Professional Documents
Culture Documents
Diagnostic Imaging Pathways Article
Uploaded by
Indra PrimaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnostic Imaging Pathways Article
Uploaded by
Indra PrimaCopyright:
Available Formats
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Population Covered By The Guidance
This pathway provides guidance on preoperative imaging of adult patients prior to laproscopic
cholecystectomy.
Date reviewed: January 2012
Date of next review: 2017/2018
Published: January 2012
Quick User Guide
Move the mouse cursor over the PINK text boxes inside the flow chart to bring up a pop up box with salient
points.
Clicking on the PINK text box will bring up the full text.
The relative radiation level (RRL) of each imaging investigation is displayed in the pop up box.
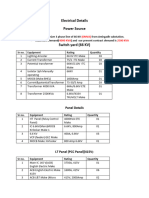
SYMBOL RRL EFFECTIVE DOSE RANGE
None 0
Minimal < 1 millisieverts
Low 1-5 mSv
Medium 5-10 mSv
High >10 mSv
Pathway Diagram
1/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
2/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Image Gallery
Note: These images open in a new page
1 Cholelithiasis
Image 1 (Ultrasound): Calculi in the gallbladder (green crosses).
2 Choledocholithiasis
Image 2 (CT Cholangiogram): Three small filling defects (arrow) are seen
within the common bile duct representing intraductal calculi.
3 Choledocholithiasis
Image 3 (ERCP): Gallstone present in the dilated common bile duct.
4 Choledocholithiasis
Image 4 (MRCP): Gallstone present in the dilated common bile duct (arrow).
5 Acute cholecystitis
Image 5: Cholecystectomy showing acute cholecystitis with gallbladder wall
oedema, vascular congestion and purulent exudate (blue arrow) caused by
a massive cholesterol stone.
6 Acute Cholecystitis
Image 6 (H&E, x2.5): Histological section of severe acute cholecystitis
showing extensive ulceration of the mucosa, haemorrhage, oedema and a
dense transmural infiltrate of neutrophils and mononuclear inflammatory
cells.
3/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Teaching Points
The aim of investigation is to identify and treat patients with common bile duct (CBD) stones prior
to surgery
Low probability of a stone - normal liver function tests (LFTs), normal CBD on ultrasound,
previously abnormal LFTs or past history of pancreatitis
High probability of a stone - cholestatic jaundice, abnormal LFTs, abnormal CBD on trans-
abdominal ultrasound or current episode of pancreatitis
If surgical expertise in laparoscopic cholecystectomy, intra-operative cholangiogram and
laparoscopic stone removal is available proceed directly to this option
Non-invasive methods of evaluation include CT cholangiography, MR cholangiopancreatographyy
and endoscopic US (EUS)
Endoscopic retrograde cholangiopancreatography (ERCP) enables retrieval of CBD stones prior to
surgery
Identifying Patients With Common Bile Duct Stones
The presence of common bile duct stones can be predicted with moderate accuracy by combining
clinical, biochemical and ultrasound features 1,2
Computed Tomography (CT) Cholangiogram
>90% sensitivity and specificity for detection of bile duct stones 25,26,27
Alternative for detection of CBD stones in intermediate risk group, if MRCP or EUS unavailable 25
,26,27
Used by some surgeons, to evaluate aberrant bile ducts before laparoscopic cholecystectomy 28
Disadvantages
Unsuccessful if bilirubin levels are more than twice the upper limit of normal
Potential risk of contrast toxicity
Radiation exposure
Does not offer therapeutic opportunity
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Routine use of ERCP to detect common bile duct stones before laparoscopic cholecystectomy is
not indicated in low risk groups 3,9,11
ERCP is indicated before laparoscopic cholecystectomy in patients in whom there is high clinical
suspicion of choledocholithiasis, based on clinical, biochemical and ultrasonographic criteria 3,10,
11,12,13
Highly accurate in diagnosis and treatment of common bile duct stones (96% success rate for
endoscopic sphincterotomy) 3,10,11,12,14
Limitations - up to 5% complication rate (e.g. pancreatitis), ~0.5-1% mortality rate and ~8%
cannulation failure rate 11,12,13,15
4/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Endoscopic Ultrasound (EUS)
Highly accurate (>95%) for the detection of choledocholithiasis (comparable to ERCP but superior
to CT and US) 3,4,6,7,18,19,20,21,32
No significant difference in diagnostic accuracy compared to MRCP. 32 Consider patient suitability,
availability and local expertise in selecting appropriate modality 33
Comparable sensitivity to that of ERCP for detection of choledocholithiasis 18,19
Can be used to detect common bile duct stones in intermediate risk group who are good surgical
