Professional Documents
Culture Documents
Literature Review Endoscopic Techniques For Spinal Oncology: A Systematic
Uploaded by
Ahana MukherjeeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Literature Review Endoscopic Techniques For Spinal Oncology: A Systematic
Uploaded by
Ahana MukherjeeCopyright:
Available Formats
Endoscopic Techniques for Spinal Oncology: A Systematic
Literature Review
Rohaid Ali, Matthew J. Hagan, Elias Shaaya, Owen P. Leary, Joshua Feler, Ankush Bajaj, Ziya
Gokaslan, Sanjay Konakondla, Mark A. Mahan, Ralf Wagner, Kai-Uwe Lewandrowski and Albert
E. Telfeian
Int J Spine Surg 2023, 17 (3) 343-349
doi: https://doi.org/10.14444/8412
http://ijssurgery.com/content/17/3/343
This information is current as of March 15, 2024.
Email Alerts Receive free email-alerts when new articles cite this article. Sign up at:
http://ijssurgery.com/alerts
The International Journal of Spine Surgery
2397 Waterbury Circle, Suite 1,
Aurora, IL 60504, Phone: +1-630-375-1432
© 2023 ISASS. All Rights Reserved.
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
International Journal of Spine Surgery, Vol. 17, No. 3, 2022, pp. 343–349
https://doi.org/10.14444/8412
© International Society for the Advancement of Spine Surgery
Endoscopic Techniques for Spinal Oncology:
A Systematic Literature Review
ROHAID ALI, MD1,2; MATTHEW J. HAGAN, BS1; ELIAS SHAAYA, MD1,2; OWEN P. LEARY, BS1,2; JOSHUA FELER,
MD1,2; ANKUSH BAJAJ, BS1; ZIYA GOKASLAN, MD1,2; SANJAY KONAKONDLA, MD3; MARK A. MAHAN, MD4;
RALF WAGNER, MD5; KAI-UWE LEWANDROWSKI, MD6; AND ALBERT E. TELFEIAN, MD, PʜD1,2
1
Warren Alpert School of Medicine of Brown University, Providence, RI, USA; 2Department of Neurosurgery, Warren Alpert School of Medicine of Brown University,
Providence, RI, USA; 3Geisinger, 100 North Academy Ave. Danville, PA, USA; 4University of Utah, Salt Lake City, UT, USA; 5Ligamenta Spine Center, Frankfurt am
Main, Germany; 6Center for Advanced Spine Care of Southern Arizona, The Surgical Institute of Tucson, Tucson, AZ, USA
ABSTRACT
Background: Due to its ultraminimally invasive nature, endoscopic spinal surgery is an attractive tool in spinal oncologic
care. To date, there has been no comprehensive review of this topic. The authors therefore present a thorough search of the
medical literature on endoscopic techniques for spinal oncology.
Methods: A systematic review using PubMed was conducted using the following keywords: endoscopic spine surgery,
spinal oncology, and spinal tumors.
Results: Collectively, 19 cases described endoscopic spine surgery for spinal oncologic care. Endoscopic spine surgery
has been employed for the care of patients with spinal tumors under the following 4 circumstances: (1) to obtain a reliable
tissue diagnosis; (2) to serve as an adjunct during traditional open surgery; (3) to achieve targeted debulking; or (4) to perform
definitive resection. These cases employing endoscopic techniques highlight the versatility of this approach and its utility when
applied to the right patient and with an experienced surgeon.
Conclusions: Our systematic review suggests that, given the right patient and an experienced surgeon, endoscopic spine
surgery should be considered in the armamentarium for spinal oncologic care for both staging and definitive resection.
Clinical Relevance: This systematic literature review showed that endoscopic techniques have been successfully applied
across the spectrum of care in spinal oncology, from diagnosis to definitive treatment.
Endoscopic Minimally Invasive Surgery
Keywords: endoscopic decompression, metastatic lesion, oncologic spine care
INTRODUCTION ultra–minimally invasive nature that allows for less
intensive anesthesia, reduced operative time, minimal
Tumors of the spinal column demand essential con- tissue and bony disruption, less blood loss, and shorter
sideration within the broader oncologic disease land- hospital length of stay and recovery. In this context,
scape. First, tumors of the spinal column are prevalent endoscopic spine surgery represents a promising tool in
among patients with cancer. It is estimated that 60% to spinal oncologic care.7–13 However, despite the promise
70% of patients with metastatic cancer have a metastatic of endoscopic spine surgery for spinal oncologic care,
disease burden to the spinal column.1–4 Second, spinal to our knowledge, there has been no comprehensive
column tumors can be incredibly debilitating. Roughly review on this topic. Therefore, the present article sum-
64% of patients with spinal bone metastasis have motor marizes and discusses published literature on endo-
dysfunction, and 90% have back pain.5 Finally, although scopic spinal oncologic care. Points of discussion will
life expectancy is increasing for patients with tumors of include indications, outcomes, challenges, and the key
the spinal column, these patients overall tend to have elements of a learning curve to be considered when
a limited prognosis.1,6 Thus, any surgical solution that integrating endoscopic protocols into an ongoing onco-
can offer practical and clinically efficacious care with a logic spine care program.
short recovery period would be desirable.
Historically, open surgery for spinal tumors has
been limited by the overall frailty of this patient pop- METHODS
ulation and the considerable recovery period required A PubMed search was conducted in January 2022 for
following such surgeries. Endoscopic spine surgery articles published in the English language between 1990
can potentially circumvent these challenges due to its and 2021 using the following keywords: endoscopic
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
Endoscopic Techniques for Spinal Oncology: A Systematic Literature Review
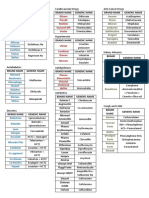
Table. Reports of endoscopic spinal oncology surgery in the literature.
