Professional Documents
Culture Documents
Neurodevelopmental Disorders
Uploaded by
Eunice Cuñada0 ratings0% found this document useful (0 votes)
50 views8 pagesOriginal Title
NEURODEVELOPMENTAL-DISORDERS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
50 views8 pagesNeurodevelopmental Disorders
Uploaded by
Eunice CuñadaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
Autism does have a genetic link; many children with
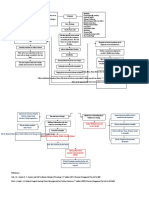
NEURODEVELOPMENTAL DISORDERS autism have a relative with autism or autistic traits.
Controversy continues about whether measles,
INTRODUCTION mumps, and rubella (MMR) vaccinations contribute
Psychiatric disorders are not diagnosed as easily in to the development of late- or regressive-onset
children as they are in adults. Children usually lack autism.
the abstract cognitive abilities and verbal skills to
describe what is happening. Because they are Autism tends to improve, in some cases substantially,
constantly changing and developing, children have as children start to acquire and use language to
limited sense of a stable, normal self to allow them to communicate with others. If behavior deteriorates in
discriminate unusual or unwanted symptoms from adolescence, it may reflect the effects of hormonal
normal feelings and sensations. changes or the difficulty meeting increasingly
Intellectual disability is the correct diagnostic term complex social demands. Autistic traits persist into
for what was once called mental retardation, a term adulthood, and most people with autism remain
often used in a disparaging manner to bully or dependent to some degree on others.
ridicule individuals with impaired cognitive abilities.
The essential feature of intellectual disability is Until the mid-1970s, children with autism were
below-average intellectual functioning (intelligence usually treated in segregated, specialty outpatient, or
quotient [1Q]<70) accompanied by significant school programs. Those with more severe behaviors
limitations in areas of adaptive functioning Such as were referred to residential programs. Since then,
communication skills, self-care, home living, social most residential programs have been closed; children
or interpersonal skills, use of community resources, with autism are being "mainstreamed" into local
self-direction, academic skills, work, leisure, and school programs whenever possible.
health and safety.
Mood and behavior disturbances vary among people Pharmacologic treatment with antipsychotics, such as
with intellectual disabilities. Some people with haloperidol (Haldol), risperidone (Risperdal),
intellectual disability are passive and dependent; aripiprazole (Abilify), or combinations of
others are aggressive and impulsive; and still others antipsychotic medications, may be effective for
may have minimal mood and behavior disturbances. specific target symptoms such as temper tantrums,
aggressive- ness, self-injury, hyperactivity, and
AUTISM SPECTRUM DISORDER stereotyped behaviors. Other medications, such as
Autism spectrum disorder (ASD) is the DSM-5 naltrexone (Re Via), clomipramine (Anafranil),
(Diagnostic and Statistical Manual of Mental clonidine (Catapres), and stimulants to diminish self-
Disorders, fifth edition) diagnosis that includes injury and hyperactive and obsessive behaviors, have
disorders previously categorized as different types of had varied but unremarkable results. there are no
a pervasive developmental disorder (PDD), medications approved for the treatment of ASD itself.
characterized by pervasive and usually severe
impairment of reciprocal social interaction skills, Behaviors Common with ASD
communication deviance, and restricted stereotypical Not responding to own name by 1 year (e.g., appears
behavioral patterns. not to hear)
Doesn't show interest by pointing to objects or people
ASD, formerly called autistic disorder, or just autism, by 14 months of age
is almost five times more prevalent in boys than in Doesn't play pretend games by 18 months of age
girls, and it is usually identified by 18 months and no Avoids eye contact
later than 3 years of age. The behaviors and Prefers to be alone
difficulties experienced vary along the continuum Delayed speech and language skills Obsessive
from mild to severe. Children with ASD have interests (e.g., gets stuck on an idea)
persistent deficits in communication and social Upset by minor changes in routine
interaction accompanied by restricted, stereotyped Repeats words or phrases over and over
patterns of behavior and interests/activities. Flaps hands, or rocks or spins in a circle; answers are
unrelated to questions
Eighty percent of cases of autism are early onset, Unusual reactions to sounds, smells, or other sensory
with developmental delays starting in infancy. The experiences
other 20% of children with autism have seemingly
normal growth and development until 2 or 3 years of Related Disorders
age, when developmental regression or loss of
abilities begins. They stop talking and relating to Tic Disorders
parents and begin to demonstrate behaviors A tic is a sudden, rapid, recurrent, nonrhythmic,
previously described. stereoyped motor movement or vocalization. Tics
can be suppressed but not indefinitely. Stress
exacerbates tics, which diminish during sleep and
when the person is engaged in an absorbing activity. rocking, head banging, and biting, that appears to
Common simple motor tics include blinking, jerking have no purpose.
the neck, shrugging the shoulders, grimacing, and
coughing. Common simple vocal tics include COMMUNICATION DISORDER
clearing the throat, grunting, sniffing, snorting, and Communication disorder
barking. Involves deficits in language, speech, and
communication and is diagnosed when deficits are
Tic disorders are usually treated with risperidone sufficient to hinder development, academic
(Risperdal) or olanzapine (Zyprexa), which are achievement, or activities of daily living, including
atypical antipsychotics. It is important for clients socialization.
with tic disorders to get plenty of rest and to manage
stress because fatigue and stress increase symptoms Language disorder
- Involves deficit(s) in language production or
Tourette disorder comprehension, causing limited vocabulary and an
Tourette disorder involves multiple motor tics and inability to form sentences or have a conversation.
one or more vocal tics, which occur many times a day
for more than 1 year. The complexity and severity of Speech sound disorder
the tics change over time, and the person experiences - It is difficulty or inability to produce intelligible
almost all the possible tics described previously speech, which precludes effective verbal
during his or her lifetime. communication.
