Professional Documents
Culture Documents
Diagnosis of Fluid Overload: From Conventional To Contemporary Concepts
Uploaded by
benitez1228Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnosis of Fluid Overload: From Conventional To Contemporary Concepts
Uploaded by
benitez1228Copyright:
Available Formats
Review Article
Cardiorenal Med Received: August 2, 2022
Accepted: August 26, 2022
DOI: 10.1159/000526902 Published online: September 12, 2022
Diagnosis of Fluid Overload: From
Conventional to Contemporary Concepts
Abhilash Koratala a Claudio Ronco b, c Amir Kazory d
aDivision
of Nephrology, Medical College of Wisconsin, Milwaukee, WI, USA; bDepartment of Nephrology,
San Bortolo Hospital and International Renal Research Institute of Vicenza (IRRIV), Vicenza, Italy; cDepartment of
Medicine, University of Padova, Padova, Italy; dDivision of Nephrology, Hypertension, and Renal Transplantation,
University of Florida, Gainesville, FL, USA
Keywords Introduction
Fluid overload · Heart failure · Point-of-care
ultrasonography · Point-of-care ultrasound · Critical illness Recognizing and treating fluid overload (FO) is a key
component of managing patients with heart failure (HF).
The pathophysiology of FO is complex and involves an
Abstract interplay of absolute volume gain, fluid redistribution
Fluid overload has been associated with morbidity and mor- from venous capacitance beds to the central venous cir-
tality in various clinical scenarios including heart failure and culation, and inadequate elimination due to renal dys-
critical illness. It exerts pathologic sequelae in almost all the function, salt and water retention, and endothelial dys-
organ systems. Proper management of patients with fluid function. FO leads to hemodynamic congestion charac-
overload requires knowledge of the underlying pathophysi- terized by elevated cardiac filling pressures, which
ology, objective evaluation of volume status, selection of ap- subsequently results in clinical congestion manifested by
propriate therapeutic options, and maintenance and modu- signs and symptoms such as orthopnea, elevated jugular
lation of tissue perfusion. There are several methods to ap- venous pressure (JVP), peripheral edema, and rales [1]. It
praise volume status but none without limitations. In this is well recognized that in patients hospitalized for decom-
review, we discuss the diagnostic utility, prognostic signifi- pensated HF, persistent congestion at discharge portends
cance, and shortcomings of various bedside tools in the de- worse outcomes [2–5]. In the recent past, the deleterious
tection of fluid overload and evaluation of hemodynamic effects of FO are being increasingly recognized in other
status. These include clinical examination, biomarkers, blood clinical settings such as critical illness where empiric ad-
volume assessment, bioimpedance analysis, point-of-care ministration of intravenous fluid (IVF) is a common sce-
ultrasound, and remote pulmonary pressure monitoring. In nario. In a meta-analysis including 19,902 patients admit-
our opinion, clinicians must adopt a multiparametric ap- ted to the intensive care unit (ICU), the cumulative fluid
proach offsetting the limitations of individual methods to balance after 1 week of ICU stay in nonsurvivors was
formulate a management plan tailored to patients’ needs. found to be 4.4 L more than in survivors. Moreover, a re-
© 2022 The Author(s). strictive fluid management was associated with a lower
Published by S. Karger AG, Basel mortality compared to liberal fluid administration (24.7
Karger@karger.com © 2022 The Author(s). Correspondence to:
www.karger.com/crm Published by S. Karger AG, Basel Abhilash Koratala, akoratala @ mcw.edu
This is an Open Access article licensed under the Creative Commons
Attribution-NonCommercial-4.0 International License (CC BY-NC)
(http://www.karger.com/Services/OpenAccessLicense), applicable to
the online version of the article only. Usage and distribution for com-
mercial purposes requires written permission.
Fig. 1. Pathologic effects of fluid overload in various organs/organ systems. BioRender® was used to create the figure.
vs. 33.2%; p < 0.0001) [6]. Similarly, in a cohort of criti- quent impaired organ perfusion is gaining recognition
cally ill patients with cirrhosis, a higher median fluid bal- challenging the traditional forward flow-centric para-
ance 7 days post-ICU admission (+13.50 vs. +6.90 L; p = digm and shifting the focus from “fluid responsiveness”
0.036) was associated with an increased risk of in-hospital to “fluid tolerance” [23, 24]. Objective assessment of fluid
mortality [7]. Interestingly, a recent clinical trial demon- status is a critical step in timely detection of FO and titrat-
strated that restrictive fluid management strategy is safe ing therapy to optimize hemodynamics. Though accu-
in patients with septic shock compared to standard care rate, the utility of invasive modalities such as pulmonary
(i.e., liberal strategy); although the outcome was not su- artery catheterization is limited to a small subset of criti-
perior in the restrictive group, it is notable that the stan- cally ill patients and does not necessarily improve out-
dard care group received substantially less fluid com- comes [25]. In this review, we will provide an overview of
pared to prior studies (a median of 3.8 L) [8]. While a various bedside tools/laboratory tests in the evaluation of
direct causative relationship cannot be established be- FO and congestion focusing on but not limited to HF.
tween FO and mortality based on the current evidence, it
is a potentially preventable cause of iatrogenic morbidity;
there are data that suggest FO adversely affects almost all Clinical Examination
the organ systems [9, 10] (Fig. 1). For example, FO leads
to pulmonary edema, low lung compliance, increased Careful history taking and physical examination of the
work of breathing [11, 12]; delirium, raised intra-cranial cardiopulmonary system are the first steps in the manage-
pressure [13–15]; prolonged ileus, impaired hepatic syn- ment of patients with FO. These are intended to detect
thetic function, cholestasis, impaired drug absorption increased cardiac filling pressures and their consequenc-
[16, 17]; impaired cardiac contractility and conduction es. However, as mentioned, hemodynamic congestion
abnormalities [18, 19]; acute kidney injury (AKI) [20, 21]; may exist in the absence of clinical congestion. Therefore,
impaired wound healing [22]; and so forth. Furthermore, it is conceivable that the sensitivity of these findings is
the contribution of FO to venous congestion and conse- relatively low to detect ongoing congestion; sole reliance
2 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
on them to manage patients eventually leads to clinically <500 pg/mL) conferred a favorable outcome in one study
apparent FO and recurrent hospitalizations. For instance, [32]. Nevertheless, natriuretic peptide-guided therapy
in a study including 50 HF patients with severely reduced was not associated with superior cardiovascular outcome
ejection fraction (18%), the combined sensitivity of rales, compared to standard care in patients with HF with re-
edema, and elevated mean JVP was just 58% to detect an duced ejection fraction in two recent clinical trials [33,
elevated pulmonary capillary wedge pressure of ≥22 mm 34]. Moreover, approximately 20–35% of outpatients
Hg despite good specificity [26]. Similarly, in a meta- with HF with preserved ejection fraction may exhibit a
analysis of 22 studies including patients presenting with state of intermittent or chronic natriuretic peptide defi-
dyspnea [27], pooled sensitivities of orthopnea, periph- ciency despite coexisting hemodynamic congestion [35,
eral edema, JVP, third heart sound, and rales were only 36]. Additionally, the concentrations of natriuretic pep-
50%, 51%, 39%, 13%, and 60%, respectively, to diagnose tides are elevated in patients with renal dysfunction ow-
congestive HF. Only parameter among these with a posi- ing to impaired clearance limiting their utility [28].
tive likelihood ratio above 10 was the third heart sound
(S3 gallop), which ironically had the lowest sensitivity. In Lactate
summary, most of the conventional physical examination HF is classically described as a condition in which the
findings are helpful when present, but their absence does cardiac pump is not able to support adequate oxygen de-
not exclude congestion. Patients’ weight is useful but lim- livery to the tissues [37]. Surprisingly however, blood lac-
ited by documentation errors, inaccurate calibration of tate, a marker of tissue hypoperfusion, is normal in ∼75%
the equipment, and inability to detect redistribution-re- of patients with advanced HF and a widened arterio-ve-
lated FO. nous oxygen difference [38]. On the other hand, the risk
of mortality is higher in patients with acute HF who have
elevated lactate levels on hospital admission [39]. Al-
Biomarkers though HF treatment may reduce lactate levels, it is un-
clear whether lactate-guided treatment translates into
Several biomarkers have been studied in patients with better clinical outcomes. This is even more vague in the
HF, which can be broadly classified into markers of in- context of septic shock where reduced lactate clearance
flammation (C-reactive protein, myeloperoxidase), fi- (as opposed to increased production) may prompt the cli-
brosis and extracellular remodeling (procollagen, galec- nician to administer IVF in the absence of tissue hypoper-
tin-3, ST2), mechanical strain/stretch (natriuretic pep- fusion, contributing to iatrogenic FO [40]. For instance,
tides, CD146, carbohydrate antigen 125 [CA125]), in the ANDROMEDA-SHOCK trial, lactate-guided re-
markers of hemodynamic homeostasis (adrenomedullin, suscitation group received an excess of 400 mL of IVF
copeptin), tissue perfusion (lactate), and cardiomyocyte within the first 8 h compared to the capillary refill time-
injury (troponins) [28, 29]. Herein, we discuss some of guided group while having more organ dysfunction at 72
the commonly tested biomarkers in clinical practice. In h [41].
the ICU setting, their utility is often limited because of
variable specificity and presence of multiple confounding Hemoglobin and Hematocrit
factors. Expansion of plasma volume (PV) leads to decreased
red blood cell concentration (hemodilution) and vice ver-
Natriuretic Peptides sa. Therefore, hemoconcentration or increasing hemato-
Natriuretic peptides are frequently used as an adjunct crit with fluid removal has been purported as a surrogate
to clinical assessment in patients presenting with symp- for evaluating decongestion and plasma refill rate [42]. In
toms suggestive of HF. In fact, B-type natriuretic peptide a study including 102 patients hospitalized for acute HF,
(BNP) levels have an excellent negative predictive value hemodilution during the first 3 days was associated with
(96% at levels ≤50 pg/mL) for HF diagnosis in such pa- a severe degree of pulmonary edema compared to those
tients [30]. In addition, they carry prognostic significance who had hemoconcentration (85 vs. 63%, p < 0.01). Ad-
with observational studies showing better outcomes in ditionally, HF-related readmission rate was higher in the
patients whose levels decrease in response to deconges- hemodilution group (34 vs. 9%, p < 0.01) [43]. Likewise,
tive therapy [28, 31]. Similar findings have been observed in the post hoc analysis of the PROTECT trial [44], a rap-
in critically ill patients with septic cardiomyopathy id increase in hemoglobin level during the first week was
though the data are sparse; a decline in BNP over time (to independently associated with a favorable outcome, de-
Fluid Overload Cardiorenal Med 3
DOI: 10.1159/000526902
spite a slight decline in renal function in patients hospital- known volume (V) and its concentration (C) is measured.
