Professional Documents
Culture Documents
Transtubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 Patients
Uploaded by
wilsonwqaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transtubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 Patients
Uploaded by
wilsonwqaCopyright:
Available Formats
CLINICAL ARTICLE
J Neurosurg Spine 37:121–129, 2022
Transtubular image-guided surgery for spinal intradural
lesions: techniques, results, and complications in a
consecutive series of 60 patients
John Michael Duff, MD,1 Patrick Omoumi, MD, MSc, PhD,2 Lukas Bobinski, MD, PhD,3
Amani Belouaer, MD,4 Sonia Plaza Wuthrich, PhD,5 Fabio Zanchi, MD,2 and Rodolfo Maduri, MD1
1
Avaton Surgical Group, Genolier Spine Care Center, Clinique de Genolier, Genolier, Switzerland; 2Department of
Radiodiagnostic and Interventional Radiology, Lausanne University Hospital, Lausanne, Switzerland; 3Department of
Orthopedics, University Hospital, Umëa, Sweden; 4Neurosurgical Service, Department of Clinical Neurosciences, Lausanne
University Hospital, Lausanne, Switzerland; and 5Centre Leenaards de la Memoire, Lausanne University Hospital, Lausanne,
Switzerland
OBJECTIVE The authors previously described the image merge tailored access resection (IMTAR) technique for resec-
tion of spinal intradural lesions (SIDLs). The authors reported their updated experience with the IMTAR technique and
compared surgical results between patients who underwent operations with 2D or 3D fluoroscopic guidance.
METHODS The authors reviewed 60 patients who underwent SIDL resection with transtubular techniques over a
14-year period. The earlier patients in the series underwent operations with 2D fluoroscopic image guidance. The latter
patients underwent operations with the IMTAR technique based on 3D image guidance. The results of both techniques
were analyzed.
RESULTS Sixty patients were included: 27 females (45%) and 33 males (55%). The median (range) age was 50.5
(19–92) years. Gross-total resection (GTR) was achieved in 52 patients (86.7%). Subtotal resection was accomplished
in 5 patients (8.3%). Neurological complications occurred in 3 patients (5%), and tumor recurrence occurred in 1 patient
(1.7%). The non-IMTAR and IMTAR cohorts showed similar postoperative Nurick scale scores and rates of neurologi-
cal complications and GTR. The median (interquartile range) bone resection surface area at the index level was 89.5
(51–147) mm2 in the non-IMTAR cohort and 35.5 (11–71) mm2 in the IMTAR cohort, with a statistically significant differ-
ence (p = 0.0112).
CONCLUSIONS Surgery for SIDLs may be challenging, and meticulous surgical planning is crucial to optimize tumor
access, maximize resection, and minimize risk of complications. Image-guided transtubular resection is an additional
surgical technique for SIDLs and facilitates microsurgical tumor removal of ventrally located lesions with a posterolateral
approach, without requiring potentially destabilizing bone resection.
https://thejns.org/doi/abs/10.3171/2021.10.SPINE211168
KEYWORDS intradural extramedullary spinal cord neoplasms; neuronavigation; minimally invasive surgical
procedures; minimal access surgical procedures; fluoroscopy; surgical technique
S
pinal intradural lesions (SIDLs) are uncommon of the lesion and therefore requires spinal cord manipula-
neoplastic lesions with an incidence of 0.3–10 per tion with increased risk of neurological complications.4,5
100,000 persons.1 The standard treatment for symp- Minimal access and tubular techniques have been de-
tomatic SIDLs is resection with a midline translaminar scribed to reduce soft-tissue morbidity in patients who un-
approach.2,3 This approach enables excellent surgical ac- dergo SIDL resection and to improve the angle of access
cess of SIDLs in the lumbosacral spine below the conus to the lesions.6–9 Studies that compared open surgical tech-
medullaris. For SIDLs located ventral or ventrolateral to niques with minimal access/transtubular techniques for
the spinal cord and above the level of the conus medul- SIDL have shown comparable rates of lesion resection and
laris, a translaminar approach provides limited exposure complications, with the latter techniques associated with
ABBREVIATIONS GTR = gross-total resection; IMTAR = image merge tailored access resection; IQR = interquartile range; MIS = minimally invasive surgery; OSAT =
optimal surgical access trajectory; SIDL = spinal intradural lesion; STR = subtotal resection.
SUBMITTED September 1, 2021. ACCEPTED October 26, 2021.
INCLUDE WHEN CITING Published online January 14, 2022; DOI: 10.3171/2021.10.SPINE211168.
©AANS 2022, except where prohibited by US copyright law J Neurosurg Spine Volume 37 • July 2022 121
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
decreased intraoperative blood loss and length of hospital spective observational parts. Some of the results of the pro-
stay.9,10 spective observational cohort were previously published.7
Since 2004, we have treated patients with SIDL with The study objective was to compare clinical results, sur-
transtubular approaches, initially using 2D fluoroscopic gical complications, and amounts of bone resection and
image guidance and subsequently 3D fluoroscopic image lesion removal between groups of patients with SIDL who
guidance. This has reduced soft-tissue morbidity due to underwent the two imaging techniques. The key inclusion
the approach while allowing standard microsurgical tu- criteria were age ≥ 18 years, consent of the patient, and
mor resection. The 2D image-guided technique relies on SIDL that was treated with a transtubular technique (for
laterally imaged vertebral bone anatomy for tumor lo- both the retrospective and prospective cohorts). The key
calization and tubular placement. The 3D image-guided exclusion criteria were spine lesion treated with any other
technique adds several layers of image guidance precision, surgical technique, concomitant medical illness that could
while still allowing standard microsurgical resection and have interfered with outcome assessment and follow-up,
perhaps enhancing quality of resection. Even if fluoro- and foreseeable difficulties in follow-up (e.g., geographic
scopic imaging–guided navigation helps to place the tubu- distance).
lar retractor during minimal access surgery,7 fluoroscopic Patient variables included age, sex, Nurick scale score,11
3D imaging alone does not permit visualization of lesions. and presence of neurological deficits such as motor or sen-
Thus, the surgical trajectory, bone resection, and lesion sory deficit and dysesthesia. These variables were assessed
exposure are planned on the basis of only bone landmarks preoperatively; postoperatively at 3, 6, and 12 months; and
with the inherent limitations associated with this tech- annually thereafter. T1-weighted MRI, T1-weighted MRI
nique, including poor visualization of certain anatomical with gadolinium enhancement, and T2-weighted MRI
zones such as the cervicothoracic junction and in some were performed preoperatively and then at every follow-
patients with a larger body habitus. up evaluation.
