Professional Documents
Culture Documents
Transfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelf
Transfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelf
Uploaded by
مودة المنعميOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelf
Transfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelf
Uploaded by
مودة المنعميCopyright:
Available Formats
An official website of the United States government Here's how you know
Log in
Bookshelf Books Search
Browse Titles Advanced Help
StatPearls [Internet].
Show details
Views
Search this book
PubReader
Print View
Transfusion-related Acute Lung Injury Cite this Page
Min S. Cho; Pranav Modi; Sandeep Sharma.
Author Information In this Page
Last Update: May 1, 2022. Continuing Education Activity
Introduction
Continuing Education Activity Go to:
Etiology
Transfusion-related acute lung injury (TRALI) is a clinical syndrome in which there is an acute, noncardiogenic
Epidemiology
pulmonary edema associated with hypoxia that occurs during or after a transfusion. This activity reviews the
Pathophysiology
evaluation and management of transfusion-related acute lung injury and highlights the role of the interprofessional
team in managing patients with this condition. Histopathology
Objectives: History and Physical
Evaluation
Identify diagnostic criteria for transfusion-related acute lung injury.
Treatment / Management
Describe the pathophysiology of transfusion-related acute lung injury.
Differential Diagnosis
Contrast transfusion-related acute lung injury (TRALI) and transfusion-associated circulatory overload Prognosis
(TACO).
Pearls and Other Issues
Review the importance of improving care coordination amongst interprofessional team members to improve Enhancing Healthcare Team Outcomes
outcomes for patients with transfusion-related acute lung injury.
Review Questions
Access free multiple choice questions on this topic. References
Introduction Go to:
Related information
Transfusion reactions are adverse events that occur after transfusing blood products such as whole blood, fresh frozen
PMC
plasma (FFP), platelets, cryoprecipitate, granulocytes, intravenous immune globulin, allogenic and autologous stem
cells, and packed red blood cells.[1] Transfusion-related acute lung injury (TRALI), is a clinical syndrome in which PubMed
there is acute, noncardiogenic pulmonary edema associated with hypoxia that occurs during or after a transfusion.[2]
It is the leading cause of death from transfusion documented by the U.S. Food and Drug Administration (FDA).
Similar articles in PubMed
Specifically, an incident of TRALI includes 1 in 5000 units of packed red blood cells, 1 in 2000 plasma-containing
An association between decreased cardiopulmonary complications
components, and 1 in 400 units of whole-blood-derived platelet concentrates. (transfusion-related acute lung injury and transfusion-associated
[Transfusion. 2010]
circulatory overload) and implementation of universal
TRALI was first reported in the 1950s but recognized as a distinctive clinical syndrome in 1983.[3] The disorder is Transfusion-related acute lung injury and pulmonary edema in
not only diagnosed clinically but is usually confirmed by radiographic findings. Diagnostic criteria for TRALI is if critically ill patients: a retrospective study. [Transfusion. 2006]
the symptoms develop during or within 6 hours of transfusion without any risk factors for developing acute lung Review Transfusion-associated circulatory overload and
injuries such as sepsis from pneumonia, aspiration, and shock.[4] Physical symptoms include fever, hypotension, and transfusion-related acute lung injury. [Blood. 2019]
tachycardia. Clinical findings include exudative bilateral infiltrates on chest radiograph, no evidence of pulmonary Review Transfusion-related acute lung injury (TRALI): a case
vascular overload, and hypoxemia of SpO2 less than 90% on room air with a ratio of the partial pressure of oxygen to report and literature review. [S D Med. 2011]
a fractional inspired oxygen concentration of less than 300 mmHg.[5][6] Possible TRALI is when there are other risk Review [Transfusion-related acute lung injury (TRALI)].
factors for acute lung injury. Delayed TRALI is when transfusion is completed after 6 to 72 hours, and it is associated [Pneumologie. 2014]
with higher mortality.[5][7] Transfusion-related circulatory overload (TACO) needs to be ruled out as it can be on See reviews...
differential diagnosis due to the similarity of pulmonary edema picture, but due to actual volume overload.[2][3][8] See all...
