Professional Documents
Culture Documents
VR Mesh 5
Uploaded by
Zaid DewachiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
VR Mesh 5
Uploaded by
Zaid DewachiCopyright:
Available Formats
Journal of Dentistry and Oral Biology Case Report
Published: 07 Sep, 2017
Three-Dimensional Surface Model Analysis of Intraoral
Maxillary Protraction Combined with Alt-RAMEC: A Case
Report
Hatice Gökalp*
Department of Orthodontics, University of Ankara, School of Dentistry, Beşevler, Ankara, Turkey
Abstract
Protraction face-mask (PFM) therapy is the most common approach for early treatment of Class III
patients with maxillary deficiency. Main goal of the therapy is to achieve the orthopedic effect rather
than dento-alveolar correction. Maxillary protraction combined with maxillary expansion simplifies
maxillary advancement. On the other hand, early Class III treatment with PFM therapy generally
needs patient’s cooperation. Effective protraction of maxilla is provided by disarticulation of maxilla
from neighbor bones. The use of intraoral protraction spring (IPS) combined with the Alternate
Rapid Maxillary Expansions and Constrictions (Alt-RAMEC) is preferred method recently not
only to eliminate patient’s cooperation but also to disarticulate maxilla from the circum-maxillary
sutures. The purpose of this case report is to evaluate the skeleto-facial effects of IPS combined
with Alt-RAMEC in pubertal growth period by cone beam computed tomography (CBCT). Alt-
RAMEC-IPS therapy affected the naso-maxillary structures entirely and showed significantly
favorable effects on maxillary advancement. The use of Alt-RAMEC/IPS appears to be a promising
treatment method instead of using PFM therapy.
Keywords: Alt-RAMEC; Intraoral maxillary protraction; Maxillary deficiency
Introduction
Treatment of Class III malocclusion with maxillary deficiency is one of the most challenging
skeletal anomalies in orthodontics. Protraction face mask (PFM) therapy combined with rapid
OPEN ACCESS maxillary expansion (RME) is the most common approach for early treatment of these patients. As
*Correspondence: well as this treatment approach results uncertain skeletal and inevitable dento-alveolar effects [1,2],
Hatice Gökalp, Department of wearing these un-aesthetic extra-oral appliance is required for 12 to 16 h per day for 9 to 12 months
Orthodontics, University of Ankara, for satisfactory clinical success [3-5]. Force delivered by rapid maxillary expansion affects directly
School of Dentistry, Beşevler, Ankara, on mid-palatal suture and partially on circumaxillary sutures. Disarticulation of the maxilla from
Turkey, circumaxillary bones is required for simplifying maxillary protraction. Double-hinged expansion
E-mail: haticegokalp@yahoo.com
screw is used by a new the expansion protocol named alternate maxillary expansions and constrictions
(Alt-RAMEC) that disarticulates the maxillary bone from the surrounding sutures for providing
Received Date: 16 Jun 2017
effective maxillary protraction. Effects of Alt-RAMEC on circumaxillary sutures are researched by
Accepted Date: 30 Aug 2017
both animal [6,7] and clinical [1,8-14] studies. Advantage of the method is to provide pure maxillary
Published Date: 07 Sep 2017
protraction without using any extra-oral protraction appliance. Furthermore, in serious maxillary
Citation: deficiencies it is recommended to use Alt-RAMEC combined with intraoral protraction spring
Gökalp H. Three-Dimensional Surface (IPS) instead of extra-oral appliance [1,14]. It is stated that using intraoral maxillary protraction
Model Analysis of Intraoral Maxillary combined with Alt-RAMEC increases the orthopedic effects [1,14]. Three dimensional images have
Protraction Combined with Alt-RAMEC: been recently used in orthodontics for eliminating the insufficiency of traditional two-dimensional
A Case Report. J Dent Oral Biol. 2017; images [15]. Purpose of this case report is to evaluate the skeleto-facial effects of the IPS combined
2(12): 1078. with Alt-RAMEC in a pubertal patient by cone beam computed tomography (CBCT).
ISSN: 2475-5680
Case Presentation
Copyright © 2017 Hatice Gökalp. This
Diagnosis and etiology
is an open access article distributed
under the Creative Commons Attribution The patient, an adolescent girl, age 13 years, came to University of Ankara, Department of
License, which permits unrestricted Orthodontics in Turkey with a complaint about her un-aesthetic facial-dental appearance and
use, distribution, and reproduction in anterior cross-bite in addition to posterior cross-bite of right side. In her medical history, her
any medium, provided the original work
uncle had similar skeletal discrepancy. She had Class III malocclusion associated with maxillary
retrusion with an -3 overjets and 8 mm overbite. There was a 3 mm midline discrepancy caused by
is properly cited.
Remedy Publications LLC. 1 2017 | Volume 2 | Issue 12 | Article 1078
Hatice Gökalp Journal of Dentistry and Oral Biology
Figure 2: Intraoral Protraction Spring (IPS). A. IPS view closed the mouth; B.
Figure 1: Extraoral and intraoral photograps before treatment. IPS view opened the mouth.
mandible. Upper and lower arch length discrepancy was -12 mm/-4
mm respectively (Figure 1). Her growing stage was stage III according
to cervical vertebra maturation (CV) method.
Treatment objectives
The main treatment objectives were to resolve transverse and
sagittal maxillary discrepancy and to establish facial and smile
esthetic.
Treatment alternatives
Two treatment alternatives were proposed. The first option
was the contemporary technique combined use of rapid maxillary
expansion (RME) and extra oral protraction facemask (PFM). On the
other hand, it was demonstrated that RME insufficiently effects on
circumaxillary sutures [16-18] and patient co-operation using PFM
leads unsuccessful results because of un-esthetic appearance of it. For
this reason, in many cases, patients would prefer to undergo surgical
correction rather than to use the extra-oral appliances when growth
was completed. Protraction spring has been the only intraoral device
that delivers reasonable orthopedic force for maxillary orthopedic
Figure 3: Extraoral and intraoral photograps after treatment of IPS combined
protraction. Because she was an adolescent nonsurgical treatment with Alt-RAMEC.
consisted of Alt-RAMEC-IPS combination was planned in this case.