- Stuttering is a disturbance of fluency and patterning
Chronic Motor or Tic Disorder of speech with sound and syllable repetitions.
Chronic motor or vocal tic differs from Tourette
disorder in that either the motor or the vocal tic is Social communication disorder
seen, but not both. Transient tic disorder may involve - Involves the inability to observe social "rules" of
single or multiple vocal or motor tics, but the conversation, deficits in applying context to
occurrences last no longer than 12 months. conversation, inability to tell a story in an
understandable manner, and inability to take turns
talking and listening with another.
Learning Disorders
A specific learning disorder is diagnosed when a
child's achievement in reading, mathematics, or ELIMINATION DISORDERS
written expression is below that expected for age, Encopresis
formal education, and intelligence. Learning - It is the repeated passage of feces into inappropriate
problems interfere with academic achievement and places such as clothing or the floor by a child who is
lite activities requiring reading, math, or writing. at least 4 years of age either chronologically or
develop mentally.
Low self-esteem and poor social skills are common 1. Involuntary encopresis
in children with learning disorders. As adults, some - Usually associated with constipation that
have problems with employment or social occurs for psychological, not medical,
adjustment; others have minimal difficulties. Early reasons.
identification of the learning disorder, effective 2. Intentional encopresis
intervention, and no coexisting problems is - is often associated with oppositional defiant
associated with better outcomes. disorder (ODD) or conduct disorder.
Motor Skills Disorder Enuresis
The essential feature of developmental coordination - It is the repeated voiding of urine during the day or at
disorder is impaired coordination severe enough to night into clothing or bed by a child at least 5 years
interfere with academic achievement or activities of of age either chronologically or developmentally.
daily living. This diagnosis is not made if the
problem with motor coordination is part of a general - Imipramine (Tofranil), an antidepressant with a side
medical condition, such as cerebral palsy or effect of urinary retention. Both elimination disorders
muscular dystrophy. respond to behavioral approaches.
Both encopresis and enuresis are more common in boys
than in girls; 1% of all 5-year-olds have encopresis and
5% of all 5-year-olds have enuresis. Encopresis can
persist with intermittent exacerbations for years, it is
Stereotypic movement disorder rarely chronic. Only 1% of all cases persist into
Stereotypic movement disorder is characterized by adulthood.
rhythmic, repetitive behaviors, such as hand waving,
Impairment associated with elimination disorders depends
on the limitations on the child's social activities, effects on
self-esteem, degree of social ostracism by peers, and cooperatively or take turns and constantly interrupts
anger, punishment, and rejection on the part of parents or others.
caregivers. Studies have shown that both teachers and peers
perceive children with ADHD as more aggressive,
Sluggish cognitive tempo (SCT) bossier, and less likable. This perception results from
- A syndrome that is not a DSM-5 diagnosis. It the child's impulsivity, inability to share or take turns,
includes daydreaming, trouble focusing and paying tendency to interrupt, and failure to listen to and
attention, mental fogginess, staring, sleepiness, little follow directions.
interest in physical activity, and slowness in finishing Thus, peers and teachers may exclude the child from
tasks. activities and play, may refuse to socialize with the
child, and/or may respond to the child in a harsh,
ATTENTION-DEFICIT/HYPERACTIVITY DISORDER punitive, or rejecting manner.
(ADHD) Previously, it was believed that children outgrew
ADHD, but it is now known that ADHD can persist
Characterized by inattentiveness, overactivity, and into adulthood. Estimates are that 60% of children
impulsiveness. with ADHD have symptoms that continue into
adulthood. In one study, adults who had been treated
ADHD is a common disorder, especially in boys, and for hyperactivity 25 years earlier were three to four
probably accounts for more child mental health times more likely than their brothers to experience
referrals than any other single disorder. nervousness, restlessness, depression, lack of friends,
and low frustration tolerance.
The essential feature of ADHD is a persistent pattern Approximately 70% to 75% of adults with ADHD
of inattention and/or hyperactivity and impulsivity have at least one coexisting psychiatric diagnosis,
more common than generally observed in children of with social phobia, bipolar disorder, major
the same age. depression, and alcohol dependence being the most
common
To avoid overdiagnosis of ADHD, a qualified
specialist, such as a pediatric neurologist or a child ETIOLOGY
psychiatrist, must conduct the evaluation for ADHD.
It is essential to have a thorough and accurate Although much research has taken place, the definitive causes
diagnosis for ADHD. There are other disorders and of ADHD remain unknown.
situations that may look similar to ADHD, such as There may be cortical-arousal, information-
bipolar disorder or behavioral acting out in response processing, or maturational abnormalities in the
to family stress. brain.
