Professional Documents
Culture Documents
Sasjs 62 56-59
Uploaded by
Marco Antonio MiraveteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sasjs 62 56-59
Uploaded by
Marco Antonio MiraveteCopyright:
Available Formats
SAS Journal of Surgery
Abbreviated Key Title: SAS J Surg
ISSN 2454-5104
Journal homepage: https://saspublishers.com/sasjs/
Proximal Sural Artery1 Flap for Knee Defects
Ganji Raveendra Reddy, M.S, M.Ch , A R Ch Mohan, M.S, M.Ch , B Jyothsna, M.S, M.Ch3*, D Balaji Sasidhar Reddy,
2
M.S, M.Ch4, Poornachandra Rao, M.S, M.Ch5
1
Associate Professor, Department of Plastic Surgery, GGH, Vijayawada, India
2
Professor, Department of Plastic Surgery, GGH, Vijayawada, India
3
Assistant Professor, Department of Plastic Surgery, GGH, Vijayawada, India
4
Orthopedic Surgeon, Sri Ramadevi Super Speciality Hospital, Tirupati, India
5
Orthopedic Surgeon, Remedy Hospital, Tirupati, India
DOI: 10.36347/sasjs.2020.v06i02.007 | Received: 30.01.2020 | Accepted: 06.02.2020 | Published: 18.02.2020
*Corresponding author: Dr. Jyostna P
Abstract Original Research Article
Proximal sural artery flap is one of the dependable options standing first on the list to reconstruct the knee defects. In
our series of 9 cases which were done in between 2017-2020, for various knee defects following road traffic accidents,
tumor exicision, metal exposure, proximal sural artery flap was used to resurface knee. Hand held Doppler was not
used to locate perforators in any case. All the cases were performed without tourniquet. Results were quite satisfactory
with near normal skin, thickness, color, and sensation. Execution of the procedure is relatively easy even in fatty
individuals in comparison to the thigh flaps. Post operative complications were negligible, with no total flap loss in
any case, with minimal donor site morbidity.
Keywords: proximal sural artery flap, knee defects, knee debridement.
Copyright @ 2020: This is an open-access article distributed under the terms of the Creative Commons Attribution license which permits unrestricted
use, distribution, and reproduction in any medium for non-commercial use (NonCommercial, or CC-BY-NC) provided the original author and source
are credited.
necrosis after trauma or plate and screw exposure, for
INTRODUCTION which debridement was done before providing flap
Defects in and around the knee are certainly cover on table. All the defects were in and around the
challenging to a reconstructive surgeon, because of its patella on anterior surface. They were all non smokers
location over mobile joint, which often demands a and non alcoholics. One man was having Diabetes,
stable, pliable tissue with sensation. Meeting these which is under control. The average size of the defect
demands, proximal sural artery flap appears to be one of was 6 X9 Cm2.
the best choices [1]. It has thin skin when compared
with thigh skin flaps, color is near normal to knee skin, Surgical Technique
sensation is quite satisfactory due to sural nerve, All the cases were done under spinal
dimensions are quite enough to cover entire anterior anesthesia. Patients were kept in prone or lateral
surface of knee, apart from- it is having reliable blood position. No tourniquet was used in any case. A
supply based on the sural arteries. Even donor site reference line was marked from the center of posterior
morbidity is also minimal in comparison to the other knee crease line to lateral malleolus. Pivot point was
alternative choices [2]. fixed 2 cm distal to this central mark on the reference
line. Based on this pivot point, a defect based island
MATERIAL AND METHODS flap (in some cases with skin extension as ‘sperm
All the 9 cases were done between 2017 – shaped’) marked on the junction of the middle and
2020 in Department of Plastic Surgery, GGH, distal third of the leg, keeping the reference line in the
Vijayawada and Sri Ramadevi Super Speciality center, which is indicative of Neuro vascular pedicle by
Hospital, Remedy Hospital, Tirupati, India. The causes doing ‘planning in reverse’. Identification of perforators
for the knee defects were following road traffic with hand held Doppler was not done in any case
accidents, tumor exicision and exposure of plate screws. assuming that they were there as described. Then distal
The age group range from 20 years to 50 years. Males incision was made first to identify the sural nerve and
were 8 and females were 1 in this group. Five cases short saphenous vein, which was clamped with
were presented with skin loss on the accidental site hemostats ligated and divided. Then the dissection
itself, and rest of the four were following delayed skin continued all along the markings, raising dermal flaps
© 2020 SAS Journal of Surgery | Published by SAS Publishers, India 56
Ganji Raveendra Reddy et al., SAS J Surg, Feb, 2020; 6(2): 56-59
over the bridge segment on either side keeping given adequately without any tension over suture line
subcutaneous pedicle with its neuro vascularity. The after keeping drain. Donor site reduced and bridge
average width of the pedicle was maintained at 4cm, on segment closed primarily. Left over raw area was cover
either side of the neuro vascular structures. Flap with split thickness skin graft taken from the thigh and
harvestation continued till the pivot point securing tie over dressing applied. Posterior slab was provided
heamostasis, simultaneously assessing the reach of the with good padding over pedicle and pivot point to avoid
flap to the defect. Then sub cutaneous tunnel created compression. Post operatively limb was elevated by
from the pivot point to the defect to bring the flap to the keeping pillow over leg avoiding pressure over
defect. In cases where, flap was raised with skin posterior aspect of knee for 10 days on an average.
