Professional Documents
Culture Documents
Lower Limb Evaluation Format Lower Limb Fracture Assesstment Form
Uploaded by
sridharOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lower Limb Evaluation Format Lower Limb Fracture Assesstment Form
Uploaded by
sridharCopyright:
Available Formats
Lower Limb Evaluation Format
LOWER LIMB FRACTURE ASSESSTMENT FORM
Demographic Data:
Name :
Age:
Gender:
IP Number:
Occupation:
Address:
History relevant to present condition:
Mode of injury:
orthopedics management:
surgical management:
Investigation:
Lab reports
Radiology
Co-Morbidities:
Diabetes mellitus
Hypertension
Osteoporosis
Observation:
General body appearance
Limb is positioned in BB splint with traction-Yes/No
Position of comfort adapted by patient when not in traction (if any):
Extent of cast/external fixator/ Surgical Incision
Swelling
Drain(if any)
Palpation:
Edema/Swelling
Capillary refill
Muscle spasm/guarding (if relevant)
Pulse
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 1/12
Lower Limb Evaluation Format
Testing:
Sensory Examination:
*In area below the fracture (Present/Absent)
Pain Examination:
pain in area other than the fracture area (if relevant)
Screening of other limbs
Motor Examination:
Muscle Girth:
Right Left
Thigh
Leg
Arm
Forearm
Hand
Range of motion:
ROM of Joint proximal and distal to the Active range
fracture site
Muscle strength:
-Manual Muscle Testing of joints proximal and distal to fracture site.
Functional Movement analysis :
- Lying to side lying / sitting
- Sit to stand
- Walking
- Stair climbing
Functional Evaluation:
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 2/12
Lower Limb Evaluation Format
FIM
Bed mobility
Transfer-bed –chair-bed
Sit-stand
Balance
Expected Function (Prognosis)
Proximal and distal joint mobility/strength
Self dependency during bed mobility/transfer/sit to stand/gait
Plan of Care: Pre-operative/Post-Operative
SMART GOALS
Treatment Plan:
*Treatment based on recent evidence /guidelines
Progress Note:
Functional range with assistance/without assistance
Active Lower limb function
Discharge Goals:
No swelling in ankle/knee
Functional range of joints proximal and distal to fracture
Minimal dependency while transfer
Ambulation upto 50 mts with assistive device
Can climb atleast 5 steps with crutch/canes
Home –exercise Program:
Exercise diagram No. of sets Repetition Do’s Don’t
Follow-Up:
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 3/12
Lower Limb Evaluation Format
Clinical Reasoning
Clinical relevance /
Special
contributing factors / Important Information
attention
Hypothesis / Reasoning
Healing / degenerative
Age changes /osteoporosis/
balance / strength / mobility
Reason for surgery
Surgical History – Incision /
HT/IHD/DM/ osteoporosis /
type of implant
previous trauma
Surgical Relevant medical conditions
history and Presenting complaints (list)
Previous Functional status
co- Relevant Past history ( Body
Activity Status
morbidities Function status/ Activity
Status) / contributing factors
Assisted devices used for
that may influence the
supports, transfers and
exercise planning)
mobility
To get information on the
Lab To correlate with the present level infection, inflammation
investigation condition of the patient and to test the level of
calcium precursors
To identify the type ,extent of
Radiology Severity of the injury
fracture
BMI
General – ( whole body To understand obesity /
appearance) overweight contributing to
OA, Joint loading
Healing
Surgical Incision, Swelling,
(stages-inflammatory/
Presence of drain tubes
Observation remodelling etc.,)
Scar (grading)
Position of comfort adapted To understand which position
by patient when not in relieves pain and also it
traction (if any): would help in educating them
regarding the position of limb
Extent of cast/external To understand the mobility
fixator/ Surgical Incision and stability of proximal and
distal joint
Edema/Swelling
Palpation Sign of inflammation/Pain
Capillary refill
To understand peripheral
perfusion(normal/decrease)
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 4/12
Lower Limb Evaluation Format
Sensory To understand if there is any
Examination
nerve involment
pain If pain
intensity is
more then
other motor
examination
should not be
performed.
Discuss with
To identify flags, relate to
nurse in
surgical history,healing,
charge
medication
regarding
pain
medication
and patient
need to be
followed up
after pain
reduction.
Girth measurement
(differentiate between
Tests for
swelling / wasting) Relate with observation
effusion /
- Limb Oedema (identify
Clinical
possible causes Test – Homan’s sign
reasoning
(decreased mobility ,
DVT, etc.,)
Active Range of Motion of Perform on
Movement pattern, quantity,
joints proximal and distal to plinth not on
muscle activity, kinematics,
fracture site. bed in supine
protective mechanism)
and sitting to
Identify
evaluate the
- Lag
muscle
- Muscle inhibition
activity
- Muscle power
(torque)
Strength of muscles proximal
Strength (MMT)
and distal to fracture site.
Perform test
to rule out
To observe the activity of
Isometric Resisted Test tightness of
muscle
capsule or
muscles
Functional Movement - Lying to side lying /
analysis sitting
- Sit to stand
( relate with normal pattern, - Walking
identify the possible - Stair climbing
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 5/12
Lower Limb Evaluation Format
structure)
Total assist/
max/mod/min assist /
Independent
Movement pattern at
Functional Status knee ( available flexion)
Distance walked
(observe for discomfort
during function and gait)
balance -sitting and standing
PT Plan of care
Pre- op / Prehabilitation
Mode Reasoning
Exercise counselling To Gain confidence
Upper limb exercise Assistance in mobility / crutches
Bed mobility exercise To prevent DVT, Pressure sores
Activation for Quads/ hams/ Hip
Exercises to affected side( knee/ Hip and Abd/Extensors / Calf muscles
ankle) ( aid in re-education during inhibition post-
surgery)
training for Quads/ hams/ Hip Abd/Extensors
Exercises to Un affected side (knee/ Hip / Calf muscles
and ankle) ( aid in re-education during inhibition post-
surgery)
Functional education and training
Mobility
Post operative
Treatment Reasoning / Progression Progress note
Gain confidence Exercise education
Decrease Pain Understand the underlying Pain rating (VAS /
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 6/12
Lower Limb Evaluation Format
causes of pain NPRS), quality and
- Cryotherapy - Inflammatory compliance at each visit.
- CPM - Chronic
- Positioning - Structural
- Muscle activation ( active - Muscle guarding
exercise / isometric - Effusion
exercises) - Cryotherapy ( once in
every 6 hours till 6th post
Support /bracing ( to avoid op day)
knee contractures/ FFD as
patient tends to keep in resting
position because of pain)
Oedema control - Compression - Active exercises with
- Elevation elevation
- ST mobilization (If - Activity modification
required) (elevation in between
with active exercises)
Restore ROM Increase Range of motion Increasing each visit (10-
15 days)
Active extension without lag
AROM –
Note: ROM returning to prior Identify active structure
level. function (Activation/
If they had contracture, they Inhibition)
are more likely to have in post
op
- Quadriceps sets
- Straight leg raise (SLR)
- Supine heel slides,
- Short arc Extension
- Sit to stand
- Supine leg press (on
pillows )
Slowly progress to
- Resisted exercises (
minimal weights / 30%
EST RM) in available
range
- Controlled flexion and
extension in high Sitting (
support if required)
- Static cycle
Modalities
- Electrical Stimulation
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 7/12
Lower Limb Evaluation Format
- COLD PACK
- CPM
Safe transfers and ambulation Distance ( 50 meters) Increase incrementally at
with assistive device Observe and train use of knee each visit ( 10- 25%)
flexion during gait Add functional training
for lower limb ( sit to
stand, stepping, stair
climbing, over obstacles)
Prevention of Tightness and Positioning / brace ( 0 degrees Progress to stretching
Contracture while sleeping / resting in bed exercises and ST
mobilization if tightness
Skin / Incisional scar Active exercises during sitting of structures are identified
Joint - PF joint / Capsule Stretching exercises
ST mobilization / scar
mobilization
Gait training / Mobility Based to type of implant Progress to
decide on weight bearing - Normal gait without
NWB-TTWB-PWB- assistive device
Weight bearing as tolerated - Stair climbing
(WBAT) – ( walker / crutches/ - Gait obstacles
canes)
Home exercise program (HEP)
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 8/12
Lower Limb Evaluation Format
Progress Notes
Components 0- 2 weeks 3-6 weeks 6-12 weeks
- Emphasis on - Emphasis on - Emphasis on
Exercise
Importance of Exercise Importance of precautions and
education
- Provide education on strength, balance and preventive
“hurt (vs) harm function measures
- Cryotherapy
- Positioning of Knee
and related joints Pain must decrease
- Muscle activation during rest at this stage. - Pain must
(active exercise / decrease at this
isometric exercises) Pain during movement stage.
