Professional Documents
Culture Documents
Radiographic Evaluation of Scoliosis 2010 Malfair
Uploaded by
febyan yohanesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radiographic Evaluation of Scoliosis 2010 Malfair
Uploaded by
febyan yohanesCopyright:
Available Formats
AJR Integrative Imaging
LIFELONG LEARNING
FOR RADIOLOGY
Radiographic Evaluation of Scoliosis: Review
David Malfair1, Anne K. Flemming1, Marcel F. Dvorak2, Peter L. Munk1, Alexandra T. Vertinsky1, Manraj K. Heran1,
Doug A. Graeb1
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
OBJECTIVE has the additional advantages of low radiation dose, low cost,
Despite enormous advances in cross-sectional imaging and wide availability.
over the past few decades, radiography remains the main- This article will concentrate on what measurements are
stay of diagnosis and evaluation of scoliosis. Knowledge of obtained in the radiographic evaluation of the spine and how
technical factors, measurement error, and measurement these values inform management. Understanding these con-
techniques is important in the comparison of serial radio- cepts and their role in surgical decision making assists the
graphs and affects surgical decision making. This article radiologist in the interpretation of preoperative and postop-
focuses on adolescent idiopathic scoliosis as a framework for erative radiographs as well as cross-sectional imaging. The
understanding the general concepts in the radiographic primary focus will be on adolescent idiopathic scoliosis as a
evaluation of the scoliotic spine. framework for understanding the general concepts in the ra-
diographic evaluation of the scoliotic spine. A limited review
CONCLUSION of other less common causes of scoliosis will be included.
The concepts of sagittal and coronal balance are critical to
the evaluation of spinal deformity. Sideward-bending views al- Technique
low the differentiation of structural and nonstructural curves Careful attention to technique is critical in scoliosis radi-
and affect the choice of levels to be included in an operative ography. Small differences in rotation or magnification and
fusion. Structural curves also are identified by the presence of other alterations in patient position can significantly alter
marked rotation that manifests clinically by the rib hump. spinal curvature measurements [1]. Strict adherence to a
Scoliosis is defined as a lateral curvature of the spine in the standardized technique reduces these errors. The scoliosis
coronal plane. The most common causes include idiopathic radiograph should include the cervical spine superiorly and
scoliosis, more common in younger patients and degenerative the pelvis inferiorly. The assessment of sagittal balance
scoliosis, seen in older patients. Other causes include neuro- makes it particularly important to include the cranium
muscular, congenital, and developmental abnormalities. Sco- down to both femoral heads on the same radiograph. Deter-
liosis also may occur secondary to tumor, infection, and trau- minations of C2 and C7 plumb lines as well as a number of
ma. Despite the enormous advances in cross-sectional imaging pelvic parameters are frequently measured preoperatively
over the past few decades, radiography remains the mainstay for planning of correction and after surgery [2, 3].
of diagnosis and evaluation of scoliosis. The key advantage This field of view may be too large for a single projection,
of radiography is the ability to image the entire spine in the particularly when the deformity is significant. Two digital
standing patient while giving the clinician an appreciation of radiographs are “stitched” together to reproduce the scolio-
the 3D rotatory nature of the scoliotic deformity. Curvatures, sis radiograph. The patient is positioned 72 in (183 cm) from
truncal imbalance, and listhesis are often more prominent on the radiation source with the feet a shoulder width apart
standing weightbearing views compared with images of the and the knees extended. On the lateral images, the patient
same patient in a recumbent position. Standing radiographs looks straight ahead with elbows flexed and hands placed
allow more reliable radiographic measurements that are im- over the clavicles [4]. This keeps the upper extremities from
portant in following the magnitude of the spinal deformity being superimposed over the spine on the lateral view.
over time and ultimately in surgical decision making. The ra- Breast and pelvic shields may be used to reduce the radia-
diographic analysis of curvatures may include sideward- tion dose. A compensating filter ensures that proper bone
bending views and flexion–extension views. Radiography density is maintained throughout the spine.
Keywords: deformity, MRI, radiography, scoliosis
DOI:10.2214/AJR.07.7145
Received December 1, 2008 accepted after revision March 14, 2009.
1
Department of Radiology, University of British Columbia and Vancouver Hospital and Health Sciences Centre, 855 W 12th Ave., Vancouver, BC, Canada V5Z 1M9. Address correspondence
to D. Malfair (dmalfair@gmail.com).
Division of Spine, Department of Orthopedics, University of British Columbia and the Combined Neurosurgical and Orthopedic Spine Program at the Vancouver Hospital and Health
2
Sciences Centre, Vancouver, BC, Canada.
AJR 2010;194:S8–S22 0361–803X/10/1943–S8 © American Roentgen Ray Society
S8 AJR:194, March 2010
Radiography of Scoliosis
The Anatomy of a Curvature rior-end vertebra. If endplates are difficult to visualize, the
Some general definitions are helpful in the discussion of borders of the pedicles may be used. The measurements ob-
spinal deformity. The largest curve in the scoliotic spine is tained using this method should be precise and reproducible
known as the primary or major curvature. A scoliotic defor- because the magnitude of the curve is a major factor in the
mity may have one or several major curves. Other small clinical decision-making process. The total error in assessing
the Cobb angle is approximately 2–7° [6–9]. This error results
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
curves (if present) are termed secondary or minor curvatures.
These minor curves may be fixed, inflexible structural curves from variations in both radiograph production and measure-
or flexible, nonstructural curves. For each curvature, there ment error. Subtle changes in radiograph production, includ-
are terminal and apical vertebrae. The terminal vertebra is ing changes in patient position and posture, caused 2° of
the most tilted superior or inferior vertebra included in a standard error in one study [6]. Overall, intraobserver vari-
curve. The apical vertebra is the most laterally displaced and ability is less than interobserver variability. Therefore, the
most horizontally oriented. It also is the most profoundly ro- radiologist should measure the Cobb angle on both the cur-
tated vertebra and is generally found at the apex of the curve rent study and the historical comparison studies to avoid in-
(Fig. 1). Terminal vertebrae are typically the most tilted and troducing the additional interobserver error. Measuring an-
are selected to make the largest Cobb angle. gles using a PACS has been shown to be equivalent to manual
measurements on conventional radiographs [10].
Measuring Curves When comparing two radiographs, both measured Cobb
The most commonly used and most accurate measurement angles introduce measurement error. A 5° difference in the
of spinal curvature is the Cobb angle [5]. It is obtained by Cobb angle measured between two radiographs represents a
measuring the maximal angle from the superior endplate of 95% chance that there is a true difference [8]. In adolescent
the superior-end vertebra to the inferior endplate of the infe- idiopathic scoliosis, an increase of 5° is thought to indicate
Fig. 1—20-year-old woman with adolescent
idiopathic scoliosis.
A and B, Anteroposterior (A) and lateral (B) standing
radiographs show typical thoracic dextroscoliosis
and thoracolumbar levoscoliosis. Thoracolumbar
curvature is larger and exhibits more rotation and
is therefore major curve in this example. Apical
vertebra of this curvature is L1.
A B
AJR:194, March 2010 S9
Malfair et al.
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
A B C
Fig. 2—13-year-old girl with adolescent idiopathic scoliosis.
A–C, Assessment of curve progression should include comparison of current study (A) with remote previous study. Over multiple 6-month follow-up examinations (B), no
significant change was seen, but when compared with study from 2 years previous (C), significant increase in deformity has occurred.
that significant curve progression is occurring at a 12-month nition that some of the curvature difference may be due to
interval. Cobb angles may also be used to describe kyphotic differences in technique. Is the patient wearing a brace in one
and lordotic angulation on the lateral view. These measure- study and not the other? The curvature is often exaggerated
ments are generally reliable and accurate [11]. Exceptions when the brace is removed (Fig. 3). Is the patient leaning on
include measuring kyphosis in the upper thoracic spine and something or sitting down? It is important to mention the
measuring Cobb angles in large curvatures because of diffi- presence of significant technical differences when comparing
culty in precisely defining the endplates. two studies. In curves of greater magnitude, simply measur-
Several common pitfalls when comparing radiographs for ing the Cobb angle may not show progression. However, as-
curve measurements exist. A patient may not show signifi- sessing the degree of rotation of the apical vertebra, overall
cant curvature progression when the new radiograph is com- spine balance using a C7 vertical line in relation to the pelvis,
pared only with the most recent previous study. However, or indirect measures such as the distance from the iliac crest
significant progression may be detected when comparisons to the lower ribs in a degenerative curve are all clinically sig-
are made with more remote imaging studies; a finding that nificant suggestions of a progressive deformity. Finally, it is
may alter management (Fig. 2). A second pitfall is the recog- important to recognize that supine radiographs and cross-
S10 AJR:194, March 2010
Radiography of Scoliosis
Fig. 3—14-year-old girl with adolescent idiopathic
scoliosis.
