Professional Documents
Culture Documents
SureScript - Eligibility and Formulary
Uploaded by
Nileima Elaine RomeroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SureScript - Eligibility and Formulary
Uploaded by
Nileima Elaine RomeroCopyright:
Available Formats
Eligibility and Formulary:
Eligibility Companion Guide 2.0
July 11, 2018
ELIGIBILITY AND FORMULARY: ELIGIBILITY COMPANION GUIDE 2.0
PUBLISHED BY
SURESCRIPTS, L.L.C.
920 2ND AVENUE S.
MINNEAPOLIS, MN 55402
PHONE: 866-267-9482
FAX: 651-855-3001
2800 CRYSTAL DRIVE
ARLINGTON, VA 22202
PHONE: 866-797-3239
FAX: 703-921-2191
WWW.SURESCRIPTS.COM
Copyright© 2018 by Surescripts, LLC.
All rights reserved. Proprietary and Confidential.
This document and all other documents, materials, and information, transmitted or orally communicated by
Surescripts® in the course of the parties’ dealings constitute and are hereby designated as proprietary and
confidential information of Surescripts, and may not be reproduced or distributed (in whole or in part) without the
express written consent of Surescripts.
FOR SECTIONS OF THIS IMPLEMENTATION GUIDE
PERTAINING TO X12 STANDARDS:
Materials Reproduced with the Consent of X12.
Eligibility CG 2.0 Table of Contents
TABLE OF CONTENTS
Section 1: Eligibility Overview 5
1.1 About Eligibility 5
1.2 About This Guide 5
1.3 Examples Disclaimer 5
1.4 Guide Disclaimer 6
1.5 Document References 6
Section 2: Integration & Production 7
2.1 Integration Process 7
2.2 Terminology Usage 7
2.3 Transition to Production 8
2.4 Communication Rules 8
2.5 Timeouts 8
2.6 Compliance 9
Section 3: Messages Overview 10
3.1 Message Descriptions 10
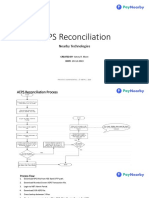
3.2 Eligibility Message Flow 11
3.3 Eligibility Detailed Message Flow Scenarios 11
3.4 General Interface Description 14
3.4.1 Dynamic Delimiters 15
3.4.2 Delimiter Examples 15
3.4.3 Representation 16
3.4.3.1 Numeric Representation 17
Character Set 17
3.5 Message Validation 18
3.6 Failure Mode/Response Approach 18
3.6.1 Error Processing for 270 and 271 18
Section 4: Eligibility Messaging 20
4.1 Relationship to X12N 270/271 Standard 20
4.2 Patient Match Verification 21
4.2.1 Insufficient Information 21
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 3
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Table of Contents
4.2.2 Non-Unique Match 22
4.3 270 Eligibility, Coverage, or Benefit Inquiry 23
4.4 271 Eligibility, Coverage, or Benefit Information 30
4.5 TA1 Interchange Acknowledgement 41
4.6 999 Implementation Acknowledgement for Health Care Insurance 43
4.7 Hierarchical Loops 46
4.8 270 and 271 Message Examples 47
Section 5: Eligibility Message Processing Summary 56
5.1 Surescripts Receives the 270 From the Requesting Party (Provider Vendor) 57
5.2 Surescripts Processes the 270 57
5.3 Surescripts Attempts to Connect with Source (PBM/payer) 59
5.4 PBM/payer Evaluates the Message 60
5.5 PBM/payer Processes the 270 60
5.6 PBM/payer Sends 271 Back to Surescripts 64
5.7 Summary of Errors Sent to Provider Vendor 65
5.8 Summary of Translated Errors 66
Section 6: Application Certification Requirements 67
6.1 Eligibility Retrieval 67
6.2 Presentation of Eligibility Information 68
Section 7: ID Load and Response Files 69
7.1 Introduction 69
7.2 ID Load Process Flow 69
7.3 Format to be Used 70
7.4 Member Processing Examples 70
7.5 Error Scenarios 71
7.6 Member Directory Maintenance Delimited File from PBM/payer 71
7.7 Member Directory Response Delimited File to PBM/payer 75
7.8 Member Directory Response Summary Delimited File to PBM/payer 78
7.9 Member Directory Codes 81
Appendix A: Dynamic Delimiters 83
Appendix B: Document Change Log 85
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 4
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 1: Eligibility Overview
SECTION 1: ELIGIBILITY OVERVIEW
1.1 ABOUT ELIGIBILITY
The Surescripts Eligibility and Formulary: Eligibility provides physicians with the electronic delivery
of PBM/payer member data in an ambulatory setting. Through the provider vendor interface, the
physician can request patient information such as eligibility and pharmacy benefit coverage
information.
1.2 ABOUT THIS GUIDE
This Surescripts Eligibility Companion Guide was created to assist Pharmacy Benefit Managers
(PBMs)/Payers and Prescriber systems in developing and transferring messages needed to
provide PBM/payer member data regarding eligibility information and pharmacy benefit coverage,
at the point of care. The ID Load message allows PBM/Payers to provide Surescripts with their
member roster to populate the Surescripts Master Patient Index (MPI).
Notes:
The terms PBM/payer or processor, who acts on behalf of the PBM/payer, are referred to as
PBM/payer throughout this guide.
The terms message and transaction are used interchangeably throughout this guide. The term
transaction will be used when referring to the X12 guide.
The audience for this document includes any customer responsible for developing a system
interface for these electronic prescribing messages.
1.3 EXAMPLES DISCLAIMER
Examples provided throughout this Guide are not intended to be all-inclusive. This pertains to
example workflows, element-specific (field) examples, or message examples. Customers should
not restrict coding to the examples used herein.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 5
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 1: Eligibility Overview
1.4 GUIDE DISCLAIMER
In the event that Customer chooses to make any changes to Customer’s software recommended in
this guide, Customer acknowledges and agrees that (1) Surescripts shall bear no responsibility or
liability for Customer’s changes or any effects thereof and (2) Customer shall be required to
transition to the new guide at such time as said guide is published, which may involve different or
additional parameters than are published in this guide.
1.5 DOCUMENT REFERENCES
This Guide is meant to support and integrate with the X12 standard guides where applicable. It
does not reproduce the base standard in its entirety. Customers should read and comprehend the
associated standards prior to reading this Guide.
Please reference the following documents when reading this Companion Guide:
Document Title
ASC X12N/005010X279A1 Health Care Eligibility Benefit Inquiry and Response (270/271) – Referred to
as the ”X12 Guide” in the rest of this guide.
ASC X12N/005010X231A1 Implementation Acknowledgement for Health Care Insurance (999)
Surescripts Connectivity and Authentication Implementation Guide
FOR SECTIONS OF THIS IMPLEMENTATION GUIDE
PERTAINING TO ASC X12 STANDARDS:
“MATERIALS REPRODUCED WITH THE CONSENT OF”
Copyright I 2009, Data Interchange Standards Association on behalf of ASC X12. Format I 2009
Washington Publishing Company. All Rights Reserved. Users of this guide must purchase their
own copy of the ASC X12N/005010X279A1 (270/271) and X12N/005010X231A1 (999) as this
guide only includes a subset of those guides. Go to http://store.x12.org to obtain your copy.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 6
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 2: Integration & Production
SECTION 2: INTEGRATION & PRODUCTION
2.1 INTEGRATION PROCESS
Once Surescripts assigns an Integration resource, customers will be contacted to begin the project
(s) and will be guided through the Surescripts Integration process. The Integration resource will
provide Surescripts documentation, product education, access to the Surescripts staging
environment, assistance during design and development phases and testing to prepare for
certification. The Integration resource will perform certification testing, and once successful, will
provide access to the Surescripts production environment.
Note: The time frame of the project can vary depending on your resource allocation for the
project.
Meeting Requirements
During Integration, customers undergo certification testing to demonstrate all requirements are
met. Certification focuses on message format, and when appropriate, application workflow and
display in accordance with Surescripts documentation and the associated Application Certification
Requirements (ACRs). Upon successful completion of certification and, when applicable, other
pre-production network requirements (e.g., Identity Proofing, DEA audit), customers may
transition to production.
For requirements, consider the following:
l Surescripts ACRs are required to be met to achieve production status on the Surescripts
network and will be enforced as part of certification.
l Surescripts business rules are data validations applied by Surescripts beyond X12
requirements that will cause a message to be successful or rejected.
l Surescripts test cases do not cover all possible scenarios in production. Customers are
responsible for testing all scenarios specific to their production environment.
l Customers must be prepared to make allowances for things that are not governed by our
ACRs or X12 requirements or recommendations.
2.2 TERMINOLOGY USAGE
The following table outlines terminology usage for this guide:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 7
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 2: Integration & Production
Term Term usage
must Requirements that are enforced as part of the production code.
shall The requirements customers are required to meet in order to be certified on the Surescripts
network. These requirements will be enforced as part of certification.
should Used for guidance and best practices. Best practices can also be found in Best Practice sections.
Participants are encouraged, but not required, to meet best practices in order to be certified on the
Surescripts network.
E.### Designates an Eligibility ACR.
2.3 TRANSITION TO PRODUCTION
Once certification is complete and all Surescripts requirements have been met, the customer is
ready to move into production. Surescripts will configure the production connection and validate
successful operations with the customer. Once production is activated and validated, Surescripts
Account Management will schedule a hand-off meeting for the customer and Surescripts to discuss
the following:
l Lessons Learned and/or Satisfaction Survey
l Production support contacts (from both Surescripts and the customer)
l Support process and training
l Support hours
2.4 COMMUNICATION RULES
Please refer to the Connectivity and Authentication Guide for additional connectivity and
authentication information. For the network to be reliable, there are communication rules to which
all customers must adhere.
2.5 TIMEOUTS
For timeouts, consider the following:
l When sending a message to Surescripts, the initiator should set the http timeout to no less
than 30 seconds.
l A receiving system must reply with a valid 271/999/TA1/NAK response within 10 seconds.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 8
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 2: Integration & Production
2.6 COMPLIANCE
Surescripts goal is efficiency and consistency across the network so that all customers can meet
the highest measures of patient safety, end-to-end reliability, and quality. To ensure that customers
comply with, and adhere to, the approved certification requirements, Surescripts:
l initiates a remediation process for identified compliance issues, and
l monitors customers in production to ensure all network customers remain in compliance with
certification requirements and contractual terms.
Customers agree to notify Surescripts when they have altered, reconfigured or disabled any
portion of a Surescripts certified software product or module, before moving such changes into
production, as they may create a circumstance of non-compliance with the Surescripts certification
issued. In those instances, Surescripts will work with the customer to perform a timely re-
certification, if required, to ensure network compliance and safety.
This Guide is intended for certification on our network only and is not intended to ensure
compliance with state and federal law. In accordance with customer’s legal agreement with
Surescripts, each customer is responsible for conducting its own due diligence to ensure
compliance with all applicable laws and requirements, including, but not limited to, local and state
laws and regulations in which the customer’s application is deployed and used.
As a reminder, Surescripts conducts certification with customers to ensure the application adheres
to network requirements. Surescripts will enforce mandatory fields as required by the Standards
body and Surescripts guide requirements. To maximize interoperability, customers are
recommended to support optional fields that have been created to address gaps in discrete data
needs and the many solutions that are in place for the benefit of the receiver. Surescripts
encourages, but does not guarantee the use of optional discrete fields to support end user
workflows.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 9
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
SECTION 3: MESSAGES OVERVIEW
3.1 MESSAGE DESCRIPTIONS
Eligibility Request/Response
The X12 Health Care Eligibility, Coverage, or Benefit Inquiry (270) and Health Care Eligibility,
Coverage, or Benefit Information (271) message sets are used to request and respond to a patient
eligibility check. These messages enable prescribers to supply a patient’s name and demographic
information to Surescripts and get back some or all of the following information from each
PBM/payer that covers the patient:
l Health Plan Number/Name
l Cardholder ID
l Relationship Code
l Person Code
l Group Number, Group Name
l Formulary ID
l Alternative List ID
l Coverage List ID
l Copay List ID
l BIN
l PCN
l Type of Prescription Benefit:
l Pharmacy (Retail)
l Mail Order
l Specialty Pharmacy
l Long Term Care (LTC)
Interchange Acknowledgment
This X12 specification, TA1, is utilized to acknowledge receipt/header errors for batch messages
and errors in real time messages. For the Surescripts message set, it only applies to the X12
specifications (270 & 271). None of the other specifications utilize this message.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 10
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
Implementation Acknowledgement
The implementation acknowledgement, or 999, informs the submitter that the functional group
arrived at the destination and is required as a response to receipt of an X12 message in a batch
environment, and only for errors with real time messages. Surescripts only supports a real time
environment for the 270/271 messages, so the 999 will only be sent if there are errors. The 999
reports on errors generated due to data or segment issues that do not comply with the X12 guide.
3.2 ELIGIBILITY MESSAGE FLOW
The following steps depict the Eligibility message flow:
1. A requester sends an Eligibility Request (270) to Surescripts.
2. Surescripts validates the format of the transaction.
3. Surescripts locates the patient based on demographic information.
4. Surescripts determines to which PBM/payers the Eligibility Request (270) should be
directed.
5. The PBM/payer verifies the patient and responds to Surescripts with an Eligibility Response
(271) indicating the patient’s eligibility status.
6. Surescripts validates the format of the incoming Eligibility Response (271), consolidates all
271 responses and sends the information back to the requester.
3.3 ELIGIBILITY DETAILED MESSAGE FLOW SCENARIOS
The following diagrams depict various scenarios where NAK, TA1, 999, and ACK messages are
sent in response to an Eligibility message.
Scenario 1 - Surescripts Cannot Recognize Message or System Error:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 11
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
1a) Eligibility Request (270) message is sent to Surescripts.
1b) Surescripts cannot recognize the message and sends error text back to the provider vendor.
Errors include:
l cannot validate the sender’s Participant ID and/or password
l cannot identify the message
l a system error occurs before the message is being processed
Scenario 2 - Surescripts Recognized Message Format but Errors Found:
2a) Eligibility Request (270) message is sent to Surescripts.
2b) Surescripts finds an error within the header and reports errors with the TA1.
Scenario 3 - Surescripts Recognized Message Format but Errors Found:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 12
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
3a) Eligibility Inquiry (270) message is sent to Surescripts.
3b) Surescripts finds a syntax error within the message and reports errors with the 999.
Scenario 4 - PBM/Payer Cannot Recognize Message or System Error:
4a) Eligibility Request (270) message is sent to Surescripts.
4b) Surescripts forwards the message on to the PBM/payer.
4c) The PBM/payer cannot recognize the message or System Error and sends error text to
Surescripts.
4d) Surescripts creates a 271 with errors and returns it to the provider vendor.
Scenario 5 - PBM/Payer Validates Message and Returns Eligibility Response with AAA
segment in the 271 showing business error to Provider Vendor
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 13
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
5a) Eligibility Request (270) message is sent to Surescripts.
5b) Surescripts forwards the message on to the PBM/payer.
5c) The PBM/payer returns (271) business error in AAA segment.
5d) Surescripts forwards the (271) message on to the provider vendor.
Scenario 6 - PBM/Payer Returns Non-Compliant 271 (i.e., syntax error or header error):
6a) Eligibility Request (270) message is sent to Surescripts.
6b) Surescripts forwards the message on to the PBM/payer.
6c) The PBM/payer returns (271) with syntax error or header error.
6d) Surescripts creates a 271 with errors and returns it to the provider vendor.
6e) Surescripts sends TA1 or an Acknowledgment (999) to PBM/payer.
6f) PBM/Payer returns ACK.
3.4 GENERAL INTERFACE DESCRIPTION
The message specifications have been defined to follow HIPAA standards where available and to
allow the most effective processing. Delimiters separate components, data elements, and
segments (see subsection Appendix A: Dynamic Delimiters for clarification). For the X12
specifications, the delimiters are defined in the ISA segment of the message. If a data element in
the middle of a segment is omitted, the separator acts as a “place holder”.
The significant characters must be left justified. Leading spaces, if used, are assumed to be
significant characters. Trailing spaces should be suppressed.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 14
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
3.4.1 DYNAMIC DELIMITERS
X12 utilizes delimiters to separate component, segments, elements, etc. or as indicators (i.e., for
segment repetition.) These delimiters are defined within specified segments of the messages.
Customer's systems need to be able to dynamically set and handle these delimiters. Surescripts
recommends the use of unprintable characters as delimiters rather than the entire full character set
(Refer to Appendix A: Dynamic Delimiters for a full list of acceptable characters).
For X12 messages, the delimiter set is defined within the ISA segment. The following is an
example:
ISA*00* *01*PWPHY12345*ZZ*POCID
*ZZ*S00000000000001*091217*0309*^*00501*000000001*1*P*>~
In the example above, the asterisk (*) is a delimiter based on its position immediately following ISA.
The segment delimiter is determined by calculating the last character of the fixed width row. The
row is 106 total bytes; therefore, the segment delimiter is the 106th character.
Choosing a Delimiter
Surescripts has published a list of allowed delimiters for the X12 messages (Refer to Appendix A:
Dynamic Delimiters for a full list of acceptable characters). The customers may choose any allowed
delimiter desired for the messages they create. However, it is important that customers
communicate which delimiters they are using to ensure they will not cause issues with their trading
partners’ messages.
Surescripts recommends the following delimiters for X12 data:
l Data Element Separator – hex 1D, decimal 29
l Segment Terminator – hex 1E, decimal 30
l Component Element Separator (ISA 16) – hex 1C, decimal 28
l Repetition Character (ISA11) – hex 1F, decimal 31
Using Dynamic Delimiters
A Surescripts customer can expect to receive delimiters that are different than the set they define
for their messages. The customer needs to determine the delimiters dynamically when the
message is processed according to the rules listed in the above section. See Appendix A: Dynamic
Delimiters for a complete list of acceptable characters.
3.4.2 DELIMITER EXAMPLES
The delimiters used in the examples below are the ~ for segment separation and the * for element
separation.
Example 1:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 15
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
NM1*IL*1*SMITH*JOHN*L***34*444115555~
Elements 6 and 7 are not included; therefore, the asterisks (**) act as placeholders for the omitted
elements.
When data elements are omitted from the end of a segment, the data element delimiters do not
need to be used. The segment is ended with a segment terminator.
Example 2:
Elements 8 and 9 can be omitted in the same segment as Example 1. The new segment would
become:
NM1*IL*1*SMITH*JOHN*L~
And not:
NM1*IL*1*SMITH*JOHN*L****~
Example 3:
Surescripts does not publish segments that are HIPAA compliant but not utilized by Surescripts. If
a message contains these segments, it will still be valid and accepted; but the data within the
segment may not be utilized.
ABC*ABC01*ABC02*ABC03*ABC04*ABC05*ABC06~
If elements ABC02 and ABC03 are not used (not shown on the Surescripts EDI specifications)
then no value should be sent. However, the elements must be represented with a place holder
because there are used elements (ABC04, 05 and 06) after them.
This is the correct representation:
ABC*ABC01***ABC04*ABC05*ABC06~
ABC02 and ABC03 must be represented so that it is known that the next data value is ABC04.
This is the INCORRECT representation:
ABC*ABC01*ABC04*ABC05*ABC06~
If the placeholders for ABC02 and ABC03 are removed, ABC04 would be mistaken for ABC02.
3.4.3 REPRESENTATION
The following table lists the Field Type Notation used within the messages:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 16
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
Type X12 Notation
Alphanumeric AN
Date DT
Decimal R
ID Number ID
Numeric Nn
String AN
Time TM
Each element, if sent, has a minimum and maximum length.
For example:
AN 1/3 means an alphanumeric with range from one to three characters.
AN 3/3 means an alphanumeric with three characters.
3.4.3.1 NUMERIC REPRESENTATION
The decimal point is represented by a period and should be used as follows:
l only when there are significant digits to the right of the decimal
l when there is a digit before and after the decimal point
l not with whole numbers
For example, consider the following possible values for a 5-digit field:
Correct: 2.515 251.5 25.15 2515 0.2515 2.5
Incorrect: .2515 2515. 3.00
Character Set
The character set contains ASCII values 32 – 126, which include:
Symbols ! " # $ % & ' ( ) * + , - . / : ; < = > ? @ [ \ ] ^ _ ` { | } ~
Numerals Ø to 9
Letters, upper and lower case A to Z, a to z
For ID File Load only:
l The decimal 94 ^ cannot be used in the ID Load process.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 17
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
3.5 MESSAGE VALIDATION
Surescripts will ensure that customers are in compliance with the message specifications outlined
in this Guide during Integration Testing and will continue to enforce once in production.
At a minimum, Surescripts validations include:
l The sender identification and authentication
l The recipient identification
l Syntax of the message, including field lengths, data types, and code values
l Surescripts business rules
Note: Surescripts ACRs are not enforced as part of validations, but instead through the
certification process.
3.6 FAILURE MODE/RESPONSE APPROACH
Surescripts’ error processing approaches are defined below.
3.6.1 ERROR PROCESSING FOR 270 AND 271
When a network communication or system failure occurs between the originating customer and
Surescripts, an error message will not be returned to the customer. Customers should establish a
timeout parameter to allow their system to recover in the event that Surescripts does not respond.
Surescripts has defined four different levels of failure for exchanging errors with the customer.
NAK: In instances where Surescripts or a customer receives a message that is unrecognizable or
a system error occurs, the recipient will send back an XML formatted NAK.
The NAK is an XML formatted message. Error (NAK) <nak status=”n”>Text Message</nak>
Message Type Status Error Message
NAK 1 Invalid Syntax Transaction cannot be identified nor processed
NAK 3 Transaction Timeout Transaction Timeout
NAK 4 System Error System Error
An example of a nak: <nak status=”4”> System Error </nak>
TA1: The TA1 acknowledges the receipt of a message. It validates the syntax of the interchange
ISA and IEA segments. It notifies the sender that the receiver got the message, or it reports errors
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 18
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 3: Messages Overview
so the sender is aware of interchange problems. Surescripts utilizes the TA1 to only report errors.
Surescripts only utilizes the TA1 to report errors when an error occurs within the header.
999: The 999 message reports functional problems to the sender. The sender will receive a 999
when a syntax error occurs in the body of the message or if the sender participant ID is invalid.
ACK: The ACK message is a small XML file, containing <ack status=”y”/>, which serves as the
PBM/Payer’s acceptance of the 999 message.
271: When a non-syntax error occurs during processing of a 270 message, AAA segments in the
271 will be used to report the errors.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 19
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
SECTION 4: ELIGIBILITY MESSAGING
This section provides guidelines for the data messaging interfaces between the provider vendor
and PBM/payers. Standard segments will be required for commonly transmitted data such as basic
patient demographics and eligibility information.
The Patient and Eligibility Data will be transmitted between the provider vendor system,
Surescripts, and PBM/payer using the currently accepted X12 envelope segments. Message
formats used include the X12N 270 (Health Care Eligibility Benefit Inquiry) and the X12N 271
(Health Care Eligibility Benefit Response).
The requester is a provider vendor system, and the eligibility responder is a PBM/payer.
4.1 RELATIONSHIP TO X12N 270/271 STANDARD
All eligibility inquiries and responses sent to Surescripts by customers must comply with the X12N
standard for eligibility for a health plan mandated under HIPAA by the Department of Health and
Human Services (the "270/271 Implementation Guide"). The descriptions in this section of 270
transactions and the 271 transactions clarify the information that Surescripts expects to be included
in 270 transactions and 271 transactions exchanged with Surescripts. Nothing in these
Specifications are intended or shall be deemed to: (a) change the definition, data condition, or use
of a data element or segment in a HIPAA-mandated standard; (b) add any data elements or
segments to the maximum defined data set of a HIPAA-mandated standard; (c) use any code or
data elements that are either marked "not used" in the 270/271 Implementation Guide; or (d)
change the meaning or intent of the 270/271 Implementation Guide.
The guidelines for data messaging interfaces provided in this document are tailored to the needs of
Physician System and PBM/payer customers related to prescription drug benefits and are a subset
of the X12N 270/271 standard. The X12N 270/271 standard covers a great number of other
business scenarios that are not described in this section; however, Surescripts will support the
minimum requirements of the X12N 270/271 transaction. See Section 1.4.7 of the 270/271
Implementation Guide (“Implementation Compliant Use of the 270/271 Transaction Set”).
Note: Even though Surescripts has implemented a subset of the X12N 270/271 standard,
customers should be able to handle receiving all the segments, elements and related codes
contained in the HIPAA X12N 270/271 standard. Refer to the Document References for the
exact reference guides needed.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 20
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
If a provider vendor's customer submits an eligibility request that does not comply with the X12N
270/271 transaction standard, Surescripts will return a 999 response. If a Physician System
customer submits an eligibility request that complies with the X12N 270/271 transaction but
contains information that is unexpected by Surescripts, Surescripts will return a 271 response
based on the information received by Surescripts that was expected, but the response may include
AAA segments if insufficient information expected by Surescripts is submitted to generate a
meaningful response.
If a PBM/payer customer submits an eligibility response that does not comply with the X12N
270/271 transaction standard, Surescripts will return a 999 response to the PBM/payer. The
response to the PBM/payer should be responded to with an ACK. If a PBM/payer customer
submits an eligibility response that complies with the X12N 270/271 transaction but contains
information that is unexpected by Surescripts, Surescripts will pass the response to the requesting
prescriber system customer. However, PBM/payer customers should be aware that such
responses may not be understood or usable by the recipient prescriber system customer.
4.2 PATIENT MATCH VERIFICATION
The specific fields that are used to match the patient are listed below. Only valid patient data should
be entered. Invalid data or filler data may result in “patient not found” or an incorrect match.
l Last Name NM103
l First Name NM104 – Use formal name. Do not use nicknames.
l Middle Name NM105
l Suffix NM107 – If relevant, the name suffix should be included in this field.
l Street Address N301
l City N401
l State N402
l Zip N403
l DOB DMG02
l Gender DMG03
4.2.1 INSUFFICIENT INFORMATION
In the event that insufficient identifying elements are sent to Surescripts to uniquely identify a
patient, Surescripts returns an Eligibility Response (271) with an AAA segment identifying
“Subscriber/Insured Not Found” or “Patient Not Found” and sends recommendations for future
searches, if appropriate.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 21
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
4.2.2 NON-UNIQUE MATCH
In the event that multiple patients are found for the submitted data elements and a unique match
cannot be determined, Surescripts returns an Eligibility Response (271) with an AAA segment
identifying “Subscriber/Insured Not Found or Patient Not Found” and, if possible, lists the missing
data elements needed to help identify an exact patient match.
PBM/payers assign a unique ID to each covered member. For this reason, customers should use
the subscriber loop since each member is being treated as a subscriber according to the standard.
Note: PBM/payers should always return the data they had in their system in the Eligibility
Response (271) and not echo back what was sent in the Eligibility Request (270).
If any of the demographic fields listed above are different from what the provider vendor sent, the
PBM/Payer must return a change flag. If a field comes in blank and the PBM/payer sends back a
value, this is considered a change. However, if the provider vendor sends a value in a field and the
PBM/payer is unable to compare this field because they do not store this field in their patient data,
the change flag must not be set and the data from the request must not be returned.
The change flag is in the INS segment. INS03 = 001, INS04 = 25.
In the case of error conditions including patient not found - AAA error 75, contract /authorization
error - AAA error 41, and general system errors – AAA error 42, do not send back patient
information from the Eligibility Request (270) request. Therefore, in these error conditions, no
patient data should be sent back. The provider vendor should disregard any patient information
under these error scenarios.
Examples:
1. This is an example where the PBM/payer should indicate that a change has been made and
set the change flag in the INS segment.
Provider vendor sends in: Joe M Doe, DOB 19550412, Gender Male, and Address 55
HIGH STREET, SEATTLE, WA 55111
PBM/payer returns: Joseph M Doe, DOB 19550412, Gender Male, and Address 55 HIGH
STREET, St. Paul, MN 55111
2. In this example, the PBM/payer does not need to set the change flag because they have not
changed any of the information returned, but the middle initial is blank due to the field not
being supported in the PBM/payer’s system:
Provider vendor sends in: Joe M Doe, DOB 19550412, Gender Male, and Address 55
HIGH STREET, St. Paul MN, 55111
PBM/payer returns: Joe Doe, DOB 19550412, Gender Male, and Address 55 HIGH
STREET, St. Paul MN, 55111
3. In this example, the PBM/payer looks up the information and finds a blank for the middle
name (which is a supported field in the PBM/payer’s system). This is considered a change so
the change flag needs to be set:
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 22
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Provider vendor sends in: Joe M Doe, DOB 19550412, Gender Male,
PBM/payer returns: Joe Doe, DOB 19550412, Gender Male,
4. This is an example where the patient is not found, so none of the patient information is
returned.
Provider vendor sends in: Joe M Doe, DOB 19550412, Gender Male, and Address 55
HIGH STREET, St. Paul MN 55111
PBM/payer returns: No Patient Data and an AAA segment with error 75 –
Subscriber/Insured Not Found.
4.3 270 ELIGIBILITY, COVERAGE, OR BENEFIT INQUIRY
Introduction
Code Description
R Required/Mandatory - the segment must be used per the specification.
S Situational/Conditional – the segment must be used if conditions are met. Some fields do not have
specific conditions. Data should be sent if available.
This section contains a subset of information on the Eligibility, Coverage or Benefit Inquiry
Transaction Set (270) for use within the context of an ePrescribing environment.
Note: This Guide only includes data elements where Surescripts has specific requirements or
further explains the field usage. Refer to the X12 implementation guide for a complete list of
segments and elements. In addition, comments below where codes are specified are either to
call out Surescripts notes and/or to show the code recommended by Surescripts. For a full list of
codes, please refer to the X12 guide.
