Professional Documents
Culture Documents
Aetritias Septica Review
Aetritias Septica Review
Uploaded by
Nancy Margarita Gutierrez CastañedaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aetritias Septica Review
Aetritias Septica Review
Uploaded by
Nancy Margarita Gutierrez CastañedaCopyright:
Available Formats
M u s c u l o s k e l e t a l I m a g i n g • R ev i ew
Chan et al.
Septic Arthritis
Musculoskeletal Imaging
Review
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
Septic Arthritis: An Evidence-
FOCUS ON:
Based Review of Diagnosis and
Image-Guided Aspiration
Brian Y. Chan1 OBJECTIVE. The purpose of this evidence-based review is to equip radiologists to dis-
Amanda M. Crawford cuss and interpret findings obtained with various imaging modalities, guide patient selection
Patrick H. Kobes for percutaneous aspiration, and safely perform arthrocentesis to assess for infection in both
Hailey Allen native and prosthetic joints.
Richard L. Leake CONCLUSION. Septic arthritis is an emergency that can lead to rapidly progressive,
irreversible joint damage. Despite the urgency associated with this diagnosis, there remains
Christopher J. Hanrahan
a lack of consensus regarding many aspects of the management of native and periprosthetic
Megan K. Mills joint infections.
Chan BY, Crawford AM, Kobes PH, et al.
eptic arthritis is an emergency arthritis when emergency surgical interven-
S that can cause rapidly progres-
sive and irreversible damage to
the affected joint, resulting in se-
tion is deemed necessary.
Differential Diagnosis, Clinical Presentation,
rious morbidity and mortality. The incidence and Causative Organisms
of septic arthritis ranges from approximately The differential diagnosis of an acutely
2 cases per 100,000 people per year [1] to 20 painful joint is broad and includes crystal-
cases per 100,000 people per year in low-in- line and inflammatory arthritides, trauma,
come settings [2]. Its presentation varies by neoplasm, and infection. Patients with septic
patient demographics and is confounded arthritis classically present with fever, chills,
by preexisting comorbidities. Radiologists and a warm, erythematous, swollen, and pain-
should be equipped to counsel the ordering ful joint. However, variation in patient pre-
provider regarding the role of preinterven- sentation necessitates a high index of clinical
tion imaging. Familiarity with clinical pre- suspicion for septic arthritis. Patients present
sentation and laboratory assessment can help with high-grade fever in only 58% and serum
the radiologist guide patient selection for leukocytosis in only 50–60% of cases [4].
percutaneous aspiration. When arthrocente- Many risk factors predispose patients to
sis is pursued, understanding the technical septic arthritis (Table 1). Coexisting primary
considerations of the procedure and subse- rheumatologic disorders have been reported
Keywords: arthrocentesis, aspiration, interventional, quent fluid analysis can minimize patient in as many as 50% of patients with bacteri-
periprosthetic joint infection, septic arthritis risk and maximize diagnostic yield. Despite al arthritis [5]. Rheumatoid arthritis may in-
the important role radiologists play, clinical crease the risk of septic arthritis as much as
doi.org/10.2214/AJR.20.22773
workflow varies widely by practice setting 15-fold [6], owing to a combination of pre-
Received January 1, 2020; accepted after revision [3]. Review of the current state of knowledge existing joint damage, baseline immune dys-
February 26, 2020. is warranted to adopt an evidence-based ap- regulation, and use of immunomodulatory
1
proach to the diagnosis and management of therapy, such as tumor necrosis factor inhibi-
All authors: Department of Radiology and Imaging
septic arthritis. tors [7]. Both infection and acute exacerba-
Sciences, University of Utah School of Medicine,
30 N 1900 E, Rm 1A071, Salt Lake City, UT 84132-2140. tion of a chronic joint disorder may present
Address correspondence to B. Y. Chan Preaspiration Assessment with joint pain and swelling.
(brian.chan@utah.edu). Appropriate patient selection before joint The most common causative agent of
aspiration is a complex process with many adult septic arthritis is Staphylococcus au-
AJR 2020; 215:568–581 variables. Appendix 1 summarizes the con- reus, which accounts for more than 50% of
ISSN-L 0361–803X/20/2153– 568
siderations before arthrocentesis discussed cases [4] (Fig. 1). The incidence of methi-
in this review. On occasion, joint aspiration cillin-resistant S. aureus infection is on the
© American Roentgen Ray Society may be deferred in the evaluation of septic rise in the United States. Coagulase-negative
568 AJR:215, September 2020
Septic Arthritis
TABLE 1: Risk Factors for Septic Arthritis
Preexisting Joint Diseases Skin Diseases Medical Conditions Medication-Induced Conditions Other
Rheumatoid arthritis Psoriasis Diabetes mellitus Chronic systemic corticosteroid Prior joint arthroplasty
therapy (e.g., prednisone)
Crystalline deposition arthropathies Eczema Cirrhosis Disease-modifying antirheumatic IV drug use
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
(gout and calcium pyrophosphate drugs
deposition)
Osteoarthritis Skin ulcers End-stage renal disease Intraarticular corticosteroids Alcoholism
Systemic lupus erythematosus Skin infection HIV infection, AIDS, and other Other immunosuppressive Human bite (fight bite)
immunosuppressed states medications
Trauma Bacteremia Low socioeconomic status
Recent surgery Advanced age
staphylococci are often contaminants but can and treatment of septic arthritis in patients flammatory arthropathy [21]. Notably, 16%
cause clinically mild, indolent infections af- with negative synovial fluid culture results of septic joints in one study [21] contained a
ter orthopedic procedures. The incidence of can instead be directed at an organism cul- subjectively normal amount of fluid; howev-
streptococcal and gonococcal septic arthritis tured from the bloodstream. Blood cultures er, the study did not specifically address sit-
has declined over the past few decades. Gram- have been reported to be the only test to iden- uations in which imaging evidence of joint
negative rods typically affect elderly patients tify an organism in 9–14% of cases of septic fluid was completely absent. IV contrast ad-
and young IV drug users. Atypical mycobac- arthritis [1, 17]. ministration can reveal synovial enhance-
terial, viral, and fungal infections also occur, ment, abscesses, and epiphyseal involvement
particularly in immunosuppressed patients. Preaspiration Imaging in children but does not increase sensitiv-
Preaspiration imaging can aid evalua- ity or specificity for septic arthritis [22].
Serum Laboratory Evaluation tion of osseous structures and surrounding Preaspiration ultrasound (US) can help con-
Serum laboratory evaluation for septic soft tissues. Radiography is appropriate as firm the presence of a joint effusion (Fig. 3B)
arthritis includes peripheral WBC count, the first imaging study, particularly for pa- and assess for fluid collection in the overly-
erythrocyte sedimentation rate (ESR), and tients who have undergone prior surgery to ing soft tissues [23], although this approach
C-reactive protein (CRP) level. However, evaluate existing hardware [18]. Radiograph- is operator and resource dependent.
the results of these laboratory tests are in- ic findings are usually normal in early septic A potential argument ordering providers
adequately specific to substantially alter the arthritis or may reveal periarticular osteope- make against advanced preaspiration imag-
pretest probability of septic arthritis [8, 9]. nia. More advanced infections may present ing is concern over delaying definitive man-
Absence of leukocytosis or elevated ESR or with nonspecific erosions or uniform joint agement and causing progressive, irreversible
CRP level does not exclude a diagnosis of space narrowing [19, 20] (Figs. 2 and 3). cartilage loss. In animal models, cartilage
septic arthritis [10]. Measurement of procal- MRI is complementary to aspiration [18] loss is seen as early as 24 hours after joint
citonin has had diagnostic performance su- and can reveal a joint effusion or deep soft- infection, and permanent cartilage injury oc-
perior to that of traditional serum laborato- tissue infection. Nonspecific bony erosions, curs within 3–4 days [24]. Lauper et al. [25]
ry tests in assessing septic arthritis [11, 12]; marrow edema, and articular cartilage de- challenged the necessity of immediate surgi-
however, procalcitonin level is insufficient struction can be seen with septic arthri- cal lavage and found similar functional out-
to differentiate periprosthetic joint infection tis (Figs. 2B, 3D, and 3E) but also with in- comes among patients who underwent joint
(PJI) from aseptic loosening [13]. d-Dimer is
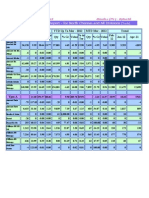
a promising serum biomarker for early de- TABLE 2: Sample Cutoff Values for Commonly Used Serum and Synovial
tection of PJI; the test had higher sensitivity Fluid Tests
and specificity than both ESR and CRP in
one study [14]. Unlike ESR and CRP levels, Sample Cutoff Value
d -Dimer level rapidly increases and returns Test Native Joint Chronic Periprosthetic Joint Infection
to baseline after elective total knee or hip ar-
Serum
throplasty, making it a potential tool in the
early detection of PJI [15]. Table 2 summa- WBC count (/µL) > 11,000
rizes commonly used cutoff values in stan- C-reactive protein level (mg/dL) >2 >1
dard serum laboratory evaluation. Erythrocyte sedimentation rate (mm/h) > 30 > 30
Although synovial fluid culture is consid-
Procalcitonin (ng/mL) > 0.3
ered the reference standard for diagnosing
septic arthritis [9], blood cultures can play d-Dimer level (ng/mL) > 860
a crucial role and are recommended as part Synovial fluid
of the initial diagnostic evaluation for sep- WBC count (/µL) > 50,000 > 3000
tic arthritis [16]. Hematogenous spread is the
Polymorphonuclear leukocytes (%) > 75 > 80
most common avenue of joint infection [8],
AJR:215, September 2020 569
Chan et al.
lavage less than 6, 6–12, 12–24, and more of shoulder PJIs [34], in which sebum-rich can present with irritability and listlessness,
than 24 hours after presentation. The need hair follicles in the axilla likely promote col- whereas toddlers may acknowledge nonspe-
for urgent intervention is balanced by the onization [35]. Organisms are typically en- cific pain [52]. Physical examination may re-
risk of missing unexpected pathologic condi- meshed in a biofilm covering the prosthesis, veal guarding, limited range of motion, and
tions. Patients without preoperative imaging which protects them from the host immune inability to bear weight. Laboratory evalua-
who are later discovered to harbor extraartic- system and antibiotics [36]. These charac- tion is likewise limited; leukocytosis is less
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
ular infection may need repeat operations to teristics make PJI a difficult clinical diagno- common in younger children and rare in ne-
rectify inadequate treatment [24, 26]. Abbre- sis. Several subspecialty societies have de- onates [52]. Kocher et al. [46] identified four
viated MRI protocols entailing solely fluid- veloped diagnostic criteria and algorithms criteria—history of fever, inability to bear
sensitive sequences are highly sensitive for to facilitate evaluation [37–40], and the Sec- weight, WBC count greater than 12,000/μL,
musculoskeletal abnormalities [27, 28] and ond International Consensus Meeting on Or- and ESR greater than 40 mm/h—to differen-
may shorten the delay to treatment while still thopedic Infections was convened to provide tiate septic arthritis from transient synovitis.
enabling comprehensive preoperative evalu- expert consensus given the heterogeneity in Another study [53] applying the criteria pro-
ation. Ultimately, the decision to perform im- practice [41]. Recommendations in these var- posed by Kocher et al. did not reproduce the
aging before aspiration should be based on ious guidelines were recently assessed to es- originally reported high predictive value.
an individualized assessment and discussion tablish updated, evidence-based diagnostic A threshold CRP greater than 2.0 mg/dL
with orthopedic colleagues. criteria and algorithms for the evaluation of has been found to have higher predictive val-
PJI [42] (Fig. 4). Elevation of either ESR or ue for septic arthritis than does leukocytosis,
Special Considerations CRP level should prompt joint aspiration; if elevated ESR, or refusal to bear weight [45].
Prosthetic joints—Suspected PJI in a pa- both ESR and CRP levels are within normal Additionally, Kingella kingae, an increas-
tient in hemodynamically stable condition limits, PJI is extremely unlikely [39]. Given ingly recognized cause of septic arthritis in
does not require immediate aspiration be- that PJIs are characterized by sessile rather children younger than 4 years [54, 55], has
cause of the absence of cartilage [29]. How- than free-floating bacteria, blood cultures are a milder clinical course often mistaken for
ever, PJI should be considered urgent and not included in the definition of PJI. a noninfectious pathologic condition and is
is a major cause of postarthroplasty failure Radiographs may reveal periprosthetic os- notoriously difficult to detect with standard
and ongoing pain. PJI can be acute or chron- teolysis but are frequently normal [43]. Al- laboratory techniques [56]. The addition of
ic; traditionally, these were differentiated by though radiographic findings are nonspecific oropharyngeal swabs and polymerase chain
amount of time elapsed since surgery (for ex- in the early postoperative period, radiographic reaction assays for K. kingae can help iden-
ample, acute infections occurring within 4 evidence of soft-tissue gas more than 14 days tify the causative organism in osteoarticular
weeks of surgery [30]). It is now agreed that after total knee arthroplasty was predictive of infections [56].
PJI is a continuum that culminates in estab- early PJI in a recent study [44] and may her- Children with septic arthritis often have
lishment of a chronic biofilm, and the time to ald a broader spectrum of microorganisms concomitant osteomyelitis and adjacent mus-
biofilm maturity depends on both the bacte- than typically encountered. Triple-phase bone culoskeletal infections [57–59], in part due
rial species and the host [31]. Chronic PJI is scintigraphy and WBC scintigraphy are high- to anatomic differences that facilitate spread
more common and often presents with pain ly sensitive for infection and can be useful in of osteomyelitis into the adjacent joint. Ro-
or functional deterioration [32]. Unlike the confounding cases. PJI is highly unlikely in bust transphyseal vessels in neonates al-
situation with aseptic prosthetic loosening, the absence of radiotracer uptake [40]. Hybrid low communication of the metaphysis with
pain is unrelated to activity and is present imaging techniques such as 18F-FDG PET/CT the adjacent nonossified epiphysis and joint.
at rest. Overt signs, such as fever, regional and 99mTc-antigranulocyte SPECT/CT can be After these vessels involute in early child-
warmth, and erythema, are frequently ab- used to improve localization of radiotracer up- hood, the metaphysis remains intraarticular
sent. A more specific sign of PJI is evidence take, although their lack of specificity limits in some long bones (e.g., proximal humer-
of deep soft-tissue involvement, including a their routine use at our institution. MRI and us and radius, proximal femur, distal fibula),
sinus tract, purulence, abscess, or extensive CT are not routinely advocated for PJI, be- and metaphyseal subperiosteal infection or
necrosis. Patients with multiple prosthetic cause aspiration and culture are needed re- abscess can progress to deposition of puru-
joints found to have one infected prosthe- gardless of advanced imaging findings (Fig. 5). lent material within the joint [60]. Schallert
sis are at increased risk of a second PJI, and Children—Clinical tools have been inves- et al. [61] found that 75% (41/55) of children
clinical assessment of all prosthetic joints is tigated for differentiating septic arthritis from with metaphyseal osteomyelitis and adjacent
important to determine the need for addi- similarly presenting nonsurgical pediatric di- joint effusion ultimately were found to have
tional aspirations [33]. agnoses, such as juvenile idiopathic arthritis, surgically confirmed septic arthritis. Those
Compared with septic arthritis in native transient synovitis, and Lyme disease [45–50]. authors concluded that children with joint
joints, PJIs are often characterized by less Slipped capital femoral epiphysis and Legg- effusions associated with metaphyseal osteo-
virulent pathogens: 50–60% of hip and knee Calve-Perthes disease are other important di- myelitis should be presumed to have septic
PJIs are caused by S. aureus and coagulase- agnostic considerations in pediatric patients arthritis [61].
negative staphylococci (e.g., Staphylococcus with hip pain. Trauma is an additional con- Rosenfeld et al. [26] proposed an algo-
epidermidis). In the upper extremity, coagu- founder; recent falls precede approximately rithm including five clinical and laboratory
lase-negative staphylococci account for ap- 20% of osteoarticular infections [51]. variables to identify patients at high risk of
proximately 40% of shoulder and elbow PJIs. Communication barriers may preclude a adjacent infections who could benefit from
Propionibacterium acnes is present in 24% comprehensive patient interview. Neonates preoperative MRI, although the generaliz-
570 AJR:215, September 2020
Septic Arthritis
ability of these criteria to other populations Recent antibiotic administration—Simi- Seeding of a sterile joint in patients with
has been questioned [62]. Investigators in lar to the situation with blood cultures [78], bacteremia is a theoretic risk. In a rabbit
several studies [63–65] and 88% of Interna- the yield of synovial fluid cultures decreases model, Olney et al. [86] found that septic ar-
tional Consensus Meeting delegates advocate after antibiotic administration. Barrack et al. thritis developed in 30% of animals if blood
percutaneous or open juxtaarticular bone bi- [79] found that 7 of 12 patients (58%) tak- drawn from a rabbit with bacteremia was in-
opsy at the time of aspiration in children to ing antibiotics who had no growth at initial jected directly into the joint. However, given
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
confirm the diagnosis of osteomyelitis and knee aspirations ultimately had a diagnosis that most cases of septic arthritis in adults
increase sensitivity for an organism when sy- of septic arthritis. Hindle et al. [80] found a are caused by hematogenous spread, patients
novial fluid culture results are negative. combined decrease in synovial fluid culture with septic arthritis presumably have con-
Immunosuppression—Immunosuppres- sensitivity from 79% to 28% in both native current bacteremia.
sion is a relative risk factor for septic arthri- and prosthetic knee aspirates after antibiotic
tis and is associated with many chronic condi- administration. Despite the lower diagnostic Aspiration Considerations
tions, including diabetes mellitus, rheumatoid value of microbiologic analysis after recent Routine approaches to image-guided joint
arthritis, and HIV infection [66]. Anti–tumor antibiotic use, no guidelines have been estab- access are well described in the literature
necrosis factor therapy in patients with rheu- lished regarding duration of antibiotic cessa- [70, 87]; however, in patients with infection
matoid arthritis doubles the risk of septic ar- tion before arthrocentesis. At our institution or altered anatomy, the standard approach
thritis [7]. Other medications, such as cortico- we do not typically defer joint aspiration af- may present undesirable risks. Planning the
steroids and disease-modifying antirheumatic ter recent antibiotic administration. optimal aspiration for an individual joint in-
drugs, may also induce an immunocompro- In the setting of prior arthroplasty, a lon- cludes assessment of body habitus and visual
mised state. Immunosuppressed patients can ger interval between antibiotic cessation and inspection for signs of soft-tissue infection.
have an atypical presentation of a blunted pain aspiration can increase the likelihood of cul- Review of preaspiration imaging can reveal
response [67]. Immunosuppressed patients ture positivity. Malekzadeh et al. [81] deter- normal structures susceptible to damage,
also have theoretic differences in laboratory mined that antimicrobial therapy within 3 soft-tissue infection, intervening obstacles,
values due to difficulty mounting a normal months was associated with increased likeli- and osseous changes. Limitations in patient
immune response. Butler et al. [68], howev- hood of culture-negative PJI (odds ratio, 4.7). positioning may necessitate a nonstandard
er, found no significant difference in labora- Both American Academy of Orthopedic Sur- approach. Larger (e.g., 18- or 20-gauge) nee-
tory values between immunosuppressed and gery [39] and Infectious Disease Society of dles are typically used for ease of aspirating
immunocompetent patients with septic arthri- America [38] guidelines call for withhold- thick purulent fluid.
tis. Notably, procalcitonin levels are unaffect- ing antibiotics for at least 2 weeks before at-
ed by steroids [69] and may be a helpful bio- tempting joint aspiration in patients with sus- Choosing an Imaging Modality for
marker in this population. pected PJI. Needle Guidance
Overlying cellulitis and other concomitant Selecting the ideal imaging modality for
Possible Contraindications to Percutaneous infections—A dreaded risk of arthrocente- needle guidance relies on several factors, in-
Aspiration sis is inducing septic arthritis in a previously cluding patient age, body habitus, suspected
Anticoagulation—There is little consen- aseptic joint. Rates of septic arthritis after in- pathologic condition, and the radiologist’s
sus in the literature [70] or anecdotally [3] re- traarticular steroid injection are as low as 1 in expertise in anatomy and percutaneous tech-
garding the handling of anticoagulation be- 10,000 [82, 83]. Although intuitively the pres- niques. Although anticipated radiation dos-
fore arthrocentesis. Porrino et al. [3] reported ence of overlying cellulitis increases the risk es are low, the radiologist should adhere to
that 39% (96/247) of surveyed radiologists of inducing septic arthritis, there is an absence the goal of achieving as low as reasonably
agreed that coagulopathy should be correct- of literature confirming the risk of seeding a achievable radiation. Other influential fac-
ed before arthrocentesis. However, the avail- sterile joint with a needle that has traversed a tors include availability of equipment and
able literature supports the notion that clini- soft-tissue infection [33]. Despite this, there is ancillary staff, characteristics of the collec-
cally significant bleeding complications after no shortage of expert opinions endorsing [23, tion, and site of aspiration.
both blind and image-guided arthrocentesis 70, 84] and discounting [33, 85] cellulitis as a Fluoroscopic guidance is frequently used
in patients undergoing anticoagulation are ex- relative contraindication to arthrocentesis. A for joint access and may be preferred be-
ceedingly rare [71–74]. A 2017 retrospective best attempt should be made to select a nee- cause of operator proficiency, equipment
study [74] showed no bleeding complications dle entry point that avoids the overlying soft- availability, and decreased ionizing radiation
following 1050 consecutive procedures over 6 tissue infection, and deferring aspiration until relative to CT. Although soft-tissue and vas-
years on patients using direct oral anticoagu- the overlying infection is treated is a consid- cular structures are fluoroscopically occult,
lants (e.g., direct thrombin inhibitors and di- eration. However, given the lack of high-level knowledge of basic anatomy can facilitate a
rect factor Xa inhibitors) during arthrocente- evidence, cellulitis is not considered an abso- needle approach that easily avoids major vas-
sis. In addition, there is a real risk of inciting lute contraindication [33]. Deeper soft-tissue cular structures.
thromboembolic events when interrupting an- infections (Figs. 6 and 7), such as abscess, US is useful for aspiration given its high
ticoagulation [75]. Overall, percutaneous joint bursitis, and pyomyositis, pose a greater chal- sensitivity for joint effusion [88] (Fig. 8).
access is considered low risk [76, 77], and at lenge. If fluoroscopic guidance is used for ar- Other advantages include lack of ionizing ra-
our institution we do not routinely discontinue throcentesis, the radiologist may be unaware diation, visualization of vascular structures,
anticoagulation or perform preprocedural co- before entering the joint that an infected col- differentiation of joint fluid from synovitis,
agulation tests before arthrocentesis. lection has been traversed. identification of extraarticular fluid collec-
AJR:215, September 2020 571
Chan et al.
tions [23], and ability to accommodate many reported to be bacteriostatic or bactericidal mended before routine performance of this
patient positions and approaches. Mobile US [91]. A 2018 study of common pathogens im- technique. Notably, aspirate obtained via sa-
units can be used for imaging of patients plicated in PJI [92] showed decreased growth line lavage will yield a dilute sample [99],
who are critically ill or in unstable condition in culture on exposure to 2% lidocaine. The and the aspirate should be clearly labeled to
for whom transport to the radiology depart- presence of preservatives in commercial avoid inaccurate cell counts.
ment may be impractical or unsafe. US al- preparations of lidocaine and other anes-
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
lows real-time needle visualization, which thetics enhances this antimicrobial effect Analysis of Aspirated Fluid
simplifies aspiration of thick or loculated [93]. Caution is advised during arthrocente- To prevent contamination, aspirate is of-
collections and avoids extraarticular collec- sis when instilling local anesthetics near the ten sent to the microbiology laboratory in the
tions. However, US depends greatly on both joint, and preservative-free lidocaine is pre- syringe used during the procedure. Howev-
operator and technologist comfort and skill. ferred to maximize organism yield. er, several studies [100–102] have shown in-
US also has limited capacity for evaluating creased pathogen yield when samples are in-
deeper structures and may be a poor choice Confirmation of Intraarticular Positioning oculated in blood culture bottles rather than
for imaging of obese patients. It is imperative to document intraarticular as conventional cultures on standard agar me-
Occasionally, sonographic and fluoro- needle tip positioning, most importantly in dia. Although the minimum amount of requi-
scopic guidance may show insufficient ana- the setting of a so-called dry tap to confirm site fluid varies by institution, small volumes
tomic detail for joint access. CT may be the the absence of obtainable fluid. Intraarticular of aspirate can be sufficient for fluid analysis.
preferred or safer modality, particularly in positioning can be determined in real time if Our microbiology laboratory requires a mini-
cases of irregular bony anatomy, presence of US is used for guidance. In the setting of flu- mal sample for culture and as little as 0.5 mL
extensive heterotopic ossification, or proxim- oroscopic guidance, contrast instillation after to determine cell count and differential.
ity of sensitive structures, such as mediasti- aspiration can verify intraarticular needle po- Standard synovial fluid analysis includes
nal vasculature. sitioning. Spread of iodinated contrast mate- culture and cell count and differential; crys-
rial (Fig. 3C) can show intraarticular commu- tal analysis is also often performed in the as-
Choosing the Approach nication with fluid collections, bursae, or sinus sessment of native joints in adults [103–106].
Patients with osseous deficiency (e.g., ex- tracts. In prior studies, investigators have ex- However, synovial WBC and polymorphonu-
tensive erosive change, prior surgery) may pressed concern over the bactericidal effects clear leukocyte counts may remain elevated
not have typical landmarks for joint access of iodinated contrast material if inadvertently as long as 90 days after arthroplasty [107].
(Fig. 9). Preaspiration imaging can delineate mixed with aspirated fluid, but this effect has Additionally, cutoff values for abnormal sy-
the confines of the altered joint capsule. The not been found with modern low-osmolar and novial WBC count and polymorphonuclear
osseous void in the expected location of the isoosmolar contrast agents [94]. Air contrast percentage appear to vary for different joint
joint space can be targeted, although lack of (Fig. 10B) is a cost-free alternative in patients sites [108, 109]. Table 2 includes potential
a tactile backstop forces the operator to es- with allergies to iodinated contrast material cutoff values for common synovial fluid tests
timate the appropriate needle depth. Famil- [95] but will introduce susceptibility artifacts to assess for infection in both native and pros-
iarity with anatomic alterations after surgery if MRI is subsequently performed. thetic joints. The presence of an adverse lo-
can be helpful in defining new approaches. cal tissue reaction can lead to falsely elevated
For example, in patients with a history of Deciding Whether to Perform Lavage synovial WBC counts and α-defensin levels,
Girdlestone arthroplasty, one potential target There is considerable debate regarding and intraoperative purulence can be present
for access is the midpoint of a line drawn be- the role of joint lavage and reaspiration af- with either adverse local tissue reaction or PJI
tween the greater and lesser trochanters [89]. ter initial failure to aspirate fluid. Kung et [33]. Samples should be incubated for at least
In patients who have previously undergone al. [96] described a hip lavage technique 14–21 days to isolate slow-growing organ-
arthroplasty, slight alterations to routine ap- involving injection of 10 mL of iodinat- isms associated with PJI [110]. Gram stain-
proaches can prevent overlapping metallic ed contrast material or sterile nonbacterio- ing is historically performed but has low di-
structures from obscuring the needle tip dur- static saline solution with average return of agnostic performance; the false-negative rate
ing fluoroscopic guidance. A frequently suc- 2.3 mL at reaspiration. Several studies have was 78% (111/143) in one study [111].
cessful technique for aspirating a total hip shown positive organism recovery by use Additional biomarkers may be beneficial
prosthesis is to advance the needle until it of percutaneous joint lavage [96–98], and a in equivocal cases. The most promising sy-
contacts the lateral aspect of the neck of the 2018 study in the orthopedic literature [97] novial biomarker at present appears to be
femoral stem component and then direct the showed similar performance between pri- α-defensin [112], which is an antimicrobial
tip laterally off the component into the more mary joint aspiration and reaspirated sa- peptide released by neutrophils in response to
dependent portion of the joint (Fig. 5C) [90]. line solution after dry tap in the diagnosis infection and is detectable with the Synova-
Familiarity with the construction of the un- of PJI. Consensus statements generally ad- sure PJI test (Zimmer Biomet). Deirmengian
derlying hardware can aid intraarticular nee- vise against saline lavage but are somewhat et al. [113] reported that use of the combina-
dle tip positioning, such as with a reverse to- ambiguous; 83% of International Consensus tion of synovial α-defensin and CRP detect-
tal shoulder prosthesis (Fig. 10). Meeting delegates opposed the use of sa- ed with immunoassay led to correct diagno-
line lavage but specified that performance ses of asepsis or infection in 99% of cases.
Local Anesthesia by a radiologist was a possible exception Leukocyte esterase reagent strips can provide
Several commonly used agents for local [33]. Given the degree of uncertainty, dis- a rapid estimate of synovial WBC count and
anesthesia, including lidocaine, have been cussion with orthopedic surgeons is recom- have been included in diagnostic algorithms
572 AJR:215, September 2020
Septic Arthritis
[114]. Newer molecular techniques, such as surgery, and other providers to maximize promising for the diagnosis of periprosthetic
polymerase chain reaction [115], microarray positive patient outcomes. joint infection and timing of reimplanta-
analysis [116], and next-generation sequenc- tion. J Bone Joint Surg Am 2017; 99:1419–1427
ing [117], are promising but require further References 15. Lee YS, Lee YK, Han SB, Nam CH, Parvizi J,
validation before widespread adoption. 1. Cooper C, Cawley MI. Bacterial arthritis in an Koo KH. Natural progress of D-dimer following
English health district: a 10 year review. Ann total joint arthroplasty: a baseline for the diagno-
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
Dealing With Suspected False- Rheum Dis 1986; 45:458–463 sis of the early postoperative infection. J Orthop
Negative Results 2. Chiappini E, Mastrolia MV, Galli L, De Martino Surg Res 2018; 13:36
A negative aspiration result (either dry M, Lazzeri S. Septic arthritis in children in re- 16. Coakley G, Mathews C, Field M, et al.; British
tap or bland fluid) in a patient with suspect- source limited and non-resource limited coun- Society for Rheumatology Standards, Guidelines
ed septic arthritis presents a clinical dilem- tries: an update on diagnosis and treatment. and Audit Working Group. BSR & BHPR, BOA,
ma. Patients with clinically suspected septic Expert Rev Anti Infect Ther 2016; 14:1087–1096 RCGP and BSAC guidelines for management of
arthritis but culture-negative synovial fluid 3. Porrino J, Richardson ML, Flaherty E, et al. Septic the hot swollen joint in adults. Rheumatology
have outcomes similar to those of patients arthritis and joint aspiration: the radiologist’s role (Oxford) 2006; 45:1039–1041
with confirmed septic arthritis, supporting in image-guided aspiration for suspected septic 17. Weston VC, Jones AC, Bradbury N, Fawthrop F,
the rationale for treating patients as having arthritis. Semin Roentgenol 2019; 54:177–189 Doherty M. Clinical features and outcome of
presumptive septic arthritis even in the ab- 4. Ross JJ. Septic arthritis of native joints. Infect septic arthritis in a single UK Health District
sence of confirmatory study results [118]. Dis Clin North Am 2017; 31:203–218 1982-1991. Ann Rheum Dis 1999; 58:214–219
Several consensus statements endorse re- 5. Kaandorp CJ, Dinant HJ, van de Laar MA, 18. Beaman FD, von Herrmann PF, Kransdorf MJ, et
peat aspiration for suspected hip PJI [33, 39]. Moens HJ, Prins AP, Dijkmans BA. Incidence al.; Expert Panel on Musculoskeletal Imaging.
The frequency of surgery for suspected PJI and sources of native and prosthetic joint infec- ACR Appropriateness Criteria® suspected osteo-
on patients with negative aspiration and pos- tion: a community based prospective survey. Ann myelitis, septic arthritis, or soft tissue infection
itive intraoperative culture results was 22% Rheum Dis 1997; 56:470–475 (excluding spine and diabetic foot). J Am Coll
(219/996) in one large institutional retrospec- 6. Doran MF, Crowson CS, Pond GR, O’Fallon Radiol 2017; 14(5 suppl):S326–S337
tive review [119]. Another recent review re- WM, Gabriel SE. Frequency of infection in pa- 19. Rousseau I, Cardinal EE, Raymond-Tremblay D,
vealed that repeat prosthetic hip joint aspira- tients with rheumatoid arthritis compared with Beauregard CG, Braunstein EM, Saint-Pierre A.
tion within 90 days of the initial aspiration controls: a population-based study. Arthritis Gout: radiographic findings mimicking infec-
changed the diagnosis for 43% of patients Rheum 2002; 46:2287–2293 tion. Skeletal Radiol 2001; 30:565–569
(26/60) [120]. 7. Galloway JB, Hyrich KL, Mercer LK, et al.; BSR 20. Santiago Restrepo C, Giménez CR, McCarthy K.
Despite uncertainty over the reliability of Biologics Register. Risk of septic arthritis in pa- Imaging of osteomyelitis and musculoskeletal
culture-negative aspiration results, there are tients with rheumatoid arthritis and the effect of soft tissue infections: current concepts. Rheum
no guidelines for the recommended time in- anti-TNF therapy: results from the British Soci- Dis Clin North Am 2003; 29:89–109
terval between or optimal number of repeat ety for Rheumatology Biologics Register. Ann 21. Graif M, Schweitzer ME, Deely D, Matteucci T.
aspirations, and whether aspiration should Rheum Dis 2011; 70:1810–1814 The septic versus nonseptic inflamed joint: MRI
be repeated should be driven by discussion 8. Carpenter CR, Schuur JD, Everett WW, Pines characteristics. Skeletal Radiol 1999; 28:616–620
between the radiologist and orthopedic sur- JM. Evidence-based diagnostics: adult septic ar- 22. Safdar NM, Rigsby CK, Iyer RS, et al.; Expert
geon. Percutaneous synovial biopsy may thritis. Acad Emerg Med 2011; 18:781–796 Panel on Pediatric Imaging. ACR Appropriateness
have a role in this population. Coiffier et al. 9. Margaretten ME, Kohlwes J, Moore D, Bent S. Criteria® acutely limping child up to age 5. J Am
[121] found that 27% (3/11) of patients with Does this adult patient have septic arthritis? Coll Radiol 2018; 15(11 suppl):S252–S262
acute arthritis and inadequate synovial fluid JAMA 2007; 297:1478–1488 23. Hadduck TA, van Holsbeeck MT, Girish G, et al.
for analysis had positive culture results after 10. Gupta MN, Sturrock RD, Field M. A prospective Value of ultrasound before joint aspiration. AJR
US-guided synovial biopsy. 2-year study of 75 patients with adult-onset septic 2013; 201:[web]W453–W459
arthritis. Rheumatology (Oxford) 2001; 40:24–30 24. Monsalve J, Kan JH, Schallert EK, Bisset GS,
Conclusion 11. Chouk M, Verhoeven F, Sondag M, Guillot X, Zhang W, Rosenfeld SB. Septic arthritis in
Despite the urgency associated with a di- Prati C, Wendling D. Value of serum procalcito- children: frequency of coexisting unsuspected
agnosis of septic arthritis, there remains a nin for the diagnosis of bacterial septic arthritis osteomyelitis and implications on imaging work-
lack of high-level evidence regarding many in daily practice in rheumatology. Clin Rheuma- up and management. AJR 2015; 204:1289–1295
aspects of management of native and peri- tol 2019; 38:2265–2273 25. Lauper N, Davat M, Gjika E, et al. Native septic
prosthetic joint infections. This results in 12. Zhao J, Zhang S, Zhang L, et al. Serum procalci- arthritis is not an immediate surgical emergency.
a heterogeneous approach to arthrocente- tonin levels as a diagnostic marker for septic ar- J Infect 2018; 77:47–53
sis across different practice settings. Under- thritis: a meta-analysis. Am J Emerg Med 2017; 26. Rosenfeld S, Bernstein DT, Daram S, Dawson J,
standing the current literature will help the 35:1166–1171 Zhang W. Predicting the presence of adjacent in-
radiologist discuss challenging cases with 13. Barrack R, Bhimani S, Blevins JL, et al. General fections in septic arthritis in children. J Pediatr
ordering providers and adopt an evidence- assembly, diagnosis, laboratory test: proceedings Orthop 2016; 36:70–74
based approach to joint aspiration. Ulti- of International Consensus on Orthopedic Infec- 27. Markhardt BK, Woo K, Nguyen JC. Evaluation
mately, the best approach will be institution tions. J Arthroplasty 2019; 34(2 suppl):S187–S195 of suspected musculoskeletal infection in
dependent and require interdisciplinary col- 14. Shahi A, Kheir MM, Tarabichi M, Hosseinzadeh children over 2 years of age using only fluid-
laboration between radiology, orthopedic HRS, Tan TL, Parvizi J. Serum D-dimer test is sensitive sequences at MRI. Eur Radiol 2019;
AJR:215, September 2020 573
Chan et al.
29:5682–5690 troduction: proceedings of International Consen- 54. Basmaci R, Lorrot M, Bidet P, et al. Comparison
28. Nguyen JC, Yi PH, Woo KM, Rosas HG. Detec- sus on Orthopedic Infections. J Arthroplasty of clinical and biologic features of Kingella
tion of pediatric musculoskeletal pathology using 2019; 34(2 suppl):S1–S2 kingae and Staphylococcus aureus arthritis at
the fluid-sensitive sequence. Pediatr Radiol 42. Shohat N, Tan TL, Della Valle CJ, et al. Develop- initial evaluation. Pediatr Infect Dis J 2011;
2019; 49:114–121 ment and validation of an evidence-based algo- 30:902–904
29. Luthringer TA, Fillingham YA, Okroj K, Ward rithm for diagnosing periprosthetic joint infec- 55. Chometon S, Benito Y, Chaker M, et al. Specific
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
EJ, Della Valle C. Periprosthetic joint infection tion. J Arthroplasty 2019; 34:2730–2736 real-time polymerase chain reaction places
after hip and knee arthroplasty: a review for 43. Tigges S, Stiles RG, Roberson JR. Appearance of Kingella kingae as the most common cause of
emergency care providers. Ann Emerg Med 2016; septic hip prostheses on plain radiographs. AJR osteoarticular infections in young children. Pedi-
68:324–334 1994; 163:377–380 atr Infect Dis J 2007; 26:377–381
30. McPherson EJ, Woodson C, Holtom P, Roidis N, 44. Li N, Kagan R, Hanrahan CJ, Hansford BG. Ra- 56. Ceroni D, Cherkaoui A, Ferey S, Kaelin A,
Shufelt C, Patzakis M. Periprosthetic total hip diographic evidence of soft-tissue gas 14 days Schrenzel J. Kingella kingae osteoarticular in-
infection: outcomes using a staging system. Clin after total knee arthroplasty is predictive of early fections in young children: clinical features and
Orthop Relat Res 2002; 403:8–15 prosthetic joint infection. AJR 2020; 214:171–176 contribution of a new specific real-time PCR as-
31. Elkins JM, Kates S, Lange J, et al. General as- 45. Caird MS, Flynn JM, Leung YL, Millman JE, say to the diagnosis. J Pediatr Orthop 2010;
sembly, diagnosis, definitions: proceedings of In- D’Italia JG, Dormans JP. Factors distinguishing 30:301–304
ternational Consensus on Orthopedic Infections. septic arthritis from transient synovitis of the hip 57. Chen WL, Chang WN, Chen YS, et al. Acute
J Arthroplasty 2019; 34(2 suppl):S181–S185 in children: a prospective study. J Bone Joint community-acquired osteoarticular infections in
32. Tsaras G, Osmon DR, Mabry T, et al. Incidence, Surg Am 2006; 88:1251–1257 children: high incidence of concomitant bone
secular trends, and outcomes of prosthetic joint 46. Kocher MS, Zurakowski D, Kasser JR. Differen- and joint involvement. J Microbiol Immunol
infection: a population-based study, Olmsted tiating between septic arthritis and transient sy- Infect 2010; 43:332–338
County, Minnesota, 1969–2007. Infect Control novitis of the hip in children: an evidence-based 58. Montgomery CO, Siegel E, Blasier RD, Suva LJ.
Hosp Epidemiol 2012; 33:1207–1212 clinical prediction algorithm. J Bone Joint Surg Concurrent septic arthritis and osteomyelitis in
33. Abdel Karim M, Andrawis J, Bengoa F, et al. Hip Am 1999; 81:1662–1670 children. J Pediatr Orthop 2013; 33:464–467
and knee section, diagnosis, algorithm: proceedings 47. Aupiais C, Basmaci R, Ilharreborde B, et al. Ar- 59. Nguyen A, Kan JH, Bisset G, Rosenfeld S. Kocher
of International Consensus on Orthopedic Infec- thritis in children: comparison of clinical and criteria revisited in the era of MRI: how often does
tions. J Arthroplasty 2019; 34(2 suppl):S339–S350 biological characteristics of septic arthritis and the Kocher criteria identify underlying osteomyeli-
34. Tande AJ, Patel R. Prosthetic joint infection. Clin juvenile idiopathic arthritis. Arch Dis Child tis? J Pediatr Orthop 2017; 37:e114–e119
Microbiol Rev 2014; 27:302–345 2017; 102:316–322 60. Perlman MH, Patzakis MJ, Kumar PJ, Holtom P.
35. Arain AR, Sullivan CW, Angelicola-Richardson 48. Baldwin KD, Brusalis CM, Nduaguba AM, The incidence of joint involvement with adjacent
K, Haddad S, Rosenbaum A. Indolent Propioni- Sankar WN. Predictive factors for differentiating osteomyelitis in pediatric patients. J Pediatr
bacterium acnes infection associated with ortho- between septic arthritis and Lyme disease of the Orthop 2000; 20:40–43
pedic hardware in the ankle: a case report and lit- knee in children. J Bone Joint Surg Am 2016; 61. Schallert EK, Kan JH, Monsalve J, Zhang W,
erature review. Clin Case Rep 2019; 7:1494–1498 98:721–728 Bisset GS 3rd, Rosenfeld S. Metaphyseal osteo-
36. Ciofu O, Rojo-Molinero E, Macià MD, Oliver A. 49. Cruz AI Jr, Anari JB, Ramirez JM, Sankar WN, myelitis in children: how often does MRI-docu-
Antibiotic treatment of biofilm infections. Baldwin KD. Distinguishing pediatric Lyme ar- mented joint effusion or epiphyseal extension of
A PMIS 2017; 125:304–319 thritis of the hip from transient synovitis and edema indicate coexisting septic arthritis?
37. Parvizi J, Zmistowski B, Berbari EF, et al. New defi- acute bacterial septic arthritis: a systematic re- Pediatr Radiol 2015; 45:1174–1181
nition for periprosthetic joint infection: from the view and meta-analysis. Cureus 2018; 10:e2112 62. Refakis CA, Arkader A, Baldwin KD, Spiegel
Workgroup of the Musculoskeletal Infection Soci- 50. Deanehan JK, Kimia AA, Tan Tanny SP, et al. DA, Sankar WN. Predicting periarticular infec-
ety. Clin Orthop Relat Res 2011; 469:2992–2994 Distinguishing Lyme from septic knee monoar- tion in children with septic arthritis of the hip:
38. Osmon DR, Berbari EF, Berendt AR, et al.; In- thritis in Lyme disease-endemic areas. Pediatrics regionally derived criteria may not apply to all
fectious Diseases Society of America. Diagnosis 2013; 131:e695–e701 populations. J Pediatr Orthop 2019; 39:268–274
and management of prosthetic joint infection: 51. Pääkkönen M, Kallio MJ, Lankinen P, Peltola H, 63. Schmale GA, Bompadre V. Aspirations of the il-
clinical practice guidelines by the Infectious Dis- Kallio PE. Preceding trauma in childhood hema- ium and proximal femur increase the likelihood
eases Society of America. Clin Infect Dis 2013; togenous bone and joint infections. J Pediatr Or- of culturing an organism in patients with pre-
56:e1–e25 thop B 2014; 23:196–199 sumed septic arthritis of the hip. J Child Orthop
39. American Academy of Orthopaedic Surgeons 52. Kang SN, Sanghera T, Mangwani J, Paterson JM, 2015; 9:313–318
website. Diagnosis and prevention of peripros- Ramachandran M. The management of septic ar- 64. Schlung JE, Bastrom TP, Roocroft JH, Newton
thetic joint infections clinical practice guideline. thritis in children: systematic review of the Eng- PO, Mubarak SJ, Upasani VV. Femoral neck
www.aaos.org/pjiguideline. Published March 11, lish language literature. J Bone Joint Surg Br aspiration aids in the diagnosis of osteomyelitis
2019. Accessed November 19, 2019 2009; 91:1127–1133 in children with septic hip. J Pediatr Orthop
40. Signore A, Sconfienza LM, Borens O, et al. Con- 53. Luhmann SJ, Jones A, Schootman M, Gordon 2018; 38:532–536
sensus document for the diagnosis of prosthetic JE, Schoenecker PL, Luhmann JD. Differentia- 65. Cooper AM, Shope AJ, Javid M, Parsa A, Chinoy
joint infections: a joint paper by the EANM, tion between septic arthritis and transient syno- MA, Parvizi J. Musculoskeletal infection in pe-
EBJIS, and ESR (with ESCMID endorsement). vitis of the hip in children with clinical predic- diatrics: assessment of the 2018 international
Eur J Nucl Med Mol Imaging 2019; 46:971–988 tion algorithms. J Bone Joint Surg Am 2004; consensus meeting on musculoskeletal infec-
41. Parvizi J, Gehrke T, Mont MA, Callaghan JJ. In- 86:956–962 tion. J Bone Joint Surg Am 2019; 101:e133
574 AJR:215, September 2020
Septic Arthritis
66. Saraux A, Taelman H, Blanche P, et al. HIV in- of antibiotic administration on blood culture MJ. In vitro study of the antimicrobial effects of
fection as a risk factor for septic arthritis. Br J positivity at the beginning of sepsis: a prospec- radiological contrast agents used in arthrogra-
Rheumatol 1997; 36:333–337 tive clinical cohort study. Clin Microbiol Infect phy. J Bone Joint Surg Br 2011; 93:126–130
67. Edwards SA, Cranfield T, Clarke HJ. Atypical 2019; 25:326–331 95. Shahid M, Shyamsundar S, Bali N, McBryde C,
presentation of septic arthritis in the immunosup- 79. Barrack RL, Jennings RW, Wolfe MW, Bertot O’Hara J, Bache E. Efficacy of using an air ar-
pressed patient. Orthopedics 2002; 25:1089–1090 AJ. The Coventry Award: the value of preopera- throgram for EUA and injection of the hip joint
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
68. Butler BA, Fitz DW, Lawton CD, Li DD, tive aspiration before total knee revision. Clin in adults. J Orthop 2014; 11:132–135
Balderama ES, Stover MD. Early diagnosis of Orthop Relat Res 1997; 345:8–16 96. Kung JW, Yablon C, Huang ES, Hennessey H,
septic arthritis in immunocompromised pa- 80. Hindle P, Davidson E, Biant LC. Septic arthritis Wu JS. Clinical and radiologic predictive factors
tients. J Orthop Sci 2018; 23:542–545 of the knee: the use and effect of antibiotics prior of septic hip arthritis. AJR 2012; 199:868–872
69. Perren A, Cerutti B, Lepori M, et al. Influence of to diagnostic aspiration. Ann R Coll Surg Engl 97. Partridge DG, Winnard C, Townsend R, Cooper R,
steroids on procalcitonin and C-reactive protein 2012; 94:351–355 Stockley I. Joint aspiration, including culture of
in patients with COPD and community-acquired 81. Malekzadeh D, Osmon DR, Lahr BD, Hanssen reaspirated saline after a ‘dry tap’, is sensitive and
pneumonia. Infection 2008; 36:163–166 AD, Berbari EF. Prior use of antimicrobial thera- specific for the diagnosis of hip and knee prosthetic
70. Hansford BG, Stacy GS. Musculoskeletal aspira- py is a risk factor for culture-negative prosthetic joint infection. Bone Joint J 2018; 100-B:749–754
tion procedures. Semin Intervent Radiol 2012; joint infection. Clin Orthop Relat Res 2010; 98. Ali F, Wilkinson JM, Cooper JR, et al. Accuracy
29:270–285 468:2039–2045 of joint aspiration for the preoperative diagnosis
71. Ahmed I, Gertner E. Safety of arthrocentesis and 82. Andreasen RA, Just SA, Hansen IMJ. of infection in total hip arthroplasty. J Arthro-
joint injection in patients receiving anticoagula- THU0299 the risk of intraarticular steroid injec- plasty 2006; 21:221–226
tion at therapeutic levels. Am J Med 2012; tions are overestimated. Ann Rheum Dis 2014; 99. Newman JM, George J, Klika AK, et al. What is
125:265–269 73:286–287 the diagnostic accuracy of aspirations performed
72. Bashir MA, Ray R, Sarda P, Li S, Corbett S. De- 83. Hunter JA, Blyth TH. A risk-benefit assessment on hips with antibiotic cement spacers? Clin
termination of a safe INR for joint injections in of intra-articular corticosteroids in rheumatic Orthop Relat Res 2017; 475:204–211
patients taking warfarin. Ann R Coll Surg Engl disorders. Drug Saf 1999; 21:353–365 100. Hughes JG, Vetter EA, Patel R, et al. Culture with
2015; 97:589–591 84. Thomsen TW, Shen S, Shaffer RW, Setnik GS. BACTEC Peds Plus/F bottle compared with con-
73. Hugo PC 3rd, Newberg AH, Newman JS, Videos in clinical medicine: arthrocentesis of the ventional methods for detection of bacteria in sy-
Wetzner SM. Complications of arthrography. knee. N Engl J Med 2006; 354:e19 novial fluid. J Clin Microbiol 2001; 39:4468–4471
Semin Musculoskelet Radiol 1998; 2:345–348 85. Dooley DP. Aspiration of the possibly septic joint 101. Peel TN, Dylla BL, Hughes JG, et al. Improved
74. Yui JC, Preskill C, Greenlund LS. Arthrocente- through potential cellulitis: just do it! J Emerg diagnosis of prosthetic joint infection by cultur-
sis and joint injection in patients receiving direct Med 2002; 23:210 ing periprosthetic tissue specimens in blood cul-
oral anticoagulants. Mayo Clin Proc 2017; 86. Olney BW, Papasian CJ, Jacobs RR. Risk of iat- ture bottles. MBio 2016; 7:e01776
92:1223–1226 rogenic septic arthritis in the presence of bacte- 102. Geller JA, MacCallum KP, Murtaugh TS, Patrick
75. Garcia DA, Regan S, Henault LE, et al. Risk of remia: a rabbit study. J Pediatr Orthop 1987; DA Jr, Liabaud B, Jonna VK. Prospective com-
thromboembolism with short-term interruption 7:524–526 parison of blood culture bottles and conventional
of warfarin therapy. Arch Intern Med 2008; 87. Rastogi AK, Davis KW, Ross A, Rosas HG. Funda- swabs for microbial identification of suspected
168:63–69 mentals of joint injection. AJR 2016; 207:484–494 periprosthetic joint infection. J Arthroplasty
76. Narouze S, Benzon HT, Provenzano D, et al. In- 88. Zawin JK, Hoffer FA, Rand FF, Teele RL. Joint ef- 2016; 31:1779–1783
terventional spine and pain procedures in patients fusion in children with an irritable hip: US diagno- 103. Archibeck MJ, Rosenberg AG, Sheinkop MB,
on antiplatelet and anticoagulant medications sis and aspiration. Radiology 1993; 187:459–463 Berger RA, Jacobs JJ. Gout-induced arthropathy
(second edition): guidelines from the American 89. Swan JS, Braunstein EM, Capello W. Aspiration after total knee arthroplasty: a report of two cas-
Society of Regional Anesthesia and Pain Medi- of the hip in patients treated with Girdlestone ar- es. Clin Orthop Relat Res 2001; 392:377–382
cine, the European Society of Regional Anaesthe- throplasty. AJR 1991; 156:545–546 104. Buck M, Delaney M. Diagnosis and management
sia and Pain Therapy, the American Academy of 90. Brandser EA, El-Khoury GY, FitzRandolph RL. of gout in total knee arthroplasty. Orthop Nurs
Pain Medicine, the International Neuromodula- Modified technique for fluid aspiration from the 2014; 33:37–40
tion Society, the North American Neuromodula- hip in patients with prosthetic hips. Radiology 105. Fokter SK, Repse-Fokter A. Acute gouty arthri-
tion Society, and the World Institute of Pain. Reg 1997; 204:580–582 tis in a patient after total knee arthroplasty. Wien
Anesth Pain Med 2018; 43:225–262 91. Xu H, Zhang L, Arita H, Hanaoka K. Antimicro- Klin Wochenschr 2010; 122:366–367
77. Patel IJ, Rahim S, Davidson JC, et al. Society of bial activity of local anesthetics. Pain Res 2003; 106. McPherson RA, Pincus MR, Henry JB. Henry’s
Interventional Radiology consensus guidelines 18:19–24 clinical diagnosis and management by labora-
for the periprocedural management of throm- 92. Liu K, Ye L, Sun W, Hao L, Luo Y, Chen J. Does tory methods, 21st ed. Philadelphia, PA: Saun-
botic and bleeding risk in patients undergoing use of lidocaine affect culture of synovial fluid ders Elsevier, 2007
percutaneous image-guided interventions. Part obtained to diagnose periprosthetic joint infec- 107. Christensen CP, Bedair H, Della Valle CJ,
2. Recommendations: endorsed by the Canadian tion (PJI)? An in vitro study. Med Sci Monit Parvizi J, Schurko B, Jacobs CA. The natural
Association for Interventional Radiology and the 2018; 24:448–452 progression of synovial fluid white blood-cell
Cardiovascular and Interventional Radiological 93. Noda H, Saionji K, Miyazaki T. Antibacterial ac- counts and the percentage of polymorphonuclear
Society of Europe. J Vasc Interv Radiol 2019; tivity of local anesthetics [in Japanese]. Masui cells after primary total knee arthroplasty: a
30:1168–1184 1990; 39:994–1001 multicenter study. J Bone Joint Surg Am 2013;
78. Scheer CS, Fuchs C, Gründling M, et al. Impact 94. Bruins MJ, Zwiers JH, Verheyen CC, Wolfhagen 95:2081–2087
AJR:215, September 2020 575
Chan et al.
108. Sendi P, Müller AM, Berbari E. Are all joints 113. Deirmengian C, Kardos K, Kilmartin P, Cameron tial of next-generation sequencing. J Bone Joint
equal? Synovial fluid analysis in periprosthetic A, Schiller K, Parvizi J. Combined measurement Surg Am 2018; 100:147–154
joint infection. J Bone Jt Infect 2018; 3:258–259 of synovial fluid α-defensin and C-reactive pro- 118. Gupta MN, Sturrock RD, Field M. Prospective
109. Strahm C, Zdravkovic V, Egidy C, Jost B. Accu- tein levels: highly accurate for diagnosing peri- comparative study of patients with culture prov-
racy of synovial leukocyte and polymorphonu- prosthetic joint infection. J Bone Joint Surg Am en and high suspicion of adult onset septic arthri-
clear cell count in patients with shoulder pros- 2014; 96:1439–1445 tis. Ann Rheum Dis 2003; 62:327–331
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
thetic joint infection. J Bone Jt Infect 2018; 114. Parvizi J, Tan TL, Goswami K, et al. The 2018 119. Tan TL, Kheir MM, Shohat N, et al. Culture-neg-
3:245–248 definition of periprosthetic hip and knee infec- ative periprosthetic joint infection: an update on
110. Parvizi J, Erkocak OF, Della Valle CJ. Culture- tion: an evidence-based and validated criteria. what to expect. JBJS Open Access 2018; 3:e0060
negative periprosthetic joint infection. J Bone J Arthroplasty 2018; 33:1309–1314 120. Hassebrock JD, Fox MG, Spangehl MJ, Neville
Joint Surg Am 2014; 96:430–436 115. Costales C, Butler-Wu SM. A real pain: diagnos- MR, Schwartz AJ. What is the role of repeat
111. Stirling P, Faroug R, Amanat S, et al. False-nega- tic quandaries and septic arthritis. J Clin Micro- aspiration in the diagnosis of periprosthetic hip
tive rate of Gram-stain microscopy for diagnosis biol 2018; 56:e01358 infection? J Arthroplasty 2019; 34:126–131
of septic arthritis: suggestions for improvement. 116. Metso L, Mäki M, Tissari P, et al. Efficacy of a 121. Coiffier G, Ferreyra M, Albert JD, et al. Ultra-
Int J Microbiol 2014; 2014:830857 novel PCR- and microarray-based method in di- sound-guided synovial biopsy improves diagnosis
112. Bonanzinga T, Ferrari MC, Tanzi G, Vandenbulcke agnosis of a prosthetic joint infection. Acta of septic arthritis in acute arthritis without enough
F, Zahar A, Marcacci M. The role of alpha defensin Orthop 2014; 85:165–170 analyzable synovial fluid: a retrospective analysis
in prosthetic joint infection (PJI) diagnosis: a liter- 117. Tarabichi M, Shohat N, Goswami K, et al. Diag- of 176 arthritis from a French rheumatology de-
ature review. EFORT Open Rev 2019; 4:10–13 nosis of periprosthetic joint infection: the poten- partment. Clin Rheumatol 2018; 37:2241–2249
APPENDIX 1: Considerations Before Joint Aspiration
1. Does the patient have a prosthetic joint?
2. Has the patient recently received antibiotic therapy?
3. Have blood cultures been obtained?
4. Review serum laboratory values: WBC count, erythrocyte sedimentation rate, C-reactive protein, d-Dimer.
5. Review prior imaging for underlying structural changes or intervening soft-tissue infection (e.g., abscess or bursitis).
6. Does the patient have any allergies?
7. Is the patient on anticoagulant therapy?
8. Does the patient have evidence of an overlying soft-tissue infection?
9. What imaging modality should be used for needle guidance? (Consider joint to be aspirated, assess body habitus.)
Others ≈ 12%
Polymicrobial 5%
Anaerobes 0.6%
Mycobacterium tuberculosis 1.8%
Neisseria gonorrhoeae 1.2%
Miscellaneous 4%
Gram-negative rods ≈ 16%
Pseudomonas aeruginosa 6%
Escherichia coli 3%
Proteus spp. 1%
Klebsiella spp. 1%
Others 4%
Staphylococcus ≈ 56%
MSSA 42%
MRSA 10%
CONS 3%
Streptococcus ≈ 16%
Unspecified spp. 11%
Viridans streptococci 1%
S. pneumoniae 1%
Other spp. 3%
Fig. 1—Chart shows infectious agents in 505 cases of septic arthritis reported
between 1999 and 2013. CONS = coagulase-negative Staphylococcus species;
MRSA = methicillin-resistant Staphylococcus aureus, MSSA = methicillin-
sensitive S. aureus, spp. = species. (Data from [4]).
576 AJR:215, September 2020
Septic Arthritis
Fig. 2—29-year-old man with septic arthritis of left
knee.
A, Anteroposterior radiograph shows uniform joint
space narrowing with articular surface irregularity
(arrowheads). Marked soft-tissue swelling is evident
around knee with effacement of fat planes lateral to
distal femur and medial to proximal tibia.
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
B, Axial T1-weighted fat-suppressed contrast-
enhanced MR image shows large joint effusion (star)
with thick irregular synovial enhancement (straight
arrows). Periarticular soft-tissue enhancement
and intramuscular abscesses are present in
gastrocnemius muscle (curved arrows).
A B
A B
C D E
Fig. 3—60-year-old man with septic arthritis of left hip.
A, Anteroposterior radiographs at baseline (left) and 2 months later (right) show rapidly progressive joint space narrowing and articular surface irregularity (arrowheads).
B, Oblique gray-scale ultrasound image shows complex hip joint effusion (star) and distention of joint capsule (arrowheads). Three milliliters of cloudy yellow fluid
was aspirated, and synovial fluid analysis revealed WBC count of 166,000/μL with 97% polymorphonuclear leukocytes. Synovial fluid culture result was positive for
methicillin-resistant Staphylococcus aureus. ACE = acetabulum, FH = femoral head.
C, Fluoroscopic image obtained during repeat hip joint aspiration shows intraarticular iodinated contrast material and multiple irregular filling defects (oval) suspicious
for synovitis.
D, Axial T1-weighted MR image shows confluent hypointense marrow in femoral head and neck (star) and anterior cortical erosion (arrow) consistent with osteomyelitis.
E, Axial proton density–weighted fat-suppressed MR image shows exuberant marrow edema corresponding to region of abnormal T1 marrow signal intensity (star) in D.
Synchronous reactive or degenerative marrow edema in acetabulum (dashed arrow) retains hyperintense T1 marrow signal relative to skeletal muscle in D. Joint effusion
(arrowhead) and fluid within greater trochanteric bursa (solid arrow) are also evident.
AJR:215, September 2020 577
Chan et al.
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
A
Fig. 4—Proposed diagnostic tools for evaluation of suspected periprosthetic joint infection (PJI). CRP =
C-reactive protein, ESR = erythrocyte sedimentation rate, LE = leukocyte esterase, PMN = polymorphonuclear
leukocytes. (Reprinted from Journal of Arthroplasty, 34, Shohat N, Tan TL, Della Valle CJ, et al. Development
and validation of an evidence-based algorithm for diagnosing periprosthetic joint infection, Pages 2730–2736.
e1, Copyright 2019, with permission from Elsevier, https://www.sciencedirect.com/journal/the-journal-of-
arthroplasty)
A, Chart shows 2018 scoring-based criteria for PJI incorporating newer biomarkers and validated with patients
with PJI as defined by Musculoskeletal Infection Society criteria.
(Fig. 4 continues on next page)
578 AJR:215, September 2020
Septic Arthritis
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
B
Fig. 4 (continued)—Proposed diagnostic tools for evaluation of suspected periprosthetic joint infection (PJI). CRP = C-reactive protein, ESR = erythrocyte sedimentation
rate, LE = leukocyte esterase, PMN = polymorphonuclear leukocytes. (Reprinted from Journal of Arthroplasty, 34, Shohat N, Tan TL, Della Valle CJ, et al. Development and
validation of an evidence-based algorithm for diagnosing periprosthetic joint infection, Pages 2730–2736.e1, Copyright 2019, with permission from Elsevier, https://www.
sciencedirect.com/journal/the-journal-of-arthroplasty)
B, Chart shows 2019 proposed evidence-based algorithm for diagnosing PJI.
AJR:215, September 2020 579
Chan et al.
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
A B C
Fig. 5—42-year-old woman with periprosthetic joint infection (PJI) after prior right total hip arthroplasty.
A, Three-hour-delayed anterior planar 99 mTc-bone scintigram of pelvis obtained during triple-phase examination shows photopenia (circle) at hip joint corresponding to
known total hip prosthesis. There is no periprosthetic radiotracer uptake to suggest PJI or loosening.
B, Coronal STIR slice encoding for metal artifact correction MR image shows complex joint effusion with thickened low-signal-intensity joint capsule (arrowheads).
C, Fluoroscopic image obtained during hip joint aspiration shows needle tip (arrow) positioned at superolateral aspect of neck of femoral stem component. Scant
greenish-brown fluid was aspirated, and synovial fluid cultures were positive for methicillin-sensitive Staphylococcus aureus. Synovial fluid analysis from intraoperative
sample during subsequent incision and drainage revealed WBC count of 35,000/μL with 93% polymorphonuclear leukocytes.
Fig. 6—55-year-old woman with left glenohumeral
septic arthritis and history of type 2 diabetes mellitus.
A, Axial proton density–weighted fat-suppressed
MR image shows large glenohumeral joint effusion
(arrow) and fluid distention of subacromial-subdeltoid
bursa (arrowheads). Numerous low-signal-intensity
punctate foci are present within nondependent
bursa, consistent with gas.
B, Sagittal T2-weighted fat-suppressed MR image
shows gas- and fluid-filled subacromial-subdeltoid
bursa, which communicates with glenohumeral joint
via full-thickness rotator cuff tear (arrowhead) and
overlying subcutaneous tissues via defect in deltoid
muscle (arrow). Thirty milliliters of turbid fluid was
aspirated, and synovial fluid analysis revealed WBC
count of 101,000/μL with 89% polymorphonuclear
leukocytes. Synovial fluid cultures were positive for
methicillin-sensitive Staphylococcus aureus.
A B
A B C
Fig. 7—37-year-old man with clinically suspected right glenohumeral septic arthritis and history of IV drug use. Fluoroscopically guided right glenohumeral joint
aspiration performed before imaging at ordering provider’s request resulted in dry tap.
A, Coronal postaspiration T1-weighted fat-suppressed contrast-enhanced MR image shows large abscess (stars) superficial to and within deltoid muscle, consistent
with pyomyositis.
B and C, Axial proton density–weighted fat-suppressed (B) and axial T1-weighted fat-suppressed contrast-enhanced (C) MR images show minimal fluid within
glenohumeral joint (arrow, B) with trace synovial enhancement (arrow, C). Soft-tissue edema (arrowheads, B) and enhancement (arrowheads, C) are evident anterior to
glenohumeral joint along needle trajectory for aspiration. Juxtaarticular abnormal marrow signal intensity is absent. Patient later had glenohumeral septic arthritis, and
gross intraoperative purulence was noted at incision and drainage.
580 AJR:215, September 2020
Septic Arthritis
Fig. 8—28-year-old woman with right glenohumeral
septic arthritis 1 week after anterior shoulder
dislocation and subsequent closed reduction and
history of uncontrolled type 2 diabetes mellitus.
A, External rotation Grashey radiograph of shoulder
shows ill-defined cortex at site of Hill-Sachs
impaction fracture (arrow). Apparent inferior
Downloaded from www.ajronline.org by 192.141.244.104 on 01/15/22 from IP address 192.141.244.104. Copyright ARRS. For personal use only; all rights reserved
subluxation of glenohumeral joint may reflect atony
or underlying effusion.
B, Transverse gray-scale ultrasound image of
posterior glenohumeral joint during aspiration shows
needle (arrowhead) positioned with tip (circle) within
complex glenohumeral joint effusion. Bulging of
posterior glenohumeral joint capsule (straight arrow)
is evident. Cortical irregularity of posterior humeral
head corresponds to known Hill-Sachs lesion (curved
arrow). Eleven milliliters of purulent white fluid was
aspirated, and synovial fluid analysis revealed WBC
count of 478,000/μL with 97% polymorphonuclear
leukocytes. Synovial fluid and blood cultures were
positive for Streptococcus agalactiae (group B
streptococcus). GLE = glenoid, HUM = humeral head.
A B
Fig. 9—Two patients undergoing aspiration to rule
out infection before arthroplasty.
A, 62-year-old man who has undergone Girdlestone
procedure. Fluoroscopic image obtained during
right hip joint aspiration shows needle tip (arrow)
positioned inferior to superior rim of acetabulum
(ACE).
B, 68-year-old woman with neuropathic shoulder.
Fluoroscopic image obtained during left
glenohumeral joint aspiration shows needle tip
(arrow) positioned along medial edge of chronically
eroded humeral head. Both aspiration attempts
yielded return of fluid.
A B
Fig. 10—Two patients with prior reverse total
shoulder arthroplasty and shoulder pain.
A, 62-year-old woman undergoing right glenohumeral
joint aspiration. Fluoroscopic still image shows
needle tip (arrow) positioned near superolateral
aspect of glenosphere component (GS).
B, 73-year-old woman undergoing right glenohumeral
joint aspiration. Fluoroscopic still image shows
needle tip (arrow) positioned at inferomedial aspect
of glenohumeral joint. Air was used for negative
contrast confirmation of intraarticular positioning
(arrowheads).
A B
AJR:215, September 2020 581
You might also like
- 2007 Confrontation in Addiction TreatmentDocument22 pages2007 Confrontation in Addiction TreatmentJason WoodruffNo ratings yet
- Fundamentals of NursingDocument50 pagesFundamentals of NursingGuruKPO67% (3)
- Oncology Drug ListDocument11 pagesOncology Drug Listashrafh100% (1)
- Sources of Drugs 2015Document33 pagesSources of Drugs 2015Rafael Paulino RimoldiNo ratings yet
- Technological Advances in Nontraditional Orthodontics PDFDocument14 pagesTechnological Advances in Nontraditional Orthodontics PDFcatherineNo ratings yet
- Evaluation of The Painful Total Knee Arthroplasty.99377Document9 pagesEvaluation of The Painful Total Knee Arthroplasty.99377Filip starcevic100% (1)
- Catatonic Schizophrenia NCP (Revised)Document13 pagesCatatonic Schizophrenia NCP (Revised)Wen Silver100% (1)
- Evidence-Based Practice Fact SheetDocument3 pagesEvidence-Based Practice Fact Sheetmohamedwhatever100% (2)
- Medical Surgical NursingDocument31 pagesMedical Surgical Nursingsingireddi1revathi100% (3)
- Extein Et Al 2017 CT Findings of Traumatic Bucket Handle Mesenteric InjuriesDocument5 pagesExtein Et Al 2017 CT Findings of Traumatic Bucket Handle Mesenteric Injuries132 Naga VamsiNo ratings yet
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocument8 pagesWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinNo ratings yet
- JurnalDocument7 pagesJurnalradenbagasNo ratings yet
- HCC NCDocument15 pagesHCC NCNEMESIS NEMESISNo ratings yet
- Subchondroplasty What TheDocument6 pagesSubchondroplasty What TheikhsanNo ratings yet
- The History of Clinical Musculoskeletal RadiologyDocument8 pagesThe History of Clinical Musculoskeletal RadiologyVALENTINA LOPEZ MARINNo ratings yet
- Orbital Fracture JournalDocument11 pagesOrbital Fracture JournalPramod KumarNo ratings yet
- Transabdominal Sonography in Assessment of The Bowel in AdultsDocument16 pagesTransabdominal Sonography in Assessment of The Bowel in AdultsСергей СадовниковNo ratings yet
- Ajr 161 6 8249719Document7 pagesAjr 161 6 8249719hotmart ventasNo ratings yet
- Jurnal B 1Document10 pagesJurnal B 1Nasayu Nadia Santika AyuNo ratings yet
- Clear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalDocument8 pagesClear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalBastian VizcarraNo ratings yet