A and B, When comparing these two frontal
radiographs in same patient, it is important to note
that patient is wearing brace (arrows) in one study,
which will affect magnitude of curvature.
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
A B
sectional imaging should not be compared with upright ra- symptoms and reducing cosmetic deformity. These goals are
diographs. Measurement of Cobb angles on cross-sectional best achieved by restoring sagittal and coronal balance.
images when the spine is not weight bearing will tend to un- Sagittal balance describes the relationship of the head
derestimate the degree of deformity. relative to the pelvis in the sagittal plane. It is measured on
In adolescent idiopathic scoliosis, the primary clinical a standing lateral view by dropping a plumb line from the
utility of the Cobb angle is in determining the risk of curve center of the C7 vertebral body vertically downward and
progression. The Cobb angle otherwise has limited prognos- assessing the distance of this line from the posterior aspect
tic value. It does not correlate with the degree of morbidity of the S1 vertebral body (Fig. 4). In healthy patients with
or pain. The degree of reduction of the Cobb angle does not neutral sagittal balance, this plumb line intersects this
correlate with patient satisfaction in postoperative outcome sacral landmark [15]. Positive sagittal balance is present if
surveys [12–15]. In fact, complete correction, decompensa- the plumb line is greater than 2 cm anterior to the poste-
tion, or imbalance in patients with neuromuscular scoliosis rior aspect of the S1 vertebral body. Similarly, negative
in whom overcorrection has been reported, results in increased sagittal balance is described with the plumb line is 2 cm
risk of instrumentation failure. posterior to the sacral landmark. Coronal balance is mea-
sured on an upright anteroposterior view. A plumb line is
Sagittal and Coronal Balance dropped vertically from the center of the C7 vertebral
The concept of truncal balance is critical in the evalua- body. This usually intersects with the central sacral verti-
tion of spinal deformity. In the setting of adolescent idio- cal line (Fig. 5). Positive and negative coronal balance are
pathic scoliosis, the primary goals of surgery are to stabi- present when this plumb is line is greater than 2 cm to the
lize the spine and prevent further progression of deformity. right and left, respectively.
This goal is achieved by surgical fusion across the spinal de- Patients with positive sagittal balance commonly present
formity. Additional goals include alleviating the patient’s with back pain, likely to be fatigue pain because the truncal
AJR:194, March 2010 S11
Malfair et al.
muscles, hips, knees, and thighs are under continual strain preoperative radiographic parameters and postoperative
to keep the patient’s head in line with the shoulders and outcomes. They found that patients presenting with loss of
hips and over the feet. Patients with positive sagittal bal- normal lumbar lordosis and positive sagittal balance showed
ance may be described as having a “flat-back” deformity the most benefit from surgery. Glassman et al. [17] present-
with loss of normal lumbar lordosis and resultant forward- ed an outcome study involving 298 patients before adult
tilting posture. These patients unknowingly will flex their scoliosis surgery. Clinical outcome did not correlate with
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
hips and knees to maintain a more erect posture, and this curve magnitude, apical rotation, or the number of major
must be accounted for during positioning for lateral radio- curves. The key radiographic abnormality that resulted in
graphs. Restoration of sagittal balance improves the suc- significant improvement in pain, function, and self image
cess rate of scoliosis surgery. Schwab et al. [16], compared was found to be sagittal balance. The authors concluded
Fig. 4—Drawing shows sagittal balance, Fig. 5—Drawing shows coronal balance, measured Fig. 6—Drawing shows Risser grading. Skeletal
measured as distance between C7 plumb line and as distance between C7 plumb line and central sacral maturity is estimated on scoliosis radiographs by
posterosuperior aspect of S1 vertebral body. Positive vertical line (CSVL). Positive and negative coronal assessment of degree of ossification of iliac crest
or negative sagittal balance is described when plumb balance is described when plumb line is to right or left hypophysis.
line is anterior and posterior to this sacral landmark, of this sacral landmark, respectively.
respectively.
S12 AJR:194, March 2010
Radiography of Scoliosis
that restoration of sagittal balance should be a primary The most common method for determining whether a
goal of spinal deformity surgery. In a related study, the curve is structural is the evaluation of sideward-bending
magnitude of sagittal imbalance correlated with the degree views. Sideward-bending views are obtained upright with
of functional impairment preoperatively [18]. the patient leaning maximally to one side or the other. Some
Coronal balance is another key factor in patient satisfac- authors advocate traction methods or bending over a ful-
tion. The restoration of coronal balance reduces several cos- crum to assess curve flexibility [22, 23]. Klepps et al. [24]
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
metic deformities including having one shoulder higher than noted that sideward-bending views were more effective in
the other. Several measurements of shoulder asymmetry showing flexibility in the proximal thoracic and lumbar
have been described [19], but assessment of the clavicle angle curves, whereas fulcrum-bending views were more effective
is the most reliable. The clavicle angle is formed by the inter- in showing flexibility in main thoracic curvatures. All meth-
section of a tangential line connecting the superior aspect of ods fell short compared with the correction found after sur-
the bilateral distal clavicles to a line parallel to the floor. Kuk- gery in this study.
lo et al. [20] suggest that the clavicle angle can be used to Regardless of the method of obtaining the views, the
determine whether the proximal thoracic curve (T1–T3) Cobb angle of the curvature is assessed on each bending
needs to be included in the fusion in adolescent idiopathic view and compared with neutral position. A curve that has
scoliosis. If the patient has a clavicle angle that is neutral or significant flexibility will straighten when the patient bends
shows elevation of the right shoulder, correction of a major toward the curve. For example, a nonstructural lumbar le-
thoracic dextroscoliosis results in symmetric shoulder posi- voscoliosis will straighten when the patient bends to the
tion. In contradistinction, surgical correction of a thoracic left. The radiographic definition of a structural curve is one
dextroscoliosis exacerbates the position of an already elevat- that does not reduce to less than 25° on bending views. A
ed left shoulder. Surgical fusion of the proximal thoracic nonstructural curve is one that will reduce on bending
curve in this subset of patients can prevent this. This same views, supine position, or after surgical correction of the
study found that normal postoperative shoulder balance cor- primary curve.
related with successful patient postoperative assessments.
In the normal spine, axial rotation is coupled with side- Adolescent Idiopathic Scoliosis
ward-bending. In severe scoliosis, bending and axial rotation Adolescent idiopathic scoliosis is a structural lateral curva-
are often decoupled [21] because of structural changes, such ture of the spine evident in otherwise healthy patients be-
as wedging of vertebrae and intervertebral disks, that occur tween the ages of 10 and 18 years. The diagnosis is confirmed
over time. This structural deformity in the axial plane is not when a 10° lateral curvature is present on a frontal upright
corrected by scoliosis surgery. This has important clinical im- radiograph. Curves smaller that this are within normal varia-
plications. Cosmetic deformities such as a rib hump caused tion, tend to be asymptomatic, and are less likely to progress.
by axial rotation may persist after correction of the scoliosis Taking these factors into account, deformities of a magni-
and may be addressed with a concomitant thoracoplasty, tude less than 10° are best termed curvatures rather than
wherein the prominent rib segments are surgically resected. scoliosis, which implies a disease state. As the name suggests,
adolescent idiopathic scoliosis is a diagnosis of exclusion af-
Structural Versus Nonstructural Curves ter careful clinical history, physical examination, and radio-
The major (largest) curve in the patient with adolescent graphic analysis. It is a common disorder affecting 2–4% of
idiopathic scoliosis is often accompanied by vertebral axial this age cohort [25]. Although small curves are equally com-
rotation and will not completely correct with side-bending mon in both genders, larger curves are 10 times more com-
views and is thus, by definition, the structural curve. Other mon in females. The prevalence of larger curves measuring
curvatures may be inflexible, structural curves or flexible, greater than 40° is 0.1% of the adolescent population [26].
nonstructural curves that are present to maintain truncal The natural history of adolescent idiopathic scoliosis is
balance. For example, a lumbar levoscoliosis may be pres- usually uncomplicated in patients with a small or moderate
ent to compensate for the major thoracic dextroscoliosis degree of deformity. Most patients with curvatures under
and keep the head above the pelvis. Over time, a nonstruc- 50° tend to have the same incidence of back pain and mor-
tural curve may become structural because of shortening tality as is found in the general population [27]. Patients
of ligaments, muscle atrophy, and osseous changes that oc- with curves with a magnitude greater than 50° have been
cur with the spine in a prolonged position. In general, the found to experience a greater prevalence of back pain. Tho-
surgeon attempts to minimize the number of fused motion racic curvatures greater than 100° affect lung function, and
segments. Shorter fusions maintain maximal range of mo- these patients had an increased mortality rate compared
tion and decrease the risk of nonunion. Recognition of a with the general population [27].
nonstructural curve can allow a shorter fusion. If the struc- The risk of curve progression depends on the magnitude of
tural curve is straightened, the nonstructural curve will cor- the curvature and the skeletal maturity. In one study of 727
rect spontaneously. patients with adolescent idiopathic scoliosis and curves mea-
AJR:194, March 2010 S13
Malfair et al.
suring between 5° and 29°, the main determinants of curve show a change in these slowly progressive curvatures. It
progression were the magnitude of the curve, skeletal matu- may be beneficial for patients to keep a copy of the original
rity, and patient’s menarchal status [28]. Skeletal maturity is imaging in these circumstances.
most commonly determined by looking at the presence and Treatment of adolescent idiopathic scoliosis is varied and
degree of ossification of the iliac crest apophysis [29]. In Ris- includes observation, bracing, and surgery. The choice of
ser stage 0, the apophysis is not present. In Risser stages I, II, treatment is based on the degree of morbidity, patient fac-
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
III, and IV, the apophysis covers 25%, 50%, 75%, and 100% tors, surgeon preference, and the risk of curve progression
of the iliac wing, respectively (Fig. 6). Stage V is the adult over time. Bracing has limited effectiveness and is generally
pelvis. Risser staging is commonly used but less accurate in recommended for curves between 25° and 40° only in skele-
the determination of skeletal maturity than the use of hand tally immature patients. Bracing has been shown to suc-
radiographs [30]. Spinal curvatures in skeletally immature cessfully prevent curve progression in 75% in this patient
patients with nonossified iliac apophysis have been found to population [33]. A radiograph showing 50% reduction of
progress in 65% with curves between 20° and 30° and in near- the Cobb angle when the patient is wearing a brace corre-
ly all patients with a curvature greater than 30° [31]. lates with a successful outcome [34]. It should be noted that
Small curvatures seldom progress in an adult. In con- good outcomes also occur with smaller or minimal reduc-
trast, thoracic curves that measure greater than 30° tend to tion of curvatures when the patient is wearing a brace. Sur-
progress. One study with 40 years of follow-up found an gery is generally the preferred option for a skeletally imma-
average of 10° of progression in patients with a 30–50° ture patient with a progressing 40° scoliosis or a skeletally
curve and 30° of progression in patients with a thoracic mature patient with a painful or progressive curve greater
curve greater than 50° [32]. Therefore, patients with a more than 45°. Skeletally immature patients continue to grow
severe curvature should undergo continued radiographic anteriorly after a posterior fusion. This may result in a rota-
evaluation. This slow rate of curve progression in the adult tional deformity, often with a stable Cobb angle, known as
patient offers a unique imaging archiving challenge in the the “crankshaft” phenomenon [35]. Clinically, this often
digital age. Images may be stored for only 7–10 years. A manifests as an increased rib hump in the postsurgical pa-
surgeon may be more likely to operate in a minimally symp- tient. The surgeon may include an anterior fusion in these
tomatic 40-year-old patient with a 60° dextroscoliosis if patients to prevent this occurrence.
that curve has significantly progressed over the past 20 The goals of surgery include restoration of truncal bal-
years and less likely to operate in a stable, unchanging de- ance; a stable, pain-free spinal fusion; and improved cosme-
formity. Comparison with recent radiographs is unlikely to sis, including rib hump, shoulder, and hip symmetry [36].
Fig. 7—Lenke classification of adolescent idiopathic
scoliosis: lumbar modifier. Lumbar A–C, Modifiers A,
B, and C are given when sacral central vertical line lies
between pedicles (A), at level of pedicles (B), and outside
pedicles (C), respectively.
A B C
S14 AJR:194, March 2010
Radiography of Scoliosis
While doing so, the surgeon attempts to spare as many mo- tween T1 and T3), main thoracic (apex between T3 and
tion segments as possible. The goal is not necessarily to com- T12) and thoracolumbar/lumbar curve (apex between T12
pletely straighten the spine. In fact, the degree of deformity and L4). The major curve is the region with the largest Cobb
correction does not correlate with clinical outcome [37]. measurement. The other curves are termed minor curves.
Overcorrection of curves may lead to truncal imbalance [38, On the lateral radiograph, thoracic kyphosis and lumbar
39] or asymmetry of the shoulders. Surgery has a 5% major lordosis are measured.
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
complication rate including a rate of neurologic sequelae of The major curve is always included in the operative fu-
approximately 0.2% [40]. sion. The purpose of the side-bending views is to determine
whether the minor curves should be included in the fusion.
Classification of Scoliosis On the side-bending views, if the lesser curve reduces to less
The Lenke classification for adolescent idiopathic scolio- than 25° Cobb angle measurement, it is a nonstructural
sis is based on the upright anteroposterior, lateral, and side- curve. If it remains greater than 25°, it is a structural curve.
ward-bending radiographs [41]. It is designed to help the On the basis of which curves are structural or nonstruc-
surgeon decide which vertebral levels should be included in tural, six types of curves are constructed (Table 1).
an operative fusion. On the frontal radiograph, three mea- Two modifiers are added to this classification system. The
surements are obtained: the proximal thoracic (apex be- lumbar modifier is determined by assessing the relationship
A B C
Fig. 8—15-year-old girl with adolescent idiopathic scoliosis.
A–C, Side-bending radiographs show thoracic curve is largest curve and therefore structural curve. On leftward-bending views, proximal thoracic and lumbar curves
reduce to below 25° and are therefore nonstructural. Only structural curve is included in operative fusion.
AJR:194, March 2010 S15
Malfair et al.
of the central sacral vertebral line (CSVL) to the apical ver- This classification system can be illustrated with two ex-
tebrae of the lumbar spine (Fig. 7). This central sacral verte- amples. The thoracic dextroscoliosis is the largest curvature
bral line lies between the pedicles in lumbar modifier “A,” and therefore by definition the major curve (Fig. 8). A proxi-
intersects the pedicle in modifier “B,” and is medial to the mal thoracic levoscoliosis and lumbar levoscoliosis are present.
pedicles in modifier “C.” The second modifier is based on the These minor curves straighten to less than 10° on leftward-
degree of thoracic kyphosis. A “–” modifier is given in the bending views. They meet the criterion for nonstructural
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
case of a kyphotic angle less than 10°. An “N” modifier indi- curves and do not need to be included in the fusion. This is
cates a 10–40° kyphosis between T5 and T12. A “+” modifier classified as a Lenke type 1 curve. Postoperative views show
indicates a thoracic kyphosis or greater than 40°. The lumbar spontaneous reduction of the minor curves after surgical fu-
modifier is important in that it guides the surgeon as to when sion of the thoracic dextroscoliosis. The largest curvature is
a selective thoracic fusion may be performed. The thoracic again a thoracic dextroscoliosis in the second example (Fig. 9).
modifier will identify those patients who have profound tho- However, in this case the proximal thoracic levoscoliosis and
racic hypokyphosis and would benefit from restoration of lumbar levoscoliosis do not reduce on leftward-bending views.
thoracic kyphosis to improve their thoracic anteroposterior All three curvatures are structural and must be included in the
dimension and thus chest capacity. fusion. This is a Lenke type 4 curve.
A B C
Fig. 9—Side-bending views in 18-year-old woman with adolescent idiopathic scoliosis.
A–C, On bending views, proximal thoracic curve, main thoracic curve, and lumbar curves do not straighten. All three curves are structural and included in surgical fusion.
S16 AJR:194, March 2010
Radiography of Scoliosis
TABLE 1: Lenke Classification of Adolescent Idiopathic Scoliosis
Curve Type Proximal Thoracic Main Thoracic Thoracolumbar/Lumbar Description
1 Nonstructural Structural Nonstructural Main thoracic
2 Structural Structural Nonstructural Double thoracic
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
3 Nonstructural Structural Structural Double major
4 Structural Structural Structural Triple major
5 Nonstructural Nonstructural Structural Thoracolumbar/lumbar
6 Nonstructural Structural Structural Thoracolumbar/lumbar; main thoracic
Note—Bold denotes major curve.
A B C
Fig. 10—10-year-old boy with scoliosis due to Chiari 1 malformation and syrinx.