Intervention Authors Patients (n) Additional Information
15
Biopsy Konakondla et al (2020) 1 Large B-cell non-Hodgkin lymphoma
Konakondla et al (2021)14 1 Pediatric; paraganglioma
Adjunct during open surgery McLain (2001)14 9 Thoracic pathology
Debulking Telfeian et al (2015)15 and Telfeian et al (2020)17 4 Resolved radicular pain
Tsai et al (2018)19 1 Sacral metastasis
Gao et al (2019)20 1 Bilateral decompression
Definitive resection Senturk et al (2019)16 1 Meningioma
Newman et al (2020)18 1 Osteoblastoma
spine surgery, percutaneous endoscopic, minimally surgery could augment posterolateral thoracic verte-
invasive spine, transforaminal, spinal oncology, and brectomies for metastatic tumors—adding endoscopic
spinal tumors. Articles that did not employ endoscopic steps during the open debulking facilitated enhanced
techniques were excluded from this literature review. visualization while decreasing manipulation of neural
Articles that incorporated endoscopic procedures and elements. There were shorter operative times and hos-
presented information in a case-based or case series pital length of stays, less blood loss, and improved out-
format were reviewed and included. comes. There were no reported complications in this
case series. While limited by being only a single case
RESULTS series, the report does demonstrate the promise of uti-
lizing an endoscopic technique to augment traditional
The Table summarizes the key findings from this open surgery.
review of the literature. Overall, 242 articles were iden-
tified on initial search, and of these, 9 articles fit the Debulking
inclusion criteria and thus were included in the analy-
sis. Collectively, 19 cases described endoscopic spine A total of 6 cases were found in the literature of
surgery for spinal oncologic care. These interventions endoscopic spine surgery being utilized for debulking
fell under 1 of 4 categories: metastatic tumors to the spinal column.19–21 All but 1 of
these cases occurred in adult patients.19 In the pediatric
1. Biopsy (2 cases) case, the authors palliatively treated a patient with tho-
2. Adjunct during open surgery (9 cases) racic radiculopathy due to a recurrent Ewing-like tumor
3. Debulking (6 cases) ventral to the midthoracic spinal cord.15 The adult cases
4. Definitive resection (2 cases) also highlighted the utility of the endoscopic approach
in alleviating radicular pain due to various metastatic
Biopsy etiologies, including non–small cell lung cancer in the
Two reports of endoscopic biopsies were found in the sacrum, prostate cancer in the lumbar spine, hepatocel-
literature. The first case was reported in a 35-year-old lular carcinoma to the sacrum, and colon cancer to the
man who had a periforaminal lumbar mass with a history lumbar spine. There were no complications seen in any
of stage IV Hodgkin and non-Hodgkin lymphoma.17 He cases. See Figures 1–4 regarding some of these cases.
had undergone a computed tomography (CT)-guided
needle biopsy, but the results of this biopsy were incon- Definitive Resection
clusive. The authors proceeded at that point with an Two cases in the literature demonstrated complete
endoscopic transforaminal approach without complica- resection of a spinal tumor via an endoscopic approach.
tions, and the results were conclusive for non-Hodgkin One case was of a 67-year-old man who presented
lymphoma. The second case was a 12-year-old boy who with a meningioma at the level of L1.22 Under general
presented with a paravertebral thoracic mass. An endo- anesthesia, the tumor was resected via an endoscopic
scopic biopsy completed here without complication approach. The surgeons were able to achieve a gross
revealed a paraganglioma.18 total resection without complication. Another case was
a 45- old woman with a lumbar osteoblastoma
year-
Adjunct During Open Surgery
presenting with lumbar radiculopathy (the lesion was
One case series reported endoscopic spine surgery centered on the L5 superior articulating process).23 The
employed as an adjunct during traditional open surgeons were able to achieve a gross total resection
surgery.5 It described 9 cases of how endoscopic spine with an endoscopic approach. At 6-month follow-up,
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
344 International Journal of Spine Surgery, Vol. 17, No. 3
Ali et al.
Figure 1. Images from a pediatric case of a ventral epidural thoracic Ewing-like tumor. Panels A and B show sagittal and axial T1 postcontrast magnetic resonance
imaging of the thoracic spine with evidence of tumor recurrence in the ventral epidural region. Panels C to F show intraoperative fluoroscopic images. Panel G is
an image from the operating room setup. Panels H and I are intraoperative images of the tumor debulking. Source: Figure reprinted with permission from Telfeian
AE, Choi DB, Aghion DM. Transforaminal endoscopic surgery under local analgesia for ventral epidural thoracic spinal tumor: case report. Clin Neurol Neurosurg.