Combined factors
Onset and Clinical Course Prenatal exposure
ADHD is usually identified and diagnosed when the Brain images of people with ADHD suggest decreased
child begins preschool or school, though many metabolism in the frontal lobes.
parents report problems from a much younger age. Studies have also shown decreased blood perfusion of the
As infants, children with ADHD are often fussy and frontal cortex in children with ADHD and frontal cortical
temperamental and have poor sleeping patterns. atrophy in young adults with a history of childhood ADHD.
Toddlers may be described as "always on the go" Another study showed decreased glucose use in the frontal
and "into everything," at times dismantling toys and lobes of parents of children with ADHD who had ADHD
cribs. They dart back and forth, jump and climb on themselves.
furniture, run through the house, and cannot tolerate
sedentary activities such as listening to stories. There seems to be a genetic link for ADHD that is most likely
associated with abnormalities in catecholamine and serotonin
By the time the child starts school, symptoms of ADHD begin metabolism.
to interfere significantly with behavior and performance:
The child fidgets constantly Risk factors for ADHD:
In and out of assigned seats family history of ADHD
Makes excessive noise by tapping or playing with female relatives with somatization disorder
pencils or other object lower socioeconomic status
Normal environmental noises male gender
He or she cannot listen to directions or complete marital or family discord, including divorce,
tasks. neglect, abuse, or parental deprivation
The child interrupts and blurts out answers before low birth weight
questions are completed. various kinds of brain insult
Socially, peers may ostracize or even ridicule the
child for his or her behavior. Forming positive peer TREATMENT
relationships is difficult because the child cannot play
No one treatment has been found to be effective for
ADHD, this gives rise to many different approaches
such is sugar-controlled diets and megavitamin
therapy. NURSING INTERVENTION FOR ADHD
ADHD is chronic. Goals of treatment involve Ensuring the child's safety and that of others
managing symptoms, reducing hyperactivity and o Stop unsafe behavior
impulsivity, and increasing the child's attention. o Provide close supervision.
o Give clear directions about acceptable and
Psychopharmacology unacceptable behavior.
Improved role performance
o Give positive feedback for meeting
STIMULANTS: expectations.
Methylphenidate - It is a stimulant that reduces o Manage the environment
hyperactivity, impulsivity, and mood lability and
helps the child pay attention more appropriately. Simplifying instructions/directions
Amphetamine compound (Adderall) - increasing - Get child's full attention
mental alertness and improving the ability to focus. - Break complex tasks into small steps.
Dextroamphetamine (Dexedrine) and pemoline - Allow breaks.
(Cylert) - are other stimulants used to treat Structured daily routine
ADHD. - Establish a daily schedule. •
The most common side effects: - Minimize changes.
- Insomnia, loss of appetite, and weight loss or failure Client/family education and support: Listen to parent's
to gain weight. feelings and frustrations.
Psychopharmacology MENTAL HEALTH PROMOTION
The SNAP-IV Teacher and Parent Rating Scale is an
When stimulant medications are not effective or their side assessment tool that can be used for initial evaluation in
effects are intolerable, antidepressants are the second choice many areas of concern such as ADHD, ODD, conduct
for treatment disorders, and depression.
Atomoxetine (Strattera) - The only nonstimulant drug
specifically developed and tested by the U.S. Food and Drug
Early identification and treatment of ASD are needed to
Administration for the treatment of ADHD. It is an
help children with these disorders reach their maximum
antidepressant, specifically a selective norepinephrine
potential. Insufficient knowledge about ASD and
reuptake inhibitor.
embarrassment or reluctance to have a child diagnosed
with ASD are reasons that some parents are hesitant to
The most common side effects:
have children evaluated if signs of developmental delays
In children:
are present.
- Decreased appetite, nausea, vomiting, tiredness, and
There is a high comorbidity between ADHD and other
upset stomach.
disorders including substance use/abuse, antisocial
In adults:
behavior, anxiety disorders, and mood disorders.
- Insomnia, dry mouth, urinary retention, decreased
appetite, nausea. Vomiting, dizziness, and sexual side
effects. To promote health through adulthood, individuals with
ADHD could benefit from strategies to prevent other
psychiatric disorders as well as early identification and
treatment of coexisting disorders.
Psychopharmacology
Disruptive Behavior Disorders
Strategies for Home and School: INTRODUCTION
Behavioral strategies are necessary to help the child Disruptive behavior disorders include problems with
master appropriate behaviors. the person's ability to regulate his or her own emotions or
Environmental strategies at school and home can behaviors. They are characterized by persistent patterns of
help the child succeed in those settings. behavior that involve anger, hostility, and/or aggression
o In therapeutic play: toward people and property.
Oppositional defiant disorder (ODD), conduct
Play techniques are used to understand the child's
disorder, and intermittent explosive disorder (IED). It has
thoughts and feelings and to promote communication.
been posited by some psychiatrists that ODD and conduct
Dramatic play is acting out an anxiety-producing
disorder can be viewed on a continuum concept that would
situation.
include antisocial personality disorder. Others believe that
Creative play techniques can help children to ODD is a milder variant of conduct disorder.
express themselves Related Disorders
exhibit impaired problem-solving abilities and deficiencies in
Kleptomania attention, flexibility of thinking, and decision-making. All of
Characterized by impulsive, repetitive theft of these problems are also present in children diagnosed with
items not needed by the person, either for personal conduct disorder-to an even greater degree.
use or monetary gain.
Tension and anxiety are high prior to the theft, and Prognosis for ODD varies by age of onset, symptom
the person feels relief, exhilaration, or gratification severity, and the presence of comorbid psychiatric disorders.
while committing the theft. The item is often Early onset, more severe symptoms, and comorbid conditions
discarded after it is stolen. are associated with poorer long-term outcomes.
More common in females and often has negative Children with this disorder can develop conduct
legal, career, family, and social consequences. disorder; some will be diagnosed with antisocial personality
disorder as adults. ODD is often comorbid with other
Related Disorders psychiatric disorders such as attention-deficit/hyperactivity
disorder (ADHD), anxiety, and/or mood disorders that need to
Pyromania be treated as well.
Characterized by repeated, intentional fire-setting. Treatment for ODD is based on parent management
The person is fascinated about fire and feels pleasure training models of behavioral interventions.
or relief of tension while setting and watching the fires. A hierarchy of problem behaviors is developed, and
the most disruptive or problematic behaviors are targeted for
There is neither any monetary gain or revenge or
intervention. Parents learn to ignore maladaptive behaviors
other reason, such as concealing other crimes, nor is it rather than giving the behaviors negative attention, positive
associated with another major mental disorder. behaviors are rewarded with praise and reinforcers and
Pyromania as a primary disorder is rare. Persons, if consistent consequences for the child's defiant behavior are
caught, become part of the legal rather than mental health implemented every time the behavior occurs.
system.
Adolescent children benefit from interventions that
OPPOSITIONAL DEFIANT DISORDER use enhancement of personal strengths to improve behavioral
and social functioning. Older children may also benefit from
❏ Consists of an enduring pattern of uncooperative, individual therapy in addition to the behavioral program. In
defiant, disobedient, and hostile behavior toward addition, focus on supporting the parents improves overall
authority figures without major antisocial violations. outcomes. Primary caregivers report that challenges can be
overwhelming, demanding, and unrelenting. The two major
❏ A certain level of oppositional behavior is common challenges for parents and caregivers are managing the
in children and adolescents, indeed, it is almost adolescent's aggressive, defiant, and deceitful behaviors, and
expected at some phases such as 2 to 3 years of age interacting frequently with multiple service providers and
and in early adolescence. agencies.
INTERMITTENT EXPLOSIVE DISORDER
Acceptable Characteristics & Abnormal Behavior in Involves repeated episodes of impulsive,
Adolescence aggressive, violent behavior, and angry verbal
The disruptive, defiant behaviors usually begin at home with outbursts usually lasting less than 30 minutes.
parents or parental figures and are more intense in this setting there may be physical injury to others, destruction
than settings outside the home. of property, and injury to the individual as well.
The intensity of the emotional outburst is grossly
The prevalence rates of ODD vary from 2% up to out of proportion to the stressor or situation.
15% of the adolescent population, which highlights the The episode may occur with seemingly no warning.
difficulty of distinguishing negative behavior from ODD and Afterward, the individual may be embarrassed and
conduct disorder-type behaviors. Average prevalence in the feel guilty or remorseful for his or her actions. But
United States is estimated at 3%. It occurs more often in that does not prevent future impulsive, aggressive
males; however, ODD in female adolescents has increased in outbursts.
recent years. Most authorities believe that genes, The onset of IED can occur at any time in life but
temperament, and adverse social conditions interact to create is most common in adolescence and young
ODD. Children with ODD have lower self-concept and lack adulthood.
competence in social situations. It is more common in males than in females.
most commonly substance use/abuse, ADHD,
Children with ODD have limited abilities to make ODD, conduct disorder, anxiety disorders, and
associations between their behavior and consequences of depression.
behavior-both negative and positive, indicative of a reduced IED is related to childhood exposure to trauma,
sensitivity to reward and punishment. neglect, or maltreatment.
Therefore, learning appropriate behavior and learning
to refrain from inappropriate behavior are impaired. They also
neurotransmitter imbalances, especially serotonin: Mild: The child has some conduct problems that
plasma tryptophan depletion; and frontal lobe cause relatively minor harm to others.
dysfunction. Examples include repeated lying, truancy,
coronary heart disease, hypertension, stroke, minor shoplifting, and staying out late without
diabetes, arthritis, back/neck pain, ulcer, headache, permission.
and other chronic pain. Moderate: The number of conduct problems
Treatment for IED includes medications increases as does the amount of harm to others.
fluoxetine (Prozac); lithium; and anticonvulsant mood Examples in clude vandalism, conning
stabilizers such as valproic acid (Depakote), phenytoin others, running away from home. verhal bullying and
(Dilantin),topiramate (Topamax), and oxcarbazepine intimidation, drinking alco hol, and sexual
(Trileptal). promiscuity
Severe: The person has many conduct problems that
Selective serotonin reuptake inhibitor antidepressants cause considerable harm to others.
particularly seem to reduce aggressive tendencies. Examples include forced sex cruelty to
Cognitive behavioral therapy, anger management strategies, animals, physical fights, cruelty to peers, use of a
avoidance of alcohol and other substances, and relaxation weapon, burglary, robbery, and violation of previous
techniques. parole or probation requirements.
CONDUCT DISORDER
Characterized by persistent behavior that violates ETIOLOGY
societal norms, rules, laws, and the rights of others. Researchers generally accept that genetic vulnerability,
Impaired abilities to function in social, academic, environmental adversity, and factors such as poor coping
or occupational areas. interact to cause the disorder.
Symptoms are clustered in four areas: aggression to
people and animals, destruction of property, Risk factors:
deceitfulness and theft, and serious violation of poor parenting
rules. low academic achievement
Children with conduct disorder often exhibit poor peer relationships
callous and unemotional traits, similar to those low self-esteem
seen in adults with antisocial personality disorder. There is a genetic risk for conduct disorder, though no specific
They have little empathy for others, do not feel gene marker has been identified. The disorder is more
"had" or guilty or show remorse for their behavior, common in children who have a sibling with conduct disorder
have shallow or superficial emotions, and are or a parent with antisocial personality disorder, substance
unconcerned about poor performance at school or abuse, mood disorder, schizophrenia, or ADHD.
home.
These children have low self-esteem poor A lack of reactivity of the autonomic nervous system
frustration tolerance, and temper outbursts. has been found in children with conduct disorder, this
Conduct disorder is frequently associated with unresponsiveness is similar to adults with antisocial
early onset of sexual behavior, drinking smoking personality disorder. The abnormality may cause more
use of illegal substances, and other reckless or risky aggression in social relationships as a result of decreased
behaviors. In the United States, of children and normal avoidance or social inhibitions.
adolescents have conduct disorder. Onset of Poor family functioning
conduct disorder behaviors before age 10 occurs marital discord
primarily in boys, onset alter age 10 occurs in girls poor parenting
and boys. As many as 30% to 50% of these a family history of substance abuse and psychiatric
children are diagnosed with antisocial personality problems
disorder as adults.
Studies have shown that adolescents with conduct disorder
ONSET and CLINICAL COURSE had their first experience with alcohol and other drugs before
age 12 years and were more likely to engage in higher risk
Two subtypes of conduct disorder are based on age at onset. behaviors, including, but not limited to, continued alcohol and
Childhood-onset type- involves symptoms before 10 substance use. Prenatal exposure to alcohol causes an
years of age, including physical aggression toward increased risk for conduct disorder. Child abuse is an
others and disturbed peer relationships. especially significant risk factor.
The specific parenting patterns considered ineffective
Adolescent-onset type- is defined by no behaviors of are inconsistent parental responses to the child's
conduct disorder until after 10 years of age. demands and giving into demands as the child's
behavior escalates.
Behaviors associated with conduct disorders fall into Exposure to violence in the media and community is
categories of aggression, destruction, deceiv/theft, and rule a contributing factor for the child at risk in other
violation, but they can vary in intensity. areas. Socioeconomic disadvantages, such as
inadequate housing, crowded conditions, and
poverty, also increase the likelihood of conduct Preschool programs, such as Head Start, result in lower rates
disorder in at-risk children. of delinquent behavior and conduct disorder through use of
parental education about normal growth and development,
Academic underachievement, learning disabilities, stimulation for the child, and parental support during crises.
hyperactivity, and problems with attention span are
all associated with conduct disorder. For school-aged children with conduct disorder, the child,
Children with conduct disorder have difficulty family and school environment are the focus of treatment.
functioning in social situations parenting education
Lack the abilities to respond appropriately to others social skills training to improve peer relationships
& to negotiate conflict, lose ability to restrain Attempts to improve academic performance and
themselves when emotionally stressed. increase the child's ability to comply with demands
They are often accepted only by peers with similar from authority figures.
problems. Family therapy is considered to be essential for children in
this age group.
Related Problems
Externalizing and Internalizing Behaviors Adolescents rely less on their parents and more on peers, so
❖ Externalizing Behaviors treatment for this age group includes individual therapy.
The most promising treatment approach includes keeping the
Lying client in his or her environment with family and individual
Cheating at school therapies.
Swearing conflict resolution
Truancy anger management
Vandalism teaching social skills.
Setting fires
Medications alone have little effect, but may be used in
Bragging
conjunction with treatment for specific symptoms.
Screaming
For example, the client who presents a clear danger to others
Inappropriate attention-seeking (physical aggression)
Arguing Risperidone (Risperdal)
Threatening
Demanding Nursing Interventions: Conduct Disorder
Relentless teasing
Anger outbursts Encourage the client to discuss his or her thoughts
and feelings.
❖ Internalizing Behaviors Give positive feedback for appropriate discussions.
Prefers to be alone o Tell the client he or she is accepted as a
Withdraws person, though a particular behavior may
Sulks not be acceptable.
Won't talk Give the client positive attention when behavior is
Is secretive not problematic.