A–C, Initial frontal radiograph (A) shows left thoracolumbar curvature as major curve. Age of presentation, sex, leftward curvature, and lack of apical rotation are
atypical for adolescent idiopathic scoliosis. MR image (B) shows peglike cerebellar tonsils and large syrinx. Significant improvement of spinal deformity occurs after
neurosurgical decompression (C).
AJR:194, March 2010 S17
Malfair et al.
From a practical standpoint, it is not necessary for the ra- Many authors contend that routine MRI examinations are
diologist to classify these curves, but an understanding of the not necessary in the absence of neurologic findings when
classification system is helpful in understanding and evaluat- there are typical radiographic findings. Pain is a common
ing these standing films in the preoperative and postopera- symptom of adolescent idiopathic scoliosis, occurring in as
tive period. many as 32% of patients in one series, although it is rarely
This classification system is not the only factor in deter- disabling [47]. Imaging studies are seldom positive when pain
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
mining which levels should be operated on. Skeletal matu-
rity, coronal–sagittal balance, shoulder alignment, and pa-
tient factors also weigh in the surgical decision making. In
the original description of this classification system, inter-
and intraobserver agreement was very good [42]. The curves
in these studies were evaluated with premeasured Cobb an-
gles. When Cobb angles are measured at the time of curve
classification, inter- and intraobserver agreement is fair,
with kappa values of 0.5–0.6 [43].
When Is MRI Indicated?
Adolescent idiopathic scoliosis is a designation that applies
once other causes of scoliosis have been clinically and radio-
logically excluded. Adolescent idiopathic scoliosis is by far
the most common cause of spinal curvature in the teenage
patient. There is a long differential diagnosis for the causes of
spinal deformity (Appendix 1). Most of these different causes
of scoliosis are easily distinguished from adolescent idiopath-
ic scoliosis by age of presentation, clinical history, radio-
graphic appearance, and physical examination. In addition,
many of the other causes of deformity present with spinal
curvatures very different from those of adolescent idiopathic
scoliosis. However, some presentations can imitate adolescent
idiopathic scoliosis. The prevalence of CNS abnormalities in
patients with presumed adolescent idiopathic scoliosis is be-
tween 2% and 4% in most series [44–46].
The typical curve pattern in adolescent idiopathic scolio-
sis is usually a right convex thoracic curve plus or minus an
additional leftward lumbar curve. An atypical curve pat-
tern, such as a thoracic levoscoliosis, may occur in adoles-
cent idiopathic scoliosis but increases the likelihood of an
underlying disorder, particularly when it is observed in a
male. Other atypical curve patterns requiring further inves-
tigation include a short segment curve (less than six seg-
ments), decreased vertebral rotation, rapid progression, and
kyphosis near the apex of the curve (Fig. 10). Aside from
the curve pattern, other findings on the scoliosis radiograph
may elicit further investigation. An underlying tumor or in-
fection may present with osseous destruction or sclerosis
(Fig. 11). Widening of an intervertebral foramen or thick-
ening of the paraspinal line are additional clues for a mass
lesion. Occasionally, however, pathology such as a tethered
cord or syrinx may mimic the typical thoracic dextroscolio-
sis of adolescent idiopathic scoliosis. In these cases, it is A B
controversial as to when MRI is needed. The positive rate Fig. 11—40-year-old man with scoliosis secondary to infection.
for screening all patients is low; however, the risk associated A, Frontal radiograph shows thoracic dextroscoliosis. T9 and T10 vertebrae at
apex of curve show prominent sclerosis and endplate irregularity.
with missing one of these neurologic diagnoses and proceed- B, Sagittal fat-saturated T2-weighted image confirms presence of osteomyelitis–
ing with surgery is extreme. discitis at this level.
S18 AJR:194, March 2010
Radiography of Scoliosis
Fig. 12—23-year-old woman with neurofibromatosis.
A and B, Frontal (A) and lateral (B) radiographs shows
characteristic short-segment kyphoscoliosis, found
in patients with neurofibromatosis.
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
A B
is the only complaint in patients with a normal neurologic Schwend et al. [50] reviewed 95 patients with possible ado-
examination and typical curvature. In a prospective series of lescent idiopathic scoliosis who were referred for MRI.
1,280 patients with adolescent idiopathic scoliosis, no pa- Fourteen of these studies showed intraspinal abnormalities,
tients presenting with only pain had positive MRI findings including 12 cases of syrinx (most secondary to an Arnold-
[46]. Significant MRI abnormalities are rare in patients with Chiari malformation) and one patient with astrocytoma.
a normal neurologic examination. In a prospective study, 327 Four of these patients required neurosurgical intervention.
patients with adolescent idiopathic scoliosis and a normal A left thoracic curve, the presence of a neurologic abnor-
neurologic examination underwent preoperative MRI of the mality, and presentation before the age of 11 years were
spine. Seven patients (2%) were found to have an abnormal- significantly associated with a positive MRI examination.
ity, most commonly an Arnold-Chiari malformation. No pa- In the prospective study by Davids et al. [46], 274 of 1,280
tient required neurosurgical intervention before deformity patients underwent MRI. Of 58 patients with an abnormal
correction [44]. It should be noted that sometimes treatment radiograph but no neurologic symptoms, six had abnormal
of a Chiari I malformation can result in spontaneous reduc- findings on MRI. Loss of apical segment lordosis was found
tion of scoliosis without the need for surgical deformity cor- to be the most specific predictor of an intraspinal abnor-
rection. A second study found that 44 (18%) of 250 consecu- mality. The highest yield was for patients with abnormal
tive patients referred for possible adolescent idiopathic neurologic findings and an atypical curve pattern. Thirteen
scoliosis had an abnormality on MRI, but only 12 (5%) re- of 53 cases referred for abnormal radiographs and positive
quired surgery before deformity correction [48]. Most pa- neurology had positive MRI studies.
tients with abnormal findings on MRI, such as small syrinx Spondylolysis at L5 is common in patients with adoles-
or a small Chiari malformation, were not treated in the ab- cent idiopathic scoliosis because of increased biomechanical
sence of neurologic symptoms. forces at this level. Identification of this finding on radio-
Atypical curves on radiographs may predict an abnor- graphs may alter management because the surgeon may
mality on MRI. In one retrospective study of 30 patients choose to extend the posterior fusion to the pelvis to include
with possible adolescent idiopathic scoliosis and preopera- the area of spondylolysis. If there is concern regarding
tive MRI, six of the seven cases with an underlying syrinx spondylolysis in the lower lumbar spine, a thin-section CT
presented with a left convex or thoracolumbar curve [49]. study is the most accurate confirmatory test.
AJR:194, March 2010 S19
Malfair et al.
Fig 13—25-year-old man patterns may occur. These are best classified as nondystrophic
with neuromuscular
scoliosis secondary
and dystrophic curves [52]. Nondystrophic curvatures appear
to spinal dysraphism. similar to those found in adolescent idiopathic scoliosis but
Radiograph shows tend to occur early and progress more quickly [53]. They are
characteristic long-
segment C-shaped curve treated more aggressively because they tend to be stiffer and
involves entire lumbar have a higher rate of pseudarthrosis [54].
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
and thoracic spine.
Lower lumbar spinal
A dystrophic curvature tends to be a short segment, have
dysraphism is present as a large degree of apical rotation, and is often associated
is ventriculoperitoneal with kyphosis [55]. The phenotype for neurofibromatosis is
shunt. Note pelvic
obliquity with left iliac variable, and patients may first present with a spinal defor-
crest higher than right. mity without a diagnosis of neurofibromatosis. The radiol-
ogist may be the first to suggest the diagnosis in this setting
of the classic curve pattern—a short-segment kyphoscolio-
sis of the upper thoracic spine (Fig. 12). The main differen-
tial diagnosis for this radiographic curve pattern is a failure
of segmentation. The presence of widening neural foramen,
thinned pedicles, and posterior vertebral body scalloping
further supports a diagnosis of neurofibromatosis. These
curvatures tend to progress quickly, and many authors rec-
ommend early surgery [56]. Severe cervical kyphosis is an-
other common abnormality and is highly suggestive of this
diagnosis [57]. It is often visualized on the radiograph but
overshadowed by the more salient thoracic curvature ab-
Degenerative Scoliosis normality. The surgical changes most commonly occur as a
Degenerative lumbar scoliosis is a common cause of back postoperative phenomenon.
