Himeo - Google SearchDocument1 pageKatayani Himeo - Google SearchSonnet XavierNo ratings yet
- Know Your Hospital - A Guide To Getting The Best CareDocument9 pagesKnow Your Hospital - A Guide To Getting The Best CareMike PosktovaNo ratings yet
- Module 5 QuizDocument3 pagesModule 5 Quizapi-329063194No ratings yet
- Veteran Help-Seeking Behaviour For Mental HealthDocument6 pagesVeteran Help-Seeking Behaviour For Mental HealthDaniel KoffmanNo ratings yet
- Estimation of Fluid Status Changes in Critically Ill PatiensDocument7 pagesEstimation of Fluid Status Changes in Critically Ill PatiensLina Mahayaty SembiringNo ratings yet
- Pathology Consultation On Reporting of Critical ValuesDocument9 pagesPathology Consultation On Reporting of Critical ValuesjantiNo ratings yet
- Mountain View Community Hospital: Goals and Critical Success FactorsDocument5 pagesMountain View Community Hospital: Goals and Critical Success Factorsfadicool007No ratings yet
- Standards For Renal DialysisDocument18 pagesStandards For Renal DialysisIbrar Ahmad100% (1)
- C-S & VbacDocument54 pagesC-S & VbacDagnachew kasayeNo ratings yet