Overly shy Teach the client about limit setting and the need for
Stares in lieu of verbal response limits. Include time for discussion.
Physically underactive Teach the client the problem-solving process as an
Somatic aches and pains alternative to acting out (identify the problem,
Dizziness consider alternatives, select and implement an
Nausea, vomiting, stomach problems alternative, and evaluate the effectiveness of the
Fatigue, lethargy solution).
Lonely Help the client practice the problem-solving process
Guilt feelings with situations on the unit, then situations the client
Nervous may face at home, school, and so forth.
Crying spells Role model appropriate conversation and social skills
Feels worthless, unloved for the client.
Specify and describe the skills you are demonstrating
Treatment Practice social skills with the client on a one-on-one
Dramatic interventions, such as "boot camp” or incarceration, basis
have not proved effective and may even worsen the situation.
Treatment must be geared toward the client's developmental Gradually introduce other clients into the inter-actions
age; no one treatment is suitable for all ages. and discussions.
Assist the client in focusing on age- and situation-
appropriate topics.
Encourage the client to give and receive feedback with
others in his or her age group.
Facilitate expression of feelings among clients in
supervised group situations.
Teach the client about transmission of HIV in-fection and
other sexually transmitted diseases(STDs).
Assess the client's use of alcohol or other substances, and
provide referrals as indicated.
You might also like
- Autism Spectrum DisorderDocument5 pagesAutism Spectrum DisorderHadamus Mustre100% (1)
- Unit-4 CHILDHOOD MENTAL DISORDERSDocument22 pagesUnit-4 CHILDHOOD MENTAL DISORDERSNeha JainNo ratings yet
- Cognitive Disorders and Their ClassificationsDocument12 pagesCognitive Disorders and Their ClassificationsyaroenNo ratings yet
- Dominica AutismDocument27 pagesDominica AutismAadeshMistryNo ratings yet
- Autism Spectrum DisordersDocument26 pagesAutism Spectrum Disordersbsndbh65wcNo ratings yet
- Medications for autism spectrum disorder symptomsDocument2 pagesMedications for autism spectrum disorder symptomsMarissa AsimNo ratings yet
- Autism Spectrum Disorder: Fouad Tahan, M.D. PsychiatristDocument35 pagesAutism Spectrum Disorder: Fouad Tahan, M.D. PsychiatristchawkatNo ratings yet
- AUTISMDocument10 pagesAUTISMRayyan AhsanNo ratings yet
- Developmental disorders in pediatrics: Global delay, autism, ADHD & moreDocument21 pagesDevelopmental disorders in pediatrics: Global delay, autism, ADHD & moreAnuj Pratap SinghNo ratings yet
- INE302 Autism Unit 4 NewDocument30 pagesINE302 Autism Unit 4 NewValencia MohlalaNo ratings yet
- AutismDocument26 pagesAutismminangsung minangnengNo ratings yet
- Autism Spectrum Disorder: Group 1Document26 pagesAutism Spectrum Disorder: Group 1LAARNI MARIE G. CARIÑONo ratings yet
- AutismDocument54 pagesAutismSai BruhathiNo ratings yet
- Autism: Dr. Muhammad Mahbubur RahmanDocument28 pagesAutism: Dr. Muhammad Mahbubur RahmanMahbubur RahmanNo ratings yet
- Autism (Asd)Document28 pagesAutism (Asd)Mona SabharwalNo ratings yet
- Autism: Autism Diagnosis DSM IV MatchDocument6 pagesAutism: Autism Diagnosis DSM IV MatchReyhan VivaldyNo ratings yet
- Understanding Autism Spectrum DisorderDocument24 pagesUnderstanding Autism Spectrum DisorderNishthaNo ratings yet
- Pervasive Developmental Disorders and Autism Spectrum DisorderDocument29 pagesPervasive Developmental Disorders and Autism Spectrum DisorderNikki BrodethNo ratings yet
- AUTISMDocument130 pagesAUTISMJalareNo ratings yet
- Presentation 1Document17 pagesPresentation 1api-547492718No ratings yet
- Understanding Pervasive Developmental DisordersDocument20 pagesUnderstanding Pervasive Developmental DisordersHikari 光 Shidou100% (1)
- Chapter 8 Childhood DisordersDocument6 pagesChapter 8 Childhood DisordersDessirie EnriquezNo ratings yet
- CHILDHOOD DISORDERS DIAGNOSEDDocument71 pagesCHILDHOOD DISORDERS DIAGNOSEDKalaivanan SelvamNo ratings yet
- Childhood Psychological DisordersDocument7 pagesChildhood Psychological DisordersineedthisforaschoolprojectNo ratings yet
- Neurodevelopmental DisordersDocument3 pagesNeurodevelopmental DisordersJustine BayabosNo ratings yet