Treatment progress
Before the treatment, patient and her parent provided written
informed consent after receiving verbal and written explanations of
the treatment. The appliance containing a hyrax expansion screw was
applied to open the maxillary suture by a protocol of Alt-RAMEC.
The patient's parent was instructed to open the screw by 0.5 mm
per day during the first week and to close it by 0.5 mm per day the
week after. This alternate opening and closing was repeated for 7
consecutive weeks and immediately after expansion period IPSs
were applied for 6 months. Alt-RAMEC effect on circumaxillary
sutures is simulated to tooth extraction in which the tooth is rocked
buccally and lingually to loosen from the alveolar socket. Similarly,
opened and closed of the expansion screw rocks the maxillary sutures
articulated circumaxillary bone. Maxillary protraction was produced
by a pair of fixed 0.036” TMA helical springs having 100° to 120°
angle with mandibular anchorage by banding first molars, premolars
and canines with 0.018 × 0.025 inch pre-adjusted bracket system and Figure 4: Extraoral and intraoral photograps after Orthodontic treatment.
a lingual arch in this case (Figure 2). Active maxillary protraction
was applied for 4 months and protraction springs was kept intra- 2 mm overbite was maintained (Figure 3). At the end of orthopedic
orally for 2 months without adding extra-oral force. After maxillary traction, hyrax expander and springs removed and trans-Palatal arch
protraction, she was in the CV stage IV growing period according to was inserted on palate. First permanent premolars in the both side
cervical vertebra maturation method. Upper and lower arch length were extracted to eliminate the upper arch length discrepancy and
discrepancy was -15 mm and 3 mm respectively and 2 mm overjet and first molars, premolars and canines banded with 0.018 × 0.025 inch
Remedy Publications LLC. 2 2017 | Volume 2 | Issue 12 | Article 1078
Hatice Gökalp Journal of Dentistry and Oral Biology
Table 1: Cephalometric analysis before treatment (T1), After Alt- RAMEC-
Protraction Spring treatment (T2) and at the end of fixed Orthodontic Treatment.
Measurements T1 T2 T3
SNA (°) 82° 8 82
Na Perp– Point A -5 0 -1
SNB (°) 86 81.5 81
Na Perp-Pogonion (mm) 0 -2 -3
Figure 5: Segmentation process. ANB (°) -4 1.5 1°
Go-Gn/FH (°) 30 34.5 32.5
Facial axis angle 90 95 96
Co–A (mm) 104 101 98
Co–Gn (mm) 145 138 136
CoGn–CoA (mm) 39 39.5 43
1-NA (mm) 5 7 7
1–NB (mm) 7 5 7
Maxillary first molar width (mm) 64 68 69
Lateroorbitale width (mm) 77 78 78
Figure 6: Color maps of 3D superimpositions of craniofacial structures at Lateronasal width (mm) 16 18 18
T1-T2.
Bizygomatic width (mm) 147 149 150
Maxillary width (mm) 75 77 77
pre-adjusted bracket system. Total treatment time was 34 months
(Figure 4). To visualize the treatment changes in 3 dimensions, Upper lip to S line (mm) -4 -2 -2.5
CBCT records were taken before treatment (T1), immediately after Lower lip tp S line (mm) 0 1.5 -1.5
orthopedic treatment included IPS-Alt-RAMEC combination (T2)
and at the end of fixed orthodontic therapy (T3). Three-dimensional cephalometric measures show on Table 1.
surface models of the anatomic region were constructed from T1, T2
and T3 images of patient by using 3D modeling software Rhinoceros Treatment results
4.0 (3670 Woodland Park Ave N, Seattle, WA 98103 USA) and match Patient was evaluated with focus on the following anatomic
and quality control software VR Mesh Studio (Virtual Grid Inc, regions:
Bellevue City, WA, USA).
1. Anterior and posterior surface of maxilla
For modeling the bone tissue, cranio-facial region was scanned by
2. Zygomatic process of maxilla
a cone beam computed tomography (ILUMA, Orthocad, CBCT, 3M
Imtec, Oklahoma, USA). 601 cross-sectional images were obtained 3. Anterior and posterior surface of mandible
at 120 kVp, 3.8 mA and a voxel size of 0.3 mm, with an exposure
4. Inferior border of mandible
time 40 s. Cross-sectional images were saved as digital imaging and
communications in medicine (DICOM) files and taken to 3D-Doctor 5. Anterior and posterior surface of condyles
programme for re-construction. By Interactive Segmentation
6. The soft tissues in nasal region, the upper and lower lips,
method, Hounsfield values were evaluated and bone tissue was
cheek and chin.
separated (Figure 5). After separation, 3D models were obtained
by 3D- Complex Render technique. At T1, T2 and T3, 3D models The skeletal and soft tissue changes between T1, T2 and T3 in
were registered on anterior cranial fossa structures, specifically the the areas of interest are shown as color maps or non-transparencies
endocrinal surfaces of the cribriform plate region of the ethmoid in (Figures 6-11). Magnitude and direction of skeletal and soft
bone and internal surface of the frontal bone. These regions were tissue movements were assessed as color changed from red to blue
chosen because of their early completion of growth [19-21]. Three represented positive (outward) and negative (inward) movement
dimensional surfaces were created for all models and loaded into respectively.