candidates 3,18,22
Not suitable in 19
Severe acute biliary pancreatitis or cholangitis, since it may delay endoscopic treatment
In elderly and high-risk surgical patients because in this population the treatment of choice
is endoscopic sphincterotomy if CBD stones are detected
Limitations
Limited availability
Invasive
Technically impossible in cases of previous gastric surgery
Difficult to interpret following sphincterotomy or previous biliary stenting procedures due to
presence of air in the biliary tract
Does not offer therapeutic opportunity
High Risk Features
Patients with the following clinical, biochemical, or sonographic features are considered at high risk
of having a CBD stone
Cholestatic jaundice
Abnormal liver function tests
Abnormal CBD on US (i.e. dilated ducts, CBD stones)
Current episode of pancreatitis
Low Risk Features
Patients with the following clinical, biochemical, or sonographic features are considered at low risk
of having a CBD stone
Normal liver function tests
Normal CBD on ultrasound
Previously abnormal LFTs and past history of pancreatitis remains low risk
Magnetic Resonance Cholangiopancreatography (MRCP)
Sensitivity of over 84% and specificity of over 90% for the diagnosis of CBD stones, with most false
negative results being for stones less than 5mm in diameter 21,23,24,25,31,32
A meta-analysis of 7 studies showed no statistically significant difference in diagnostic accuracy
between MRCP and EUS for the detection of CBD stones. 32 Consider patient suitability,
availability and local expertise in selecting appropriate modality 33
Advantages
Non-invasive
5/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
No ionising radiation
Allows diagnosis and treatment planning without invasive cholangiography
Limitations
Does not offer therapeutic opportunity
Expensive and limited availability
Less sensitive for stones smaller than 5mm in diameter 31
Ultrasound
Has a sensitivity of 36-75% and specificity of 83-97% for the diagnosis of CBD stones 5,8,16,17,29
,30
Limitations 8
False negative results due to inability to see the extra-hepatic biliary tree (often because of
interposed bowel gas) and absence of biliary dilation in the presence of obstruction
Advantages
Non-invasive and readily available
No ionising radiation
References
References are graded from Level I to V according to the Oxford Centre for Evidence-Based Medicine,
Levels of Evidence. Download the document
1. Abboud PAC, Malet PF, Berlin JA, et al. Predictors of common bile duct stone prior to
cholecystectomy: a meta-analysis. Gastrointest Endosc. 1996;44:450-9. (Level II evidence).
View the reference
2. Kama NA, Atli M, Doganay M, et al. Practical recommendations for the prediction and
management of common bile duct stones in patients with gallstones. Surg Endosc.
2001;15:942-5. (Level II evidence). View the reference
3. Berdah SV, Orsoni P, Bege T, et al. Follow-up of selective endoscopic ultrasonography and/or
endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy: a
prospective study of 300 patients. Endoscopy. 2001;33:216-20. (Level II evidence). View the
reference
4. Canto MI, Chak A, Stellato T, et al. Endoscopic ultrsonography versus cholangiography for
the diagnosis of choledocholithiasis. Gastrointest Endosc. 1998;47:439-48. (Level II/III
evidence)
5. Stott MA, Farrands PA, Guyer PB, et al. Ultrasound of the common bile duct in patients
undergoing cholecystectomy. J Clin Ultrasound. 1991:19:73-6. (Level II/III evidence)
6. Sugiyama M, Atomi Y. Endoscopic Ultrasonography for diagnosing choledocholithiasis: a
prospective comparative study with ultrasonography and computed tomography. Gastrintest
Endosc. 1997;45:143-6. (Level II evidence). View the reference
7. Amouyal P, Amouyal G, Levy P, et al. Diagnosis of choledocholithiasis by endoscopic
ultrasonography. Gastroenterology. 1994;106:1062-7. (Level II/III evidence)
8. Dong B, Chen M. Improved sonographic visualisation of choledocholithiasis. J Clin
Ultrasound. 1987;15:185-90. (Level II/III evidence)
9. Urbach DR, Khajanchee YS, Jobe BA, et al. Cost-effective management of common bile duct
stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography
(ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg
6/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Endosc. 2001;15:4-13. (Level III evidence)
10. Cuschieri A, Lezoche E, Morino M, et al. E.A.E.S multicenter prospective randomized trial
comparing two-stage vs single-stage management of patients with gallstone disease and
ductal calculi. Surg Endosc. 1999;13:952-7. (Level II evidence). View the reference
11. Neuhaus H, Feussner H, Ungeheuer A, et al. Prospective evaluation of the use of endoscopic
retrograde cholangiography prior to laparoscopic cholecystectomy. Endoscopy.