In the US, TRALI has to be reported to the Blood Banking services.
Recent Activity
Etiology Go to:
Turn Off Clear
True TRALI should not have any risk factors for acute lung injury according to diagnostic criteria. TRALI is caused Transfusion-related Acute Lung Injury - StatPearls
by damage to pulmonary vasculature from neutrophil-mediated in forms of human neutrophil antigen (HNA) or
human leukocyte antigen (HLA) antibodies in donor blood which bind to antigens of a recipient. Storage of blood See more...
products can accumulate proinflammatory mediators that can cause TRALI as well. A two-hit hypothesis applies in
this clinical syndrome. Neutrophil sequestration occurs in the pulmonary vasculature, and neutrophils activate to
damage the endothelial layer, causing leakage of protein and fluid into alveolar space.[9][10]
Epidemiology Go to:
Comorbidities suggest risk factors for having TRALI, mechanical ventilation, sepsis, massive transfusion, coronary
artery bypass graft, and end-stage liver disease.[3] Higher TRALI incidence was reported with plasma from female
donors because the literature found parous female donors with multiple HLA antibodies.[11] Other literature
mentioned female donor plasma has larger quantities of anti-HLA class II and HNA positive antibodies. Blood
products that have high plasma contents have been associated with an increased rate of TRALI. Critically ill patients
have a higher incidence of TRALI, not only because they receive more blood products, but they also have clinical
manifestations that activate neutrophil sequestration before the blood transfusion which places them at a higher risk of
acquiring TRALI than the general patient population.
In the US, TRALI has been responsible for at least 30% of transfusion-related deaths. While the mortality rates have
dropped over the past decade, continued awareness is key.
Pathophysiology Go to:
Due to the two-hit hypothesis, the first hit takes place by priming of neutrophils from who are already ill from shock,
sepsis, having organ damage who also had surgery or experienced a great deal of stress from trauma.[12] Increased
levels of interleukin-8, interleukin-6, and elastase-alpha 1-antitrypsin complex cause neutrophil recruitment to the
pulmonary vasculature.[5] Conformational change in beta-2 integrins allows neutrophil to adhere to pulmonary
capillaries.[13][14] The second hit comes from the transfusion itself. Antibodies and bioactive lipids stored in blood
products activate neutrophils, resulting in capillary leakage of intracellular content-releasing proteases and elastase
from the activation of NADPH which eventually oxidase, causing pulmonary edema. Another hypothesis is called the
threshold hypothesis. There is no first hit involved. TRALI can happen in healthy patients who are transfused with
plasma that has high amounts of antibodies whose neutrophil has already activated.
Histopathology Go to:
Histopathology consists of early acute lung distress syndrome (ARDS), revealing interstitial and intra-alveolar edema
and the presence of neutrophils in the interstitial and airway. Lung sections have shown numerous neutrophils in
pulmonary capillaries and small pulmonary vessels.[15]
History and Physical Go to:
Before a blood transfusion, a complete history and physical exam needs to be done to assess the patient's clinical
status. Most likely, the hemoglobin is lower than 7, or they are actively bleeding and need a red blood cell transfusion.
Abnormal coagulation studies with consumptive coagulopathy also warrant correction with FFP or cryoprecipitate
before any interventions or emergent surgery. Within 6 hours of blood transfusion for acute TRALI or 6 to 72 hours
for delayed TRALI, patients can develop body temperature of greater than 100.4 degrees Fahrenheit or 37 degrees
Celcius or hypotension along with acute dyspnea requiring more oxygen via nasal cannula, nonbreathable mask or
even mechanical ventilation depending on severity.[8][5] Patients might use accessory muscles for respiration and
appear to be in acute distress with breathing. Because this is not fluid overload or cardiogenic edema, neck veins are
not distended. Auscultation of the lungs reveals rales and sometimes diminished breath sounds due to pulmonary
edema. TRALI is almost impossible to distinguish from ARDs based on clinical presentation.
