Professional Documents
Culture Documents
Cit0515 F4 Steinberg
Uploaded by
Nasru llahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cit0515 F4 Steinberg
Uploaded by
Nasru llahCopyright:
Available Formats
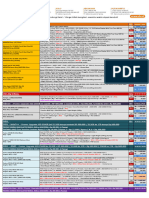
COVER STORY
Managing Complications
of Transradial
Catheterization
How to address challenges that may occur with this outcome-improving access procedure.
BY DANIEL H. STEINBERG, MD
D
uring the 25 years since the first report of success-
A B
ful coronary catheterization via the radial artery,1
transradial access for catheterization and inter-
vention has evolved from a trendy idea with spo-
radic adoption to a routine practice and standard of care.
Following on the heels of small series and meta-analyses
suggesting a reduction in bleeding and access site complica-
tions, larger studies and randomized trials have consistently
demonstrated that transradial access leads to reduced
access site complications and improved outcomes.2-6
Despite these findings, the use of transradial access in the
United States remains relatively low.7
Although there is little argument that the transradial
approach is associated with decreased access site complica-
tions, it is important to remember that it is not completely
benign. There are a number of complications that are
unique to transradial catheterization. Although the majority
of these are not clinically dramatic, they occasionally require Figure 1. Radial artery spasm (blue arrows) with perforation
dedicated management. These complications include arte- (red arrow; A). Subsequent resolution of both spasm and per-
rial injury, spasm, occlusion, perforation, hematoma, and foration (B).
pseudoaneurysm. Additionally, and perhaps more impor-
tantly, many of these can be prevented by meticulous tech- the outer diameter of most 6-F sheaths are approximately
nique in access, procedural performance, and hemostasis. 2.6 mm, and passage of multiple wires and catheters
With relatively straightforward strategies, these complica- through the radial artery raises the potential for damage.
tions can be managed without downstream issues. This A number of studies have employed intravascular imag-
article provides an overview of common transradial compli- ing techniques to assess the frequency and extent of radial
cations and outlines strategies for their management. artery injury during catheterization. In one such study,
Yonetsu et al performed optical coherence tomography
RADIAL ARTERY INJURY in 73 arteries in 69 patients. They found that 67% of radial
The radial artery ranges in diameter from 2 to 4 mm, arteries had some degree of intimal tear, whereas 35.6% of
with an average of 3.1 ± 0.6 mm and 2.8 ± 0.6 mm in men vessels exhibited medial dissection.9 Chronically, the vessels
and women, respectively.8 This is considerably smaller than were found to have thickened intimal walls consistent with
the average nondiseased common femoral artery, which healing after previous injury. The degree of injury is often
ranges from 7 to 9 mm in diameter. As a result, arterial clinically silent, and usually, no specific management strate-
injury can occur with standard equipment. For instance, gies are necessary.
58 CARDIAC INTERVENTIONS TODAY MAY/JUNE 2015
COVER STORY
RADIAL ARTERY SPASM
One of the more common complications of tran-
sradial catheterization that requires attention is spasm
(Figure 1). Even with modern equipment, including
hydrophilic sheaths, appreciable radial artery spasm
occurs in up to 20% of cases, and it remains an impor-
tant reason for procedural failure.10,11 It is most often
recognized by difficulties in accessing the vessel or
passing, manipulating, or withdrawing equipment.
Additionally, spasm may lead to catheter kinking or
entrapment because of increased resistance to catheter
movement and excessive torque necessary to manipu-
late the catheter.
The management of radial artery spasm centers on
preventive antispasmodic administration of a cocktail
consisting of nitrates and/or calcium channel blockers.
The exact formula or ratio of individual agents is largely a
matter of style. When patients develop spasm, manage- Figure 2. Radial artery occlusion with evidence of retrograde
ment options include a tincture of time, increased seda- flow through collateralization of the palmar arch (yellow
tion, additional or alternative antispasmodic medica- arrow).
tions, catheter downsizing, or abandoning the access site
altogether. In rare cases, a patient may require deep con- fied Allen test or the Barbeau test. In either case, patency
scious sedation or even intubation (in order to achieve of the ulnar artery is established before radial artery access
profound sedation) to manage spasm. to ensure adequate circulation to the hand if radial artery
In a study of 1,868 patients (56.5% of whom under- occlusion occurs. Although this remains the standard of
went percutaneous coronary intervention), 188 cases of care in many institutions, in a recent international survey,
spasm were identified. Of these, 51 cases were classified 23.4% of transradial operators do not routinely assess dual
as moderate or severe, defined as those requiring some circulation.16 Importantly, there is no definitive link between
form of dedicated intervention. The most common poor dual circulation and hand ischemia, and sufficient
intervention was additional medication (42% of cases), collateralization of the palmar arch likely exists to allow
and crossover to the contralateral radial artery or the safe transradial access in the absence of a normal Allen test
femoral artery occurred in 25% of cases.12 result.17
Nevertheless, if for no other reason other than to preserve
RADIAL ARTERY OCCLUSION the access site for future use, radial artery occlusion is ide-
Radial artery occlusion (Figure 2) is perhaps the most ally avoided. Occlusion is associated with sheath size, lack
widely discussed complication of transradial catheteriza- of or underdosing of anticoagulation, occlusive hemostasis,
tion. The perception that it occurs commonly and leads and prolonged compression times. As previously noted, the
to ischemic complications remains a significant barrier to sheath-to-artery diameter ratio of standard interventional
increased use of this technique. With modern equipment equipment is almost occlusive in a significant minority of
and technique, the incidence of radial artery occlusion patients, and small sheath sizes are associated with lower
is likely around 4% and ranges from 3% to 10%.13,14 The risks of occlusion.8 Regarding anticoagulation, Spaulding
majority of these occlusions are asymptomatic, with res- et al published their initial transradial experience in 1996.
olution in approximately 50% at 30 days.14 Symptomatic Radial artery occlusion occurred in 71% of their first 49
radial artery occlusion is uncommon, but its occurrence patients, who received no anticoagulation, and it decreased
is well documented both anecdotally and in case reports to 4% in their later 210 patients, who received 5,000 units
throughout the literature. Clinically significant sequelae of unfractionated heparin upon vascular access.18 Although
are exceedingly rare, especially in the presence of ade- the ideal dose may vary by individual preference, most agree
quate dual circulation, but ischemic complications can that procedural anticoagulation with at least 50 units/kg
occur and are usually the result of thromboembolism.15 of unfractionated heparin is necessary to reduce the risk of
One commonly employed strategy in managing (or radial artery occlusion.19
preventing the consequences of) radial artery occlusion Another important practice for reducing radial artery
is assessing dual circulation through either the modi- occlusion is that of “patent hemostasis.” Compared to
MAY/JUNE 2015 CARDIAC INTERVENTIONS TODAY 59
COVER STORY
A more immediate technique for treating occlu-
sion is forced ulnar compression. In this technique,
the patient is anticoagulated, and the hemostatic
device is shifted over to the ulnar artery, forcing flow
through the occluded radial artery. In a study of 465
patients undergoing transradial catheterization with
5-F access and randomized as part of a larger study to
either 2,000 or 5,000 units of unfractionated heparin,
all patients were assessed for radial artery patency 4
hours after the procedure with a protocol specifying
immediate 1-hour ulnar occlusion in the case of radial
artery occlusion. The overall initial occlusion rate was
4.3% (5.9% with 2,000 units vs 2.9% with 5,000 units;
P = .17). After ulnar compression, occlusion improved
to 2.4% (4.1% with 2,000 units, 0.8% with 5,000 units;
P = .03).21 This study not only confirms the benefit of
an increased heparin dose, but also suggests further
improvement with ulnar compression in the case of
radial artery occlusion.
In cases of symptomatic occlusion, pain is the most
common symptom, and it is usually self-limited. Patients
with hand ischemia may develop signs of embolism
including intractable pain, pallor, and eventual gangrene.
Management strategies include conservative medical
management with analgesia and/or anticoagulation
Figure 3. Radial artery perforation (red arrow) at the level of or invasive management with intent to restore flow.
the brachial artery. Amputation has been reported secondary to gangrene.22
Although each of these strategies has merit, insufficient
traditional compressive hemostasis, patent hemostasis evidence exists to support a definitive recommendation
uses various compressive devices to provide sufficient for early management.
hemostatic pressure over the arterial puncture site, but
not enough to prevent antegrade flow through the radial PERFORATION AND HEMATOMA
artery into the distal arterial bed. In a randomized study Additional complications of transradial catheterization
of 436 patients undergoing transradial catheterization, include perforation (Figures 1 and 3) and hematoma.
Pancholy and colleagues compared compressive hemo- It is important to remember that the radial artery is
stasis to patent hemostasis and demonstrated a signifi- relatively small compared to the femoral artery, and
cant 59% reduction in early occlusion (12% compressive with variations in anatomy (loops, tortuosity, and acces-
vs 5% patent; P < .05) and a significant 75% reduction in sory branches) occurring in up to 10% of cases, it is not
late occlusion (7% compressive vs 1.8% patent; P < .05).13 uncommon to encounter resistance when advancing
As previously noted, early radial artery occlusion often either the wire or the catheter. When this occurs, care
resolves over time. However, techniques directed toward must be taken to avoid pushing too hard and causing a
treating occlusion and potentially minimizing long-term perforation.
