Professional Documents
Culture Documents
Obstructive Jaundice Klerida Shehu-1
Uploaded by
Klerida Shehu0 ratings0% found this document useful (0 votes)
5 views15 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views15 pagesObstructive Jaundice Klerida Shehu-1
Uploaded by
Klerida ShehuCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 15
Advanced imagery examinations on the
diagnosis of obstructive jaundice.
Dr. Shk. M Klerida Shehu
Universiteti Mjekesise Tirane
FSHMT
ALLPPT.com _ Free PowerPoint Templates, Diagrams and Charts
Introduction
• Obstructive jaundice is defined as the impossibility of inflow of a
normal quantity of bile into the duodenum due to lesions or obstacles
at the level of the choledochus or the common hepatic duct
• Obstructive jaundice is not a definitive diagnosis and the early investi-
gation of the cholestasis cause is of great importance
• The main causes of extra hepatic jaundice are:
• common bile duct (CBD) stones,
• CBD strictures and congenital malformations (cysts, Caroli dis-
ease),
• cholangiocarcinoma,
• ampullary carcinoma,
• pancreatic diseases (pancreatic head carcinoma or pseudocysts,
pseudotumoral chronic pancreatitis),
• duodenal diverticulas,
• ascaridiasis, and hemobilia.
Introduction
In the recent years there is a continuous development in the
diagnosis of biliary obstructive disease.
The examinations modality includes :
• Transabdominal ultrasound (TUS)
• EUS
• Computed tomography (CT),
• HIDA CT
• Endoscopic retrograde cholangiopancreatography (ERCP),
• Percutaneous transhepatic cholangiography (PTC),
• Magnetic resonance cholangiopancreatography (MRCP)
• Cholangio computed tomography (CCT).
The use of accurate methods in patients with obstructive
jaundice is important to surgeons, imageries and endo-
scopists.
Ultrasound TUS
• First choice option in diagnosing of biliary tract disease for sev-
eral years. It Is considered relatively cheap, readily available and
noninvasive.
• Routine transabdominal ultrasound indicates the size of the bile
ducts, and thus it may define the level of bile duct obstruction,
identify the cause and provide other information related to the
disease (e.g. presence of gallstones or hepatic metastases, -be-
nign and malignant causes of obstruction or any associated con-
ditions and complications).
• TUS is particularly useful because it offers the ability to assess
no-invasively in real-time the pancreaticobiliary tracts, it does not
expose the patient to radiation.
• TUS is highly dependent on the operator and requires technical
skills and experience to produce consistently good results.
EUS
• Endoscopy aided ultrasound
• Distal common bile duct and ampulla
• Staging & vascular invasion
• EUS duided FNA
CT
• The computed tomography (CT) is another non-invasive procedure used in
initial patient evaluation. It has variable sensitivity in detecting of different
etiology of obstructive jaundice.
• The accuracy of conventional CT in determining the presence and level of
obstruction has been 81 to 94% and 88 to 92% respectively.
• CT has a limited availability due to the high costs and exposure to radia-
tion, both of which reduce the routine use.
• It is contraindicated in pregnant patients, as well as in those allergic to
contrast agents.
• Using of intravenous contrast helps to differentiate and define the vascular
structures and the biliary tract more accurately than TUS.
• Thus, traditional computed tomography (CT) scanning is usually consid-
ered more accurate than TUS on determining the specific obstruction’s
cause and level.
ERCP
• Over the past years, ERCP has been the principal diagnostic examination
of the biliary tract and it is considered to be the gold standard for the
evaluation of pancreaticobiliary disease. (9, 13-16).
• ERCP differentiates between the intra hepatic and extra-hepatic biliary
duct dilatation, presence of stones and the site of bile duct stricture with
the highest accuracy ( 90-100%).
• Nevertheless, diagnostic ERCP is an uncomfortable and painful procedure
associated with a complication rate of up to 9% (9).
• ERCP is associated with significant complications such as pancreatitis, per-
foration, hemorrhage, sepsis, and bile leak. ERCP procedure has been re-
ported to be accompanied by a mortality of up to 1% (5, 13-16).
• PTC and ERCP have high accuracy rates on detecting the presence and
level of obstruction, but they are invasive and have high complication
rates. Thus, the need for an accurate and patient friendly technique has
been consistently evident over the past years.
PTC
• PTC and ERCP are direct cholangiographic techniques. If the in-
tra-hepatic ducts are dilated, the success diagnostic rate of PTC
is very high. The accuracy in defining the level of obstruction is
more than 90%.