extension over pedicle, the bridge segment was incised Suture removal was done after 2 weeks, mobilization
undermined on either side to accommodate the pedicle started after 3 weeks depending on other associated
skin to avoid tension and compression. Flap inset was injuries.
Fig-1: Schematic picture showing pre op defect, planning, flap harvestation, results after two weeks
© 2020 SAS Journal of Surgery | Published by SAS Publishers, India 57
Ganji Raveendra Reddy et al., SAS J Surg, Feb, 2020; 6(2): 56-59
RESULTS Similarly in one case with distal necrosis was managed
All the flaps were survived. No total loss of conservatively with regular dressings - no skin grafting
flap noted in any case. However, the common was done. Donor site graft take was also satisfactory
complication observed was epidermal necrosis either at and healed primarily. The color thickness pliability was
the distal end or at the margins of the flap. This was well matched on par with the surrounding skin. Over all
managed conservatively without any debridement to patient satisfaction was good.
heal by secondary intention as it is partial dermal loss.
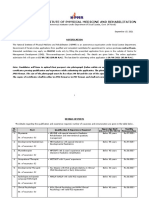
Table-1: Schematic representation of out come
S. Age Presentation of Defect Defect Risk factor Flap Complications
No (years) Dimensions dimension
(Cm) (Cm)
1 19 With loss of tissue 4X4 5X5 Superficialepidermal necrosis
2 50 Surgical debridement 15X12 15X12 Uneventful
3 26 With tissue loss 5X6 6X7 Uneventful
4 35 Following debridement 8X7 9X8 Uneventful
5 53 Tumor exicixion 8X7 Diabetes 9X8 Distal necrosis
mellitus
6 25 With tissue loss 7X8 8X9 Uneventful
7 32 With tissue loss 4X12 5X12 Uneventful
8 41 Wound gap following 4X10 5X12 Superficial eidermal necrosis
plate and screws
9 22 With tissue loss 5X6 6X8 Uneventful
Fig-2: Schematic picture showing delayed necrosis of skin following trauma, defect after wound debridement, resurfaced with proximal
sural artery flap-after suture removal
Fig-3: Schematic picture showing pre op knee defect and post op picture with flap cover
© 2020 SAS Journal of Surgery | Published by SAS Publishers, India 58
Ganji Raveendra Reddy et al., SAS J Surg, Feb, 2020; 6(2): 56-59
DISSCUSSION congestion is rarely observed in these flaps. The
Before selecting proximal sural artery flap as marginal epidermal necrosis of the flap was probably
an option for knee defects, we used to do medial and due to shearing force between the skin and fascia,
lateral gastrocnemius muscle and musculo-cutaneous which has been overcome by meticulous dissection and
flaps as first option. However, we have noticed that, simultaneous fixation of two in our later cases. Donor
muscle based flaps are often too bulky and with limited site complications like minimal graft loss are not
reach up to lower half of the knee. Later we shifted our uncommon either due to pressure from plaster slab or
focus on distal based medial and lateral genicular artery depending position of the graft. Sensation of the flap is
flaps from thigh with retrograde blood supply as an also quite satisfactory in compare to flaps of other
other alternative. In planning these flaps location of options due to intact sural nerve [5].