Evaluation Go to:
A chest radiograph will show bilateral pulmonary infiltrates. Clinical characteristics of TRALI include acute dyspnea,
hypoxemia, fever, hypotension, tachycardia, leukopenia, thrombocytopenia, and normal pulmonary artery occlusion
pressure due to noncardiogenic pulmonary edema.[8]
Nearly 30% of patients will have low levels of BNP and transient leucopenia.
Treatment / Management Go to:
Immediate management of TRALI is to stop the transfusion and notify the blood bank to screen the donor unit for
antileukocyte antibodies, anti-HLA or anti-neutrophil-specific antibodies.[5] Supportive measures must be taken to
improve oxygenation. Although there is no specific treatment for TRALI, low tidal volume application is feasible in
this case as TRALI's pathophysiology is similar to acute lung distress syndrome (ARDS). Best practice is prevention.
In the United Kingdom, the incidence of TRALI was substantially reduced by using plasma from male donors and
screening female donors for HLA and HNA antibodies which are strong risk factors.
Once the transfusion is stopped, gradual recovery may take 2-4 days. The chest x-ray will improve within 2-5 days.
Differential Diagnosis Go to:
When there is a transfusion reaction with acute dyspnea from respiratory distress, acute pulmonary edema with
diffuse bilateral infiltrates in the chest x-ray, transfusion-associated circulatory overload (TACO) is in the differential
diagnosis. TACO is also a clinical diagnosis with similar clinical pictures as TRALI. However, there are distinct
features that separate two syndromes. TACO can present with fever and hypotension. Even though normal fluid
balance does not rule out TACO, it can happen to patients who have high fluid intake before the transfusion. Due to
volume overload, patients with TACO can have distended neck veins and already reduced ejection fraction (EF) from
heart failure with reduced EF. Pulmonary artery occlusion pressures could be 18 mmHg or greater, secondary to
cardiogenic pulmonary edema with elevated brain natriuretic peptide. Because of cardiogenic pulmonary edema,
TACO has transudate fluids which are low in plasma proteins.[3]
Prognosis Go to:
Despite aggressive support, mortality rates of more than 12% are reported once TRALI is diagnosed. Even those who
survive have a slow recovery.
Pearls and Other Issues Go to:
TRALI can develop within 6 hours to 72 hours of blood transfusions that are rich in plasma. Despite suspected
various hypothesis, it could certainly be prevented with a careful approach in blood transfusions, especially in those
who are more vulnerable for acquiring TRALI. Due to no definitive treatment, prevention is the best key to keep
TRALI from occurring by treating underlying diseases first.
Enhancing Healthcare Team Outcomes Go to:
The diagnosis and management of TRALI is not simple and is best done with an interprofessional team that includes a
hematologist, cardiologist, pulmonologist, internist, and a specialty trained nurse experienced with the care of these
patients. TRALI can develop within 6 hours to 72 hours of blood transfusions that are rich in plasma. Despite
suspected various hypotheses, it could certainly be prevented with the careful approach in blood transfusions,
especially in those who are more vulnerable to acquire TRALI. Due to no definitive treatment, prevention is the best
key to keep TRALI from occurring by treating underlying diseases first.
Nurses who administer blood should be aware of this syndrome as it may present with shortness of breath. At the first
sign of symptoms, the blood transfusion should be discontinued, and the patient monitored in the ICU.[16] The
patient should be closely monitored for at least the next 48-96 hours, and some patients may even require mechanical
ventilation. Nurses should ensure that the patient has DVT prophylaxis and bedsore precautions.
The outcome of patients with TRALI depends on age, the number of other organs involved, the need for mechanical
ventilation, and response to treatment.
Review Questions Go to:
Access free multiple choice questions on this topic.
Comment on this article.