We developed a technique that superimposes or merges For patients who underwent operations with the IMTAR
preoperative MR images with intraoperatively obtained technique, preoperative MRI (Medtronic Navigation,
3D fluoroscopically images, so the MR images of the tar- Inc.) was performed with the following parameters: im-
get lesion and spinal cord can be seen on the workstation age thickness 1–2 mm; images included half the vertebra
for the 3D fluoroscopic images. This is the basis of the im- above and below the region of interest; and acquisition of
age merge tailored access resection (IMTAR) technique.7 the sacrum included both sciatic notches. The radiological
In the present study, we have reported the surgical results variables were lesion position in relation to the dura mater
of our patients with SIDL who underwent operations with and spinal cord (extradural, intradural extramedullary, or
non-IMTAR and IMTAR techniques. The aim of this intradural intramedullary), and lesion position in the spi-
study was to show that both techniques are safe and reli- nal canal in relation to the spinal cord (ventral, dorsal, and
able, as well as to compare the outcomes of the IMTAR lateral [left or right]). For analytical and descriptive pur-
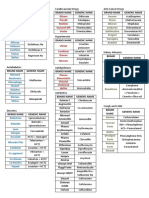
technique such as bone resection area and clinical results poses, all tumors were assigned an optimal surgical access
with those of the more readily available 2D fluoroscopic trajectory (OSAT) (Fig. 1). With this classification system,
(non-IMTAR) technique. the horizontal axis was defined as 0° on either side, with
radii every 30°. The vertical axis was assigned a value
Methods of 3. The intervening axes were in numerical sequence,
such that 30° off the midline was 2 (OSAT 2) and 60° off
Study Design the midline was 1 (OSAT 1). Tumors located ventral to
We performed a retrospective analysis of anonymized the spinal cord and cauda equina were assigned negative
data of a consecutive series of patients with SIDL who numbers, and tumors located dorsal to the spinal cord and
were surgically treated between 2004 and 2018 at Lau- cauda equina were assigned positive numbers. With this
sanne University Hospital. A transtubular technique was system, we assigned a number (range −3 to +3) and sign
used to treat all patients. All patients had the same lead to each tumor that most closely described the epicenter of
surgeon (J.M.D.). the tumor relative to the neural elements. The principle
Ethics committee approval was obtained in December was that smaller numbers indicated more difficult surgical
2015 from the Vaud Ethics Committee Board. Prespeci- access. Left and right modifiers were assigned to indicate
fied uniform definitions were used to record variables, and laterality.
data were entered into a secuTrial platform (InterActive The treatment variables were bone resection (partial or
Systems GmbH) at the time of preoperative consultation, total hemilaminectomy, mini extracavitary costotransver-
during the immediate postoperative period, and at the fol- sectomy, facetectomy [defined as none, partial (≤ 70%) or
low-up evaluations. complete (> 70%)]), planned voluntary nerve root sacri-
fice, surgical time (in minutes), blood loss (in milliliters),
Patients and Variables local complications (e.g., CSF leak, wound infection, he-
Patients with SIDL were treated with 2D fluoroscopic matoma), neurological complications (e.g., unanticipated
image guidance between January 1, 2004, and December motor or sensory radicular deficit, dysesthesia, myelopa-
31, 2012. For the remainder of the study period, IMTAR thy according to a worsened Nurick scale score), lesion
was used because intraoperative 3D fluoroscopic imaging resection on the first postoperative T1-weighted MRI scan
became available at our institution. with gadolinium enhancement, bone resection surface
The study comprised retrospective descriptive and pro- area (in square millimeters), lesion surface area (in square
122 J Neurosurg Spine Volume 37 • July 2022
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
3D Fluoroscopic Guidance Technique With IMTAR.
A 10-mm midline incision is made 1 vertebral level be-
low the caudal segment of the tumor, as determined with
manual counting on 2D fluoroscopic images, and the navi-
gation reference frame (NavLock, Medtronic) is attached
to the corresponding spinous process (Fig. 2A).7 3D fluo-
roscopic images are acquired using the O-arm (Medtron-
ic). Then, the 3D images are manually merged with the
preoperative MR images on the Stealth workstation us-
ing Synergy Cranial 2.2 and StealthMerge 1.2 software
(Medtronic) (Fig. 2B).
Specific morphological and anatomical features of
the vertebrae within the field of view are used to ensure
appropriate matching of vertebrae. The accuracy of the
merged superimposed images is verified on the worksta-
tion by manually windowing back and forth between MR
and 3D fluoroscopic images. Windowing is then set at an
intermediate level, where the bone anatomy and tumor
are simultaneously visualized. After registration, track-
able instruments are used to provisionally and visually
FIG. 1. Drawing showing the OSAT classification system. The horizontal
verify navigation accuracy through the small midline
axis is defined as 0° on both sides, with radii every 30°. The vertical axis incision and the exposed spinous process. With virtual
is assigned a value of 3. The intervening axes are described numerically projection, ideal access to the tumor through the canal is
and sequentially at 30° and 60° off the midline. Left and right modifiers chosen on the basis of the relative positions of the tumor
are assigned to indicate laterality. and spinal cord or cauda equina. This virtual trajectory
defines the locations of the skin incision and transmus-
cular corridor. The first of a series of tubular dilatators
is placed adjacent to this transmuscular corridor, and the
millimeters), and ratio between the bone resection and le- pointer is then removed. The transmuscular corridor is
sion surface areas. progressively dilated, and an expandable tubular retractor
is placed along the intended trajectory and docked onto
the vertebral surface overlying the center of the tumor ac-
Surgical Techniques
cess. The position of the retractor is verified using track-
Patient Positioning and Skin Incision able instruments, and expandable retractor blades are
After intubation, patients are placed prone on a Jackson opened to span beyond the upper and lower poles of the
table. A Mayfield head holder is used for patients with cer- tumor.
vical and upper thoracic tumors. Continuous neurophysio-
logical monitoring, with transcranial motor evoked poten- Bone Removal and Tumor Resection
tial and somatosensory evoked potential monitoring and The operating microscope is used during bone resec-
free running electromyography, is used for all patients. tion with a drill, small Kerrison punches, and microcu-
The transtubular technique utilizes a 3-cm paramedian rettes. Care is taken regarding the extent of facet resec-
skin incision centered at a variable distance from the mid- tion to minimize risk of postoperative instability. With
line depending on patient “thickness” and the desired an- the non-IMTAR technique, extent of bone resection is tai-
gle of approach deduced from the preoperative axial MR lored to the needs of each lesion on the basis of bony ana-
images. Subcutaneous tissues are divided using monop- tomical landmarks that are identified preoperatively and
olar cautery, and the underlying fascia is opened in line verified with 2D fluoroscopy intraoperatively. With the
with the skin incision to expose the underlying muscles. IMTAR technique, planned intraoperative neuronaviga-
Deep intramuscular injection of local anesthesia with bu- tion is used to optimize tumor access but avoid excessive
pivacaine (0.5% carbostesin with 1:200,000 adrenaline; bone resection, with the lesion visible on the workstation
AstraZeneca) is administered along the intended trans- (StealthStation, Medtronic Navigation, Inc.). Tumor expo-
muscular trajectory. sure is also verified using navigated instruments prior to
dural opening.
