Professional Documents
Culture Documents
Psychological Impact of COVID-19 On Children and A
Uploaded by
Arantxa Caycho FigueroaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Psychological Impact of COVID-19 On Children and A
Uploaded by
Arantxa Caycho FigueroaCopyright:
Available Formats
Review Article
Psychological Impact of COVID-19 on Children
and Adolescents: A Systematic Review
Nishtha Chawla1 , Ashlyn Tom1, Mahadev Singh Sen1 and Rajesh Sagar1
ABSTRACT correlating with anxiety/depression. transmission, based on evidence gath-
Efforts to address bias, discussion on ered from past influenza outbreaks,
Background and aims: The outbreak of generalizability of their results, and sample school closures were prolonged, even
COVID-19 led to a significant psychological size calculation were not reported in most
impact on individuals, particularly those when various lockdown measures were
studies.
belonging to vulnerable groups. This study lifted. The psychosocial impact of the
aimed to synthesize literature on the Conclusion: Psychological impact on pandemic and the social isolation on chil-
psychological impact of COVID-19 among children/adolescents is significant, either dren are innumerable, including sleep
children and adolescents. due to the fear of the illness or social problems, depressive and anxiety symp-
isolation related to COVID-19. One may toms, worsening of preexisting psychiat-
Methods: Electronic search engines were
focus on improving sleep habits and
used to identify studies till March 2021 that ric symptoms, etc.3,4 Some authors have
physical activity and regulating internet
reported symptoms of psychological origin even proposed a silver lining to the clo-
use for maintaining psychological well-
in children and adolescents. Information sure of schools and home confinement,
being.
was extracted using a predefined template, such as delay in initiation of substance
and qualitative analysis was conducted Keywords: COVID-19, social-isolation,
use and higher opportunity for the par-
using STROBE. children, adolescents, psychological impact
ents to bond with their children.5
A
Results: One hundred and two relevant fter the COVID-19 outbreak There is now adequate literature on
papers were identified. Most of the studies was declared a pandemic by the the psychological impact of COVID-19
were conducted online or telephonically.
World Health Organization on children and adolescents. Various sys-
The study designs were primarily single
group cross-sectional, though a few (WHO) in March 2020,1 to contain the tematic reviews have been done focusing
prospective/retrospective designs spread of this infection, nations across on the psychosocial impact of COVID-19
were also identified. Studies assessing the globe have adopted various measures on children/adolescents.6,7 However, one
emotional distress showed variable levels including nationwide lockdown, school of them focused only on one set of pop-
of anxiety and depressive symptoms in closures, online lectures, and postpone- ulation, that is, adolescents only,7 and
the study population, with greater severity ment of elective procedures. This has the other was conducted after only three
of anxiety symptoms among females
led to a psychological impact on various months of declaration of the pandemic,6
and older adolescents. Reduced physical
populations, particularly the vulnera- resulting in a modest sample size of 4
activity; delayed sleep time; increased
sleep duration, screen time, internet use, ble groups, like children, older adults, and 12 studies, respectively. Moreover,
and sedentary habits, poor quality of and healthcare and frontline workers.2 the search terms used in these reviews
life were other notable findings, often In order to break the chain of social have either been ill-defined or limited
Dept. of Psychiatry, All India Institute of Medical Sciences, New Delhi, Delhi, India.
1
HOW TO CITE THIS ARTICLE: Chawla N, Tom A, Sen MS, Sagar R. Psychological Impact of COVID-19 on Children and Adolescents:
A Systematic Review. Indian J Psychol Med. 2021;XX:1–6.
Address for correspondence: Rajesh Sagar, Dept. of Psychiatry, All India Institute Submitted: 15 Jan. 2021
of Medical Sciences, New Delhi, Delhi 110001, India. E-mail: rsagar29@gmail.com Accepted: 14 May. 2021
Published Online: xxxx
Copyright © The Author(s) 2021
Creative Commons Non Commercial CC BY-NC: This article is distributed under the terms of the Creative ACCESS THIS ARTICLE ONLINE
Commons Attribution- NonCommercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/)
Website: journals.sagepub.com/home/szj
which permits non-Commercial use, reproduction and distribution of the work without further permission
provided the original work is attributed as specified on the SAGE and Open Access pages (https:// DOI: 10.1177/02537176211021789
us.sagepub.com/en-us/nam/open-access-at-sage).
Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021 1
Chawla et al.
in number which might have resulted in “symptoms of emotional distress, such as and any discrepancies were resolved by
the extraction of very few studies. With anxiety/depression/post-traumatic stress mutual consensus. The findings were
ever-emerging literature on this topic, it disorder experienced by the patients, or summarized and synthesized, and pre-
is imperative to update and synthesize behavioral changes such as irritability, sented in the form of tables. Quantitative
the findings to date. Thus, the present increased use of internet or increased synthesis (meta-analysis) of the literature
review aims to appraise the literature screen time, onset or increase in was not done as a part of the review.
from across the globe on the psychologi- substance-related behavior observed
cal impact of COVID-19 and its associated by the parents/guardians, or changes Results
situations, like social isolation and quar- in sleep pattern, quality, and duration.” Our literature search found 102 relevant
antine, on children and adolescents, and Studies on experiences of children or studies pertaining to the psychological
descriptively assess their quality. adolescents, and parents’ perception of impact of COVID-19 on children/ado-
behavioral changes in their children were lescents. Out of these 102 studies, four,
Materials and Methods also included. Both direct (being infected showing results from original research
with COVID-19) and indirect (social iso- work, were published as letters to the
Search Strategy lation, quarantine, school closure) effects editor. The studies are presented in
The PRISMA guidelines for system- of COVID-19 were considered for inclu- Tables S1–S4, categorized into behav-
atic reviews and meta-analysis were sion. ioral problems (Table S1), emotional
employed for the conduct of the litera- Studies done in children/adoles- problems (Table S2), sleep problems
ture search following a systematic and cents with psychiatric (Attention deficit (Table S3), and findings on well-being/
structured approach.8 Major medical, hyperactivity disorder, autism, intellec- resilience/coping/quality of life/correla-
health, and psychological literature tual disability, etc.) or physical (obesity, tions with parental stress (Table S4).