pain in the elderly patient. Greater than 50% of elderly
women showed curves of greater than 10% in some referral Neuromuscular Scoliosis
centers [51]. The initial event in these patients is asymmetric Spinal deformity may occur because of a variety of dis-
degenerative change of the disks or facet joints. These chang- orders involving the CNS, peripheral nervous system, a pri-
es result in asymmetric biomechanical forces that result in mary muscle abnormality, or a combination of these disor-
additional asymmetric disk space collapse and eventual lat- ders. The spinal deformity pattern, natural history, and
eral listhesis and segmental rotator listhesis between lumbar treatment of these heterogeneous disorders are similar. Spi-
segments. This degenerative cascade culminates in a defor- nal deformity occurs in the majority of cases when a disor-
mity seen in the coronal, sagittal, and transverse planes. der of the nervous system or muscles manifests in the grow-
Degenerative scoliosis tends to occur in the lumbar spine ing patient. Although the cause of scoliosis in these patients
and is often associated with hypolordosis, lumbar flat-back, is incompletely understood, most authors consider asym-
and coronal plane decompensation, although any number metric muscular tone, including spasticity and paralysis, to
of curve patterns may occur. Rotatory listhesis is common, be an important factor [58].
often in the coronal plane. Patients with degenerative sco- The goals of treatment are significantly different in this
liosis often present with pain and disability, which are often patient population than in adolescent idiopathic scoliosis.
associated with either radicular pain due to foraminal or far Halting progression of the curve is important in this popu-
lateral root compression or claudication symptoms due to lation, and the magnitude of scoliosis continues to increase
central, foraminal, or subarticular spinal stenosis [17, 18]. in adulthood. Respiratory compromise in neuromuscular
Degenerative scoliosis represents a complex heterogeneous disorders can be further compromised by a superimposed
group of disorders. The surgical treatment choices are nu- spinal deformity with reports of improvement after surgi-
merous and beyond the scope of this article. The goals of cal fusion [59]. The concept of seating balance is another
surgical treatment are primarily neural decompression and consideration in treatment. The curve correction may be
correction of truncal balance. performed to allow easier seating balance, use of a wheel
chair, pain control, and trunk support to facilitate respira-
Neurofibromatosis tory function. Ideally, the patient should be able to sit in a
Neurofibromatosis is a genetic disorder involving both neu- wheelchair without using the arms as a support.
roectodermal and mesenchymal elements. Spinal deformity is A long C-shaped curvature is usually the presenting de-
the most common skeletal abnormality and occurs in approxi- formity in the patient with neuromuscular scoliosis (Fig.
mately one fourth of patients. Any number of different curve 13). The presence of pelvic obliquity is important in radio-
S20 AJR:194, March 2010
Radiography of Scoliosis
graphic evaluation. When present, this obliquity increases dicting outcome and complications in the surgical treatment of adult scoliosis.
the risk of skin breakdown and ischial ulcers. Sitting obliq- Spine 2008; 33:2243–2247
17. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of ra-
uity is measured as an angle between a line tangential to the diographic parameters and clinical symptoms in adult scoliosis. Spine 2005;
iliac crests and one parallel to the floor [60]. The operative 30:682–688
fusion will often need to include the pelvis in this circum- 18. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The
stance. In some cases, visualized kyphosis is actually sec- impact of positive sagittal balance in adult spinal deformity. Spine 2005;
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
30:2024–2029
ondary to rotation of the apical vertebra. For example, if
19. Bagó J, Carrera L, March B, Villanueva C. Four radiological measures to esti-
the apical vertebra is rotated 90°, the lateral curvature has mate shoulder balance in scoliosis. J Pediatr Orthop B 1996; 5:31–34
the appearance of a kyphosis relative to the trunk. Defor- 20. Kuklo TR, Lenke LG, Graham EJ, et al. Correlation of radiographic, clinical,
mity correction is more challenging in this patient popula- and patient assessment of shoulder balance following fusion versus nonfusion
tion. An increased incidence of infection, neurologic com- of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine 2002;
27:2013–2020
plications, and pseudarthrosis has been reported [61].
21. Beuerlein MJ, Raso VJ, Hill DL, Moreau MJ, Mahood JK. Changes in alignment
of the scoliotic spine in response to lateral bending. Spine 2003; 28:693–698
Acknowledgment 22. Watanabe K, Kawakami N, Nishiwaki Y, et al. Traction versus supine side-
We thank Lorie Marchinkow for creating the drawings in bending radiographs in determining flexibility: what factors influence these
this article. techniques? Spine 2007; 32:2604–2609
23. Luk KD, Don AS, Chong CS, Wong YW, Cheung KM. Selection of fusion
References levels in adolescent idiopathic scoliosis using fulcrum bending prediction: a
1. Deacon P, Flood BM, Dickson RA. Idiopathic scoliosis in three dimensions: a ra- prospective study. Spine 2008; 33:2192–2198
diographic and morphometric analysis. J Bone Joint Surg Br 1984; 66:509–512 24. Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton J. Prospective com-
2. Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal parison of flexibility radiographs in adolescent idiopathic scoliosis. Spine 2001;
deformity: analysis of spinopelvic and gravity line parameters. Spine 2008; 26:E74–E79
33:1572–1578 25. Roach JW. Adolescent idiopathic scoliosis. Orthop Clin North Am 1999;
3. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. An analysis of sagittal 30:353–365
spinal alignment following long adult lumbar instrumentation and fusion to L5 26. Miller NH. Cause and natural history of adolescent idiopathic scoliosis. Orthop
or S1: can we predict ideal lumbar lordosis? Spine 2006; 31:2343–2352 Clin North Am 1999; 30:343–352
4. Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there 27. Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up
an optimal patient stance for obtaining a lateral 36” radiograph? A critical com- and prognosis in untreated patients. J Bone Joint Surg Am 1981; 63:702–712
parison of three techniques. Spine 2005; 30:427–433 28. Lonstein JE. Scoliosis: surgical versus nonsurgical treatment. Clin Orthop
5. Cobb JR. Outline for the study of scoliosis. Am Acad Orthop Surg Inst Course Relat Res 2006; 443:248–259
Lect 1948; 5:261–275 29. Risser JC. The iliac apophysis: an invaluable sign in the management of scolio-
6. Goldberg MS, Poitras B, Mayo NE, Labelle H, Bourassa R, Cloutier R. Ob- sis. Clin Orthop Relat Res 1958; 11:111–119
server variation in assessing spinal curvature and skeletal development in ado- 30. Little DG, Sussman MD. The Risser sign: a critical analysis. J Pediatr Orthop
lescent idiopathic scoliosis. Spine 1988; 13:1371–1377 1994; 14:569–575
7. Morrissy RT, Goldsmith GS, Hall EC, Kehl D, Cowie GH. Measurement of the 31. Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of
Cobb angle on radiographs of patients who have scoliosis: evaluation of intrin- criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on
sic error. J Bone Joint Surg Am 1990; 72:320–327 Bracing and Nonoperative Management. Spine 2005; 30:2068–2075
8. Pruijs JE, Hageman MA, Keessen W, van der Meer R, van Wieringen JC. Variation 32. Weinstein SL. Idiopathic scoliosis: natural history. Spine 1986; 11:780–783
in Cobb angle measurements in scoliosis. Skeletal Radiol 1994; 23:517–520 33. Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau
9. Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis D. A meta-analysis of the efficacy of non-operative treatments for idiopathic
radiographs: intraobserver and interobserver variation. J Bone Joint Surg Am scoliosis. J Bone Joint Surg Am 1997; 79:664–674
1990; 72:328–333 34. Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV.
10. Kuklo TR, Potter BK, O’Brien MF, Schroeder TM, Lenke LG, Polly DW Jr; Health and function of patients with untreated idiopathic scoliosis: a 50-year
Spinal Deformity Study Group. Reliability analysis for digital adolescent idio- natural history study. JAMA 2003; 289:559–567
pathic scoliosis measurements. J Spinal Disord Tech 2005; 18:152–159 35. Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pe-
11. Kuklo TR, Potter BK, Polly DW Jr, O’Brien MF, Schroeder TM, Lenke LG. diatr Orthop 1989; 9:541–550
Reliability analysis for manual adolescent idiopathic scoliosis measurements. 36. Arlet V, Reddi V. Adolescent idiopathic scoliosis. Neurosurg Clin N Am 2007;
Spine 2005; 30:444–454 18:255–259
12. D’Andrea LP, Betz RR, Lenke LG, et al. Do radiographic parameters correlate 37. Moreland MS. Outcomes of scoliosis fusion: is stiff and straight better? Stud
with clinical outcomes in adolescent idiopathic scoliosis? Spine 2000; 25:1795– Health Technol Inform 2002; 91:492–497
1802 38. Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. De
13. Wilson PL, Newton PO, Wenger DR, et al. A multicenter study analyzing the compensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis.
relationship of a standardized radiographic scoring system of adolescent idio- Spine 1990; 15:927–931
pathic scoliosis and the Scoliosis Research Society outcomes instrument. Spine 39. Benli IT, Tüzüner M, Akalin S, Kiş M, Aydin E, Tandoğan R. Spinal imbalance
2002; 27:2036–2040 and decompensation problems in patients treated with Cotrel-Dubousset instru-
14. White SF, Asher MA, Lai SM, Burton DC. Patients’ perceptions of overall mentation. Eur Spine J 1996; 5:380–386
function, pain, and appearance after primary posterior instrumentation and fu- 40. Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R. Complica-
sion for idiopathic scoliosis. Spine 1999; 24:1693–1699 tions in spinal fusion for adolescent idiopathic scoliosis in the new millennium:
15. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and a report of the Scoliosis Research Society Morbidity and Mortality Committee.
balance in standing volunteers and patients with low back pain matched for age, sex Spine 2006; 31:345–349
and size: a prospective controlled clinical study. Spine 1994; 19:1611–1618 41. Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new clas-
16. Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Pre- sification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;
AJR:194, March 2010 S21
Malfair et al.