1992;24:745-9. (Level II/III evidence)
12. Rieger R, Wayand W. Yield of prospective, noninvasive evaluation of the common bile duct
combined with selective ERCP/sphincterotomy in 1390 consecutive laparoscopic
cholecystectomy patients. Gastrointest Endosc. 1995;42:6-12. (Level II/III evidence)
13. Rijna H, Borgstein PJ, Meuwissen SGM, et al. Selective preoperative endoscopic retrograde
cholangiopancreatography in laparoscopic biliary surgery. Br J Surg. 1995;82:1130-3. (Level
II/III evidence)
14. Bergamaschi R, tuech JJ, Braconier L, et al. Selective endoscopic retrograde cholangiography
prior to laparoscopic cholecystectomy for gallstones. Am J Surg. 1999;178:46-9. (Level II
evidence). View the reference
15. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary
sphincterotomy. N Engl J Med. 1996;335:909-18. (Level II evidence). View the reference
16. Khandelwal N, Suri S, Malik M, et al. Ultrasound in choledocholithiasis. J Indian Med Assoc.
1991;89:95-7. (Level III evidence)
17. Thornton JR, Lobo AJ, Lintott DJ, Axon AT. Value of ultrasound and liver function tests in
determining the need for endoscopic retrograde cholangiopancreatography in unexplained
abdominal pain. Gut. 1992;33:1559-61. (Level III evidence)
18. Palazzo L, Girollet PP, Salmeron M, et al. Value of endoscopic ultrasonography in the
diagnosis of common bile duct stones: comparison with surgical exploration and ERCP.
Gastrointest Endosc. 1995;42:225-31. (Level II/III evidence)
19. Prat F, Amouyal G, Amouyal P, et al. Prospective controlled study of endoscopic
ultrasonography and endoscopic retrograde cholangiography in patients with suspected
common bile duct lithiasis. Lancet. 1996;347:75-9. (Level II/III evidence)
20. Aubertin JM, Levoir D, Bouillot JL, et al. Endoscopic ultrasonography immediately prior to
laparoscopic cholecystectomy: a prospective evaluation. Endoscopy. 1996;28:667-73. ( Level
II/III evidence)
21. De Ledinghen V, Lecesne R, Raymond JM, et al. Diagnosis of choledocholithiasis: EUS or
magnetic resonance cholangiography? A prospective controlled study. Gastrointest Endosc.
1999;49:26-31. (Level III evidence)
22. Sahai AV, Mauldin PD, Marsi V, Hawes RH, et al. Bile duct stones and laparoscopic
cholecystectomy: a decision analysis to assess the roles of intraoperative cholangiography,
EUS, and ERCP. Gastrointest Endosc. 1999;49:334-43. (Level II/III evidence)
23. Demartines N, Eisner L, Schnabel K, et al. Evaluation of magnetic resonance cholangiography
in the management of bile duct stones. Arch Surg. 2000;135:148-52. (Level II/III evidence)
24. Dwerryhouse SJ, Brown E, Vipond MN, et al. Prospective evaluation of magnetic resonance
cholangiography to detect common bile duct stones before laparoscopic cholecystectomy.