- Support /bracing ( to must be identified and
avoid knee patient must be given - Identify pain
contractures/ FFD as exercise education. due to fatigue,
Pain patient tends to keep in educate patient
resting position Eg. Pain at the end of appropriately
because of pain) flexion may be due to
Pain must decrease stretch in anterior - Identify
gradually after 24 – 48 structures / Qaud structures
hours, indicate if there is (identify and treat the causing pain
increase. cause) (possibly due to
Observe for pain pattern tight structure )
during movements.
Educate about pain, during
exercise
- Compression
- ST mobilization Usually minimal
- Elevation
Oedema - Active exercises of or no swelling at
- ST mobilization (If
knee with elevation. this stage.
required)
- Ultra sound
(US) – Flexion
- CPM –Knee (0-100)
contracture/ scar
(progress to 125)
Modalities - Moist heat
- TENS if necessary - ES
(Pain and - Contrast bath
- Cryotherapy (once in - Cryotherapy after
oedema - Whirl pool bath
every 6 hours till 6th exercises
management) or pool ( after 6
post op day)
weeks and
- Electrical Stimulation
incision is
(ES)
completely
healed)
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 9/12
Lower Limb Evaluation Format
AROM –
Identify active structures
limiting ROM and function AROM – expected
(Activation/ Inhibition) 0 – 110 active / passive
IF inhibited start with
Increasing each visit
facilitation techniques ( If not achieved continue
(10-15 days) toward
EST / Isometric exercise) exercise as 2 weeks
125 degrees flexion,
and 0 degrees
Stretching Knee /Hip - Active
extension.
Use techniques based on Exercises
examination & reasoning Resisted exercises
- Functional
- Passive structure - 1 RM evaluation
movements (re-
tightness (use static (Functional – leg
education)
stretching) press)
- Lateral and
- Active structure - Theraband standing
multidirectional
shortening (use PNF total knee extension
movements
techniques ) (TKE)
- Strengthening
- High sitting
exercise (1RM
Achieve 0 degrees active exercises (knee
60% to 80%)
extension without lag extension and
- Quadriceps, hip
(100 degrees flexion, and 0 flexion) with weights
and core
degrees extension – - Hip ( weights at
strengthening
increase to 110 degrees at thigh)
nd - emphasis on use
Restore the end of 2 week) - Stand to sit / bed
of the affected
ROM - Quadriceps sets transfer training
side during
- Straight leg raise (SLR) Proprioception and
function such as
- Patellar glides Neuromuscular re-
rising from
(mobilization) education
sitting
- Supine heel slides, - Gait / movement/
- Stand to sit
- Short arc Extension balance /weight
(independent)
- Sit to stand squats transfers)
- Proprioception
- Supine leg press (on - Standing balance
training
pillows ) training – even and
- Progress
- Resisted exercises uneven surface
Functional
(minimal weights / (wobble board)
training for
30% RM) in available - Progress to single
lower limb
range leg standing ( with
without support
- Controlled flexion and short duration
and increased in
extension in high progress
the repetition
Sitting ( support if incrementally)
and distance
required) - Add functional
(sit to stand,
- Static cycle / pedo training for lower
stepping, stair
cycle limb (with support if
climbing, over
required) (sit to
obstacles)
Note: ROM returning to stand, stepping, stair
prior level. climbing, over
If they had contracture, obstacles)
they are more likely to
have in post op
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 10/12
Lower Limb Evaluation Format
- Increase distance
incrementally at each
visit ( 10%) – Full
With assistive device - Normal gait
Weight bearing with
- Distance at patients without assistive
no of minimal
comfort device
support
NWB,TTWB,PWB,We
ight bearing as - Stairs with
- Attain normal
tolerated (WBAT) – reciprocal gait
Safe transfers kinematics and
(walker / crutches/ for without
and weight bearing
canes) increase support
ambulation
incrementally day by - Independent
- Temporal and
day (based on transfers to and
Spatial parameters of
evaluation) from the bed/
gait normalization
- Observe and train use ground
and training
of knee flexion during - Independent
gait function
- Stairs with assistance
(rail support)
Positioning / brace ( 0
degrees while sleeping /
resting in bed
Tightness Progress to stretching
Active exercises during ST mobilization
and exercises and ST
sitting Stretching ( static)
Contracture mobilization if tight
Stretching exercises
ST mobilization / scar
mobilization
Home
HEP written based on HEP written based on HEP written based
exercise
patient goals with special patient goals with on patient goals
program
precautions special precautions with dos and don’ts
(HEP)
- PROM to be
achieved with
minimal force - Lifting more
- Watch incision for
- Avoid rapid forced than 10 kgs
signs of separation
during Gait and during
and/or infection.