- Imaging and Classification of Congenital Cystic Renal DiseasesDocument11 pagesImaging and Classification of Congenital Cystic Renal DiseasessuhartiniNo ratings yet
- Calcific Tendinitis of The Longus Colli MuscleDocument2 pagesCalcific Tendinitis of The Longus Colli Musclemloureiro17No ratings yet
- Chapter 025Document4 pagesChapter 025Emma KnoxNo ratings yet
- Cardiac MRI 1Document8 pagesCardiac MRI 1drpankajsNo ratings yet
- Kutkut 2011 Sinus WidthDocument5 pagesKutkut 2011 Sinus WidthLamis MagdyNo ratings yet
- Femoroacetabular Impingement A Cause For13 231106 161042Document9 pagesFemoroacetabular Impingement A Cause For13 231106 161042Cristian SanchezNo ratings yet
- Examination of The Wrist.37Document11 pagesExamination of The Wrist.37Filipe AlbuquerqueNo ratings yet
- Solid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaDocument11 pagesSolid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaTạ Minh ZSNo ratings yet
- Uas CT Scan - Jurnal - Dwi Ajeng Risqy Hasanah Syam - P1337430219162 PDFDocument6 pagesUas CT Scan - Jurnal - Dwi Ajeng Risqy Hasanah Syam - P1337430219162 PDFDwi Ajeng Risqy HasanahSyamNo ratings yet
- Of Fice-Based Needle Arthroscopy: A Standardized Diagnostic Approach To The KneeDocument6 pagesOf Fice-Based Needle Arthroscopy: A Standardized Diagnostic Approach To The KneeΗΛΙΑΣ ΠΑΛΑΙΟΧΩΡΛΙΔΗΣNo ratings yet
- Acupuncture For Chronic PainDocument10 pagesAcupuncture For Chronic PaindanielNo ratings yet
- Shoulder USG Anatomy, Technique, Scanning PitfallDocument10 pagesShoulder USG Anatomy, Technique, Scanning PitfallRonaldNo ratings yet
- Computed Tomography Versus Nasal Endoscopy For The Measurement of The Internal Nasal Valve Angle in AsiansDocument5 pagesComputed Tomography Versus Nasal Endoscopy For The Measurement of The Internal Nasal Valve Angle in AsiansPutri HakimNo ratings yet
- CT Scan PDFDocument12 pagesCT Scan PDFBunga alaraafNo ratings yet
- OsteoartritisDocument10 pagesOsteoartritis0128 Nurul Wahidah YasidNo ratings yet
- IJOrtho 52 638Document7 pagesIJOrtho 52 638dr usmanNo ratings yet
- Ajr 10 5540Document9 pagesAjr 10 5540Pepe pepe pepeNo ratings yet
- Control and Management of Hospital Indoor Air QualityDocument8 pagesControl and Management of Hospital Indoor Air QualityKanokwan BorwornphiphattanachaiNo ratings yet
- Ajr 2Document3 pagesAjr 2anon_302681452No ratings yet
- Inferior Alveolar Neurovascular Bundle Repositioning: A Retrospective AnalysisDocument6 pagesInferior Alveolar Neurovascular Bundle Repositioning: A Retrospective Analysisr1comfupchNo ratings yet
- PDF History Physical Examination Laboratorytesting and Emergency Department DDDocument17 pagesPDF History Physical Examination Laboratorytesting and Emergency Department DDNurul FatimahNo ratings yet
- Lin 2017Document11 pagesLin 2017Ibnu CaesarNo ratings yet
- Cystic Hepatic Lesions: A Review and An Algorithmic ApproachDocument13 pagesCystic Hepatic Lesions: A Review and An Algorithmic Approachhusni gunawanNo ratings yet
- AJRAmJRoentgenol 2013Aug2012W206-14Document10 pagesAJRAmJRoentgenol 2013Aug2012W206-14asdfghjm.,nmnbvcxNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Bcs Article RoleDocument15 pagesBcs Article RoleSowmya ANo ratings yet
- Examen Fisico RodillaDocument10 pagesExamen Fisico RodillaURGENCIAS HUSRTNo ratings yet
- JCM 11 02152Document8 pagesJCM 11 02152Natalia LujanNo ratings yet
- Discovering Knee Osteoarthritis Using CNN Enhanced With AlexnetDocument26 pagesDiscovering Knee Osteoarthritis Using CNN Enhanced With Alexnetrevathi pNo ratings yet
- Donovan 2012Document11 pagesDonovan 2012carlosso16hotmail.comNo ratings yet
- Angiographic Assessment of Collateral Connections inDocument6 pagesAngiographic Assessment of Collateral Connections inSitiMaghfirahHafizNo ratings yet
- Chronic Inflammatory AppendicealDocument4 pagesChronic Inflammatory AppendicealIkki DongNo ratings yet
- What Are The Indications For The Use of Computed Tomography Before Septoplasty?Document3 pagesWhat Are The Indications For The Use of Computed Tomography Before Septoplasty?Putri HakimNo ratings yet
- Standfor Refrence 3Document6 pagesStandfor Refrence 3Harshoi KrishannaNo ratings yet
- Ultrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Document9 pagesUltrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Сергей СадовниковNo ratings yet
- Fundamentals of Joint Injection: A. Keith Rastogi Kirkland W. Davis Andrew Ross Humberto G. RosasDocument11 pagesFundamentals of Joint Injection: A. Keith Rastogi Kirkland W. Davis Andrew Ross Humberto G. Rosasgrahapuspa17No ratings yet
- Bergmark Et Al 2022 Decision Making During PCI Guided by OCTpdfDocument10 pagesBergmark Et Al 2022 Decision Making During PCI Guided by OCTpdfSajjad HussainNo ratings yet
- Manifestations of Systemic Diseases and Conditions That A!ect The Periodontal Attachment Apparatus: Case De"nitions and Diagnostic ConsiderationsDocument50 pagesManifestations of Systemic Diseases and Conditions That A!ect The Periodontal Attachment Apparatus: Case De"nitions and Diagnostic Considerationsandrea guillénNo ratings yet
- Effect of Timing of ACL Reconstruction in Surgery and Development of Meniscal and Chondral LesionsDocument6 pagesEffect of Timing of ACL Reconstruction in Surgery and Development of Meniscal and Chondral LesionsPascha ParamurthiNo ratings yet
- Jmri 24311Document17 pagesJmri 24311Rakesh JhaNo ratings yet
- AJR Clinical PET MRI 2018 UpdateDocument19 pagesAJR Clinical PET MRI 2018 Updatealfred benedict bayanNo ratings yet
- Resultados de Artroplastía en Pacientes Con Vih, Metanalisis 2019Document7 pagesResultados de Artroplastía en Pacientes Con Vih, Metanalisis 2019Daniel Cancino CallirgosNo ratings yet
- Ankle Impingement: A Critical Analysis ReviewDocument10 pagesAnkle Impingement: A Critical Analysis ReviewSusan Ly VillalobosNo ratings yet
- Treatment Evaluation of Odontogenic Keratocyst by Using CBCTDocument6 pagesTreatment Evaluation of Odontogenic Keratocyst by Using CBCTShinta PurnamasariNo ratings yet
- Arthroscopic Surgery For Degenerative Knee Arthritis and Meniscal Tears: A Clinical Practice GuidelineDocument8 pagesArthroscopic Surgery For Degenerative Knee Arthritis and Meniscal Tears: A Clinical Practice Guidelineyehezkiel feriNo ratings yet
- Suo 2020Document10 pagesSuo 2020Hải Dương MinhNo ratings yet
- Article2 1Document10 pagesArticle2 1Cristian OñateNo ratings yet
- NCPDocument14 pagesNCPTamil VillardoNo ratings yet
- Overexertion and DehydrationDocument30 pagesOverexertion and DehydrationCharvy SalvacionNo ratings yet
- 20 Working Length DeterminationDocument20 pages20 Working Length DeterminationModerator Zhi Ling YauNo ratings yet
- Paper Lips1Document11 pagesPaper Lips1dominiqueNo ratings yet
- Queenie Drug StdyDocument11 pagesQueenie Drug StdyJonas OrbetaNo ratings yet
- Health Care Waste Management 14bDocument18 pagesHealth Care Waste Management 14bMokua FedinardNo ratings yet
- MVP Health Care Chapter20 ExternalCausesMorbidityDocument55 pagesMVP Health Care Chapter20 ExternalCausesMorbidityAnonymous OOJjtp86F50% (1)
- Pharmacologic Use of Glucocorticoids - UpToDateDocument11 pagesPharmacologic Use of Glucocorticoids - UpToDateSergio M Junior100% (1)
- Second Quarter Examination in Health 8Document16 pagesSecond Quarter Examination in Health 8PENTIL HIGH SCHOOLNo ratings yet
- Asphalt Emulsion: Material Safety Data SheetDocument8 pagesAsphalt Emulsion: Material Safety Data Sheetsmanoj354No ratings yet
- April BaseDocument3 pagesApril BaseDinesh Chandramohan CNo ratings yet
- Surgical Techniques CorpectomyDocument18 pagesSurgical Techniques CorpectomyJulian VargasNo ratings yet
- Formative 3 - Ans KeyDocument41 pagesFormative 3 - Ans KeyDhine Dhine ArguellesNo ratings yet
- Presented By: Dr. Vishal Bathma Asst. Professor Community Medicine PCMS&RCDocument42 pagesPresented By: Dr. Vishal Bathma Asst. Professor Community Medicine PCMS&RCtorr123No ratings yet
- Report Rehab NewDocument25 pagesReport Rehab Newarissa razaliNo ratings yet
- Psihologie Medicală Şi Ştiinţele Comport. Sociologie EnglezăDocument4 pagesPsihologie Medicală Şi Ştiinţele Comport. Sociologie EnglezăAnonymous NK07LsS9lNo ratings yet
- Chapter 4 Physical Therapist As Patient Client ManagerDocument21 pagesChapter 4 Physical Therapist As Patient Client Managersdr fahadNo ratings yet
- A New Surgical Treatment of Keloid Keloid Core ExcisionDocument7 pagesA New Surgical Treatment of Keloid Keloid Core Excisiongalih widodoNo ratings yet
- Community Herbal Monograph On Devils ClawDocument7 pagesCommunity Herbal Monograph On Devils ClawLesley HollardNo ratings yet
- Treatments For Infantile Postural AsymmetryDocument7 pagesTreatments For Infantile Postural AsymmetryraquelbibiNo ratings yet
- Mary Jane Brown, For Orin B. Brown, Deceased v. Donna E. Shalala, Secretary of Health and Human Services, 5 F.3d 545, 10th Cir. (1993)Document5 pagesMary Jane Brown, For Orin B. Brown, Deceased v. Donna E. Shalala, Secretary of Health and Human Services, 5 F.3d 545, 10th Cir. (1993)Scribd Government DocsNo ratings yet
- No Change in Serum Metal Ions Levels After Primary Total Hip R - 2022 - ArthroplDocument4 pagesNo Change in Serum Metal Ions Levels After Primary Total Hip R - 2022 - ArthroplSanty OktavianiNo ratings yet