issues are gaining popularity. Anticoagulation with low- Perforation is usually discovered by contrast extrava-
molecular-weight heparin has been shown to reduce the sation and staining beyond the normal architecture of
30-day incidence of symptomatic occlusion. In a study of the vessel. Once perforation has been established, man-
488 patients undergoing transradial catheterization, 51 agement depends upon whether wire access is main-
(10.5%) had evidence of occlusion. Thirty of these patients tained. With wire access, the case can generally continue
had symptoms, and they were treated with 4 weeks of through the radial access site. Some operators recom-
anticoagulation. The 30-day occlusion rate in these patients mend transitioning to a long sheath in order to tam-
was 13.3%, compared to 80.9% of the 21 patients who ponade the perforation and maintain access beyond the
were without symptoms and therefore were not treated perforation site. In the case of lost wire access, the sheath
(P < .001).20 should be removed with patent hemostasis maintained,
60 CARDIAC INTERVENTIONS TODAY MAY/JUNE 2015
COVER STORY
ing occurring proximal or distal to the elbow (open- vs
closed-space bleeding, respectively).23 Hematoma
originating proximally in the open space will manifest
similarly to a retroperitoneal bleed, in which signs of
hypotension, tachycardia, and anemia may indicate a
significant issue. Hematoma originating distally in the
closed space may manifest as tightness and expanding
visible hematoma. The feared complication in such cases
is compartment syndrome, an extremely rare (0.004%)
but potentially catastrophic event.24 For patients with
visible hematoma, arm elevation and compression with
either a bandage wrap or blood pressure cuff may help
contain the hematoma. During compression, patients
should be monitored by continuous pulse oximetry for
digital ischemia.24
Figure 4. Asymptomatic pseudoaneurysm (white arrow) PSEUDOANEURYSM
noted 1 week after catheterization. Pseudoaneurysm (Figure 4) is another rare complica-
tion that occurs from inadequate hemostasis at the radi-
and the patient should be monitored for hematoma al access site. This complication is also associated with
formation. systemic anticoagulation.25 It is recognized as a pulsatile
Anatomically, hematoma can be divided into those mass and diagnosed either visually or by ultrasound or
related to the puncture site or intramuscular bleed- angiography. Treatment options include compression,
COVER STORY
thrombin injection, or surgical ligation, depending on the received research grants and honoraria from Terumo
presence or severity of symptoms. Interventional Systems, Boston Scientific, St. Jude Medical,
Edwards Lifesciences, and Abbott Vascular. Dr. Steinberg
NERVE DAMAGE may be reached at steinbe@musc.edu.
The radial artery is anatomically isolated from the
1. Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3-7.
major nerves that supply the hand, and significant neu- 2. Jolly SS, Amlani S, Hamon M, et al. Radial versus femoral access for coronary angiography or intervention and
rological injury is rare. It is not uncommon for patients the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am
Heart J. 2009;157:132-140.
to report minor numbness of the hand or wrist follow- 3. Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention
ing catheterization, and this often resolves after min- in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet.
2011;377:1409-1420.
utes to hours. On the other end of the spectrum, com- 4. Mehta SR, Jolly SS, Cairns J, et al. Effects of radial versus femoral artery access in patients with acute coronary
plex regional pain has been reported following transra- syndromes with or without ST-segment elevation. J Am Coll Cardiol. 2012;60:2490-2499.
5. Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment
dial catheterization. The syndrome consists of continu- elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-
ous pain, allodynia, and hyperalgesia and may appear in Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481-2489.
6. Feldman DN, Swaminathan RV, Kaltenbach LA, et al. Adoption of radial access and comparison of outcomes to
two forms, type I or type II. The latter is differentiated femoral access in percutaneous coronary intervention: an updated report from the National Cardiovascular Data
by pain in the distribution of a demonstrably damaged Registry (2007-2012). Circulation. 2013;127:2295-2306.
7. Dehmer GJ, Weaver D, Roe MT, et al. A contemporary view of diagnostic cardiac catheterization and percutane-
nerve.26 Both have been reported after transradial cath- ous coronary intervention in the United States: a report from the CathPCI registry of the National Cardiovascular
eterization, and they are exceedingly rare issues with a Data Registry, 2010 through June 2011. J Am Coll Cardiol. 2012;60:2017-2031.
8. Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and
spattering of case reports throughout the literature.27,28 sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc Interv.
Management is typically conservative and can include 1999;46:173-178.
9. Yonetsu T, Kakuta T, Lee T, et al. Assessment of acute injuries and chronic intimal thickening of the radial artery
pain management, steroids, antidepressants, nerve after transradial coronary intervention by optical coherence tomography. Eur Heart J. 2010;31:1608-1615.
10. Kiemeneij F. Prevention and management of radial artery spasm. J Invasive Cardiol. 2006;18:159-160.
blocks, occupational therapy, and counseling. 29 11. Rathore S, Stables RH, Pauriah M, et al. Impact of length and hydrophilic coating of the introducer sheath
on radial artery spasm during transradial coronary intervention: a randomized study. JACC Cardiovasc Interv.
2010;3:475-483.