Since PBM/payers uniquely identify each member, the subscriber level should be used
instead of the dependent level. However, receivers of the 270 should be able to handle
patients at the dependent level since the standard allows it.
Req
Seg ID Name
Des
Header
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 23
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA Interchange Control Header R
ISA01Authorization Information Qualifier
l Value:
00 – No Authorization Information Present (No Meaningful Information in I02)
ISA02 Authorization Information:
l Not used. Fill with blanks.
ISA03 Security Information Qualifier
l Code to identify the type of information in the Security Information.
l Value:
01 - Password
ISA04 Security Information
l From the provider vendor, this is the Password assigned by Surescripts for the
provider vendor.
l From Surescripts, this is the password Surescripts uses when sending to the
PBM/Payer.
ISA05 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA06 Interchange Sender ID
l From the provider vendor system, this is the Participant ID as assigned by
Surescripts.
l From Surescripts to the PBM/payer, this is Surescripts’ ID.
ISA07 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA08 Interchange Receiver ID
l The provider vendor system must use the Surescripts ID designated by Surescripts
Integration for the customer’s specific use case.
l From Surescripts to the PBM/payer, this is PBM/payer's Participant ID.
ISA09 Interchange Date
l Date format YYMMDD required.
ISA10 Interchange Time
l Time format HHMM required.
ISA11 Repetition Separator
l Surescripts recommends using Hex 1F.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 24
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA12 Interchange Control Version Number
l This version number covers the interchange control segments.
l 00501 – Standards Approved for Publication by ASC X12 Procedures Review Board
through October 2003
ISA13 Interchange Control Number
l From the provider vendor system, this is a unique ID assigned by the provider
vendor system for transaction tracking.
l From Surescripts, this is a unique ID assigned by Surescripts for transaction
tracking.
l This ID will be returned on a TA1 if an error occurs. Providing a unique number will
assist in resolving errors and tracking messages.
ISA14 Acknowledgement Requested
l Since these transactions are real time only, Surescripts does not use this field to
determine whether to create a TA1 acknowledgment.
l Value:
0 – No Acknowledgment Requested (Recommended by Surescripts)
ISA15 Interchange Usage Indicator
l Values
P – Production Data
T – Test Data
ISA16 Component Element Separator
l Surescripts recommends using Hex 1C.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 25
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
GS Functional Group Header R
GS01 Functional Identifier Code
l Functional Group Value: HS
GS02 Application Sender’s Code
l From the provider vendor system, this is the Participant ID as assigned by
Surescripts.
l From Surescripts to PBM/payer, this is Surescripts’ ID.
GS03 Application Receiver’s Code
l The provider vendor system must use the Surescripts ID designated by Surescripts
Integration for the customer’s specific use case.
l From Surescripts to PBM/payer, this is PBM/payer's Participant ID.
GS06 Group Control Number
l The control number should be unique across all groups within this transaction set.
This ID will be returned on an AK102 of the 999 acknowledgment if an error occurs.
Providing unique numbers will assist in resolving errors and tracking messages.
Avoid using leading zeros in this field.
ST Transaction Set Header R
ST02 Transaction Set Control Number
l Identifying control number that must be unique within the transaction set
functional group assigned by the originator for a transaction set.
l The transaction set control numbers in ST02 and SE02 must be identical. This
unique number also aids in error resolution research. Start with the number, for
example "0001", and increment from there. This number must be unique within a
specific group and interchange, but can repeat in other groups and interchanges.
l Note: This ID will be returned on an AK202 of the 999 acknowledgment if an error
occurs. Providing a unique number will assist in resolving errors and tracking
messages.
BHT Beginning of Hierarchical Transaction R
BHT02 Transaction Set Purpose Code
l Value:
13 – Request (Surescripts customers utilize this option only.)
BHT03 Reference Identification
l Because Surescripts only supports Real Time, this element is required.
Detail
LOOP ID – 2000A INFORMATION SOURCE LEVEL
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 26
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
HL Information Source Level (PBM/payer) R
LOOP ID – 2100A INFORMATION SOURCE NAME
NM1 Information Source Name R
NM101 Entity Identifier Code
l Value:
2B – Third-Party Administrator (Recommended by Surescripts)
NM102 Entity Type Qualifier
l Value:
2 – Non-Person Entity (Recommended by Surescripts)
NM103 Name Last
l From the provider vendor system, the source is unknown so this would be
Surescripts.
l From Surescripts, Surescripts will place the source name here.
NM108 Identification Code Qualifier
l Value:
PI – Payer Identification (Recommended by Surescripts)
NM109 Identification Code
l The provider vendor system must use the Surescripts ID designated by Surescripts
Integration for the customer’s specific use case.
l From Surescripts to PBM/payer, Surescripts will place the Participant ID of the
PBM/payer's here.
LOOP ID – 2000B INFORMATION RECEIVER LEVEL
HL Information Receiver Level (Physician) R
LOOP ID – 2100B INFORMATION RECEIVER NAME
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 27
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
NM1 Information Receiver Name R
NM101 Entity Identifier Code
l Value:
1P – Provider (Recommended by Surescripts)
NM102 Entity Type Qualifier
l Value:
1 – Person (Recommended by Surescripts)
NM103 Name Last or Organization Name
l Physician Name
NM108 Identification Code Qualifier
l Qualifier:
XX – Centers for Medicare and Medicaid Services National Provider Identifier.
NM109 Identification Code
l The NPI is mandated. Surescripts will reject if the NM108 and the NM109 are not
populated.
l The NPI check digit will be validated using the LUHN formula. For specific
information see https://www.cms.gov/Regulations-and-Guidance/Administrative-
Simplification/NationalProvIdentStand/Downloads/NPIcheckdigit.pdf.
l Must be a valid 10 digit NPI.
REF Information Receiver Additional Identification (Physician System Identification) S
REF01 Reference Identification Qualifier
l Value:
EO – Submitter Identification Number (A unique number identifying the submitter of
the transaction set.)
REF02 Reference Identification
l Surescripts defined Participant ID for the provider vendor system.
REF03 Description
l Must not be used for the EO qualifier.
N3 Information Receiver Address S
N4 Information Receiver City/State/ZIP Code S
Note: State (N402) and Postal Code (N403) are required if City Name (N401) is in the U.S.
or Canada.
N404 Country Code
l Do not send the US Country Code.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 28
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
LOOP ID – 2000C SUBSCRIBER LEVEL
HL Subscriber Level R
TRN Subscriber Trace Number S
LOOP ID – 2100C SUBSCRIBER NAME
NM1 Subscriber Name R
NM108 Identification Code Qualifier
l From the provider vendor system this is blank. Surescripts will put the Qualifier "MI"
into this field.
l Value:
MI - Member Identification Number
NM109 Identification Code
l From the provider vendor system this is blank. Surescripts will put the PBM Unique
Member ID into this field.
REF Subscriber Additional Identification (SSN#, Person Code) S
N3 Subscriber Address S
N4 Subscriber City/State/ZIP Code S
Note: State (N402) and Postal Code (N403) are required if City Name (N401) is in the U.S.
or Canada.
N404 Country Code
l Do not send US Country Code.
DMG Subscriber Demographic Information S
DTP Subscriber Date S
Note: Absence of a Plan date indicates the request is for the date the transaction is
processed and the information source is to process the transaction in the same manner as
if the processing date was sent.
The Eligibility Date of Service and the Eligibility Transmission Date must be within three (3)
days of the patient interaction (Past and Future).
LOOP ID - 2110C SUBSCRIBER ELIGIBILITY OR BENEFIT INQUIRY
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 29
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
EQ Subscriber Eligibility or Benefit Inquiry Information (Health Benefit Plan Coverage) S
EQ01 Service Type Code
l Value:
30 – Health Benefit Plan Coverage (Recommended by Surescripts)
l Instead of specifying a specific service type code, this code allows the information
source to respond with all the relevant service types. If other service types are sent,
the responder will only respond to pharmacy-related coverages.
l An information source may support the use of Service Type Codes other than “30"
(Health Benefit Plan Coverage) in EQ01 at their discretion.
Trailer
SE Transaction Set Trailer R
GE Functional Group Trailer R
IEA Interchange Control Trailer R
4.4 271 ELIGIBILITY, COVERAGE, OR BENEFIT INFORMATION
This section contains a subset of information on the Eligibility, Coverage or Benefit Information
Transaction Set (271) for use within the context of ePrescribing.
PBM/payer's uniquely identify each patient, thus the subscriber level should be used instead of the
dependent level. However, receivers of the Eligibility Request (270) should be able to handle
patients at the dependent level since the standard allows it. Also, when the patient is submitted in
the dependent loop (in 270) they must be returned in the subscriber loop (in 271). This is due to the
fact that PBM/payer's assign unique identifiers to all members thus they are deemed to be
subscribers according to the standard.
Note: This Guide only includes data elements where Surescripts has specific requirements or
further explains the field usage. Refer to the X12 implementation guide for a complete list of
segments and elements. In addition, comments below where codes are specified are either to
call out Surescripts notes and/or to show the code recommended by Surescripts. For a full list of
codes, please refer to the X12 guide.
Req
Seg ID Name
Des
Header
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 30
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA Interchange Control Header R
ISA01 Authorization Information Qualifier
l Value:
00 – No Authorization Information Present (No Meaningful Information in I02)
ISA02 Authorization Number
l Not used. Fill with blanks.
ISA03 Security Information Qualifier
l Code to identify the type of information in the Security Information.
l Value:
01 - Password
ISA04 Security Information
l From the PBM/payer to Surescripts, this is the Surescripts system assigned
password to the PBM/payer.
l From Surescripts, this is the password Surescripts uses when sending to the
provider vendor.
ISA05 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA06 Interchange Sender ID
l From the PBM/payer to Surescripts, this is the PBM/payer's Participant ID.
l From Surescripts to the provider vendor system, this is Surescripts’ ID.
ISA07 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA08 Interchange Receiver ID
l From the PBM/payer, this is Surescripts’ ID.
l From Surescripts to the provider vendor system, this is the provider vendor’s
Participant ID.
ISA09 Interchange Date
l Date format YYMMDD required.
ISA10 Interchange Time
l Time format HHMM required.
ISA11 Repetition Separator
l Surescripts recommends using Hex 1F.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 31
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA12 Interchange Control Version Number
l This version number covers the interchange control segments.
l 00501 – Standards Approved for Publication by X12 Procedures Review Board
through October 2003
ISA13 Interchange Control Number
l From the PBM/payer, this is the PBM/payer's unique identification of this
transaction.
l From Surescripts, this is Surescripts’ unique identification of this transaction.
l This number is returned on a TA1 if an error occurs. Providing a unique number will
assist in resolving errors and tracking messages.
ISA14 Acknowledgement Requested
l The TA1 segment will only be transmitted in the event of a header or trailer ERROR.
l TA1 segments should not be returned for accepted transactions. If there are no
errors at the envelope level (ISA, GS, GE, IEA segments) then TA1 segments
should not be returned.
l Since these transactions are real time only, Surescripts does not use this field to
determine whether to create a TA1 acknowledgment.
ISA15 Interchange Usage Indicator
l Values
P – Production Data
T – Test Data
ISA16 Component Element Separator
l Surescripts recommends using Hex IC.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 32
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
GS Functional Group Header R
GS01 Functional Identifier Code
l Functional Group Value:
HB
GS02 Application Sender’s Code
l From the PBM/payer, this is the PBM/payer's Participant ID.
l From Surescripts, this is Surescripts’ ID.
GS03 Application Receiver’s Code
l From the PBM/payer to Surescripts, this is Surescripts’ ID.
l From Surescripts to the provider vendor system, this is the provider vendor’s
Participant ID.
GS06 Group Control Number
l The control number should be unique across all functional groups within this
transaction set.
l This number is returned on an AK102 of the 999 acknowledgment if an error occurs.
Providing a unique number will assist in resolving errors and tracking messages.
ST Transaction Set Header R
ST02 Transaction Set Control Number
l This ID will be returned on an AK202 of the 999 acknowledgment if an error occurs.
Providing a unique number will assist in resolving errors and tracking messages.
BHT Beginning of Hierarchical Transaction R
BHT03 Reference Identification
l Because this Implementation is Real Time, this number from the 270 is to be
returned in this field.
Detail
LOOP ID – 2000A INFORMATION SOURCE LEVEL
HL Information Source Level (PBM/payer) R
AAA Request Validation S
AAA03 Reject Reason Code
l Value:
42 – Unable to Respond at Current Time
Note: Surescripts could not process the transaction.
LOOP ID – 2100A INFORMATION SOURCE NAME
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 33
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
NM1 Information Source Name R
NM101 Entity Identifier Code
l Value:
2B – Third-Party Administrator (Recommended by Surescripts)
NM102 Entity Type Qualifier
l Value:
2 – Non-Person Entity (Recommended by Surescripts)
NM103 Organization Name
l This is the name of the PBM/payer that provides the data. It does not include
Surescripts at any point.
NM108 Identification Code Qualifier
l Surescripts will utilize PI to identify the Payer (the PBM/payer).
l Value:
PI – Payer Identification (Recommended by Surescripts)
NM109 Identification Code
l This is the PBM/payer’s Participant ID.
AAA Request Validation S
AAA03 Reject Reason Code
l Values:
41 – Authorization/Access Restrictions
To the provider vendor system from Surescripts, 41 would indicate that the
provider vendor system cannot request transactions for the identified
PBM/payer.
To Surescripts from the PBM/payer, 41 would indicate that Surescripts
cannot request eligibility from this PBM/payer.
42 – Unable to Respond at Current Time
PBM/payer cannot process at current time.
79 – Invalid Participant Identification
The PBM/payer will use this code to indicate that Information Source
Identified in Loop 2100A is invalid.
LOOP ID – 2000B INFORMATION RECEIVER LEVEL
HL Information Receiver Level(Physician) S
LOOP ID – 2100B INFORMATION RECEIVER NAME
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 34
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
NM1 Information Receiver Name R
NM101 Entity Identifier Code
l Value:
1P – Provider (Recommended by Surescripts)
NM102 Entity Type Qualifier
l Value:
1 – Person (Recommended by Surescripts)
NM108 Identification Code Qualifier
l Qualifier:
XX – Centers for Medicare and Medicaid Services National Provider Identifier.
NM109 Identification Code
l The NPI is mandated. Surescripts will reject if the NM108 and the NM109 are not
populated.
l The NPI check digit will be validated using the LUHN formula. For specific
information see https://www.cms.gov/Regulations-and-Guidance/Administrative-
Simplification/NationalProvIdentStand/Downloads/NPIcheckdigit.pdf.
l Must be a valid 10 digit NPI.
REF Information Receiver Additional Identification (Physician System Identification) S
Note: Surescripts defined Participant ID for the provider vendor system.
REF01 Reference Identification Qualifier
l Value:
EO – Submitter Identification Number (A unique number identifying the submitter of
the transaction set.)
REF02 Reference Identification
l Surescripts defined Participant ID for the provider vendor system.