Retractor Placement and Image Guidance Dural opening is performed close to or at the midline,
2D Fluoroscopic Guidance Technique. After fascial and the lateral dural margin is retracted with 5-0 Prolene
opening, the first of a series of tubular dilatators is placed sutures. The arachnoid is opened with drainage of cere-
adjacent to the transmuscular corridor, and the target level brospinal fluid and tacked to the dural margins using mi-
is verified with lateral fluoroscopy. The transmuscular croclips. Standard microsurgical resection of the lesion is
corridor is progressively dilated, and an expandable tubu- then carried out. For the few selected patients with intra-
lar retractor (Metrx Quadrant, Medtronic Sofamor Danek) medullary tumors, myelotomy is performed at either the
is placed along the intended trajectory and docked onto dorsal root entry zone or the point of posterolateral pial
the vertebral surface. contact with the lesion.
J Neurosurg Spine Volume 37 • July 2022 123
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
FIG. 2. A: Intraoperative photograph showing the tubular retractor in place and the reference arch for navigation docked onto the
spinous process. B: Probe’s-eye views, obtained from the navigation suite during planning of the skin incision and the transmus-
cular trajectory, of tumor access based on the virtual projection of the navigation probe (straight purple markers). Images obtained
at the end of manual merging show preoperative MR and intraoperative 3D fluoroscopic data of a right-sided C6–7 meningioma,
with visualization of both the tumor and bone structures. C and D: GTR is shown on sagittal and axial postoperative images of the
same patient described in panel B. Panels A and B are reprinted from Maduri et al. World Neurosurg. 2017;98:594–602.7 © Else-
vier Inc., published with permission.
Dural Closure postoperative CT of the non-IMTAR and IMTAR cohorts
After tumor resection and hemostasis, the dura is (Fig. 3). Multiplanar reconstructions were used to com-
closed from the apices to the center of the dural opening pare measurements between methods. The articular sur-
with two running 5-0 Prolene sutures. A Chitwood Knot faces of the facet joints were measured on the operated
Pusher (Scanlan International) is used to assist with dural side at the target level. Differences in articular surfaces on
closure. Dural sutures are reinforced with DuraSeal (Con- preoperative and postoperative CT scans were then com-
fluent Surgical, Inc.). pared between the non-IMTAR and IMTAR cohorts.
The tubular retractor is removed, and after epidural and
muscle hemostasis, the wound is closed in layers without Statistical Analysis
drainage. All patients underwent 24 hours of postopera- Continuous variables were presented as median (in-
tive bed rest to reduce the risk of postoperative CSF leak. terquartile range [IQR]), and categorical variables were
expressed as number and proportion. Comparisons of
Radiological Assessment Nurick scale scores, rates of complications, and quality
Two radiologists (F.Z. and P.O.), who were blinded to of lesion resection were analyzed with the chi-square test.
the surgical technique, assessed tumor surface area on Change in Nurick scale scores between preoperation and
preoperative 3D MRI and bone resection surface area on postoperation was analyzed with the paired chi-square
124 J Neurosurg Spine Volume 37 • July 2022
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
TABLE 1. Patient population
Characteristic Value
Age, yrs 50.5 (39.5–62.0; 19–92)
Sex
Female 27 (45.0)
Male 33 (55.0)
Clinical presentation
Myelopathy 29 (48.4)
Radicular deficit 21 (35.0)
Dysesthesia 5 (8.3)
Back pain 5 (8.3)
Spinal level
Cervical 11 (18.3)
Thoracic 26 (43.4)
Lumbar 21 (35)
Sacral 2 (3.3)
Values are shown as median (IQR; range) or number (%).
FIG. 3. A: Preoperative 3D T2-weighted MR imaging sequence show-
ing a left-sided C6 schwannoma. The multiplanar reformatted coronal 1.7% had combined intra- and extramedullary lesions (n =
oblique plane used to measure the largest surface area of the tumor (S1) 1). The median (IQR) follow-up was 35 (14–60) months.
is shown. B and C: The sagittal and transverse planes of the tumor, with Surgical details, histological subtypes, and complica-
reference (white lines) to panel A, are shown. D: A 10-mm maximum tions are detailed in Table 2. The transtubular technique
intensity projection image of a postoperative CT scan of the cervical
spine of the same patient is shown, with the bone resection surface area
was used for all patients. Image guidance with 2D fluoros-
(S2 [red circle]) indicated. copy was used for 27 patients, and the IMTAR technique
was used for 33 cases. The median (IQR) surgical time
was 265 (210–300) minutes for the 2D fluoroscopic cohort
and 295 (236–334) minutes for the IMTAR cohort. The
test. Changes in bone resection surface area and articular median (IQR) estimated blood loss was 300 (250–300) ml
surface area were analyzed with the Wilcoxon test. for the 2D fluoroscopic cohort and 200 (100–300) ml for
Confidence intervals for differences in mean values the IMTAR cohort. No statistical differences in surgical
were determined with the noninferiority test for the fol- time and blood loss were found between the two tech-
lowing variables: surgical time, blood loss, bone resec- niques.
tion surface area, tumor surface area, and preoperative Extent of bone resection varied depending on lesion
and postoperative articular surface area at the index level. morphology and location relative to the spinal cord. Par-
The margin of the noninferiority analysis was defined as tial or complete hemilaminectomy was carried out in 54
a 10% difference in mean values. The ratios of bone re- patients (90%). Extracavitary costotransversectomy was
section surface area to tumor surface area were compared performed in 6 patients (10%), all with ventrally located
between the non-IMTAR and IMTAR cohorts with the thoracic lesions.
chi-square test. In this study, p < 0.05 was considered sig- Concerning bone removal at the segmental posterior
nificant. Statistical analyses were performed using Stata articulations, complete facetectomy was carried out in 7
version 15.0 (StataCorp). patients (11.6%) (all with lesions in the thoracic spine),
and partial facetectomy was accomplished in 44 patients
(73.4%). Facetectomy was not necessary in 9 patients
Results (15%). Fusion was not required during follow-up.
The demographic, clinical, and radiological charac- Gross-total resection (GTR) was achieved in 52 patients
teristics of the patient population are outlined in Table 1. (86.8%). Planned subtotal resection (STR) was carried
Of 60 patients, there were 27 females (45%) and 33 males out in 4 patients (6.6%). All these lesions were tumors: 1
(55%). The median (range) age was 50.5 (19–92) years. myxopapillary ependymoma, 1 thoracic meningioma ad-
Clinical presentations included myelopathy in 48.4% of herent to the anterior spinal artery, 1 multifocal anaplastic
patients (n = 29), radicular deficit in 35% (n = 21), dyses- astrocytoma, and 1 extramedullary and intramedullary
thesia in 8.3% (n = 5), and back pain in 8.3% (n = 5). teratoma of which the intramedullary component was
MRI localized the lesions in the following locations: deliberately not resected. The remaining 4 lesions (6.6%)
cervical in 18.3% of patients (n = 11), thoracic in 43.4% (n were arachnoid cysts, for which marsupialization and not
= 26), lumbar in 35% (n = 21), and sacral in 3.3% (n = 2). In GTR was the surgical goal.
total, 91.7% of patients had intradural-extramedullary tu- Intentional nerve root sacrifice was performed to fa-
mors (n = 55), 6.7% had intramedullary tumors (n = 4), and cilitate resection of a nerve sheath tumor in 26 patients
J Neurosurg Spine Volume 37 • July 2022 125
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
TABLE 2. Results and complications TABLE 3. Comparison of the non-IMTAR and IMTAR cohorts
Characteristic Value Variable Non-IMTAR Cohort IMTAR Cohort p Value
Image guidance Surgical time, mins 265 (210–300) 295 (236–334) 0.1064
2D (non-IMTAR) 27 (45.0) Blood loss, ml 300 (250–300) 200 (100–300) 0.1609
3D (IMTAR) 33 (55.0) Nurick scale, grade
Follow-up, mos 35 (14–60) Preop 1 (0–3) 3 (0–3) 0.4354
Nerve root sacrifice 26 (43.3) Postop 0 (0–2) 0 (0–1) 0.3923
Bone resection approach
Values are shown as median (IQR) unless indicated otherwise.
Partial/complete hemilaminectomy 54 (90)
Mini extracavitary costotransversectomy 6 (10)
Facetectomy
Complete 7 (11.6) In terms of general medical complications, only 1 pa-
tient (1.7%) presented with transient delirium related to
Partial 44 (73.4)
medications. Neurological complications occurred in 3
None 9 (15) patients (5%). One patient with a C6–7 meningioma had
Lesion removal worsened right triceps weakness that improved at follow-
GTR 52 (86.8) up. Postoperative Horner’s syndrome after resection of an
STR 4 (6.6) extraforaminal C8 root schwannoma occurred in 1 patient,
NA* 4 (6.6) and 1 patient presented with dysesthesias in the distribu-
tion of the right L3 nerve root that were controlled with
Histology
gabapentin at follow-up.
Schwannoma 22 (36.6) Recurrence of an S1 sacral synovial cyst occurred after
Meningioma 19 (31.7) GTR in only 1 patient (1.7%), but without clinical manifes-
Other† 19 (31.7) tations. Comparison of the 2D fluoroscopic group with the
Local complications 5 (8.3) IMTAR group showed no significant differences in terms
CSF leak 1 (1.7) of the rates of GTR and neurological complications (p >
0.05). Furthermore, when we compared lesions with posi-
Wound infection 3 (5.0)
tive OSAT values (dorsal lesions) and those with negative
Subcutaneous hematoma 1 (1.7) OSAT values (ventral lesions) between the 2D fluoroscopic
General medical complications‡ 1 (1.7) and IMTAR groups, no differences were found in terms of
Overall neurological complications 3 (5.0) the rates of complications (p = 0.717) and GTR (p = 0.983).
Postop dysesthesia 1 (1.7) Patients in the non-IMTAR and IMTAR groups had simi-
Lesion recurrence 1 (1.7) lar amounts of blood loss, surgical times, and Nurick scale
scores preoperatively and at follow-up (Table 3).
NA = not applicable. The median (IQR) bone resection surface area at the
Values are shown as number (%) or median (IQR). index level was 89.5 (51–147) mm2 in the non-IMTAR co-
* Three lesions were arachnoid cysts, and GTR was not attempted.
hort and 35.5 (11–71) mm2 in the IMTAR cohort, and this
† Included neurofibroma (n = 4), myxopapillary ependymoma (n = 6),
hemangioblastoma (n = 1), teratoma (n = 1), anaplastic astrocytoma (n = 2),
difference was statistically significant (p = 0.0112) (Table
cavernoma (n = 1), and arachnoid cyst (n = 4). 4). No differences were found between groups in terms of
‡ Included pulmonary embolism, cardiac infarction, and delirium. tumor dimensions and extent of facet resection. At follow-
up, no patient presented with mechanical pain suggestive
of instability.
(43.3%). Among patients who underwent voluntary nerve
root sacrifice, an expected new or worsened sensory deficit Discussion
presented in 4 patients (6.7%) and persisted in 2 patients Minimally invasive surgery (MIS) is defined as a pro-
(3.3%) at last follow-up. Twenty-two of 29 myelopathic pa- cedure that “by virtue of the extent and means of surgical
tients (75.9%) improved postoperatively, but the status of 7 technique results in less collateral tissue damage.”12 Thus,
of 29 patients (24.1%) remained unchanged at last follow- the bedrock of MIS is minimal disruption of soft and osse-
up. Histologically, the majority of SIDLs were schwanno- ous tissue while not compromising extent and/or quality of
mas (22 patients [36.6%]) and meningiomas (19 [31.7%]). decompressive or resective surgery. Since the first develop-
Local complications occurred in 5 patients (8.3%). One ment of MIS techniques for spine surgery, instrumentation
patient (1.7%) with CSF leak required surgical revision of and procedures have improved.13 Since the introduction of
the dural closure. Three patients presented with superficial the operating microscope during midline approaches for
wound infections that were treated with wound care and subperiosteal muscle dissection and hemilaminectomy,
oral antibiotics, and 1 patient presented with a subcutane- muscle-sparing MIS techniques for the spine have used
ous hematoma that resolved spontaneously. In 1 patient, the tubular and expandable retractors to allow serial muscle
wrong level at the cervicothoracic junction was exposed, dilation and a less traumatic approach compared with the
which required extension of the surgical exposure for tu- mini open midline approach.14
mor resection and a subsequently longer operative time. We believe that tubular techniques with and without 3D
126 J Neurosurg Spine Volume 37 • July 2022
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
TABLE 4. Comparison of radiologic measurements between the non-IMTAR and IMTAR cohorts
Variable Non-IMTAR Cohort IMTAR Cohort p Value
Bone resection surface area, mm 2
89.5 (51–147) 35.5 (11–71) 0.0112
Tumor surface area, mm2 226.1 (150.7–357.2) 250.8 (233.5–535.4) 0.4127
Articular surface area at index level, mm2
Preop 96 (81–112) 88 (83–93) 0.55
Postop 81.5 (42.5–147.0) 66 (37–120) 0.575
Values are shown as median (IQR) unless indicated otherwise. Boldface type indicates statistical significance.
fluoroscopy are viable alternatives to traditional laminec- relative to the spinal cord (a higher OSAT classification
tomy for SIDL. Laminectomy has limitations for certain number indicates better surgical accessibility). The preop-
ventrally located lesions at the level of the spinal cord. erative plan was verified intraoperatively with 3D imaging
Studies have reported a link between laminectomy and and neuronavigation and direct visualization of the tumor
increased risk of intraoperative neurological complica- lesion based on the merged MR images.