References Go to:
1. Suddock JT, Crookston KP. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 11, 2021.
Transfusion Reactions. [PubMed]
2. Roubinian N. TACO and TRALI: biology, risk factors, and prevention strategies. Hematology Am Soc Hematol
Educ Program. 2018 Nov 30;2018(1):585-594. [PMC free article] [PubMed]
3. Friedman T, Javidroozi M, Lobel G, Shander A. Complications of Allogeneic Blood Product Administration, with
Emphasis on Transfusion-Related Acute Lung Injury and Transfusion-Associated Circulatory Overload. Adv
Anesth. 2017;35(1):159-173. [PubMed]
4. Toy P, Popovsky MA, Abraham E, Ambruso DR, Holness LG, Kopko PM, McFarland JG, Nathens AB, Silliman
CC, Stroncek D., National Heart, Lung and Blood Institute Working Group on TRALI. Transfusion-related acute
lung injury: definition and review. Crit Care Med. 2005 Apr;33(4):721-6. [PubMed]
5. Marik PE, Corwin HL. Acute lung injury following blood transfusion: expanding the definition. Crit Care Med.
2008 Nov;36(11):3080-4. [PubMed]
6. Kim KN, Kim DW, Jeong MA. The usefulness of a classification and regression tree algorithm for detecting
perioperative transfusion-related pulmonary complications. Transfusion. 2015 Nov;55(11):2582-9. [PubMed]
7. Khan H, Belsher J, Yilmaz M, Afessa B, Winters JL, Moore SB, Hubmayr RD, Gajic O. Fresh-frozen plasma and
platelet transfusions are associated with development of acute lung injury in critically ill medical patients. Chest.
2007 May;131(5):1308-14. [PubMed]
8. Skeate RC, Eastlund T. Distinguishing between transfusion related acute lung injury and transfusion associated
circulatory overload. Curr Opin Hematol. 2007 Nov;14(6):682-7. [PubMed]
9. Sachs UJ. Recent insights into the mechanism of transfusion-related acute lung injury. Curr Opin Hematol. 2011
Nov;18(6):436-42. [PubMed]
10. Popovsky MA, Abel MD, Moore SB. Transfusion-related acute lung injury associated with passive transfer of
antileukocyte antibodies. Am Rev Respir Dis. 1983 Jul;128(1):185-9. [PubMed]
11. Toy P, Gajic O, Bacchetti P, Looney MR, Gropper MA, Hubmayr R, Lowell CA, Norris PJ, Murphy EL,
Weiskopf RB, Wilson G, Koenigsberg M, Lee D, Schuller R, Wu P, Grimes B, Gandhi MJ, Winters JL, Mair D,
Hirschler N, Sanchez Rosen R, Matthay MA., TRALI Study Group. Transfusion-related acute lung injury:
incidence and risk factors. Blood. 2012 Feb 16;119(7):1757-67. [PMC free article] [PubMed]
12. Otrock ZK, Liu C, Grossman BJ. Transfusion-related acute lung injury risk mitigation: an update. Vox Sang.
2017 Nov;112(8):694-703. [PubMed]
13. Langereis JD. Neutrophil integrin affinity regulation in adhesion, migration, and bacterial clearance. Cell Adh
Migr. 2013 Nov-Dec;7(6):476-81. [PMC free article] [PubMed]