ized with HF. Conversely, a subset of patients with HF Then, the unknown volume can be calculated by the for-
may have true polycythemia as a response to chronic low mula, V = q/C [46]. In the method that is commercially
cardiac output state, hypoxemic tissue perfusion, and tis- available currently (BVA-100 Blood Volume Analyzer;
sue acidosis; this may predispose to increased risk of Daxor Corp., New York, NY, USA), a standard dose of
thrombosis and myocardial work burden from blood hy- radioactive iodine-labeled albumin (I-131) is injected in-
perviscosity. In such cases, clinicians must exercise cau- travenously. A pre-injection blood sample is collected fol-
tion not to mistake dilution-related pseudo-anemia for lowed by a series of samples at timed intervals once the
true anemia, especially if contemplating erythropoietin tracer has fully circulated in the bloodstream. Plasma ra-
therapy [45, 46]. Quantitative analysis of PV may be help- dioactivity of each sample is then measured using a semi-
ful in some cases to titrate diuretic therapy based on ad- automated computerized counter which calculates pa-
justed red blood cell volume. tient’s PV by comparing the concentration of undiluted
tracer prior to injection to the tracer concentration di-
Carbohydrate Antigen 125 luted over time due to transudation of albumin into ex-
CA125 is a high molecular weight transmembrane gly- tracellular space (Fig. 2). Total BV is determined based on
coprotein used in the diagnosis and prognostication of the measured PV and patient’s hematocrit [50]. Normal
ovarian cancer. In the recent past, there has been a re- total BV is generally defined as measured volumes within
newed interest in its role as a biomarker for congestion in ±8% (approximately 3 standard deviations) of the expect-
HF. It has been proposed that CA125 is shed from meso- ed normal for the patient, and red blood cell mass and PV
thelial cell surfaces in response to mechanical stress such as measured volumes within ±10% of expected normal.
as FO, and inflammatory stimuli. High CA125 levels are Mild to moderate total BV expansion is defined as >8%
associated with the presence of serosal fluid and positive- (>10% for red blood cell mass and PV) to <25%, and se-
ly correlate with inflammatory markers including serum vere expansion as ≥25% of the normal volume [51]. In a
TNF-α, IL-6, and IL-10 levels in patients with HF [47]. In cohort of 177 patients hospitalized for HF (mixed ejection
a systematic review and meta-analysis including 23 stud- fraction), decongestion strategy guided by admission
ies investigating its role in HF management, serum levels BVA was associated with lower 30-day mortality and re-
of CA125 were found to increase in parallel with decline admission rates compared to propensity-matched con-
in cardiac function from the New York Heart Association trols (2.0 vs. 11.1% and 12.2 vs. 27.7%, respectively; p <
(NYHA) class I/II to III and further from class III to IV. 0.001) [52]. In another study including 26 HF patients, 24
Further, HF patients with higher CA125 level had poorer of whom were hypervolemic at hospital admission (BV
outcomes [48]. In a recent prospective observational +39%), there was only marginal decrease (+30%) in BV at
study including 191 patients admitted with acute HF, discharge despite large reductions in body weight (−6.9
CA125 has demonstrated a positive and independent as- kg) [53]. This observation is in line with previously re-
sociation with the presence of peripheral edema, pleural ported data raising concerns about inadequate deconges-
effusion, and an increased diameter of the inferior vena tion when using conventional monitoring tools.
cava (IVC). On the other hand, NT-proBNP was associ- The utility of BVA is generally limited in critically ill
ated with pleural effusion and IVC diameter but not pe- patients with hemodynamic instability or those undergo-
ripheral edema. Notably, CA125 exhibited a better cor- ing acute volume transitions as the analysis presumes
relation with IVC diameter [49]. These findings have led steady-state conditions. Nevertheless, carefully selected
to the premise that CA125 is a better marker for right patients at increased risk for FO may benefit from this
heart dysfunction and venous congestion whereas NT- technique. In a clinical trial including 100 critically ill sur-
proBNP is more indicative of left-sided filling pressures gical patients, Yu et al. [54] have demonstrated that BVA-
and pulmonary congestion. guided fluid management strategy is associated with im-
proved outcome compared to control group managed ac-
cording to pulmonary artery catheter parameters
Quantitative Blood Volume Analysis (mortality rate 8 vs. 24%, p = 0.03) . As mentioned, BVA
can provide information about albumin transudation
Blood volume analysis (BVA) is based on the indica- rate based on the dilution of tracer over time. In an inter-
tor-dilution technique, in which a known quantity of a esting case series including 4 critically ill patients with
substance (q) is dissolved in a fluid compartment of un- COVID-19, Bakker et al. [55] leveraged this characteristic
4 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
Fig. 2. Principle of blood volume assessment: a dose of albumin from the intravascular to the extravascular space (depicted as the
I-131 tracer is injected intravenously. Once the tracer has fully cir- pink dots moving outside the red vein), its quantity decreases in-
culated in the bloodstream, a series of small blood samples are travascularly implying a higher dilution factor and therefore high-
drawn. The blood volume analyzer automatically calculates pa- er blood volume. Red line represents the regression calculation of
tient’s blood volume by comparing the concentration of undiluted the analyzed draws to time 0 or time of injection, which indicates
tracer prior to injection to the tracer concentration diluted in the the level of true total intravascular blood volume. The red line is
patient blood samples. The human figures represent sequential also a measure of albumin transudation, a measure of capillary
calculated blood volumes at the recommended intervals for draw- permeability. Figure adapted from https://www.daxor.com/how-
ing blood samples after tracer injection. As the tracer transudates bva-100-works/ with kind permission of Daxor Corporation.
to assess capillary permeability . Larger studies are needed reveal alternative causes of dyspnea, coexisting thoracic
to understand how this information can be utilized to ti- diseases, and valvular or pericardial calcification. Notably,
trate therapy. a normal chest radiograph should not be used to exclude
the diagnosis of HF as up to 20% of the patients presenting
with acute HF do not demonstrate any radiographic ab-
Chest Radiography normalities. A supine chest radiograph further limits the
diagnostic utility [56, 57]. Having said that, residual pul-
Chest radiography is the most common modality used monary congestion at hospital discharge assessed by ra-
in the diagnosis of acute HF and FO. Key findings include diographic scoring has shown to predict worse outcome
central vascular congestion, interstitial edema with Kerley outperforming physical assessment, echocardiographic
B-lines, cardiomegaly, and pleural effusions. It may also parameters, and BNP [58]. In our practice, we prefer lung
Fluid Overload Cardiorenal Med 5
DOI: 10.1159/000526902
ultrasonography over chest radiographs to diagnose and or narrow the differential or guide a procedure. Over the
monitor congestion. In addition to being radiation-free, past several years, multi-organ POCUS has evolved as an
ultrasound has better diagnostic accuracy for the detec- adjunct to physical examination in specialties such as
tion of cardiogenic pulmonary edema. For instance, in a emergency medicine, critical care, and nephrology [74,
recent meta-analysis, sensitivity and specificity for lung 75]. We previously proposed the pump-pipes-leaks ap-
ultrasound compared to chest radiography were 91.8% proach to conduct a goal-directed POCUS-assisted he-
versus 76.5% and 92.3% versus 87%, respectively [59]. modynamic evaluation in patients with HF and FO [76].
Pump represents focused cardiac ultrasound (FoCUS),
pipes represent IVC ultrasound and Doppler assessment
Bioimpedance Analysis of venous congestion, and leaks signify extravascular
lung and abdominal fluid. This allows assessment of both
Bioimpedance analysis (BIA) involves application of al- forward flow and effects of elevated cardiac filling pres-
ternating current to the body and measuring changes in im- sures.
pedance/resistance as it relates to changes in volume. It can
be used to quantify total body water, intracellular water, ex- Focused Cardiac Ultrasound
tracellular water, protein, and fat levels. BIA has been suc- In patients presenting with symptoms and signs of FO,
cessfully employed in the assessment of peri-operative fluid a quick subjective assessment or “eyeballing” of the left
depletion, measuring body composition in chronic HF, liver ventricular (LV) size and motion provides a qualitative
disease, and kidney disease [60–63]. In patients undergoing estimate of EF, which is reasonably accurate when per-
maintenance dialysis, there are conflicting data on whether formed by noncardiologists with short training [77]. In
routine BIA-guided dry weight adjustment portends favor- addition, presence or absence of pericardial effusion,
able outcomes. For example, a single-center study showed gross valvular dysfunction, and chamber enlargement
BIA-guided ultrafiltration strategy confers mortality benefit can be evaluated. Volume overload and acute pressure
compared to routine care (hazard ratio [HR] 0.1, p = 0.03) overload are associated with right ventricular (RV) en-
[64]; these findings were not replicated in other clinical trials largement and interventricular septal flattening in dias-
in hemodialysis as well as peritoneal dialysis patients though tole (leading to a D-shaped LV assessed in the parasternal
there was a suggestion toward better FO control [65–67]. It short axis cardiac view), whereas chronic pressure over-
might still benefit a selected subset of these patients with dif- load causes flattening in both systole and diastole [78, 79].
ficult to manage fluid status as FO negatively impacts qual- RV enlargement is often associated with functional tri-
ity of life [68]. In patients with acute HF, BIA reliably reflects cuspid regurgitation, which further exacerbates RV over-
changes in hydration status, correlates with echocardio- load at end-diastole as well as causes increased right atri-
graphic parameters, natriuretic peptide levels, and predicts al pressure (RAP) and central venous congestion [80].
hospital length of stay. However, BIA-guided decongestive IVC ultrasound can be used to estimate RAP. Figure 3
therapy has not shown to be superior compared to standard shows FoCUS images obtained from a patient who pre-
care with respect to outcome [69–72]. In critically ill pa- sented with HF exacerbation and FO. There was near-
tients, the accuracy of BIA as a measure of hydration status complete resolution of the septal flattening and tricuspid
remains unclear at this time [73]. A key limitation of BIA is regurgitation after approximately 14 L fluid removal. Us-
its inability to detect the location of extracellular volume ex- ers trained in Doppler applications can assess stroke vol-
pansion (e.g., pleural effusion vs. pulmonary edema vs. asci- ume at the bedside by measuring LV outflow tract veloc-
tes vs. venous congestion). Further, misinterpretation of the ity time integral. This helps get an idea of the cardiac in-
results can occur if the patient’s body position is not correct, dex and also evaluate fluid responsiveness in selected
or electrodes cannot be appropriately placed due to chest patients, potentially avoiding iatrogenic FO [76]. Fur-
hair, diaphoresis, or skin lesions. thermore, ability to perform Doppler-enhanced FoCUS
allows assessment of LV filling pressures, which can be
used to titrate diuretic therapy in the outpatient setting.