Br J Surg. 1998;85:1364-6. (Level II/III evidence)
25. Soto JA, Alvarez O, Munera F, et al. Diagnosing bile duct stones: comparison of unenhanced
helical CT, oral contrast enhanced CT cholangiography, and MR cholangiography. AJR Am J
Roentgenol. 2000;175:1127-34. (Level III evidence)
26. Polkowski M, Palucki J, Regula J, et al. Helical computed tomographic cholangiography
versus endosonography for suspected bile duct stones: a prospective blinded study in non-
jaundiced patients. Gut. 1999;45:744-9. (Level II/III evidence)
27. Van Beers BE, Lacrosse M, Trigaux JP, et al. Noninvasive imaging of the biliary tree before or
after laparoscopic cholesystectomy: use of three-dimensional spiral CT cholangiography.
7/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
AJR Am J Roentgenol. 1994;162:1331-5. (Level III evidence)
28. Hirao K, Miyazaki A, Fujimoto T, et al. Evaluation of aberrant bile ducts before laparoscopic
cholecystectomy: helical CT cholangiography versus MR cholangiography. AJR Am J
Roentgenol. 2000;175:713-20. (Level III evidence)
29. O'Connor HJ, Hamilton I, Ellis WR, et al. Ultrasound detection of choledocholithiasis:
prospective comparison with ERCP in the post cholecystectomy patient. Gastrointest Radiol.
1986;11:161-4. (Level II evidence). View the reference
30. Cronan JJ. US diagnosis of choledocholithiasis: a reappraisal. Radiology. 1986;161:133-4.
(Level III evidence)
31. Griffin N, Wastle ML, Dunn WK, Ryder SD, Beckingham IJ. Magnetic resonance
cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the
diagnosis of choledocholithiasis. Eur J Gastroenterol Hepatol. 2003;15:809-13 (Level II
evidence). View the reference
32. Ledro-Cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic
resonance cholangio-pancreatography? A systematic review. Eur J Gastroenterol Hepatol.
2007;19(11);1007-11. (Level I/II evidence)
33. Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the
management of common bile duct stones (CBDS). Gut. 2008;57(7);1004-21. (Guidelines)
Further Reading
1. Shah SK, Mutignani, Costamagna G, et al. Therapeutic biliary endoscopy. Endoscopy.
2002;34(1):43-53. (Review article)
2. Palazzo L. Which test for common bile duct stones? Endoscopic and intraductal
ultrasonography. Endoscopy. 1997;29:655-65. (Review article)
Information for Consumers
Information from this website Information from the Royal
Australian and New Zealand
College of Radiologists’ website
Consent to Procedure or Treatment Computed Tomography (CT)
Radiation Risks of X-rays and Scans Iodine-Containing Contrast Medium
Computed Tomography (CT) Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) Radiation Risk of Medical Imaging During
Pregnancy
Ultrasound
Radiation Risk of Medical Imaging for
Adults and Children
Ultrasound
8/9 Phoca PDF
Diagnostic Imaging Pathways - Laparoscopic Cholecystectomy
Printed from Diagnostic Imaging Pathways
www.imagingpathways.health.wa.gov.au
© Government of Western Australia
Copyright
© Copyright 2015, Department of Health Western Australia. All Rights Reserved. This web site and its
content has been prepared by The Department of Health, Western Australia. The information contained on
this web site is protected by copyright.
Legal Notice
Please remember that this leaflet is intended as general information only. It is not definitive and The
Department of Health, Western Australia can not accept any legal liability arising from its use. The
information is kept as up to date and accurate as possible, but please be warned that it is always subject
to change
File Formats
Some documents for download on this website are in a Portable Document Format (PDF). To read these
files you might need to download Adobe Acrobat Reader.