14. Rossaint J, Zarbock A. Tissue-specific neutrophil recruitment into the lung, liver, and kidney. J Innate Immun.
2013;5(4):348-57. [PMC free article] [PubMed]
15. Nossaman BD. Transfusion-Related Acute Lung Injury (TRALI): Report of 2 Cases and a Review of The
Literature. Ochsner J. 2008 Spring;8(1):32-8. [PMC free article] [PubMed]
16. Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung
injury. Blood. 2019 Apr 25;133(17):1840-1853. [PubMed]
Copyright © 2022, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which
permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s)
and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
Bookshelf ID: NBK507846 PMID: 29939623
FOLLOW NCBI
Connect with NLM National Library of Medicine Web Policies Help
8600 Rockville Pike FOIA Accessibility
Bethesda, MD 20894 HHS Vulnerability Disclosure Careers
NLM NIH HHS USA.gov
You might also like
- Acute Bronchitis - StatPearls - NCBI BookshelfDocument1 pageAcute Bronchitis - StatPearls - NCBI BookshelfJulian Muhammad YasinNo ratings yet
- Fluorescein Angiography - StatPearls - NCBI BookshelfDocument2 pagesFluorescein Angiography - StatPearls - NCBI BookshelfQherine BhelqisNo ratings yet
- Cardiac Disease in Pregnancy - StatPearls - NCBI BookshelfDocument1 pageCardiac Disease in Pregnancy - StatPearls - NCBI BookshelfSi NguyenNo ratings yet
- Nursing Process - StatPearls - NCBI BookshelfDocument1 pageNursing Process - StatPearls - NCBI Bookshelfestical.23nick2No ratings yet
- 71 OriginalArticle 250 1 10 20211123Document9 pages71 OriginalArticle 250 1 10 20211123stephen fadareNo ratings yet
- Physiology, Cardiovascular Murmurs: COVID-19 InformationDocument1 pagePhysiology, Cardiovascular Murmurs: COVID-19 InformationCecil-An DalanonNo ratings yet
- Jurnal IPE - JIC Editorial - Cox Et Al 2016Document4 pagesJurnal IPE - JIC Editorial - Cox Et Al 2016Benk GazeNo ratings yet
- Fever of Unknown Origin - StatPearls - NCBI BookshelfDocument1 pageFever of Unknown Origin - StatPearls - NCBI BookshelfAadya PandeyNo ratings yet
- Do Continence Management Strategies Reduce FallsDocument7 pagesDo Continence Management Strategies Reduce FallsWardah Fauziah El SofwanNo ratings yet
- WWW Ncbi NLM Nih Gov Books NBK513297Document4 pagesWWW Ncbi NLM Nih Gov Books NBK513297Dina Aprilia SariNo ratings yet
- Li Deng 2019 Acupuncture Combined With Swallowing Training For Poststroke Dysphagia A Meta Analysis of RandomisedDocument10 pagesLi Deng 2019 Acupuncture Combined With Swallowing Training For Poststroke Dysphagia A Meta Analysis of RandomisedrezteevicNo ratings yet
- State of Interprofessional Education in Nursing: Nurse EducatorDocument5 pagesState of Interprofessional Education in Nursing: Nurse EducatorAndi Fajrin PermanaNo ratings yet
- Heart Failure and Ejection FractionDocument1 pageHeart Failure and Ejection FractionCecil-An DalanonNo ratings yet
- Schizophrenia - StatPearls - NCBI BookshelfDocument1 pageSchizophrenia - StatPearls - NCBI Bookshelflensa perspectiveNo ratings yet
- Niu 2022Document12 pagesNiu 2022Javiera Abigail Espinoza AlvarezNo ratings yet
- Owen 2014Document6 pagesOwen 2014David PintoNo ratings yet
- Clostridioides Difficile Infection - StatPearls - NCBI BookshelfDocument1 pageClostridioides Difficile Infection - StatPearls - NCBI BookshelfSayyidati IlmiyahNo ratings yet
- 1 s2.0 S0260691718300960 Main PDFDocument3 pages1 s2.0 S0260691718300960 Main PDFAbdulWakhidNo ratings yet
- Thistlethwaite 2015 Anatomical Sciences EducationDocument6 pagesThistlethwaite 2015 Anatomical Sciences EducationIkhwanYudaKusumaNo ratings yet
- Apple and Pear ShapeDocument2 pagesApple and Pear ShapeFirda AnamiNo ratings yet