REF03 Description
l Not used for the EO qualifier.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 35
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
AAA Information Receiver Request Validation S
AAA03 Reject Reason Code
l Values:
15 – Required application data missing
Use this code only when the information receiver’s additional identification
is missing. (Not enough information given to identify the provider vendor
system.)
41 – Authorization/Access Restrictions (A contract does not exist between this
provider vendor system and the PBM/payer to exchange eligibility information.)
43 – Invalid/Missing Provider Identification (Surescripts recommends this for NPI
error.)
79 – Invalid Participant Identification. (Surescripts cannot validate the receiver.)
LOOP ID – 2000C SUBSCRIBER LEVEL
HL Subscriber Level S
TRN Subscriber Trace Number S
LOOP ID – 2100C SUBSCRIBER NAME
NM1 Subscriber Name R
NM103 Name Last
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
NM104 Name First
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
NM105 Name Middle
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
NM107 Name Suffix
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
NM108 Identification Code Qualifier
l Value:
MI - Member Identification Number
NM109 Identification Code
l Subscriber PBM Unique Member ID.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 36
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
REF Subscriber Additional Identification (Person Code, Cardholder ID, SSN, Patient Account S
Number)
REF01 Reference Identification Qualifier
l Value:
49 – Family Unit Member (Person Code)
N3 Subscriber Address S
N301 Address Information
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
N302 Address Information
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
N4 Subscriber City/State/ZIP Code S
N401 City Name
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
N402 State or Province Code
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
N403 Postal Code
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
N404 Country Code
l Do not send US Country Code.
AAA Subscriber Request Validation S
AAA03 Reject Reason Code
l Value:
15 – Required application data missing
At Surescripts – Not enough information for Surescripts to identify patient.
At PBM/payer – Wants more information than what was supplied.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 37
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
DMG Subscriber Demographic Information S
DMG02 Date Time Period
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
DMG03 Gender Code
l This data is to be returned from the PBM/payer system, and should not be echoed
back from the 270.
INS Subscriber Relationship S
INS01 Yes/No Condition or Response Code
l For the Physician System, this will always be Yes (Y), if supplied.
INS02 Individual Relationship Code
l For the Physician System, this will always be Self (18).
INS03 Maintenance Type Code
l Code identifying the reason for the maintenance change.
l Use this element (and code “001” in INS03) if any of the identifying elements for the
subscriber have been changed from those submitted in the 270.
l Value:
001 - Change
INS04 Maintenance Reason Code
l Code identifying the reason for the maintenance change.
l Use this element (and code “001” in INS03) if any of the identifying elements for the
subscriber have been changed from those submitted in the 270.
l Value:
25 - Change in Identifying Data Elements
Use this code to indicate that a change has been made to the primary
elements that identify a specific person. Such elements are first name, last
name, date of birth, identification numbers, and address.
DTP Subscriber Date S
DTP02 Date Time Period Format Qualifier
l Value:
D8 – Date Expressed in Format CCYYMMDD (Surescripts recommends D8.)
LOOP ID – 2110C SUBSCRIBER ELIGIBILITY OR BENEFIT INFORMATION
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 38
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
EB Subscriber Eligibility or Benefit Information. This segment indicates active and inactive S
coverage.
If the first iteration of the EB loop is set to “1” (Active), then use one loop for retail, one for
mail order, and optionally, one for specialty pharmacy, and/or LTC. If the EB loop is set to
“6” (Inactive), then no other EB loops are required.
EB01 Eligibility or Benefit Information
l Code identifying eligibility or benefit information.
l Values:
1 - Active Coverage
6 - Inactive
If the member is inactive, then no other EB loops are required to be sent.
V - Cannot Process
G - Out of Pocket (Stop Loss)
I - Non-covered
EB03 Service Type Code
l Values:
88 – Pharmacy (Retail Benefit)
90 – Mail Order Prescription Drug
Empty/Null – Specialty Pharmacy or LTC (See MSG.)
EB05 Plan Coverage Description
l The health plan name for patients that are eligible should be sent at this level.
l Surescripts requires applications display this if sent.
EB07 Monetary Amount
l Surescripts is utilizing this field for Out of Pocket Accumulator. EB01 set to G.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 39
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
REF Subscriber Additional Identification (Plan ID, Group ID/Name, Formulary ID, Alternative S
ID, Coverage List ID, BIN/PCN, and Copay ID)
REF01 Code Qualifying the Reference Identification
l Values:
18 – Plan ID
6P – Group Number
ALS – Alternate List ID
CLI – Coverage List ID
FO – Drug Formulary Number ID
IG – Insurance Policy Number (Copay ID)
N6 – Plan Network ID (*BIN (aka IIN)/PCN) (Strongly recommended by
Surescripts.)
REF03 Description
l This element should only be used for Group Name and/or PCN number.
l REF01=6P (This is the group name.)
l REF01=N6 (This is the PCN Number.)
l Note: Group number (6P) refers to the prescription benefit coverage Group ID
(which is typically 15 characters or less), not the Member Plan Group ID Number
that refers to Medical, Dental, etc. coverage.
DTP Subscriber Eligibility/Benefit Date S
Note: Surescripts recommends sending back the date range of the health plan benefit for
this patient’s coverage.
DTP02 Date Time Period Format Qualifier
l Value:
RD8 – Range of Dates expressed in Format CCYYMMDD-CCYYMMDD
(Surescripts recommends RD8.)
AAA Subscriber Request Validation S
MSG Message Text S
MSG01 Free-Form Message Text
l This free text field will be populated by Surescripts as a hint to the requester on what
fields would assist in identifying the patient. This is sent if patient is not found and
one or more of the following fields are missing; first name, last name, zip code or
date of birth.
LS Loop Header S
LOOP ID – 2120C SUBSCRIBER BENEFIT RELATED ENTITY NAME
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 40
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
NM1 Subscriber Benefit Related Entity Name S
NM101 Entity Identifier Code
l Values:
13 – Contracted Service Provider (Use for Mail Only Benefit. Used to further clarify
benefits, including Mail Only, Specialty and Long Term Care.)
NM102 Entity Type Qualifier
l Values:
2 – Non-Person Entity (Surescripts recommends using 2)
NM108 Identification Code Qualifier
l Value:
SV – Service Provider Number (Recommended by Surescripts)
Use this code for the identification number assigned by the information source.
LE Loop Trailer S
Trailer
SE Transaction Set Trailer R
GE Functional Group Trailer R
IEA Interchange Control Trailer R
4.5 TA1 INTERCHANGE ACKNOWLEDGEMENT
ICS Interchange Control Structures
Introduction
The purpose of this standard is to define the control structures for the electronic interchange of one
or more encoded business transactions including the EDI (Electronic Data Interchange) encoded
transactions of Accredited Standards Committee X12. This standard provides the interchange
envelope of a header and trailer for the electronic interchange through a data transmission, and it
provides a structure to acknowledge the receipt and processing of this envelope.
Note: This Guide only includes data elements where Surescripts has specific requirements or
further explains the field usage. Refer to the X12 implementation guide for a complete list of
segments and elements. In addition, comments below where codes are specified are either to
call out Surescripts notes and/or to show the code recommended by Surescripts. For a full list of
codes, please refer to the X12 guide.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 41
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA Interchange Control Header R
ISA01Authorization Information Qualifier
l Value:
00 – No Authorization Information Present (No Meaningful Information in I02)
ISA02 Authorization Information
l Not used. Fill with blanks.
ISA03 Security Information Qualifier
l Code to identify the type of information in the Security Information.
l Value:
01 - Password
ISA04 Security Information
l Password utilized by the sender to access the receiver system.
ISA05 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA06 Interchange Sender ID
l The Sender Participant ID. Participant ID is the Surescripts system
Participant ID.
ISA07 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA08 Interchange Receiver ID
l The Receiver Participant ID. Participant ID is assigned by Surescripts.
ISA09 Interchange Date
l Date format YYMMDD required.
ISA10 Interchange Time
l Time format HHMM required.
ISA11 Repetition Separator
l Surescripts recommends using Hex 1F.
ISA12 Interchange Control Version Number
l This version number covers the interchange control segments.
l 00501 – Standards Approved for Publication by ASC X12 Procedures Review
Board through October 2003
ISA13 Interchange Control Number
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 42
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
l A unique number assigned by the sender. Used to communicate from the
receiver back to the sender to identify this transaction.
ISA14 Acknowledgment Requested
l No TA1s are returned for TA1s.
ISA15 Interchange Usage Indicator
l Values
P – Production Data
T – Test Data
ISA16 Component Element Separator
l Surescripts recommends using Hex 1C.
TA1 Interchange Acknowledgment S
Note: Surescripts only supports the TA1 for errors. It is not sent as an
acknowledgment for successful messages.
IEA Interchange Control Trailer R
4.6 999 IMPLEMENTATION ACKNOWLEDGEMENT FOR HEALTH CARE
INSURANCE
Note: This Guide only includes data elements where Surescripts has specific requirements or
further explains the field usage. Refer to the X12 implementation guide for a complete list of
segments and elements. In addition, comments below where codes are specified are either to
call out Surescripts notes and/or to show the code recommended by Surescripts. For a full list of
codes, please refer to the X12 guide.
Req
Seg ID Name
Des
Header
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 43
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
ISA Interchange Control Header R
ISA01Authorization Information Qualifier
l Value:
00 – No Authorization Information Present (No Meaningful Information in I02)
ISA02 Authorization Number
l Information used for additional identification or authorization of the interchange
sender or the data in the interchange; the type of information is set by the
Authorization Information Qualifier (I01).
ISA03 Security Information Qualifier
l Code to identify the type of information in the Security Information
l Value:
01 - Password
ISA04 Security Information
l Password used by the sender to access the receiver system. Password assigned
by Surescripts.
ISA05 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA06 Interchange Sender ID
l From Surescripts to the PBM/payer, this is Surescripts’ ID.
ISA07 Interchange ID Qualifier
l Qualifier
ZZ - Mutually Defined
ISA08 Interchange Receiver ID
l The Receiver Participant ID. Participant ID is assigned by Surescripts.
ISA09 Interchange Date
l Date format YYMMDD required.
ISA10 Interchange Time
l Time format HHDD required.
ISA11 Repetition Separator
l Surescripts recommends using Hex 1F.
ISA12 Interchange Control Version Number
l This version number covers the interchange control segments.
l 00501 – Standards Approved for Publication by ASC X12 Procedures Review Board
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 44
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
through October 2003
ISA13 Interchange Control Number
l The sender’s unique identification of this transaction.
ISA14 Acknowledgment Requested
l No TA1s are returned for 999s.
ISA15 Interchange Usage Indicator
l Values
P – Production Data
T – Test Data
ISA16 Component Element Separator
l Surescripts recommends using Hex 1C.
GS Functional Group Header R
GS02 Application Sender’s Code
l The Sender Participant ID. Participant ID is assigned by Surescripts.
GS03 Application Receiver’s Code
l The Receiver Participant ID. Participant ID is assigned by Surescripts.
ST Transaction Set Header R
AK1 Functional Group Response Header R
LOOP ID - 2000 - AK2 TRANSACTION SET RESPONSE HEADER
AK2 Transaction Set Response Header S
AK203 Implementation Convention Reference
l Required when the ST03 value is available in the transaction set to which this 999
transaction set is responding.
l Since ST03 is required the AK203 must be present.
LOOP ID - 2100 - AK2/IK3 ERROR IDENTIFICATION
IK3 Error Identification S
CTX Segment Context S
CTX Business Unit Identifier S
LOOP ID - 2110 - AK2/IK3/IK4 IMPLEMENTATION DATA ELEMENT NOTE
IK4 Implementation Data Element Note S
CTX Element Context S
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 45
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Req
Seg ID Name
Des
IK5 Transaction Set Response Trailer R
IK501 Transaction Set Acknowledgment Code Value:
l R – Rejected (Surescripts recommends R.)
AK9 Functional Group Response Trailer R
AK901 Functional Group Acknowledgment Code Value:
l R – Rejected (Surescripts recommends use of R.)
Trailer
SE Transaction Set Trailer R
GE Functional Group Trailer R
IEA Interchange Control Trailer R
4.7 HIERARCHICAL LOOPS
The diagram below depicts the hierarchical organization of all loops and includes those related
specifically to the EB segments.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 46
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
4.8 270 AND 271 MESSAGE EXAMPLES
This is an example of a prescriber/clinic checking a patient’s benefit plan. The lifecycle consists of:
l Prescriber System creates the 270 and sends to Surescripts.
l Surescripts identifies the patient and sends a 270 to the PBM/payer.
l The PBM/payer processes the 270 and returns a 271 to Surescripts.
l Surescripts returns the 271 to the Prescriber System.
Note: In the examples, line breaks are used at the end of the segments for display purposes –
live transactions should not contain line breaks.
Eligibility Request (from Prescriber System to Surescripts)
ISA*00* *01*PWPHY12345*ZZ*POCID
*ZZ*S00000000000001*171217*0309*^*00501*000000001*1*P*>~
GS*HS*POCID*S00000000000001*20171217*16150000*1*X*005010X279A1~
ST*270*0001*005010X279A1~
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 47
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
BHT*0022*13*3920394930203*20171217*16150000~
HL*1**20*1~
NM1*2B*2*SURESCRIPTS LLC*****PI*S00000000000001~
HL*2*1*21*1~
NM1*1P*1*JONSON*TIM*T**M.D.*XX*3334444555~
REF*EO*POCID~
N3*55 HIGH STREET~
N4*SEATTLE*WA*98123~
HL*3*2*22*0~
NM1*IL*1*CROSS*DAVID*M~
N3*6785 LAUGHALOT LANE~
N4*TRENTON*NJ*08608~
DMG*D8*19720910*M~
DTP*291*D8*20171217~
EQ*30~
SE*17*0001~
GE*1*1~
IEA*1*000000001~
Segment Value Note
ISA PWPHY12345 The Password needed to correspond with the Surescripts’ system.
ISA POCID The Physician System’s Participant ID.
ISA S00000000000001 Participant ID for Surescripts.
BHT 3920394930203 The Transaction reference number that ties the request to the
response.
HL1:NM1 SURESCRIPTS Source does not know PBM/payer so they put in Surescripts.
LLC
HL2:NM1 TIM JONSON Dr.’s Name.
HL2:NM1 3334444555 Dr. Jonson NPI Number 3334444555.
HL3:NM1 DAVID CROSS David Cross is the patient.