databases, PubMed and Cochrane, cystic fibrosis, cancer, etc.) comorbidity From the studies conducted on both
were searched using the MeSH were excluded. We also excluded record- parents and children/adolescents, only
terms (((“COVID-19”[Title/Abstract] OR based studies assessing changes in the the findings pertaining to children’s/
“COVID-2019”[Title/Abstract] OR “severe rates or statistics of an event (e.g., emer- adolescents’ mental health have been
acute respiratory syndrome coronavi- gency visits, suicide rates, maltreatment highlighted in the tables.
rus 2”[Title/Abstract] OR “2019-nCoV” cases, etc.) Studies assessing the phys- Maximum studies (n = 27) were con-
[Title/Abstract] OR “SARS-CoV2”[Title/ ical effects, immunological markers, ducted in China. The study design in
Abstract] OR “2019nCoV”[Title/Abstract] or genetics of COVID-19, and studies most studies was single cross-sectional
OR “coronavirus”[Title/Abstract])) AND carried out on adults (more than 18 years) observational, except eleven studies that
((“Children”[Title/Abstract] OR “Child” were excluded from the review. Studies had a prospective/retrospective design
[Title/Abstract] OR “Adolescent”[Title/ assessing anxiety among parents or (retrospective data being commonly
Abstract] OR “Toddler”[Title/Abstract] caregivers of children with special needs taken from electronic health records).9–19
OR “Preschooler”[Title/Abstract] OR during COVID-19 were also excluded. Almost all of them were conducted
“Paediatric”[Title/Abstract]))) AND ((psy- Articles written in languages other than through online survey or telephonic
chiatr* OR psycholog* OR mental OR English were also excluded. Inclusion in interviews. The sample size ranged from
“mental health” OR “mental illness” OR the final review was done after assessing 61 to nearly 10,000. One study even had
“mental outcomes” OR “mental disor- the titles, abstracts, and full text of the an enormous sample size of 1,199,320.20
der” OR depress* OR anxiety OR stress* articles. After the search, the reference Age range of the sample population
OR “posttraumatic stress” OR PTSD OR lists of the shortlisted articles were also ranged from 6 to 18 years in majority of
wellbeing OR well-being OR mood* scanned for papers that might have been the studies. However, preschoolers were
OR insomnia OR “coping” OR “Sleep” missed. also enrolled in some studies.10,16,21–24 In
OR “Eating disorder” OR “behavioral certain studies, adolescents were taken
changes” OR “ADHD” OR “Autism” OR
Data Extraction and up to 20–24 years of age.25–27 In majority
“Intellectual disability”)) till March 12th, Qualitative Assessment of the studies, parents were assessed or
interviewed solely or additionally about
2021. In addition, we also searched for
Data extraction was carried out by three the changes in their wards’ behavior
these terms in the WHO Global Health
authors (NC, MSS, AT) independently. patterns and emotions. Average age
research database on COVID-19.
Quality appraisal of the included studies of parents was in late thirties or early
was carried out using the Strengthening
Selection Criteria the Reporting of Observational Studies
forties in most studies.
The majority of studies assessing
Observational and exploratory quan- in Epidemiology (STROBE) checklist symptoms of distress looked into the
titative studies with their full texts in for quantitative studies by two authors prevalence of depressive and anxiety
English language were searched. The (AT and MSS). Parameters explored by symptoms during COVID-19. Behavioral
studies with focus on psychological each author included authors with the changes most often assessed included
effects, stress, communication issues, year and place of study, type of study, screen time or internet use and changes
or sleep disturbances in children/ study participants, the parameter being in physical activities, which showed
adolescents were included. Psycho- assessed, and each study’s results. Com- correlations with emotional symptoms’
logical impact was operationalized as pilation by each author was compared, severity. While the most commonly used
2 Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021
Review Article
scales for emotional and behavioral prob- situations on sleep. Most studies assess- Among individual psychological
lems were Patient Health Questionnaire, ing sleep patterns and quality showed symptoms, depressive symptoms were
7-item Generalized anxiety disorder worsening in the form of increased sleep the most prevalent in most studies, fol-
scale, Screen for Child Anxiety Related latency and duration of sleep (increase lowed by anxiety symptoms. However,
Emotional Disorders, and Strengths in sleep timings) and a reduced overall different scales that measure vari-
and Difficulties Questionnaire, the most sleep quality. able constructs were used in different
common assessment method across surveys. Moreover, the findings have
different types of studies remained Studies on Quality of been synthesized from different parts
self-constructed questionnaires. of the globe and at different time points
Life/Well-being/Coping/ (immediately during lockdown to
Studies on Behavioral Resilience months after lockdown), thus explaining
Changes with Emotional Table S4 shows miscellaneous studies the spatial, cultural, and temporal varia-
tions in the findings. It is also important
Changes identified on quality of life, coping, resil-
to take into consideration the type of
ience, association with parental practices,
Table S1 shows the summary of studies survey, the age group evaluated (pre-
and stress. Most studies showed a poorer
assessing behavioral changes along with schoolers/school-going/adolescents),
quality of life, stress correlating with
emotional changes during COVID-19. parental factors (employment, educa-
parental practices, and parental stress.