Precautions functional functional
- Keep incision strain at
movements ( sit to activities
a minimum, watch
stand etc.,) - Body weight
blanching during
- Incision/ infection (maintenance)
flexion to monitor this.
issues / scar
- Avoid running and
jumping
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 11/12
Lower Limb Evaluation Format
- Continuing
improvement in
ROM
- No extension lag
- Improvement in
- Achievement of
quadriceps function,
- Improvement in ROM, ROM
Progression gait and activity
muscle function and
criteria tolerance
gait over the first 2 - No extensor lag
- Single crutch or a
weeks.
cane
- Walking short
distances without
anassistive device.
- Non-antalgic gait
pattern
Knee range – 110
Functional range – 100
degrees achieved
degrees achieved
Gait – 100 meters with
Gait – 50 meters with - Achievement of
minimum support or 50
Discharge minimal support / No ROM 0-125
meters without support
summary support HEP – adherence
Stair climbing minimum
Stair climbing minimum 4
10 steps up and down
steps up and down with
support
HEP – adherence
If goals are NOT achieved and patient is maximally dependent for ADL
Note then refer to Physical Medicine and Rehabilitation centre (PMRC) -JSSH
for further evaluation and rehabilitation.
If Patient is moderately dependent for ADL refer to Physiotherapy OPD
If patient is not stable with co-morbidities and not willing to stay
inPMR/visit OPD,refer Home care physiotherapy
JSS COLLEGE OF PHYSIOTHERAPY
DEPT OF MUSCULOSKELETAL AND SPORTS Page 12/12
You might also like
- Detoxification and Chelation Protocols GuideDocument213 pagesDetoxification and Chelation Protocols Guidedoggydog100% (3)
- Three Components of Energy ExpenditureDocument26 pagesThree Components of Energy ExpenditureDustin HarrisonNo ratings yet
- A Foot Core Approach To Treating Plantar Fasciitis SmallDocument4 pagesA Foot Core Approach To Treating Plantar Fasciitis SmallLeticia MeleganNo ratings yet
- Design of A Hand OrthosisDocument251 pagesDesign of A Hand OrthosisIsrael BlancoNo ratings yet
- Optimising The Late Stage Rehabilitation and Return To Sport Training and Testing Process After ACL ReconstructionDocument16 pagesOptimising The Late Stage Rehabilitation and Return To Sport Training and Testing Process After ACL ReconstructionDeivison Fellipe da Silva CâmaraNo ratings yet
- Gait Analysis: Prerequisite of Normal GaitDocument4 pagesGait Analysis: Prerequisite of Normal GaitKieran Levi100% (1)
- The Foot Posture Index: Six Item Version FPI-6 User Guide and ManualDocument19 pagesThe Foot Posture Index: Six Item Version FPI-6 User Guide and ManualBryan AlimNo ratings yet
- Gait Analysis 16th JuneDocument40 pagesGait Analysis 16th JuneNaveen BharatNo ratings yet
- ACL Opitz PresentationDocument90 pagesACL Opitz PresentationJuli ElvianiNo ratings yet
- Abbreviations in PhysiotherapyDocument53 pagesAbbreviations in PhysiotherapyPhysiotherapist AliNo ratings yet
- PT Ed Hiprehab PDFDocument13 pagesPT Ed Hiprehab PDFwanderlastNo ratings yet
- GAIT 2 - Clinical Gait Analysis - HandoutDocument32 pagesGAIT 2 - Clinical Gait Analysis - Handoutj100% (1)
- GaitDocument15 pagesGaitआशिष दादाNo ratings yet