- Child and Adolescent DisorderDocument38 pagesChild and Adolescent DisorderZeref KakarotNo ratings yet
- Persistent Impairments in Social Communication, and Restricted, Repetitive and Stereotyped Patterns If Behaviours, Interests, or ActivitiesDocument4 pagesPersistent Impairments in Social Communication, and Restricted, Repetitive and Stereotyped Patterns If Behaviours, Interests, or ActivitiesWaqas AhsanNo ratings yet
- AutismDocument25 pagesAutismGreatchie Mabala100% (1)
- Autism Spectrum Disorder (Asd) : PRESENTED BY: Ms Mamta BishtDocument21 pagesAutism Spectrum Disorder (Asd) : PRESENTED BY: Ms Mamta BishtRudra prasad SahuNo ratings yet
- Autism Spectrum Disorder Final HandoutDocument2 pagesAutism Spectrum Disorder Final Handoutapi-264629576No ratings yet
- Peads ConditionDocument9 pagesPeads ConditionzikryshafiqahNo ratings yet
- Other DisabilitiesDocument42 pagesOther DisabilitiesRica MarquezNo ratings yet
- Definition of Autism and ADHDDocument4 pagesDefinition of Autism and ADHDNJ BesanaNo ratings yet
- James Morrison - Chapter 1 and 14Document5 pagesJames Morrison - Chapter 1 and 14Amanda ParrellaNo ratings yet
- Abnormal Psychology Mental Retardation Autism Childhood DisordersDocument15 pagesAbnormal Psychology Mental Retardation Autism Childhood DisordersAraNo ratings yet
- Developmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianDocument75 pagesDevelopmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianCarol Rombaoa Serdenia100% (1)
- Childhood and Adolescent Psychiatric DisordersDocument10 pagesChildhood and Adolescent Psychiatric DisorderslamuraoNo ratings yet
- Submitted By:: Sabroso, Shery Love C. Ricardel, LalaineDocument5 pagesSubmitted By:: Sabroso, Shery Love C. Ricardel, LalaineLove Shery SabrosoNo ratings yet
- Filamer Christian University Curriculum for Autism Spectrum DisordersDocument8 pagesFilamer Christian University Curriculum for Autism Spectrum DisordersJechsa De GuiaNo ratings yet
- DARAN (Research Activity)Document14 pagesDARAN (Research Activity)Jeanette Fernandez DNo ratings yet
- AutismDocument57 pagesAutismsehaab91No ratings yet
- High-Functioning Autism Spectrum Disorder: Parent's Guide to Creating Routines, Diagnosis, Managing Sensory and Autism Awareness in Kids.From EverandHigh-Functioning Autism Spectrum Disorder: Parent's Guide to Creating Routines, Diagnosis, Managing Sensory and Autism Awareness in Kids.Rating: 5 out of 5 stars5/5 (1)
- ASDC - Article - Autism in Deaf ChildrenDocument2 pagesASDC - Article - Autism in Deaf ChildrenEchoNo ratings yet
- Handbook of Childhood Developmental DisordersDocument20 pagesHandbook of Childhood Developmental DisordersObiajuru Ikechukwu100% (1)
- Gomez, Frances Lou T. Eintsped1 E - 2se July 27, 2016Document18 pagesGomez, Frances Lou T. Eintsped1 E - 2se July 27, 2016Frances Lou GomezNo ratings yet
- Autism: Kuliah Blok Xvi FK UMP 2015Document24 pagesAutism: Kuliah Blok Xvi FK UMP 2015Ragil Putra Jaya UtamaNo ratings yet
- Child Psychiatry: DR - Howaida AbbasDocument76 pagesChild Psychiatry: DR - Howaida AbbasEng Abdulahi HajiNo ratings yet
- AutismDocument9 pagesAutismAmr Ramazan IbrahimNo ratings yet
- Cognitive DisabilitiesDocument4 pagesCognitive Disabilitieshannalee13No ratings yet
- Autism TalaDocument14 pagesAutism TalaAgus BarretoNo ratings yet
- Mental disorders signs and symptoms overviewDocument19 pagesMental disorders signs and symptoms overviewMia Charisse FigueroaNo ratings yet
- About ADHD: Undermethylators Undermethylators UndermethylationDocument8 pagesAbout ADHD: Undermethylators Undermethylators UndermethylationsherazbthNo ratings yet
- Childhood DisorderDocument7 pagesChildhood DisorderJerryNo ratings yet
- Classifications of AutismDocument3 pagesClassifications of Autismfaber vbNo ratings yet
- AustismDocument17 pagesAustismslpheyNo ratings yet
- Sexual DysfunctionsDocument2 pagesSexual DysfunctionsEunice CuñadaNo ratings yet
- Neurodevelopmental DisordersDocument8 pagesNeurodevelopmental DisordersEunice CuñadaNo ratings yet
- Psych MidtermsDocument50 pagesPsych MidtermsEunice CuñadaNo ratings yet
- Introduction To NicotineDocument18 pagesIntroduction To NicotineEunice CuñadaNo ratings yet
- Sexual DysfunctionsDocument2 pagesSexual DysfunctionsEunice CuñadaNo ratings yet
- Diabetes Management TipsDocument7 pagesDiabetes Management TipsEunice CuñadaNo ratings yet
