Professional Documents
Culture Documents
Interpretation: Diverticulosis With Diverticulitis, Ruptured, Hinchey Type III Internal Hemorrhoids, Grade II
Uploaded by
Luke Matthew MondaresOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Interpretation: Diverticulosis With Diverticulitis, Ruptured, Hinchey Type III Internal Hemorrhoids, Grade II
Uploaded by
Luke Matthew MondaresCopyright:
Available Formats
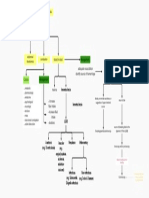
Plain X ray of abdomen
Plain X-rays of the abdomen (supine, upright, and
diaphragmatic views) are useful for detecting free intra-
abdominal air, bowel gas patterns suggestive of small or large
bowel obstruction, and volvulus
Contrast studies
Contrast studies are useful for evaluating obstructive
symptoms, delineating fistulous tracts, and diagnosing small
perforations or anastomotic leaks.
Detection of small lesions can be extremely difficult,
especially in a patient with extensive diverticulosis. For this
reason, a colonoscopy is preferred for evaluating
nonobstructing mass lesions in the colon. Double-contrast
barium enema has been used as a back-up examination if
colonoscopy is incomplete.
Flexible sigmoidoscopy and colonoscopy
Sigmoidoscopes measure 60 cm in length.
Colonoscopes measure 100 to 160 cm in length and are
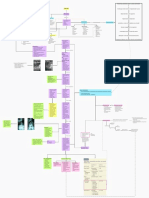
Xavier, 58 year old male capable of examining the entire colon and terminal ileum.
Both sigmoidoscopy and colonoscopy can be used
presents with Diagnostics diagnostically and therapeutically.
Additional info
skips the usual morning ritual of going to the toilet to move his
bowel
abdominal PHYSICAL EXAM
known smoker for about 45 years consuming about 4-5 sticks a constipation blood in stool Management:
bloatedness
day,
drinks alcohol almost every week only during weekends often to adequate resuscitation The patient is alert, cooperative, oriented but obviously Interpretation
NGT aspiration
point of intoxication. identify source of hemorrhage uncomfortable. Indeterminate abdomen with feces filled with colon
Indications
3-4 episodes of watery stools a day since 2 days ago, described Causes: Management: Vital signs: BP 140/70 mmHg HR: 100/min RR: 18/min
as brownish to dark colored, with 1-2 occasions of mucoid Temp: 36.7oC Height: 167 cm Weight: 75 Kgs. Hemorrhoids
metabolic melena hemetochezia Prostatitis developed moderate fever and abdominal distention
stools. pharmacologic
experienced severe left Abdominal exam reveals a globular abdomen, Prostate CA
endocrine bloody or non-bile secretions, or BPH clinical manifestations: On physical examination:
iliac and hypogastric pain. increase return of bile normoactive bowel sounds, hypertympanitic, Anal and rectal CA
psychological suggestive of upper intestinal left-sided abdominal pain, with/ hypertensive, tachycardic, tachypneic, febrile
neurologic fiber intake hemetochezia source soft with tender left iliac with no muscle guarding, no Anal condylomas without fever and leukocytosis
stricture increase fluid palpable masses Constipation abdomen was slightly distended, direct tenderness at left lower quadrant
mass
Fecal incontinence and muscle guarding, hypoactive bowel sounds and tympanitic Differentials:
intake Anal fissures Diverticulitis
slow-transit constipation DRE: tight sphincter tone, enlarged palpable fleshy non
laxatives LGIB IBD - UC and Crohn’s ds
Colonic malignancy
outlet obstruction
source of bleeding distal to the
tender mass at the left lateral and right
Esophagogastroduodenoscopy ligament of Treitz (LGIB) anterior anus, smooth mucosa, brownish feces slight Pelvic pain
blood tinged flecks on gloved examining Contraindications
Patient was started Ertapenem 1gm IV once daily Groin pain
finger. Severe neutropenia IV hydration Inguinal hernia
Anatomic Vascular Neoplasm Inflammatory Prostatic abscess
Anoscopy and/or proctoscopy
(e.g. Diverticulosis) (e.g. Younger children - more careful
angiodysplasia,
ERTAPENEM
ischemia, failure to identify source of
bleeding
radiation-
induced)
Infectious Non-infectious Colonoscopy indications:
(e.g. Salmonella, (e.g.Crohn's Disease) Colonoscopy 1. + fecal occult blood LABORATORIES MOA used for
2. unexplained IDA
Shigella infection) Ertapenem exhibits bactericidal activity due inhibition treatment of complicated community-acquired intraabdominal
of cell wall synthesis mediated via binding to penicillin infections with adequate source control, including infections due
Stool Exam: binding proteins (PBPs). to resistant gram-negative organisms
RBC- high
Color : brown Work up:
Wbc- high
Consistency: soft CT, MRI, UTZ
Presence of
Microscopic: RBC/hpf - 35-40 E.histolytica cyst Contrast enemas/or endoscopy
WBC/hpf – 8-10 relatively contraindicated because
Ova and Parasites: E. histolytica cyst of risk of perforation
Bacteria: abundant
Blood type: O Rh+
CBC:
WBC – 13.6 K/uL RBC – 3.9 M/uL
Neu – 89.0 % Hgb – 11.3 g/dl Leukocytosis
Lym- 5.29% Hct – 34.0 Neutrophilic predominance
Mono – 5.36% MCV- 87.1 fL Hgb decreased - mild anemia
Eos – 0.169% Platelet – 259 K/uL
Baso – 0.195% RBC Morphology – Normal
FLAT PLATE AND UPRIGHT FILM OF
ABDOMEN: Exhibit A
The patient was given Metronidazole and
Diosmin + Hesperidin and was sent home.
Metronidazole
Against anaerobes
Amoebicidal
Trichomonacidal
Disrupts DNA and causes
breakage
TOC for amoebiasis
Interpretation Interpretation
Diosmin + Hesperidin Pericolic fat stranding at the sigmoid area likely due to inflammation, presence of colonic diverticula, The liver is not enlarged with normal echogenic pattern. There is no
Derived from plants bowel wall thickening, soft tissue inflammatory masses raising possibility of phlegmon, and abscesses at thickening of the Gallbladder wall with bile sludge. The biliary tree is not
the area of the sigmoid colon. Consider diverticulitis or colonic malignancy with pericolic abscess dilated. Pancreas and spleen are normal, the right kidney is normal in
Vascular protective effect formation. echopattern, renal calyces not dilated. The left
Supplements kidney is mildly echogenic with no pelvocalyceal dilatation. There are dilated
bowel loops which obscure the examination of the rest of the abdomen.
Diverticular Disease
CT SCAN findings:
Diverticulosis Diverticulitis
presence of diverticula without
Uncomplicated pericolic soft tissue stranding bowel resection
refers to inflammation and infection
Diverticulitis colonic wall thickening
inflammation associated with diverticula indications:
phlegmon
after 1st episode in children
after first episode of complicated
diverticulitis
outpatient immunosuppresed patients
Management
broad spectrum antibiotics for 7-days symptoms
sigmoid colon most common site
(LLQ) resolve
with more severe pain perform colonoscopy after 4-6
hospitalized weeks to r/o malignancy
Patient showed give parenteral antibiotics
Management suspect abscess formation NO improvement bowel rest
after 48 hours.