STERILE GRANULOMA 12. Goldsmit A, Kiemeneij F, Gilchrist IC, et al. Radial artery spasm associated with transradial cardiovascular
Granuloma formation has been reported following procedures: results from the RAS registry. Catheter Cardiovasc Interv. 2014;83:E32-36.
13. Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion-patent hemostasis evalu-
transradial catheterization. It is hypothesized that the ation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after
coating on a specific hydrophilic sheath may lead to transradial catheterization. Catheter Cardiovasc Interv. 2008;72:335-340.
14. Stella PR, Kiemeneij F, Laarman GJ, et al. Incidence and outcome of radial artery occlusion following transradial
the formation of these sterile granulomas, although artery coronary angioplasty. Cathet Cardiovasc Diagn. 1997;40:156-158.
the hemostatic technique has also been implicated.30-32 15. Kim KS, Park HS, Jang WI, Park JH. Thrombotic occlusion of the radial artery as a complication of the transradial
coronary intervention. J Cardiovasc Ultrasound. 2010;18:31.
These granulomas are benign, with no specific manage- 16. Bertrand OF, Rao SV, Pancholy S, et al. Transradial approach for coronary angiography and interventions: results
ment necessary. of the first international transradial practice survey. JACC Cardiovasc Interv. 2010;3:1022-1031.
17. Valgimigli M, Campo G, Penzo C, et al. Transradial coronary catheterization and intervention across the whole
spectrum of Allen test results. J Am Coll Cardiol. 2014;63:1833-1841.
CONCLUSION 18. Spaulding C, Lefevre T, Funck F, et al. Left radial approach for coronary angiography: results of a prospective
study. Cathet Cardiovasc Diagn. 1996;39:365-370.
There is little argument that transradial catheterization 19. Rao SV, Tremmel JA, Gilchrist IC, et al. Best practices for transradial angiography and intervention: a consensus
is associated with lower rates of access site complica- statement from the Society for Cardiovascular Angiography and Intervention’s transradial working group. Catheter
Cardiovasc Interv. 2014;83:228-236.
tions. Although this has led to increased use of transra- 20. Zankl AR, Andrassy M, Volz C, et al. Radial artery thrombosis following transradial coronary angiography:
dial access across the world, it is important to remember incidence and rationale for treatment of symptomatic patients with low-molecular-weight heparins. Clin Res
Cardiol. 2010;99:841-847.
that transradial access is not without complications. 21. Bernat I, Bertrand OF, Rokyta R, et al. Efficacy and safety of transient ulnar artery compression to recanalize
acute radial artery occlusion after transradial catheterization. Am J Cardiol. 2011;107:1698-1701.
Importantly, despite the significant reduction in access 22. de Bucourt M, Teichgraber U. Digital ischemia and consecutive amputation after emergency transradial cardiac
site complications with transradial access in the RIVAL catheter examination. Cardiovasc Intervent Radiol. 2012;35:1242-1244.
23. Bertrand OF. Acute forearm muscle swelling post transradial catheterization and compartment syndrome:
(Radial vs Femoral Access for Coronary Intervention) prevention is better than treatment. Catheter Cardiovasc Interv. 2010;75:366-368.
trial, we must remember that the incidence of death, 24. Tizon-Marcos H, Barbeau GR. Incidence of compartment syndrome of the arm in a large series of transradial
approach for coronary procedures. J Interv Cardiol. 2008;21:380-384.
myocardial infarction, stroke, and major bleeding were 25. Collins N, Wainstein R, Ward M, et al. Pseudoaneurysm after transradial cardiac catheterization: case series and
similar between the transradial and transfemoral access review of the literature. Catheter Cardiovasc Interv. 2012;80:283-287.
26. Marinus J, Moseley GL, Birklein F, et al. Clinical features and pathophysiology of complex regional pain
groups.3 Additionally, as noted in this article, a number syndrome. Lancet Neurol. 2011;10:637-648.
of complications unique to transradial catheterization 27. Papadimos TJ, Hofmann JP. Radial artery thrombosis, palmar arch systolic blood velocities, and chronic regional
pain syndrome 1 following transradial cardiac catheterization. Catheter Cardiovasc Interv. 2002;57:537-540.
exist, and although they are not necessarily clinically sig- 28. Cho EJ, Yang JH, Song YB. Type II complex regional pain syndrome of the hand resulting from repeated arterial
nificant, they do require attention and respect. n punctures during transradial coronary intervention. Catheter Cardiovasc Interv. 2013;82:E465-468.
29. Gierthmuhlen J, Binder A, Baron R. Mechanism-based treatment in complex regional pain syndromes. Nature
reviews. Neurology. 2014;10:518-528.
Daniel H. Steinberg, MD, is with the Division of 30. Kozak M, Adams DR, Ioffreda MD, et al. Sterile inflammation associated with transradial catheterization and
hydrophilic sheaths. Catheter Cardiovasc Interv. 2003;59:207-213.
Cardiology, Medical University of South Carolina in 31. Saririan M, Pyne CT. Sterile granuloma formation following radial artery catheterization: too many Cooks?
Charleston, South Carolina. He has disclosed that he has Catheter Cardiovasc Interv. 2010;76:907-908; author reply 909-910.
32. De Leon D, Swank G, Mirza MA. Radial artery sterile granulomatous reaction secondary to hydrophilic-coated
served as consultant to, advisory board member of, and sheath used for transradial cardiac catheterization: a case series. Angiology. 2012;63:560-562
62 CARDIAC INTERVENTIONS TODAY MAY/JUNE 2015
You might also like
- 701 2022 Article 5445Document9 pages701 2022 Article 5445PeyepeyeNo ratings yet
- Adenosine-Induced Transient Asystole: Gavin W. Britz, M.D., M.P.HDocument4 pagesAdenosine-Induced Transient Asystole: Gavin W. Britz, M.D., M.P.HAnkitaNo ratings yet
- Articulo 2Document3 pagesArticulo 2Henoch SierraNo ratings yet
- Advanced Cardiopulmonary Support For Pulmonary EmbolismDocument6 pagesAdvanced Cardiopulmonary Support For Pulmonary EmbolismJavier Enrique Barrera PachecoNo ratings yet
- Chapter-15-Step-by-step-guide-Trans-carotid-trans-caval-and-direct-aortic-March-2-2018Document9 pagesChapter-15-Step-by-step-guide-Trans-carotid-trans-caval-and-direct-aortic-March-2-2018Jacinto ThèauxNo ratings yet
- Bacaan PPT RebleedingDocument61 pagesBacaan PPT RebleedingseliNo ratings yet
- 2022 Transvenous Embolization Technique For Brain Arteriovenous MalformationsDocument7 pages2022 Transvenous Embolization Technique For Brain Arteriovenous MalformationsstaseaditNo ratings yet
- Glomus CcarotidasDocument8 pagesGlomus CcarotidasJuan TijerinaNo ratings yet
- Endovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and LimitationsDocument10 pagesEndovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and Limitationsafso afsoNo ratings yet
- Embolisation in ENTDocument9 pagesEmbolisation in ENTsudheer joelNo ratings yet
- Multimodal Tretment of Intracranial Aneurysm: A. Chiriac, I. Poeata, J. Baldauf, H.W. SchroederDocument10 pagesMultimodal Tretment of Intracranial Aneurysm: A. Chiriac, I. Poeata, J. Baldauf, H.W. SchroederApryana Damayanti ARNo ratings yet
- Ulnar Acces 2006Document10 pagesUlnar Acces 2006Rodrigo MartinNo ratings yet
- Use of Optitorque & TR Band in PatientsDocument9 pagesUse of Optitorque & TR Band in PatientsankitNo ratings yet
- ResOpinAnesthIntensiveCare83159-6419947 174959Document8 pagesResOpinAnesthIntensiveCare83159-6419947 174959paulosabino1977No ratings yet
- Solid-State Mid-Infrared Laser Facilitated Coronary Angioplasty: Clinical and Quantitative Coronary AngiographicDocument13 pagesSolid-State Mid-Infrared Laser Facilitated Coronary Angioplasty: Clinical and Quantitative Coronary Angiographicfriiday.qNo ratings yet
- Evolving Approaches To The Iliacs, Femorals, Popliteals, and RenalsDocument12 pagesEvolving Approaches To The Iliacs, Femorals, Popliteals, and RenalsSohil ElfarNo ratings yet
- Primary Angioplasty Guiding Catheters SelectionDocument25 pagesPrimary Angioplasty Guiding Catheters SelectionBeatrice KühnNo ratings yet
- Clinical Cardiology - 2008 - ZhouuhDocument4 pagesClinical Cardiology - 2008 - ZhouuhlolopoponakerNo ratings yet
- Catheter Ablation of Intramural Outflow Tract Premature Ventricular Complexes - A Multicentre StudyDocument9 pagesCatheter Ablation of Intramural Outflow Tract Premature Ventricular Complexes - A Multicentre Studyahmed mostafaNo ratings yet
- 59 Minimally Invasive CV Surgery and ECMODocument7 pages59 Minimally Invasive CV Surgery and ECMOVictor PazNo ratings yet
- (10920684 - Neurosurgical Focus) Transvenous Embolization of Brain Arteriovenous Malformations - A Review of Techniques, Indications, and OutcomesDocument7 pages(10920684 - Neurosurgical Focus) Transvenous Embolization of Brain Arteriovenous Malformations - A Review of Techniques, Indications, and Outcomesns52h22pvzNo ratings yet