While self-constructed questionnaire tion, psychological state, relationship
However, most adolescents, as per differ-
was the most common form of assess- with the child), the influence of social
ent studies, showed adaptive behavior
ment used in the studies, SDQ was the media and news in the region, and
and positive coping.
most common standardized scale used various other cross-cultural factors (type
of family, number of siblings, living with
to assess behavioral difficulties. The Qualitative Assessment grandparents, family values, and usual
commonest changes found in behav-
ior included reduced physical activity, The quality assessment of the studies bonding between children, parents, and
increased sedentary habits, and increased is shown in Table S5 (excludes data other household members). All such
screen time or technology/social media published in the form of letters to the factors have been found to influence the
usage. One study discussed increased editor). The clear rationale for conduct- emotional health of children and adoles-
intake of alcohol and cannabis.28 Some ing the study, assessment instruments, cents, as depicted in our review.
studies also showed increased use of and outcome data were clearly defined An increase in the time spent using
social media, television, and smart- in all the studies (100%). Some elements social media and smart phones and a
phone among children, often correlating were missed by almost 40%–50% of the sedentary lifestyle correlated with symp-
with severity of anxiety. Association of studies, such as describing the study type toms of anxiety and depression. Exercise
increased stress or symptoms of emo- and population discretely in their title, has been shown to reduce the symp-
tional distress with reduced physical clear specification of the study’s objec- toms of anxiety and depression.32 Lack
activity was a common finding. tives, and discussing the generalizability of exercise and physical activity during
of the findings. Efforts to address poten- the COVID-19-associated restrictions
Symptoms of Emotional tial sources of bias, and how the sample may have confounded or aggravated the
Distress association of anxiety/depression with
size was arrived at, were explained in
COVID-19 and related situations. Lack
less than 12% of studies.
Table S2 shows the summary of studies of outdoor activities paved the way for
assessing symptoms of emotional dis-
tress. Overall findings showed variable
Discussion more indoor activities for children/ado-
lescents. The increased amount of time
levels of anxiety and depressive symp- The current review represents litera- spent using smartphones/internet has
toms in the study population, with a few ture about the psychological impact on implications in leading to poor mental
studies estimating that nearly half the children/adolescents during the time health.33 The same findings have also
individuals studied had depressive or of COVID-19. Psychological impact been replicated by the studies included
anxiety symptoms. The most common during COVID-19 seems to be partially in the review. However, the conclusions
range, however, was 10%–30%. Most driven by the fear related to COVID- must be made keeping in mind that the
studies used a screening questionnaire 19 and partially, the indirect effect of internet is also the source of education
and stated their findings as “symptoms” COVID-19, that is, the situations created for most school-going children during
rather than “disorder.” The majority of in the environment due to lockdown, the COVID-19 pandemic.
studies that assessed sex and age dif- school closures, quarantine, etc.29,30 A Various studies had focused on dis-
ferences in the psychological impact wide variety of symptoms have been turbances in children’s/adolescents’
showed greater severity, particularly of reported amongst children in varying sleep during COVID-19. Delayed sleep
anxiety symptoms, among females and severity and prevalence, as depicted in timings, increased duration, worsening
older adolescents. the current review. These findings echo of sleep quality, and disruption or rever-
the findings from the adult population, sal of circadian rhythm (all correlating
Impact on Sleep estimating higher rates of depressive with the levels of stress or psychological
Table S3 summarizes studies done on and anxiety symptoms than the general symptoms) were some common find-
the impact of COVID-19 and its related population.31 ings across studies (Table S3). Similarly,
Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021 3
Chawla et al.
delay in sleep timings, loss of sleep, and on adequate sleep habits and physical longitudinal course of psychological
disruption of the circadian rhythm also activity within the limits of physical dis- symptoms, especially in connection
negatively affect psychological health.34 tancing for improving mental well-being to the changes in the prevailing situa-
Delayed sleep onset has been associated in children/adolescents. Also, due to fear tion (lockdown/relaxation in lockdown
with depressive symptoms.35 So, the of contracting COVID-19, one may not restrictions, home isolation/hospital-
association of sleep disturbances with seek professional help for their children’s ization, closure/re-opening of schools).
COVID-19 as identified in our review behavioral and emotional changes. Studies may also look at the help-seeking
may be an association of symptoms Second, those who are fearful may para- regarding the psychological symptoms
of emotional disturbance occurring in doxically be less compliant with hygiene associated with COVID-19.
response to COVID-19-related restric- and preventive measures. Such children Some limitations of the present review
tions, a consequence of increased screen must be screened for any psychologi- should be considered while drawing
time/sedentary lifestyle, or an indepen- cal symptoms. Third, parents should be inferences from the findings. We did
dent phenomenon. advised to use the “free time” to better not conduct a meta-analysis of the study
In addition to the assessment of psy- bond with their children so that they are findings, which did not allow summary
chological impact, some studies also not engaged in excessive use of social analysis. In addition to PubMed and
evaluated the children’s knowledge media, which has been shown to cor- Cochrane, only the WHO Global Health
about COVID-19, their source of infor- relate with higher severity of anxiety and research database on COVID-19 was the
mation, and their compliance to the depressive symptoms.
database used in searching the articles.
measures dictated to prevent the spread Some gaps in the current literature
Thus, some studies might have been
of COVID-19.36–39 While a large majority include the limited number of prospec-
missed, though we attempted to gather
were seen to be following at least some tive studies. Prospective assessment of
all relevant literature. Also, we did not
social distancing, most of them were not psychological symptoms over time as
venture into the impact of COVID-19
able to follow all the measures outlined the environmental situations change
and its related situations on patients
to prevent the spread. A sense of social (e.g., reduction in media coverage of
with preexisting psychiatric/physical
responsibility was seen to be associated COVID-19-related morbidities/mortal-
illness and studies on the prevalence of
with a higher prevalence of following ity, relaxation in lockdown restrictions,
COVID-19 among psychiatry in-patients/
the hygiene and sanitization measures as opening of schools) is worth exploring.