83-A:1169–1181 51. Murata Y, Takahashi K, Hanaoka E, Utsumi T, Yamagata M, Moriya H. Chang-
42. Lenke LG, Betz RR, Bridwell KH, et al. Intraobserver and interobserver reli- es in scoliotic curvature and lordotic angle during the early phase of degenera-
ability of the classification of thoracic adolescent idiopathic scoliosis. J Bone tive lumbar scoliosis. Spine 2002; 27:2268–2273
Joint Surg Am 1998; 80:1097–1106 52. Crawford AH, Herrera-Soto J. Scoliosis associated with neurofibromatosis.
43. Richards BS, Sucato DJ, Konigsberg DE, Ouellet JA. Comparison of reli- Orthop Clin North Am 2007; 38:553–562
ability between the Lenke and King classification systems for adolescent id- 53. Mineiro J, Weinstein SL. Subcutaneous rodding for progressive spinal curva-
iopathic scoliosis using radiographs that were not premeasured. Spine 2003; tures: early results. J Pediatr Orthop 2002; 22:290–295
Downloaded from www.ajronline.org by Childrens Hospital on 04/14/14 from IP address 134.174.21.158. Copyright ARRS. For personal use only; all rights reserved
28:1148–1156 54. Crawford AH. Pitfalls of spinal deformities associated with neurofibromatosis
44. Do T, Fras C, Burke S, Widmann RF, Rawlins B, Boachie-Adjei O. Clinical in children. Clin Orthop Relat Res 1989; 245:29–42
value of routine preoperative magnetic resonance imaging in adolescent idio- 55. Hunt JC, Pugh DG. Skeletal lesions in neurofibromatosis. Radiology 1961;
pathic scoliosis: a prospective study of three hundred and twenty-seven pa- 76:1–20
tients. J Bone Joint Surg Am 2001; 83-A:577–579 56. Calvert PT, Edgar MA, Webb PJ. Scoliosis in neurofibromatosis: the natural
45. Maiocco B, Deeney VF, Coulon R, Parks PF Jr. Adolescent idiopathic scoliosis history with and without operation. J Bone Joint Surg Br 1989; 71:246–251
and the presence of spinal cord abnormalities: preoperative magnetic resonance 57. Holt JF, Wright EM. The radiologic features of neurofibromatosis. Radiology
imaging analysis. Spine 1997; 22:2537–2541 1948; 51:647–664
46. Davids JR, Chamberlin E, Blackhurst DW. Indications for magnetic resonance 58. Berven S, Bradford DS. Neuromuscular scoliosis: causes of deformity and
imaging in presumed adolescent idiopathic scoliosis. J Bone Joint Surg Am principles for evaluation and management. Semin Neurol 2002; 22:167–178
2004; 86-A:2187–2195 59. Banta JV, Park SM. Improvement in pulmonary function in patients having
47. Ramirez N, Johnston CE, Browne RH. The prevalence of back pain in children combined anterior and posterior spine fusion for myelomeningocele scoliosis.
who have idiopathic scoliosis. J Bone Joint Surg Am 1997; 79:364–368 Spine 1983; 8:765–770
48. Inoue M, Minami S, Nakata Y, et al. Preoperative MRI analysis of patients with 60. Osebold WR, Mayfield JK, Winter RB, Moe JH. Surgical treatment of para-
idiopathic scoliosis: a prospective study. Spine 2005; 30:108–114 lytic scoliosis associated with myelomeningocele. J Bone Joint Surg 1982; 64-
49. Barnes PD, Brody JD, Jaramillo D, Akbar JU, Emans JB. Atypical idiopathic A:841–856
scoliosis: MR imaging evaluation. Radiology 1993; 186:247–253 61. Sponseller PD, LaPorte DM, Hungerford MW, Eck K, Bridwell KH, Lenke
50. Schwend RM, Hennrikus W, Hall JE, Emans JB. Childhood scoliosis: clinical LG. Deep wound infections after neuromuscular scoliosis surgery: a multi-
indications for magnetic resonance imaging. J Bone Joint Surg Am 1995; center study of risk factors and treatment outcomes. Spine 2000; 25:2461–
77:46–53 2466
APPENDIX 1: Causes of Scoliosis
Idiopathic
Adolescent, juvenile, infantile
Degenerative neuromuscular
Neuropathic
Spina bifida, cerebral palsy
Musculopathic
Muscular dystrophy
Congenital
Anomalous formation
Hemivertebra, wedge vertebra
Failure of segmentation
Unilateral bar or vertebral fusion
Neurogenic
Chiari malformation, syrinx, tethered cord, diastematomyelia
Developmental
Skeletal dysplasias
Achondroplasia, mucopolysaccharidoses
Skeletal dysostoses
Neurofibromatosis, osteogenesis imperfecta, Marfan, Ehlers-Danlos
Secondary
Tumors, infection, trauma
F O R YO U R I N F O R M AT I O N
The reader’s attention is directed to the Self-Assessment Module for this article, which appears on the following pages.
S22 AJR:194, March 2010
You might also like
- Radiographic Evaluation of Scoliosis: Review: ObjectiveDocument15 pagesRadiographic Evaluation of Scoliosis: Review: ObjectivenandagemaNo ratings yet
- Case-Based Review and Self-Assessment Module: Radiologic Signs in Thoracic ImagingDocument15 pagesCase-Based Review and Self-Assessment Module: Radiologic Signs in Thoracic ImagingdiniNo ratings yet
- AJR Radiologic Signs in Thoracic Imaging 2008Document15 pagesAJR Radiologic Signs in Thoracic Imaging 2008wfranelicNo ratings yet
- RG Low-Cost PhantomsDocument13 pagesRG Low-Cost PhantomsAzucena BCNo ratings yet
- The Tutonal For Residents: Aapm/Rsna PhysicsDocument20 pagesThe Tutonal For Residents: Aapm/Rsna PhysicsDeannisa P WardhaniNo ratings yet
- Koong-2012-Australian Dental JournalDocument7 pagesKoong-2012-Australian Dental JournalLaura Victoria Alvarez RodriguezNo ratings yet
- 2305.18221 (1)Document10 pages2305.18221 (1)Worl BossNo ratings yet
- Adult Spinal Deformity Classifi Cation: Frank Schwab Sigurd Berven Keith H. BridwellDocument8 pagesAdult Spinal Deformity Classifi Cation: Frank Schwab Sigurd Berven Keith H. Bridwellmetasoniko81No ratings yet
- Scoliosis ManagementDocument5 pagesScoliosis ManagementYandriyaneStephanieNo ratings yet
- Australian Dental Journal outlines basic principles of radiological interpretationDocument10 pagesAustralian Dental Journal outlines basic principles of radiological interpretationdrg santuy chandnugNo ratings yet
- Reviews-D-19-00020 1..10Document10 pagesReviews-D-19-00020 1..10Alvaro Perez HenriquezNo ratings yet
- Digital radiography workflow review focuses on advantages and challengesDocument9 pagesDigital radiography workflow review focuses on advantages and challengesKaty Tarco RojasNo ratings yet
- Panchmatia Et Al 2015 - Lido PDFDocument8 pagesPanchmatia Et Al 2015 - Lido PDFProfa Luciana GuimarãesNo ratings yet
- 586 2003 Article 613Document9 pages586 2003 Article 613Jossie AcuñaNo ratings yet
- Digital Radiography ReviewDocument4 pagesDigital Radiography ReviewEka JuliantaraNo ratings yet
- Diagnostic Accuracy of Panoramic Radiography and Ultrasonography in Detecting Periapical Lesions Using Periapical Radiography As A Gold StandardDocument7 pagesDiagnostic Accuracy of Panoramic Radiography and Ultrasonography in Detecting Periapical Lesions Using Periapical Radiography As A Gold StandardRafika OljNo ratings yet
- Cury 2004Document5 pagesCury 2004NareshNo ratings yet
- Neonatal Lung Disorders: Pattern Recognition Approach To DiagnosisDocument12 pagesNeonatal Lung Disorders: Pattern Recognition Approach To DiagnosisMeiriyani LembangNo ratings yet
- Ridge Regression Neural Network For Pediatric Bone Age AssessmentDocument10 pagesRidge Regression Neural Network For Pediatric Bone Age AssessmentAliza MustafaNo ratings yet
- Deep Learning For Chest X-Ray Analysis: A Survey: A A A A ADocument33 pagesDeep Learning For Chest X-Ray Analysis: A Survey: A A A A Amayank kumarNo ratings yet
- Radiographic Assessment of Pediatric Foot Alignment: Review: ObjectiveDocument8 pagesRadiographic Assessment of Pediatric Foot Alignment: Review: ObjectiveEGNo ratings yet
- Radiographic Image Analysis e Book 5th Edition Ebook PDFDocument61 pagesRadiographic Image Analysis e Book 5th Edition Ebook PDFroy.mula62298% (42)
- Evaluación - RadiologíaDocument14 pagesEvaluación - RadiologíamonseibanezbarraganNo ratings yet
- Butler2013 Carpo y MenudilloDocument7 pagesButler2013 Carpo y MenudilloBrayandavid Brayan124No ratings yet
- Ajr 21 25606Document11 pagesAjr 21 25606ecavalcantiNo ratings yet
- OMT Migliora Funzioni VisiveDocument2 pagesOMT Migliora Funzioni VisiveEleonora FiocchiNo ratings yet
- Esr Ebook Conventional X-Ray ImagingDocument65 pagesEsr Ebook Conventional X-Ray ImagingkarolynaNo ratings yet
- Progressive Addition Lenses - Matching The Specific Lens To Patient Needs - White PaperDocument20 pagesProgressive Addition Lenses - Matching The Specific Lens To Patient Needs - White Paperataofeeq222No ratings yet
- Clark's Rule: Teknik " " Dalam Bidang Kedokteran GigiDocument4 pagesClark's Rule: Teknik " " Dalam Bidang Kedokteran GigiFelicia HandaliNo ratings yet
- Muscloskeletal UsDocument9 pagesMuscloskeletal UsJERAM SINKONDENo ratings yet
- Bab Ii HNPDocument10 pagesBab Ii HNPSiti Hidayatul FitriNo ratings yet
- Radiological Assessment of Lung Disease in Small Animals 1. Bronchial and Vascular PatternsDocument9 pagesRadiological Assessment of Lung Disease in Small Animals 1. Bronchial and Vascular PatternsSamantha Orozco PinedaNo ratings yet
- Imaging of Spine Trauma: Neuroradiology Review Series Neuroradiology Review SeriesDocument17 pagesImaging of Spine Trauma: Neuroradiology Review Series Neuroradiology Review SeriesSalman Alfarisy GaulNo ratings yet
- Fundamentals Medical ImagingDocument69 pagesFundamentals Medical ImagingViktorya Stoyanova 78563217856321No ratings yet
- PosterolateralDocument16 pagesPosterolateralHENRIQUE AUGUSTO LINONo ratings yet
- Analytical Radiography of Club Feet Reveals Seven Deformity CombinationsDocument5 pagesAnalytical Radiography of Club Feet Reveals Seven Deformity CombinationsrhlzuraNo ratings yet
- Projection RadiographyDocument37 pagesProjection RadiographyAde WijayaNo ratings yet
- Panchbhai 2012Document8 pagesPanchbhai 2012gbaez.88No ratings yet
- MaxFac RadiologyDocument172 pagesMaxFac RadiologyDr. Debbie SabladaNo ratings yet
- Impact of Radiotherapy On Mandibular Bone: A Retrospective Study of Digital Panoramic RadiographsDocument6 pagesImpact of Radiotherapy On Mandibular Bone: A Retrospective Study of Digital Panoramic Radiographsboooow92No ratings yet
- Fracture of The Distal Radius: Epidemiology and Premanagement Radiographic CharacterizationDocument9 pagesFracture of The Distal Radius: Epidemiology and Premanagement Radiographic CharacterizationodivarNo ratings yet
- Imaging Analyses of Bone Tumors JBJSDocument11 pagesImaging Analyses of Bone Tumors JBJSVera VeraNo ratings yet
- Tam Et Al-2015-Journal of NeurochemistryDocument16 pagesTam Et Al-2015-Journal of NeurochemistryAMNo ratings yet
- Imaging of The Osteoporotic Spine Quantitative Approaches inDocument12 pagesImaging of The Osteoporotic Spine Quantitative Approaches insandrashesaria1No ratings yet
- Radiology For Maxillofacial Surgeons The EssentialDocument49 pagesRadiology For Maxillofacial Surgeons The EssentialAbdulkadir AwadhNo ratings yet
- EOS Imaging: Insight Into This Emerging Musculoskeletal Imaging SystemDocument4 pagesEOS Imaging: Insight Into This Emerging Musculoskeletal Imaging SystemAwadhNo ratings yet
- Radiol 2015154026Document1 pageRadiol 2015154026Musculus PopliteusNo ratings yet
- Skeletal System Learning OutcomesDocument67 pagesSkeletal System Learning OutcomesAVE MAE ALEXIS NAVATANo ratings yet
- Velopulos 2017Document9 pagesVelopulos 2017Jansen BrunoNo ratings yet
- Tips&TechniquesforPelvicRadiography (CB, 2009)Document4 pagesTips&TechniquesforPelvicRadiography (CB, 2009)Tuyet-Anh HoangNo ratings yet
- Imaging The Spine: Orthopaedics E Ii: Spine and PelvisDocument13 pagesImaging The Spine: Orthopaedics E Ii: Spine and Pelvisraul ramboyongNo ratings yet
- Medical Image Analysis: Medical Image Analysis On Left Atrial LGE MRI For Atrial Fibrillation Studies: A ReviewDocument30 pagesMedical Image Analysis: Medical Image Analysis On Left Atrial LGE MRI For Atrial Fibrillation Studies: A ReviewNazifa AdhoraNo ratings yet
- ESR Ebook For Undergraduate Education in Radiology - 14 Paediatric Imaging PDFDocument108 pagesESR Ebook For Undergraduate Education in Radiology - 14 Paediatric Imaging PDFANAS ALINo ratings yet
- Pi Is 0002817777560254Document5 pagesPi Is 0002817777560254BogdanNo ratings yet
- MRI Monitoring of Pathological Changes in The Spinal Cord in Patients With Multiple SclerosisDocument13 pagesMRI Monitoring of Pathological Changes in The Spinal Cord in Patients With Multiple SclerosisIreneNo ratings yet
- Computers in Biology and Medicine: Chandrasekaran Raja, Narayanan GangatharanDocument12 pagesComputers in Biology and Medicine: Chandrasekaran Raja, Narayanan GangatharanRaja ChandruNo ratings yet
- ESR Ebook For Undergraduate Education in Radiology - 08a Liver Imaging PDFDocument80 pagesESR Ebook For Undergraduate Education in Radiology - 08a Liver Imaging PDFANAS ALINo ratings yet
- Reject Rates in DMFRDocument10 pagesReject Rates in DMFRDerya İçözNo ratings yet
- Song 2018Document6 pagesSong 2018febyan yohanesNo ratings yet
- Epidemiology of Traumatic Spinal Cord Injury in Developing Countries From 2009 To 2020: A Systematic Review and Meta-AnalysisDocument21 pagesEpidemiology of Traumatic Spinal Cord Injury in Developing Countries From 2009 To 2020: A Systematic Review and Meta-Analysisfebyan yohanesNo ratings yet
- Dhawan 2016Document12 pagesDhawan 2016febyan yohanesNo ratings yet
- MatthewVaracalloMD TotalKneeArthroplastyDocument11 pagesMatthewVaracalloMD TotalKneeArthroplastyfebyan yohanesNo ratings yet
- "ACL Surgery: When To Do It?": Volker Musahl Theresa Diermeier Darren de SA Jon KarlssonDocument4 pages"ACL Surgery: When To Do It?": Volker Musahl Theresa Diermeier Darren de SA Jon Karlssonfebyan yohanesNo ratings yet
- Yukawa 2007Document6 pagesYukawa 2007febyan yohanesNo ratings yet
- Lee 2014Document7 pagesLee 2014febyan yohanesNo ratings yet
- The Clinician's Guide To Prevention and Treatment of OsteoporosisDocument54 pagesThe Clinician's Guide To Prevention and Treatment of Osteoporosisfebyan yohanesNo ratings yet
- Woods 2010Document8 pagesWoods 2010febyan yohanesNo ratings yet