2015;134:1–3. doi:10.1016/j.clineuro.2015.03.022.
the patient was no longer in any pain, and a magnetic Endoscopic biopsies can be very reliable forms
resonance imaging showed no evidence of residual of tissue sampling. Endoscopic biopsies can be
disease. performed under direct visualization, and signifi-
cant tissue samples can be obtained. Although the 2
DISCUSSION reported cases of endoscopic biopsies differ in terms
of 1 case being pediatric and 1 adult, they share
The literature review shows that endoscopic tech-
common lessons. The adult case highlights the lim-
niques have been applied across the spectrum of
itations of CT-guided needle biopsies, which, owing
care in spinal oncology, from diagnosis to defini-
to the small sample size inherent to biopsies with
tive treatment. The cases demonstrate the versatil-
ity of this approach and its utility when applied to this approach, can often be nondiagnostic. Addition-
the right patient and with an experienced surgeon. ally, the pediatric case highlights how an endoscopic
Furthermore, there were no reported complications procedure can facilitate reduced radiation exposure
in the literature. The following areas relevant to compared with a CT-guided approach. Both cases
establishing and mastering the learning curve of an demonstrate how the endoscopic approach mini-
endoscopic spinal oncology protocol are worthy of mizes tissue and bony disruption compared with
discussion. more invasive techniques while still preserving the
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
International Journal of Spine Surgery, Vol. 17, No. 3 345
Endoscopic Techniques for Spinal Oncology: A Systematic Literature Review
Figure 2. Images from the case of a 75-year-old patient with metastatic nonsmall cell lung cancer. Panels A and B show a magnetic resonance imaging
demonstrating a metastatic focus at the left L5-S1 foramen compressing the exiting left L5 nerve. Panels C and D show intraoperative fluoroscopic imaging
localizing this region. Source: Figure reprinted with permission fromTelfeian AE, Oyelese A, Fridley J, Doberstein C, Gokaslan ZL. Endoscopic surgical treatment for
symptomatic spinal metastases in long-term cancer survivors. J Spine Surg. 2020;6(2):372-382. doi:10.21037/jss.2019.10.14.
ability to maintain patient safety, such as perform- quick recovery time permits patients to return more
ing hemostasis under direct visualization. Finally, quickly to an improved quality of life.
patients can be discharged from the hospital quickly Complete resection of spinal column tumors
because of the short recovery period required after an can be very destabilizing and necessitate fusion.
endoscopic biopsy. Because the large tissue samples However, the definitive resection cases demonstrate
obtained from this technique facilitate more accu- that in 2 inherently less stable regions of the spinal
rate diagnoses, definitive treatment can start sooner. column—the thoracolumbar junction and at the L5
Despite having incredibly varied pathologies, superior articulating process—a gross total resec-
the debulking cases collectively share some key tion without the need for instrumented fusion was
insights. Endoscopic spine surgery can be used suc- possible. The cases demonstrate the feasibility of
cessfully to treat radicular pain due to metastatic endoscopic gross complete resection of select spinal
tumors by alleviating the mass effect from these tumors with all of the benefits inherent to this ultra-
tumors compressing nerve roots exiting the spinal minimally invasive approach.
column. This can be achieved in an ambulatory sur- Highly experienced spine surgeons performed
gical setting. Blood loss is minimal in these surgeries these advanced endoscopic cases. As impressive
due to minimal tissue and bony disruption, ability to as the results of these published cases are that it is
perform hemostasis under direct visualization, and essential to consider challenges to endoscopic spine
short operative times. The minimally invasive nature surgery when applied during spinal oncologic care. It
of these surgeries can facilitate faster adjuvant treat- has been well acknowledged that the learning curve
ment (ie, chemoradiotherapy), and the relatively is one of the primary barriers to the broader adoption
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
346 International Journal of Spine Surgery, Vol. 17, No. 3
Ali et al.
Figure 3. Images from the case of a 76-year-old patient with metastatic prostate cancer status after radiation. Panels A to C demonstrate a magnetic resonance
imaging showing a fracture fragment from the L5 superior endplate compressing the traversing L5 nerve root. Panels D to F show intraoperative fluoroscopic
localization, and panel G shows intraoperative tumor debulking. Panel H demonstrates the decompressed traversing L5 nerve root. Source: Figure reprinted with
permission from Telfeian AE, Oyelese A, Fridley J, Doberstein C, Gokaslan ZL. Endoscopic surgical treatment for symptomatic spinal metastases in long-term
cancer survivors. J Spine Surg. 2020;6(2):372-382. doi:10.21037/jss.2019.10.14.
of endoscopic spine surgery.22,24 The problem is tumor boards. Patient selection is paramount with
compounded by the relative rarity of spinal onco- this approach, since achieving the surgical aims may
logic cases compared with degenerative ones and the require spinal column destabilization requiring fixa-
presumed lack of familiarity with these techniques tion. Some hypervascular tumors may present a high
by surgeons and physicians on multidisciplinary bleeding risk, which might need to be addressed via
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
International Journal of Spine Surgery, Vol. 17, No. 3 347
Endoscopic Techniques for Spinal Oncology: A Systematic Literature Review
Figure 4. Images from the case of an 86-year-old patient with metastatic prostate cancer. Panel A shows severe left L3-L4 stenosis on magnetic resonance
imaging (site marked with arrow), and panels B and C demonstrate intraoperative fluoroscopy localizing to the correct level prior to debulking. Source: Figure
reprinted with permission from Telfeian AE, Oyelese A, Fridley J, Doberstein C, Gokaslan ZL. Endoscopic surgical treatment for symptomatic spinal metastases in
long-term cancer survivors. J Spine Surg. 2020;6(2):372-382. doi:10.21037/jss.2019.10.14.
preoperative embolization or more invasive tech- effectively debulk tumors and relieve radicular pain
niques. Additional published cases, including unsuc- as a method of alleviating mass oncologic effects on
cessful ones or ones with complications, would help the spinal neural elements. Finally, as a means to
better define the indications and limitations for the perform complete resection, endoscopic techniques
endoscopy in an oncologic spine care program. may avoid the need to perform an instrumented
fusion. The learning curve is one of the primary bar-
CONCLUSION riers to broader adoption. However, the success of
the cases presented in this review calls for contin-
The 19 cases presented here showcase the feasi- ued efforts to adopt endoscopic techniques in spinal
bility of applying endoscopic techniques to spinal oncologic care.
oncologic care, from biopsy to complete resection.
To perform a biopsy, an endoscopic approach can
obtain a large sample to yield a reliable tissue-based REFERENCES
diagnosis. As an adjunct to traditional open surgery, 1. Wewel JT, O’Toole JE. Epidemiology of spinal cord
endoscopic techniques may facilitate enhanced visu- and column tumors. Neurooncol Pract. 2020;7(Suppl 1):i5–i9.
alization for the surgeon. Endoscopic procedures can doi:10.1093/nop/npaa046
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
348 International Journal of Spine Surgery, Vol. 17, No. 3
Ali et al.
2. Rades D, Stalpers LJA, Veninga T, et al. Evaluation of five World Neurosurgery. 2019;125:S1878-8750(19)30317-1:146–149:.
radiation schedules and prognostic factors for metastatic spinal cord doi:10.1016/j.wneu.2019.01.206
compression. J Clin Oncol. 2005;23(15):3366–3375. doi:10.1200/ 17. Konakondla S, Sofoluke N, Xia J, et al. Transforaminal
JCO.2005.04.754 endoscopic approach for large-sample tumor biopsy using beveled
3. Sutcliffe P, Connock M, Shyangdan D, Court R, Kandala working channel for core technique: a technical note. World Neuro-
NB, Clarke A. A systematic review of evidence on malignant spinal surg. 2020;141:346–351. doi:10.1016/j.wneu.2020.05.096
metastases: natural history and technologies for identifying patients 18. Konakondla S, Nakhla J, Xia J, et al. A novel endoscopic
at high risk of vertebral fracture and spinal cord compression. technique for biopsy and tissue diagnosis for A paraspinal tho-
Health Technol Assess. 2013;17(42):1–274. doi:10.3310/hta17420 racic tumor in A pediatric patient: A case report. Int J Spine Surg.
4. Prasad D, Schiff D. Malignant spinal- cord compres- 2021;14(s4):S66–S70. doi:10.14444/7167
sion. Lancet Oncol. 2005;6(1):15–24. doi:10.1016/S1470- 19. Telfeian AE, Oyelese A, Fridley J, Doberstein C, Gokaslan
2045(04)01709-7 ZL. Endoscopic surgical treatment for symptomatic spinal metasta-
5. Gokaslan ZL, York JE, Walsh GL, et al. Transtho- ses in long-term cancer survivors. J Spine Surg. 2020;6(2):372–382.
racic vertebrectomy for metastatic spinal tumors. J Neurosurg. doi:10.21037/jss.2019.10.14
1998;89(4):599–609. doi:10.3171/jns.1998.89.4.0599 20. Tsai S-H, Wu H-H, Cheng C-Y, Chen C-M. Full endo-
6. Barzilai O, McLaughlin L, Lis E, Yamada Y, Bilsky scopic interlaminar approach for nerve root decompression of sacral
MH, Laufer I. Outcome analysis of surgery for symptomatic metastatic tumor. World Neurosurg. 2018;112:57–63. doi:10.1016/j.
spinal metastases in long- term cancer survivors. J Neurosurg. wneu.2018.01.075
2019;31(2):285–290. doi:10.3171/2019.2.SPINE181306 21. Gao Z, Wu Z, Lin Y, Zhang P. Percutaneous transforami-
7. Telfeian AE, Veeravagu A, Oyelese AA, Gokaslan ZL. nal endoscopic decompression in the treatment of spinal metasta-
A brief history of endoscopic spine surgery. Neurosurg Focus. ses: a case report. Medicine (Baltimore). 2019;98(11):e14819):11:.
2016;40(2):E2. doi:10.3171/2015.11.FOCUS15429 doi:10.1097/MD.0000000000014819
8. Jasper GP, Francisco GM, Telfeian AE. Transforaminal 22. Lewandrowski K-U, Telfeian AE, Hellinger S, et al. Dif-
endoscopic discectomy with foraminoplasty for the treatment ficulties, challenges, and the learning curve of avoiding com-
of spondylolisthesis. Pain Physician. 2014;17(6):E703–E708. plications in lumbar endoscopic spine surgery. Int J Spine Surg.
doi:10.36076/ppj.2014/17/E703 2021;15(suppl 3):S21–S37. doi:10.14444/8161
23. Newman WC, Vaynrub M, Bilsky MH, Laufer I, Barzilai O.
9. Barber SM, Nakhla J, Konakondla S, et al. Outcomes of
Full endoscopic resection of a lumbar osteoblastoma: technical note.
endoscopic discectomy compared with open microdiscectomy
J Neurosurg Spine. 2020::1–4. doi:10.3171/2020.2.SPINE191091
and tubular microdiscectomy for lumbar disc herniations: a meta-
24. Ransom NA, Gollogly S, Lewandrowski KU, Yeung
analysis. J Neurosurg Spine. 2019::1–14. doi:10.3171/2019.6.SP
A. Navigating the learning curve of spinal endoscopy as an
INE19532
established traditionally trained spine surgeon. J Spine Surg.