out-patients, if any. Only articles written
well as social distancing. Similar findings Similarly, prospective assessment of chil-
in the English language were consid-
have been observed in adults aged 18–59 dren with preexisting psychiatric illness
or family history of psychiatric illness ered for this review. The studies’ quality
years who reported avoiding going out
may provide new insights into the issue. appraisal was done using the STROBE
(74.2%), going to crowded places (72.7%),
and attending social gatherings of more In addition, almost all the studies have checklist, which is actually a reporting
than four people (59.7%). It has been seen been conducted online, which have been guideline for quantitative studies. But
that poor social distancing measures are suspected of overestimating the actual since there are no other tools available
associated with higher levels of anxiety prevalence.42 Although operationally to assess the quality of such studies com-
and depressive symptoms in adults.40 questionable, but with the opening up prehensively and since it is commonly
Quality appraisal of the studies was of routine out-patient services, physical used in similar studies, we had to resort
done using STROBE. The quality of the interview and assessment may help in a to the same.
included studies can have implications more accurate estimation of psychologi-
on the generalizability of the results. cal impact related to COVID-19. Conclusion
This makes it important to assess the Moreover, studies that have assessed
quality of the studies in a review. Sample smartphone/internet usage during COVID-19 impacts the mental health of
size calculation was not attempted in COVID-19 have not separately evalu- youth, particularly causing symptoms of
many studies, while almost none of the ated the time spent on a smartphone anxiety and depression. The teachers or
studies reported any attempts to address for education-related activities. In addi- parents should also be vigilant to iden-
potential bias. The titles of many studies tion, a variety of instruments have been tify behavioral and emotional changes
were inadequate, lacking particularly in used for assessment, which makes com- in their students or children during this
specifying the type of study. In almost parisons difficult, and concurrence of time so that early management can be
half of the included studies, the authors psychological symptoms according to sought. Measures may also be taken up at
had not specified discrete objectives and various scales should also be studied. the government and administrative level
often failed to comment upon the gener- Another gap in the current literature to screen vulnerable children, like those
alizability of their findings. is the lack of studies that assessed the infected with COVID-19, or with COVID-
There are several implications from correlation of clinical variables, like 19 affected family members/parents, or
the present review. First and foremost, temperament, family history, COVID those with a family history of psychiatric
psychological symptoms of distress are status/severity, etc., with psychological illness. It is imperative to gather more
common in children during COVID-19 dysfunction. To our knowledge, only empirical evidence on the impact of the
and have been found to be higher than one study has been done till now on pandemic on youth’s mental health,
in the general population in the pre- COVID positive children/adolescents.43 using robust study designs and stan-
COVID era.41 It is important to focus Future research should explore the dardized assessment tools.
4 Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021
Review Article
9. Poulain T, Meigen C, Sobek C, et al. Loss lockdown in France: (how) did they
Declaration of Conflicting Interests
of childcare and classroom teaching change? Appetite 2021; 161: 105132.
The authors declared the following potential during the Covid-19-related lockdown 19. Liu Z, Tang H, Jin Q, et al. Sleep of pre-
conflicts of interest with respect to the research,
in spring 2020: a longitudinal study on schoolers during the coronavirus disease
authorship, and/or publication of this article: The
consequences on leisure behavior and 2019 (COVID-19) outbreak. J Sleep Res
manuscript has been read and approved by all the
authors, the requirements for authorship have schoolwork at home. PLoS One 2021; 16: 2021; 30(1): e13142.
been met and the manuscript represents honest e0247949. 20. Qin Z, Shi L, Xue Y, et al. Prevalence and
work. The author declares that the paper submit- 10. Markovic A, Mühlematter C, Beaugrand risk factors associated with self-reported
ted has not been published, simultaneously sub- M, et al. Severe effects of the COVID-19 psychological distress among children
mitted or accepted for publication elsewhere. We confinement on young children’s sleep: and adolescents during the COVID-19
also declare that the manuscript, to the best of pandemic in China. JAMA Netw Open
a longitudinal study identifying risk and
our knowledge, does not infringe upon any copy-
protective factors. J Sleep Res 2021; 18: 2021; 4: e2035487–e2035487.
right or property right of any third party.
e13314. 21. Dellagiulia A, Lionetti F, Fasolo M,
11. Magson NR, Freeman JYA, Rapee RM, et al. Early impact of COVID-19 lock-
Funding
et al. Risk and protective factors for pro- down on children’s sleep: a 4-week longi-
The authors received no financial support for the tudinal study. J Clin Sleep Med 2020; 16:
research, authorship, and/or publication of this spective changes in adolescent mental
health during the COVID-19 pandemic. J 1639–1640.
article.
Youth Adolesc 2021; 50: 44–57. 22. Glynn LM, Davis EP, Luby JL, et al.
12. Lorenzo NE, Zeytinoglu S, Morales S, A predictable home environment may
Supplemental Material
et al. Transactional associations between protect child mental health during the
Supplemental material for this article is available COVID-19 pandemic. Neurobiol Stress
online. parent and late adolescent internaliz-
2021; 14: 100291.
ing symptoms during the COVID-19
23. Di Giorgio E, Di Riso D, Mioni G, et al.
ORCID iD pandemic: the moderating role of
The interplay between mothers’ and
avoidant coping. J Youth Adolesc 2021;
Nishtha Chawla https://orcid.org/0000-0002- children behavioral and psychological
50: 459–469.
9009-4105 factors during COVID-19: an Italian
13. Giménez-Dasí M, Quintanilla L, Lucas-
study. Eur Child Adolesc Psychiatry
Molina B, et al. Six weeks of confine-
References ment: psychological effects on a sample
24.
2020; 31: 1–2.