- Efficacy and Safety o A Dedicated LAAO Protocol 2022Document3 pagesEfficacy and Safety o A Dedicated LAAO Protocol 2022吳醫師No ratings yet
- Percutaneous Aortic Valve Implantation: The Anesthesiologist PerspectiveDocument11 pagesPercutaneous Aortic Valve Implantation: The Anesthesiologist Perspectiveserena7205No ratings yet
- Carotid Artrey DiseaseDocument6 pagesCarotid Artrey DiseaseOnon EssayedNo ratings yet
- Arteriovenous Fistula Care GuideDocument29 pagesArteriovenous Fistula Care GuideMuhammad HaneefNo ratings yet
- Peripherally Inserted Central Venous Acces - 2021 - Seminars in Pediatric SurgerDocument8 pagesPeripherally Inserted Central Venous Acces - 2021 - Seminars in Pediatric Surgeralergo.ramirezNo ratings yet
- Pseudoanuerysms Made EasyDocument15 pagesPseudoanuerysms Made EasyFooffscribdNo ratings yet
- CathSap BDocument153 pagesCathSap BSajjad HussainNo ratings yet
- Rutman Et Al 2022 Incidental Vascular Findings On Brain Magnetic Resonance AngiographyDocument13 pagesRutman Et Al 2022 Incidental Vascular Findings On Brain Magnetic Resonance AngiographySofía ValdésNo ratings yet
- Radial Artery Access For Peripheral Endovascular ProceduresDocument6 pagesRadial Artery Access For Peripheral Endovascular Proceduresvam buddhaNo ratings yet
- Nhjuiy Uyiyui Yuighjjjjjjjjjjjjjjjjjjjjjjjjjjjjhg GHJHGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGJ GHJGHJGHJGHJ L MGLFGKJFDGJKJ FGNGKFDGMNN DFJKDGH DJHGJ MNVGMFDXGNMGNFDMGNMDFGDocument16 pagesNhjuiy Uyiyui Yuighjjjjjjjjjjjjjjjjjjjjjjjjjjjjhg GHJHGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGJ GHJGHJGHJGHJ L MGLFGKJFDGJKJ FGNGKFDGMNN DFJKDGH DJHGJ MNVGMFDXGNMGNFDMGNMDFGHasan AlkhawaldehNo ratings yet
- PAD III TrialDocument8 pagesPAD III TrialMary IvojdaNo ratings yet
- Dialysis Access and Recirculation: Evaluation, Placement, and ComplicationsDocument14 pagesDialysis Access and Recirculation: Evaluation, Placement, and ComplicationsaeleandrosNo ratings yet
- Bauer 2014Document8 pagesBauer 2014zixzaxoffNo ratings yet
- Distal Radial and Ulnar Arteries: The Alternative Forearm AccessDocument12 pagesDistal Radial and Ulnar Arteries: The Alternative Forearm AccessAlejandro Vazquez ManniseNo ratings yet
- The Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionDocument10 pagesThe Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionRobert ChristevenNo ratings yet
- Pinch Off Syndrome - A Rare Complication of Chemo Port: Dr. C. Ramachandra, Dr. Pavan Kumar J, Dr. C. SrinivasDocument4 pagesPinch Off Syndrome - A Rare Complication of Chemo Port: Dr. C. Ramachandra, Dr. Pavan Kumar J, Dr. C. SrinivasPavan JonnadaNo ratings yet
- Off-Pump Versus On-Pump Coronary Artery Bypass Grafting in Consecutive Patients: Decision-Making Algorithm and OutcomesDocument7 pagesOff-Pump Versus On-Pump Coronary Artery Bypass Grafting in Consecutive Patients: Decision-Making Algorithm and Outcomesfluid_man_brazilNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- Arterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmDocument8 pagesArterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmJuan Jose Velasquez GutierrezNo ratings yet
- Et0420 MedAffairs MouawadDocument5 pagesEt0420 MedAffairs MouawadAna Silvia LebrOnNo ratings yet
- Angio Acces OsDocument16 pagesAngio Acces OsKarely TapiaNo ratings yet
- (10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionDocument7 pages(10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionCharles MorrisonNo ratings yet
- (10920684 - Neurosurgical Focus) Arteriovenous Malformation Presenting With Epilepsy - A Multimodal Approach To Diagnosis and TreatmentDocument7 pages(10920684 - Neurosurgical Focus) Arteriovenous Malformation Presenting With Epilepsy - A Multimodal Approach To Diagnosis and TreatmentNurul FajriNo ratings yet
- Placement of Arterial Line: Renae Stafford, MDDocument7 pagesPlacement of Arterial Line: Renae Stafford, MDBotond LukacsNo ratings yet
- PCI or PTCADocument30 pagesPCI or PTCAMelissa KanggrianiNo ratings yet