EQ 30 Health Plan Benefit Coverage
Eligibility Request (from Surescripts to PBM/payer)
Note: Surescripts has located the patient and populated the PBM Unique Member ID.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 48
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
ISA*00* *01*PW12345PBM*ZZ*S00000000000001*ZZ*PBM123
*171217*0309*^*00501*000000001*1*P*>~
GS*HS*S00000000000001*PBM123*20171217*16150000*1*X*005010X279A1~
ST*270*0001*005010X279A1~
BHT*0022*13*3920394930203*20171217*16150000~
HL*1**20*1~
NM1*2B*2*PBM COMPANY*****PI*PBM123~
HL*2*1*21*1~
NM1*1P*1*JONSON*TIM*T**M.D.*XX*3334444555~
REF*EO*POCID~
N3*55 HIGH STREET~
N4*SEATTLE*WA*98123~
HL*3*2*22*0~
NM1*IL*1*CROSS*DAVID*M***MI*DD145645645601~
N3*6785 LAUGHALOT LANE~
N4*TRENTON*NJ*08608~
DMG*D8*19720910*M~
DTP*291*D8*20171217~
EQ*30~
SE*17*0001~
GE*1*1~
IEA*1*000000001~
Segment Value Note
ISA PW12345PBM The Password needed to correspond with the PBM/payer’s
system.
ISA S00000000000001 Surescripts’ ID.
ISA PBM123 The PBM/payer's Participant ID.
BHT 3920394930203 The Transaction reference number that ties the request to the
response.
HL1:NM1 PBM COMPANY Name of the Source (PBM/payer Name).
HL2:NM1 TIM JONSON Name of the Physician.
HL2:NM1 3334444555 Dr. Jonson NPI number 3334444555.
HL2:REF POCID Participant ID for the provider vendor.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 49
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Segment Value Note
HL3:NM1 DAVID CROSS David Cross with PBM Unique Member ID DD145645645601
DD145645645601
EQ 30 Health Plan Benefit Coverage.
Eligibility Response (from PBM/payer to Surescripts)
ISA*00* *01*PWPBM12345*ZZ*PBM123
*ZZ*S00000000000001*171217*0345*^*00501*000000001*1*P*>~
GS*HB*PBM123*S00000000000001*20171217*16150000*1*X*005010X279A1~
ST*271*0001*005010X279A1~
BHT*0022*11*3920394930203*20171217*16150000~
HL*1**20*1~
NM1*2B*2*PBM COMPANY*****PI*PBM123~
HL*2*1*21*1~
NM1*1P*1*JONSON*TIM*T**M.D.*XX*3334444555~
REF*EO*POCID~
HL*3*2*22*0~
NM1*IL*1*CROSS*DAVID*M***MI*DD145645645601~
REF*49*01~
N3*6785 LAUGHALOT LANE~
N4*TRENTON*NJ*08608~
DMG*D8*19720910*M~
INS*Y*18~
DTP*291*D8*20171217~
EB*1**30**PLANA~
REF*18*1234~
REF*6P*DD1*ABCGROUP~
REF*FO*201~
REF*CLI*201~
REF*N6*234876*AV~
REF*IG*201~
REF*ALS*142345~
DTP*291*RD8*20100801-20991231~
EB*1**88~
EB*1**90~
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 50
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
SE*27*0001~
GE*1*1~
IEA*1*000000001~
Segment Value Note
ISA PWPBM12345 The Password needed to correspond with the Surescripts’
system.
ISA PBM123 The PBM/payer’s Participant ID.
ISA S00000000000001 Participant ID for Surescripts.
BHT 3920394930203 The Transaction reference number that ties the request to the
response.
HL1:NM1 PBM COMPANY Name of the Source (PBM/payer Name).
HL2:NM1 TIM JONSON: 3334444555 Dr. Jonson with NPI number 3334444555.
HL2:REF POCID Participant ID for the Physician System.
HL3:NM1 DAVID CROSS: David Cross with PBM Unique Member ID
DD145645645601 DD145645645601.
HL3:REF 49 Family Unit Number
EB 1:30 1 This patient has coverage.
HL3:REF 18 Plan Number
HL3:REF 6P*DD1*ABCGROUP Group Number and Group Name
HL3:REF FO Formulary ID
HL3:REF CLI Coverage List ID
HL3:REF N6 Bin = 234876: Processor Control Number = AV
HL3:REF IG Copay ID
HL3:REF ALS Alternative List ID
EB1:88 1 Eligible for Retail Pharmacy Benefits
EB1:90 1 Eligible for Mail Order Pharmacy Benefits.
Eligibility Response (from Surescripts to Physician System)
ISA*00* *01*PW12345PHY*ZZ*S00000000000001*ZZ*POCID
*171217*0345*^*00501*000000001*1*P*>~
GS*HB*S00000000000001*POCID*20171217*16150000*1*X*005010X279A1~
The rest of this message is the same as the prior message Eligibility Response (from PBM/payer to
Surescripts).
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 51
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Segment Value Note
ISA PW12345PHY The Password needed to correspond with the Physician System’s
system.
ISA S00000000000001 Participant ID for Surescripts.
ISA POCID The Physician System’s Participant ID.
Eligibility Response (Not Active)
ISA*00* *01*PWPBM12345*ZZ*PBM123
*ZZ*S00000000000001*171217*0345*^*00501*000000001*1*P*>~
GS*HB*PBM123*S00000000000001*20171217*16150000*1*X*005010X279A1~
ST*271*0001*005010X279A1~
BHT*0022*11*3920394930203*20171217*16150000~
HL*1**20*1~
NM1*2B*2*PBM COMPANY*****PI*PBM123~
HL*2*1*21*1~
NM1*1P*1*JONSON*TIM*T**M.D.*XX*3334444555~
REF*EO*POCID~
HL*3*2*22*0~
NM1*IL*1*CROSS*DAVID*M***MI*DD145645645601~
N3*6785 LAUGHALOT LANE~
N4*TRENTON*NJ*08608~
DMG*D8*19720910*M~
INS*Y*18~
DTP*291*RD8*20160101-20161231~
EB*6**30~
SE*16*0001~
GE*1*1~
IEA*1*000000001~
Segment Value Note
ISA PWPBM12345 The Password needed to correspond with the Surescripts’
system.
ISA PBM123 The PBM/payer’s Participant ID.
ISA S00000000000001 Participant ID for Surescripts.
BHT 3920394930203 The Transaction reference number that ties the request to the
response.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 52
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Segment Value Note
HL1:NM1 PBM COMPANY Name of the Source (PBM/payer Name).
HL2:NM1 Tim Jonson : 3334444555 Dr. Jonson with NPI number 3334444555.
HL2:REF POCID Participant ID for the Physician System.
HL3:NM1 DAVID CROSS: David Cross with PBM Unique Member ID DD145645645601
DD145645645601
EB 6:30 1 This patient does not have coverage.
Eligibility Response (for Specialty and Long Term Care)
ISA*00* *01*PWPBM12345*ZZ*PBM123
*ZZ*S00000000000001*171217*0345*^*00501*000000001*1*P*>~
GS*HB*PBM123*S00000000000001*20171217*16150000*1*X*005010X279A1~
ST*271*0001*005010X279A1~
BHT*0022*11*3920394930203*20171217*16150000~
HL*1**20*1~
NM1*2B*2*PBM COMPANY*****PI*PBM123~
HL*2*1*21*1~
NM1*1P*1*JONSON*TIM*T**M.D.*XX*3334444555~
REF*EO*POCID~
HL*3*2*22*0~
NM1*IL*1*CROSS*DAVID*M***MI*DD145645645601~
REF*49*01~
N3*6785 LAUGHALOT LANE~
N4*TRENTON*NJ*08608~
DMG*D8*19720910*M~
INS*Y*18~
DTP*291*RD8*20160101-20161231~
EB*1**30**PLANA~
REF*18*1234~
REF*6P*DD1*ABCGROUP~
REF*FO*201~
REF*CLI*201~
REF*N6*234876*AV~
REF*IG*201~
REF*ALS*142345~
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 53
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
EB*1**88~
EB*1**90~
EB*1~
MSG*SPECIALTY PHARMACY~
EB*1~
MSG*LTC~
SE*30*0001~
GE*1*1~
IEA*1*000000001~
Segment Value Note
ISA PWPBM12345 The Password needed to correspond with the Surescripts’
system.
ISA PBM123 The PBM/payer’s Participant ID.
ISA S00000000000001 Participant ID for Surescripts.
BHT 3920394930203 The Transaction reference number that ties the request to the
response.
HL1:NM1 PBM COMPANY Name of the Source (PBM/payer Name).
HL2:NM1 Tim Jonson : 3334444555 Dr. Jonson with NPI number 3334444555.
HL2:REF POCID Participant ID for the Physician System.
HL3:NM1 DAVID CROSS: David Cross with PBM Unique Member ID DD145645645601
DD145645645601
HL3:REF 49 Family Unit Number
EB 1:30 1 This patient has coverage.
HL3:REF 18 Plan Number
HL3:REF 6P*DD1*ABCGROUP Group Number and Group Name
HL3:REF FO Formulary ID
HL3:REF CLI Coverage List ID
HL3:REF N6 Bin = 234876: Processor Control Number = AV
HL3:REF IG Copay ID
HL3:REF ALS Alternative List ID
EB1:88 1 Eligible for Retail Pharmacy Benefits
EB1:90 1 Eligible for Mail Order Pharmacy Benefits.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 54
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 4: Eligibility Messaging
Segment Value Note
EB1 1 Eligible for benefit specified in the MSG segment.
MSG SPECIALTY PHARMACY Eligible for Specialty Pharmacy Benefits.
EB1 1 Eligible for benefit specified in the MSG segment.
MSG LTC Eligible for Long Term Care Pharmacy Benefits.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 55
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
SECTION 5: ELIGIBILITY MESSAGE
PROCESSING SUMMARY
Depending on the connectivity between customers, the error processing may differ slightly. This
section lays out the error processing for the supported connection types. It also contains the error
processing that happens within the 270/271 message that will be consistent regardless of
connectivity type.
The system (Surescripts) will store the request until the receiver responds to the message or until
the specified time has elapsed. If the timeout elapses before the message is processed, an error
message will be returned to the sender as the reply (explained below). If the sender has timed out,
the message is discarded.
The Eligibility (270/271) message is a message where Surescripts is a defined customer in the
process and adds processing value in the middle. For that reason, additional error processing
needs to be handled. The following section outlines the life of the Eligibility message with the
expected responses to different flows of events. It is broken down into the following stages:
l Surescripts receives the 270 from the requesting party.
l Surescripts processes the 270, identifying the coverage(s).
l Surescripts passes the 270 on to the defined source. (If multiple coverages are found,
multiple 270’s are sent.)
l The source processes the request(s) and returns a 271 response.
l Surescripts combines the response(s) into one envelope.
l Surescripts passes the response back to the original requester.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 56
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
5.1 SURESCRIPTS RECEIVES THE 270 FROM THE REQUESTING PARTY
(PROVIDER VENDOR)
Event Surescripts Requestor
Location Event Error Description
Id Response Follow-Up
1.0 Connectivity Cannot get response None None Investigate
Error from Surescripts and contact
Surescripts
production
support
1.1 Translation Surescripts cannot NAK A Negative Acknowledgement Investigate
identify the message (NAK) with a message that and contact
or does not have says: “TRANSACTION Surescripts
enough info to create a CANNOT BE IDENTIFIED production
TA1 NOR PROCESSED” support
1.2 Translation Translator cannot TA1 Refer to X12 005010 Data Investigate
identify the file (bad Element Dictionary for and contact
ISA or IEA segments) acceptable codes Surescripts
but can produce a TA1 production
response support
1.3 Translation EDI Format has Fatal 999 Refer to the 999 spec for a Investigate
errors - complete list of errors and contact
At any Level: Surescripts
Data Segment production
Data Element support
Transaction Set
Functional Group
5.2 SURESCRIPTS PROCESSES THE 270
Event Surescripts Requestor
Location Event Error Description
Id Response Follow-up
2.0 Source Wrong platform Participant 271 Loop ID 2000A C – Please
Segment ID and/or password. AAA – Error 42 Unable correct and
Loop ID – to Respond a current resubmit
2000A time
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 57
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
Event Surescripts Requestor
Location Event Error Description
Id Response Follow-up
2.1 Source Responder system goes 271 Loop ID 2000A P – Please
Segment down at any time in the AAA – Error 42 Unable resubmit
Loop ID – process (Surescripts). to Respond a current
2000A time
2.2 Source Requester puts bad data in 271 Loop ID 2000A C – Please
Segment the source segment. This AAA – Error 79 correct and
Loop ID – should be Surescripts’ resubmit
Invalid participant
2000A Participant ID.
identification
2.3 Source Requester is not set up to 271 Loop ID 2000A N–
Segment send eligibility message to AAA – Error 41 Resubmission
Loop ID – Surescripts. not allowed
Authorization/Access
2000A Restrictions
2.4 Subscriber Surescripts cannot find the 271 Subscriber Segment N–
Name desired patient Loop ID 2100C Resubmission
Segment AAA – Error 75 - not allowed
Loop ID Subscriber/Insured Not
2100C Found
2.4a Subscriber Surescripts cannot find the 271 Subscriber Segment C – Please
Name desired patient Loop ID 2100C correct and
Segment One of the demographic AAA – Error 75 – resubmit (Hint
Loop ID fields is missing Subscriber/Insured Not is sent back)
2100C Found. Hint is in MSG
segment.
2.4b Subscriber Version translation fails for 271 Subscriber Segment C – Please
Request outgoing 270 Loop ID 2110C correct and
Validation AAA – Error 15 - resubmit
Segment Required application
Loop ID data missing
2110C MSG – Details of Error
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 58
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
5.3 SURESCRIPTS ATTEMPTS TO CONNECT WITH SOURCE
(PBM/PAYER)
PBM/payer Provider
Event PBM/payer Surescripts Requestor
Location Event Error Vendor
Id Response Follow up Follow Up
Description Error
3.0 Surescripts Time Out – None None Investigate Source P – Please
to PBM/payer and create Segment Resubmit
PBM/payer failed to reply to AAA error Loop 2100A Original
Connector Surescripts in for Transaction
AAA – Error
the specified requestor
80
time
No
Response
received -
Transaction
Terminated
3.1 PBM/payer Some failure at NAK Text Error Investigate Source S – Do not
Internal PBM/payer Message and create Segment resubmit;
where they AAA error Loop 2000A Inquiry
cannot produce for initiated to a
AAA – Error
a TA1 or 999 requestor third party.
42
Unable to
respond at
current time
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 59
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
5.4 PBM/PAYER EVALUATES THE MESSAGE
PBM/payer Provider
Event PBM/payer Surescripts Requestor
Location Event Error Vendor
Id Response Follow up Follow Up
Description Error
4.0 Translation Fatal Error TA1 Refer to X12 Investigate Source S – Do not
Initiation with the 005010 Data and create Segment resubmit;
ISA, GS Element AAA error Loop Inquiry
Dictionary for for 2000A initiated to a
acceptable requestor third party.
AAA –
codes
Error 42
Unable
to
respond
at
current
time
4.1 Translation EDI Format 999 Refer to the 999 Investigate Source S – Do not
Initiation has Fatal spec to and create Segment resubmit;
errors - determine AK AAA error Loop Inquiry
At any level and for 2000A initiated to a
Level: appropriate error requestor third party.
AAA –
Data
Error 42
Segment
Data Unable
Element to
respond
Transaction at
Set current
Functional time
Group
5.5 PBM/PAYER PROCESSES THE 270
Note: Errors that occur during any mapping/translation exercise would result in an AAA
segment within the 2000A Source Segment. The error would be a 42 – Unable to respond at
current time.
Generic Error messages for the following messages would result in a 42 within the segment where
the error occurred.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 60
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
PBM/pa PBM/pay Surescri
Eve PBM/payer
yer er pts Provider Requestor
nt Location Event Error
Respon Follow Follow Vendor Error Follow Up
Id Description
se up up
5.0 Source Any issue 271 Source Investig None Source P – Please
Segment that Segment ate and Segment Resubmit
Loop ID caused Loop 2100A contact Loop 2100A Original
2100A the Surescri Transactio
AAA – Error AAA – Error 42
(Note: process pts n
42 Unable to
Informati to halt producti
during Unable to on respond at
on
respond at current time
Source is processin support
g current time if
the
PBM/pay additiona
er info l
that was informati
supplied on or
by clarificati
Surescrip on is
ts) needed.
5.1 Source PBM/pay 271 Source Investig Investig Source S – Do not
Segment er Segment ate and ate and Segment resubmit;
Loop ID validates Loop 2100A contact translate Loop 2100A Inquiry
2100A the Surescri to AAA initiated to
AAA – Error AAA – Error 79
(Note: Source pts system a third
79 Invalid
Informati Identifier producti error for party
to make Invalid on requesto participant
on
participant Identification
Source is sure it’s support r
their own. Identificatio
the
n
PBM/pay Surescript
er info s puts in
that was wrong
supplied identifier
by
Surescrip
ts)
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 61
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
PBM/pa PBM/pay Surescri
Eve PBM/payer
yer er pts Provider Requestor
nt Location Event Error
Respon Follow Follow Vendor Error Follow Up
Id Description
se up up
5.2 Source PBM/pay 271 Source Investig Investig Source S – Do not
Name er Segment ate and ate and Segment resubmit;
Segment validates Loop 2100A contact translate Loop 2100A Inquiry
Loop ID the Surescri to AAA initiated to
AAA – Error AAA – Error 79
2100A source pts system a third
79 Invalid
(Note: contact producti error for party
Informati informatio Invalid on requesto participant
on n. participant support r Identification
Source is Surescript Identificatio
the s puts in n
PBM/pay wrong
er info PBM/pay
that was er contact
supplied name,
by etc.
Surescrip
ts)
5.3 Receiver PBM/pay 271 Receiver None None Receiver C – Please
Segment er Segment Segment Loop correct and
Loop ID validates Loop ID ID 2100B resubmit
2100B the 2100B AAA – Error 15 Surescripts
(This receiver. AAA – Error recommen
Required
loop PBM/pay 15 ds this
application
contains er wants value,
Required data missing
the more however a
application
physician fields PBM/Paye
data
info and populated r might
missing
the than what send a
Physicia is required different
n System by value
info) Surescript
s; i.e. –
the POC
is not
identified.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 62
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
PBM/pa PBM/pay Surescri
Eve PBM/payer
yer er pts Provider Requestor
nt Location Event Error
Respon Follow Follow Vendor Error Follow Up
Id Description
se up up
5.4 Receiver PBM/pay 271 Receiver None None Receiver N–
Segment er Segment Segment Loop Resubmiss
Loop ID validates Loop ID ID 2100B ion not
2100B receiver. 2100B AAA – Error 41 allowed
(This PBM/pay AAA – Error – Surescripts
loop er cannot 41 – Authorization/ recommen
contains return Authorizatio ds this
Access
the eligibility n/ value,
restrictions
physician for this however a
Access
info and patient PBM/Paye
restrictions
the because r might
Physicia of the send a
n System patients different
info) group or value
plan.
5.5 Receiver PBM/pay 271 Receiver None None Receiver C – Correct
Name er Name Name and
Segment validates Segment Segment Loop Resubmit
Loop ID – the Loop ID – ID – 2100B Surescripts
2100B physician 2100B Physician recommen
Identifier AAA – Error Loop ds this
43 AAA – Error 43 value,
Invalid/Mis however a
Invalid/Missing
sing PBM/Paye
Provider
Provider r might
Identification
Identificatio send a
n different
value
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 63
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
PBM/pa PBM/pay Surescri
Eve PBM/payer
yer er pts Provider Requestor
nt Location Event Error
Respon Follow Follow Vendor Error Follow Up
Id Description
se up up
5.8 Subscrib Patient 271 AAA – Error None None AAA – Error 75 S – Do not
er Name found at 75 – - resubmit;
Loop ID Surescript Subscriber / Subscriber/Ins Inquiry
2100C s, but not Insured Not ured Not initiated to
in the Found Found a third
PBM/pay party
er’s
system
(could be
caused by
a
difference
between
Surescript
s and the
PBM/pay
er’s
patient
database
s or
caused by
the
patient
demograp
hic
mismatch
between
requestor
and
PBM/pay
er).
5.6 PBM/PAYER SENDS 271 BACK TO SURESCRIPTS
Surescripts evaluates the message.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 64
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
Provide Request
Surescript Surescripts PBM/paye Surescript
Even r or
Location Event s Error r Follow s Follow
t Id Vendor Follow
Response Description up up
Error Up
6.0 Translatio Fatal Error TA1 Refer to Investigat Investigat Source S - Do
n of 271 with ISA Implementation e and e and Segme not
from or GS contact translate nt resubmit;
PBM/pay segments Acknowledgme Surescript to AAA Loop Inquiry
er nt For Health s system 2100A initiated
Care Insurance productio error for to a third
AAA –
(999) n support requestor party
Error 42
Unable
to
respond
at
current
time
6.1 Translatio EDI 999 Refer to Investigat Investigat Source S - Do
n of 271 Format Implementation e and e and Segme not
from has Fatal Acknowledgme contact translate nt resubmit;
PBM/pay errors - nt For Health Surescript to AAA Loop Inquiry
er At any Care Insurance s system 2100A initiated
Level: (999) to productio error for to a third
AAA –
Data determine AK n support requestor party
Error 42
Segment level and
Data appropriate Unable
Element error to
respond
Transacti at
on Set current
time
Functional
Group
5.7 SUMMARY OF ERRORS SENT TO PROVIDER VENDOR
The following is a summary of some of the errors a provider vendor can expect to see.
Error Description
Source Segment Generic error message for all errors that occurred that were not caused by the
Loop 2000A Physician System.
AAA – Error 42
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 65
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 5: Eligibility Message Processing Summary
Error Description
Receiver Segment If the provider vendor fails to give enough information in the message to identify
Loop ID- 2100B themselves or the physician to the PBM/payer.
AAA – Error 15
Source Segment The sending customer is not set up to send an eligibility message.
Loop ID- 2000A
AAA – Error 41
Receiver Segment If the PBM/payer determines that they cannot return information for this patient
Loop ID- 2100B based off of the plan or group.
AAA – Error 41
Receiver Segment If the PBM/payer requires a DEA or state license number for the prescribing
Loop ID- 2100B office but the provider vendor does not provide it.
AAA – Error 43
Subscriber Name Surescripts cannot find the patient in the MPI.
Segment Loop ID
AAA – Error 75
5.8 SUMMARY OF TRANSLATED ERRORS
Segment Error Translation for Provider Vendor
Connectivity Type All (Timeouts, NAKs, 999) Source Segment
Loop 2000A
AAA – Error 42
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 66
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 6: Application Certification Requirements
SECTION 6: APPLICATION CERTIFICATION
REQUIREMENTS
6.1 ELIGIBILITY RETRIEVAL
E.100: The participant shall ensure an eligibility request is associated with a patient interaction, is
part of a medication reconciliation, or is associated with the electronic prior authorization process.
Definition of Patient Interaction - “Patient interaction with the prescriber with the probability that a
prescription will take place in the course of that interaction. The interaction can take the form of a
physical visit, phone call, telemedicine, or email from the patient to the prescriber/prescriber to the
patient. The eligibility request generally occurs within 24 hours prior to the patient interaction.”
Examples of what is not considered a patient interaction for the purposes of a billable eligibility
request:
1. Activities associated with health care operations, including but not limited to:
a. Calls to schedule or check in appointments
b. Opening a chart for:
i. Billing questions
ii. Reference purposes
iii. Post visit transcription
iv. Updating patient information
2. Clinical information activities not associated with a prescribing medication reconciliation or
electronic prior authorization process, including but not limited to:
a. Lab test results or follow up
b. Post visit reviews
c. Coordination of care
E.101: Participants shall ensure that:
1. Information returned in the eligibility response shall be used within 3 calendar days/72
hours of receipt.
2. Eligibility requests are sent only once during that period (unless an error is encountered in
the eligibility retrieval process).
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 67
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 6: Application Certification Requirements
Definition: A calendar day runs from 12:00 a.m. to 11:59 p.m. Central Time, regardless of
the location of the patient encounter.
E.102: Participant/PBM must be able to process any valid 270 request and 271 response (valid
data elements and values, including optional elements, supported by X12 must not cause
processing failure at the end-point).
6.2 PRESENTATION OF ELIGIBILITY INFORMATION
E.103: The participant application shall display the following information returned in the eligibility
response for an active coverage:
l PBM/Payer name (NM103 loop 2100A)
l All pharmacy coverage types received (e.g. Retail) with associated eligibility status (e.g.
Covered/Not Covered). If displaying pharmacy coverage types that are not received in the
eligibility response, the associated eligibility statuses must be clearly differentiated from the
eligibility statuses of the pharmacy coverage types that are received.
l Health plan name returned in the Plan Coverage Description data element in the 2110C1
loop.
E.104: The application shall allow the user to switch between all active, eligibility coverages.
E.105: When the change flag is present, at a minimum, the participant application shall display an
alert indicating there is a difference between the patient demographics sent in the 270 and those
returned in the 271 for all active coverages and shall make all of the demographics returned
available for the prescriber to review.
E.106: If available, PBMs shall send the health plan name in the Plan Coverage Description data
element in the 2110C1 loop in the 270 transactions.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 68
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
SECTION 7: ID LOAD AND RESPONSE FILES
7.1 INTRODUCTION
PBM/payers use the ID Load file to provide Surescripts with their member roster to populate the
Surescripts Master Patient Index (MPI). Surescripts uses these files from the PBM/payers to
establish uniqueness for individuals across PBM/payers. Surescripts’ search process uses
demographics to identify a patient and then uses the PBM/payer's unique member ID to
communicate with the PBM/payers.
Surescripts responds to PBM/payer ID Loads with a Member Directory Response File indicating
the status of each load, including details at both the file and detail level. Information provided by
Surescripts indicates if a file loaded successfully, loaded with errors or was not loaded at all.
Affected records are detailed in the response file which indicates the specific reason each line had
an error or warning.
Surescripts will also provide statistical data about the processing for a given Delimited File received
from a PBM/payer. The Member Directory Response Summary File will allow PBM/payers new
insight into the processing of MPI files, and will allow them to better determine whether all of the
records sent to Surescripts were loaded as expected.
7.2 ID LOAD PROCESS FLOW
The following steps depict the flow of the ID load:
1. The PBM/payer creates a directory of patients, assigning each occurrence a unique member
ID.
Note: It is recommended to update the MPI daily.
2. The PBM/payer submits the initial load to Surescripts.
3. Surescripts populates the MPI internal directory with the initial file load.
4. Surescripts creates a response file for the PBM/payer indicating the process success and
failure details.
Note: All date/times within response files are in UTC.
5. The PBM/payer creates an update file to keep the Surescripts MPI internal directory up-to-
date.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 69
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Note: Updates should only be sent if there is a change in the members’ demographic
data that Surescripts has defined in the file layout. If other member information not
contained in the file layout changes, no update should be sent.
6. Surescripts processes the updates.
7. Surescripts sends a response to the PBM/payer indicating the process success and failure
details.
7.3 FORMAT TO BE USED
Surescripts has implemented a custom specification that contains demographic and PBM/payer
specific information in a delimited field file format. Use the same character set as referenced in
Character Set except for the “^” character – decimal 94 which cannot be used in the ID Load
Process.
Note: Delimited files designated in the header record as a Full file that contain more than 8M
records must be scheduled with Surescripts Support, and will be manually processed.
7.4 MEMBER PROCESSING EXAMPLES
File
Purpose Method
Type
Terminate a member Update Send the cancellation or termination date
(past/present/future) along with the 024 –
Cancel code.
Terminate a member Full Either send the cancellation/termination date
Refresh (past/present/future) along with the 024 –
Cancel code.
Or
Do not include the member in the full refresh
file.
Add new member Full Send the new member data in the full refresh or
Refresh update file along with the 021 – Addition code.
or
Update
Update member demographics Full Send the updated member demographics along
Refresh with the 001 – Change code.
or
Update
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 70
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
File
Purpose Method
Type
Reinstate a previously terminated member Update Send either a future termination date or leave
where the record has not been removed via the termination field blank along with the 025 –
the full refresh process Reinstatement code.
7.5 ERROR SCENARIOS
Note: Error scenarios do not vary based on file type (full refresh or update).
MPI
Code Sent in MPI
Database Error Code and
Full Refresh or Response File Action
Record Message
Update File
Status
Change (001) Record Add the MPI database record. W04 - Change
does not Record not found,
exist record added.
Addition (021) Record Change the MPI database record. W05 - Record to
already Add exists, record
exists updated.
Cancellation or Record Add the MPI database record with the W06 - Record to
Termination (024) does not termination date. The record must contain a Term does not exist,
exist termination date or it will be rejected. record added.
Reinstatement Record Add the MPI database record. The record must W07 - Record to
(025) does not contain a future termination date or no Reinstate not found,
exist termination date. record added.
7.6 MEMBER DIRECTORY MAINTENANCE DELIMITED FILE FROM
PBM/PAYER
Each field is delimited by the pipe character (|). Each line is separated by a new line (Hex 0A)
character. The tilde character (~) is used as a repetition character – currently only supported in the
postal code field.
Header Info
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 71
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Name Type Required Comments Examples
#
1 Record Type AN Yes Identifies record type
3/5 Value:
HDR
2 Version/Release AN Yes Version Number of this specification
Number 3/5 Value:
2.0
3 Sender ID AN Yes ID as assigned by Surescripts P11111111111111
3/30 identifying customer sending the file.
4 Sender Participant AN Yes Password for this customer identified ABCDE12345
Password 10/10 in field 3 (Sender ID).