Tso WWY, Wong RS, Tung KTS, et al.
of children in early childhood and
1. Timeline: WHO’s COVID-19 response Vulnerability and resilience in children
primary education. Front Psychol 2020;
[Internet]. https://www.who.int/ during the COVID-19 pandemic. Eur
11. DOI: 10.3389/fpsyg.2020.590463
emergencies/diseases/novel- Child Adolesc Psychiatry 2020; 17: 1–6
14. Chen I-H, Chen C-Y, Pakpour AH, et al.
coronavirus-2019/interactive-timeline 25. Gotlib IH, Borchers LR, Chahal R,
Problematic internet-related behaviors
(2019, accessed 27 October 2020) et al. Early life stress predicts depressive
mediate the associations between levels
2. Kuy S, Tsai R, Bhatt J, et al. Focusing on symptoms in adolescents during the
of internet engagement and distress
vulnerable populations during COVID- COVID-19 pandemic: the mediating role
among schoolchildren during COVID- of perceived stress. Front Psychol 2020;
19. Acad Med. 2020; 95(11): e2–e3.
19 lockdown: a longitudinal structural 11: 603748.
3. Gupta S and Jawanda MK. The impacts
equation modeling study. J Behav Addict 26. Matovu JKB, Kabwama SN, Ssekamatte
of COVID-19 on children. Acta Paediatr
2021; 10. DOI: 10.1556/2006.2021.00006 T, et al. COVID-19 awareness, adoption
2020; 109(11): 2181–2183.
15. Chen I-H, Chen C-Y, Pakpour AH, et al. of COVID-19 preventive measures, and
4. Ghosh R, Dubey M, Chatterjee S, et al.
Internet-related behaviors and psycho- effects of COVID-19 lockdown among
Impact of COVID-19 on children: special
focus on psychosocial aspect. Minerva logical distress among schoolchildren adolescent boys and young men in
Pediatr 2020; 72: 226–235. during COVID-19 school suspension. J Kampala, Uganda. J Community Health
5. Chawla N, Sharma P, and Sagar R. Am Acad Child Adolesc Psychiatry 2020; 2021; 22: 1–2
Psychological impact of COVID-19 on 59: 1099–1102.e1. 27. Commodari E and La Rosa VL.
Children and adolescents: is there a 16. Aguilar-Farias N, Toledo-Vargas Adolescents in quarantine during
silver lining? Indian J Pediatr 2021; M, Miranda-Marquez S, et al. COVID-19 pandemic in Italy: perceived
88(1): 91. Sociodemographic predictors of changes health risk, beliefs, psychological expe-
6. Nearchou F, Flinn C, Niland R, et al. in physical activity, screen time, and riences and expectations for the future.
Exploring the impact of COVID-19 on sleep among toddlers and preschoolers Front Psychol 2020 Sep 23; 11: 2480
mental health outcomes in children and in Chile during the COVID-19 pandemic. 28. Dumas TM, Ellis W, and Litt DM. What
adolescents: a systematic review. Int Int J Environ Res Public Health 2021; does adolescent substance use look
J Environ Res Public Health 2020; 17: 18: 176. like during the COVID-19 pandemic?
8479. 17. Alves J, Yunker AG, DeFendis A, et al. Examining changes in frequency, social
7. Octavius GS, Silviani FR, Lesmandjaja Children’s anxiety and physical activity contexts, and pandemic-related predic-
A, et al. Impact of COVID-19 on ado- during COVID-19 in relation to prena- tors. J Adolesc Health 2020; 67:
lescents’ mental health: a systematic tal exposure to gestational diabetes. 354–361.
review. Middle East Curr Psychiatry medRxiv. Epub ahead of print August 29. Carvalho Aguiar Melo M and de Sousa
2020; 27: 72. 7, 2020. http://medrxiv.org/lookup/ Soares D. Impact of social distancing
8. Moher D, Shamseer L, Clarke M, et al. doi/10.1101/2020.08.06.20169565 on mental health during the COVID-19
Preferred reporting items for systematic 18. Philippe K, Chabanet C, Issanchou S, pandemic: an urgent discussion. Int J
review and meta-analysis protocols et al. Child eating behaviors, parental Soc Psychiatry 2020; 66: 625–626.
(PRISMA-P) 2015 statement. Syst Rev feeding practices and food shopping 30. Vernooij-Dassen M, Verhey F, and
2015; 4(1): 1. motivations during the COVID-19 Lapid M. The risks of social distancing
Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021 5
Chawla et al.
for older adults: a call to balance. Int young people. BMC Psychiatry 2014; Italian adolescents’ attitudes and behav-
Psychogeriatr 2020; 32(10): 1235–1237. 14: 33. iors. Ital J Pediatr 2020; 46: 69.
31. Rajkumar RP. COVID-19 and mental 36. Saurabh K and Ranjan S. Compliance 40. Zhao SZ, Wong JYH, Wu Y, et al. Social
health: a review of the existing litera- and psychological impact of quaran- distancing compliance under COVID-19
ture. Asian J Psychiatry 2020; 52: 102066. tine in children and adolescents due pandemic and mental health impacts:
32. Sharma A, Madaan V, and Petty FD. to Covid-19 pandemic. Indian J Pediatr a population-based study. Int J Environ
Exercise for mental health. Prim Care 2020; 87: 532–6. Res Public Health 2020 Jan; 17(18): 6692.
Companion J Clin Psychiatry 2006; 8: 37. Esposito S, Giannitto N, Squarcia A, 41. Merikangas KR, Nakamura EF, and
106. et al. Development of psychological Kessler RC. Epidemiology of mental
33. Sohn SY, Rees P, Wildridge B, et al. problems among adolescents during disorders in children and adolescents.
Prevalence of problematic smartphone school closures because of the COVID-19 Dialogues Clin Neurosci 2009; 11: 7–20.
usage and associated mental health lockdown phase in Italy: a cross- 42. Sagar R, Chawla N, and Sen MS. Is it
outcomes amongst children and young sectional survey. Front Pediatr 2021 correct to estimate mental disorder
people: a systematic review, meta-anal- Jan 22; 8: 975. through online surveys during COVID-
ysis and GRADE of the evidence. BMC 38. Xue Q, Xie X, Liu Q, et al. Knowledge, 19 pandemic? Psychiatry Res 2020; 291:
Psychiatry 2019; 19: 356. attitudes, and practices towards 113251.