Point-Of-Care Ultrasonography For example, in a study including 1,135 patients with HF
with reduced ejection fraction, the group in which man-
Point-of-care ultrasonography (POCUS) is a limited agement was guided by LV filling pressures and BNP lev-
bedside ultrasound examination performed by the clini- el had a lower incidence of death (HR 0.45, p < 0.0001),
cian to answer focused questions to confirm a diagnosis and death or worsening renal function (HR 0.49, p <
6 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
a b
c d
Fig. 3. Cardiac ultrasound images obtained from a patient with head] on the apical 4-chamber view (c); images at hospital dis-
heart failure exacerbation: at presentation, diastolic interventricu- charge (b–d) demonstrate near-complete resolution of these ab-
lar septal flattening is seen on the parasternal long axis view (a), normalities. RV, right ventricle; LV, left ventricle.
qualitatively moderate to severe tricuspid regurgitation [arrow-
0.0001) compared to standard care group over a median IVC Ultrasound
follow-up of 37.4 months [81]. In critically ill patients, the IVC size and collapsibility are used to estimate RAP
diagnostic utility of FoCUS is well established, particu- and are standard components of comprehensive echo-
larly in the context of undifferentiated hypotension and cardiography. However, the correlation between IVC pa-
acute respiratory failure [82–85]. With respect to prog- rameters and right heart catheterization-derived RAP is
nostication, echocardiographic markers of both LV and modest at best [88–90] and not valid in mechanically
RV dysfunction have shown to be associated with in- ventilated patients [91]. In addition, IVC POCUS is sub-
creased morality in these patients [86, 87]. Currently, ject to numerous technical pitfalls limiting its practical
there are no randomized controlled trials that have exam- utility, especially when interpreted in isolation [24]. Hav-
ined the effect of FoCUS on improving outcomes in crit- ing said that, IVC is a good indicator of fluid tolerance as
ical illness. It is unlikely that such a trial will ever be per- a plethoric IVC almost always indicates elevated RAP in
formed owing to difficulty of defining outcome variables patients with high pretest probability of FO; in other
beyond mortality, the difficulty of recruiting ICU teams words, such patients have elevated right-sided filling
with clinical equipoise, and developing standardized pressures and are intolerant to IVF administration. In
treatment protocols based on FoCUS findings in hetero- patients with HF, an elevated IVC diameter has shown to
geneous groups [82]. be associated with adverse outcomes. For example, in a
Fluid Overload Cardiorenal Med 7
DOI: 10.1159/000526902
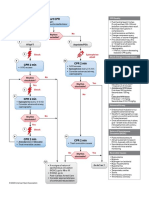
Fig. 4. Venous excess ultrasound (VExUS) grading: when the di- is considered mildly abnormal when the pulsatility is 30–50%, and
ameter of IVC is >2 cm, three grades of congestion are defined severely abnormal when it is ≥50%. Asterisks represent points of
based on the severity of abnormalities on hepatic, portal, and renal pulsatility measurement. Renal parenchymal vein Doppler is mild-
parenchymal venous Doppler. Hepatic vein Doppler is considered ly abnormal when it is pulsatile with distinct S, D components, and
mildly abnormal when the systolic (S) wave is smaller than the severely abnormal when it is monophasic with D-only pattern. Fig-
diastolic (D) wave, but still below the baseline; it is considered se- ure adapted from NephroPOCUS.com with permission.
verely abnormal when the S-wave is reversed. Portal vein Doppler
study involving 80 patients hospitalized for acute HF, an pressure (RAP) impairs perfusion and leads to organ
admission IVC diameter ≥1.9 cm was associated with a dysfunction (e.g., AKI). A protocol to quantify system-
higher mortality at 90 days (25.4 vs. 3.4%; p = 0.009) and ic venous congestion called venous excess ultrasound
180 days (29.3 vs. 3.4%; p = 0.003) [92]. Similarly, in a (VExUS) has been recently validated in cardiac surgery
large cohort of HF patients (N = 355) managed in the patients and is rapidly gaining acceptance in various
ambulatory care clinic, every 0.5 cm increase in the IVC clinical settings including HF and critical illness [94].
diameter was associated with a 38% increase in risk of HF In a nutshell, VExUS involves assessing flow patterns in
admission (risk ratio [RR] 1.38, p < 0.01). The risk of HF hepatic, portal, and renal parenchymal veins and as-
admission increased proportionately in those with IVC signing a score based on the severity of flow alteration.
diameter 2–2.49 cm (RR 1.79, p < 0.01) versus ≥2.5 cm Figure 4 depicts the VExUS scoring system, and Figure
(RR 2.39, p < 0.01) compared to patients with diameter 5 illustrates waveforms obtained from a patient with se-
<2 cm [93]. vere congestion. Notably, neither IVC nor components
of VExUS can differentiate between pressure overload
Venous Congestion Assessment by Doppler Ultrasound (e.g., pulmonary hypertension) and volume overload,
Doppler evaluation of the systemic veins allows us to and hence, the findings must be interpreted in the ap-
gauge the downstream effects of elevated RAP. This is propriate clinical context. Regardless of the cause, a
important as the organ perfusion depends on both in- high VExUS score still indicates end organ congestion.
flow and outflow pressures; increase in the outflow In the original study [94], presence of severe flow ab-
8 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
Fig. 5. Left panel: Plethoric IVC (arrowhead), diastolic (D)-only pattern on hepatic vein Doppler, pulsatile portal
vein Doppler, and D-only or monophasic renal parenchymal vein Doppler obtained from a patient with fluid
overload and severe venous congestion; right panel: normal-appearing IVC with <2 cm diameter (arrowhead)
and normal venous waveforms.
normalities in two or more of the abovementioned diovascular morbidity and death [97, 98]. A key advan-
veins together with a dilated IVC (≥2 cm) has shown to tage of these Doppler waveforms is that they are dy-
predict the risk of AKI (HR 3.69, p = 0.001), outper- namic and allow monitoring the response to deconges-
forming isolated central venous pressure measurement. tive therapy in real time [99–105]. Clinical trials are in
Several other studies demonstrated prognostic signifi- progress to study the effect of waveform-guided thera-
cance of individual components of VExUS. For exam- py on patient outcomes [24].
ple, in another cardiac surgery cohort, portal vein pul-
satility and altered intra-renal venous flow were associ- Lung POCUS
ated with AKI (HR 2.09, p = 0.02, and HR 2.81, p = Lung POCUS can detect extravascular lung water be-
0.003, respectively) [95]. A prospective observational fore the onset of symptoms, even outperforming chest
study evaluated the prognostic utility of VExUS in 114 radiography in diagnosing cardiogenic pulmonary ede-
patients admitted to medical ICU [96]; abnormal he- ma [59, 106]. In normal state, the lung tissue is not vi-
patic vein Doppler flow has shown to predict 30-day sualized on ultrasound as the underlying air scatters the
risk of kidney events with an odds ratio of 4; however, ultrasound beam. Instead, a bright shimmering pleural
portal and renal parenchymal venous abnormalities did line followed by equidistant hyperechoic horizontal ar-
not share this association. The heterogenous nature of tifacts called the A-lines is seen. B-lines, which are ver-
AKI in an unselected cohort of critically ill patients tical hyperechoic artifacts, occur when the air content
could have contributed to the discrepancy. In the con- in the lung decreases due to interstitial thickening (typ-
text of HF, flow alterations in renal parenchymal veins ically from fluid). The number of B-lines correlates with
have shown to confer worse prognosis in terms of car- the degree of pulmonary edema and dynamically re-
Fluid Overload Cardiorenal Med 9
DOI: 10.1159/000526902
a b c
Fig. 6. Common lung ultrasound findings: A-lines (arrows; a); B-lines (arrows; b); right pleural effusion (asterisk;
c). IVC, inferior vena cava.
duces with decongestive therapy [107]. Caution must Other POCUS Applications
be exercised as B-lines are not specific to cardiogenic In patients with FO, POCUS helps identify ascites,
pulmonary edema and can be seen in conditions such bowel wall edema, and ileus [76]. POCUS can also aid in
as acute respiratory distress syndrome, pneumonia, the assessment of JVP in cases where the vein is difficult
lung fibrosis, and contusion. A pleural effusion appears to visualize. JVP can be estimated by measuring the height
as an anechoic area above the diaphragm, around the of the collapse point (analogous to highest point of ve-
atelectatic lung (Fig. 6). Prognostic significance of lung nous pulsation in the inspection method) or change in the
ultrasound-detected pulmonary congestion has been vein diameter with respiration/head positioning or as-
well established in multiple clinical settings including sessing change in the cross-sectional area with Valsalva
HF, hemodialysis, and critical illness [108]. For exam- maneuver in spontaneously breathing patients [117, 118].
ple, in a cohort of 185 HF patients who underwent lung Jugular vein POCUS has shown to correlate well with
POCUS in the outpatient clinic, those who had ≥3 B- congestion parameters as well as mortality in patients
lines on an 8-zone scanning protocol had 4-fold higher with HF [119, 120]. However, it is prone to misinterpreta-
risk of the primary outcome, i.e., a composite of HF tion due to inadvertent excess transducer pressure, inap-
hospitalization or all-cause mortality (adjusted HR propriate patient positioning, restricted access to the neck
4.08, p < 0.001) [109]. Notably, auscultation was normal because of the presence of catheters, tracheostomy col-
in 81% of these patients, highlighting the poor sensitiv- lars, braces, etc. Requirement of additional instruments
ity of conventional physical examination. Likewise, in a such as a ruler and a card to accurately measure the height
cohort of 349 patients admitted for acute HF, the risk of the collapse point is another limitation, especially in
of HF hospitalization or all-cause mortality was signifi- the acute care settings [121, 122].