5 Receiver ID AN Yes ID identifying the receiver of the file.
1/30 Value:
RXHUB
6 Source Name AN Not Future use
1/35 Used
7 Transmission AN Yes Unique identifier defined by the 0000001000
Control Number 1/10 sender
8 Transmission Date DT Yes Date message was created (D8 - 20170701
8/8 CCYYMMDD)
9 Transmission Time TM Yes Time message was created 12200101
8/8 (HHMMSSDD)
10 Transmission File AN Yes Identifier telling the type of message
Type 1/3 Value:
MPI
11 Transmission AN No Values: U
Action 1/1 U=Update
F=Full file
If blank, default to U=Update
12 Extract Date DT Yes Date File was created (D8 - 20170630
8/8 CCYYMMDD)
13 File Type AN Yes Test or Production P
1/1 Values:
T=Test
P=Production
Detail Info
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 72
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Name Type Required Comments Examples
#
1 Record Type AN Yes Identifies record type
3/3 Value:
MEM
2 Record AN Yes Number for this detail row in the message
Sequence 1/10
Number
3 PBM Unique AN Yes Unique ID as identified by the PBM/payer for
Member ID 1/60 the member
4 PBM Unique ID AN No Unique ID as identified by the PBM/payer for
for Subscriber 1/60 the subscriber of the member
5 Health Plan AN No Health Plan Unique Member identification
Member 1/30 number on the Health Plan card identifying the
Number patient (Either a subscriber or a dependent)
6 Health Plan AN No Health Plan Unique Subscriber identification
Subscriber 1/30 number - Number on the Health Plan card
Number identifying the subscriber
7 Policy Number AN No Health Plan policy or group number
1/30
8 Member DT No Date that the member is no longer eligible (D8)
Expiration Date 8/8 If multiple dates are available (i.e. Term Date,
Expired Date, End Date), use the earliest date
of the three.
9 Last Name AN Yes Last Name of the Member
1/35
10 First Name AN Yes First Name of the Member
1/25
11 Middle Name AN No Middle Name of the Member
1/25
12 Prefix AN No Member Prefix
1/10
13 Suffix AN No Member Suffix
1/10
14 Social Security N No Member SSN - No dashes
Number 9/9
15 Address Line 1 AN Yes First Line of the Address (No C/O type info)
1/55
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 73
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Name Type Required Comments Examples
#
16 Address Line 2 AN No Second Line of the Address (No C/O type info)
1/55
17 City Name AN Yes Member City Name
2/30
18 State or AN Yes Member State Code
Province Code 2/2
19 Postal Code AN Yes Member zip code 5 or 9 numeric no punctuation. 55123~55102
3/15
20 Country Code AN No Member Country Code
2/3
21 Comm Number AN No 1st Comm. Number Type
1 Type 2/2 Values:
EM = Email
EX = Telephone Extension
FX = Facsimile
HP = Home Phone
TE = Telephone
WP = Work Phone
22 Communication AN No 1st Communication Number
Number 1 1/80
23 Communication AN No 2nd Communication Number Type
Number 2 Type 2/2 Values:
EM = Email
EX = Telephone Extension
FX = Facsimile
HP = Home Phone
TE = Telephone
WP = Work Phone
24 Communication AN No 2nd Communication Number
Number 2 1/80
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 74
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Name Type Required Comments Examples
#
25 Communication AN No 3rd Communication Number Type
Number 3 Type 2/2 Values:
EM = Email
EX = Telephone Extension
FX = Facsimile
HP = Home Phone
TE = Telephone
WP = Work Phone
26 Communication AN No 3rd Communication Number
Number 3 1/80
27 Date of Birth DT No Member DOB (CCYYMMDD)
8/8
28 Gender AN Yes Member Gender (M,F,U)
1/1 If gender not given, a blank space will be used.
29 Employer AN No Employer Name
Name 1/35
30 Transaction AN Yes Type of Action needed
Type 3/3 Values:
001 – Change
021 – Addition
024 - Cancellation or Termination
025 – Reinstatement
Trailer Info
Field
Field Name Type Required Comments Examples
#
1 Record Type AN Yes Identifies record type
3/3 Value:
TRL
2 Total Records N Yes Total Records Processed
1/10
7.7 MEMBER DIRECTORY RESPONSE DELIMITED FILE TO PBM/PAYER
The file name reflects the file name from the PBM/payer with a .rsp file extension.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 75
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Example: NewPatient_TestingPBMC_MPI.1450188243095.rsp
Note: If the source file had an extension, the extension remains and the .rsp is added after it.
For example: NewPatient_TestingPBMC_MPI.1450188243095.txt.rsp
Header
Field Description Type Required Comments Examples
Record Type Identifies AN Yes Value:
record type 3/3 SHD
Version/Release Version AN Yes Value:
Number Number of 1/2
2.0
this
specification
Recipient ID ID assigned AN Yes If the inbound MPI file P11111111111111
by 3/30 included an invalid Sender
Surescripts ID, Sender Participant
for the Password, Transmission
recipient of Date, or Transmission time,
the this field in the response file
response file will be populated with: “INV_
(original HEADER”.
sender of
the ID load
file)
Sender ID ID as AN Yes Value:
assigned by 3/30 RXHUB
Surescripts
identifying
Surescripts
Recipient Password AN Yes If the inbound MPI file
Participant assigned by 10/10 included an invalid Sender
Password Surescripts ID, Sender Participant
for Password, Transmission
accessing Date, or Transmission time,
the this field in the response file
PBM/payer will be populated with: “INV_
system. HEADER”.
Transaction Unique AN Yes
Control Number identifier 1/10
defined by
the sender
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 76
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field Description Type Required Comments Examples
Transaction Date DT Yes CCYYMMDD
Date message 8/8
was created
Transaction Time TM Yes HHMMSSDD
Time message 8/8
was created
Transaction File Identifier AN Yes Value:
Type telling 1/3 MPR
receiver the
type of file.
Transaction Number of AN Yes
Number - the original 1/10
Originating report
message
Transaction Date DT Yes CCYYMMDD
Date- Original 8/8 If the inbound MPI file
Originating Incoming included an invalid Sender
File was ID, Sender Participant
created (D8) Password, Transmission
Date, and/or Transmission
time, this field in the
response file will be
populated with: “20000101”.
Transaction Time TM Yes HHMMSSDD
Time- Original 8/8 If the inbound MPI file
Originating Incoming included an invalid Sender
File was ID, Sender Participant
created Password, Transmission
Date, and/or Transmission
time, this field in the
response file will be
populated with: “00000000”.
File Type Test or AN Yes Values:
Production 1/1 T=Test
(T/P)
P=Production
Load Status Code AN Yes See Member Directory
Explaining 2/2 Codes
the status of
the load.
Detail Info
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 77
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field Description Type Required Comments Examples
Record Type Identifies record type N Yes Value:
1/1 SDT
Record Sequence Number that identified the row in AN Yes
Number the incoming message 1/10
PBM Unique ID for Unique ID as identified by the AN No
the member PBM/payer for the member 1/60
Error Code Describes error for this row AN Yes See Member
3/3 Directory Codes
W - Signifies a Warning
E - Signifies a Error
Trailer Info
Field Description Type Required Notes Examples
Record Identifies AN Yes Value:
Type record type. 3/3 STR
Total Rows N Yes
in Error 1/10
7.8 MEMBER DIRECTORY RESPONSE SUMMARY DELIMITED FILE TO
PBM/PAYER
File Naming Convention:
l A human readable file (on Admin Console) will have a .smt file extension. Example: erx_
RXHUB_member_directory_02082015_201919.1423456259313.smt
l A pipe delimited file (on FTP) will have a .smd file extension.
Note: The PBM/payer needs to request an opt-in from Surescripts in order to receive this .smd
file.
Example: erx_RXHUB_member_directory_02082015_201919.1423456259313.smd
Field
Field Description Type Comments Example
#
1 File Load Date Date the MPI file was processed DT 12/05/2014
by Surescripts. 10/10
UTC Date in MM/DD/CCYY
format.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 78
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Description Type Comments Example
#
2 Transmission Unique identifier defined by the AN 0000001000
Control Number sender from inbound MPI file. 1/10
3 Participant ID Surescripts ID assigned to the AN P111111111111111
PBM/payer. 3/30
4 Sender ID The Sender ID is Surescripts. AN Value:
3/30 Surescripts
5 Incoming File Date time that Surescripts AN 12/05/2014
Received received the inbound file. 24 hour 19/19 04:34:02
time used - UTC Datetime in
MM/DD/YYYY HH:MM:SS format.
6 Total Number of Number of active lives in the MPI N 10000
Active Lives in before processing. 1/12
MPI Before Note: Number of active lives
Processing reflects the customer's requested
lag days. For example, if the
customer's lag day value is 7, all
members in their MPI file are
considered active for 7 days
beyond the Member Expiration
date provided by the customer in
the MPI file.
Incoming File Record Count
7 Total Records Number of patient records in the N 1000
in File MPI file. 1/12
8 Number of Number of records in the inbound N 200
Adds MPI file where Transaction Type 1/12
== 021.
9 Number of Number of records in the inbound N 300
Terms MPI file where Transaction Type 1/12
== 024.
10 Number of Number of records in the inbound N 500
Changes MPI file where Transaction Type 1/12
== 001.
11 Number of Number of records in the inbound N 5
Reinstatements MPI file where Transaction Type 1/12
== 025.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 79
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Description Type Comments Example
#
Results of Processing the File
12 Requested Number of records with N 300
Number of Transaction Type == 021 that were 1/12
Records Added added.
13 Requested Number of records with N 600
Number of Transaction Type == 001 that were 1/12
Records changed.
Changed
14 Requested Number of records with N 50
Number of Transaction Type == 024 that were 1/12
Records terminated.
Termed
15 Requested Number of records with N 4
Number of Transaction Type == 025 that were 1/12
Reinstatements reinstated.
16 Number of Number of errors generated. N 50
Errors 1/12
17 Number of Number of cases on update file N 75
Adds That loads where a record in the inbound 1/12
Already Existed file had Transaction Type == 021,
but the patient already existed in
the Surescripts system.
18 Number of Number of cases on update file N 100
Changed that loads where a record in the inbound 1/12
Did Not Exist file had Transaction Type == 001,
but the patient record did not exist
in the Surescripts system.
19 Number of Number of cases on update file N 50
Terms that Did loads where a record in the inbound 1/12
Not Exist file had Transaction Type == 024,
but the patient record did not exist
in the Surescripts system.
20 Number of Number of cases on update file N 1
Reinstatements loads where a record in the inbound 1/12
that Did Not file had Transaction Type == 025,
Exist but the patient record did not exist
in the Surescripts system (patient
was not found in either an active or
inactive state).
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 80
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Field
Field Description Type Comments Example
#
21 Total Number of Number of active lives in the MPI N 10300
Active Lives in after processing. 1/12
MPI After After processing the new file, the
Processing number of records where the
Member Expiration Date is >= to
today's date in the Surescripts
system.
22 Processing Date time the new MPI file began AN 12/05/2014
Start Time processing in 24 hour clock - UTC 19/19 05:04:00
Datetime in MM/DD/YYYY
HH:MM:SS format
23 Processing End Date time the new MPI file began AN 12/05/2014
Time processing in 24 hour clock - UTC 19/19 07:16:02
Datetime in MM/DD/YYYY
HH:MM:SS format
24 Processing Time it took to process the file in DT 002:12:02
Time for File HHH:MM:SS format. 9/9
25 Member Version ID of the Member AN 1.0
Directory Directory Response Summary. 3/3
Response
Summary
Version ID
7.9 MEMBER DIRECTORY CODES
Header Response Codes
Code Description
01 File loaded correctly.
02 File loaded with errors.
03 Invalid file format - File Not loaded.
04 System error - Please resend.
05 Invalid header section ID - File not loaded (Not Used).
06 Invalid header Participant ID or password - File not loaded.
07 Invalid header transaction number format - File not loaded.
08 Invalid header transaction datetime format - File not loaded.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 81
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Section 7: ID Load and Response Files
Code Description
09 Invalid header usage indicator - File not loaded.
10 Invalid header filler - File not loaded.
11 Invalid header new line character - File not loaded.
12 Invalid trailer section ID – Trailer not validated - File not loaded.
13 Invalid trailer filler - Trailer not validated. - File not loaded.
14 Invalid reported number of records - File not loaded.
15 Contract does not exist - File not loaded.
17 Invalid header version number - File not loaded (Not Used).
Detail Error/Warning Codes
Code Description
E01 Missing PBM Unique Member ID, record not loaded.
E02 Missing required fields, record not loaded.
E03 Invalid characters in row, record not loaded.
E04 Invalid record length, record not loaded.
E05 Invalid record type, record not loaded.
E07 Invalid transaction type, record not loaded.
E09 Missing Term Date, record not loaded.
E10 Maximum repetitions exceeded.
E13 Term Date must be a future date or not populated when 25-Reinstatement Transaction Type is
used.
W04 Change Record not found, record added.
W05 Record to Add exists, record updated.
W06 Record to Term does not exist, record added.
W07 Record to Reinstate not found, record added.
W08 Duplicate PBM Unique Member ID found in update file, record not loaded. This warning will only
occur for the membership update process. If a duplicate PBM Unique Member ID is found in the
initial membership load, no records are loaded and the entire file is rejected.
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 82
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Appendix A: Dynamic Delimiters
APPENDIX A: DYNAMIC DELIMITERS
This section contains a full list of characters that are acceptable to use as delimiters.
Surescripts uses the following delimiters:
l Data Element Separator – hex 1D, decimal 29
l Segment Terminator – hex 1E, decimal 30
l Component Element Separator (ISA 16) – hex 3E, decimal 62
l Repetition Character (ISA11) – hex 1F, decimal 31
Char Dec Oct Hex
(bel) 7 0007 0x07
(ht) 9 0011 0x09
(nl) 10 0012 0x0a
(vt) 11 0013 0x0b
(cr) 13 0015 0x0d
(np) 12 0014 0x0c
(fs) 28 0034 0x1c
(gs) 29 0035 0x1d
(rs) 30 0036 0x1e
(us) 31 0037 0x1f
! 33 0041 0x21
" 34 0042 0x22
% 37 0045 0x25
& 38 0046 0x26
' 39 0047 0x27
( 40 0050 0x28
) 41 0051 0x29
* 42 0052 0x2a
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 83
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Appendix A: Dynamic Delimiters
Char Dec Oct Hex
+ 43 0053 0x2b
, 44 0054 0x2c
- 45 0055 0x2d
. 46 0056 0x2e
/ 47 0057 0x2f
: 58 0072 0x3a
Ã; 59 0073 0x3b
< 60 0074 0x3c
= 61 0075 0x3d
> 62 0076 0x3e
? 63 0077 0x3f
@ 64 0100 0x40
[ 91 0133 0x5b
\ 92 0134 0x5c
] 93 0135 0x5d
^ 94 0136 0x5e
_ 95 0137 0x5f
` 96 0140 0x60
{ 123 0173 0x7b
| 124 0174 0x7c
} 125 0175 0x7d
~ 126 0176 0x7e
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 84
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
Eligibility CG 2.0 Appendix B: Document Change Log
APPENDIX B: DOCUMENT CHANGE LOG
The table below tracks significant changes made to the document since it was last published.