perforator is sublime and plays a key role. The flaps are
too big and bulky hence rotation is often technically Overall the merits of the proximal sural artery
difficult unless perforator is totally skeletonised, taking flap with its ease of dissection (even without
the imminent risk of venous congestion. And in females tourniquet), consistent perforators (no need of Doppler),
technical difficulty is further enhanced due to ante grade blood supply, adequate venous drainage, thin
cumulative fat on the thigh [3]. skin- made superior among surrounding peer flaps and
To overcome these odds, we started applying with satisfactory outcome [6].
proximal sural artery flap for the knee defects since
2017 with quite satisfactory results with good patient REFERENCES
compliance. Proximal sural artery flap is based on the 1. Deng C, Wei Z, Wang B, Jin W, Zhang W, Tang
sural artery (medial, median and lateral sural arteries), X, Wu B, Sun G, Wang D. The proximally based
which are often direct branches of popliteal artery and lateral superficial sural artery flap: a convenient
in few cases from genicular arteries (medial or lateral). and optimal technique for the reconstruction of
These arteries supply the skin of calf region especially soft-tissue defects around the knee. Int J Clin Exp
upper two third of leg. The sural arteries are so Med. 2016 Jan 1;9(8):15167-76.
consistent that, no need to use Doppler to locate the 2. Masquelet A C, Romana M C, Wolf G. Skin island
perforators. These arteries accompany the sural nerve flaps supplied by the vascular axis of the sensitive
throughout its course and joins with the perforators of superficial nerves: anatomic study and clinical
peroneal artery distally, which is the basis for ‘reverse experience in the leg. Plast Reconstr Surg, 1992;
sural artery flap’. It is a fascio cutaneous flap. The exact 89(6)1115-1121.
flap dimensions are not clearly defined. However in our 3. Suri MP, Friji MT, Ahmad QG, Yadav PS. Utility
series, we have found that, side to side- from lateral of proximally based sural artery flap for lower
midline to medial midline, proximo distally- from knee thigh and knee defects. Ann Plast Surg,
crease line to junction of middle and distal third of leg 2010;64:462-465.
can be harvested safely without compromising 4. Pan H, Zheng Q, Yang S. Utility of proximally
circulation to the flap. Flap planning and size is based sural fasciocutaneous flap for knee and
depending on the defect dimensions. Flap can be proximal lower leg defects. Wounds, 2014;26:132-
harvested as an island flap with sub cutaneous pedicle, 138.
or as a pedicle flap. Apart from these two, there is 5. Cheon SJ, Kim IB, Park WR, Kim HT. The
another variation, which is an island with skin extension proximally-based sural artery flap for coverage of
over pedicle like a tail - ‘sperm shaped’, to lay over at soft tissue defects around the knee and on the
the bridge segment between the pivot point and the proximal third and middle third of the lower leg:
defect – to avoid tension over pedicle. In cases of 10 patients followed for 1–2.5 years. Acta Orthop,
‘island’ type, flaps are passed subcutaneously through a 2008;79:370-375.
tunnel by creating adequate pocket [4]. In both 6. Meyer C, Hartmann B, Horas U, Kilian O, Heiss
variations flaps behaved well without compromising C, Schnet-Tler R. Reconstruction of the lower leg
circulation. Sural artery is accompanied by two venae with the sural artery flap. Langenbecks Arch Surg,
commitantes with antegrade blood flow and also having 2002; 387(7-8)320-325.
short saphenous vein and sural nerve, thus venous
© 2020 SAS Journal of Surgery | Published by SAS Publishers, India 59
You might also like
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Tom Skin-Sparing Approach To Treatemen of NSTI 2016Document14 pagesTom Skin-Sparing Approach To Treatemen of NSTI 2016Sadaf Raisa KhanNo ratings yet
- Trim Bos 2002Document4 pagesTrim Bos 2002Gaetano De BiaseNo ratings yet
- Madsen 2020Document10 pagesMadsen 2020fabian hernandez medinaNo ratings yet
- Lee 2015Document7 pagesLee 2015AncaVerdesNo ratings yet
- Standardized Sternal Coverage Bota Et AlDocument7 pagesStandardized Sternal Coverage Bota Et AlOli BotaNo ratings yet
- 2014 Article 1741Document4 pages2014 Article 1741anton suponoNo ratings yet
- 224f619eb8367c58fb5338cb7f5363a3Document5 pages224f619eb8367c58fb5338cb7f5363a3Janardana GedeNo ratings yet
- Brief Communication: Nitin Mokal, Navdeep ChavanDocument4 pagesBrief Communication: Nitin Mokal, Navdeep ChavanANOOP HANDANo ratings yet
- PIIS0363502317318403Document4 pagesPIIS0363502317318403Juan HoyosNo ratings yet
- Poster Extended Groin FlapDocument1 pagePoster Extended Groin FlapDharmendra WidetyaNo ratings yet
- Is Mesh Always Necessary in Every Small UmbilicalDocument8 pagesIs Mesh Always Necessary in Every Small UmbilicalLeonardo RibeiroNo ratings yet
- Perforator Pedicled Propeller Flaps For Soft TissuDocument6 pagesPerforator Pedicled Propeller Flaps For Soft TissuMuhammad RifkiNo ratings yet
- Skin Graft: Technique, Indications and OutcomesDocument9 pagesSkin Graft: Technique, Indications and OutcomesIJAR JOURNALNo ratings yet
- The Reverse Posterior Interosseous Artery Flap: Technical Considerations in Raising An Easier and More Reliable FlapDocument9 pagesThe Reverse Posterior Interosseous Artery Flap: Technical Considerations in Raising An Easier and More Reliable FlapyeapdshengNo ratings yet
- Delta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesDocument4 pagesDelta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Archive of SIDDocument5 pagesArchive of SIDEdy Anugrah PutraNo ratings yet
- Yang 2018Document7 pagesYang 2018Robert ChristevenNo ratings yet
- Desyndactylization of Simple Complete Syndactyly of Great Toe and Second Toe Case Report and Operative TechniqueDocument3 pagesDesyndactylization of Simple Complete Syndactyly of Great Toe and Second Toe Case Report and Operative TechniqueInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Prospective Observational Study On Scola For Ventral Hernia With Diastasis Recti - Our Experience at A Tertiary Care HospitalDocument4 pagesA Prospective Observational Study On Scola For Ventral Hernia With Diastasis Recti - Our Experience at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- OMX Volume 12 Issue 1 Pages 14-20Document7 pagesOMX Volume 12 Issue 1 Pages 14-20JyothishNo ratings yet
- Comparison of The Repair Techniques For Extensor Tendon Injuries in The HandDocument6 pagesComparison of The Repair Techniques For Extensor Tendon Injuries in The HandInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10 1016@j Jhsa 2019 01 007Document7 pages10 1016@j Jhsa 2019 01 007Deborah SalinasNo ratings yet
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDocument11 pagesUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanNo ratings yet
- Z Plasty Closure of The Donor Defect of The Radial Forearm Free FlapDocument3 pagesZ Plasty Closure of The Donor Defect of The Radial Forearm Free FlapMuhammad AbdurrahmanNo ratings yet
- Comparison Between Antegrade Nailing and Retrograde Nailing in Humeral Diaphyseal FracturesDocument5 pagesComparison Between Antegrade Nailing and Retrograde Nailing in Humeral Diaphyseal FracturesPrabhakaran NarayanasamyNo ratings yet
- Retromandibular Approach JournalDocument4 pagesRetromandibular Approach JournalAldo AguilarNo ratings yet
- Minimal Incision in Parotidectomy: Reconstructive SurgeryDocument5 pagesMinimal Incision in Parotidectomy: Reconstructive SurgeryUriel Tre CaNo ratings yet
- Skin Graft Techniques Khan2020Document15 pagesSkin Graft Techniques Khan2020danielNo ratings yet