cantly higher in patients with a greater number of B-
lines at discharge (HR 3.3 at 60 days, p = 0.002; 2.94 at Remote Pulmonary Pressure Monitoring
90 days, p = 0.003; 2.01 at 180 days, p = 0.021) [110]. In Wireless implantable hemodynamic monitoring sys-
patients with end-stage kidney disease undergoing he- tems (e.g., CardioMEMS HF System [Abbott Medical,
modialysis, those with severe congestion, defined as Inc., Abbott Park, IL, USA]) allow remote monitoring of
>60 B-lines on a 28-zone lung POCUS, had a 4.2-fold the pulmonary artery pressures and titrate decongestive
risk of death and 3.2-fold risk of cardiac events adjusted therapy. In a prospective multi-center study, ambulatory
for NYHA class and other risk factors [111]. While lung patients managed using CardioMEMS had a 39% reduc-
POCUS-guided therapy has not shown to have mortal- tion in HF-related hospitalization compared with the
ity benefit, favorable outcomes have been demonstrated control group (HR 0.64, p < 0.0001) during a mean fol-
in terms of reduced hospital admissions in HF patients low-up of 15 months [123]. Due to its partially invasive
[112, 113]; improved ambulatory blood pressure and nature (right heart catheterization is needed to implant
LV filling pressures in hemodialysis patients [114, 115]; the sensor) and the need for trained personnel to manage
and improved lung aeration scores in critically ill pa- therapy based on the readings, patients who might ben-
tients on mechanical ventilation [116]. efit from this modality must be carefully selected. Fur-
10 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
thermore, pressure-based assessment of congestion in Conflict of Interest Statement
ambulatory HF patients does not accurately represent in-
Amir Kazory received consultancy fee from Baxter Inc. The
travascular volume and diuretic titration may not always other authors have no conflicts of interest to declare.
be the appropriate therapeutic choice [124].
Funding Sources
Conclusions and Future Directions
No specific financial support was obtained for preparation of
It is well recognized that FO has detrimental effects on this article.
organ function and portends worse patient outcomes.
While several bedside tools and techniques are available
for objective assessment of fluid status, each suffers from Author Contributions
inherent limitations. Physicians must be aware of these
Abhilash Koratala drafted the initial version of the manuscript.
limitations and adopt a multiparametric approach to for- Amir Kazory and Claudio Ronco reviewed and revised the manu-
mulate individualized management plan for their pa- script for critical intellectual content. Abhilash Koratala, Claudio
tients. Such an approach eventually needs standardiza- Ronco, and Amir Kazory have approved the final version for sub-
tion, independent validation with a randomized con- mission.
trolled trial design to demonstrate precision, and
reproducibility of the findings as well as impact on the
measurable outcomes.
References
1 Gheorghiade M, Shin DD, Thomas TO, Bran- 7 Cardoso FS, Pereira R, Laranjo A, Gamelas V, 14 Veiga D, Luis C, Parente D, Fernandes V, Botel-
dimarte F, Fonarow GC, Abraham WT. Con- Bagulho L, Germano N, et al. Positive fluid ho M, Santos P, et al. Postoperative delirium in
gestion is an important diagnostic and thera- balance was associated with mortality in pa- intensive care patients: risk factors and out-
peutic target in heart failure. Rev Cardiovasc tients with acute-on-chronic liver failure: a come. Rev Bras Anestesiol. 2012;62(4):469–83.
Med. 2006;7(Suppl 1):S12–24. cohort study. J Crit Care. 2021;63:238–42. 15 Scheuermann K, Thiel C, Thiel K, Klingert W,
2 Binanay C, Califf RM, Hasselblad V, 8 Meyhoff TS, Hjortrup PB, Wetterslev J, Siv- Hawerkamp E, Scheppach J, et al. Correlation
O’Connor CM, Shah MR, Sopko G, et al. Eval- apalan P, Laake JH, Cronhjort M, et al. Re- of the intracranial pressure to the central ve-
uation study of congestive heart failure and striction of intravenous fluid in ICU patients nous pressure in the late phase of acute liver
pulmonary artery catheterization effective- with septic shock. N Engl J Med. 2022;386(26): failure in a porcine model. Acta Neurochir
ness: the ESCAPE trial. JAMA. 2005;294(13): 2459–70. Suppl. 2012;114:387–91.
1625–33. 9 O’Connor ME, Prowle JR. Fluid overload. 16 Gieling RG, Ruijter JM, Maas AAW, Van Den
3 Lucas C, Johnson W, Hamilton MA, Fonarow Crit Care Clin. 2015;31(4):803–21. Bergh Weerman MA, Dingemans KP, ten
GC, Woo MA, Flavell CM, et al. Freedom 10 Beaubien-Souligny W, Bouchard J, Desjar- Kate FJW, et al. Hepatic response to right ven-
from congestion predicts good survival de- dins G, Lamarche Y, Liszkowski M, Robillard tricular pressure overload. Gastroenterology.
spite previous class IV symptoms of heart fail- P, et al. Extracardiac signs of fluid overload in 2004;127(4):1210–21.
ure. Am Heart J. 2000;140(6):840–7. the critically ill cardiac patient: a focused eval- 17 Lobo DN. Fluid, electrolytes and nutrition:
4 O’Connor CM, Stough WG, Gallup DS, Has- uation using bedside ultrasound. Can J Car- physiological and clinical aspects. Proc Nutr
selblad V, Gheorghiade M. Demographics, diol. 2017;33(1):88–100. Soc. 2004;63(3):453–66.
clinical characteristics, and outcomes of pa- 11 National Heart, Lung, and Blood Institute 18 Desai KV, Laine GA, Stewart RH, Cox CS Jr,
tients hospitalized for decompensated heart Acute Respiratory Distress Syndrome ARDS Quick CM, Allen SJ, et al. Mechanics of the
failure: observations from the IMPACT-HF Clinical Trials Network; Wiedemann HP, left ventricular myocardial interstitium: ef-
registry. J Card Fail. 2005;11(3):200–5. Wheeler AP, Bernard GR, Thompson BT, fects of acute and chronic myocardial edema.
5 Rubio-Gracia J, Demissei BG, Ter Maaten JM, Hayden D, et al. Comparison of two fluid- Am J Physiol Heart Circ Physiol. 2008;294(6):
Cleland JG, O’Connor CM, Metra M, et al. management strategies in acute lung injury. N H2428–34.
Prevalence, predictors and clinical outcome of Engl J Med. 2006;354(24):2564–75. 19 Boyle A, Maurer MS, Sobotka PA. Myocellu-
residual congestion in acute decompensated 12 Sakka SG, Klein M, Reinhart K, Meier-Hell- lar and interstitial edema and circulating vol-
heart failure. Int J Cardiol. 2018;258:185–91. mann A. Prognostic value of extravascular ume expansion as a cause of morbidity and
6 Malbrain MLNG, Marik PE, Witters I, Corde- lung water in critically ill patients. Chest. mortality in heart failure. J Card Fail. 2007;
mans C, Kirkpatrick AW, Roberts DJ, et al. 2002;122(6):2080–6. 13(2):133–6.
Fluid overload, de-resuscitation, and out- 13 Warrillow SJ, Weinberg L, Parker F, Calzavac- 20 Husain-Syed F, Gröne HJ, Assmus B, Bauer P,
comes in critically ill or injured patients: a sys- ca P, Licari E, Aly A, et al. Perioperative fluid Gall H, Seeger W, et al. Congestive nephropa-
tematic review with suggestions for clinical prescription, complications and outcomes in thy: a neglected entity? Proposal for diagnos-
practice. Anaesthesiol Intensive Ther. 2014; major elective open gastrointestinal surgery. tic criteria and future perspectives. ESC Heart
46(5):361–80. Anaesth Intensive Care. 2010;38(2):259–65. Fail. 2021 Feb;8(1):183–203.
Fluid Overload Cardiorenal Med 11
DOI: 10.1159/000526902
21 Mullens W, Abrahams Z, Francis GS, Sokos 34 Felker GM, Anstrom KJ, Adams KF, Ezekow- 47 Huang F, Chen J, Liu Y, Zhang K, Wang J,
G, Taylor DO, Starling RC, et al. Importance itz JA, Fiuzat M, Houston-Miller N, et al. Ef- Huang H. New mechanism of elevated CA125
of venous congestion for worsening of renal fect of natriuretic peptide-guided therapy on in heart failure: the mechanical stress and in-
function in advanced decompensated heart hospitalization or cardiovascular mortality in flammatory stimuli initiate CA125 synthesis.
failure. J Am Coll Cardiol. 2009;53(7):589–96. high-risk patients with heart failure and re- Med Hypotheses. 2012;79(3):381–3.
22 Brandstrup B, Tønnesen H, Beier-Holgersen duced ejection fraction: a randomized clinical 48 Zhuang J, Faggiano P, Li Q, Pradelli D, Med
R, Hjortsø E, Ørding H, Lindorff-Larsen K, et trial. JAMA. 2017;318(8):713–20. V, Peng W, et al. Insights into the clinical im-
al. Effects of intravenous fluid restriction on 35 Shah SJ. BNP: Biomarker Not Perfect in heart plications of carbohydrate antigen 125 as a
postoperative complications: comparison of failure with preserved ejection fraction. Eur biomarker of heart failure: a meta-analysis
two perioperative fluid regimens: a random- Heart J. 2022;43(20):1952–4. and systematic review of published studies. J
ized assessor-blinded multicenter trial. Ann 36 Verbrugge FH, Omote K, Reddy YNV, Sori- Cardiovasc Med. 2014;15(12):864–72.
Surg. 2003;238(5):641–8. machi H, Obokata M, Borlaug BA. Heart fail- 49 Llàcer P, Gallardo MÁ, Palau P, Moreno MC,
23 Kattan E, Castro R, Miralles-Aguiar F, ure with preserved ejection fraction in pa- Castillo C, Fernández C, et al. Comparison
Hernández G, Rola P. The emerging concept tients with normal natriuretic peptide levels is between CA125 and NT-proBNP for evaluat-
of fluid tolerance: a position paper. J Crit associated with increased morbidity and mor- ing congestion in acute heart failure. Med
Care. 2022;71:154070. tality. Eur Heart J. 2022;43(20):1941–51. Clin. 2021;156(12):589–94.