Change Log
Sec. # Sec. Title Change Description Reason
N/A – First release
P UBLISHED 07/11/2018 COPYRIGHT © 2018 BY S URESCRIPTS, LLC. P AGE 85
A LL RIGHTS RESERVED . P ROPRIETARY AND CONFIDENTIAL
You might also like
- TD.57 v36.5 - TAP Format SpecsDocument317 pagesTD.57 v36.5 - TAP Format SpecsSamir Zemmache0% (1)
- Trust, Complexity and Control: Confidence in a Convergent WorldFrom EverandTrust, Complexity and Control: Confidence in a Convergent WorldNo ratings yet
- CardGateV6-TM 001Document71 pagesCardGateV6-TM 001information revenuenetworkNo ratings yet
- SGP 22-v3 1Document501 pagesSGP 22-v3 1Abrosimov OlegNo ratings yet
- Etherisct WhitepaperDocument44 pagesEtherisct WhitepaperGabi HabiNo ratings yet
- Pay As You Sail (PAYS) Specification V2.0Document12 pagesPay As You Sail (PAYS) Specification V2.0Jotace CastilloNo ratings yet
- User Description, Multiband OperationDocument12 pagesUser Description, Multiband OperationYura SaskevychNo ratings yet
- EMVCo White Paper On Payment Account Reference v2.1.1 FinalDocument25 pagesEMVCo White Paper On Payment Account Reference v2.1.1 FinalPriyanka PalNo ratings yet
- Es-Cs - Bc.if Native - Eng.mdDocument217 pagesEs-Cs - Bc.if Native - Eng.mdDavid SakhelashviliNo ratings yet
- Staff Travel and Expenses Policy and Procedures v1.0Document19 pagesStaff Travel and Expenses Policy and Procedures v1.0bogdand20100% (1)
- General Revi Si OnDocument30 pagesGeneral Revi Si OnAEK BKHSNo ratings yet
- A343 2022 03 Captions and SubtitlesDocument16 pagesA343 2022 03 Captions and SubtitlesRoman GilNo ratings yet
- Egypt gas feasibility study examines energy efficiency opportunitiesDocument53 pagesEgypt gas feasibility study examines energy efficiency opportunitieskawmawNo ratings yet
- A-Bis Over IP Interface v02 00Document172 pagesA-Bis Over IP Interface v02 00g3tech79No ratings yet
- RCC.07 v8.0Document368 pagesRCC.07 v8.0prashantNo ratings yet
- Nokia MBB in Critical Communications White Paper enDocument61 pagesNokia MBB in Critical Communications White Paper enÖzer DenizNo ratings yet
- Trustwave Pci Dss v2.0 Pci Roc Banred 14feb2014 FinalDocument273 pagesTrustwave Pci Dss v2.0 Pci Roc Banred 14feb2014 FinalLUIS ALBERTO MOSQUERA HERNANDEZNo ratings yet
- 2301 5.4 Tech Overview FINALDocument43 pages2301 5.4 Tech Overview FINALAnghy Quinteros SalazarNo ratings yet
- Carequality FHIR Implementation GuideDocument67 pagesCarequality FHIR Implementation GuideBlankNo ratings yet
- PTVVisum14 ManualDocument2,798 pagesPTVVisum14 ManualWilliam GuartazacaNo ratings yet
- WhitepaperDocument39 pagesWhitepaperwww.hardbitNo ratings yet
- IMS Profile For Voice and SMS 15 June 2017: This Is A Non-Binding Permanent Reference Document of The GSMADocument57 pagesIMS Profile For Voice and SMS 15 June 2017: This Is A Non-Binding Permanent Reference Document of The GSMAdineshNo ratings yet
- SGP 22-v2 2 1-2Document250 pagesSGP 22-v2 2 1-2Pradeep SiriwardanaNo ratings yet
- R4 Discover D-PASU.S.terminalGuide2017Document40 pagesR4 Discover D-PASU.S.terminalGuide2017Kevin HuNo ratings yet
- Service Automation and Dynamic Provisioning Techniques in IP / MPLS EnvironmentsFrom EverandService Automation and Dynamic Provisioning Techniques in IP / MPLS EnvironmentsNo ratings yet
- Obtaining the Professional Master in Software EngineeringDocument17 pagesObtaining the Professional Master in Software EngineeringRita MarrounNo ratings yet
- VPNcontentsDocument2 pagesVPNcontentspradi66554433No ratings yet
- NG 114-v1 0-8 PDFDocument74 pagesNG 114-v1 0-8 PDFLasya SravyaNo ratings yet
- BBD Bank AccountingDocument29 pagesBBD Bank AccountingChris LoureyNo ratings yet
- Contador de Partículas RexrothDocument44 pagesContador de Partículas RexrothJohnny Eddy DantasNo ratings yet
- SRS School Management SysDocument49 pagesSRS School Management Sysshahroz AhmadNo ratings yet
- GCR PDFDocument19 pagesGCR PDFmutaisteveNo ratings yet
- DICOM Validation Tool Conformance StatementDocument29 pagesDICOM Validation Tool Conformance StatementIago NunesNo ratings yet
- Srs CadastralMappingv1.4 22092009 FinalDocument149 pagesSrs CadastralMappingv1.4 22092009 FinalEsshwar AndroidNo ratings yet
- RCC 07-v11 0Document389 pagesRCC 07-v11 0Elektro TomekNo ratings yet
- Logistics Supplier Manual GuideDocument36 pagesLogistics Supplier Manual GuideRuliani Putri SinagaNo ratings yet
- This Project Has Received Funding From The European Union's Horizon 2020 ResearchDocument54 pagesThis Project Has Received Funding From The European Union's Horizon 2020 ResearchJohnnyNo ratings yet
- Rubber Nanocomposites: Preparation, Properties, and ApplicationsFrom EverandRubber Nanocomposites: Preparation, Properties, and ApplicationsNo ratings yet
- IMS Profile For Voice and SMS 14 May 2020: This Is A Non-Binding Permanent Reference Document of The GSMADocument70 pagesIMS Profile For Voice and SMS 14 May 2020: This Is A Non-Binding Permanent Reference Document of The GSMALiba BaliNo ratings yet
- SGP 22-v2 0Document230 pagesSGP 22-v2 0Pradeep SiriwardanaNo ratings yet
- IMS Service Centralization and Continuity Guidelines 15 September 2015Document23 pagesIMS Service Centralization and Continuity Guidelines 15 September 2015dineshNo ratings yet
- IMS Call FlowsDocument40 pagesIMS Call FlowsVivek Nagal100% (1)
- Lxm23A Canopen: Fieldbus Protocol For Servo Drive Fieldbus ManualDocument120 pagesLxm23A Canopen: Fieldbus Protocol For Servo Drive Fieldbus Manualabolqassem fakherNo ratings yet
- 01 - RFP - EDMS - Vdraft2-Updated PDFDocument174 pages01 - RFP - EDMS - Vdraft2-Updated PDFBireshwar DasNo ratings yet
- DRAFT QuickStartGuideForMappingToLaboratoryLoincDocument48 pagesDRAFT QuickStartGuideForMappingToLaboratoryLoincaffan ekaNo ratings yet
- Analisis Keuangan - Fakhri UIDocument72 pagesAnalisis Keuangan - Fakhri UIbyfadia5No ratings yet
- A341 2019 Video HEVCDocument38 pagesA341 2019 Video HEVCBernardo Álvarez LópezNo ratings yet
- SGP.22 v2.1Document247 pagesSGP.22 v2.1Pradeep SiriwardanaNo ratings yet
- Ocean Protocol: A Decentralized Substrate For AI Data & ServicesDocument59 pagesOcean Protocol: A Decentralized Substrate For AI Data & ServicesJ. JNo ratings yet
- GSMA Coordinated Vulnerability Disclosure Program 16 July 2020Document32 pagesGSMA Coordinated Vulnerability Disclosure Program 16 July 2020Roei ZoharNo ratings yet
- Pcnse Study GuideDocument226 pagesPcnse Study Guidedebjyoti GhoshNo ratings yet
- Madeeha Shah - Online Bank Management SystemDocument61 pagesMadeeha Shah - Online Bank Management Systemghulam muhammadNo ratings yet
- Beer PEFCR June 2018 FinalDocument88 pagesBeer PEFCR June 2018 FinalRobert CoffinNo ratings yet
- IMS Service Centralization and Continuity Guidelines 08 December 2016Document24 pagesIMS Service Centralization and Continuity Guidelines 08 December 2016ssssNo ratings yet
- KT-10 User Manual (GR)Document115 pagesKT-10 User Manual (GR)Hal MicheaNo ratings yet
- VRIOGS 013.4 ICT Nomenclature SpecificationDocument59 pagesVRIOGS 013.4 ICT Nomenclature SpecificationCK TangNo ratings yet
- School Managment SystemDocument12 pagesSchool Managment SystemNaveen kumarNo ratings yet
- Declaration of Trust - Statuttory Trust SampleDocument33 pagesDeclaration of Trust - Statuttory Trust SampleLancau CibaiNo ratings yet
- Annex A3 Mogden SS CDRDocument36 pagesAnnex A3 Mogden SS CDRkwaikwai1089No ratings yet
- Cyxtera-Ecosystem-Connect-Service-DescriptionDocument10 pagesCyxtera-Ecosystem-Connect-Service-DescriptiondkmgapkgNo ratings yet
- V2017071 SCRIPT STANDARD - Example - GuideDocument599 pagesV2017071 SCRIPT STANDARD - Example - GuideNileima Elaine RomeroNo ratings yet
- ManageEngine ServiceDeskPlusMSP 8.1 Help UserGuideDocument53 pagesManageEngine ServiceDeskPlusMSP 8.1 Help UserGuideNileima Elaine RomeroNo ratings yet
- Formulary CG 2.0.1 2020-06-29Document141 pagesFormulary CG 2.0.1 2020-06-29Nileima Elaine RomeroNo ratings yet
- SCRIPT Implementation RecommendationsDocument201 pagesSCRIPT Implementation RecommendationsNileima Elaine RomeroNo ratings yet
- Prescription Benefit IG 2016-12-12Document303 pagesPrescription Benefit IG 2016-12-12Nileima Elaine RomeroNo ratings yet
- Medication History Early Adopter Draft Companion GuideDocument45 pagesMedication History Early Adopter Draft Companion GuideNileima Elaine RomeroNo ratings yet
- QRadar SIEM and Palo Alto ApprovedDocument13 pagesQRadar SIEM and Palo Alto ApprovedNileima Elaine RomeroNo ratings yet
- Guardium Data EncryptionDocument9 pagesGuardium Data EncryptionNileima Elaine RomeroNo ratings yet
- ICD For APSDocument11 pagesICD For APSNileima Elaine RomeroNo ratings yet
- SIEM For BeginnersDocument18 pagesSIEM For BeginnersАлексей ЦибиногинNo ratings yet
- PERFORMANCE QUALIFICATION FinalDocument5 pagesPERFORMANCE QUALIFICATION Finalkrishna murthyNo ratings yet
- NXP Elec Boq - 15.04.2022 - FDocument24 pagesNXP Elec Boq - 15.04.2022 - FShreya BhattacharyaNo ratings yet
- EXCAVATOR CAT 330D2L SpecalogDocument32 pagesEXCAVATOR CAT 330D2L Specalogganendra santantika100% (1)
- Term Paper On CarsDocument4 pagesTerm Paper On Carsc5p4r60c100% (1)
- Updating The QR Factorization and The Least Squares Problem (2008)Document73 pagesUpdating The QR Factorization and The Least Squares Problem (2008)Eran MaromNo ratings yet
- RESEARCH REVIEWER 2nd GRADINGDocument13 pagesRESEARCH REVIEWER 2nd GRADINGAngelica AlfonsoNo ratings yet
- Mainframes: z-OS Overview Concepts and ArchitectureDocument5 pagesMainframes: z-OS Overview Concepts and ArchitectureNagfaceNo ratings yet
- 238 2316 LED UserDocument44 pages238 2316 LED UserKangyerka AndrásNo ratings yet
- JetCat Binary Protocol V22 04 06 BDocument30 pagesJetCat Binary Protocol V22 04 06 BRoberto AlmeidaNo ratings yet
- Evaluating The Condition & Remaining Life of Older Power PlantsDocument7 pagesEvaluating The Condition & Remaining Life of Older Power PlantsAlif Nur FirdausNo ratings yet
- What Are Your Children Watching On Youtube?: December 2011Document11 pagesWhat Are Your Children Watching On Youtube?: December 2011Quỳnh nhiNo ratings yet
- Lec 1 IntroductionDocument11 pagesLec 1 IntroductionHajipur RajNo ratings yet
- Unit I Lesson 4 Computing The Variance of A Discrete Probability DistributionDocument23 pagesUnit I Lesson 4 Computing The Variance of A Discrete Probability DistributionKira MilestoneNo ratings yet
- Modular 3 phase relay dataDocument8 pagesModular 3 phase relay dataPyramid ElectricalNo ratings yet
- AEPS ReconciliationDocument5 pagesAEPS ReconciliationAmey More100% (1)
- Dresser 10C25 Meter IOM Manual CompressedDocument74 pagesDresser 10C25 Meter IOM Manual Compressedangel017No ratings yet
- MercuryAPI v1.31.3 Release Notes - v1cDocument119 pagesMercuryAPI v1.31.3 Release Notes - v1cWallace MunizNo ratings yet
- LogcatDocument39 pagesLogcatazarane38No ratings yet
- Google Drive Resume Template FreeDocument4 pagesGoogle Drive Resume Template Freec2k2x8ds100% (1)
- Unisonic Technologies Co., LTD: NPN Epitaxial Silicon TransistorDocument5 pagesUnisonic Technologies Co., LTD: NPN Epitaxial Silicon TransistorDuvan AriasNo ratings yet
- GLORIANET NETWORKING HUBDocument5 pagesGLORIANET NETWORKING HUBrenoNo ratings yet
- Flujometro SierraDocument52 pagesFlujometro SierraCapacitacion TodocatNo ratings yet
- Fundamentals of Computers: Reema TharejaDocument39 pagesFundamentals of Computers: Reema TharejaYash SharmaNo ratings yet
- Gtu MCQ: Dynamics of Machinery (3151911)Document2 pagesGtu MCQ: Dynamics of Machinery (3151911)kannu19802550No ratings yet
- Huawei Data Center Facility Handbook 20230425-1Document67 pagesHuawei Data Center Facility Handbook 20230425-1SatriaWahyuEkaSaputraNo ratings yet
- Draw wiring diagram in Orcad CaptureDocument28 pagesDraw wiring diagram in Orcad CapturedanyNo ratings yet
- TuTuApp VIP Free Download On iOS, Android & PC (OFFICIAL)Document1 pageTuTuApp VIP Free Download On iOS, Android & PC (OFFICIAL)vinabondowosoNo ratings yet
- 1-MHz Self-Driven ZVS Full-Bridge Converter For 48-V Power Pod and DC-DC BrickDocument10 pages1-MHz Self-Driven ZVS Full-Bridge Converter For 48-V Power Pod and DC-DC Brick李漢祥No ratings yet
- The Category Partition MethodDocument11 pagesThe Category Partition MethodAndrew FuNo ratings yet
- Om MFL67851603-15Document92 pagesOm MFL67851603-15josehugoqrNo ratings yet