- Are Crunches and Back Extensions Breaking Your SpineDocument1 pageAre Crunches and Back Extensions Breaking Your SpineInfinity RapidfireNo ratings yet
- Pregnancy Induced Hypertension (Pih)Document56 pagesPregnancy Induced Hypertension (Pih)shandi23100% (5)
- Walking AidsDocument38 pagesWalking AidsMurad KurdiNo ratings yet
- Mri Signa Ge Book PDFDocument74 pagesMri Signa Ge Book PDFDicky YkcidNo ratings yet
- Imaging Findings and Clinical Correlation: Cerebral Herniation SyndromesDocument64 pagesImaging Findings and Clinical Correlation: Cerebral Herniation SyndromessridharNo ratings yet
- Imaging Findings and Clinical Correlation: Cerebral Herniation SyndromesDocument64 pagesImaging Findings and Clinical Correlation: Cerebral Herniation SyndromessridharNo ratings yet
- Ex Phys - ContentDocument41 pagesEx Phys - ContentxanaduNo ratings yet
- Screenshot - Ankle and Foot ComplexDocument4 pagesScreenshot - Ankle and Foot Complexno nameNo ratings yet
- Sudden Infant Death SyndromeDocument20 pagesSudden Infant Death SyndromesridharNo ratings yet
- Lean Eating for Women – Phase 2 Intensifies WorkoutsDocument21 pagesLean Eating for Women – Phase 2 Intensifies WorkoutsĐạt NguyễnNo ratings yet
- Vinayagar Agaval - Avvaiyar PDFDocument17 pagesVinayagar Agaval - Avvaiyar PDFkckejaman100% (1)
- Stair Climbing StudyDocument9 pagesStair Climbing StudyEric ChambersNo ratings yet
- Effects of Plyometric Training Versus Traditional Weight Training On Strength Power and Aesthetic Jumping Ability in Female Collegiate DancersDocument8 pagesEffects of Plyometric Training Versus Traditional Weight Training On Strength Power and Aesthetic Jumping Ability in Female Collegiate DancersJessica FoongNo ratings yet
- Clinical Training Profile:: PhysiotherapyDocument17 pagesClinical Training Profile:: Physiotherapyrenata miateliNo ratings yet
- Biomaterials (BIOL 1120) Professor Beth Zielinski Professor Jeffrey R. Scott Jacqueline Chang Timothy ChouDocument12 pagesBiomaterials (BIOL 1120) Professor Beth Zielinski Professor Jeffrey R. Scott Jacqueline Chang Timothy Choukuy thanNo ratings yet
- Morse Fall Scale AssessmentDocument5 pagesMorse Fall Scale AssessmentQueen ShNo ratings yet
- Patterns of PNFDocument39 pagesPatterns of PNFsridhar100% (1)
- NutritionCenter CalorieNeeds PDFDocument3 pagesNutritionCenter CalorieNeeds PDFAbhishek RajNo ratings yet
- Perineum RepairDocument5 pagesPerineum RepairYwagar YwagarNo ratings yet
- EYE Emergency Manual An Illustrated Guide: Second EditionDocument51 pagesEYE Emergency Manual An Illustrated Guide: Second EditionMin MawNo ratings yet
- WHO Smallpox Eradication Programme Strategy EvolutionDocument56 pagesWHO Smallpox Eradication Programme Strategy EvolutionRahul NetragaonkarNo ratings yet
- Bag technique nursing careDocument2 pagesBag technique nursing careDanz KieNo ratings yet
- Grand Case PresentationDocument28 pagesGrand Case PresentationRae Marie AquinoNo ratings yet
- Orthosis For Sports InjuryDocument38 pagesOrthosis For Sports InjuryIipo ChennaiNo ratings yet
- SKOLIOSIS MANAGEMENTDocument16 pagesSKOLIOSIS MANAGEMENThunter_axl01No ratings yet
- 5 - JenislatihanDocument55 pages5 - JenislatihanANDREW CHUA ZHI YUNo ratings yet
- CONCEPTS OF MOVEMENtDocument40 pagesCONCEPTS OF MOVEMENtCliff LentoNo ratings yet
- Uerm RoodsDocument53 pagesUerm RoodsNikka VentorilloNo ratings yet
- Tulsa Track and Field Drill Sheet WarmupsDocument9 pagesTulsa Track and Field Drill Sheet WarmupsJon HughesNo ratings yet
- Neural Adaptations To Resistance TrainingDocument12 pagesNeural Adaptations To Resistance TrainingDanusa AlvesNo ratings yet
- 肌肉骨骼及復健學 考古題統整Document43 pages肌肉骨骼及復健學 考古題統整祁慕杰No ratings yet
- MPT Syllabus 2018Document125 pagesMPT Syllabus 2018ajaykumar soddalaNo ratings yet
- Orthopedic Physical Examination (DR - Bayu)Document45 pagesOrthopedic Physical Examination (DR - Bayu)Ghisca Chairiyah AmiNo ratings yet
- Chap 2 Pengukuran Kekuatan OtotDocument64 pagesChap 2 Pengukuran Kekuatan OtottianNo ratings yet
- Levers Pulleys Human BodyDocument41 pagesLevers Pulleys Human BodyAzfar Khurshid MalghaniNo ratings yet
- Volkmann's Ischemic Contracture by Innocent C. AbuguDocument38 pagesVolkmann's Ischemic Contracture by Innocent C. AbuguChukwuemeka ChidogoNo ratings yet
- Gait by SRSDocument109 pagesGait by SRSSreeraj S RNo ratings yet
- ISSA Online Coaching Certification Everyday Athlete Block 1Document10 pagesISSA Online Coaching Certification Everyday Athlete Block 1Sven PhamNo ratings yet
- Olympic Weight Lifting Explosive Full-Body WorkoutDocument24 pagesOlympic Weight Lifting Explosive Full-Body WorkoutIyappan SubramaniNo ratings yet
- B.P.Ed. Third Semester (CBS) Examination Sports Medicine Physiotherapy and Rehabilitation (Elective Course)Document6 pagesB.P.Ed. Third Semester (CBS) Examination Sports Medicine Physiotherapy and Rehabilitation (Elective Course)Devashish SahasrabudheNo ratings yet
- Functional Re EducationDocument45 pagesFunctional Re EducationThopu UmamaheswariNo ratings yet
- KMC Dept of Orthopaedics Floor Reaction OrthosisDocument5 pagesKMC Dept of Orthopaedics Floor Reaction OrthosischinmayghaisasNo ratings yet
- CKC vs OKC Exercises - Functional Strength TrainingDocument2 pagesCKC vs OKC Exercises - Functional Strength Traininginrmpt77No ratings yet
- Field-Based Health-Related Physical Fitness Tests in Children and Adolescents: A Systematic ReviewDocument10 pagesField-Based Health-Related Physical Fitness Tests in Children and Adolescents: A Systematic ReviewAyamKalkun BandungNo ratings yet
- Sidorkewicz 2014 - Efectos de Orientación de La Cadera en La Activación de Glúteo Medio y TFL, en Ejercicios Sin Carga de PesoDocument6 pagesSidorkewicz 2014 - Efectos de Orientación de La Cadera en La Activación de Glúteo Medio y TFL, en Ejercicios Sin Carga de PesoVanesaSandovalNo ratings yet
- Functional Re-EducationDocument8 pagesFunctional Re-EducationPratibha SalkarNo ratings yet
- 231a - Reconsidering The Way We Look at Movement-VCUDocument19 pages231a - Reconsidering The Way We Look at Movement-VCUwolfgate0% (1)
- Elbow Biomechanics 2019Document18 pagesElbow Biomechanics 2019Smriti Grover100% (1)
- Tele Rehabilitation Service Delivery Journey From Prototype To Robust in Home Use D and R OnlineDocument10 pagesTele Rehabilitation Service Delivery Journey From Prototype To Robust in Home Use D and R OnlineFelipe Palma UrrutiaNo ratings yet