Legal Matters
9/9 Phoca PDF
Powered by TCPDF (www.tcpdf.org)
You might also like
- The Role of Imaging Methods in Identifying The Causes of Extrahepatic CholestasisDocument7 pagesThe Role of Imaging Methods in Identifying The Causes of Extrahepatic CholestasisValian IndrianyNo ratings yet
- The Value of MRCPDocument5 pagesThe Value of MRCPBella YulandaNo ratings yet
- The Role of Imaging Methods in Identifying The CausesDocument7 pagesThe Role of Imaging Methods in Identifying The CausesJOSE ERNESTO AGUIRRE ALVAREZNo ratings yet
- Modern Imaging in Obstructive JaundiceDocument4 pagesModern Imaging in Obstructive JaundicedanaogreanuNo ratings yet
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Ultrasonic Diagnosis Methods For CholedocholithiasisDocument5 pagesUltrasonic Diagnosis Methods For CholedocholithiasisCentral Asian StudiesNo ratings yet
- Diagnostic Imaging Pathways ArticleDocument10 pagesDiagnostic Imaging Pathways ArticleSuhayatra PutraNo ratings yet
- Exploración VBDocument24 pagesExploración VBEstefania Van der VazcomNo ratings yet
- 10 1016@j Suc 2018 12 007Document24 pages10 1016@j Suc 2018 12 007Gabriel RangelNo ratings yet
- Clinical Spotlight Review For The Management of CholedocholithiasisDocument10 pagesClinical Spotlight Review For The Management of CholedocholithiasisLourdes MarquezNo ratings yet
- Clinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationDocument15 pagesClinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationMu TelaNo ratings yet
- Aresia de Vias Biliares UltrasonidoDocument14 pagesAresia de Vias Biliares UltrasonidoArturo GarciaNo ratings yet
- 12 BuenoDocument7 pages12 BuenoFlipNo ratings yet
- Schwartz2002 PDFDocument7 pagesSchwartz2002 PDFnova sorayaNo ratings yet
- Accuracy of Abbreviated Protocol ofDocument5 pagesAccuracy of Abbreviated Protocol ofBella YulandaNo ratings yet
- Distal Cholangiocarcinoma (DCC) : Paxton V. Dickson, MD, Stephen W. Behrman, MDDocument57 pagesDistal Cholangiocarcinoma (DCC) : Paxton V. Dickson, MD, Stephen W. Behrman, MDALberta YosheNo ratings yet
- Wiles2017 Article ManagementAndFollow-upOfGallblDocument11 pagesWiles2017 Article ManagementAndFollow-upOfGallblTrần Quốc KhánhNo ratings yet
- 012011SCNA3Document14 pages012011SCNA3mariafmhNo ratings yet
- Bile Duct DilatedDocument4 pagesBile Duct DilatedAmit GauravNo ratings yet
- Technicalaspectsofbileduct Evaluationandexploration: Sean B. Orenstein,, Jeffrey M. Marks,, Jeffrey M. HardacreDocument16 pagesTechnicalaspectsofbileduct Evaluationandexploration: Sean B. Orenstein,, Jeffrey M. Marks,, Jeffrey M. HardacreBattousaih1No ratings yet
- Choledocholithiasis: Evolving Standards For Diagnosis and ManagementDocument6 pagesCholedocholithiasis: Evolving Standards For Diagnosis and ManagementAngel Princëzza LovërzNo ratings yet
- Technical Solutions To Improve The Management of Non-muscle-Invasive Transitional Cell CarcinomaDocument42 pagesTechnical Solutions To Improve The Management of Non-muscle-Invasive Transitional Cell CarcinomaZICONo ratings yet
- Exploración Del ColédocoDocument14 pagesExploración Del ColédocoJavier VegaNo ratings yet
- Background: Open Access Original Article DOI: 10.7759/cureus.10987Document5 pagesBackground: Open Access Original Article DOI: 10.7759/cureus.10987hengkyNo ratings yet
- Intraoperative CholangiographyDocument6 pagesIntraoperative CholangiographyPolly LombardiniNo ratings yet
- Acute and Chronic in Ammation of The Biliary SystemDocument4 pagesAcute and Chronic in Ammation of The Biliary Systemfawzan mohammadNo ratings yet