34. Walker WH, Walton JC, DeVries AC, COVID-19 among primary school 43. Kılınçel Ş, Altun FT, Nuryüz Ö, et
et al. Circadian rhythm disruption and students in Hubei Province, China. al. Effects of COVID-19 outbreak on
mental health. Transl Psychiatry 2020; Child Youth Serv Rev 2021; 120: children’s mental health: a comparative
10: 1–13. 105735. study with children diagnosed and
35. Glozier N, O’Dea B, McGorry PD, et 39. Buzzi C, Tucci M, Ciprandi R, et al. The isolated from their parents. Psychiatry
al. Delayed sleep onset in depressed psycho-social effects of COVID-19 on Investig 2021; 18: 140–146.
6 Indian Journal of Psychological Medicine | Volume XX | Issue X | XXXX-XXXX 2021
You might also like
- Jurnal InterDocument8 pagesJurnal InterRinna MerlinNo ratings yet
- Investigating The Mental Health of Nesh Shs Students With Covid Postivie Relatives Final VersionDocument23 pagesInvestigating The Mental Health of Nesh Shs Students With Covid Postivie Relatives Final VersionDiwata BuenviajeNo ratings yet
- How Is COVID-19 Pandemic Impacting Mental Health of ChildrenDocument9 pagesHow Is COVID-19 Pandemic Impacting Mental Health of ChildrenSuzanne LauNo ratings yet
- 2021 - Investigacion - Publicaciones - Detectaweb DistressDocument14 pages2021 - Investigacion - Publicaciones - Detectaweb DistressJose Antonio Piqueras RodríguezNo ratings yet
- Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic ReviewDocument16 pagesMental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic ReviewHeartgwea BuladacoNo ratings yet
- Ajph 2020 306037Document2 pagesAjph 2020 306037smmendoncaNo ratings yet
- Mental Health - Journal FormatDocument9 pagesMental Health - Journal FormatMarivic Bagtas GachoNo ratings yet
- Impact of LockdownDocument6 pagesImpact of LockdownBastenvnNo ratings yet
- The Perceived Effects of COVID-19 To Mental Health of Grade 9 Students and ParentsDocument8 pagesThe Perceived Effects of COVID-19 To Mental Health of Grade 9 Students and ParentsPsychology and Education: A Multidisciplinary JournalNo ratings yet
- El Adolescente Covid PDFDocument24 pagesEl Adolescente Covid PDFLyd PensadoNo ratings yet
- NCM 111 LEC - Research ActivityDocument3 pagesNCM 111 LEC - Research ActivityBea HernandezNo ratings yet
- CovidDocument7 pagesCovidLILIANA IVONNE FLORES MOLINANo ratings yet
- Rapid Systematic Review: The Impact of Social Isolation and Loneliness On The Mental Health of Children and Adolescents in The Context of COVID-19 (2020)Document26 pagesRapid Systematic Review: The Impact of Social Isolation and Loneliness On The Mental Health of Children and Adolescents in The Context of COVID-19 (2020)Alberto Martínez GNo ratings yet
- Ijerph 19 16154Document11 pagesIjerph 19 16154Keisha Azzahra TetadrianNo ratings yet
- Related Studies AyeeeDocument6 pagesRelated Studies AyeeeNoelle CaballeraNo ratings yet
- Is There A Silver Lining in This Cloud? Future Expectations of Adolescents With Human Immunodeficiency VirusDocument5 pagesIs There A Silver Lining in This Cloud? Future Expectations of Adolescents With Human Immunodeficiency VirusJanardhan NNo ratings yet
- Fear of LonelinessDocument25 pagesFear of LonelinessHà Anh Lê VũNo ratings yet
- Depresión y Covid 19 CELL PRESSDocument9 pagesDepresión y Covid 19 CELL PRESSRonnieVidelaNo ratings yet
- Sintomas de Ansiedad y Depresion Post PandemiaDocument7 pagesSintomas de Ansiedad y Depresion Post Pandemiayahaira marquezNo ratings yet
- Age Advantages in Emotional Experience Covid 2020Document12 pagesAge Advantages in Emotional Experience Covid 2020Estevão SaviottiNo ratings yet
- 1 s2.0 S0165178122004073 MainDocument16 pages1 s2.0 S0165178122004073 MainEgy Sunanda Putra Direktorat Poltekkes JambiNo ratings yet
- To Study The Effect of Lockdown On Physical, Mental and Emotional Health of Common PeopleDocument9 pagesTo Study The Effect of Lockdown On Physical, Mental and Emotional Health of Common PeopleInternational Journal of Innovative Science and Research Technology100% (1)
- Impact of COVID-19 and Lockdown On Mental Health of Children and Adolescents: A Narrative Review With RecommendationsDocument10 pagesImpact of COVID-19 and Lockdown On Mental Health of Children and Adolescents: A Narrative Review With RecommendationsS. M. MUNAWAR MAHTAB 1603061100% (1)
- The Impact of Post Covid 19 On Youth's Mental IllnessDocument10 pagesThe Impact of Post Covid 19 On Youth's Mental Illness23005583No ratings yet
- The Mental Stability of Grade Eleven Students Who Chose Blended Mode of Learning in San Roque National High School in Antipolo City, S.Y.2020-2021Document19 pagesThe Mental Stability of Grade Eleven Students Who Chose Blended Mode of Learning in San Roque National High School in Antipolo City, S.Y.2020-2021SRHeart Nikcole Dela PazNo ratings yet