- Case Report of Uneventful Resurfacing of The Dorsum 2024 International JournDocument4 pagesCase Report of Uneventful Resurfacing of The Dorsum 2024 International JournRonald QuezadaNo ratings yet
- OverlappingDocument2 pagesOverlappingKrezsa StiffensiNo ratings yet
- Supraclavicular Flap Reconstruction For Skin Defect After HugeParotid Region Lesion - Case ReportDocument6 pagesSupraclavicular Flap Reconstruction For Skin Defect After HugeParotid Region Lesion - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Negative Pressure Wound TherapyDocument5 pagesNegative Pressure Wound TherapyarfahNo ratings yet
- Medip, ISJ-2381 ODocument6 pagesMedip, ISJ-2381 OmarvinmtcirujanoNo ratings yet
- Syndactyly and ClinodactylyDocument47 pagesSyndactyly and ClinodactylychlondNo ratings yet
- Ishida 2016Document9 pagesIshida 2016stoia_sebiNo ratings yet
- Is It Safe To Extract The Reverse Sural Artery Flap From The Proximal Third of The Leg?Document7 pagesIs It Safe To Extract The Reverse Sural Artery Flap From The Proximal Third of The Leg?yennysabriniNo ratings yet
- Wa0086.Document9 pagesWa0086.Brampp HimawanNo ratings yet
- Practical Applications: Decision Making in Gingival Recession Treatment: Scientific Evidence and Clinical ExperienceDocument12 pagesPractical Applications: Decision Making in Gingival Recession Treatment: Scientific Evidence and Clinical ExperienceAlexa LoyaNo ratings yet
- A Rare Case of Large Size Undifferentiated Pleomorphic Sarcoma of AnkleDocument5 pagesA Rare Case of Large Size Undifferentiated Pleomorphic Sarcoma of AnkleIJAR JOURNALNo ratings yet
- Bridging Plate Osteosynthesis of Humeral Shaft Fractures: Bruno Livani, William Dias BelangeroDocument9 pagesBridging Plate Osteosynthesis of Humeral Shaft Fractures: Bruno Livani, William Dias BelangeroMiguel Angel Lamas RamirezNo ratings yet
- Endoskopik 2.brankialDocument5 pagesEndoskopik 2.brankialDogukan DemirNo ratings yet
- Residual CystDocument4 pagesResidual Cyst053 Sava Al RiskyNo ratings yet
- ShoelaceDocument5 pagesShoelaceJoe JoeNo ratings yet
- Sural Island Flap - A Good Option For Coverage of The Exposed Heel (Tendo-Achillis)Document6 pagesSural Island Flap - A Good Option For Coverage of The Exposed Heel (Tendo-Achillis)yennysabriniNo ratings yet
- Fingertip and Nail Bed InjuriesDocument27 pagesFingertip and Nail Bed InjuriesiwanbaongNo ratings yet
- Fai 2011 0818Document4 pagesFai 2011 0818Mohamed GoudaNo ratings yet
- Intramedullary Nailing of Distal Metaphyseal.5Document9 pagesIntramedullary Nailing of Distal Metaphyseal.5Joël Clarck EkowongNo ratings yet
- Extracapsular Dissection of Deep Lobe Parotid Mass Aided by Retromandibular Vein On Imaging: Case ReportDocument6 pagesExtracapsular Dissection of Deep Lobe Parotid Mass Aided by Retromandibular Vein On Imaging: Case Reportbasem.t.jamalNo ratings yet
- Anterior Cervical Discectomy With Fusion in Patients With Degenerative Cervical Disc DiseaseDocument10 pagesAnterior Cervical Discectomy With Fusion in Patients With Degenerative Cervical Disc DiseaseNasrullah nsrNo ratings yet
- Base Segudo Caso ClinicoDocument6 pagesBase Segudo Caso Clinicogatos965669988No ratings yet
- Reversed Z-Plasty and Its Variations To Release Wide-Scar ContractionDocument4 pagesReversed Z-Plasty and Its Variations To Release Wide-Scar ContractionmarethadwiNo ratings yet
- Rjad 529Document3 pagesRjad 529Jefferson RuizNo ratings yet
- Adams 2006Document13 pagesAdams 2006AncaVerdesNo ratings yet
- Superiorly Based Perforator Plus FL Ap For Inguinal Defects: Original ArticleDocument5 pagesSuperiorly Based Perforator Plus FL Ap For Inguinal Defects: Original ArticleamdreyNo ratings yet
- 31MDI RET '17 JacksonDocument6 pages31MDI RET '17 Jacksoncd.brendasotofloresNo ratings yet
- Soleus Muscle Flap For The Coverage of Pre-Tibial Defect of Middle Third of LegDocument6 pagesSoleus Muscle Flap For The Coverage of Pre-Tibial Defect of Middle Third of LegHassan KhanNo ratings yet
- Rosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NerveDocument4 pagesRosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NervedanielpohlmanNo ratings yet
- Clinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesDocument9 pagesClinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesAndika FahruroziNo ratings yet
- VYplastyDocument6 pagesVYplastyVineet ArunNo ratings yet
- Factors Affecting The Outcome of Frontalis Sling.32Document7 pagesFactors Affecting The Outcome of Frontalis Sling.32Marco Antonio MiraveteNo ratings yet
- Original Article: AbstractDocument3 pagesOriginal Article: AbstractMarco Antonio MiraveteNo ratings yet
- En V29n1a07Document6 pagesEn V29n1a07Marco Antonio MiraveteNo ratings yet
- Aes 05 37Document13 pagesAes 05 37Marco Antonio MiraveteNo ratings yet
- The Proximally Based Sural Artery Flap For Coverage of Soft Tissue Defects Around The Knee and On The Proximal Third and Middle Third of The Lower LegDocument7 pagesThe Proximally Based Sural Artery Flap For Coverage of Soft Tissue Defects Around The Knee and On The Proximal Third and Middle Third of The Lower LegMarco Antonio MiraveteNo ratings yet
- NigerJClinPract216726-113084 030828Document5 pagesNigerJClinPract216726-113084 030828Marco Antonio MiraveteNo ratings yet
- Norman 2017Document7 pagesNorman 2017Lee HaeunNo ratings yet
- BrookfieldDocument8 pagesBrookfieldFariha Naseer Haral - 28336/TCHR/JVAITNo ratings yet
- Chapter 5Document24 pagesChapter 5Tadi SaiNo ratings yet
- PPG ReviewerDocument8 pagesPPG Reviewerryanbaldoria.immensity.ictNo ratings yet
- Pemphigus Subtypes Clinical Features Diagnosis andDocument23 pagesPemphigus Subtypes Clinical Features Diagnosis andAnonymous bdFllrgorzNo ratings yet
- ProfessionalresumeDocument1 pageProfessionalresumeapi-299002718No ratings yet
- Math 10 Module - Q2, WK 8Document5 pagesMath 10 Module - Q2, WK 8Reygie FabrigaNo ratings yet
- Edward William Lane's Lexicon - Volume 7 - Page 186 To 277Document92 pagesEdward William Lane's Lexicon - Volume 7 - Page 186 To 277Serge BièvreNo ratings yet
- Sample File: A of TheDocument6 pagesSample File: A of TheMegan KennedyNo ratings yet
- Ghosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthDocument7 pagesGhosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthCinthia MtzNo ratings yet
- A Portrayal of Gender and A Description of Gender Roles in SelectDocument429 pagesA Portrayal of Gender and A Description of Gender Roles in SelectPtah El100% (1)
- PDF Certificacion 3dsmaxDocument2 pagesPDF Certificacion 3dsmaxAriel Carrasco AlmanzaNo ratings yet
- Geographical Milieu of Ancient KashiDocument14 pagesGeographical Milieu of Ancient Kashismk11No ratings yet
- 100 Commonly Asked Interview QuestionsDocument6 pages100 Commonly Asked Interview QuestionsRaluca SanduNo ratings yet
- Does Moore Succeed in Refuting IdealismDocument5 pagesDoes Moore Succeed in Refuting IdealismharryNo ratings yet
- MSC Nastran 20141 Install GuideDocument384 pagesMSC Nastran 20141 Install Guiderrmerlin_2No ratings yet
- NIPMR Notification v3Document3 pagesNIPMR Notification v3maneeshaNo ratings yet
- Total Recall and SkepticismDocument4 pagesTotal Recall and Skepticismdweiss99No ratings yet
- Modbus Manual TD80 PDFDocument34 pagesModbus Manual TD80 PDFAmar ChavanNo ratings yet
- Dwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFDocument36 pagesDwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFscreamsoaring.pm7hcv100% (13)
- They Cried MonsterDocument13 pagesThey Cried MonstermassuroNo ratings yet
- Simple Linear Equations A Through HDocument20 pagesSimple Linear Equations A Through HFresgNo ratings yet
- Ped Xi Chapter - 3Document15 pagesPed Xi Chapter - 3DebmalyaNo ratings yet
- MC2 Sewing Patterns: Dressmaking Learning ModuleDocument91 pagesMC2 Sewing Patterns: Dressmaking Learning ModuleMargie JariñoNo ratings yet
- Lesson Plan 2 Revised - Morgan LegrandDocument19 pagesLesson Plan 2 Revised - Morgan Legrandapi-540805523No ratings yet
- 9 Prospect EvaluationDocument40 pages9 Prospect EvaluationgeorgiadisgNo ratings yet
- The Old Man and The SeaDocument6 pagesThe Old Man and The Seahomeless_heartNo ratings yet
- MNLG 4Document2 pagesMNLG 4Kanchana Venkatesh39% (18)
- 1654557191.969365 - Signed Contract Application 212143Document11 pages1654557191.969365 - Signed Contract Application 212143ella may sapilanNo ratings yet
- PDF Document 2Document12 pagesPDF Document 2Nhey VergaraNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)