tions. One study reported a 41.6% overall rate of compli- Our results are in line with those reported by previ-
cations, of which 25% were neurological complications, ous authors, with a GTR rate (86.7%) between 61.5% and
and a 1.5% rate of mortality.4 When we compared patients 100%. The rate of neurological complications in the pres-
with ventrally and dorsally located lesions in our series, ent series was 5%, and the rate of CSF leak was 1.7% (0%–
we found no differences in the rates of complications and 7% in previous series). We found no reports of integrated
tumor removal between the patients who underwent 2D 3D navigation methods for SIDL (other than those report-
fluoroscopic guidance and those who received 3D guid- ed by our group) among previously reported studies on the
ance. This finding suggests that the use of tubular tech- use of paramedian access, tubular retractors, and MIS to
niques, and specifically enhanced flexibility regarding the achieve lesion resection of spinal lesions (Table 5).8,10,15–21
angle of approach trajectory, may reduce the complication Reduced approach-related morbidity in terms of bone
rate without compromising tumor removal. Our series removal is an additional advantage. The senior surgeon
showed a significant reduction in bone removal with the had significant experience with transtubular tumor resec-
3D IMTAR technique compared with that achieved with tion without image guidance, but it was possible to refine
2D fluoroscopic image guidance, without compromised and reduce bone resection even further with image guid-
extent of tumor resection and without increased rates of ance. The use of such techniques is also helpful for ju-
neurological complications or CSF fistulae. Regarding nior spine surgeons because use of navigation-guided tube
tumor location as a risk factor (i.e., OSAT classification), placement and bone resection avoids unnecessary bone
we were unable to show a difference between ventral and removal. Studies in the literature provide evidence of cor-
dorsal lesions in terms of the GTR and complication rates, relations between amount of bone resection and risk of
thus supporting the added value of MIS techniques for the subsequent deformity and instability after spinal intradu-
resection of ventrally located intradural spinal tumors. ral resection.22 Use of MIS techniques for intradural tumor
Tubular techniques add flexibility to the approach tra- removal permits the surgeon to tailor exposure while lim-
jectory, perhaps allowing for an easier and possibly safer iting unnecessary bone removal and thus diminishing the
microsurgical resection. We used the OSAT classification risk of postoperative instability.
system to help us define the ideal approach trajectory to The use of MIS techniques for spinal intradural lesions
the spinal lesions on the basis of their precise locations has technical challenges and limitations. The learning
TABLE 5. Findings of the literature review of minimally invasive intradural tumor series
Total No. Paramedian Tubular Retractors Intraop Image GTR Neurological CSF Leak
Authors & Year of Cases Access for Muscular Dilation Guidance (%) Complications (%) (%)
Mannion et al., 201121 13 Yes Yes No 92.3 0 0
Haji et al., 201120 22 Yes Yes No 77.2 5 5
Nzokou et al., 20138 13 Yes Yes No 90 0 0
Wong et al., 201510 27 Yes Yes No 92.5 0 3.7
Afathi et al., 201518 18 Yes Yes No 100 0 0
Formo et al., 201817 83 Yes Variable No 87 4.9 2.4
Thavara et al., 201916 13 Yes Yes No 61.5 0 7.6
Soriano Sánchez et al., 202015 13 Yes Yes No 84.6 0 0
Present study 60 Yes Yes Yes 86.7 5.0 1.67
J Neurosurg Spine Volume 37 • July 2022 127
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
curve for tumor resection with MIS is shallow,23 and the Acknowledgments
surgeon needs to master the use of 3D imaging–based nav- This study received funding from the Department of Clinical
igation and microsurgery with tubular retractors in order Neurosciences, Lausanne University Hospital, Lausanne,
to improve their surgical results. In our series, the opera- Switzerland.
tive times for the conventional 2D fluoroscopic technique
and the 3D navigated technique for tumor resection with References
MIS were similar, thus showing that the additional steps of
1. Kurland LT. The frequency of intracranial and intraspinal
the IMTAR technique did not prolong surgery. neoplasms in the resident population of Rochester, Minne-
Although theoretically MIS techniques may be used to sota. J Neurosurg. 1958;15(6):627-641.
treat patients with any subtype of spinal intradural tumor, 2. Chiou SM, Eggert HR, Laborde G, Seeger W. Microsurgical
there are some limitations.14 Better access to lesions that unilateral approaches for spinal tumour surgery:eight years’
extend over 3 or more vertebrae and require extensive sur- experience in 256 primary operated patients. Acta Neurochir
gical exposure may be obtained with an open surgical ap- (Wien). 1989;100(3-4):127-133.
proach. Rarely, excessive bone removal may require spine 3. Yaşargil MG, Tranmer BI, Adamson TE, Roth P. Unilateral
partial hemi-laminectomy for the removal of extra- and intra-
fixation. The availability of image guidance and specific medullary tumours and AVMs. Adv Tech Stand Neurosurg.
MRI sequences is a technical limitation, particularly for 1991;18:113-132.
the IMTAR technique. Furthermore, use of the IMTAR 4. Mehta AI, Adogwa O, Karikari IO, et al. Anatomical loca-
technique may be more useful for resection of tumors at tion dictating major surgical complications for intradural
the level of the spinal cord, where open translaminar ap- extramedullary spinal tumors:a 10-year single-institutional
proaches provide limited exposure of ventral and ventro- experience. J Neurosurg Spine. 2013;19(6):701-707.
lateral tumors. 5. Slin’ko EI, Al-Qashqish II. Intradural ventral and ventrolat-
eral tumors of the spinal cord:surgical treatment and results.
In our series, no complications were related to midline Neurosurg Focus. 2004;17(1):ECP2.
placement of the reference frame, and the impact of post- 6. Gandhi RH, German JW. Minimally invasive approach for
operative pain was minimal owing to limited tissue dissec- the treatment of intradural spinal pathology. Neurosurg Fo-
tion. Nevertheless, the patient should receive preoperative cus. 2013;35(2):E5.
counseling regarding the additional aesthetic compromise 7. Maduri R, Bobinski L, Duff JM. Image merge tailored access
related to an additional incision. resection (IMTAR) of spinal intradural tumors. Technical
report of 13 cases. World Neurosurg. 2017;98:594-602.
The present study had some limitations. The retrospec- 8. Nzokou A, Weil AG, Shedid D. Minimally invasive removal
tive nature of the series, with a small number of patients of thoracic and lumbar spinal tumors using a nonexpandable
who underwent operations by the same surgeon, had an tubular retractor. J Neurosurg Spine. 2013;19(6):708-715.
inherent selection bias. It was also difficult to draw final 9. Raygor KP, Than KD, Chou D, Mummaneni PV. Comparison
conclusions regarding potential differences between tech- of minimally invasive transspinous and open approaches for
niques. Furthermore, spinal alignment parameters were thoracolumbar intradural-extramedullary spinal tumors. Neu-
not radiologically measured. Even though no patients in rosurg Focus. 2015;39(2):E12.