upon
Hinchey Stage I and 2
CT scan
drain abscess percutaneously
Small abscesses (<2cm) may be treated with
Physical Further Imaging parenteral antibiotics
Examination Larger abscesses are best treated with CT-guided
percutaneous drainage and antibiotics
patient deteriorates and/or
peritonitis
Abdomen: Hinchey Stage 3 and 4
laparotomy globular, tense, with direct
tenderness on LLQ and RRQ
w/ rebound tenderness, Patients with larger abscesses, peritoneal soiling,
muscle guarding, absent or peritonitis, sigmoid colectomy with end
bowel sounds, tympanitic colostomy and Harmann's pouch (most common)
Febrile
or
Left Lateral Decubitus Film
Interpretation
Sigmoid colectomy with end colostomy, primary
Presence of gas on the patient's R
anastomosis, with or without on-table lavage,
1. abscess is inaccessible to percutaneous drainage Upright Film side. Diverticulitis on the sigmoid
2. patient deteriorates or fails to improve and proximal diversion
3. patient presents with free intra-abdominal air
Interpretation colon might have perforated
4. peritonitis Presence of gas distended large causing pneumoperitoneum
bowel loops; pattern nonspecific
and non-obstructive
Made up of cushions of submucosal tissue,
pneumoperitoneum Hemorrhoids vessels + smooth muscle fiber
Graded depending on extent
Complicated - Diverticulitis with abscess, obstruction, diffuse
Diverticulitis peritonitis (free perforation), or fistulas
Adenocarcinoma
most common cancer of GIT
recommends to start screening dominant risk factor: age (>50 years old)
for malignancy at 50 years old other factors include: hereditary risk factors,
environment and dietary factors
advice patient:
1. a diet high in vegetable fibers
2. decrease alcohol intake
3. quit smoking Management:
4. Take supplements such as calcium, selenium, Vit. A,c, and E, carotenoids
Management:
Hinchey staging system
may progress to
FINAL
DIAGNOSIS
Diverticulosis with diverticulitis,
ruptured, Hinchey type III
Internal Hemorrhoids, Grade II
You might also like
- Referat EndosDocument29 pagesReferat EndosShenaquitaIvandraNo ratings yet
- Diagnostic Studies - GI BleedingDocument21 pagesDiagnostic Studies - GI BleedingnoemilauNo ratings yet
- Kevin Santosh Joseph 15M4245Document12 pagesKevin Santosh Joseph 15M4245Kevin JosephNo ratings yet
- Mesenteric Cyst in InfancyDocument27 pagesMesenteric Cyst in InfancySpica AdharaNo ratings yet
- Grup 11 - Fritzienico Zachary Baskoro (20711031) - Hafizh Cahya Aryansyah (20711034) - Daffa Alief Ramadhan (20711164) - Tugas Inggris MmapDocument1 pageGrup 11 - Fritzienico Zachary Baskoro (20711031) - Hafizh Cahya Aryansyah (20711034) - Daffa Alief Ramadhan (20711164) - Tugas Inggris MmapFritzienico BaskoroNo ratings yet
- Colonic Intussusception: Clinical and Radiographic Features: Marc J. GollubDocument6 pagesColonic Intussusception: Clinical and Radiographic Features: Marc J. GollubvinaNo ratings yet
- Wale 2016Document12 pagesWale 2016Radiologi RSPDNo ratings yet
- Last PartDocument1 pageLast PartGrachell AshleyNo ratings yet
- Complete Intestinal ObstructionDocument8 pagesComplete Intestinal ObstructionThuganamix100% (2)
- Koas Radiologi Audriana Jurding Ileus22Document29 pagesKoas Radiologi Audriana Jurding Ileus22Anto TriwibowoNo ratings yet