- Lower Extremity Artery Aneurysms and Their Management-An Institutional ExperienceDocument8 pagesLower Extremity Artery Aneurysms and Their Management-An Institutional ExperienceIJAR JOURNALNo ratings yet
- Transcatheter Coil Embolotherapy: A Safe and Evective Option For Major Colonic HaemorrhageDocument7 pagesTranscatheter Coil Embolotherapy: A Safe and Evective Option For Major Colonic Haemorrhagemuhammad gagas sasongkoNo ratings yet
- 394 Endovascular Hunterian LigationDocument6 pages394 Endovascular Hunterian Ligationlonsilord17No ratings yet
- Very Distal Transradial Approach (VITRO) For Coronary InterventionsDocument4 pagesVery Distal Transradial Approach (VITRO) For Coronary InterventionsDeebanshu GuptaNo ratings yet
- JUMDC 6 Arterio VenousDocument6 pagesJUMDC 6 Arterio VenousMudassar SaeedNo ratings yet
- Evaluation and Management of Acute Vascular Trauma: Gloria M.M. Salazar, MD, and T. Gregory Walker, MDDocument15 pagesEvaluation and Management of Acute Vascular Trauma: Gloria M.M. Salazar, MD, and T. Gregory Walker, MDfranciscoreynaNo ratings yet
- Acute Limb Ischemic: Divisi Bedah Vaskular Melfrits R Siwabessy, MDDocument26 pagesAcute Limb Ischemic: Divisi Bedah Vaskular Melfrits R Siwabessy, MDMelfrits SiwabessyNo ratings yet
- Conduits For Coronary Bypass: Vein Grafts: Hendrick B Barner, M.D., Emily A Farkas, M.DDocument12 pagesConduits For Coronary Bypass: Vein Grafts: Hendrick B Barner, M.D., Emily A Farkas, M.DGaetano Di GiovanniNo ratings yet
- 1 s2.0 S1078588406004801 Main PDFDocument8 pages1 s2.0 S1078588406004801 Main PDFkadek sanggingNo ratings yet
- Preventing Acute Radial Artery Occlusion A Batt - 2018 - JACC Cardiovascular IDocument3 pagesPreventing Acute Radial Artery Occlusion A Batt - 2018 - JACC Cardiovascular INouman HameedNo ratings yet
- Cardiac CatheterizationDocument9 pagesCardiac CatheterizationAnurag Gupta100% (1)
- HemodialysisDocument11 pagesHemodialysisjuan_sioNo ratings yet
- Long Saphenous Vein Harvesting Techniques and Their Effect On Graft PatencyDocument8 pagesLong Saphenous Vein Harvesting Techniques and Their Effect On Graft PatencyElías MendezNo ratings yet
- Endovascular InterventionsFrom EverandEndovascular InterventionsJose M. WileyNo ratings yet
- 101161@circinterventions119008487 230823 233136Document13 pages101161@circinterventions119008487 230823 233136Nasru llahNo ratings yet
- 101161@circinterventions119008487 230823 233136Document13 pages101161@circinterventions119008487 230823 233136Nasru llahNo ratings yet
- MASS Storage Solutions EMAILDocument8 pagesMASS Storage Solutions EMAILNasru llahNo ratings yet
- ELS 31 Agustus 2023Document20 pagesELS 31 Agustus 2023Nasru llahNo ratings yet
- BROSUR MEDINA Emergency Trolley MX300Document1 pageBROSUR MEDINA Emergency Trolley MX300Nasru llahNo ratings yet
- Rotablator System Reference Guide - IC 193906 AADocument22 pagesRotablator System Reference Guide - IC 193906 AANasru llahNo ratings yet
- HARRY Surgical Instruments - Pinset Forceps (146-152)Document1 pageHARRY Surgical Instruments - Pinset Forceps (146-152)Nasru llahNo ratings yet
- Intrasight Mobile Three DatasheetDocument2 pagesIntrasight Mobile Three DatasheetNasru llahNo ratings yet
- Rotablator Brochure (PI-208403-AD)Document3 pagesRotablator Brochure (PI-208403-AD)Nasru llahNo ratings yet
- WhatsApp Image 2023-05-25 at 14.27.19 (1) (2) - CompressedDocument3 pagesWhatsApp Image 2023-05-25 at 14.27.19 (1) (2) - CompressedNasru llahNo ratings yet
- Medscimonit 25 240Document8 pagesMedscimonit 25 240Nasru llahNo ratings yet
- Dedic AdmirDocument216 pagesDedic AdmirNasru llahNo ratings yet
- Mehran1999 220903 094007Document9 pagesMehran1999 220903 094007Nasru llahNo ratings yet
- Aplication and Removal Guidelines - TR BandDocument2 pagesAplication and Removal Guidelines - TR BandNasru llahNo ratings yet
- PENYULUHAN KELUARGA BERENCANA CompressedDocument3 pagesPENYULUHAN KELUARGA BERENCANA CompressedNasru llahNo ratings yet