10. Wong AP, Lall RR, Dahdaleh NS, et al. Comparison of open
our series presented with mechanical back pain or under- and minimally invasive surgery for intradural-extramedul-
went further surgery for progressive postoperative defor- lary spine tumors. Neurosurg Focus. 2015;39(2):E11.
mity, the difference between the IMTAR and non-IMTAR 11. Nurick S. The pathogenesis of the spinal cord disorder
techniques in terms of postoperative deformity remains associated with cervical spondylosis. Brain. 1972;95(1):87-
unknown. 100.
12. McAfee PC, Phillips FM, Andersson G, et al. Minimally
invasive spine surgery. Spine (Phila Pa 1976). 2010;35(26)
Conclusions (suppl):S271-S273.
MIS techniques are viable options for resection of SIDLs. 13. Huang TJ, Kim KT, Nakamura H, Yeung AT, Zeng J. The
The potential incremental gain that may be achieved with state of the art in minimally invasive spine surgery. BioMed
Res Int. 2017;2017:6194016.
the use of these techniques is certainly less in the region 14. Barzilai O, Robin AM, O’Toole JE, Laufer I. Minimally
of the cauda equina. However, as suggested in a previ- invasive surgery strategies:changing the treatment of spine
ously published study,4 we believe that the use of tubular tumors. Neurosurg Clin N Am. 2020;31(2):201-209.
techniques and image guidance may provide an advantage 15. Soriano Sánchez JA, Soto García ME, Soriano Solís S, et al.
for the treatment of ventrally located SIDLs at the level Microsurgical resection of intraspinal benign tumors using
of the spinal cord by reducing unnecessary bone removal, non-expansile tubular access. World Neurosurg. 2020;133:
e97-e104.
optimizing tumor resection, and minimizing spinal cord 16. Thavara BD, Kidangan GS, Rajagopalawarrier B. Analysis
manipulation. Reduced bone removal, specifically mini- of the surgical technique and outcome of the thoracic and
mization of facet joint resection, may decrease the risk of lumbar intradural spinal tumor excision using minimally
iatrogenic instability after SIDL resection. Not only does invasive tubular retractor system. Asian J Neurosurg. 2019;
the flexibility of these techniques allow for microsurgical 14(2):453-460.
resection that is at least equivalent to standard translami- 17. Formo M, Halvorsen CM, Dahlberg D, et al. Minimally
nar approaches, but it may enhance and facilitate resection invasive microsurgical resection of primary, intradural
spinal tumors is feasible and safe:a consecutive series of 83
by allowing a better angle for tumor access. The advan- patients. Neurosurgery. 2018;82(3):365-371.
tages of MIS techniques may become better defined with 18. Afathi M, Peltier E, Adetchessi T, Graillon T, Dufour H,
more widespread availability of the technology and fur- Fuentes S. Minimally invasive transmuscular approach for
ther experience by multiple centers. the treatment of benign intradural extramedullary spinal cord
128 J Neurosurg Spine Volume 37 • July 2022
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
Duff et al.
tumours:technical note and results. Neurochirurgie. 2015; Author Contributions
61(5):333-338. Conception and design: Maduri, Bobinski. Acquisition of data:
19 Kumar N, Malhotra R, Maharajan K, et al. Metastatic spine Maduri, Omoumi, Belouaer, Zanchi. Analysis and interpretation
tumor surgery:a comparative study of minimally invasive of data: Maduri, Omoumi, Belouaer, Plaza Wuthrich. Zanchi.
approach using percutaneous pedicle screws fixation versus Drafting the article: Maduri, Duff, Omoumi, Bobinski, Plaza
open approach. Clin Spine Surg. 2017;30(8):E1015-E1021. Wuthrich, Zanchi. Critically revising the article: Maduri, Duff,
20. Haji FA, Cenic A, Crevier L, Murty N, Reddy K. Minimally Bobinski. Reviewed submitted version of manuscript: Maduri.
invasive approach for the resection of spinal neoplasm. Spine Approved the final version of the manuscript on behalf of all
(Phila Pa 1976). 2011;36(15):E1018-E1026. authors: Maduri. Administrative/technical/material support:
21. Mannion RJ, Nowitzke AM, Efendy J, Wood MJ. Safety and Maduri, Belouaer, Plaza Wuthrich. Study supervision: Maduri,
efficacy of intradural extramedullary spinal tumor removal Duff.
using a minimally invasive approach. Neurosurgery. 2011;
68(1 Suppl Operative):208-216. Supplemental Information
22. Tumialán LM, Theodore N, Narayanan M, Marciano FF,
Nakaji P. Anatomic basis for minimally invasive resection Previous Presentations
of intradural extramedullary lesions in thoracic spine. World The abstract of the paper was presented at the European
Neurosurg. 2018;109:e770-e777. Association of Neurosurgical Societies Congress, Hamburg,
23. Sharif S, Afsar A. Learning curve and minimally invasive Germany, October 4, 2021.
spine surgery. World Neurosurg. 2018;119:472-478.
Correspondence
Rodolfo Maduri: Avaton Surgical Group, Genolier Spine Care
Disclosures Center, Genolier, Switzerland. rodolfo.maduri@gmail.com.
The authors report no conflict of interest concerning the materi-
als or methods used in this study or the findings specified in this
paper.