- 7 - Proteus Syndrome - A Case Report and Review of The LiteratureDocument5 pages7 - Proteus Syndrome - A Case Report and Review of The LiteratureJosé Paulo Ribeiro JúniorNo ratings yet
- An Investigation Into The Barriers To and Priorities For Research Engagement in Health LibrarianshipDocument22 pagesAn Investigation Into The Barriers To and Priorities For Research Engagement in Health LibrarianshipKrisha FernandezNo ratings yet
- Cast On Guay 2014Document6 pagesCast On Guay 2014Jorge Urrutia OrtizNo ratings yet
- Gandhi Steele 2021 Effectiveness of Interventions For Dysphagia in Parkinson Disease A Systematic ReviewDocument23 pagesGandhi Steele 2021 Effectiveness of Interventions For Dysphagia in Parkinson Disease A Systematic ReviewcatalinaNo ratings yet
- A Critical Review of Interventions Targeting ProsodyDocument7 pagesA Critical Review of Interventions Targeting ProsodyDigilindaNo ratings yet
- 2020 - Designing An Intervention in ReadingDocument13 pages2020 - Designing An Intervention in ReadingsofiaNo ratings yet
- Recomendações de OA de Quadril e JoelhoDocument19 pagesRecomendações de OA de Quadril e Joelhokmilapinheiro7No ratings yet
- The Association of Body Mass Index With Difficult Tracheal Intubation Management by Direct Laryngoscopy: A Meta-AnalysisDocument13 pagesThe Association of Body Mass Index With Difficult Tracheal Intubation Management by Direct Laryngoscopy: A Meta-AnalysisdullzineaaNo ratings yet
- Evidence-Based Practice: Joslin John Assistant Professor Caritas College of NursingDocument30 pagesEvidence-Based Practice: Joslin John Assistant Professor Caritas College of NursingJOSLINNo ratings yet
- Enteral Nutrition Provided Within 48 Hours AfterDocument9 pagesEnteral Nutrition Provided Within 48 Hours AfterRoberto MaresNo ratings yet
- Fascistas Plantar y PlaceboDocument12 pagesFascistas Plantar y PlaceboEver MedinaNo ratings yet
- Levett-Jones Et Al-2018-Journal of Nursing Scholarship1Document10 pagesLevett-Jones Et Al-2018-Journal of Nursing Scholarship1Nande BandeNo ratings yet
- Ptj/pzaa 200Document39 pagesPtj/pzaa 200Yenie YenNo ratings yet
- Petechiae - StatPearls - NCBI BookshelfDocument1 pagePetechiae - StatPearls - NCBI Bookshelfmdrnh6shbmNo ratings yet
- Jurnal Nausea and VomitingDocument15 pagesJurnal Nausea and VomitingRisa KarmeylithaNo ratings yet
- Research Developments in Pediatric Intensive CareDocument7 pagesResearch Developments in Pediatric Intensive CareJose VasquezNo ratings yet
- The Sociocultural Contribution To Learning Why Did My Students Fail To Learn Aseptic Non-Touch Technique Multidimensional Factors Involved Inmedical Students' Failure To Learn This SkillDocument14 pagesThe Sociocultural Contribution To Learning Why Did My Students Fail To Learn Aseptic Non-Touch Technique Multidimensional Factors Involved Inmedical Students' Failure To Learn This SkillErza GenatrikaNo ratings yet
- Telerehabilitation 5Document6 pagesTelerehabilitation 5Jerrin JacobNo ratings yet
- VMRR 53266 Diagnosis Prevention and Management of Canine Hip Dysplasia - 051915Document12 pagesVMRR 53266 Diagnosis Prevention and Management of Canine Hip Dysplasia - 051915Lauura Cristina BarriosNo ratings yet
- Neurourology and Urodynamics - 2023 - B - Can You Breathe Yourself To A Better Pelvic Floor A Systematic ReviewDocument19 pagesNeurourology and Urodynamics - 2023 - B - Can You Breathe Yourself To A Better Pelvic Floor A Systematic ReviewDanielle GadelhaNo ratings yet
- Session 1 - Manuskrip SR M11 - Innani Wildania Husna - Innani Wildania With CommentsDocument15 pagesSession 1 - Manuskrip SR M11 - Innani Wildania Husna - Innani Wildania With Commentsrenata JeslynNo ratings yet