• The technique of performing of PTC is not easy and it requires a
considerable experience in order to achieve the desired sensitiv-
ity and specificity. There is the opportunity of complication de-
velopment during PTC.
• The complication rates are estimated to be high, probably up to
10% of cases. The complications during PTC can include skin in-
fection and sepsis, intra-peritoneal hemorrhage, hemobilia and
bile leak, hepatic and perihepatic abscess, pneumothorax and
granuloma at the catheter entry site.
MRCP
• Magnetic resonance cholangiopancreatography is a new applica-
tion of MR, considered as a non-invasive, simple, and accurate
method.
• MRCP defines the biliary tract in patients suspected of obstruc-
tive jaundice, and it can provide both a high quality cross-sec-
tional image of duct structures, as well as projectional images of
the biliary tract and pancreatic duct.
• Unlike ERCP, MRCP is noninvasive and the images are obtained
without any use of oral or intravenous contrast agents (17).
• MRCP has a sensitivity of 95% and specificity of 95% on defining
the level and presence of biliary obstruction (9, 13).
• MRCP, for its high diagnostic value, is necessary to be performed
prior to invasive procedures of ERCP and/or PTC in patients
showing a suspicious clinical and laboratory findings and nega-
tive finding on TUS/CT (17).
MRCP Complications/limitations
• There are no known risks associated with MRCP.
• The limitations of MR are related to claustrophobia,
cardiac pacemakers, massive ascite or hemodynamic
instability.
• Claustrophobia and emotional distress prevent
completion of MRI procedure in up to 5% of pa-
tients (13, 18).
• The impracticality of its therapeutic application after
detecting the cause of the obstruction is another
limitation. Patient obesity may limit the quality of
MRCP images and prevent patients from being able
to enter the MRI scanner. In addition, the MRCP
cannot detect lesions or calculi smaller than 3 mm
MRCP vs Other procedures
• MRCP allow the accurate imaging of the extraductal structures, and thus
MRCP is a fundamental procedure for the characterization and stage of
spreading tumors with a sensitivity and specificity comparable to those of CT
• Diagnostic capability of CCT is comparable to that of MRCP, and it is appro-
priate and recommended if MRCP is not applicable.
• The main advantages of CCT are quick performance with few motion arti-
facts, good patient compliance and further identification of confusing lesions
of the liver, pancreas and hepato-duodenal ligament.
• Due to use of adverse reactions and contraindications of ionizing radiation
CCT is used more to correct MRCP false negatives and not as a proper alter-
native of MRCP
MRCP vs ERCP
• MRCP is particularly useful where ERCP is difficult,
hazardous or impossible, such as in patients who
have had Billroth II gastrectomy, pancreatic pseudo-
cysts, sclerosing cholangitis etc.
• MRCP is particularly useful where ERCP is difficult,
hazardous or impossible, such as in patients who
have had Billroth II gastrectomy, pancreatic pseudo-
cysts, sclerosing cholangitis and prior serious ERCP
complications (24).
• Another important advantage of MRCP is that it can
be coupled with MRI of adjacent viscera for identifi-
cation, characterization and staging of malignant
strictures.
MRCP vs ERCP
• In addition, MRCP is a non-invasive technique which does not
necessitate iodinated intravenous contrast agent or ionizing radi-
ation, and enables a quick and reliable diagnosis in almost all
cases.
• MRCP permits a complete accurate imaging of the biliary tract
above and below the obstruction site. MRCP provides a full im-
age, as well as a detailed visualization of the whole biliary tract
enables projection of the drainage catheters’ location and pre-
operatory evaluation especially in those patients with bilioenteric-
anastomosis, along with the evaluation of stenoses and calculi re-
sulting from cholecystectomy.
Obstructive jaundice management algorithm
Conclusion
• Although transabdomial ultrasound examination still con-
tinues to be the preliminary investigation modality to
identify the presence of obstructive jaundice, its incapabil-
ity to answer the true extent and cause of obstructive
jaundice demands the use of another imaging modality
like MRCP or ERCP, which scores over ultrasound in diag-
nostic accuracy.
• MRCP can be considered as the new gold standard for
the diagnosing of obstruction jaundice, and allow use of
ERCP only to patients with a high probability of therapeu-
tic intervention.