- Knee, Ankle and Foot Joint MobilizationDocument17 pagesKnee, Ankle and Foot Joint MobilizationLokesh SharmaNo ratings yet
- Biomechanicks of Snatch Technique of Hghly Skilled and Skilled WeigthliftersDocument6 pagesBiomechanicks of Snatch Technique of Hghly Skilled and Skilled WeigthliftersStuarNo ratings yet
- PPTDocument61 pagesPPTNazia ArifNo ratings yet
- NKT FlowChart - PDF Version 1 PDFDocument2 pagesNKT FlowChart - PDF Version 1 PDFJay SarkNo ratings yet
- CPT Exam Study Guide: Program Design and Exercise ModalitiesDocument5 pagesCPT Exam Study Guide: Program Design and Exercise Modalitiessiriamma wiliamsNo ratings yet
- SC RunningDocument18 pagesSC RunningNiña PanganibanNo ratings yet
- (BAL) What Is A Balance BoardDocument2 pages(BAL) What Is A Balance Boardapi-3695814No ratings yet
- Damage Control Orthopaedics in Spinal Trauma JAAOSDocument12 pagesDamage Control Orthopaedics in Spinal Trauma JAAOSAzmi FarhadiNo ratings yet
- Pedia TablesDocument4 pagesPedia TablesVanCancioNo ratings yet
- A Kinetic Chain Approach For Shoulder RehabDocument9 pagesA Kinetic Chain Approach For Shoulder RehabRicardo QuezadaNo ratings yet
- Gait Biomechanics 1Document43 pagesGait Biomechanics 1Dibyendunarayan Bid50% (2)
- JSS College of PhysiotherapyDocument8 pagesJSS College of PhysiotherapyDANIA NAJUA BINTI ZAINALNo ratings yet
- Hepatitis B VirusDocument47 pagesHepatitis B VirusDiah Puspita RiniNo ratings yet
- Guidelines For Pre Submission Seminar-LPUDocument1 pageGuidelines For Pre Submission Seminar-LPUsridharNo ratings yet
- IIITDM Yoga HandbookDocument24 pagesIIITDM Yoga HandbookBenoit HsuNo ratings yet
- Liver Enzymes (AST-ALT)Document3 pagesLiver Enzymes (AST-ALT)sridharNo ratings yet
- Adverse Reaction To DrugsDocument22 pagesAdverse Reaction To DrugssridharNo ratings yet
- Inflammatory My Opa ThiesDocument10 pagesInflammatory My Opa ThiessridharNo ratings yet
- Brachial Plexus InjuryDocument43 pagesBrachial Plexus InjurysridharNo ratings yet
- PNFDocument39 pagesPNFsridhar100% (1)
- Nerve Conduction Velocity StudiesDocument12 pagesNerve Conduction Velocity StudiessridharNo ratings yet
- Brachial Plexus InjuryDocument43 pagesBrachial Plexus InjurysridharNo ratings yet
- 01-13 2 End Diastolic Pneumatic Compression Boot As A Treatment of PVD or LymphedemaDocument4 pages01-13 2 End Diastolic Pneumatic Compression Boot As A Treatment of PVD or LymphedemasridharNo ratings yet
- 10-11 Gbs General Neuro 2nd YearDocument29 pages10-11 Gbs General Neuro 2nd YearsridharNo ratings yet
- Brachial Plexus InjuryDocument43 pagesBrachial Plexus InjurysridharNo ratings yet
- College of NursingDocument1 pageCollege of NursingsridharNo ratings yet
- Ankle MobilizationDocument16 pagesAnkle MobilizationsridharNo ratings yet
- Tardieu ScaleDocument2 pagesTardieu ScalesridharNo ratings yet
- Thoracic Spine AnatomyDocument5 pagesThoracic Spine AnatomysridharNo ratings yet
- Infra RedDocument7 pagesInfra RedsridharNo ratings yet
- Windlass Effect Ankle JointDocument35 pagesWindlass Effect Ankle JointsridharNo ratings yet
- Application FormatDocument2 pagesApplication FormatsridharNo ratings yet
- Clavicle FractureDocument4 pagesClavicle FracturesridharNo ratings yet