- Abdominal Ultrasonographyin Small AnimalsDocument10 pagesAbdominal Ultrasonographyin Small AnimalsAna Clara SevasteNo ratings yet
- Lecture-3 GIT RKDocument46 pagesLecture-3 GIT RKmuhammadameerhamza4786No ratings yet
- Diagnostic Operation of The Liver and Techniques of Hepatic ResectionDocument17 pagesDiagnostic Operation of The Liver and Techniques of Hepatic ResectionjuaoNo ratings yet
- Imaging: Laras Prasast NIM 1320111034Document11 pagesImaging: Laras Prasast NIM 1320111034Andyn RobiolenyNo ratings yet
- Radiological Anatomy of The Colon and Rectum in Children: Gastroenterology & Hepatology: Open AccessDocument5 pagesRadiological Anatomy of The Colon and Rectum in Children: Gastroenterology & Hepatology: Open AccesseugeniaNo ratings yet
- 2015 - Small-Bowel Capsule Endoscopy and Device-Assisted Enteroscopy For Diagnosis and Treatment of Smallbowel Disorders - European Society of Gastrointestinal Endoscopy (ESGE) Clinical GuidelineDocument25 pages2015 - Small-Bowel Capsule Endoscopy and Device-Assisted Enteroscopy For Diagnosis and Treatment of Smallbowel Disorders - European Society of Gastrointestinal Endoscopy (ESGE) Clinical GuidelineOrlando QuirosNo ratings yet
- David J Ott - 1988 - Current Problems in Diagnostic RadiologyDocument28 pagesDavid J Ott - 1988 - Current Problems in Diagnostic RadiologysharfinaNo ratings yet
- Feline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Document14 pagesFeline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Ветеринарная хирургия Dvm Тозлиян И. А.No ratings yet
- Assignment GiDocument14 pagesAssignment GiVoid LessNo ratings yet
- Plain Abdominal XrayDocument10 pagesPlain Abdominal XrayviKиҼswAяAи LiиGaM100% (3)
- Review: Bowel Wall Thickening On Transabdominal SonographyDocument11 pagesReview: Bowel Wall Thickening On Transabdominal Sonographygrahapuspa17No ratings yet
- Abdominal RadiographDocument13 pagesAbdominal RadiographBagasNo ratings yet
- Walker - Explorarea Radiologica A Tubului DigestivDocument11 pagesWalker - Explorarea Radiologica A Tubului DigestivDiana AndriucNo ratings yet
- Genitourinary SystemDocument8 pagesGenitourinary Systemsarguss14100% (1)
- Gastroenterologist in The WoodlandsDocument1 pageGastroenterologist in The WoodlandsHoward HamatNo ratings yet
- Recurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Document2 pagesRecurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Motivational SpeechNo ratings yet
- Rectal Computer 2Document5 pagesRectal Computer 2Su-sake KonichiwaNo ratings yet
- Defecography: Technique, Interpretation, and Current Use: Arden M. Morris and Susan C. ParkerDocument14 pagesDefecography: Technique, Interpretation, and Current Use: Arden M. Morris and Susan C. ParkerSuraj KurmiNo ratings yet
- Diverticular Disease and Intestinal ObstructionDocument31 pagesDiverticular Disease and Intestinal ObstructionPauLa Cheneree Peña ÜNo ratings yet
- General Surgical Considerations, Inflammatory Bowel DiseaseDocument7 pagesGeneral Surgical Considerations, Inflammatory Bowel DiseaseDesa RefuerzoNo ratings yet
- 27 34 PDFDocument8 pages27 34 PDFMusdah MulyaNo ratings yet
- Cistic VeinDocument4 pagesCistic VeinAFJimenezONo ratings yet