- Du 2013Document9 pagesDu 2013febyan yohanesNo ratings yet
- Blizzard 2016Document9 pagesBlizzard 2016febyan yohanesNo ratings yet
- Magnetic Resonance Imagination of The Peroneus Longus Tendon After Anterior Cruciate Ligament ReconstructionDocument5 pagesMagnetic Resonance Imagination of The Peroneus Longus Tendon After Anterior Cruciate Ligament Reconstructionfebyan yohanesNo ratings yet
- Distaltibiafractures 150630175305 Lva1 App6891Document26 pagesDistaltibiafractures 150630175305 Lva1 App6891febyan yohanesNo ratings yet
- Sun 2015Document5 pagesSun 2015febyan yohanesNo ratings yet
- Laminoplasty Versus Laminectomy With Posterior Spinal Fusion For Multilevel Cervical Spondylotic MyelopathyDocument10 pagesLaminoplasty Versus Laminectomy With Posterior Spinal Fusion For Multilevel Cervical Spondylotic Myelopathyfebyan yohanesNo ratings yet
- Management of Proximal Femur Fractures in The Elderly: Current Concepts and Treatment OptionsDocument15 pagesManagement of Proximal Femur Fractures in The Elderly: Current Concepts and Treatment Optionsfebyan yohanesNo ratings yet
- v1 500197 Reva Navio 7 All Knees Surgical Technique 06.19Document52 pagesv1 500197 Reva Navio 7 All Knees Surgical Technique 06.19febyan yohanesNo ratings yet
- Oac Author Disclosure FormDocument2 pagesOac Author Disclosure Formfebyan yohanesNo ratings yet
- Rbo IfaDocument18 pagesRbo Ifafebyan yohanesNo ratings yet
- Slight Femoral Under-Correction Versus Neutral Alignment in Total Knee Arthroplasty With Preoperative Varus Knees: A Comparative StudyDocument8 pagesSlight Femoral Under-Correction Versus Neutral Alignment in Total Knee Arthroplasty With Preoperative Varus Knees: A Comparative Studyfebyan yohanesNo ratings yet
- Blount Disease: An Update: Orthopedic Clinics of North America December 2014Document12 pagesBlount Disease: An Update: Orthopedic Clinics of North America December 2014febyan yohanesNo ratings yet
- Brachymetacarpia and Brachymetatarsia: Do We Need To Operate?Document10 pagesBrachymetacarpia and Brachymetatarsia: Do We Need To Operate?febyan yohanesNo ratings yet
- Pii s2667254522000130Document8 pagesPii s2667254522000130febyan yohanesNo ratings yet
- Wjo 8 107Document9 pagesWjo 8 107febyan yohanesNo ratings yet
- Principles of Frame Construction: September 2012Document38 pagesPrinciples of Frame Construction: September 2012febyan yohanesNo ratings yet
- Open Fractures: September 2012Document28 pagesOpen Fractures: September 2012febyan yohanesNo ratings yet
- Leber Hereditary Optic Neuropathy: Respiratory Chain Dysfunction and Degeneration of The Optic NerveDocument10 pagesLeber Hereditary Optic Neuropathy: Respiratory Chain Dysfunction and Degeneration of The Optic Nervefebyan yohanesNo ratings yet
- Blountdisease:: An UpdateDocument11 pagesBlountdisease:: An Updatefebyan yohanesNo ratings yet
- Exfix Basic Principles (Solomin Ed.) : February 2016Document11 pagesExfix Basic Principles (Solomin Ed.) : February 2016febyan yohanesNo ratings yet
- Journal Complications of Corneal Collagen Cross LinkingDocument9 pagesJournal Complications of Corneal Collagen Cross LinkingsuryanegraNo ratings yet
- A Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IDocument28 pagesA Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IJorge Ramírez100% (1)
- Coachman Pink QDT 2010 PDFDocument15 pagesCoachman Pink QDT 2010 PDFHugoMoralesTecnicoDentalNo ratings yet
- COWELL Implant Solution v28Document146 pagesCOWELL Implant Solution v28Julian MachoNo ratings yet
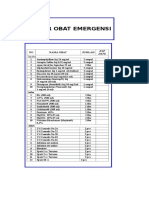
- Daftar Obat Alkes Trolley EmergencyDocument15 pagesDaftar Obat Alkes Trolley EmergencyPRIHATINNo ratings yet
- THORACENTESISDocument9 pagesTHORACENTESISJohn Ray J. PaigNo ratings yet
- SuccinylcholineDocument2 pagesSuccinylcholineSalma KarimahNo ratings yet
- Vitreous Gel Eye Retinal Detachment OphthalmologistDocument12 pagesVitreous Gel Eye Retinal Detachment OphthalmologistLesTrechSaNo ratings yet
- Multi-modality imaging assessment of native valvular regurgitationDocument62 pagesMulti-modality imaging assessment of native valvular regurgitationВенцислав МирчевNo ratings yet
- Thyroid Gland NotesDocument21 pagesThyroid Gland NotesbryanNo ratings yet
- Uro-Final MCQDocument45 pagesUro-Final MCQع كيف كيفك Dhaif-saeedNo ratings yet
- HMDA Mechanical Services Data Book Medical Gas Systems 2021 Edition Medical GasesDocument35 pagesHMDA Mechanical Services Data Book Medical Gas Systems 2021 Edition Medical GaseseimrehNo ratings yet
- Docifu30002940j Perfecttcsii Ifu Eu Languagessallaindv1Document196 pagesDocifu30002940j Perfecttcsii Ifu Eu Languagessallaindv1Miguel De Los Santos PavisicNo ratings yet
- Hernia Repair and Colectomy Course: TR400.HCOL - SiDocument2 pagesHernia Repair and Colectomy Course: TR400.HCOL - SiShayne JacobsonNo ratings yet
- The Bainbridge and The Reverse Bainbridge.8Document13 pagesThe Bainbridge and The Reverse Bainbridge.8Archisha KapoorNo ratings yet
- cEEG Monitoring in The ICU: Treating Subclinical Seizures Is Cost EffectiveDocument26 pagescEEG Monitoring in The ICU: Treating Subclinical Seizures Is Cost EffectiveVijay GadagiNo ratings yet
- Spondylolisthesis PDFDocument2 pagesSpondylolisthesis PDFkriswantiNo ratings yet
- Medical Supplies Part 1 PDFDocument11 pagesMedical Supplies Part 1 PDFPaulo ManuelNo ratings yet
- 1 CathDocument12 pages1 CathHashem AlsmadiNo ratings yet
- 2 Study of Female Pelvic Pain ..Document69 pages2 Study of Female Pelvic Pain ..Ghofran Ibrahim HassanNo ratings yet
- A Shade Selection TechniqueDocument4 pagesA Shade Selection TechniqueKirti JajooNo ratings yet
- Choanal AtresiaDocument4 pagesChoanal AtresiaAshitha S KabeerNo ratings yet
- Brosur Carl Zeiss Visumax Corneal Surgery Mel 90Document21 pagesBrosur Carl Zeiss Visumax Corneal Surgery Mel 90khairul ihsanNo ratings yet
- Emergency Nursing (Medical Emergencies - ABC) - StudentsDocument19 pagesEmergency Nursing (Medical Emergencies - ABC) - StudentsAngielyn Ramos OlorazaNo ratings yet
- Malleolar Fractures - Handout PDFDocument14 pagesMalleolar Fractures - Handout PDFAlin Bratu100% (2)
- Surgical Handrub Technique PosterDocument1 pageSurgical Handrub Technique PosterAbi Zaki0% (1)
- Go With The Flow of Chest Tube Therapy: by Arlene M. Coughlin, RN, MSN, and Carolyn Parchinsky, RN, MADocument14 pagesGo With The Flow of Chest Tube Therapy: by Arlene M. Coughlin, RN, MSN, and Carolyn Parchinsky, RN, MAhady920100% (1)
- Pediatric Surgery: Review Questions: Self-Assessment in General SurgeryDocument3 pagesPediatric Surgery: Review Questions: Self-Assessment in General Surgerymkct111No ratings yet
- Ultrasound Imaging of The NeckDocument25 pagesUltrasound Imaging of The Neckmark jacob dela rosaNo ratings yet
- Cardiopulmonary Resuscitation - Lesson PlanDocument17 pagesCardiopulmonary Resuscitation - Lesson Planmonika makwanaNo ratings yet