- Learning Outcomes For Interprofessional Education (IPE) : Literature Review and SynthesisDocument11 pagesLearning Outcomes For Interprofessional Education (IPE) : Literature Review and SynthesisJane BagaporoNo ratings yet
- 17 - Jic - Learning Outcomes For Interprofessional Education 2010 Thistlethwaite and Moran PDFDocument11 pages17 - Jic - Learning Outcomes For Interprofessional Education 2010 Thistlethwaite and Moran PDFRizka ArifahNo ratings yet
- TAN Assignment BDocument11 pagesTAN Assignment BBea TanNo ratings yet
- European J Cancer Care - 2021 - Kerr - Evaluation of The Role of The Clinical Nurse Specialist in Cancer Care AnDocument13 pagesEuropean J Cancer Care - 2021 - Kerr - Evaluation of The Role of The Clinical Nurse Specialist in Cancer Care AnmfarooqafzalNo ratings yet
- 2020 1830048 PDFDocument14 pages2020 1830048 PDFMarietou SidibeNo ratings yet
- Quality and Safety: Critical Care NursingDocument3 pagesQuality and Safety: Critical Care NursingKristine Marie YlayaNo ratings yet
- Tratamiento Deglución en Enfermedad de ParkinsonDocument8 pagesTratamiento Deglución en Enfermedad de ParkinsonMacarena Paz ÁlvarezNo ratings yet
- Participatory Action ResearchDocument9 pagesParticipatory Action ResearchGilbert BaltazarNo ratings yet
- Radiology and Imaging Diagnosis in Undergraduate Medicine in A Curriculum Using Active Methodologies: A Systematic Review From 2011 To 2021Document5 pagesRadiology and Imaging Diagnosis in Undergraduate Medicine in A Curriculum Using Active Methodologies: A Systematic Review From 2011 To 2021Monika GuptaNo ratings yet
- Act Fisica Reduce La PeriodontitisDocument13 pagesAct Fisica Reduce La PeriodontitisJohnny CHNo ratings yet
- Association Between Otitis Media and Gastroesophageal Reflux: A Systematic ReviewDocument8 pagesAssociation Between Otitis Media and Gastroesophageal Reflux: A Systematic Reviewputri balqisNo ratings yet
- Hydroxyurea Toxicity - StatPearls - NCBI BookshelfDocument1 pageHydroxyurea Toxicity - StatPearls - NCBI BookshelfJatin AnandNo ratings yet
- The Clinical Implementation of Pain Neuroscience Education: A Survey StudyDocument13 pagesThe Clinical Implementation of Pain Neuroscience Education: A Survey Studycookiepower54321No ratings yet
- AITCSArticle InstrumenDocument11 pagesAITCSArticle InstrumenYulianti WulandariNo ratings yet
- Literature Review Back Pain Among NursesDocument9 pagesLiterature Review Back Pain Among Nursesafmzeracmdvbfe100% (1)
- The Relationship Between Physical Activity and Health Status in Patients With Chronic Obstructive Pulmonary Disease Following Pulmonary RehabilitationDocument11 pagesThe Relationship Between Physical Activity and Health Status in Patients With Chronic Obstructive Pulmonary Disease Following Pulmonary RehabilitationJose Luis ParraNo ratings yet
- Fpubh 10 715566Document6 pagesFpubh 10 715566AprillianRizkyaNo ratings yet
- The Effects of Exercise On Balance in Persons WithDocument14 pagesThe Effects of Exercise On Balance in Persons WithMiguelangel AlemánNo ratings yet
- Impact of Serological and Histological Factors On Neurological Manifestations in Children and Adults With Celiac DiseaseDocument10 pagesImpact of Serological and Histological Factors On Neurological Manifestations in Children and Adults With Celiac Diseaseمودة المنعميNo ratings yet
- The Present and The Future in The Diagnosis and Management of Celiac DiseaseDocument9 pagesThe Present and The Future in The Diagnosis and Management of Celiac Diseaseمودة المنعميNo ratings yet