superimposition program. The initial and registered final models
were superimposed, and treatment changes were expressed via color Figure 5 and 6 show skeletal changes between T1 and T2 in
maps that represent the closest-point surface distance from the final maxilla, mandible, zygomatic process, condyles as color maps and
model to the initial one. For additional comparative assessment of non-transparencies. Positive (outward) movement showed in anterior
changes between the models, non-transparent superimpositions and posterior maxillary regions through inferior border of the
were also used. DICOM files were also used to create synthetic lateral zygomatic process. Changes in the anterior and posterior mandibular
cephalograms for T1, T2 and T3 by using imaging software (version regions were more variable in both magnitude and direction (Figure
10.1, Dolphin Imaging, Chastworth, Calf), which uses an algorithm 6). Surface distance between left and right condyles were similar
that recreates perspective projections. The software allows the user to each other. Condyles showed negative (inward) change on anterior
specify where the central ray of the imaginary x-ray beam is focused. surfaces and positive (outward) change on posterior surfaces. Inferior
Lateral cephalograms for T1, T2 and T3 were digitally traced. The border of mandible showed positive change (Figure 7).
Remedy Publications LLC. 3 2017 | Volume 2 | Issue 12 | Article 1078
Hatice Gökalp Journal of Dentistry and Oral Biology
Figure 7: Nontransparent 3D superimpositions of craniofacial structures at
T1-T2.
Figure 10: Color maps of 3D superimpositions of craniofacial structures at
T2-T3.
Figure 8: Nontransparent 3D superimpositions of facial soft tissues at T1-T2.
Figure 11: Color maps of 3D superimpositions of facial soft tissues at T2-T3.
Change in upper lip was invariable in both magnitude and direction.
Negative movement (inward) showed in lower lip but there were
considerable variations in magnitude. Nose tip and cheeks showed
positive (outward) movement but more variable in both magnitude
and direction (Figure 11). Cephalometric assessment for skeletal, soft
tissue and dental changes for Alt-RAMEC/IPS treatment summarize
on Table 1. By the therapy, a point showed a great improvement (5
mm) in horizontal movement. Increase in SNA and decrease in SNB
angles improved the inter-maxillary relationship (ANB +5.5°) and by
Figure 9: Color maps of 3D superimpositions of facial soft tissues at T1-T2. this way overjet decreased. A relative increase in vertical dimension at
expansion-protraction phase, decreased immediately after acquiring
The soft tissues in the upper lip and lateral side of nasal regions molar contacts by the fixed orthodontic therapy. Clockwise rotation
showed positive changes. Chin and cheeks showed negative changes of the mandible and minimal retroclination of lower incisors were
(Figure 8). Non-transparency of 3D superimpositions was made to obtained. Upper/lower lips changes were variable in T2 and T3 (Table
evaluate changes of maxilla, circum-maxillary bones, mandible and 1).
soft tissues on T1-T2. Gray color showed T1 and red color showed
T2 3D model. To evaluate changes of maxillary expansion and Discussion
protraction (T1-T2), 3D model of red color (T2) was superimposed The aim of this case report was to assess a new treatment approach
on 3D model of gray color (T1). Maxillary bone included zygomatic for growing Class III patients combined with maxillary retrusion and
process through bilateral zygomatico-maxillary junction, bilateral to describe the skeletal, dental and soft tissue changes in 3 dimensions.
inferior orbital border and lateral walls of nasal cavity moved forward The cephalometric and 3D measurements seem to confirm that Alt-
bodily (Figure 7). While posterior border of ramus mandible through RAMEC-IPS treatment combination comprised more orthopedic
posterior condylar region moved backward, inferior border of corpus correction with less dentoalveoler effect when compared with PFM/
mandible moved downward. Red color was covered by gray color so RME [22-27]. The 3D assessments for this case report have been
that chin moved backward in T2. Therefore, red color no visualized shown to be more reliable than 2D imaging alone. Color maps and
in chin because of non-transparency of 3D superimposition. While non-transparencies were preferred to obtain more accurate data.
soft tissues of nose, sub-nasal region and upper lip moved forward, Reports about the effects of maxillary expansion on maxillary position
soft tissue chin moved backward (Figures 8 and 9). Figure 10 show have inconsistencies. Wertz [28], reported forward change in the
skeletal changes between T2 and T3 in maxilla, mandible, condyles position of maxilla, whereas Pangrazio-Kulbersh et al. [3] reported no
as color maps and non-transparencies. Maxillary anterior teeth and significant displacement, or even Sarver and Johnston [29] reported a
maxillary premolars moved forward and lateral. Mandibular anterior posterior displacement of maxilla. Alt-RAMEC protocol is developed
teeth moved backward and overjet was positive. Mandibular corpus, for a greater anterior displacement of maxilla by eliminating resistance
ramus and condyle showed positive (outward) movement. Change of circum-maxillary sutures Liou and Tsai [14] presented the Alt-
in chin was invariable in both magnitude and direction (Figure 10). RAMEC protocol in 3 components: a double-hinged rapid maxillary
Remedy Publications LLC. 4 2017 | Volume 2 | Issue 12 | Article 1078
Hatice Gökalp Journal of Dentistry and Oral Biology
expander, repetitive weekly protocol of Alt-RAMEC and IPSs. Conclusion
Researchers introduced the new kind of expander as a more superior
device than the other types of expanders for the treatment of a hypo- 1. Alt-RAMEC/IPS treatment, improves skeletal relationships
plastic maxilla in growing Class III patients. In this case, protocol in Class III malocclusion associated with maxillary deficiency with
has been modified by using Alt-RAMEC protocol with a Hyrax-type minimal dentoalveolar compensation in adolescent patient.
maxillary expander and IPSs to assess the treatment differences versus 2. This treatment method could be preferred instead of extra-
the original one. Liou and Tsai [14] reported an excessive anterior oral appliances for adolescents.
movement of maxilla after Alt-RAMEC with double-hinged palatal
expander in 2D measurements; while Yilmaz and Kucukkeles [30] 3. 3D data from CBCT allows for documentation of treatment
found slight forward and downward movement of maxilla in pre- changes.
adolescents by 3D evaluation. In this case, maxilla moved forward References
but pure maxillary displacement by maxillary expansion couldn’t be
1. Liou EJ. Toothborne orthopedic maxillary protraction in Class III patients.
assessed because second record taken at the end of protraction phase
J Clin Orthod. 2005;39(2):68-75.
by reason of given ionizing radiation exposure. Efficiency of maxillary
protraction is based on opening the circum-maxillary sutures. Alt- 2. Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. The effectiveness
RAMEC disarticulates maxilla from circum-maxillary sutures and of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial
Orthop. 1999;115(6):675-85.
enables maxillary protraction. A point showed a great improvement
(5 mm) in horizontal movement and A-point displacement is more 3. Pangrazio-Kulbersh V, Berger J, Kersten G. Effects of protraction mechanics
excessive than those reported with PFM in limited 2D studies. on the midface. Am J Orthod Dentofacial Orthop. 1998;114(5):484-91.
Assessment of treatment effects on 3D color-map superimpositions 4. Tortop T, Keykubat A, Yuksel S. Facemask therapy with and without
becomes possible not only for maxilla but also for circum-maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132(4):467-74.
region. Maxillary bone included zygomatic process through bilateral
5. Keles A, Tokmak E C, Erverdi N, Nanda R. Effect of varying the
zygomatico-maxillary junction, bilateral inferior orbital border and force direction on maxillary orthopedic protraction. Angle Orthod.
lateral walls of nasal cavity is affected by Alt-RAMEC/IPS treatment. 2002;72(5):387-96.
Inferior border of the zygomatic process showed a positive change in
6. Huang CT, Wang YC, Huang CS, Liou EJ. Maxillary displacement after
this case. Wang showed that Alt-RAMEC opens coronally running
rapid maxillary expansions: An animal study. J Taiwan Assoc Orthod.
circum-maxillary sutures (Fronto-maxillary, zygomatico-maxillary 2008;20(2):19-31.
and inside the orbit) quantatively more than conventional RME in an
animal study. This case is the first attempt to explore that a modified 7. Wang YC, Chang PM, Liou EJ. Opening of circumaxillary sutures by
alternate rapid maxillary expansions and constrictions. Angle Orthod.
Alt-RAMEC procedure affects the circum-maxillary sutures and
2009;79(2):230-4.
facilitates the maxillary protraction.
8. Isci D, Turk T, Elekdag-Turk S. Activation–deactivation rapid palatal
There is a great deal of controversy in the literature regarding to expansion and reverse headgear in Class III cases. Eur J Orthod.
optimal force of PFM treatment, but after summarizing the studies, 2010;32(6):706-15.
it could be concluded that 300 g to 400 g of force is more efficient
9. Liou EJ, Chen PKT. New orthodontic and orthopaedic managements on
for maxillary protraction. IPS is activated when the mandible closes
the premaxillary deformities in patients with bilateral cleft before alveolar
and a 300 g to 400 g horizontal and upward force on each side is bone grafting. Ann R Coll Surg. 2003;7(3):73-82.
created. Cephalometric measurements showed that increase in SNA
and decrease in SNB angles improved inter-maxillary relationship 10. Tsai WC, Huang CS, Lin CT, Liou EJ. Dentofacial changes of combined
double-hinged rapid maxillary expansion and protraction facemask
(ANB +5.5°) and by this way overjet decreased. In this case, a skeletal
therapy. J Taiwan Assoc Orthod. 2008;20(2):5-18.
maxillary forward displacement was obtained just in 5, 5 months
by an intraoral approach which motivates the patient. However, 11. da Luz Vieira G, de Menezes LM, de Lima EM, Rizzatto S. Dentoskeletal
IPS made by titanium-molybdenum was frequently broken due to Effects of Maxillary Protraction in Cleft Patients with Repetitive Weekly
Protocol of Alternate Rapid Maxillary Expansions and Constrictions. Cleft
material fatique or chewing force and during treatment IPSs needed
Palate Craniofac J. 2009;46(4):391-8.
to be fabricated for multiple times. In addition, IPS is indicated in
low angle cases depending on the opening of the bite at the anterior 12. Do-deLatour TB, Ngan P, Martin CA, Razmus T, Gunel E. Effect of
and backward rotation of the mandible. The magnitude of changes alternate maxillary expansion and contraction on protraction of the
maxilla: a pilot study. Hong Kong Dent J. 2009;6:72-82.
in the mandible is more variable in this case. Anterior and partially
posterior surface of the mandible showed negative changes by reason 13. Kaya D, Kocadereli I, Kan B, Tasar F. Effects of facemask treatment
of clockwise rotation of mandible. Lingual holding arch is used for anchored with miniplates after alternate rapid maxillary expansions and
mandibular anchorage but despite this precaution, upper segment constrictions; A pilot study. Angle Orthod. 2011;81(4):639-46.
of the corpus mandible moved inward while lower segment of the 14. Liou EJ, Tsai WC. A new protocol for maxillary protraction in cleft patients:
corpus mandible moved outward. Collum and ramus mandible Repetitive weekly protocol of alternate rapid maxillary expansions and
moved inward at protraction phase owing to the backward force by constrictions. Cleft Palate Craniofac J. 2005;42(2):121-7.
the IPSs but on the contrary opposite changes observed after fixed 15. Varghese S, Kailasam V, Padmanabhan S, Vikraman B, Chithranjan A.
orthodontic treatment because of the late mandibular growing. One Evaluation of the accuracy of linear measurements on spiral computed
of the goals of treatment of Class III malocclusion is to significantly tomography-derived three dimensional images and its comparison
improve the dento-facial profile. Forward movement of the skeletal with digital cepha lometric radiography. Dentomaxillofac Radiol.
structures in naso-maxillary region shows similar variations in soft 2010;39(4):216-23.
tissues. Favorable soft tissue changes were observed by the treatment 16. Ngan P, Yiu C, Hu A, Hagg U, Wei SH, Gunel E. Cephalometric and
similarly in PFM/RME studies. occlusal changes following maxillary expansion and protraction. Eur J
Remedy Publications LLC. 5 2017 | Volume 2 | Issue 12 | Article 1078
Hatice Gökalp Journal of Dentistry and Oral Biology
Orthod. 1998;20(3):237-54. 25. Nanda R. Biomechanical and clinical consideration of a modified
protraction headgear. Am J Orthod Dentofacial Orthop. 1980;78(2):125-
17. Williams MD, Sarver DM, Sadowsky PL, Bradley E. Combined rapid
39.
maxillary expansion and protraction facemask in the treatment of Class III
malocclusions in growing children: A prospective long-term study. Semin 26. Ngan PW, Hagg U, Yiu C, Wei SH. Treatment response and longterm
Orthod. 1997;3(4):265-74. dentofacial adaptations to maxillary expansion and protraction. Semin
Orthod. 1997;3(4):255-64.
18. Alcan T, Keles A, Erverdi N. The effects of a modified protraction headgear
on maxilla. Am J Orthod Dentofacial Orthop. 2000;117(1):27-38. 27. Yepes E, Quintero P, Rueda ZM, Pedroze A. Systematic Review Optimal
force for maxillary protraction facemask therapy in the early treatment of
19. Melsen B, Melsen F. The cranial base. The postnatal development of the
Class III malocclusion. Eur J Orthod. 2014;36(5):586-94.
cranial base studied histologically on human autopsy material. Am J
Orthod. 1982;82(4):329-42. 28. Wertz RA. Skeletal and dental changes accompanying rapid midpalatal
suture opening. Am J Orthod Dentofacial Orthop. 1970;58(1):41-66.
20. Ford EHR. Growth of the human cranial base. Am J Orthod.
1958;44(7):498-506. 29. Sarver DM, Johnston MW. Skeletal changes in vertical and anterior
displacement of the maxilla with bonded rapid palatal expansion
21. Scott JH. The cranial base. Am J Phys Anthropol. 1958;16(3):319-48.
appliances. Am J Orthod Dentofacial Orthop. 1989;95(6):462-6.
22. Mermigos J, Full CA, Andreasen G. Protraction of the maxillofacial
30. Yilmaz BS, Kucukkeles N. Skeletal, soft tissue, and airway changes
complex. Am J Orthod Dentofacial Orthop. 1990;98(1):47-55.
following the alternate maxillary expansions and constrictions protocol.
23. Ishii H, Morita S, Takeuchi Y, Nakamura S. Treatment effect of combined Angle Orthod. 2014;84(5):868-77.
maxillary protraction and chin cup appliance in severe skeletal Class III
cases. Am J Orthod Dentofacial Orthop. 1987:92(4);304-12.
24. Takada K, Petachai S, Sakuda M. Changes in dentofacial morphology
in skeletal Class III children treated by a modified maxillary protraction
headgear and a chin cup: A longitudinal cephalometric appraisal. Eur J
Orthod. 1993;15(3):211-21.
Remedy Publications LLC. 6 2017 | Volume 2 | Issue 12 | Article 1078
You might also like
- Effects of Facemask Treatment Anchored With Miniplates After Alternate Rapid Maxillary Expansions and Constrictions A Pilot StudyDocument8 pagesEffects of Facemask Treatment Anchored With Miniplates After Alternate Rapid Maxillary Expansions and Constrictions A Pilot StudyMariana SantosNo ratings yet
- Dentofacial Effects of Two Facemask Therapies For Maxillary Protraction Miniscrew Implants Versus Rapid Maxillary ExpandersDocument9 pagesDentofacial Effects of Two Facemask Therapies For Maxillary Protraction Miniscrew Implants Versus Rapid Maxillary ExpandersMariana SantosNo ratings yet
- Correction of Late Adolescent Skeletal Class III Using The Alt-RAMEC Protocol and Skeletal AnchorageDocument11 pagesCorrection of Late Adolescent Skeletal Class III Using The Alt-RAMEC Protocol and Skeletal AnchoragePorchiddioNo ratings yet
- 1 s2.0 S2666430522000036 MainDocument12 pages1 s2.0 S2666430522000036 MainDANTE DELEGUERYNo ratings yet
- Kaya 2011Document8 pagesKaya 2011ortodoncia 2022No ratings yet
- Benedict Wimes, Mascara FacialDocument8 pagesBenedict Wimes, Mascara FacialjamilistccNo ratings yet
- Rapid Maxillary Expansion Compared To Surgery For Assistance in Maxillary Face Mask ProtractionDocument8 pagesRapid Maxillary Expansion Compared To Surgery For Assistance in Maxillary Face Mask ProtractionMariana SantosNo ratings yet
- Three-Dimensional Evaluation of Hybrid Expander Appliances: A Pilot StudyDocument6 pagesThree-Dimensional Evaluation of Hybrid Expander Appliances: A Pilot Studydruzair007No ratings yet
- 2176 9451 Dpjo 24 05 52Document8 pages2176 9451 Dpjo 24 05 52Crisu CrisuuNo ratings yet
- New Treatment Modality For Maxillary Hypoplasia in Cleft PatientsDocument9 pagesNew Treatment Modality For Maxillary Hypoplasia in Cleft PatientsKaranPadhaNo ratings yet
- Comparison of Root Resorption After Bone-Borne and Tooth-Borne Rapid Maxillary Expansion Evaluated With The Use of MicrotomographyDocument9 pagesComparison of Root Resorption After Bone-Borne and Tooth-Borne Rapid Maxillary Expansion Evaluated With The Use of MicrotomographyMonojit DuttaNo ratings yet
- Yildirim2019 PDFDocument9 pagesYildirim2019 PDFMonojit DuttaNo ratings yet
- Sarah Salah PaperDocument14 pagesSarah Salah PaperdentistsurorNo ratings yet
- Effectiveness of Maxillary Protraction Using A Hybrid Hyrax-Facemask Combination: A Controlled Clinical StudyDocument7 pagesEffectiveness of Maxillary Protraction Using A Hybrid Hyrax-Facemask Combination: A Controlled Clinical StudyKarin UchimaNo ratings yet
- Roll Man 2013Document6 pagesRoll Man 2013SergioNo ratings yet
- 2010-Three Dimensional Analysis of Maxillary Protraction WithDocument22 pages2010-Three Dimensional Analysis of Maxillary Protraction WithMariana SantosNo ratings yet
- ExpansãoDocument4 pagesExpansãoMiguel OcanhaNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMIDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMIAlla MushkeyNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMI PDFDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMI PDFAlla MushkeyNo ratings yet
- ALTRAMECARTICULODocument12 pagesALTRAMECARTICULOAlejandra NietoNo ratings yet
- Angle Orthod. 2012 82 5 846-52Document7 pagesAngle Orthod. 2012 82 5 846-52brookortontiaNo ratings yet
- JCDP 22 1135Document9 pagesJCDP 22 1135Thang Nguyen TienNo ratings yet
- International Journal of Surgery Case Reports: Kanistika Jha, Manoj AdhikariDocument4 pagesInternational Journal of Surgery Case Reports: Kanistika Jha, Manoj AdhikariYeraldin EspañaNo ratings yet
- Tejido Conectivo Implantes Inmediatos y Provisionales 2Document9 pagesTejido Conectivo Implantes Inmediatos y Provisionales 2James Alexander Toruño GordonNo ratings yet
- 2000 J C. H S W A: Udson Ickey Cientific Riting WardDocument6 pages2000 J C. H S W A: Udson Ickey Cientific Riting WardPremshith CpNo ratings yet
- Ajodo 3Document10 pagesAjodo 3ayisNo ratings yet
- Angle Orthod. 2016 86 5 746-52Document7 pagesAngle Orthod. 2016 86 5 746-52brookortontiaNo ratings yet
- Surgically Assisted Rapid Maxillary Expansion Combined With MaxillaryDocument21 pagesSurgically Assisted Rapid Maxillary Expansion Combined With MaxillaryKumar NiwalikarNo ratings yet
- 7 Articulo Bone-Anchored Maxillary Protraction in A Patient With Complete Cleft Lip and Palate: A Case ReportDocument8 pages7 Articulo Bone-Anchored Maxillary Protraction in A Patient With Complete Cleft Lip and Palate: A Case ReportErika NuñezNo ratings yet
- Dentofacial Effects of Modified Alt-RAMEC Protocol Combined With The Facial Mask For Treatment of Preadolescent Caucasian Class III PatientsDocument7 pagesDentofacial Effects of Modified Alt-RAMEC Protocol Combined With The Facial Mask For Treatment of Preadolescent Caucasian Class III PatientsMariana SantosNo ratings yet
- Assessment of Changes in The Nasal Airway After Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansion in Young Adults.Document8 pagesAssessment of Changes in The Nasal Airway After Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansion in Young Adults.Natan GussNo ratings yet
- Maxillary Expansion AppliancesDocument8 pagesMaxillary Expansion Appliancesmotivation munkeyNo ratings yet
- 2020 Article 265Document7 pages2020 Article 265Fabian BarretoNo ratings yet
- Three-Dimensional Soft Tissue Evaluation After Rapid Maxillary Expansion and Mandibular Midline Distraction OsteogenesisDocument7 pagesThree-Dimensional Soft Tissue Evaluation After Rapid Maxillary Expansion and Mandibular Midline Distraction OsteogenesisayisNo ratings yet
- Ajodo 1Document7 pagesAjodo 1ayis100% (1)
- Comparison of Two Protocols For Maxillary Protraction: Bone Anchors Versus Face Mask With Rapid Maxillary ExpansionDocument8 pagesComparison of Two Protocols For Maxillary Protraction: Bone Anchors Versus Face Mask With Rapid Maxillary ExpansionBeatriz ChilenoNo ratings yet
- Borgia Gonzalo, Ravecca Tabaré, Fumero Miriam, Pebé PabloDocument13 pagesBorgia Gonzalo, Ravecca Tabaré, Fumero Miriam, Pebé PabloJaime Angel Ortiz DiazNo ratings yet
- Bong 2011 PDFDocument14 pagesBong 2011 PDFkarenchavezalvanNo ratings yet
- Nonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationDocument11 pagesNonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationNeycer Catpo NuncevayNo ratings yet
- Journal of Surgery and Insights: Transpalatal Distraction As A Method of Maxillary Expansion: A Case ReportDocument4 pagesJournal of Surgery and Insights: Transpalatal Distraction As A Method of Maxillary Expansion: A Case ReportjabbarNo ratings yet
- 2011-Orthopedic Treatment of Class III Malocclusion With Rapid Maxillary Expansion Combined With A Face Mask A Cephalometric Assessment of Craniofacial Growth PatternsDocument7 pages2011-Orthopedic Treatment of Class III Malocclusion With Rapid Maxillary Expansion Combined With A Face Mask A Cephalometric Assessment of Craniofacial Growth PatternsMariana SantosNo ratings yet
- Scientific Dental Journal: Lower Facial Height and Soft Tissue Changes in Bimaxillary Protrusion CasesDocument7 pagesScientific Dental Journal: Lower Facial Height and Soft Tissue Changes in Bimaxillary Protrusion Casesyuni madjidNo ratings yet
- APOSTrendsOrthod 2016 6 4 228 186439 PDFDocument5 pagesAPOSTrendsOrthod 2016 6 4 228 186439 PDFDr sneha HoshingNo ratings yet
- Abbé - EstlanderDocument4 pagesAbbé - EstlanderKoretta Esmeral AtehortúaNo ratings yet
- Angle Orthod. 2015 85 2 284-91Document8 pagesAngle Orthod. 2015 85 2 284-91brookortontiaNo ratings yet
- Treatment Effects After Maxillary Expansion Using Tooth-Borne Vs Tissue-Borne Miniscrew-Assisted Rapid Palatal Expansion ApplianceDocument9 pagesTreatment Effects After Maxillary Expansion Using Tooth-Borne Vs Tissue-Borne Miniscrew-Assisted Rapid Palatal Expansion ApplianceRolando Huaman BravoNo ratings yet
- Lanza 2017Document7 pagesLanza 2017Promocoes PromoNo ratings yet
- Articol PMFDocument6 pagesArticol PMFclaudia lupuNo ratings yet
- Australian Dental Journal: Craniofacial DisordersDocument11 pagesAustralian Dental Journal: Craniofacial DisordersMantili TasrifNo ratings yet
- 2021 Does The Timing of 1-Stage Palatoplasty With Radical Muscle Dissection Effect Long-Term Midface Growth A Single-Center Retrospective AnalysisDocument7 pages2021 Does The Timing of 1-Stage Palatoplasty With Radical Muscle Dissection Effect Long-Term Midface Growth A Single-Center Retrospective AnalysisDimitris RodriguezNo ratings yet
- Alt Ramec - Estructuras DentalesDocument8 pagesAlt Ramec - Estructuras DentalesAna Clara ClaveroNo ratings yet
- Miniscrew-Assisted Rapid Palatal Expansion For Managing Arch Perimeter in An Adult PatientDocument12 pagesMiniscrew-Assisted Rapid Palatal Expansion For Managing Arch Perimeter in An Adult PatientAkash AmbhoreNo ratings yet
- Brandt2013 MDocument4 pagesBrandt2013 MAnkita GuravNo ratings yet
- Maxillary ExpansionDocument8 pagesMaxillary ExpansionJoji IsacNo ratings yet
- Mohammed 2019Document29 pagesMohammed 2019RafailiaNo ratings yet
- Case Report Treatment of An Adult Skeletal Class III Patient With Surgically Assisted Rapid Palatal Expansion and FacemaskDocument7 pagesCase Report Treatment of An Adult Skeletal Class III Patient With Surgically Assisted Rapid Palatal Expansion and FacemaskMirza GlusacNo ratings yet
- Mini-Implant Assisted Rapid Palatal Expansion: New PerspectivesDocument18 pagesMini-Implant Assisted Rapid Palatal Expansion: New PerspectivesKhyati GuptaNo ratings yet
- Maxillary Arch Distalization Using Interradicular Miniscrews and The Lever-Arm ApplianceDocument8 pagesMaxillary Arch Distalization Using Interradicular Miniscrews and The Lever-Arm ApplianceJuan Carlos CárcamoNo ratings yet
- Rapid Maxillary Expansion. Is It Better in The Mixed or in The Permanent Dentition?Document8 pagesRapid Maxillary Expansion. Is It Better in The Mixed or in The Permanent Dentition?Gustavo AnteparraNo ratings yet
- Coating With Zelodronic AcidDocument30 pagesCoating With Zelodronic AcidZaid DewachiNo ratings yet
- NCBIDocument13 pagesNCBIZaid DewachiNo ratings yet
- Study of Erosive Alterations in Dental Enamel Exposed To Medicinal SyrupsDocument3 pagesStudy of Erosive Alterations in Dental Enamel Exposed To Medicinal SyrupsZaid DewachiNo ratings yet
- Non-Surgical Treatment of Class III With Multiloop Edgewise Arch-Wire (MEAW) TherapyDocument22 pagesNon-Surgical Treatment of Class III With Multiloop Edgewise Arch-Wire (MEAW) TherapyZaid DewachiNo ratings yet
- Kjod 48 236Document9 pagesKjod 48 236Zaid DewachiNo ratings yet
- Tjo-29-2-4-91 Very ImportantDocument7 pagesTjo-29-2-4-91 Very ImportantZaid DewachiNo ratings yet
- Luki Gummetal W Ortodoncji 0Document16 pagesLuki Gummetal W Ortodoncji 0Zhiao Liu100% (1)
- Comparative Reliability Assessment of Tooth VolumeDocument12 pagesComparative Reliability Assessment of Tooth VolumeZaid DewachiNo ratings yet
- Straight Wire PIODocument16 pagesStraight Wire PIOZaid DewachiNo ratings yet
- Nackaerts 2014Document10 pagesNackaerts 2014Zaid DewachiNo ratings yet
- Cui ToothNet Automatic Tooth Instance Segmentation and Identification From Cone Beam CVPR 2019 PaperDocument10 pagesCui ToothNet Automatic Tooth Instance Segmentation and Identification From Cone Beam CVPR 2019 PaperZaid DewachiNo ratings yet
- Accuracy of in Vitro Mandibular Volumetric Measurements From CBCT of Different Voxel Sizes With Different Segmentation Threshold SettingsDocument7 pagesAccuracy of in Vitro Mandibular Volumetric Measurements From CBCT of Different Voxel Sizes With Different Segmentation Threshold SettingsZaid DewachiNo ratings yet
- Discuss 3Document7 pagesDiscuss 3Zaid DewachiNo ratings yet
- Ne 2Document7 pagesNe 2Zaid DewachiNo ratings yet
- Enoxaparin - Safe Prescribing - Check It Out 1Document3 pagesEnoxaparin - Safe Prescribing - Check It Out 1Zaid DewachiNo ratings yet
- Drishti Software Installation ManualDocument12 pagesDrishti Software Installation ManualZaid DewachiNo ratings yet
- Relationship Between Midpalatal Suture MaturationDocument6 pagesRelationship Between Midpalatal Suture MaturationZaid DewachiNo ratings yet
- Ne 3Document8 pagesNe 3Zaid DewachiNo ratings yet
- StemcellreviewinorthoDocument13 pagesStemcellreviewinorthoZaid DewachiNo ratings yet
- Skeletal and Dental Considerations in OrthodonticDocument11 pagesSkeletal and Dental Considerations in OrthodonticZaid DewachiNo ratings yet
- Laser Doopler Perfusi̇on İmagerDocument4 pagesLaser Doopler Perfusi̇on İmagerAli ÖzdemirNo ratings yet
- Ofertas Buen Fin SulkaDocument76 pagesOfertas Buen Fin SulkaCarlos QuirozNo ratings yet
- Physical Fitness CertificateDocument1 pagePhysical Fitness CertificateKavisa Ghosh85% (20)
- First Aid ChecklistDocument1 pageFirst Aid ChecklistGopal Choudhary0% (1)
- Ventstar Helix Heated Pi 9102433 enDocument8 pagesVentstar Helix Heated Pi 9102433 enDikka AzizNo ratings yet
- Accredited Colleges of Veterinary Medicine: Section 12.11Document5 pagesAccredited Colleges of Veterinary Medicine: Section 12.11ਰੋਹਿਤ ਬਾਵਾNo ratings yet
- Niva HSL Mediclaim Ghi Gpa Ss v3Document2 pagesNiva HSL Mediclaim Ghi Gpa Ss v3bradburywillsNo ratings yet
- Phar Assignment MR Sim V1.22Document3 pagesPhar Assignment MR Sim V1.22Kristoff Cardenas-RamosNo ratings yet
- CCH210604I83 Recibidas 2021 11 FacturasDocument42 pagesCCH210604I83 Recibidas 2021 11 FacturasAlexis Julian FloresNo ratings yet
- Hemophilia Powerpoint-Kuliah FKIK UNTANDocument33 pagesHemophilia Powerpoint-Kuliah FKIK UNTANAgung TriatmojoNo ratings yet
- Herbs, Laboratories, and RevolDocument15 pagesHerbs, Laboratories, and Revolhung tsung jenNo ratings yet
- DrugDocument90 pagesDrugamalia noviyantiNo ratings yet
- Bumil Anemia KekDocument7 pagesBumil Anemia KekRita WahyuningsihNo ratings yet
- Filehost - Professional English in Use MedicineDocument262 pagesFilehost - Professional English in Use MedicineCosmin Berechet0% (2)
- Taking-Patient-History-British-English-StudentDocument8 pagesTaking-Patient-History-British-English-Studentdr.huongnguyen.geneticsNo ratings yet
- Model Kemitraan Puskesmas-Praktisi Swasta Dalam Penanggulangan Tuberkulosis Paru Di Kecamatan Kalasan, Kabupaten Sleman, Provinsi DiyDocument9 pagesModel Kemitraan Puskesmas-Praktisi Swasta Dalam Penanggulangan Tuberkulosis Paru Di Kecamatan Kalasan, Kabupaten Sleman, Provinsi DiyDesvolim DesoNo ratings yet
- Brosur Pelayanan LaboratoriumDocument1 pageBrosur Pelayanan LaboratoriumChristian OktavianoNo ratings yet
- New Instructor Application: MEDIC FIRST AID International, IncDocument2 pagesNew Instructor Application: MEDIC FIRST AID International, IncjhoniNo ratings yet
- Đề Thi Tuyển Sinh Vào Lớp 10 Chuyên Anh – Trường THPT Chuyên NGUYỄN DU – Năm Học 2015-2016 – LonggleDocument8 pagesĐề Thi Tuyển Sinh Vào Lớp 10 Chuyên Anh – Trường THPT Chuyên NGUYỄN DU – Năm Học 2015-2016 – LongglerolandvietnamNo ratings yet
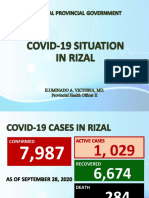
- Covid19 Situation in RizalDocument23 pagesCovid19 Situation in RizalToni Quitalig GamezNo ratings yet
- List of Hospitals Under Bombay Nursing Home Act - Patoda BlockDocument1 pageList of Hospitals Under Bombay Nursing Home Act - Patoda BlockCampaign MediaNo ratings yet
- Dissecting The Opioid Heroin Epidemic To Discover Its Ugly RootsDocument7 pagesDissecting The Opioid Heroin Epidemic To Discover Its Ugly RootsThavamNo ratings yet
- ახალშობილის მოვლაDocument28 pagesახალშობილის მოვლაNino KochuashviliNo ratings yet
- Asia TestDocument7 pagesAsia TestAsheNo ratings yet
- Stent Pricing: S. NO. Stent Discription Cost To Patient CompanyDocument1 pageStent Pricing: S. NO. Stent Discription Cost To Patient CompanyMohammad Ali ImranNo ratings yet
- Periodesasi Judo Herlina GitaDocument6 pagesPeriodesasi Judo Herlina GitaAhmad Al'FredoNo ratings yet
- Madya Visha & MadatyayaDocument33 pagesMadya Visha & Madatyayaraghabendrasahu1998No ratings yet
- Endovive: Enteral Access DevicesDocument16 pagesEndovive: Enteral Access Devicesmarcilene vitorianoNo ratings yet
- Job Application FormDocument3 pagesJob Application Formnrynaybae.iiNo ratings yet
- Menpinmw NCPDocument1 pageMenpinmw NCPLevin MenpinNo ratings yet