- Medscimonit 25 240Document8 pagesMedscimonit 25 240Nasru llahNo ratings yet
- Re Stenosis After Pci Jukema2011 - 220902 - 123201Document11 pagesRe Stenosis After Pci Jukema2011 - 220902 - 123201Nasru llahNo ratings yet
- 18Document1 page18Nasru llahNo ratings yet
- Mehran1999 220903 094007Document9 pagesMehran1999 220903 094007Nasru llahNo ratings yet
- Jurnal B.ing Terap BermainDocument8 pagesJurnal B.ing Terap BermainNasru llahNo ratings yet
- 1814 d01 PDFDocument20 pages1814 d01 PDFteletrabbiesNo ratings yet
- 3.0MP 4G Smart All Time Color Bullet Cam 8075Document2 pages3.0MP 4G Smart All Time Color Bullet Cam 8075IshakhaNo ratings yet
- Xray Order FormDocument1 pageXray Order FormSN Malenadu CreationNo ratings yet
- EngM6 TB WebDocument161 pagesEngM6 TB WebNong BillNo ratings yet
- Concentration Seed Company OwnershipDocument2 pagesConcentration Seed Company OwnershipC'estMoiNo ratings yet
- Al-Qawlul Mufeed: Backbiting and Its Impact On SocietyDocument2 pagesAl-Qawlul Mufeed: Backbiting and Its Impact On SocietyMountainofknowledgeNo ratings yet
- New Life in Christ by Wilson HerreraDocument18 pagesNew Life in Christ by Wilson Herreralesantiago100% (1)
- Units 3 - 4 Workshop A2Document3 pagesUnits 3 - 4 Workshop A2S4N7Y PRONo ratings yet
- Learning and Teaching in The Clinical EnvironmentDocument4 pagesLearning and Teaching in The Clinical EnvironmentDaniel Alejandro Lozano MorenoNo ratings yet
- KF2.5-200 - With-M-C - GB - 03-15 KRACHT Bomba PDFDocument8 pagesKF2.5-200 - With-M-C - GB - 03-15 KRACHT Bomba PDFJairo Andrés FA100% (1)
- Cambodia's Rich Literary HeritageDocument5 pagesCambodia's Rich Literary HeritageChelle LancetaNo ratings yet
- General Dynamics F-16 Fighting Falcon - Wikipedia, The Free EncyclopediaDocument28 pagesGeneral Dynamics F-16 Fighting Falcon - Wikipedia, The Free EncyclopediaJulie MerrillNo ratings yet
- The Man Who Married A Hen, Stories of A Zambian SchoolboyDocument78 pagesThe Man Who Married A Hen, Stories of A Zambian SchoolboyGerard StoutNo ratings yet
- Cost ReductionDocument8 pagesCost Reductionmlganesh666100% (3)
- Shyness and Social AnxietyDocument22 pagesShyness and Social Anxietybeleanadrian-1No ratings yet
- Oracle VMDocument243 pagesOracle VMАскандар Каландаров100% (1)
- Appointment Slip: 2 X 2 ID PictureDocument1 pageAppointment Slip: 2 X 2 ID PictureDarwin Competente LagranNo ratings yet
- Early Daoist Dietary Practices: Examining Ways To Health and Longevity. by Shawn ArthurDocument6 pagesEarly Daoist Dietary Practices: Examining Ways To Health and Longevity. by Shawn ArthurlsdkNo ratings yet
- 9 - The Relationship Between CEO Characteristics and Leverage - The Role of Independent CommissionersDocument10 pages9 - The Relationship Between CEO Characteristics and Leverage - The Role of Independent Commissionerscristina.llaneza02100% (1)
- Final MTech ProjectDocument30 pagesFinal MTech ProjectArunSharmaNo ratings yet
- Yu Gi Oh Card DetailDocument112 pagesYu Gi Oh Card DetailLandel SmithNo ratings yet
- Nursing Health History SummaryDocument1 pageNursing Health History SummaryHarvey T. Dato-onNo ratings yet
- Reflection Paper IIDocument1 pageReflection Paper IIHazel Marie Echavez100% (1)
- Hydrolics Final Year ProjectDocument23 pagesHydrolics Final Year ProjectHarsha VardhanaNo ratings yet
- XETEC 4g300 / 4g600Document6 pagesXETEC 4g300 / 4g600Harun ARIKNo ratings yet
- Accounting for Inventory Valuation Methods Research ProposalDocument66 pagesAccounting for Inventory Valuation Methods Research ProposalAyman Ahmed Cheema100% (1)
- QuickZChargerZAC DCDocument2 pagesQuickZChargerZAC DCLucaspasNo ratings yet
- TB170LSDocument4 pagesTB170LSDary ArroyoNo ratings yet
- Band Theory of Soids5!1!13Document20 pagesBand Theory of Soids5!1!13Ravi Kumar BanalaNo ratings yet
- Victory Over Sin Through Total ConsecrationDocument3 pagesVictory Over Sin Through Total ConsecrationJhon Ray OtañesNo ratings yet