J Neurosurg Spine Volume 37 • July 2022 129
Brought to you by AOSpine | Unauthenticated | Downloaded 08/02/22 02:13 AM UTC
You might also like
- Self Care Handout-1Document3 pagesSelf Care Handout-1Wandarh RhNo ratings yet
- 50 Famous Proverbs Meaning and ExamplesDocument7 pages50 Famous Proverbs Meaning and ExamplesAnonymous fjFtyLi100% (1)
- ABE 153 Lab Exercise No. 2Document9 pagesABE 153 Lab Exercise No. 2Billy AgustinNo ratings yet
- Community As Partner - Chapter 2Document2 pagesCommunity As Partner - Chapter 2KTNo ratings yet
- Interdisciplinary Neurosurgery: Advanced Techniques and Case ManagementDocument16 pagesInterdisciplinary Neurosurgery: Advanced Techniques and Case ManagementEvelyn JudithNo ratings yet
- 2015 6 jns1546Document7 pages2015 6 jns1546ROHITNo ratings yet
- Minimally Invasive Posterior Cervical Foraminotomy: Microscopic Tubular Assisted (With Technical Tips)Document7 pagesMinimally Invasive Posterior Cervical Foraminotomy: Microscopic Tubular Assisted (With Technical Tips)Nasrullah nsrNo ratings yet
- PIIS000293942200246XDocument8 pagesPIIS000293942200246XIoana ElenaNo ratings yet
- Teo 2010Document7 pagesTeo 2010Sebastian GiovanniniNo ratings yet
- 1536636589472962 - iPhoneDocument8 pages1536636589472962 - iPhonegerrymikepalisocNo ratings yet
- 223654-Article Text-546414-1-10-20220403Document6 pages223654-Article Text-546414-1-10-20220403Christopher Freddy Bermeo RiveraNo ratings yet
- TMP 33 BFDocument6 pagesTMP 33 BFFrontiersNo ratings yet
- Percutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsDocument7 pagesPercutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsAmina GoharyNo ratings yet
- (19330693 - Journal of Neurosurgery) MRI-guided Stereotactic Laser Corpus Callosotomy For Epilepsy: Distinct Methods and OutcomesDocument13 pages(19330693 - Journal of Neurosurgery) MRI-guided Stereotactic Laser Corpus Callosotomy For Epilepsy: Distinct Methods and Outcomeswafaa moNo ratings yet
- Preoperative Close Reduction of Cervical Fracture DislocationsDocument8 pagesPreoperative Close Reduction of Cervical Fracture DislocationsIJAR JOURNALNo ratings yet
- Evaluation of Functional Outcome of Surgical Management of Intra-Articular Calcaneum FractureDocument23 pagesEvaluation of Functional Outcome of Surgical Management of Intra-Articular Calcaneum FractureInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jandrol 112 016444Document7 pagesJandrol 112 016444Павел ГичакNo ratings yet
- Effect of Ultrasound Image-Guided Nerve BlockDocument9 pagesEffect of Ultrasound Image-Guided Nerve BlockMarce SiuNo ratings yet
- Treatment of Condylar Fractures With An Intraoral ApproachDocument26 pagesTreatment of Condylar Fractures With An Intraoral Approachdhiraj.2367No ratings yet
- Phacoemulsification Versus Small Incision Cataract Surgery in Patients With UveitisDocument6 pagesPhacoemulsification Versus Small Incision Cataract Surgery in Patients With UveitisYahya Iryianto ButarbutarNo ratings yet
- Comparison of MISS and limbal techniquesDocument7 pagesComparison of MISS and limbal techniquesvikrizkaNo ratings yet
- Phacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearDocument6 pagesPhacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearRagni MishraNo ratings yet
- Jcen 22 2 78Document7 pagesJcen 22 2 78Aik NoeraNo ratings yet
- Magnesium AbstractDocument1 pageMagnesium Abstracthkw8g5snyxNo ratings yet
- Research Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryDocument8 pagesResearch Article: The Effect of Parkinson's Disease On Patients Undergoing Lumbar Spine SurgeryMelanie Arabsky LedgerNo ratings yet
- Retrospective Study of Craniovertebral Junction (CVJ) Anomalies: A Clinical Profi Le and Outcome Analysis of Surgically Treated PatientsDocument7 pagesRetrospective Study of Craniovertebral Junction (CVJ) Anomalies: A Clinical Profi Le and Outcome Analysis of Surgically Treated PatientsNaga MuthuNo ratings yet
- (10920684 - Neurosurgical Focus) Surgery For Clival Lesions - Open Resection Versus The Expanded Endoscopic Endonasal ApproachDocument8 pages(10920684 - Neurosurgical Focus) Surgery For Clival Lesions - Open Resection Versus The Expanded Endoscopic Endonasal ApproachAleksandar DimovskiNo ratings yet
- Legnani 2013Document6 pagesLegnani 2013wedawisnawaNo ratings yet
- CBCT Article SandyDocument9 pagesCBCT Article Sandysandeep lachhwaniNo ratings yet
- Literature Review Endoscopic Techniques For Spinal Oncology: A SystematicDocument8 pagesLiterature Review Endoscopic Techniques For Spinal Oncology: A SystematicAhana MukherjeeNo ratings yet
- (10920684 - Neurosurgical Focus) Petroclival Meningiomas - An Update On Surgical Approaches, Decision Making, and Treatment ResultsDocument10 pages(10920684 - Neurosurgical Focus) Petroclival Meningiomas - An Update On Surgical Approaches, Decision Making, and Treatment ResultsDr MorellNo ratings yet
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocument9 pagesLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNo ratings yet
- Fraktur FrakDocument11 pagesFraktur FrakRirin SeptianiNo ratings yet
- Spine Minimally Invasive Spine Surgery Historical PerspectivesDocument10 pagesSpine Minimally Invasive Spine Surgery Historical PerspectivesNoura RoseNo ratings yet
- Measurement of Tip Apex Distance and Its Relation With Cut-Out After Fixation of Proximal Femoral Fractures With Dynamic Hip Screw or Proximal Femoral Nail a Retrospective Longitudinal Analysis of 106 PatientsDocument4 pagesMeasurement of Tip Apex Distance and Its Relation With Cut-Out After Fixation of Proximal Femoral Fractures With Dynamic Hip Screw or Proximal Femoral Nail a Retrospective Longitudinal Analysis of 106 PatientsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- J Wneu 2010 08 021Document9 pagesJ Wneu 2010 08 021Boukhenoufa Mouhammed ElamineNo ratings yet
- Sebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfDocument9 pagesSebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfKaustubh KeskarNo ratings yet
- Precontoured Locking CompressiDocument8 pagesPrecontoured Locking CompressiPrincess BabyNo ratings yet
- Locking Plate Fixation of Three-And Four-Part Proximal Humeral FracturesDocument8 pagesLocking Plate Fixation of Three-And Four-Part Proximal Humeral FracturesrezaaamuhammadNo ratings yet
- Delta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesDocument4 pagesDelta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Indications, Surgical Approach, Reduction, and Stabilization Techniques of Distal Radius FracturesDocument11 pagesIndications, Surgical Approach, Reduction, and Stabilization Techniques of Distal Radius FracturesSylvinho46No ratings yet
- Analysis of Surgical Management of Proximal Humeral FracturesDocument5 pagesAnalysis of Surgical Management of Proximal Humeral FracturesRhizka djitmauNo ratings yet
- International Journal of Surgery Case ReportsDocument5 pagesInternational Journal of Surgery Case Reportscarlos javier andraadeNo ratings yet