- International Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. ChitheerDocument7 pagesInternational Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. Chitheersamer falconNo ratings yet
- Jurnal MRCPDocument18 pagesJurnal MRCPMaharani Eka SaputriNo ratings yet
- Revisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsDocument26 pagesRevisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsArturo García MarquezNo ratings yet
- Cholecystectomy and Common Bile Duct ExplorationDocument22 pagesCholecystectomy and Common Bile Duct ExplorationmohamedhazemelfollNo ratings yet
- Open CholecystectomyDocument35 pagesOpen CholecystectomywqNo ratings yet
- CholedocholithiasisDocument9 pagesCholedocholithiasisOsiithaa CañaszNo ratings yet
- CholangitisDocument20 pagesCholangitisNikoFebriRyandoNo ratings yet
- Advantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct StonesDocument5 pagesAdvantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct Stonesnaili nsnNo ratings yet
- Imaging in Chronic PancreatitisDocument7 pagesImaging in Chronic Pancreatitisdesy 102017135No ratings yet
- It Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaDocument5 pagesIt Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaIJAR JOURNALNo ratings yet
- Ureteral Calculi Imaging: A Literature Review Comparing Plain Film Studies, Contrast Media Studies, Ultrasound and Computed TomographyDocument6 pagesUreteral Calculi Imaging: A Literature Review Comparing Plain Film Studies, Contrast Media Studies, Ultrasound and Computed TomographyAvicenna Shafhan ArfiNo ratings yet
- Ictericia Obstructiva, Tratamiento EndoscópicoDocument6 pagesIctericia Obstructiva, Tratamiento EndoscópicoGeraldine RuizNo ratings yet
- J10 - T3 Criterios de Cotton ColedocolitiasisDocument7 pagesJ10 - T3 Criterios de Cotton ColedocolitiasisJuan Camilo MoralesNo ratings yet
- Cholelithiasis With Choledocholithiasis: Epidemiological, Clinical ProfileDocument3 pagesCholelithiasis With Choledocholithiasis: Epidemiological, Clinical ProfileShashank KumarNo ratings yet
- Chapter 10Document9 pagesChapter 10Kanishka SamantaNo ratings yet
- Hepatocellular Carcinoma - Diagnosis and TreatmentDocument46 pagesHepatocellular Carcinoma - Diagnosis and TreatmentSigh BalaNo ratings yet
- Accuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureDocument4 pagesAccuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureAnasriNstNo ratings yet
- PIIS0923753422046993Document14 pagesPIIS0923753422046993Justitia Yudiarti BasriNo ratings yet
- The Gallbladder Diseases Bile Duct StoneDocument69 pagesThe Gallbladder Diseases Bile Duct Stoneحميد حيدرNo ratings yet
- Diagnostic Imaging Pathways Article PDFDocument12 pagesDiagnostic Imaging Pathways Article PDFchald ald smithNo ratings yet
- Diagnostic DecisionDocument9 pagesDiagnostic DecisionfrigandraNo ratings yet
- ERCP Diagnostik Dan TerapeutikDocument5 pagesERCP Diagnostik Dan Terapeutikrisyda_mkhNo ratings yet
- Ni Wayan Dwi NovitaDocument6 pagesNi Wayan Dwi NovitaDwi ZirobeNo ratings yet
- 02 PDFDocument17 pages02 PDFDrelsayed HagagNo ratings yet
- Surg 2 JaundicedDocument94 pagesSurg 2 Jaundicedapi-3728522No ratings yet
- Lower Gastrointestinal Cancer - ColorectalDocument17 pagesLower Gastrointestinal Cancer - ColorectalSyakinah SabudinNo ratings yet
- Articulo ColedocolitiasisDocument6 pagesArticulo ColedocolitiasisMartha Carolina Hernandez UribeNo ratings yet
- Obstructive Jaundice Klerida Shehu-1Document15 pagesObstructive Jaundice Klerida Shehu-1Klerida ShehuNo ratings yet
- Coledocolitiasis CurrentDocument6 pagesColedocolitiasis CurrentvalNo ratings yet
- Del Beke 2004Document7 pagesDel Beke 2004nitsuga oneNo ratings yet