10. Telfeian AE, Oyelese A, Fridley J, Gokaslan ZL. Trans-
2020;6(Suppl 1):S197–S207. doi:10.21037/jss.2019.10.03
foraminal endoscopic decompression in the setting of lateral
lumbar spondylolisthesis. World Neurosurg. 2018;117:321–325. Funding: The authors received no financial support
doi:10.1016/j.wneu.2018.06.106
11. Jasper GP, Francisco GM, Telfeian AE. A retrospective
for the research, authorship, and/or publication of this
evaluation of the clinical success of transforaminal endoscopic dis- article.
cectomy with foraminotomy in geriatric patients. Pain Physician.
2013;16(3):225–229. doi:10.36076/ppj.2013/16/225 Declaration of Conflicting Interests: The
12. Telfeian AE, Oyelese A, Fridley J, Gokaslan ZL. Trans- authors report no conflicts of interest in this work.
foraminal endoscopic surgical treatment for posterior migration of
polyetheretherketone transforaminal lumbar interbody fusion cage: Ethics Approval: Institutional review board
case series. World Neurosurg. 2021;147:e437–e443. doi:10.1016/j. authorization was not necessary for the present article.
wneu.2020.12.080
13. Sen RD, White-Dzuro G, Ruzevick J, et al. Intra- and peri- Corresponding Author: Dr. Albert E. Telfeian,
operative complications associated with endoscopic spine surgery: a Department of Neurosurgery, Warren Alpert School of
multi-institutional study. World Neurosurg. 2018;120:e1054–e1060. Medicine, Brown University, Rhode Island Hospital,
doi:10.1016/j.wneu.2018.09.009 593 Eddy St, APC 6, Providence, RI 02903, USA; atel-
14. McLain RF. Spinal cord decompression: an endoscop- feian@lifespan.org
ically assisted approach for metastatic tumors. Spinal Cord.
2001;39(9):482–487. doi:10.1038/sj.sc.3101194 Published 28 November 2022
15. Telfeian AE, Choi DB, Aghion DM. Transforaminal endo- This manuscript is generously published free of charge
scopic surgery under local analgesia for ventral epidural thoracic
spinal tumor: case report. Clin Neurol Neurosurg. 2015;134:1–3.
by ISASS, the International Society for the Advance-
doi:10.1016/j.clineuro.2015.03.022 ment of Spine Surgery. Copyright © 2023 ISASS. To
16. Şentürk S, Ünsal ÜÜ. Percutaneous full-endoscopic removal see more or order reprints or permissions, see http://
of lumbar intradural extramedullary tumor via translaminar approach. ijssurgery.com.
Downloaded from http://ijssurgery.com/ by guest on March 15, 2024
International Journal of Spine Surgery, Vol. 17, No. 3 349
You might also like
- Endoscopic Procedures on the SpineFrom EverandEndoscopic Procedures on the SpineJin-Sung KimNo ratings yet
- Thoracic Endoscopic Spine Surgery A ComprehensiveDocument11 pagesThoracic Endoscopic Spine Surgery A Comprehensivesanjay chhawraNo ratings yet
- (Journal of Neurosurgery - Spine) Need For Arthrodesis Following Facetectomy For Spinal Peripheral Nerve Sheath Tumors - An Institutional Experience and Review of The Current LiteratureDocument146 pages(Journal of Neurosurgery - Spine) Need For Arthrodesis Following Facetectomy For Spinal Peripheral Nerve Sheath Tumors - An Institutional Experience and Review of The Current LiteratureMohammed Ali AlviNo ratings yet
- Nerve-Sparing Radical Hysterectomy in Cervical CancerDocument6 pagesNerve-Sparing Radical Hysterectomy in Cervical CancerdenisdeniNo ratings yet
- 1 s2.0 S1028455922000262 MainDocument8 pages1 s2.0 S1028455922000262 MainDanica SavićNo ratings yet
- Ultrasoud Guidance For Lumbar PunctureDocument12 pagesUltrasoud Guidance For Lumbar PunctureDavid Avellaneda TalledoNo ratings yet
- Fsurg 10 1277997Document3 pagesFsurg 10 1277997Abhilash VemulaNo ratings yet
- PIIS1529943021008196Document11 pagesPIIS1529943021008196Juan Carlos del ReyNo ratings yet
- Fonc 09 00597Document13 pagesFonc 09 00597Giann PersonaNo ratings yet
- JCM 10 01853Document16 pagesJCM 10 01853Katrina Mae FajardoNo ratings yet
- Vulva 2023Document25 pagesVulva 2023Zaniru Raúl Marín MartínezNo ratings yet
- Advancements in Upper Gastrointestinal Endoscopic Therapy: A Comprehensive ReviewDocument12 pagesAdvancements in Upper Gastrointestinal Endoscopic Therapy: A Comprehensive ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesDocument11 pagesA Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesJeremyNo ratings yet
- 5550-Article Text-42309-3-10-20220104Document8 pages5550-Article Text-42309-3-10-20220104the OGs. 96No ratings yet
- Efficacy of Minimally Invasive Surgery On Giant Cell Tumor of The Bone: A Systematic ReviewDocument14 pagesEfficacy of Minimally Invasive Surgery On Giant Cell Tumor of The Bone: A Systematic ReviewAnonymous MLXWLzNo ratings yet
- Bacciu 2013Document10 pagesBacciu 2013AshokNo ratings yet
- Surgical Management of Chordoma - A Systematic ReviewDocument17 pagesSurgical Management of Chordoma - A Systematic ReviewHugo JBNo ratings yet