- Feline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Document8 pagesFeline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Ветеринарная хирургия Dvm Тозлиян И. А.No ratings yet
- Colonic ObstructionDocument4 pagesColonic ObstructionKristine AlejandroNo ratings yet
- Gastrointestinal System Three Phases of Gastric SecretionDocument21 pagesGastrointestinal System Three Phases of Gastric SecretiontychynNo ratings yet
- IndianJRadiolImaging213170-7050884 193508 PDFDocument6 pagesIndianJRadiolImaging213170-7050884 193508 PDFAndri Tri AtmojoNo ratings yet
- Sonography of GITDocument11 pagesSonography of GITsononik1674100% (1)
- Diagnostic Procedures GITDocument5 pagesDiagnostic Procedures GITMaria Ellah C. BELASOTONo ratings yet
- Radiologic Manifestations of Malabsorption: A Nonspecific FindingDocument6 pagesRadiologic Manifestations of Malabsorption: A Nonspecific FindingTara NareswariNo ratings yet
- CholelithiasisDocument11 pagesCholelithiasisMhae De GuzmanNo ratings yet
- AbdomenDocument3 pagesAbdomenHazel ConjeNo ratings yet
- Biliary ImagingDocument35 pagesBiliary ImagingJb MalabagNo ratings yet
- Mikrokolon & TerjemahanDocument35 pagesMikrokolon & Terjemahanizza mumtazatiNo ratings yet
- Fibroscan® and Transient Elastography: What Are The Indications For This Test?Document4 pagesFibroscan® and Transient Elastography: What Are The Indications For This Test?Clarisa AnindyaNo ratings yet
- Ultrasonographic Detection and Assessment of The Severity of Crohn's Disease Recurrence After Ileal ResectionDocument11 pagesUltrasonographic Detection and Assessment of The Severity of Crohn's Disease Recurrence After Ileal ResectionСергей СадовниковNo ratings yet
- Imaging Modalities of Large Bowel: DR. Srijit SahaDocument38 pagesImaging Modalities of Large Bowel: DR. Srijit SahasrijitNo ratings yet
- (Aganglionic Megacolon) : Hirschsprung'S DiseaseDocument2 pages(Aganglionic Megacolon) : Hirschsprung'S DiseaseLalisaM ActivityNo ratings yet
- Basic Investigations: Endoscopy, X-Ray, Mri, EcgDocument6 pagesBasic Investigations: Endoscopy, X-Ray, Mri, EcgAndrei DragosNo ratings yet
- 1 s2.0 S2212097113701730 MainDocument3 pages1 s2.0 S2212097113701730 MainSueNo ratings yet
- Intestinal Ascariasis in Children: &) M. Rather G. Naikoo S. Mushtaq M. NazirDocument7 pagesIntestinal Ascariasis in Children: &) M. Rather G. Naikoo S. Mushtaq M. Nazirimamlutfi13No ratings yet
- BAIRANIAH GOGO - NGT Learning TaskDocument5 pagesBAIRANIAH GOGO - NGT Learning TaskDm KeeNo ratings yet
- Insignis Surgery 2 Gallbladder and Extrahepatic Biliary SystemDocument7 pagesInsignis Surgery 2 Gallbladder and Extrahepatic Biliary SystemPARADISE JanoNo ratings yet
- 3 MerilDocument1 page3 MerilGuntur Aji PrasetyoNo ratings yet
- Congenital Pyloric Atresia With Distal Duodenal Atresia-Role of CT ScanDocument3 pagesCongenital Pyloric Atresia With Distal Duodenal Atresia-Role of CT Scanhaidar HumairNo ratings yet
- 2 Intestinal Obstruction. IntussusceptionDocument28 pages2 Intestinal Obstruction. IntussusceptionGede SubhagaNo ratings yet
- Ictericia Obstructiva, Tratamiento EndoscópicoDocument6 pagesIctericia Obstructiva, Tratamiento EndoscópicoGeraldine RuizNo ratings yet