24 Koratala A, Reisinger N. Venous excess 37 Wagner S, Cohn K. Heart failure. A proposed 50 Daxor BVA-100, principle of blood volume
Doppler ultrasound for the nephrologist: definition and classification. Arch Intern measurement. Available from: https: //www.
pearls and pitfalls. Kidney Med. 2022 May; Med. 1977;137(5):675–8. daxor.com/how-bva-100-works/ (Last ac-
4(7):100482. 38 Adamo L, Nassif ME, Novak E, LaRue SJ, cessed April 7, 2022).
25 Shah MR, Hasselblad V, Stevenson LW, Bi- Mann DL. Prevalence of lactic acidaemia in 51 Miller WL. Assessment and management of vol-
nanay C, O’Connor CM, Sopko G, et al. Im- patients with advanced heart failure and de- ume overload and congestion in chronic heart
pact of the pulmonary artery catheter in criti- pressed cardiac output. Eur J Heart Fail. 2017; failure: can measuring blood volume provide
cally ill patients: meta-analysis of randomized 19(8):1027–33. new insights? Kidney Dis. 2017;2(4):164–9.
clinical trials. JAMA. 2005 Oct 5; 294(13): 39 Zymliński R, Biegus J, Sokolski M, Siwołowski 52 Strobeck JE, Feldschuh J, Miller WL. Heart
1664–70. P, Nawrocka-Millward S, Todd J, et al. In- failure outcomes with volume-guided man-
26 Stevenson LW, Perloff JK. The limited reli- creased blood lactate is prevalent and identi- agement. JACC Heart Fail. 2018;6(11):940–8.
ability of physical signs for estimating hemo- fies poor prognosis in patients with acute 53 Miller WL, Mullan BP. Understanding the
dynamics in chronic heart failure. JAMA. heart failure without overt peripheral hypo- heterogeneity in volume overload and fluid
1989;261(6):884–8. perfusion. Eur J Heart Fail. 2018;20(6):1011– distribution in decompensated heart failure is
27 Wang CS, FitzGerald JM, Schulzer M, Mak E, 8. key to optimal volume management: role for
Ayas NT. Does this dyspneic patient in the 40 Hernandez G, Bellomo R, Bakker J. The ten blood volume quantitation. JACC Heart Fail.
emergency department have congestive heart pitfalls of lactate clearance in sepsis. Intensive 2014;2(3):298–305.
failure? JAMA. 2005;294(15):1944–56. Care Med. 2019;45(1):82–5. 54 Yu M, Pei K, Moran S, Edwards KD, Domin-
28 Koratala A, Kazory A. Natriuretic peptides as 41 Hernández G, Ospina-Tascón GA, Damiani go S, Steinemann S, et al. A prospective ran-
biomarkers for congestive states: the cardio- LP, Estenssoro E, Dubin A, Hurtado J, et al. domized trial using blood volume analysis in
renal divergence. Dis Markers. 2017; 2017: Effect of a resuscitation strategy targeting pe- addition to pulmonary artery catheter, com-
1454986. ripheral perfusion status vs serum lactate lev- pared with pulmonary artery catheter alone,
29 Liquori ME, Christenson RH, Collinson PO, els on 28-Day mortality among patients with to guide shock resuscitation in critically ill
Defilippi CR. Cardiac biomarkers in heart septic shock: the ANDROMEDA-SHOCK surgical patients. Shock. 2011;35(3):220–8.
failure. Clin Biochem. 2014;47(6):327–37. randomized clinical trial. JAMA. 2019;321(7): 55 Bakker J, Horowitz JM, Hagedorn J, Kozloff
30 Maisel AS, Krishnaswamy P, Nowak RM, Mc- 654–64. S, Kaufman D, Castro R. Blood volume and
Cord J, Hollander JE, Duc P, et al. Rapid mea- 42 Boyle A, Sobotka PA. Redefining the thera- albumin transudation in critically ill CO-
surement of B-type natriuretic peptide in the peutic objective in decompensated heart fail- VID-19 patients. Crit Care. 2021;25(1):269.
emergency diagnosis of heart failure. N Engl J ure: hemoconcentration as a surrogate for 56 Yancy CW, Jessup M, Bozkurt B, Butler J,
Med. 2002;347(3):161–7. plasma refill rate. J Card Fail. 2006;12(4):247– Casey DE Jr, Drazner MH, et al. 2013 ACCF/
31 Latini R, Masson S, Wong M, Barlera S, Car- 9. AHA guideline for the management of heart
retta E, Staszewsky L, et al. Incremental prog- 43 Fujita T, Inomata T, Yazaki M, Iida Y, Kaida failure: a report of the American College of
nostic value of changes in B-type natriuretic T, Ikeda Y, et al. Hemodilution after initial Cardiology Foundation/American Heart As-
peptide in heart failure. Am J Med. 2006; treatment in patients with acute decompen- sociation Task Force on practice guidelines. J
119(1):70e23–30. sated heart failure. Int Heart J. 2018; 59(3): Am Coll Cardiol. 2013;62(16):e147–239.
32 Papanikolaou J, Makris D, Mpaka M, Palli E, 573–9. 57 Long B, Koyfman A, Gottlieb M. Diagnosis of
Zygoulis P, Zakynthinos E. New insights into 44 van der Meer P, Postmus D, Ponikowski P, acute heart failure in the emergency depart-
the mechanisms involved in B-type natriuret- Cleland JG, O’Connor CM, Cotter G, et al. ment: an evidence-based review. West J
ic peptide elevation and its prognostic value The predictive value of short-term changes in Emerg Med. 2019;20(6):875–84.
in septic patients. Crit Care. 2014;18(3):R94. hemoglobin concentration in patients pre- 58 Kobayashi M, Watanabe M, Coiro S, Bercker
33 Stienen S, Salah K, Moons AH, Bakx AL, van senting with acute decompensated heart fail- M, Paku Y, Iwasaki Y, et al. Mid-term prog-
Pol P, Kortz RAM, et al. NT-proBNP (N-Ter- ure. J Am Coll Cardiol. 2013;61(19):1973–81. nostic impact of residual pulmonary conges-
minal pro-B-type natriuretic peptide)-guided 45 Sharma R, Francis DP, Pitt B, Poole-Wilson tion assessed by radiographic scoring in pa-
therapy in acute decompensated heart failure: PA, Coats AJS, Anker SD. Haemoglobin pre- tients admitted for worsening heart failure.
PRIMA II randomized controlled trial (Can dicts survival in patients with chronic heart Int J Cardiol. 2019;289:91–8.
NT-ProBNP-guided therapy during hospital failure: a substudy of the ELITE II trial. Eur 59 Chiu L, Jairam MP, Chow R, Chiu N, Shen M,
admission for acute decompensated heart Heart J. 2004;25(12):1021–8. Alhassan A, et al. Meta-analysis of point-of-
failure reduce mortality and readmissions?). 46 Miller WL. Fluid volume overload and con- care lung ultrasonography versus chest radi-
Circulation. 2018;137(16):1671–83. gestion in heart failure: time to reconsider ography in adults with symptoms of acute de-
pathophysiology and how volume is assessed. compensated heart failure. Am J Cardiol.
Circ Heart Fail. 2016;9(8):e002922. 2022;174:89–95.
12 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
60 Ackland GL, Singh-Ranger D, Fox S, McClas- 73 Madsen JM, Wichmann S, Bestle MH, Itenov 87 Gajanana D, Seetha Rammohan H, Alli O,
key B, Down JF, Farrar D, et al. Assessment of TS. Bioimpedance as a measure of fluid status Romero-Corral A, Purushottam B, Ponamgi
preoperative fluid depletion using bioimped- in critically ill patients: a systematic review. S, et al. Tricuspid annular plane systolic ex-
ance analysis. Br J Anaesth. 2004;92(1):134–6. Acta Anaesthesiol Scand. 2021;65(9):1155–67. cursion and its association with mortality in
61 Uszko-Lencer NHMK, Bothmer F, van Pol 74 Koratala A, Reisinger N. POCUS for nephrol- critically Ill patients. Echocardiography.
PEJ, Schols AMWJ. Measuring body compo- ogists: basic principles and a general ap- 2015;32(8):1222–7.
sition in chronic heart failure: a comparison proach. Kidney360. 2021;2(10):1660–8. 88 Magnino C, Omedè P, Avenatti E, Presutti D,
of methods. Eur J Heart Fail. 2006; 8(2): 208– 75 Koratala A, Olaoye OA, Bhasin-Chhabra B, Iannaccone A, Chiarlo M, et al. Inaccuracy of
14. Kazory A. A blueprint for an integrated point- right atrial pressure estimates through infe-
62 Panella C, Guglielmi FW, Mastronuzzi T, of-care ultrasound curriculum for nephrolo- rior vena cava indices. Am J Cardiol. 2017;
Francavilla A. Whole-body and segmental gy trainees. Kidney360. 2021;2(10):1669–76. 120(9):1667–73.
bioelectrical parameters in chronic liver dis- 76 Koratala A, Kazory A. Point of care ultraso- 89 Brennan JM, Blair JE, Goonewardena S,
ease: effect of gender and disease stages. Hep- nography for objective assessment of heart Ronan A, Shah D, Vasaiwala S, et al. Reap-
atology. 1995;21(2):352–8. failure: integration of cardiac, vascular, and praisal of the use of inferior vena cava for es-
63 Piccoli A; Italian CAPD-BIA Study Group. extravascular determinants of volume status. timating right atrial pressure. J Am Soc Echo-
Bioelectric impedance vector distribution in Cardiorenal Med. 2021;11(1):5–17. cardiogr. 2007;20(7):857–61.
peritoneal dialysis patients with different hy- 77 Moore CL, Rose GA, Tayal VS, Sullivan DM, 90 Seo Y, Iida N, Yamamoto M, Machino-Oht-
dration status. Kidney Int. 2004; 65(3): 1050– Arrowood JA, Kline JA. Determination of left suka T, Ishizu T, Aonuma K. Estimation of
63. ventricular function by emergency physician central venous pressure using the ratio of
64 Onofriescu M, Hogas S, Voroneanu L, Apetrii echocardiography of hypotensive patients. short to long diameter from cross-sectional
M, Nistor I, Kanbay M, et al. Bioimpedance- Acad Emerg Med. 2002;9(3):186–93. images of the inferior vena cava. J Am Soc
guided fluid management in maintenance he- 78 Kingma I, Tyberg JV, Smith ER. Effects of di- Echocardiogr. 2017;30(5):461–7.