- Proponent:: Nabasca, Charry M. Villacrusis, Charyl P. Bulataolo, Glory MieDocument5 pagesProponent:: Nabasca, Charry M. Villacrusis, Charyl P. Bulataolo, Glory MieCherry Ann Marcial NabascaNo ratings yet
- Mental Health of Adolescents During Lockdown Period of Covid 19Document10 pagesMental Health of Adolescents During Lockdown Period of Covid 19nikhil yadavNo ratings yet
- Zhang 2020Document9 pagesZhang 2020hanafinurrahmadNo ratings yet
- Artigo PrincipalDocument9 pagesArtigo PrincipalVictoria AlmeidaNo ratings yet
- Impact of Cyberbullying On AdoDocument2 pagesImpact of Cyberbullying On Adomabarak abdisalmNo ratings yet
- Covid-19: Psychological Aspect On Health of The AdoloscentDocument5 pagesCovid-19: Psychological Aspect On Health of The AdoloscentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Literature Review For Mental HealthDocument7 pagesLiterature Review For Mental Healthastrid san joseNo ratings yet
- Basta LiteratureDocument7 pagesBasta Literatureastrid san joseNo ratings yet
- Journal of Affective Disorders: Yan Liu, Song Yue, Xiaoran Hu, Jin Zhu, Zifan Wu, Jianli Wang, Yili WuDocument6 pagesJournal of Affective Disorders: Yan Liu, Song Yue, Xiaoran Hu, Jin Zhu, Zifan Wu, Jianli Wang, Yili WuCECILIA BELEN FIERRO ALVAREZNo ratings yet
- The Prevalence of Mental Problems For Chinese Children and Adolescents During COVID-19 in China A Systematic Review and Meta-AnalysisDocument11 pagesThe Prevalence of Mental Problems For Chinese Children and Adolescents During COVID-19 in China A Systematic Review and Meta-AnalysishappyanylandNo ratings yet
- COVID-19 and Mental Health: A Multi-Country Study-The Effects of Lockdown On The Mental Health of Young AdultsDocument12 pagesCOVID-19 and Mental Health: A Multi-Country Study-The Effects of Lockdown On The Mental Health of Young Adultsjunairahali32No ratings yet
- Data Driven Assessment of Adolescents M - 2023 - Journal of The American AcademDocument18 pagesData Driven Assessment of Adolescents M - 2023 - Journal of The American AcademsmmendoncaNo ratings yet
- Biopsychosocial Factors Linked With Overall Well Being of Students and Educators During The COVID 19 PandemicDocument20 pagesBiopsychosocial Factors Linked With Overall Well Being of Students and Educators During The COVID 19 PandemicYanti Harjono100% (1)
- 2changes in Emotions and Worries During The Covid-19 Pandemic - An Online-Survey With Children and Adults With and Without Mental Health ConditionsDocument10 pages2changes in Emotions and Worries During The Covid-19 Pandemic - An Online-Survey With Children and Adults With and Without Mental Health Conditionswhether913No ratings yet
- Tuhay Na Talaga IniDocument16 pagesTuhay Na Talaga IniTatsuo YamazakiNo ratings yet
- Journal of Psychosomatic ResearchDocument11 pagesJournal of Psychosomatic ResearchEvy LiesniawatiNo ratings yet
- Fatimah Sri Ayu Bijak Lestari Assagaf 1Document17 pagesFatimah Sri Ayu Bijak Lestari Assagaf 1Fatimah AssagafNo ratings yet
- Effects of COVID-19 On College Students' Mental Health in The United States: Interview Survey StudyDocument14 pagesEffects of COVID-19 On College Students' Mental Health in The United States: Interview Survey StudyAndhika DNo ratings yet
- Petrocchi Bs 2021Document16 pagesPetrocchi Bs 2021Anselmo GonzalezNo ratings yet
- Uso de Pantallas y Síntomas de Salud Mental en Niños y Jóvenes Canadienses Durante La Pandemia de COVID-19Document20 pagesUso de Pantallas y Síntomas de Salud Mental en Niños y Jóvenes Canadienses Durante La Pandemia de COVID-19IVAN DARIO RODRIGUEZ SALAMANCANo ratings yet
- Child and Adolescent Anxiety As A Risk Factor For Bipolar Disorder: A Systematic Review of Longitudinal StudiesDocument11 pagesChild and Adolescent Anxiety As A Risk Factor For Bipolar Disorder: A Systematic Review of Longitudinal StudiesMaría Fernanda Parada ValenciaNo ratings yet
- Ouput1 JulietDocument6 pagesOuput1 JulietmontieropauNo ratings yet
- Self Efficacy and Optimism As Predictors of Coping With Stress As Assessed During The Coronavirus Outbreak. 2022Document15 pagesSelf Efficacy and Optimism As Predictors of Coping With Stress As Assessed During The Coronavirus Outbreak. 2022stefdNo ratings yet
- Spencer Et Al-2021-Child and Adolescent Psychiatry and Mental HealthDocument12 pagesSpencer Et Al-2021-Child and Adolescent Psychiatry and Mental HealthKJ HiramotoNo ratings yet
- Mood and Emotional Reactivity of Adolescents During The COVID-19 Pandemic Short-Term and Long-Term Effects and The Impact of Social and Socioeconomic StressorsDocument13 pagesMood and Emotional Reactivity of Adolescents During The COVID-19 Pandemic Short-Term and Long-Term Effects and The Impact of Social and Socioeconomic Stressorschristiancraig1987No ratings yet
- Stress, Online Courses and Parenting During COVID19 PandemicDocument19 pagesStress, Online Courses and Parenting During COVID19 PandemicUrban StoriesNo ratings yet