- Filling of The Bladder For Pelvic Sonograms: An Ancient Form of TortureDocument3 pagesFilling of The Bladder For Pelvic Sonograms: An Ancient Form of Torturemjk deguzmanNo ratings yet
- Wa0002Document14 pagesWa0002Katya RizqitaNo ratings yet
- Case Sample Pertinent Data: HistoryDocument3 pagesCase Sample Pertinent Data: HistoryNeil AlviarNo ratings yet
- Selina Kaylo, 29/F Scott Sommer, 64/M: Basic Ophthalmologic ExamDocument1 pageSelina Kaylo, 29/F Scott Sommer, 64/M: Basic Ophthalmologic ExamLuke Matthew MondaresNo ratings yet
- Xavier, 58 Year Old Male Presents With: Hemetochezia HemetocheziaDocument1 pageXavier, 58 Year Old Male Presents With: Hemetochezia HemetocheziaLuke Matthew MondaresNo ratings yet
- Maye Bato 47 Yo, F: Surgery Module 5 Facilitator: Dr. Jerry Alinsug Group 7Document1 pageMaye Bato 47 Yo, F: Surgery Module 5 Facilitator: Dr. Jerry Alinsug Group 7Luke Matthew MondaresNo ratings yet
- Lois, 23/F: Candida Albicans Trichomonas Vaginalis Chlamydia Trachomatis Neisseria GonorrhoeaeDocument1 pageLois, 23/F: Candida Albicans Trichomonas Vaginalis Chlamydia Trachomatis Neisseria GonorrhoeaeLuke Matthew MondaresNo ratings yet
- Enthusiasm: If There Is A Catalog, Read It Ahead Good Questions Demonstrate Both Enthusiasm and IntelligenceDocument2 pagesEnthusiasm: If There Is A Catalog, Read It Ahead Good Questions Demonstrate Both Enthusiasm and IntelligenceLuke Matthew MondaresNo ratings yet
- Aptitude Test SampleDocument8 pagesAptitude Test SampleRJ Sumonod Jr.No ratings yet
- Author(s) : Brenda Gunderson, PH.D., 2012 License: Unless Otherwise Noted, This Material Is Made Available Under TheDocument8 pagesAuthor(s) : Brenda Gunderson, PH.D., 2012 License: Unless Otherwise Noted, This Material Is Made Available Under TheCher Jay-ar DoronioNo ratings yet
- Number Series SolutionsDocument10 pagesNumber Series Solutionsbittu maityNo ratings yet
- Geometrical Properties of Vectors and Covectors AnDocument15 pagesGeometrical Properties of Vectors and Covectors AnSayantanNo ratings yet
- Social ScienceDocument7 pagesSocial ScienceChoy Savilla100% (1)
- Intermediate Dictionary PDFDocument733 pagesIntermediate Dictionary PDFarturoNo ratings yet
- Psychometric Success Abstract Reasoning - Practice Test 1Document13 pagesPsychometric Success Abstract Reasoning - Practice Test 1Ambrose Zaffar75% (16)
- 1000 Most Common Words (SAT)Document70 pages1000 Most Common Words (SAT)grellian95% (20)
- 100 Most Important Questions of RC (ANSWERS)Document3 pages100 Most Important Questions of RC (ANSWERS)Luke Matthew MondaresNo ratings yet
- Reasoning Verbal PDFDocument31 pagesReasoning Verbal PDFLucid LynxNo ratings yet
- Mock 1 - PA PDFDocument7 pagesMock 1 - PA PDFlorrainebarandonNo ratings yet
- ChemistryDocument7 pagesChemistryPaul Anthony LontokNo ratings yet
- TextDocument1 pageTextLuke Matthew MondaresNo ratings yet
- 100 Most Important Questions of RCDocument15 pages100 Most Important Questions of RCLuke Matthew MondaresNo ratings yet
- NMAT Practice Set Part 1 & Part 2 With Answer KeyDocument64 pagesNMAT Practice Set Part 1 & Part 2 With Answer KeyLucid Lynx100% (1)
- Rationale NmatDocument3 pagesRationale NmatLuke Matthew MondaresNo ratings yet
- Mock 2 IRDocument3 pagesMock 2 IRWendell Kim LlanetaNo ratings yet
- Evaluation of Acute Abdomen 2013ADocument4 pagesEvaluation of Acute Abdomen 2013AEdison Tan SantamariaNo ratings yet
- US Gall Bl. Biliary TreeDocument20 pagesUS Gall Bl. Biliary TreeNenad V. DjokicNo ratings yet
- AUF SOM - Dse of Small Intestine PDFDocument166 pagesAUF SOM - Dse of Small Intestine PDFYestin Reece Corpus ArcegaNo ratings yet
- Finals ConferenceDocument50 pagesFinals Conferenceangel_sagun_1No ratings yet
- TERMINOLOGI 2 ST - PencernaanDocument61 pagesTERMINOLOGI 2 ST - PencernaanSarah Suzanna Sitepu0% (1)
- Amoebiasis - and GiardiasisDocument59 pagesAmoebiasis - and GiardiasisSaurabh AgarwalNo ratings yet
- Anal FissuraDocument14 pagesAnal FissuraAnonymous LoQcj2xENo ratings yet
- Abdominal TuberculosisDocument12 pagesAbdominal TuberculosisBimlesh ThakurNo ratings yet
- Acute AbdomenDocument54 pagesAcute AbdomenMoses ChatipaNo ratings yet
- Case Study FormatDocument13 pagesCase Study Formatعبداللة العمراني الحويطيNo ratings yet
- Gastrointestinal SystemDocument218 pagesGastrointestinal Systemnursereview92% (12)
- Print SGD Ein Fix Gastritis BHDocument21 pagesPrint SGD Ein Fix Gastritis BHSagita Wulan SariNo ratings yet
- List of Common Antacid DrugsDocument3 pagesList of Common Antacid DrugsJoyce NatoNo ratings yet
- Pharmacology of Gastrointestinal SystemDocument4 pagesPharmacology of Gastrointestinal SystemZaira KimNo ratings yet
- Liver and Gallbladder: With Dr. James PickeringDocument17 pagesLiver and Gallbladder: With Dr. James PickeringVathana SorNo ratings yet
- Ebook Sleisenger and Fordtrans Gastrointestinal and Liver Disease PDF Full Chapter PDFDocument67 pagesEbook Sleisenger and Fordtrans Gastrointestinal and Liver Disease PDF Full Chapter PDFronald.hartford579100% (25)
- Abdominal Pain: Differential DiagnosisDocument12 pagesAbdominal Pain: Differential Diagnosisransh100% (1)
- AP Bio Digestion System (Kfogler)Document34 pagesAP Bio Digestion System (Kfogler)julie rainesNo ratings yet
- Answers To Questions:: Analysis of SalivaDocument2 pagesAnswers To Questions:: Analysis of Salivaerisseval14No ratings yet
- AnatomyvsPhysiology1 11Document12 pagesAnatomyvsPhysiology1 11Florilyn CabezoNo ratings yet
- Esomeprazole: A N D PDocument9 pagesEsomeprazole: A N D PHadiNugrahaNo ratings yet
- Digestive System - MefloresDocument117 pagesDigestive System - MefloresJohnMichaelDominguezNo ratings yet
- Comprehensive Guide To Why Fart SmellsDocument6 pagesComprehensive Guide To Why Fart SmellsRonanNo ratings yet
- Coffee Enema InstructionsDocument6 pagesCoffee Enema InstructionsCristi PascalNo ratings yet
- Anh Văn Chuyên NgànhDocument7 pagesAnh Văn Chuyên Ngành19150004No ratings yet
- High Yield General Surgery Topics PDFDocument85 pagesHigh Yield General Surgery Topics PDF1031 Muhammad zaryabNo ratings yet
- AppendicitisDocument3 pagesAppendicitisNathalie Joy Gagtan100% (1)
- Parasitology (Quiz 2)Document6 pagesParasitology (Quiz 2)Frances Jewel Len SuyoNo ratings yet
- NCP-fluid Volume DeficitDocument4 pagesNCP-fluid Volume DeficitChrissa Mae Aranilla MayoNo ratings yet
- Virtual Colonoscopy: in Colorectal Cancer ScreeningDocument27 pagesVirtual Colonoscopy: in Colorectal Cancer ScreeningEwhied RuslamNo ratings yet