modialysis: a pilot randomized controlled tri- astolic transseptal pressure gradient on ven- 91 Jue J, Chung W, Schiller NB. Does inferior
al. Am J Kidney Dis. 2014;64(1):111–8. tricular septal position and motion. Circula- vena cava size predict right atrial pressures in
65 Siriopol D, Onofriescu M, Voroneanu L, tion. 1983;68(6):1304–14. patients receiving mechanical ventilation? J
Apetrii M, Nistor I, Hogas S, et al. Dry weight 79 Denault AY, Langevin S, Lessard MR, Cour- Am Soc Echocardiogr. 1992;5(6):613–9.
assessment by combined ultrasound and bio- val JF, Desjardins G. Transthoracic echocar- 92 Cubo-Romano P, Torres-Macho J, Soni NJ,
impedance monitoring in low cardiovascular diographic evaluation of the heart and great Reyes LF, Rodríguez-Almodóvar A, Fernán-
risk hemodialysis patients: a randomized con- vessels. Can J Anaesth. 2018;65(4):449–72. dez-Alonso JM, et al. Admission inferior vena
trolled trial. Int Urol Nephrol. 2017; 49(1): 80 Konstam MA, Kiernan MS, Bernstein D, Boz- cava measurements are associated with mor-
143–53. kurt B, Jacob M, Kapur NK, et al. Evaluation tality after hospitalization for acute decom-
66 Tian N, Yang X, Guo Q, Zhou Q, Yi C, Lin J, and management of right-sided heart failure: pensated heart failure. J Hosp Med. 2016;
et al. Bioimpedance guided fluid management a scientific statement from the American 11(11):778–84.
in peritoneal dialysis: a randomized con- heart association. Circulation. 2018; 137(20): 93 Khandwalla RM, Birkeland KT, Zimmer R,
trolled trial. Clin J Am Soc Nephrol. 2020; e578–622. Henry TD, Nazarian R, Sudan M, et al. Use-
15(5):685–94. 81 Simioniuc A, Carluccio E, Ghio S, Rossi A, Bi- fulness of serial measurements of inferior
67 Yoon HE, Kwon YJ, Shin SJ, Lee SY, Lee S, agioli P, Reboldi G, et al. Echo and natriuretic vena cava diameter by VscanTM to identify
Kim SH, et al. Bioimpedance spectroscopy- peptide guided therapy improves outcome patients with heart failure at high risk of hos-
guided fluid management in peritoneal dialy- and reduces worsening renal function in sys- pitalization. Am J Cardiol. 2017; 119(10):
sis patients with residual kidney function: a tolic heart failure: an observational study of 1631–6.
randomized controlled trial. Nephrology. 1,137 outpatients. Int J Cardiol. 2016; 224: 94 Beaubien-Souligny W, Rola P, Haycock K,
2019;24(12):1279–89. 416–23. Bouchard J, Lamarche Y, Spiegel R, et al.
68 Yoon HE, Kwon YJ, Song HC, Kim JK, Song 82 Singh K, Mayo P. Critical care echocardiogra- Quantifying systemic congestion with point-
YR, Shin SJ, et al. Overhydration negatively af- phy and outcomes in the critically ill. Curr of-care ultrasound: development of the ve-
fects quality of life in peritoneal dialysis pa- Opin Crit Care. 2018;24(4):316–21. nous excess ultrasound grading system. Ul-
tients: evidence from a prospective observa- 83 Laursen CB, Sloth E, Lambrechtsen J, Lassen trasound J. 2020;12(1):16.
tional study. Int J Med Sci. 2016;13(9):686–95. AT, Madsen PH, Henriksen DP, et al. Focused 95 Beaubien-Souligny W, Benkreira A, Robillard
69 Massari F, Scicchitano P, Ciccone MM, Cald- sonography of the heart, lungs, and deep veins P, Bouabdallaoui N, Chassé M, Desjardins G,
arola P, Aspromonte N, Iacoviello M, et al. identifies missed life-threatening conditions et al. Alterations in portal vein flow and intra-
Bioimpedance vector analysis predicts hospi- in admitted patients with acute respiratory renal venous flow are associated with acute
tal length of stay in acute heart failure. Nutri- symptoms. Chest. 2013;144(6):1868–75. kidney injury after cardiac surgery: a prospec-
tion. 2019;61:56–60. 84 Silva S, Biendel C, Ruiz J, Olivier M, Bataille tive observational cohort study. J Am Heart
70 Génot N, Mewton N, Bresson D, Zouaghi O, B, Geeraerts T, et al. Usefulness of cardiotho- Assoc. 2018;7(19):e009961.
Francois L, Delwarde B, et al. Bioelectrical im- racic chest ultrasound in the management of 96 Spiegel R, Teeter W, Sullivan S, Tupchong K,
pedance analysis for heart failure diagnosis in acute respiratory failure in critical care prac- Mohammed N, Sutherland M, et al. The use
the ED. Am J Emerg Med. 2015;33(8):1025–9. tice. Chest. 2013;144(3):859–65. of venous Doppler to predict adverse kidney
71 van Veldhuisen DJ, Braunschweig F, Con- 85 Vignon P, Begot E, Mari A, Silva S, Chimot L, events in a general ICU cohort. Crit Care.
raads V, Ford I, Cowie MR, Jondeau G, et al. Delour P, et al. Hemodynamic assessment of 2020;24(1):615.
Intrathoracic impedance monitoring, audible patients with septic shock using transpulmo- 97 Iida N, Seo Y, Sai S, Machino-Ohtsuka T, Ya-
patient alerts, and outcome in patients with nary thermodilution and critical care echo- mamoto M, Ishizu T, et al. Clinical implica-
heart failure. Circulation. 2011; 124(16): cardiography: a comparative study. Chest. tions of intrarenal hemodynamic evaluation
1719–26. 2018;153(1):55–64. by Doppler ultrasonography in heart failure.
72 De Ieso F, Mutke MR, Brasier NK, Raichle CJ, 86 Sanfilippo F, Corredor C, Fletcher N, Landes- JACC Heart Fail. 2016;4(8):674–82.
Keller B, Sucker C, et al. Body composition berg G, Benedetto U, Foex P, et al. Diastolic
analysis in patients with acute heart failure: dysfunction and mortality in septic patients:
the scale heart failure trial. ESC Heart Fail. a systematic review and meta-analysis. Inten-
2021;8(6):4593–606. sive Care Med. 2015 Jun;41(6):1004–13.
Fluid Overload Cardiorenal Med 13
DOI: 10.1159/000526902
98 Ohara H, Yoshihisa A, Horikoshi Y, Ishi- 108 Reisinger N, Koratala A. Quantitative lung 116 Mojoli F, Bouhemad B, Mongodi S, Lichten-
bashi S, Matsuda M, Yamadera Y, et al. Re- ultrasonography for the nephrologist: appli- stein D. Lung ultrasound for critically ill pa-
nal venous stasis index reflects renal conges- cations in dialysis and heart failure. Kid- tients. Am J Respir Crit Care Med. 2019;
tion and predicts adverse outcomes in pa- ney360. 2022;3(1):176–84. 199(6):701–14.
tients with heart failure. Front Cardiovasc 109 Platz E, Lewis EF, Uno H, Peck J, Pivetta E, 117 Hilbert T, Ellerkmann RK, Klaschik S,
Med. 2022;9:772466. Merz AA, et al. Detection and prognostic Putensen C, Thudium M. The use of inter-
99 Mahmud S, Koratala A. Assessment of ve- value of pulmonary congestion by lung ul- nal jugular vein ultrasonography to antici-
nous congestion by Doppler ultrasound: a trasound in ambulatory heart failure pa- pate low or high central venous pressure
valuable bedside diagnostic tool for the tients. Eur Heart J. 2016;37(15):1244–51. during mechanical ventilation. J Emerg
new-age nephrologist. CEN Case Rep. 2021; 110 Platz E, Campbell RT, Claggett B, Lewis EF, Med. 2016;50(4):581–7.
10(1):153–5. Groarke JD, Docherty KF, et al. Lung ultra- 118 Simon MA, Kliner DE, Girod JP, Moguil-
100 Samant S, Koratala A. Point-of-care Dopp- sound in acute heart failure: prevalence of lansky D, Villanueva FS, Pacella JJ. Detec-
ler ultrasound in the management of hypo- pulmonary congestion and short- and long- tion of elevated right atrial pressure using a
natremia: another string to nephrologists’ term outcomes. JACC Heart Fail. 2019; simple bedside ultrasound measure. Am
Bow. Clin Case Rep. 2021;9(8):e04687. 7(10):849–58. Heart J. 2010;159(3):421–7.
101 Bajaj D, Koratala A. Utility of portal venous 111 Zoccali C, Torino C, Tripepi R, Tripepi G, 119 Pellicori P, Kallvikbacka-Bennett A, Dier-
Doppler in the assessment of fluid status in D’Arrigo G, Postorino M, et al. Pulmonary ckx R, Zhang J, Putzu P, Cuthbert J, et al.
end-stage kidney disease: think beyond IVC congestion predicts cardiac events and mor- Prognostic significance of ultrasound-as-
ultrasound. CEN Case Rep. 2022; 11(2): tality in ESRD. J Am Soc Nephrol. 2013; sessed jugular vein distensibility in heart
285–7. 24(4):639–46. failure. Heart. 2015;101(14):1149–58.
102 Koratala A, Sturgill D. Point-of-care venous 112 Rivas-Lasarte M, Álvarez-García J, Fernán- 120 Pellicori P, Kallvikbacka-Bennett A, Zhang
Doppler ultrasound in the management of dez-Martínez J, Maestro A, López-López L, J, Khaleva O, Warden J, Clark AL, et al. Re-
heart failure and hyponatremia. Clin Solé-González E, et al. Lung ultrasound- visiting a classical clinical sign: jugular ve-
Nephrol. 2021;96(1):63–6. guided treatment in ambulatory patients nous ultrasound. Int J Cardiol. 2014 Jan 1;
103 Koratala A. Utilizing point-of-care ultra- with heart failure: a randomized controlled 170(3):364–70.
sound in the cardiorenal clinic to enhance clinical trial (LUS-HF study). Eur J Heart 121 Mondal S, Mondal H, Das D, Alam N, Saha
patient care. J Bras Nefrol. 2021 Jan–Mar; Fail. 2019;21(12):1605–13. K. Reliability of a jugular venous pressure
43(1):135–6. 113 Marini C, Fragasso G, Italia L, Sisakian H, scale in cardiovascular clinical examination.