- 3rd DLSU SHS Research Congress Paper PresentationsDocument560 pages3rd DLSU SHS Research Congress Paper Presentationsanthonydatu99No ratings yet
- Child - 2022 - Hale - Physical Activity Interventions For The Mental Health of Children A Systematic ReviewDocument19 pagesChild - 2022 - Hale - Physical Activity Interventions For The Mental Health of Children A Systematic ReviewNaeema MosaNo ratings yet
- PSMUDocument12 pagesPSMUSyifaa IrawanNo ratings yet
- Fpubh 10 1040676Document14 pagesFpubh 10 1040676李玉博No ratings yet
- Mental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesDocument9 pagesMental Health of Parents and Preschool-Aged Children During The COVID-19 Pandemic The Mediating Role of Harsh Parenting and Child Sleep DisturbancesToth Fanni-BarbaraNo ratings yet
- Mental Health Status of Students' Parents During COVID-19 Pandemic and Its Influence FactorsDocument9 pagesMental Health Status of Students' Parents During COVID-19 Pandemic and Its Influence FactorspangaribuansantaNo ratings yet
- PPC 12721Document7 pagesPPC 12721John PaulNo ratings yet
- Constructing Sustainable Public Spaces Dhaka City PerspectiveDocument11 pagesConstructing Sustainable Public Spaces Dhaka City Perspectivetowhidul alamNo ratings yet
- Parental Monitoring of Adolescents: Current Perspectives for Researchers and PractitionersFrom EverandParental Monitoring of Adolescents: Current Perspectives for Researchers and PractitionersNo ratings yet
- National ScientistDocument2 pagesNational ScientistHu T. BunuanNo ratings yet
- Performance Task in Mathematics 10 First Quarter: GuidelinesDocument2 pagesPerformance Task in Mathematics 10 First Quarter: Guidelinesbelle cutiee100% (3)
- TesisDocument388 pagesTesisHadazaNo ratings yet
- Porn Sex Versus Real Sex: How Sexually Explicit Material Shapes Our Understanding of Sexual Anatomy, Physiology, and BehaviourDocument23 pagesPorn Sex Versus Real Sex: How Sexually Explicit Material Shapes Our Understanding of Sexual Anatomy, Physiology, and Behaviourzyryll yowNo ratings yet
- Reading Listening 2Document5 pagesReading Listening 2Lisbet GomezNo ratings yet
- BrookfieldDocument8 pagesBrookfieldFariha Naseer Haral - 28336/TCHR/JVAITNo ratings yet
- Supply Chain Analytics For DummiesDocument69 pagesSupply Chain Analytics For DummiesUday Kiran100% (7)
- Complexity. Written Language Is Relatively More Complex Than Spoken Language. ..Document3 pagesComplexity. Written Language Is Relatively More Complex Than Spoken Language. ..Toddler Channel TVNo ratings yet
- Functions of Ecgc and Exim BankDocument12 pagesFunctions of Ecgc and Exim BankbhumishahNo ratings yet
- Ped Xi Chapter - 3Document15 pagesPed Xi Chapter - 3DebmalyaNo ratings yet
- Afghanistan Law Bibliography 3rd EdDocument28 pagesAfghanistan Law Bibliography 3rd EdTim MathewsNo ratings yet
- FORTRESS EUROPE by Ryan BartekDocument358 pagesFORTRESS EUROPE by Ryan BartekRyan Bartek100% (1)
- EP105Use of English ArantxaReynosoDocument6 pagesEP105Use of English ArantxaReynosoArantxaSteffiNo ratings yet
- Types of CostsDocument9 pagesTypes of CostsPrathna AminNo ratings yet
- The Palatability, and Potential Toxicity of Australian Weeds To GoatsDocument163 pagesThe Palatability, and Potential Toxicity of Australian Weeds To Goatsalshokairsaad513No ratings yet
- Cyrano de BergeracDocument209 pagesCyrano de BergeracKayleeNo ratings yet
- Geographical Milieu of Ancient KashiDocument14 pagesGeographical Milieu of Ancient Kashismk11No ratings yet
- Simple Linear Equations A Through HDocument20 pagesSimple Linear Equations A Through HFresgNo ratings yet
- Caste & PoliticsDocument4 pagesCaste & PoliticsGIRISHA THAKURNo ratings yet
- Winifred Breines The Trouble Between Us An Uneasy History of White and Black Women in The Feminist MovementDocument279 pagesWinifred Breines The Trouble Between Us An Uneasy History of White and Black Women in The Feminist MovementOlgaNo ratings yet
- Paper 2Document8 pagesPaper 2Antony BrownNo ratings yet
- ECON 4035 - Excel GuideDocument13 pagesECON 4035 - Excel GuideRosario Rivera NegrónNo ratings yet
- Chiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFDocument59 pagesChiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFJuzer Songerwala100% (1)
- Case Study On TQMDocument20 pagesCase Study On TQMshinyshani850% (1)
- Norman 2017Document7 pagesNorman 2017Lee HaeunNo ratings yet
- Elements of Visual Design in The Landscape - 26.11.22Document15 pagesElements of Visual Design in The Landscape - 26.11.22Delnard OnchwatiNo ratings yet
- Fruitful Outreaches Intercessory Prayer GuidelinesDocument5 pagesFruitful Outreaches Intercessory Prayer GuidelinesPaul Moiloa100% (1)
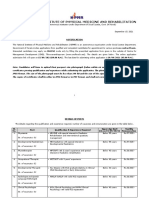
- NIPMR Notification v3Document3 pagesNIPMR Notification v3maneeshaNo ratings yet
- Gaulish DictionaryDocument4 pagesGaulish DictionarywoodwyseNo ratings yet
- Present Tenses ReviewDocument6 pagesPresent Tenses ReviewRamona DinuNo ratings yet