You might also like
- Ultrasonography of The Hepatobiliary TractDocument9 pagesUltrasonography of The Hepatobiliary TractPaola Méndez NeciosupNo ratings yet
- Carcinomagallbladder PDFDocument61 pagesCarcinomagallbladder PDFZaki DhiifNo ratings yet
- Prometric Pharmacy MCQs (Solved)Document45 pagesPrometric Pharmacy MCQs (Solved)cuami84% (45)
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- Exercise Physiology Lab ReportDocument10 pagesExercise Physiology Lab Reportapi-253305501100% (1)
- Obstructive Jaundice: Abdel Rahman A. Al Manasra, MDDocument56 pagesObstructive Jaundice: Abdel Rahman A. Al Manasra, MDAmyandNo ratings yet
- Gall Bladder CarcinomaDocument29 pagesGall Bladder CarcinomaUsman FarooqNo ratings yet
- Liver Cirrhosis Case PresentationDocument146 pagesLiver Cirrhosis Case Presentationjennachristy0395% (21)
- Final Myocardial Infarction Pathophysiology PDFDocument3 pagesFinal Myocardial Infarction Pathophysiology PDFDave JoshuaNo ratings yet
- Investigation and Treatment of Surgical JaundiceDocument38 pagesInvestigation and Treatment of Surgical JaundiceUjas PatelNo ratings yet
- BAM Chapter 12 - Staphylococcus Aureus - FDADocument9 pagesBAM Chapter 12 - Staphylococcus Aureus - FDAfood tecknologistNo ratings yet
- Lassa Fever IntroductionDocument22 pagesLassa Fever IntroductionCj LowryNo ratings yet
- Sindroma Nefrotik Vs NefritikDocument23 pagesSindroma Nefrotik Vs NefritikBobby Fildian Siswanto100% (3)
- The Role of Imaging Methods in Identifying The Causes of Extrahepatic CholestasisDocument7 pagesThe Role of Imaging Methods in Identifying The Causes of Extrahepatic CholestasisValian IndrianyNo ratings yet
- Technicalaspectsofbileduct Evaluationandexploration: Sean B. Orenstein,, Jeffrey M. Marks,, Jeffrey M. HardacreDocument16 pagesTechnicalaspectsofbileduct Evaluationandexploration: Sean B. Orenstein,, Jeffrey M. Marks,, Jeffrey M. HardacreBattousaih1No ratings yet
- Modern Imaging in Obstructive JaundiceDocument4 pagesModern Imaging in Obstructive JaundicedanaogreanuNo ratings yet
- Exploración Del ColédocoDocument14 pagesExploración Del ColédocoJavier VegaNo ratings yet
- MRCP Vs ErcpDocument1 pageMRCP Vs ErcpgastropovNo ratings yet
- Acutecholangitis 110927014348 Phpapp01Document25 pagesAcutecholangitis 110927014348 Phpapp01shintameliaNo ratings yet
- 012011SCNA3Document14 pages012011SCNA3mariafmhNo ratings yet
- The Role of Imaging Methods in Identifying The CausesDocument7 pagesThe Role of Imaging Methods in Identifying The CausesJOSE ERNESTO AGUIRRE ALVAREZNo ratings yet
- Cholangiocarcinoma: R.KarthikeyanDocument49 pagesCholangiocarcinoma: R.KarthikeyanKarthikeyan R100% (2)
- Background: Endoscopic Retrograde Cholangiopancreatography (ERCP)Document4 pagesBackground: Endoscopic Retrograde Cholangiopancreatography (ERCP)Resci Angelli Rizada-NolascoNo ratings yet
- 10 1016@j CLD 2014 09 006Document23 pages10 1016@j CLD 2014 09 006Felix camilo GonzálezNo ratings yet
- Coledocolitiasis CurrentDocument6 pagesColedocolitiasis CurrentvalNo ratings yet
- Acutecholangitis 110927014348 Phpapp01Document25 pagesAcutecholangitis 110927014348 Phpapp01Rabecca TobingNo ratings yet
- Gall Bladder CancerDocument29 pagesGall Bladder CancerJoju SebastianNo ratings yet
- UTUCDocument39 pagesUTUCShalini shreeNo ratings yet
- EAU Pocket On Renal Cell Carcinoma 2022Document28 pagesEAU Pocket On Renal Cell Carcinoma 2022Dane QhNo ratings yet
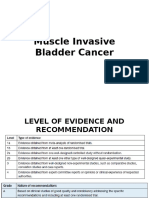
- Muscle Invasive Bladder CancerDocument39 pagesMuscle Invasive Bladder CancerBernardNo ratings yet
- Advances in Liver Uts, CT Towards The FuturesDocument28 pagesAdvances in Liver Uts, CT Towards The FuturesMika OdevilasNo ratings yet
- Clinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationDocument15 pagesClinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationMu TelaNo ratings yet
- Otto Van Delden and Robin SmithuisDocument11 pagesOtto Van Delden and Robin SmithuisSheila AnisaNo ratings yet
- Ictericia Obstructiva, Tratamiento EndoscópicoDocument6 pagesIctericia Obstructiva, Tratamiento EndoscópicoGeraldine RuizNo ratings yet
- LAR Alternative Anastomotic TechniquesDocument15 pagesLAR Alternative Anastomotic Techniquesdrneeraj168No ratings yet
- 10 1016@j Suc 2018 12 007Document24 pages10 1016@j Suc 2018 12 007Gabriel RangelNo ratings yet
- Endoscopic Retrograde Cholangiopancreatography (Ercp) : Jinu Janet Varghese Group IV Year IIIDocument22 pagesEndoscopic Retrograde Cholangiopancreatography (Ercp) : Jinu Janet Varghese Group IV Year IIIManish DhapolaNo ratings yet
- Exploración VBDocument24 pagesExploración VBEstefania Van der VazcomNo ratings yet
- Imaging in The Diagnosis of Pediatric UrolithiasisDocument16 pagesImaging in The Diagnosis of Pediatric UrolithiasisAulia ErizalNo ratings yet
- Selection of Modality - Computed Tomography (CT) of The Abdomen andDocument3 pagesSelection of Modality - Computed Tomography (CT) of The Abdomen andevanNo ratings yet
- CA Gall BladderDocument24 pagesCA Gall BladderTheoder RobinsonNo ratings yet
- Preferred Examination: Right Ureteral Calculus With Periureteral StrandingDocument26 pagesPreferred Examination: Right Ureteral Calculus With Periureteral StrandingErrina YustiraNo ratings yet
- Common Bile Duct Stones StrictureDocument48 pagesCommon Bile Duct Stones StrictureSyarif MalawatNo ratings yet
- Multiple Nodul Hepar NcbiDocument6 pagesMultiple Nodul Hepar NcbisyaymaNo ratings yet
- Pproach TO Bstructive Aundice: Yeo Quan YouDocument40 pagesPproach TO Bstructive Aundice: Yeo Quan YouThaer HafiNo ratings yet
- Colorectal Carcinoma SurgeryDocument19 pagesColorectal Carcinoma SurgeryDaanishNo ratings yet
- Renal LectureDocument28 pagesRenal Lecturejohn promaNo ratings yet
- Diagnostic Imaging Pathways ArticleDocument9 pagesDiagnostic Imaging Pathways ArticleIndra PrimaNo ratings yet
- 1-Urinary Tract Imaging TechniquesDocument27 pages1-Urinary Tract Imaging TechniquesallordNo ratings yet
- EAU Pocket On Renal Cell Carcinoma 2023Document29 pagesEAU Pocket On Renal Cell Carcinoma 2023Phuoc LeNo ratings yet
- Radiologi Onkologi: Muhammad Iqbal Dr. Rony Rustam, SPB (K) OnkDocument8 pagesRadiologi Onkologi: Muhammad Iqbal Dr. Rony Rustam, SPB (K) OnkakreditasirsurNo ratings yet
- Magnetic Resonance Cholangiography: Past, Present and Future: A ReviewDocument5 pagesMagnetic Resonance Cholangiography: Past, Present and Future: A ReviewYusron Adi FachrudinNo ratings yet
- EAU 2024 Pocket GuidelinesDocument571 pagesEAU 2024 Pocket Guidelinesgreatkhanjee82No ratings yet
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Comparison Between Outcomes of Laparoscopic Cholecystectomy in Patients With Liver Cirrhosis or With Normal Liver FunctionDocument40 pagesComparison Between Outcomes of Laparoscopic Cholecystectomy in Patients With Liver Cirrhosis or With Normal Liver FunctionSudhanshu PathakNo ratings yet
- Hepatocellular Carcinoma - Diagnosis and TreatmentDocument46 pagesHepatocellular Carcinoma - Diagnosis and TreatmentSigh BalaNo ratings yet
- Format For Manuscript Submission: ReviewDocument26 pagesFormat For Manuscript Submission: ReviewMariaNo ratings yet
- Renal CancerDocument13 pagesRenal CancerDavid RyanNo ratings yet
- Hepatobiliary SystemDocument66 pagesHepatobiliary SystemBikash SubediNo ratings yet