104 Argaiz ER, Koratala A, Reisinger N. Com- Tufaro V, Ingallina G, et al. Lung ultra- J Clin Prev Cardiol. 2020;9(2):61–6.
prehensive assessment of fluid status by sound-guided therapy reduces acute de- 122 Galindo P, Gasca C, Argaiz ER, Koratala A.
point-of-care ultrasonography. Kidney360. compensation events in chronic heart fail- Point of care venous Doppler ultrasound:
2021;2(8):1326–38. ure. Heart. 2020c;106(24):1934–9. exploring the missing piece of bedside he-
105 Argaiz ER, Rola P, Gamba G. Dynamic 114 Loutradis C, Papadopoulos CE, Sachpekidis modynamic assessment. World J Crit Care
changes in portal vein flow during decon- V, Ekart R, Krunic B, Karpetas A, et al. Lung Med. 2021;10(6):310–22.
gestion in patients with heart failure and ultrasound-guided dry weight assessment 123 Abraham WT, Adamson PB, Bourge RC,
cardio-renal syndrome: a POCUS case se- and echocardiographic measures in hyper- Aaron MF, Costanzo MR, Stevenson LW, et
ries. Cardiorenal Med. 2021;11(1):59–66. tensive hemodialysis patients: a randomized al. Wireless pulmonary artery haemody-
106 Koratala A, Ronco C, Kazory A. The prom- controlled study. Am J Kidney Dis. 2020; namic monitoring in chronic heart failure:
ising role of Lung ultrasound in assessment 75(1):11–20. a randomised controlled trial. Lancet. 2011;
of volume status for patients receiving 115 Loutradis C, Sarafidis PA, Ekart R, Papado- 377(9766):658–66.
maintenance renal replacement therapy. poulos C, Sachpekidis V, Alexandrou ME, et 124 Yaranov DM, Jefferies JL, Silver MA, Burk-
Blood Purif. 2020;49(6):643–6. al. The effect of dry-weight reduction guid- hoff D, Rao VN, Fudim M. Discordance of
107 Noble VE, Murray AF, Capp R, Sylvia-Rear- ed by lung ultrasound on ambulatory blood pressure and volume: potential implica-
don MH, Steele DJR, Liteplo A. Ultrasound pressure in hemodialysis patients: a ran- tions for pressure-guided remote monitor-
assessment for extravascular lung water in domized controlled trial. Kidney Int. 2019; ing in heart failure. J Card Fail. 2022; 28(5):
patients undergoing hemodialysis. Time 95(6):1505–13. 870–2.
course for resolution. Chest. 2009; 135(6):
1433–9.
14 Cardiorenal Med Koratala/Ronco/Kazory
DOI: 10.1159/000526902
You might also like
- Diagnosis FluidDocument14 pagesDiagnosis FluidCristianMP96No ratings yet
- Current and Future Issues in Hemophilia CareFrom EverandCurrent and Future Issues in Hemophilia CareEmérito Carlos Rodríguez-MerchánNo ratings yet
- 510732Document13 pages510732PaulHerreraNo ratings yet
- Joacp 35 29Document6 pagesJoacp 35 29kenjiNo ratings yet
- Assessment of Volume Status and Fluid Responsiveness in The Emergency Department: A Systematic ApproachDocument8 pagesAssessment of Volume Status and Fluid Responsiveness in The Emergency Department: A Systematic ApproachandreaNo ratings yet
- 2019 Article 1596Document9 pages2019 Article 1596Arina FitrianiNo ratings yet
- Personalized Electrolyte Prescription For Dialysis PatientsDocument13 pagesPersonalized Electrolyte Prescription For Dialysis PatientsSa7arNo ratings yet
- Quantifying Systemic Congestion With Point of Care Ultrasound. VEXUS PDFDocument12 pagesQuantifying Systemic Congestion With Point of Care Ultrasound. VEXUS PDFFIA SlotNo ratings yet
- Hemodynamic Parameters To Guide Fluid Therapy: Review Open AccessDocument9 pagesHemodynamic Parameters To Guide Fluid Therapy: Review Open AccessClaudioValdiviaNo ratings yet
- Fluid Overload in Peritoneal Dialysis PatientsDocument11 pagesFluid Overload in Peritoneal Dialysis PatientsHaryonoNo ratings yet
- Choque Septico en CirrosisDocument19 pagesChoque Septico en CirrosisAzael HaggardNo ratings yet
- Blood Transfusion in Anaesthesia and Critical Care: Less Is More!Document4 pagesBlood Transfusion in Anaesthesia and Critical Care: Less Is More!Maya_AnggrainiKNo ratings yet
- Fluid Management Strategies in Heart Failure PDFDocument16 pagesFluid Management Strategies in Heart Failure PDFFandy Hazzy AlfataNo ratings yet
- Which Echocardiographic Parameter Is A Better Marker of Volume Status in Hemodialysis PatientsDocument7 pagesWhich Echocardiographic Parameter Is A Better Marker of Volume Status in Hemodialysis PatientsmalisalukmanNo ratings yet
- Contemporary Perioperative Haemodynamic MonitoringDocument12 pagesContemporary Perioperative Haemodynamic MonitoringrjerezrNo ratings yet
- Fluid Management in The Critically Ill: Jean-Louis VincentDocument6 pagesFluid Management in The Critically Ill: Jean-Louis VincentFlorentina NadisaNo ratings yet
- Continuous Renal Replacement Therapy Among Patients With COVID-19 and Acute Kidney InjuryDocument8 pagesContinuous Renal Replacement Therapy Among Patients With COVID-19 and Acute Kidney InjuryPIR BanjarmasinNo ratings yet
- Micro y SepsisDocument14 pagesMicro y SepsisjimmyivaNo ratings yet
- Shock UciDocument16 pagesShock UciTania Parra MoralesNo ratings yet
- Best Clinical Practice: Red Blood Cell Transfusion in The Emergency DepartmentDocument11 pagesBest Clinical Practice: Red Blood Cell Transfusion in The Emergency DepartmentOscar F RojasNo ratings yet
- KDIGO HF Conf Report FINAL PDFDocument14 pagesKDIGO HF Conf Report FINAL PDFKarl Martin PinedaNo ratings yet
- Optimizing Fluid Management Guided by Volumetric Parameters in Patients With Sepsis and ARDS - 2023Document14 pagesOptimizing Fluid Management Guided by Volumetric Parameters in Patients With Sepsis and ARDS - 2023Chang TruNo ratings yet
- NPT El FinalDocument40 pagesNPT El FinalSelma Alonso BuenabadNo ratings yet
- Fluid Management in The Critically Ill: Jean-Louis VincentDocument6 pagesFluid Management in The Critically Ill: Jean-Louis VincentLucas MontanhaNo ratings yet
- 9) Fluid and HemodynamicsDocument13 pages9) Fluid and HemodynamicsPablo MartinezNo ratings yet
- Deschamps Jean Venous Doppler To Assess Congestion ADocument15 pagesDeschamps Jean Venous Doppler To Assess Congestion AGibran HolmesNo ratings yet
- Mechanisms, Clinical Implications, and Treatment of Intradialytic HypotensionDocument7 pagesMechanisms, Clinical Implications, and Treatment of Intradialytic Hypotensionhemer hadyn calderon alvitesNo ratings yet
- Fluid and HemodynamicsDocument13 pagesFluid and HemodynamicsJoelGámezNo ratings yet
- Goal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialDocument7 pagesGoal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialkenjiNo ratings yet
- Artículo Manejo de CoagulopatíaDocument17 pagesArtículo Manejo de CoagulopatíaSMIBA MedicinaNo ratings yet
- 2017 Article 133Document8 pages2017 Article 133Sastra NopiNo ratings yet
- Decongestion: Diuretics and Other Therapies For Hospitalized Heart FailureDocument8 pagesDecongestion: Diuretics and Other Therapies For Hospitalized Heart FailureRizky Agus MNo ratings yet
- Update On Hepatorenal Syndrome Definition, Pathogenesis, and ManagementDocument9 pagesUpdate On Hepatorenal Syndrome Definition, Pathogenesis, and ManagementYassine vNo ratings yet
- Haemodialysis With On-Line Monitoring EquipmentDocument12 pagesHaemodialysis With On-Line Monitoring EquipmentConnie Alva GutierrezNo ratings yet
- Early Goal-Directed Therapy in Severe Sepsis and Septic Shock RevisitedDocument17 pagesEarly Goal-Directed Therapy in Severe Sepsis and Septic Shock RevisitedSusana ViafaraNo ratings yet
- 10 Respuestas para Manejo de LíquidosDocument11 pages10 Respuestas para Manejo de Líquidosfrida casdelNo ratings yet
- Perio PBM J FluidsDocument6 pagesPerio PBM J Fluidsjamiro345No ratings yet
- Lung Ultrasound A “ Biomarker” For FDocument8 pagesLung Ultrasound A “ Biomarker” For Flegap27No ratings yet
- 2014 Journal - Patient With Congenital Systemic To Pulmonary Shunts and Increased Pulmonary Vascular ResistanceDocument7 pages2014 Journal - Patient With Congenital Systemic To Pulmonary Shunts and Increased Pulmonary Vascular ResistanceAryfKurniawanNo ratings yet
- UCI Shock Valoracion BuenoDocument7 pagesUCI Shock Valoracion BuenoJuan Camilo Cruz VegaNo ratings yet
- Journal Pone 0035634Document5 pagesJournal Pone 0035634Nathaly AráuzNo ratings yet
- 2020 Ortoleva - Vasoplegia During Cardiopulmonary Bypass Current Literature and Rescue Therapy OptionsDocument10 pages2020 Ortoleva - Vasoplegia During Cardiopulmonary Bypass Current Literature and Rescue Therapy OptionsRizal MuhammadNo ratings yet
- Journal of Intensive Medicine: Florence Boissier, Nadia AissaouiDocument9 pagesJournal of Intensive Medicine: Florence Boissier, Nadia AissaouiMaudiel BrionesNo ratings yet
- Diuretics in Heart Failure GuidelinesDocument8 pagesDiuretics in Heart Failure GuidelinesMihai CebotariNo ratings yet
- Lactato y Perfusion Kattan y GlennDocument5 pagesLactato y Perfusion Kattan y GlennAna Belén Artero CastañoNo ratings yet