- Care of Clients with Maladaptive PatternsDocument55 pagesCare of Clients with Maladaptive PatternsEunice CuñadaNo ratings yet
- Anatomy and Physiology of Adrenal GlandsDocument14 pagesAnatomy and Physiology of Adrenal GlandsEunice CuñadaNo ratings yet
- Pathophysiology of FractureDocument2 pagesPathophysiology of FractureEunice CuñadaNo ratings yet
- Compilation Medsurg PrelimsDocument29 pagesCompilation Medsurg PrelimsEunice CuñadaNo ratings yet
- CBCP Pastoral Exhortation On The Era of New EvangelizationDocument8 pagesCBCP Pastoral Exhortation On The Era of New EvangelizationGlenn Mar DomingoNo ratings yet
- Oxford Handbook Of Psychiatry 4Th Edition Edition David Semple download pdf chapterDocument51 pagesOxford Handbook Of Psychiatry 4Th Edition Edition David Semple download pdf chapterpriscilla.villegas794100% (4)
- Disorders of Children and AdolescentsDocument13 pagesDisorders of Children and AdolescentsJay Mark Samson CabreraNo ratings yet
- The Personality Inventory For DSM-5-Brief Form (PID-5-BFDocument8 pagesThe Personality Inventory For DSM-5-Brief Form (PID-5-BFMaryam safa100% (1)
- Critique PaperDocument1 pageCritique PaperMichelle CastroNo ratings yet
- Appendix XXX - PTSD Checklist For DSM-5 (PCL-5)Document3 pagesAppendix XXX - PTSD Checklist For DSM-5 (PCL-5)lediana afriyantiNo ratings yet
- DSM MnemonicsDocument16 pagesDSM MnemonicsIgwe SolomonNo ratings yet
- Faktor Risiko Attention Deficit Hyperactivity DisoDocument5 pagesFaktor Risiko Attention Deficit Hyperactivity Disochoco cookiesNo ratings yet
- Case of LeticiaDocument3 pagesCase of LeticiaPrincess Ann ErmacNo ratings yet
- Effectiveness of Inpatient Dialectical Behavioral Therapy For Borderline Personality Disorder: A Controlled TrialDocument13 pagesEffectiveness of Inpatient Dialectical Behavioral Therapy For Borderline Personality Disorder: A Controlled TrialBarbara RomeroNo ratings yet
- Stages of Change Readiness and Treatment Eagerness Scale-Drug (SOCRATES 8D)Document4 pagesStages of Change Readiness and Treatment Eagerness Scale-Drug (SOCRATES 8D)RAFAEL OLIMPIO DA SILVANo ratings yet
- MH Dir COMPLETEDocument115 pagesMH Dir COMPLETEgracetoday1001No ratings yet
- Conversion DisorderDocument27 pagesConversion DisorderKhalil Ullah100% (1)
- Literature Review NSG2104Document6 pagesLiterature Review NSG2104Assignment HelpNo ratings yet
- 2022 23 Mental Health Awareness ToolkitDocument182 pages2022 23 Mental Health Awareness ToolkitCraig MongerNo ratings yet
- Trauma-Informed Supervision Clinical Supervision of Substance Use D o CounselorsaDocument17 pagesTrauma-Informed Supervision Clinical Supervision of Substance Use D o Counselorsaapi-626136134No ratings yet
- SFH Mod 4Document14 pagesSFH Mod 4goutami SunthankarNo ratings yet
- Case Report1Document8 pagesCase Report1Sahil MushafNo ratings yet
- Adult ADHD checklist symptoms self-assessmentDocument1 pageAdult ADHD checklist symptoms self-assessmentbob cretNo ratings yet
- Does Chinese Calligraphy Therapy Reduce Neuropsychiatric Symptoms - A Systematic Review and Meta - AnalysisDocument9 pagesDoes Chinese Calligraphy Therapy Reduce Neuropsychiatric Symptoms - A Systematic Review and Meta - AnalysisSAMNo ratings yet
- Venessa Shannen Wah Pei Yue 2020277834 - Elc 231 - Mid Sem TestDocument8 pagesVenessa Shannen Wah Pei Yue 2020277834 - Elc 231 - Mid Sem TestVenessa WahNo ratings yet
- Guilford Child & Adolescent Psychology Chapter SamplerDocument97 pagesGuilford Child & Adolescent Psychology Chapter SamplerAdelaKočanBahtoNo ratings yet
- Case Formulation in PsychiatryDocument8 pagesCase Formulation in PsychiatryMarius PaţaNo ratings yet
- ADHDDocument4 pagesADHDshreya DahalNo ratings yet
- Understanding Avoidant Restrictive Food Intake Disorder (ARFIDDocument11 pagesUnderstanding Avoidant Restrictive Food Intake Disorder (ARFIDPirandello100% (1)
- The Americanization of Mental IllnessDocument4 pagesThe Americanization of Mental Illnessfiona.tangNo ratings yet
- Mental HealthDocument16 pagesMental HealthnataliaNo ratings yet
- BH DBT Skills Distress Tolerance pt2Document12 pagesBH DBT Skills Distress Tolerance pt2Jana100% (1)
- CADDRA ADHD Information Resources HandoutDocument2 pagesCADDRA ADHD Information Resources HandoutMustafa AlmasoudiNo ratings yet
- Neelam UDPD Report 1Document50 pagesNeelam UDPD Report 1adiba KhanNo ratings yet
- DeliriumDocument37 pagesDeliriumalishba iqbal 1112No ratings yet