- Endoscopic Endonasal Reconstruction of Anterior Skull Base Defects What Factors Really Affect The OutcomesDocument8 pagesEndoscopic Endonasal Reconstruction of Anterior Skull Base Defects What Factors Really Affect The OutcomesSanooj SeyedNo ratings yet
- 11.1 AP Accuracy of Fine Needle Aspiration Cytology FNAC IDocument7 pages11.1 AP Accuracy of Fine Needle Aspiration Cytology FNAC IdrdivyeshgoswamiNo ratings yet
- 1530 Jul 27Document6 pages1530 Jul 27kelvin amahNo ratings yet
- Advantage and Limitation of Endoscopic SepDocument6 pagesAdvantage and Limitation of Endoscopic SepTareq MohammadNo ratings yet
- Advantages and Limitations of Endoscopic Septoplasty Experience of 120 CasesDocument6 pagesAdvantages and Limitations of Endoscopic Septoplasty Experience of 120 CasesInternational Journal of Innovative Science and Research Technology100% (1)
- Retrospective Study of Craniovertebral Junction (CVJ) Anomalies: A Clinical Profi Le and Outcome Analysis of Surgically Treated PatientsDocument7 pagesRetrospective Study of Craniovertebral Junction (CVJ) Anomalies: A Clinical Profi Le and Outcome Analysis of Surgically Treated PatientsNaga MuthuNo ratings yet
- Identifying Vascular Pathologies or Flow Limitations Important Aspects inDocument4 pagesIdentifying Vascular Pathologies or Flow Limitations Important Aspects inDiana ArevaloNo ratings yet
- Clinical Neurology and Neurosurgery: SciencedirectDocument15 pagesClinical Neurology and Neurosurgery: SciencedirectPedroNo ratings yet
- j-neurosurg-article-p1554Document8 pagesj-neurosurg-article-p1554emuemi556No ratings yet
- HNPDocument10 pagesHNPNico LieNo ratings yet
- 2017 Results of Endoscopically-Assisted Cubital Tunnel Release Without Using Any Specific InstrumentDocument4 pages2017 Results of Endoscopically-Assisted Cubital Tunnel Release Without Using Any Specific InstrumentDimitris RodriguezNo ratings yet
- Transtubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 PatientsDocument9 pagesTranstubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 PatientswilsonwqaNo ratings yet
- Journal Homepage: - : IntroductionDocument7 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Spine Minimally Invasive Spine Surgery Historical PerspectivesDocument10 pagesSpine Minimally Invasive Spine Surgery Historical PerspectivesNoura RoseNo ratings yet
- BJUI Compass - 2020 - Anderson - Subinguinal Orchiectomy A Minimally Invasive Approach To Open SurgeryDocument5 pagesBJUI Compass - 2020 - Anderson - Subinguinal Orchiectomy A Minimally Invasive Approach To Open SurgeryKaroo_123No ratings yet
- CA Endometrio Guia Europea.Document28 pagesCA Endometrio Guia Europea.MartinNo ratings yet
- Abdi Et Al 2023 Operative Treatment of Tarlov Cysts Outcomes and Predictors of Improvement After Surgery a Series of 97Document8 pagesAbdi Et Al 2023 Operative Treatment of Tarlov Cysts Outcomes and Predictors of Improvement After Surgery a Series of 97jabarin.hNo ratings yet
- Flexible CO2 Laser Treatment For Subglottic Stenosis, 2017Document2 pagesFlexible CO2 Laser Treatment For Subglottic Stenosis, 2017Araceli BarreraNo ratings yet
- New Developments in Minimally Invasive Gynecologic OncologyDocument22 pagesNew Developments in Minimally Invasive Gynecologic OncologyDanica SavićNo ratings yet
- Alesina et al., 2021Document9 pagesAlesina et al., 2021NyomantrianaNo ratings yet
- Deutsch 2017Document7 pagesDeutsch 2017Kelly AgudeloNo ratings yet
- Cancers: Opportunities and Limitations of Pelvic Exenteration SurgeryDocument15 pagesCancers: Opportunities and Limitations of Pelvic Exenteration SurgeryFlaviu Ionuț FaurNo ratings yet
- Sebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfDocument9 pagesSebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfKaustubh KeskarNo ratings yet
- Comparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourDocument9 pagesComparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourtasyadelizaNo ratings yet
- Outcome of Primary Repair of Severed (Partial Complete) TendoachillesDocument15 pagesOutcome of Primary Repair of Severed (Partial Complete) TendoachillesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Imagenes de Flujo Humor Acuoso PDFDocument18 pagesImagenes de Flujo Humor Acuoso PDFSussan Tatiana Castro AguilarNo ratings yet
- 1 s2.0 S2405857220300218 MainDocument5 pages1 s2.0 S2405857220300218 MainIkea BalhonNo ratings yet
- 690 FullDocument8 pages690 Fulldanielalexandersinaga.xiiipa2No ratings yet
- Umbilical Hernia: When and How: Raquel A. Maia, Hrishikesh P. Salgaonkar, Davide Lomanto, Lynette LooDocument8 pagesUmbilical Hernia: When and How: Raquel A. Maia, Hrishikesh P. Salgaonkar, Davide Lomanto, Lynette LooZauzaa NabilaNo ratings yet