- The Use of Bioimpedance Spectroscopy To Guide Fluid Management in Patients Receiving DialysisDocument7 pagesThe Use of Bioimpedance Spectroscopy To Guide Fluid Management in Patients Receiving Dialysisnelbut2No ratings yet
- -- Clinical and Experimental Emergency MedicineDocument56 pages-- Clinical and Experimental Emergency MedicineAlfonso Ga MaNo ratings yet
- Special Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionDocument8 pagesSpecial Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionDavid SantosoNo ratings yet
- Tatalaksana GUCH Di ICUDocument12 pagesTatalaksana GUCH Di ICUBima AryaputraNo ratings yet
- Elia Jennifer Perioperative Fluid Management andDocument19 pagesElia Jennifer Perioperative Fluid Management andSiddhartha PalaciosNo ratings yet
- AnemiaDocument7 pagesAnemiaAttilio Del RossoNo ratings yet
- Clinical Review: Management of Weaning From Cardiopulmonary Bypass After Cardiac SurgeryDocument18 pagesClinical Review: Management of Weaning From Cardiopulmonary Bypass After Cardiac SurgeryAdilZyaniNo ratings yet
- FALLA HEPÁTICA AGUDA SOBRE CRÓNICA 2024Document10 pagesFALLA HEPÁTICA AGUDA SOBRE CRÓNICA 2024MarcoNo ratings yet
- Acute Care and Emergency General Surgery in Patients With Chronic Liver Disease: How Can We Optimize Perioperative Care? A Review of The LiteratureDocument9 pagesAcute Care and Emergency General Surgery in Patients With Chronic Liver Disease: How Can We Optimize Perioperative Care? A Review of The LiteratureJœnríčk AzueloNo ratings yet
- Albumin in aSAH NeuroCrit2023Document11 pagesAlbumin in aSAH NeuroCrit2023Ahida VelazquezNo ratings yet
- Research Open Access: Samoni Et Al. Critical Care (2016) 20:95 DOI 10.1186/s13054-016-1269-6Document8 pagesResearch Open Access: Samoni Et Al. Critical Care (2016) 20:95 DOI 10.1186/s13054-016-1269-6Suis MionooNo ratings yet
- A Review Article: Access Recirculation Among End Stage Renal Disease Pa-Tients Undergoing Maintenance HemodialysisDocument6 pagesA Review Article: Access Recirculation Among End Stage Renal Disease Pa-Tients Undergoing Maintenance HemodialysisIrma HermaliaNo ratings yet
- Expert Statement For Management Hypovolemia in Sepsis PDFDocument8 pagesExpert Statement For Management Hypovolemia in Sepsis PDFRobi HeryantoNo ratings yet
- Early Goal-Directed Therapy, Follow-UpDocument19 pagesEarly Goal-Directed Therapy, Follow-Upalfred1294No ratings yet
- TEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For ManagementDocument10 pagesTEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For Managementbenitez1228No ratings yet
- Anaesthesia - 2022 - Migdady - Management of Status Epilepticus A Narrative Review-1Document14 pagesAnaesthesia - 2022 - Migdady - Management of Status Epilepticus A Narrative Review-1Verónica Rojas NavaNo ratings yet
- Rev 2022 Acid Base Disorders in The Critically Ill Patient1665692570153Document11 pagesRev 2022 Acid Base Disorders in The Critically Ill Patient1665692570153benitez1228No ratings yet
- Nej Mo A 2200433Document12 pagesNej Mo A 2200433benitez1228No ratings yet
- 1 s2.0 S0140673622014854 MainDocument12 pages1 s2.0 S0140673622014854 Mainsilvia100% (1)
- Emergencias HipertensivasDocument13 pagesEmergencias HipertensivasÁngel Rodolfo Maldonado AzamarNo ratings yet
- 1 s2.0 S0140673622014398 MainDocument14 pages1 s2.0 S0140673622014398 MainsilviaNo ratings yet
- Procedural Sedation AnalgesiaDocument24 pagesProcedural Sedation Analgesiabenitez1228No ratings yet
- Wa0000.Document7 pagesWa0000.benitez1228No ratings yet
- Modos Basicos de VentilacionDocument16 pagesModos Basicos de Ventilacionbenitez1228No ratings yet
- Emergency Ultrasound Standard Reporting Guidelines. ACEP. 2011Document29 pagesEmergency Ultrasound Standard Reporting Guidelines. ACEP. 2011benitez1228No ratings yet
- 1022 AngioedemaDocument24 pages1022 Angioedemabenitez1228No ratings yet
- Cetoacidosis AlcoholicaDocument8 pagesCetoacidosis Alcoholicabenitez1228No ratings yet
- Hipertensión Pulmonar (2022)Document114 pagesHipertensión Pulmonar (2022)Mauricio CabreraNo ratings yet
- Early Norepinephrine Use in Septic ShockDocument6 pagesEarly Norepinephrine Use in Septic Shockbenitez1228No ratings yet
- Blood Lactate Levels in Sepsis in 8 QuestionsDocument5 pagesBlood Lactate Levels in Sepsis in 8 Questionsbenitez1228No ratings yet
- Cerebral Venous Thrombosis: A Practical GuideDocument12 pagesCerebral Venous Thrombosis: A Practical Guidedanby danbyNo ratings yet
- 1 s2.0 S2667100X21000347Document5 pages1 s2.0 S2667100X21000347benitez1228No ratings yet
- Acido BaseDocument10 pagesAcido Basebenitez1228No ratings yet
- Iam 2022Document14 pagesIam 2022Mateo Daniel Gutierrez CastañedaNo ratings yet
- The Impact of Coffee Subtypes On Incident Cardiovascular Disease, Arrhythmias, and MortalityDocument10 pagesThe Impact of Coffee Subtypes On Incident Cardiovascular Disease, Arrhythmias, and MortalityJenny RojoNo ratings yet
- PC 4 NursingcareplanDocument2 pagesPC 4 Nursingcareplanapi-316769247No ratings yet
- Tui Na PDFDocument368 pagesTui Na PDFyadi85% (27)
- Education PreparationDocument17 pagesEducation Preparationpraveen praveen100% (2)
- Rhinosporidiosis Still An EnigmaDocument12 pagesRhinosporidiosis Still An EnigmaDr. T. BalasubramanianNo ratings yet
- Staff Handbook SECTION 8Document27 pagesStaff Handbook SECTION 8Funda HandaNo ratings yet
- Bagan KejangDocument10 pagesBagan KejangNie' MKNo ratings yet
- UTI Small Cap Fund - Equity Funds - UTI Mutual FundDocument23 pagesUTI Small Cap Fund - Equity Funds - UTI Mutual FundRinku MishraNo ratings yet
- The Breast - Part 2 Dr. Roberto B. Acuña: Hormonal Non-HormonalDocument14 pagesThe Breast - Part 2 Dr. Roberto B. Acuña: Hormonal Non-HormonalMaf BNo ratings yet
- Fact Sheet 11 - DebriefingDocument3 pagesFact Sheet 11 - Debriefingkhushi.avatharaNo ratings yet
- Course Details - CHC32015 Certificate III in Community Services - Mark Oliphant CollegeDocument1 pageCourse Details - CHC32015 Certificate III in Community Services - Mark Oliphant CollegeSaroja ChhetriNo ratings yet
- San Pedro Hospital Case Vignette on Pulmonary TBDocument7 pagesSan Pedro Hospital Case Vignette on Pulmonary TBShareen Joyce AgbayaniNo ratings yet
- The Standard - 2014-07-30Document71 pagesThe Standard - 2014-07-30jorina8070% (1)
- Kirk D. Strosahl, Patricia J. Robinson, Thomas Gustavsson Brief Interventions For Radical Change Principles and Practice of Focused Acceptance and Commitment Therapy PDFDocument297 pagesKirk D. Strosahl, Patricia J. Robinson, Thomas Gustavsson Brief Interventions For Radical Change Principles and Practice of Focused Acceptance and Commitment Therapy PDFebiznes100% (18)
- Type 1 Diabetes Epidemiology, Pathogenesis, and TreatmentDocument27 pagesType 1 Diabetes Epidemiology, Pathogenesis, and TreatmentJuan Pablo PérezNo ratings yet
- Research Time ManagementDocument39 pagesResearch Time ManagementArnel Belza Torrejas79% (14)
- Compensation Management Practice of Garments Industries in BangladeshDocument30 pagesCompensation Management Practice of Garments Industries in BangladeshHamidur Rahman HanyNo ratings yet
- CoC7 PC Sheet - Beat Cop - 1920s - Standard - GreyscaleDocument3 pagesCoC7 PC Sheet - Beat Cop - 1920s - Standard - GreyscaleD DeeNo ratings yet
- Flexible Learning and Teaching PDFDocument32 pagesFlexible Learning and Teaching PDFHazel Faye JuridicoNo ratings yet
- Clostridium Tetani NotesDocument10 pagesClostridium Tetani NotesGame GameNo ratings yet
- 2022 - Epidemiologia - Sifilis VIH en Homosexuales HombresDocument25 pages2022 - Epidemiologia - Sifilis VIH en Homosexuales HombresEduardo RodriguezNo ratings yet
- Risk Assessment for Elevator MaintenanceDocument5 pagesRisk Assessment for Elevator MaintenanceMahran Mastouri100% (4)
- ISO 18001 ChecklistDocument7 pagesISO 18001 ChecklistRohit SharmaNo ratings yet
- HOPE 1 - Exercise For FitnessDocument3 pagesHOPE 1 - Exercise For FitnessReàgan Buela II0% (1)
- QMS PresentationDocument18 pagesQMS PresentationadsfsNo ratings yet
- 11 cсынып емтихан сурактарыDocument6 pages11 cсынып емтихан сурактарыakzharNo ratings yet
- Buku Kerja Guru 3Document15 pagesBuku Kerja Guru 3ismail salehNo ratings yet
- DG Document Requirements Reference SheetDocument7 pagesDG Document Requirements Reference SheetJosé Larragaña OsunaNo ratings yet
- Bab 10 (Hortatory Exposition-Written)Document11 pagesBab 10 (Hortatory Exposition-Written)kokotopnemenNo ratings yet
- Biology Form 4 Chapter 6 NutritionDocument5 pagesBiology Form 4 Chapter 6 NutritionzaedmohdNo ratings yet
- Housekeeping For Grades 7 and 8Document38 pagesHousekeeping For Grades 7 and 8melvin ariasNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (17)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)