- Rotavirus Infection Frequency and Risk of Celiac Disease Autoimmunity in Early Childhood. A Longitudinal StudyDocument9 pagesRotavirus Infection Frequency and Risk of Celiac Disease Autoimmunity in Early Childhood. A Longitudinal Studyمودة المنعميNo ratings yet
- Epidemic of Coeliac Disease in Swedish Children.Document7 pagesEpidemic of Coeliac Disease in Swedish Children.مودة المنعميNo ratings yet
- Yoga and Multiple SclerosisDocument6 pagesYoga and Multiple SclerosisTanja TanjićNo ratings yet
- Austin Journal of Cardiovascular Disease and AtherosclerosisDocument33 pagesAustin Journal of Cardiovascular Disease and AtherosclerosisAustin Publishing GroupNo ratings yet
- Emetogenicity Tool PDFDocument2 pagesEmetogenicity Tool PDFKurnia AnharNo ratings yet
- A Community-Based Mothers and Infants CenterDocument10 pagesA Community-Based Mothers and Infants CenterRazonable Morales RommelNo ratings yet
- Guideline, Management of HypoglycemiaDocument5 pagesGuideline, Management of HypoglycemianellieauthorNo ratings yet
- Demi Lovato - Bipolar Disorder - Presentation-1Document9 pagesDemi Lovato - Bipolar Disorder - Presentation-1api-528422127No ratings yet
- 1 PBDocument10 pages1 PBNisha VertianaNo ratings yet
- Paralytic Strabismus ChapterDocument7 pagesParalytic Strabismus ChapterYunita ManurungNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaReza Ridho PahleviNo ratings yet
- Heartworm Disease in DogsDocument5 pagesHeartworm Disease in DogspebawaNo ratings yet
- USMLE STEP 1 Review - StudentDocument81 pagesUSMLE STEP 1 Review - StudentKawther AbdallahNo ratings yet
- Lip LesionsDocument59 pagesLip Lesionspasser by100% (1)
- Nursing Care Plan Name: Group: Group DateDocument5 pagesNursing Care Plan Name: Group: Group DateKen PerezNo ratings yet
- Portal HypertensionDocument41 pagesPortal Hypertensionams_1234100% (2)
- Safety and Infection ControlDocument7 pagesSafety and Infection Controlarcci balinasNo ratings yet
- Dane Sultzer, OD: Condition CPT Codes Imaging/Procedure Codes Consider CommentsDocument1 pageDane Sultzer, OD: Condition CPT Codes Imaging/Procedure Codes Consider CommentsMaharNadirAliNo ratings yet
- Diabetic FootDocument18 pagesDiabetic FootFAMED RESIDENTS CESMEDNo ratings yet
- Arterial Blood Gas Values Case Study 2Document3 pagesArterial Blood Gas Values Case Study 2julissaNo ratings yet
- Arterial Hypertension1Document20 pagesArterial Hypertension1prabhat kumarNo ratings yet
- Nursing Care Plan and Sample OutlineDocument2 pagesNursing Care Plan and Sample Outlinekpop feverNo ratings yet
- N C C N D: Ursing ARE OF Lients With Eurologic IsordersDocument96 pagesN C C N D: Ursing ARE OF Lients With Eurologic IsordersMatt Lao DionelaNo ratings yet
- REVIEWERDocument12 pagesREVIEWERCynde KerrNo ratings yet
- Increased Intracranial PressureDocument16 pagesIncreased Intracranial PressureArleth Fabian Sandoval GómezNo ratings yet
- Alcoholism: Samjhana GautamDocument17 pagesAlcoholism: Samjhana GautamSamjhana GautamNo ratings yet
- Urine Analysis 1429 - RH - FinalDocument3 pagesUrine Analysis 1429 - RH - Finalrjalavazo1989No ratings yet
- Craig2014 PDFDocument10 pagesCraig2014 PDFCristinaNo ratings yet
- List of Diseases and Its Causative AgentDocument46 pagesList of Diseases and Its Causative AgentPʀɩŋcɘss LɩʌNo ratings yet
- Emphysema NCPDocument5 pagesEmphysema NCPAbegail Bautista DoriaNo ratings yet
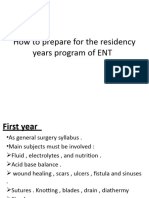
- Syllabus of Ent Residency ProgramJMOHDocument30 pagesSyllabus of Ent Residency ProgramJMOHadham bani younesNo ratings yet
- 3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Document4 pages3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Dr Thushar T.SNo ratings yet