- QolDocument8 pagesQolanviNo ratings yet
- Automatic Tool Segmentation and Tracking During Robotic Intravascular Catheterization For Cardiac InterventionsDocument23 pagesAutomatic Tool Segmentation and Tracking During Robotic Intravascular Catheterization For Cardiac InterventionsNishant UzirNo ratings yet
- 08 Subasi NecmiogluDocument7 pages08 Subasi Necmiogludoos1No ratings yet
- Diffusion Tensor Imaging, Intra-Operative Neurophysiological Monitoring and Small Craniotomy: Results in A Consecutive Series of 103 GliomasDocument11 pagesDiffusion Tensor Imaging, Intra-Operative Neurophysiological Monitoring and Small Craniotomy: Results in A Consecutive Series of 103 GliomasGeneration GenerationNo ratings yet
- EJMCM Volume 9 Issue 6 Pages 2361-2368Document8 pagesEJMCM Volume 9 Issue 6 Pages 2361-2368ManikyaRameshNo ratings yet
- Complications of Posterior Cranial Fossa PDFDocument7 pagesComplications of Posterior Cranial Fossa PDFemilio9fernandez9gatNo ratings yet
- Menegozzo2020 Article PopInAScopeAttemptToDecreaseThDocument7 pagesMenegozzo2020 Article PopInAScopeAttemptToDecreaseThlaviniaNo ratings yet
- 4 03000605221103974Document13 pages4 03000605221103974Teuku FadhliNo ratings yet
- 10 1 1 525 6842Document6 pages10 1 1 525 6842sandyNo ratings yet
- Fneur 12 724811Document6 pagesFneur 12 724811JEAN GEMNo ratings yet
- Guidelines Endoscopic Spine SurgeryDocument11 pagesGuidelines Endoscopic Spine SurgerynhieuntnNo ratings yet
- Stabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternDocument5 pagesStabilization of Distal Humerus Fractures by Precontoured Bi-Condylar Plating in A 90-90 PatternmayNo ratings yet
- Trans-Subxiphoid Robotic Surgery For Anterior Mediastinal DiseaseDocument7 pagesTrans-Subxiphoid Robotic Surgery For Anterior Mediastinal DiseaseFebrian Parlangga MuisNo ratings yet
- Functional Outcome of Displaced Clavicle Fracture Treated by Intramedullary Nailing: A Prospective StudyDocument9 pagesFunctional Outcome of Displaced Clavicle Fracture Treated by Intramedullary Nailing: A Prospective StudyIJAR JOURNALNo ratings yet
- Treatment of Pathological Fractures Due To Simple Bone Cysts by Extended Curettage Grafting and Intramedullary DecompressionDocument9 pagesTreatment of Pathological Fractures Due To Simple Bone Cysts by Extended Curettage Grafting and Intramedullary DecompressionHendra AjahNo ratings yet
- (10920684 - Neurosurgical Focus) Decision-Making Algorithm For Minimally Invasive Approaches To Anterior Skull Base MeningiomasDocument8 pages(10920684 - Neurosurgical Focus) Decision-Making Algorithm For Minimally Invasive Approaches To Anterior Skull Base MeningiomasBedussa NuritNo ratings yet
- Ortog Com AR - RaffainiDocument7 pagesOrtog Com AR - RaffainiÂngelo Rosso LlantadaNo ratings yet
- Functiuonal Out5come After Sugical Tratment of Ankle Fracture Using Baird Jackon ScoreDocument4 pagesFunctiuonal Out5come After Sugical Tratment of Ankle Fracture Using Baird Jackon ScoreAxell C MtzNo ratings yet
- Kim 2014Document6 pagesKim 2014anviNo ratings yet
- Badie 2004Document11 pagesBadie 2004Bhayu Rizallinoor BhayuNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Spinal Deformity Surgery A Critical Review of Alignment and BalanceDocument9 pagesSpinal Deformity Surgery A Critical Review of Alignment and BalancewilsonwqaNo ratings yet
- Repair Nobel DuralDocument6 pagesRepair Nobel DuralwilsonwqaNo ratings yet
- Dural Tear Repair Surgery Comparative Analysis A Stitch in Time SavesDocument21 pagesDural Tear Repair Surgery Comparative Analysis A Stitch in Time SaveswilsonwqaNo ratings yet
- (Journal of Neurosurgery - Spine) Effects of The Difference Between Lumbar Lordosis in The Supine and Standing Positions On The Clinical Outcomes of Decompression Surgery For Lumbar Spinal StenosisDocument7 pages(Journal of Neurosurgery - Spine) Effects of The Difference Between Lumbar Lordosis in The Supine and Standing Positions On The Clinical Outcomes of Decompression Surgery For Lumbar Spinal StenosiswilsonwqaNo ratings yet
- A novel radiographic classification of severe spinal curvatures exceeding 100° the Omega (Ω), gamma (γ) and alpha (α) deformities - Karikari et al. 2019Document12 pagesA novel radiographic classification of severe spinal curvatures exceeding 100° the Omega (Ω), gamma (γ) and alpha (α) deformities - Karikari et al. 2019Mohammad KaramNo ratings yet
- Final Molecular BiologyDocument8 pagesFinal Molecular Biologyrachyb7100% (1)
- 210-241 UrinaryDocument34 pages210-241 UrinaryYaj Cruzada100% (1)
- Cambridge International AS & A Level: BIOLOGY 9700/21Document20 pagesCambridge International AS & A Level: BIOLOGY 9700/21jamalNo ratings yet
- CDC 2017 0019 0010 - ContentDocument156 pagesCDC 2017 0019 0010 - ContentTrey Martin-EllisNo ratings yet
- FORM I-601 Waiver Application USDocument9 pagesFORM I-601 Waiver Application USChaudhry WathraNo ratings yet
- NCM 109 (ECG and Cardiac Monitoring)Document7 pagesNCM 109 (ECG and Cardiac Monitoring)Kyla BungayNo ratings yet
- Pyloric StenosisDocument14 pagesPyloric Stenosisgangguan hepatobilierNo ratings yet
- Final Concept MapDocument7 pagesFinal Concept Mapapi-405374041No ratings yet
- Festivals and The EnvironmentDocument20 pagesFestivals and The EnvironmentSohel Bangi75% (4)
- St. Paul University PhilippinesDocument4 pagesSt. Paul University PhilippinesAshley DayagNo ratings yet
- BrightDocument279 pagesBrightfernando100% (1)
- Thyroid Gland Resection Causes Appetite LossDocument14 pagesThyroid Gland Resection Causes Appetite LossRodriguez Vivanco Kevin DanielNo ratings yet
- NCP - LeprosyDocument3 pagesNCP - LeprosyKevin DareNo ratings yet
- Colds and Their BenefitsDocument105 pagesColds and Their BenefitsAlmiranteAckbarNo ratings yet
- Documentation On Medicinal Plants Sold I PDFDocument9 pagesDocumentation On Medicinal Plants Sold I PDFGbadeyanka O WuraolaNo ratings yet
- Description of The StrategyDocument6 pagesDescription of The Strategyiulia9gavrisNo ratings yet
- Cardiovascular Exam GuideDocument4 pagesCardiovascular Exam GuidearchanaNo ratings yet
- AdhdDocument7 pagesAdhdAnca CzifraNo ratings yet
- Diabetic Living - Summer 2016Document108 pagesDiabetic Living - Summer 2016Lohrasp Suraliwala100% (2)
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Z-03 Digest Part EVDocument50 pagesZ-03 Digest Part EVXaveer AzadNo ratings yet
- MSDS Buffer PH10Document6 pagesMSDS Buffer PH10Ardhy LazuardyNo ratings yet
- English For Science and Technology - Paper 2Document11 pagesEnglish For Science and Technology - Paper 2Alaister Bernard JampongNo ratings yet
- DelusionsDocument8 pagesDelusionsvenkyreddy97No ratings yet
- Healing Through Loss and GriefDocument3 pagesHealing Through Loss and Griefjackieob123No ratings yet
- Session 5 - Performing Cardiovascular System ExaminationDocument22 pagesSession 5 - Performing Cardiovascular System ExaminationOtsward OwdenNo ratings yet