- Impact of Endoscopy System, High Definition, and Virtual Chromo-Endoscopy in Daily Routine Colonoscopy: A Randomized TrialDocument7 pagesImpact of Endoscopy System, High Definition, and Virtual Chromo-Endoscopy in Daily Routine Colonoscopy: A Randomized Trialm_manuela2002No ratings yet
- Radiotherapy of Liver CancerFrom EverandRadiotherapy of Liver CancerJinsil SeongNo ratings yet
- Fast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesFrom EverandFast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesNo ratings yet
- Gastrointestinal Endoscopy in the Cancer PatientFrom EverandGastrointestinal Endoscopy in the Cancer PatientJohn C. DeutschNo ratings yet
- A Case Report of Pilocytic Astrocytoma Mimicking Meningioma On ImagingDocument4 pagesA Case Report of Pilocytic Astrocytoma Mimicking Meningioma On ImagingIndra PrimaNo ratings yet
- Intrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationDocument13 pagesIntrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationIndra PrimaNo ratings yet
- Hepatic BilomaDocument1 pageHepatic BilomaIndra PrimaNo ratings yet
- Hepatic Subcapsular BIloma A Rare Complication of Laparoscopic CholecystectomyDocument4 pagesHepatic Subcapsular BIloma A Rare Complication of Laparoscopic CholecystectomyIndra PrimaNo ratings yet
- Rising Incidennce of Sporadic Vestibular Schwannoma True Biological Shift Versus Simpply Greater DetectionDocument5 pagesRising Incidennce of Sporadic Vestibular Schwannoma True Biological Shift Versus Simpply Greater DetectionIndra PrimaNo ratings yet
- Air Cisternography of The Cerebellopontine Angle Using High Resolution Computed TomographyDocument3 pagesAir Cisternography of The Cerebellopontine Angle Using High Resolution Computed TomographyIndra PrimaNo ratings yet
- Segmentation of Vestibular Schwannoma From MRI, An Open Annotated Dataset and Baseline AlgorithmDocument6 pagesSegmentation of Vestibular Schwannoma From MRI, An Open Annotated Dataset and Baseline AlgorithmIndra PrimaNo ratings yet
- Extrahepatic Biloma Potential Imaging Pitfall With No Touch Wedge Ablation of Subcapsular Liver TumorsDocument2 pagesExtrahepatic Biloma Potential Imaging Pitfall With No Touch Wedge Ablation of Subcapsular Liver TumorsIndra PrimaNo ratings yet
- Imaging of Vestibular Schwannoma With Prevalent Cystic Component Cystic Vestibular SchwannomaDocument2 pagesImaging of Vestibular Schwannoma With Prevalent Cystic Component Cystic Vestibular SchwannomaIndra PrimaNo ratings yet
- Clinical Features of Intracranial Vestibular SchwannomasDocument6 pagesClinical Features of Intracranial Vestibular SchwannomasIndra PrimaNo ratings yet
- Epidemiology of Vestibular Schwannomas Prospective 40 Year Data From An Unselected Antional CohortDocument6 pagesEpidemiology of Vestibular Schwannomas Prospective 40 Year Data From An Unselected Antional CohortIndra PrimaNo ratings yet
- Current Imaging Tools For Vestibular SchwannomaDocument6 pagesCurrent Imaging Tools For Vestibular SchwannomaIndra PrimaNo ratings yet
- Epidemiology of Vestibular Schwannoma in The United States 2004-2016Document8 pagesEpidemiology of Vestibular Schwannoma in The United States 2004-2016Indra PrimaNo ratings yet
- Congenital Brain Anomalies Neuroimaging FindingsDocument9 pagesCongenital Brain Anomalies Neuroimaging FindingsIndra PrimaNo ratings yet
- Non Perforated Peptic Ulcer Disease, Multidetector CT Finding, Complication, and Differential DiagnosisDocument15 pagesNon Perforated Peptic Ulcer Disease, Multidetector CT Finding, Complication, and Differential DiagnosisIndra PrimaNo ratings yet
- Imaging Manifestations of Peptic Ulcer Disease On Computed TomographyDocument25 pagesImaging Manifestations of Peptic Ulcer Disease On Computed TomographyIndra PrimaNo ratings yet
- Arc 488Document7 pagesArc 488Apoorva SinghNo ratings yet
- Hacienda Starke V CuencaDocument2 pagesHacienda Starke V CuencaGino Alejandro SisonNo ratings yet
- ARI - CAPEX FFE FormDocument2 pagesARI - CAPEX FFE FormWaleed AhmedNo ratings yet
- Acknowledgement Sheet: InformationDocument1 pageAcknowledgement Sheet: InformationRisa Al AdewiyaNo ratings yet
- 10, Electrical DetailDocument4 pages10, Electrical Detailrp63337651No ratings yet
- Speaking Templates For All 8 Parts of CELPIP. Structure & SamplesDocument11 pagesSpeaking Templates For All 8 Parts of CELPIP. Structure & SamplesPiyush Sharma100% (2)
- He A IgnitorDocument36 pagesHe A IgnitorE.C.MADHUDUDHANA REDDYNo ratings yet
- Politeness Theory and Conversational Refusals Associations Between Various Types of Face Threatand Perceived CompetenceDocument21 pagesPoliteness Theory and Conversational Refusals Associations Between Various Types of Face Threatand Perceived CompetenceDavid LeNo ratings yet
- Metgraf Data SheetDocument1 pageMetgraf Data SheetFlorin BargaoanuNo ratings yet
- Analysis of Risk and Its Management in Indian Banks: A Case of SBI BankDocument19 pagesAnalysis of Risk and Its Management in Indian Banks: A Case of SBI BankRITIKANo ratings yet
- PCX 160 (Ultimate Excellence) : Honda Premium Matic Day (HPMD) #Cari - AmanDocument4 pagesPCX 160 (Ultimate Excellence) : Honda Premium Matic Day (HPMD) #Cari - AmanMUHAMMAD RIDHO AZHARNo ratings yet
- CAT Asphalt Paver Maintenance PDFDocument45 pagesCAT Asphalt Paver Maintenance PDFDaniloRullanNo ratings yet
- Ece Scheme-2017 IIIIV Sem SyllabusDocument42 pagesEce Scheme-2017 IIIIV Sem Syllabusapi-279049687No ratings yet
- Introduction To Computing Final ExamDocument19 pagesIntroduction To Computing Final ExamAji Nikka AngelesNo ratings yet
- A Study On Job Satisfaction Among Nursing Staff in A Tertiary Care Teaching HospitalDocument5 pagesA Study On Job Satisfaction Among Nursing Staff in A Tertiary Care Teaching HospitalIOSRjournalNo ratings yet
- Carti Vertical Flight PDFDocument214 pagesCarti Vertical Flight PDFsaitoc0% (1)
- GRDC BPG Snails Southwest1 PDFDocument16 pagesGRDC BPG Snails Southwest1 PDFVladut BratfaleanNo ratings yet
- Migracion WAS8Document472 pagesMigracion WAS8ikronos0No ratings yet
- Assignement Primark AnitaDocument16 pagesAssignement Primark AnitaAnita Krishnan100% (1)
- Geography SyllabusDocument4 pagesGeography SyllabusmvrthedocNo ratings yet
- Splitted Biogas Plant Project - Group 6 (1) - 1Document5 pagesSplitted Biogas Plant Project - Group 6 (1) - 1SOUNAK BANDYOPADHYAYNo ratings yet
- DHA Procedure InformationDocument3 pagesDHA Procedure InformationShan Shani60% (5)
- Rhino Craft BrochureDocument12 pagesRhino Craft Brochurebond007phNo ratings yet
- Zebrafish Poster Portrait Eupfi Sep 2106 Final SubmittedDocument1 pageZebrafish Poster Portrait Eupfi Sep 2106 Final Submittedapi-266268510No ratings yet
- Standard Chartered PLC Is A British Multinational BankingDocument8 pagesStandard Chartered PLC Is A British Multinational Bankingaditya saiNo ratings yet
- Module 1: Exploring EntrepreneurshipDocument5 pagesModule 1: Exploring EntrepreneurshipZara DelacruzNo ratings yet
- 7.city Development Plan - NagpurDocument34 pages7.city Development Plan - Nagpurapi-27095887100% (2)
- ABEN70a LR02 Briones Rachel DDocument5 pagesABEN70a LR02 Briones Rachel DRACHEL BRIONESNo ratings yet
- Gemba WalkDocument10 pagesGemba WalkAsmamaw FirewNo ratings yet
- Shashank Sasane 02Document1 pageShashank Sasane 02Pratik BajiNo ratings yet