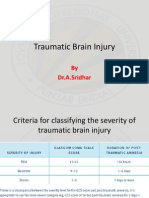
- Traumatic Brain InjuryDocument26 pagesTraumatic Brain InjurysridharNo ratings yet
- Skanda Shasti KavachamDocument6 pagesSkanda Shasti KavachamsriramanaNo ratings yet
- Clavicle FractureDocument9 pagesClavicle FracturesridharNo ratings yet
- Doctors - Dermatologists Area Phone: Tuesday, 13 November 2007 13:51Document18 pagesDoctors - Dermatologists Area Phone: Tuesday, 13 November 2007 13:51pinakindpatelNo ratings yet
- Polidocanol Asclera Varithena National Drug Monograph FinalDocument27 pagesPolidocanol Asclera Varithena National Drug Monograph FinalbvarianoNo ratings yet
- The 5 Best Homeopathic Medicines For Foot Corns AreDocument6 pagesThe 5 Best Homeopathic Medicines For Foot Corns AreKamalakarAthalyeNo ratings yet
- MS2 - Neurologic Disorder My ReportDocument30 pagesMS2 - Neurologic Disorder My ReportNeil Lansang BallobanNo ratings yet
- Palatal SwellingsDocument6 pagesPalatal Swellingsopi akbarNo ratings yet
- Ayurvedic Treatment of PCOSDocument5 pagesAyurvedic Treatment of PCOSArun AchalamNo ratings yet
- Price Needs Updating, Should We Call The Police?: C M Bleakley, P Glasgow, D C MacauleyDocument2 pagesPrice Needs Updating, Should We Call The Police?: C M Bleakley, P Glasgow, D C MacauleyAna BelchiorNo ratings yet
- Guide to General Dermatology Disorders and DiseasesDocument147 pagesGuide to General Dermatology Disorders and DiseasesCarlos DNo ratings yet
- NonCytotoxic Dibenzyl and Also Difluoroborate Capmatinibxlsxoid Fluorophores Permit Visual Image Involving Nucleus or Even Cytoplasm Inside Bioimagingixvwj PDFDocument1 pageNonCytotoxic Dibenzyl and Also Difluoroborate Capmatinibxlsxoid Fluorophores Permit Visual Image Involving Nucleus or Even Cytoplasm Inside Bioimagingixvwj PDFtubweed4No ratings yet
- Venepuncture in Adults: Take A Blood Sample Using Vacuum Collection TubesDocument4 pagesVenepuncture in Adults: Take A Blood Sample Using Vacuum Collection TubesimaguestuserNo ratings yet
- Bilirubin Kit PDFDocument2 pagesBilirubin Kit PDFArasNo ratings yet
- 33 Sharalaya - Cardiac Risk of Extreme Exercise (2019)Document7 pages33 Sharalaya - Cardiac Risk of Extreme Exercise (2019)Yuri medranoNo ratings yet
- Guaifenesin Elixir PACKAGE INSERTDocument5 pagesGuaifenesin Elixir PACKAGE INSERTEllie Marie RoyalesNo ratings yet
- Gram StainDocument3 pagesGram StainAbduladheemNo ratings yet
- IMI RANO Critieria Booklet Nov 2011Document18 pagesIMI RANO Critieria Booklet Nov 2011johnthomas75No ratings yet
- Varicose VeinsDocument12 pagesVaricose Veinscheo sealyNo ratings yet
- Urinalysis: Clin. Immunol. / Lab. Work/ Renal Disorders/ Urine Analysis/ Dr. Batool Al-HaidaryDocument11 pagesUrinalysis: Clin. Immunol. / Lab. Work/ Renal Disorders/ Urine Analysis/ Dr. Batool Al-HaidaryIM CTNo ratings yet
- Tetanus LectureDocument34 pagesTetanus LectureWonyenghitari GeorgeNo ratings yet
- 2 2 1Document14 pages2 2 1LaurenGoNo ratings yet
- Unstable Blood Glucose Level: Criteria Computation Actual Score JustificationDocument5 pagesUnstable Blood Glucose Level: Criteria Computation Actual Score JustificationGiselle EstoquiaNo ratings yet
- Angina, MI, CHFDocument7 pagesAngina, MI, CHFJoanne LagusadNo ratings yet