- Urology Sample Osce Exam e PDFDocument8 pagesUrology Sample Osce Exam e PDFLana LocoNo ratings yet
- EAU Pocket On Renal Cell Carcinoma 2024Document35 pagesEAU Pocket On Renal Cell Carcinoma 2024nadaelhaousNo ratings yet
- EUS Solid Pancreatic LesionsDocument42 pagesEUS Solid Pancreatic LesionsAhmed ElwassiefNo ratings yet
- Del Beke 2004Document7 pagesDel Beke 2004nitsuga oneNo ratings yet
- Anterior Resection With Low AnastomosisDocument10 pagesAnterior Resection With Low AnastomosisOhana S.No ratings yet
- Cholangiocarcinoma Differential DiagnosisDocument2 pagesCholangiocarcinoma Differential DiagnosisPremaKurniaNo ratings yet
- Biliopancreatic Endoscopy: Practical ApplicationFrom EverandBiliopancreatic Endoscopy: Practical ApplicationKwok-Hung LaiNo ratings yet
- Terjemahan Artikel ManuscriptDocument43 pagesTerjemahan Artikel ManuscriptettyNo ratings yet
- Psoriasis in UnaniDocument15 pagesPsoriasis in UnaniAbdul Jalil HridoyNo ratings yet
- Recent Advances in Orthognathic SurgeryDocument5 pagesRecent Advances in Orthognathic Surgerypedroalmeida37920No ratings yet
- 2 Prevalence of Sarcopenia in Multi EthnicsDocument10 pages2 Prevalence of Sarcopenia in Multi EthnicsdavidtuanandartuaNo ratings yet
- Ch.11. Transportation in Animals and PlantsDocument3 pagesCh.11. Transportation in Animals and PlantsSharath ChandraNo ratings yet
- Ya 20.2 Lung Cancer StagingDocument14 pagesYa 20.2 Lung Cancer StagingJuan Francisco Antonio VázquezNo ratings yet
- Charles River Editors Fighting The Plague in Antiquity and The Middle Ages - The History of Ancient ADocument70 pagesCharles River Editors Fighting The Plague in Antiquity and The Middle Ages - The History of Ancient AIury RangelNo ratings yet
- Essay My Role ModelDocument7 pagesEssay My Role Modelezke4pq2100% (2)
- Kode Icd 10Document38 pagesKode Icd 10interna squardNo ratings yet
- Analysis of Heavy Metals in Vegetable and Agricultural Soil Samples in Gemikonagi and Dipkarpaz (North Cyprus)Document82 pagesAnalysis of Heavy Metals in Vegetable and Agricultural Soil Samples in Gemikonagi and Dipkarpaz (North Cyprus)Ibrahim MoserayNo ratings yet
- JAH3 6 E004305Document9 pagesJAH3 6 E004305G1993NCKNo ratings yet
- Diabetic Foot CmeDocument29 pagesDiabetic Foot CmeAli emillyNo ratings yet
- TEJASWINIDocument8 pagesTEJASWINIAyush JamwalNo ratings yet
- Home Economics II PresentationDocument22 pagesHome Economics II PresentationEmmanuel S JamesNo ratings yet
- Multiple Choice Questions - Answers: 1. A B C DDocument5 pagesMultiple Choice Questions - Answers: 1. A B C Dsafa_sabaNo ratings yet
- Pfas Letter To Epw 11.15.2021Document10 pagesPfas Letter To Epw 11.15.2021WXMINo ratings yet
- Dental CariesDocument8 pagesDental CariesThe KittyNo ratings yet
- Financial ExpressDocument11 pagesFinancial Expresspath_of_success3569No ratings yet
- Early Adulthood: Stages in The Life SpanDocument6 pagesEarly Adulthood: Stages in The Life SpanAngelica Mae DanaoNo ratings yet
- MiscarriageDocument3 pagesMiscarriageCatherine PradoNo ratings yet
- AOAC Rapid Method ValidationDocument60 pagesAOAC Rapid Method ValidationPiruzi MaghlakelidzeNo ratings yet
- Secdocument - 813download Goodman and Snyders Differential Diagnosis For Physical Therapists Screening For Referral 7E Jun 2 2022 - 0323722040 - Elsevier 7Th Edition John Heick Full ChapterDocument68 pagesSecdocument - 813download Goodman and Snyders Differential Diagnosis For Physical Therapists Screening For Referral 7E Jun 2 2022 - 0323722040 - Elsevier 7Th Edition John Heick Full Chapterclara.yanez755100% (5)
- Medical Examiner's Report On Daniel PrudeDocument8 pagesMedical Examiner's Report On Daniel PrudePatrick Crozier100% (1)