- Delineation of de Quervain Tenosynovitis in Saudi Arabia and Literature ReviewDocument6 pagesDelineation of de Quervain Tenosynovitis in Saudi Arabia and Literature ReviewIJAR JOURNALNo ratings yet
- Fine Needle Aspiration Cytology Fnac in EvaluationDocument4 pagesFine Needle Aspiration Cytology Fnac in EvaluationHakim naufaldiNo ratings yet
- Paper 37Document5 pagesPaper 37Dr Vineet KumarNo ratings yet
- JNS Role of Electrophysiology in Guiding Near Total Resection For Preservation of Facial Nerve Function in The Surgical Treatment of Large Vestibular SchwannomasDocument8 pagesJNS Role of Electrophysiology in Guiding Near Total Resection For Preservation of Facial Nerve Function in The Surgical Treatment of Large Vestibular SchwannomasAlejandro CheritNo ratings yet
- 17-Potential Medicolegal RisksDocument1 page17-Potential Medicolegal RisksSUSANNo ratings yet
- Curroncol 29 00465Document10 pagesCurroncol 29 00465jongsu kimNo ratings yet
- Articulo - Intubación en Inestabilidad de ColumnaDocument12 pagesArticulo - Intubación en Inestabilidad de ColumnaNFSOTNo ratings yet
- Guidelines Endoscopic Spine SurgeryDocument11 pagesGuidelines Endoscopic Spine SurgerynhieuntnNo ratings yet
- What's New in Spine Surgery: Specialty UpdateDocument11 pagesWhat's New in Spine Surgery: Specialty UpdatePoliceNo ratings yet
- (10920684 - Neurosurgical Focus) Decompression Surgery For Spinal Metastases - A Systematic ReviewDocument35 pages(10920684 - Neurosurgical Focus) Decompression Surgery For Spinal Metastases - A Systematic ReviewsukiyantoNo ratings yet
- Comparative Evaluation of Thyroid Imaging ReportinDocument5 pagesComparative Evaluation of Thyroid Imaging ReportinisahNo ratings yet
- Ying 2016Document7 pagesYing 2016karemiaNo ratings yet
- Evolution of The Surgical Management of Cauda Equina SyndromeDocument13 pagesEvolution of The Surgical Management of Cauda Equina SyndromeAtul JainNo ratings yet
- Anterior Cervical Discectomy and FusionDocument7 pagesAnterior Cervical Discectomy and FusionGeraldine Alvarez ANo ratings yet
- 31576697Document8 pages31576697Ahana MukherjeeNo ratings yet
- 31697365Document9 pages31697365Ahana MukherjeeNo ratings yet
- Role of AI and Digital Pathology For Colorectal Immuno-OncologyDocument9 pagesRole of AI and Digital Pathology For Colorectal Immuno-OncologyAhana MukherjeeNo ratings yet
- 32001530Document10 pages32001530Ahana MukherjeeNo ratings yet
- 31358541Document8 pages31358541Ahana MukherjeeNo ratings yet
- Biomedicines: Virus-Based Immuno-Oncology ModelsDocument16 pagesBiomedicines: Virus-Based Immuno-Oncology ModelsAhana MukherjeeNo ratings yet
- COVID-19: Biologic and Immunosuppressive Therapy in Gastroenterology and HepatologyDocument11 pagesCOVID-19: Biologic and Immunosuppressive Therapy in Gastroenterology and HepatologyAhana MukherjeeNo ratings yet
- A Systematic Review of Time and Resource Use Costs of Subcutaneous Versus Intravenous Administration of Oncology Biologics in A Hospital SettingDocument34 pagesA Systematic Review of Time and Resource Use Costs of Subcutaneous Versus Intravenous Administration of Oncology Biologics in A Hospital SettingAhana MukherjeeNo ratings yet
- A Systematic Review of Patient Education Strategies For Oncology Patients in Low-And Middle-Income CountriesDocument10 pagesA Systematic Review of Patient Education Strategies For Oncology Patients in Low-And Middle-Income CountriesAhana MukherjeeNo ratings yet
- Gastrointestinal PathophysiologyDocument1,643 pagesGastrointestinal PathophysiologyAhana MukherjeeNo ratings yet
- CXCR4 Targeted Theranostics in OncologyDocument12 pagesCXCR4 Targeted Theranostics in OncologyAhana MukherjeeNo ratings yet
- PD-L1 Testing by Immunohistochemistry in Immuno-Oncology: ReviewDocument11 pagesPD-L1 Testing by Immunohistochemistry in Immuno-Oncology: ReviewAhana MukherjeeNo ratings yet
- OB by ManaswiniDocument71 pagesOB by ManaswiniAhana MukherjeeNo ratings yet
- Evolution and Evaluation of A Structured Applied Physics Course For Radiation Oncology and Radiation Physics TraineesDocument8 pagesEvolution and Evaluation of A Structured Applied Physics Course For Radiation Oncology and Radiation Physics TraineesAhana MukherjeeNo ratings yet
- What Is The Future of Impedance Planimetry in Gastroenterology?Document16 pagesWhat Is The Future of Impedance Planimetry in Gastroenterology?Ahana MukherjeeNo ratings yet
- Position Statement: Reco Mme Ndati O NsDocument9 pagesPosition Statement: Reco Mme Ndati O NsAhana MukherjeeNo ratings yet
- The Fear of Gastric Cancer in Patients With Dyspepsia: Challenge in Specialist Care GastroenterologyDocument8 pagesThe Fear of Gastric Cancer in Patients With Dyspepsia: Challenge in Specialist Care GastroenterologyAhana MukherjeeNo ratings yet
- Indian JudiciaryDocument9 pagesIndian JudiciaryAhana MukherjeeNo ratings yet
- POM Module I (Part 2)Document45 pagesPOM Module I (Part 2)Ahana MukherjeeNo ratings yet
- ESP V-Discrete MathematicsDocument12 pagesESP V-Discrete MathematicsAhana MukherjeeNo ratings yet
- British Society of Gastroenterology Position Statement On Serrated Polyps in The Colon and RectumDocument16 pagesBritish Society of Gastroenterology Position Statement On Serrated Polyps in The Colon and RectumAhana MukherjeeNo ratings yet
- Lelm 504Document11 pagesLelm 504Vaibhav Pratap SinghNo ratings yet
- Gastroenterology Clinical Focus High Yield Gi and HepatologyDocument426 pagesGastroenterology Clinical Focus High Yield Gi and HepatologyAhana MukherjeeNo ratings yet
- Lelm 501Document28 pagesLelm 501Ahana MukherjeeNo ratings yet
- SRS +++a+++Document30 pagesSRS +++a+++Ahana MukherjeeNo ratings yet
- ESP V-Programming & Data StructureDocument70 pagesESP V-Programming & Data StructureAhana MukherjeeNo ratings yet
- New Doc 2019-05-08 17.45.34Document18 pagesNew Doc 2019-05-08 17.45.34Ahana MukherjeeNo ratings yet
- CBSE Class 12 English Writing SkillsDocument27 pagesCBSE Class 12 English Writing SkillsAhana MukherjeeNo ratings yet
- Maths Lab BookDocument30 pagesMaths Lab BookAhana MukherjeeNo ratings yet
- Fiitjee AIITS Jee Advanced PaperDocument19 pagesFiitjee AIITS Jee Advanced PaperAhana MukherjeeNo ratings yet
- Understanding ALS: A Case Study of Mr. CooperDocument24 pagesUnderstanding ALS: A Case Study of Mr. CooperJeanessa Delantar QuilisadioNo ratings yet
- Undo It!: How Simple Lifestyle Changes Can Reverse Most Chronic Diseases - Dean Ornish M.D.Document5 pagesUndo It!: How Simple Lifestyle Changes Can Reverse Most Chronic Diseases - Dean Ornish M.D.besahahu7% (15)
- EnucleationDocument6 pagesEnucleationRameez SarwarNo ratings yet
- Dosage Form ExamDocument9 pagesDosage Form ExamsongaNo ratings yet
- Causes, Incidence, and Risk Factors: Hepatitis A Hepatitis C Hepatitis DDocument41 pagesCauses, Incidence, and Risk Factors: Hepatitis A Hepatitis C Hepatitis DAmber ShrivastavaNo ratings yet
- Forensic MCQ (1) - 1Document18 pagesForensic MCQ (1) - 1hassan qureshiNo ratings yet
- Online CatalogueDocument21 pagesOnline CatalogueAsishmukundan AsishNo ratings yet
- THE AGEING BRAIN. P Sachdev PDFDocument359 pagesTHE AGEING BRAIN. P Sachdev PDFAlejandro Israel Garcia EsparzaNo ratings yet
- 1 Choosing An Org Worksheet 2Document4 pages1 Choosing An Org Worksheet 2api-562131193No ratings yet
- Clinical Nutrition in Gerontology: Chronic Renal Disorders of The Dog and CatDocument8 pagesClinical Nutrition in Gerontology: Chronic Renal Disorders of The Dog and CatKhairul Ihsan Pengusaha MudaNo ratings yet
- Trochanteric Bursitis and HomoeopathyDocument5 pagesTrochanteric Bursitis and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Pathology and Physiology Nums McqsDocument68 pagesPathology and Physiology Nums McqsZara100% (1)
- Health Add OnsDocument6 pagesHealth Add OnssureshNo ratings yet
- Diagnosis of Pancreatitis in Dogs and Cats: ReviewDocument14 pagesDiagnosis of Pancreatitis in Dogs and Cats: ReviewMiruna ChiriacNo ratings yet
- Managing corticosteroids and their side effectsDocument6 pagesManaging corticosteroids and their side effectsKrista Madranca CastroNo ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Project BiomaterialsDocument2 pagesProject Biomaterials9782279059No ratings yet
- Book IndentDocument6 pagesBook Indentpushpajachar95No ratings yet
- VN 400 Obstetric Nursing VN 430A Internal Clinical Experience September 2013Document9 pagesVN 400 Obstetric Nursing VN 430A Internal Clinical Experience September 20131sylvialeeNo ratings yet
- Kasus Sistem Endokrin 1Document3 pagesKasus Sistem Endokrin 1lilik kartiniNo ratings yet
- Heartsaver SlidesDocument21 pagesHeartsaver SlidesBelLa EakoiNo ratings yet
- 3.46B1 Blood Worksheet 1Document4 pages3.46B1 Blood Worksheet 1Nakeisha Joseph100% (1)
- Navi Cure - Customer Information Sheet: Product Name What Am I Covered ForDocument12 pagesNavi Cure - Customer Information Sheet: Product Name What Am I Covered ForsandeepfoxNo ratings yet
- B. Natural History of Disease WorksheetDocument3 pagesB. Natural History of Disease WorksheetYahya MoralesNo ratings yet
- Understanding AuditDocument10 pagesUnderstanding AuditSara YehiaNo ratings yet
- Learning TaskDocument4 pagesLearning TaskAngelica GuillermoNo ratings yet
- Aia Plus Booster Insurance PlanDocument25 pagesAia Plus Booster Insurance PlandensnnowNo ratings yet
- Kidney 360 2020 MicrohematuriaDocument7 pagesKidney 360 2020 MicrohematuriaRichardNo ratings yet
- Dr. Tariq Mahmood Sheikh GP-Diploma MRT (ONCOLOGY)Document3 pagesDr. Tariq Mahmood Sheikh GP-Diploma MRT (ONCOLOGY)cdeekyNo ratings yet