0% found this document useful (0 votes)
91 views10 pagesHEPATITIS
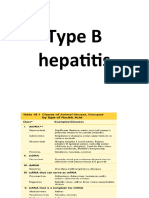
Viral hepatitis is caused by five main hepatitis viruses that infect the liver. Hepatitis B and C can cause chronic infections and lead to cirrhosis or liver cancer. Hepatitis A virus is transmitted via the fecal-oral route while hepatitis B can also be transmitted via blood or bodily fluids. Laboratory diagnosis of hepatitis A involves detecting IgM antibodies or the virus itself. Hepatitis B diagnosis involves detecting hepatitis B surface antigen, e antigen, or core antigen to determine active or past infection. There is no treatment for hepatitis A but hepatitis B has vaccines to prevent infection.
Uploaded by
Vanlal RemruatiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
91 views10 pagesHEPATITIS
Viral hepatitis is caused by five main hepatitis viruses that infect the liver. Hepatitis B and C can cause chronic infections and lead to cirrhosis or liver cancer. Hepatitis A virus is transmitted via the fecal-oral route while hepatitis B can also be transmitted via blood or bodily fluids. Laboratory diagnosis of hepatitis A involves detecting IgM antibodies or the virus itself. Hepatitis B diagnosis involves detecting hepatitis B surface antigen, e antigen, or core antigen to determine active or past infection. There is no treatment for hepatitis A but hepatitis B has vaccines to prevent infection.
Uploaded by
Vanlal RemruatiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd