Professional Documents
Culture Documents
2007bg 11
Uploaded by
souq alkanzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2007bg 11
Uploaded by
souq alkanzCopyright:
Available Formats
2007 BUYER’S GUIDE
Overview of Endovenous
Thermal Ablation of
Varicose Veins
BY PETER GLOVICZKI, MD; ALESSANDRA PUGGIONI, MD; AND MANJU KALRA, MD
Endovenous interventions have trans- In a recent issue of Endovascular Today, leaders of the
formed the treatment of varicose veins field expressed their opinion of currently used tech-
during the past decade. Interest in mini- niques for varicose veins including RF, EVLT, endove-
mally invasive endovenous thermal abla- nous chemical ablation with ultrasound-guided foam
tion of the saphenous vein has substan- sclerotherapy, as well as the conventional open sur-
tially increased due to multiple reasons. gery of saphenous stripping and high ligation.1 This
Peter Gloviczki
Both radiofrequency ablation (RFA) and article reviews currently used endovenous thermal
endovenous laser therapy (EVLT) can be treatments for saphenous vein ablation in patients
performed as an office procedure; they with varicose veins and presents the most recent
are less invasive and usually less painful results. We also provide an insight of what is on the
than conventional open surgical strip- horizon from the medical industry to improve effica-
ping and appear to be equally as effec- cy, expand indications, and decrease complications of
Alessandra tive. In addition, there is apparent benefit these procedures.
Puggioni of earlier return to work and less tempo-
rary decrease in quality of life. Public ENDOVENOUS THERMAL
awareness of varicose veins and venous ABLATION DEVICES
disease has increased considerably, in The principle of treatment using either RFA or EVLT is
part because of activities of the to inflict direct endovenous thermal damage to the vein
American Venous Forum and the wall resulting in destruction of the intima and collagen
American College of Phlebology, but also denaturation of the media, with eventual fibrotic occlu-
Manju Kalra because of increasing public advertise- sion of the vein. EVLT may also cause thermal damage
ment of minimally invasive techniques by the medical by indirect heating of the vein wall by generation of
industry. Informed patients seeking medical help for intravascular steam bubbles in the venous blood. For
Varicose Veins
aching legs with unsightly veins or venous ulcers EVLT, laser wavelengths from 810 µm to 1,320 µm have
request RFA or EVLT for treatment of venous disease. been used with similar success (Table 1).
TABLE 1. ENDOVENOUS ABLATION DEVICES APPROVED FOR USE IN THE US
Device Name Manufacturer Wavelength (µm)
Laser
EVLT Diomed, Inc. (Andover, MA) 810
Venacure AngioDynamics, Inc. (Queensbury, NY) 810, 980
Medilas D Dornier MedTech (Kennesaw, GA) 940
VariLase Vascular Solutions, Inc. (Minneapolis, MN) 810
CTEV CoolTouch, Inc. (Roseville, CA) 1,320
Pro-V Sciton (Palo Alto, CA) 1,319
Radiofrequency
Closure VNUS Inc. (San Jose, CA) N/A
68 I ENDOVASCULAR TODAY I 2007 BUYER’S GUIDE
2007 BUYER’S GUIDE
TABLE 2. KEY STEPS TO PERFORM ENDOVENOUS INDICATIONS
THERMAL ABLATION OF THE SAPHENOUS VEIN EVLT and RFA are now widely accepted as minimally
invasive percutaneous endovenous techniques for abla-
• Use the micropuncture kit and needle to gain access tion of the great saphenous vein (GSV). They are also
under ultrasound guidance into the saphenous vein used with increasing frequency to treat the small saphe-
in the patient placed in the reversed Trendelenburg nous vein (SSV), accessory saphenous veins, and the per-
position. forating veins. Indications for endovenous ablation are
• Position tip of the catheter in the great saphenous identical to those for surgical high ligation and stripping:
vein 1 cm distal to confluence of the superficial epi- reflux at the saphenofemoral or saphenopopliteal junc-
gastric vein. tion identified on duplex ultrasound in patients with vari-
• Use a single-dose, intraoperative, low-molecular- cose veins or advanced chronic venous insufficiency,
weight heparin for DVT prophylaxis. including venous ulcers. It is prudent to avoid endovenous
• Infiltrate tumescent anesthetic solution (50 mL 1% lido- thermal ablation in patients with large saphenous varices
caine with and 1 mL epinephrine [1:1,000] diluted in 1 L or venous aneurysm located within 2 cm of the saphe-
normal saline) into the saphenous subcompartment. nofemoral junction, or in patients who have the great
• Place the patient in the Trendelenburg position and saphenous vein located immediately under the skin.
check position of the tip of the laser or RF device
with ultrasound immediately before treatment. TECHNIQUE
• Image the vein after treatment, re-treat if needed. Endovenous ablations can be performed as office
• Apply compression bandage from toes to groin with procedures under femoral block and/or local anesthesia,
selective padding over the treated saphenous vein to with minimal discomfort and high patient satisfaction.
optimize local compression. The patient is placed in the reversed Trendelenburg
• Ambulate immediately after surgery. position, and the target vein is accessed percutaneously
• Patients should take nonsteroidal anti-inflammatory under ultrasound guidance at the knee (GSV) or ankle
drug (ibuprofen, 400 mg three times daily po) for 5 days level (SSV) using a micropuncture kit and needle (Table 2).
after therapy to minimize aching and inflammation. A guidewire is inserted into the vein followed by place-
• Perform postoperative ultrasound within 24 to 72 hours. ment of a 5-F sheath.2,3 The laser catheter or RF probe is
introduced through the sheath into the vein and
TABLE 3. RESULTS OF RFA AND EVLT
Investigator, Year Type of No. of Limbs Procedure Follow-Up Total Partial
Study (y) Occlusion (%) Occlusion (%)
Rautio,6 2001 RCT 33 RFA 1 75 26
Lurie,4,5 2003, 2005 RCT 44 RFA 2 89 7
Merchant,26 2002 CS 125 RFA 3 85 4
Pichot,27 2004 CS 65 RFA 2 90 10
Varicose Veins
Merchant,28 2005 CS 55 RFA 5 92
29
Nicolini, 2005 CS 330 RFA 3 75 17
Merchant,8 2005 CS 1,222 RFA 5 87 8
9
Min, 2003 CS 499 EVLT 2 93
Sadick,30 2004 CS 30 EVLT 2 97
Timperman,31 2005 CS 100 EVLT 1 91 4
Puggioni,3 2005 CS 53 RFA <1 94
Puggioni,3 2005 CS 77 EVLT <1 91
Kavuturu,32 2006 CS 66 EVLT 0.75 97 3
Myers,33 2006 CS 396 EVLT 3 80% (95% CI, 69%-87%)
Ravi,34 2006 CS 1,250 EVLT or RF 3 (143 limbs) 100% (GSV) 95% (SSV)
RCT = randomized controlled trial; CS=case series; RFA=radiofrequency ablation; EVLT=endovenous laser therapy; GSV=great saphenous vein; SSV=small saphenous vein.
2007 BUYER’S GUIDE I ENDOVASCULAR TODAY I 69
2007 BUYER’S GUIDE
advanced proximally to the saphenofemoral or EndoVenous Obliteration versus Ligation and Vein
saphenopopliteal junction. When treating the GSV, the Stripping (EVOLVeS), a company-sponsored prospective
tip of the catheter is positioned 1 cm distal to the super- randomized trial, demonstrated a 91% initial occlusion
ficial epigastric vein. For treatment of the SSV, the tip of rate with RFA and a complication rate that was similar in
the probe is positioned 1 cm to 1.5 cm distal to the both groups.4 The study found that postoperative pain
saphenopopliteal junction. The patient is then placed in was significantly less severe, absence from work was short-
the Trendelenburg position, and the vein is emptied by er, and physical function was restored faster after RFA than
elevation and by instillation of perivenous tumescent stripping (Table 3). At 2 years, recurrent varicose veins
anesthetic solution (50 mL 1% lidocaine with and 1 mL epi- were noted in 14% of the RFA group versus 21% in the sur-
nephrine [1:1,000] diluted in 1 L normal saline) into the gical group, with statistically maintained better quality-of-
saphenous subcompartment. The instilled fluid ensures life scores in the RFA group.5 A prospective randomized
good contact of the vein wall with the treating catheter study by Rautio also showed less pain and more rapid
for optimal therapeutic effectiveness; it also provides recovery after RFA versus stripping.6 Hinchliffe randomized
analgesia and a heat sink around the treated vein there- 16 patients with recurrent GSV reflux to RFA and strip-
by decreasing heat-related injury to surrounding tissues ping; RFA was faster, and the pain and bruising score was
and reduces the risk of skin burns and paresthesias. The less after RFA versus stripping.7 The Closure Study Group
vein is then ablated by withdrawing the catheter to a studied more than 1,200 limbs;8 occlusion rates at 1, 2, and
few centimeters above the puncture site. The EVLT 5 years were 87.1%, 88.2%, and 87.2%, respectively (Table
catheter is withdrawn at a rate of 1 to 2 mm/s for the 3). Duplex ultrasound identified 185 limbs with anatomi-
first 10 cm and 2 to 3 mm/s for the remaining distance cal failures, most (70%) due to recanalization of the
to deliver 60 to 70 J/cm using 14 W continuous laser occluded saphenous vein; in 12%, the vein failed to
energy. With RFA, the target temperature is either 85°C occlude initially and never occluded during follow-up,
or 90°C. When 85°C is used, the pullback rate is approxi- whereas in 18%, the treated vein remained occluded, but
mately 2 to 3 cm/min, and when 90°C is used, the pull- an accessory saphenous vein produced reflux.
back rate is commonly 4 cm/min. The pullback rate is less
for treatment of the 4-cm to 5-cm segment of the GSV Endovenous Laser Therapy
closest to the saphenofemoral junction. At the end of Large, single-center experiences with lasers have
the procedure, the saphenous vein is imaged with ultra- achieved 97% to 98% early occlusion rates and have main-
sound to confirm occlusion and absence of thrombus in tained occlusion in 93% of limbs at 3 years, with the
the common femoral or popliteal veins. If a patent seg- majority of recurrences occurring by the first 3 months.9-11
ment is identified, re-treatment is advisable. Direct com- Min recently reported 98% occlusion up to 5 years after
pression of the saphenous vein with pads under the laser treatment of 1,000 limbs.12 In an international registry
compression stocking or elastic bandage is advised. It is that included 5,262 patients, Kabnick et al reported a 96%
important to get the patients ambulatory as soon as early success rate after GSV ablation with the 980-µm
possible. Data to support the routine administration of laser.13 Navarro et al reported a 95% success rate with fol-
thromboprophylaxis with heparin are not available. low-up extending to 4 years; recurrence was due to saphe-
Because we have observed extension of the saphenous nous recanalization and not neovascularization.14
thrombus into the femoral vein, in our practice, a single The success of EVLT has been shown to depend on
Varicose Veins
dose of low-molecular-weight heparin is used routine- the amount of energy delivered, with nonocclusion
ly.2,3 If one prefers selective prophylaxis, it should be and early reopening of the GSV seen more frequently
used for patients with a history of thrombophlebitis, when <70 J/cm laser energy is used for saphenous vein
deep vein thrombosis (DVT), obesity, or in patients occlusion.15,16
older than 50 years of age.3 A systematic review of EVLT was performed by Mundy
et al.17 None of the 13 studies analyzed had an open surgi-
RESULTS cal control group. Occlusion of the GSV and abolition of
Radiofrequency Ablation venous reflux occurred in 87.9% to 100% of limbs, with
The RFA system received Food and Drug Administration low rates of re-treatment and recanalization. The study
(FDA) clearance in March of 1999. As of mid-2006, there concluded that EVLT benefits most patients in the short-
were more than 135,000 RFA procedures performed term, but rates of recanalization, re-treatment, occlusion,
worldwide. The Closure technique (VNUS Inc., San Jose, and reflux may change with longer follow-up and that
CA) is well tolerated with minimal short- and long-term there is a need for a randomized trial of EVLT versus con-
morbidity. The clinical benefits of RFA have been demon- ventional surgery.
strated through randomized clinical studies comparing A recent study by Mekako et al18 compared early quali-
this technique with conventional vein stripping. The ty-of-life outcomes after EVLT and surgery between two
70 I ENDOVASCULAR TODAY I 2007 BUYER’S GUIDE
2007 BUYER’S GUIDE
nonrandomized groups of patients. Seventy patients were Endovascular Working Group registry were recently
in the EVLT group and 62 were in the surgery group. The reported by Kabnick.20 In more than 7,000 limbs treated
quality-of-life scores were significantly better in the EVLT with EVLT in 10 countries, the incidence of bruising was
group at 1 and 6 weeks, but not at 12 weeks. The investi- 75% (2,781 of 3,696), paresthesias occurred in 3% (114 of
gators concluded that EVLT removed the quality-of-life 3,696), thrombophlebitis occurred in 1.87% (69 of 3696),
limitations experienced by patients in the early postopera- skin burns occurred in 0.46% (17 of 3,696), DVT/EHIT
tive period. occurred in 0.27% (10 of 3,696), and PE occurred in 0.023%
(one of 3,696).20
COMPLICATIONS Labrapoulos et al reported on early development of
Major complications after endovenous thermal ablation arteriovenous fistulae in 4.9% of limbs undergoing RFA
of the saphenous veins are rare, but minor complications treatment22; our group has observed the same after
have been reported in 3% to 20% of patients, including EVLT. It is likely that arteriovenous fistulae develop dur-
bruising around the puncture site, bleeding, transient ing the process of recanalization of the organized saphe-
paresthesias, superficial phlebitis, skin burns, or pigmenta- nous thrombus, although heat injury to small arteries in
tion. In the Closure Registry, paresthesia was observed in the vasa vasorum cannot be completely excluded. It is
12.3% (121 of 985 limbs) at 1 week, in 7.3% at 6 months, very likely that arteriovenous neovascularization con-
and in 2.6% at 5 years.8 The incidence of skin burns and tributes to recanalization or recurrence after endove-
paresthesias decreased to less than 1% with increasing nous ablation procedures.22 A rare but severe potential
operator experience and with routine use of tumescent complication of EVLT is a retained foreign body. This
anesthesia.8 complication is extremely rare, and the etiology is
Patients undergoing laser therapy frequently experience unclear. A possible cause is if the probe (RF or laser) is
a tight, pulling sensation in the medial thigh along the pulled back in the sheath and the tip of the sheath is
course of the GSV, due to a mild-to-moderate form of separated by direct heat.
saphenous thrombophlebitis. Because blood is a chro-
mophore for all laser wavelengths used, any blood present INNOVATIONS
in the vein will predispose to thrombosis and throm- As a result of the lessons learned from initial experi-
bophlebitis. ence, a number of changes have been introduced by
Major complications of EVLT include DVT and pul- device manufacturers. The newest addition to the RF
monary embolism (PE). Although both DVT and PE are catheter family, released in early 2006, was the VNUS
rare, extension of thrombus from the saphenous into the Closure RFS Stylet for ultrasound-guided ablation of per-
femoral or popliteal vein has been reported to occur in 0% forating veins. The device has a thermocouple tempera-
to 6% of the patients: in one study by Hingorani, extension ture feedback control to allow controlled, consistent
of thrombus occurred in 16% of the limbs after RFA.19 delivery of thermal energy to the vein wall. The tech-
Kabnick recently introduced the term “endovenous heat- nique is gaining popularity rapidly, and initial experience
induced thrombus” (EHIT).20 The natural history of EHIT is has been satisfactory.
likely more benign than that of a frank DVT; the registry of A second innovation from VNUS is the next genera-
Kabnick identified 16 observed cases with class 2 EHIT tion of RFA systems, the ClosureFast catheter. Recently
(thrombus protruding into the femoral vein and occluding cleared by the FDA, the ClosureFast catheter is expected
Varicose Veins
up to 50% of the lumen). Currently, short-term (2 to 6 to be launched in the first quarter of 2007. This new
weeks) treatment with anticoagulation is recommended catheter eliminates the drawbacks of previous-genera-
to prevent thrombus progression or PE. tion catheters (slow pullback rates, pullback time to
In 77 EVLT procedures, our group measured the median measure, high impedance interruptions, normal saline
distance between the tip of the saphenous vein thrombus
and the common femoral vein (CFV): the median distance
was 9.5 mm (range, -20 mm [protrusion in the CFV] to 50
mm), significantly less in older patients (r2=.12; P=.006).2
Thrombus protruded into the CFV in three limbs after
EVLT (2.3%).3,21 All three patients were treated with antico-
agulation; one underwent placement of a temporary infe-
rior vena cava filter because of a floating thrombus in the
CFV. Duplex scan at 12, 14, and 95 days, respectively,
showed complete resolution of the thrombus in all three
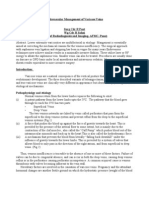
patients. Figure 1. Key comparisons between ClosurePlus and
The rate of complications after EVLT in the International ClosureFast.
72 I ENDOVASCULAR TODAY I 2007 BUYER’S GUIDE
2007 BUYER’S GUIDE
A B C
Figure 2. New Diomed EVLT device (A) with Spotlight sheath (B) and multimedia card (C).
drip) and allows a shorter treatment time. Instead of the a vein wall temperature of 100ºC to 110ºC. The RF gen-
traditional continuous pullback, this device operates erator measures temperature continuously to adjust
with a segmental ablation approach. The catheter is power to the heating element; it detects when the
composed of a 7-F–diameter heating element that has catheter is not in firm contact with the vein wall and the
no expanding electrodes so that one size fits all. The computer advises to apply better compression. It is cru-
catheter can be used with 8-F sheaths and is .025-inch cial to collapse the vein around the catheter using eleva-
guidewire compatible; the device is available in 60-cm tion and perivenous tumescent solution infiltration
and 100-cm lengths. The heating coil is 7 cm long and (Figure 1). Preliminary data provided by the manufactur-
the shaft marks are 6.5 cm apart, providing 0.5 cm treat- er on 70 limbs demonstrate a 98% early occlusion rate
ment overlap. The main difference between ClosureFast and a 100% reflux-free state after an average procedure
and the old Closure system (or EVLT) is that the amount time of 21 minutes. No DVT, skin burn, or phlebitis
of energy does not depend on the speed of pullback and occurred, and 83% of limbs experienced no tenderness
that a long vein segment is treated all at once. With this postoperatively.
device, a 7-cm segment (0.5 cm overlap) can be treated New from Diomed (Andover, MA) is the EVLT
in 20 seconds with set device temperature of 120ºC and Procedure Kit with the Spotlight Sheath and enhanced fea-
tures. The new Spotlight Sheath has an echogenic tip for
enhanced visibility under ultrasound, easy-to-confirm
location determination, and numbered sheath markings to
calculate length of segment treated. The Spotlight Sheath
is available in lengths of 45 cm and 70 cm. The sheath is
made with a new material that has enhanced lubricity and
stiffness to reduce the risk of kinking during insertion.
Further innovations in the new device are the fiber recog-
nition system and the multimedia card. The fiber recogni-
tion system allows the user to program the procedure pre-
sets and activate them upon starting the procedure, while
the multimedia card allows for storage of the digital data
Varicose Veins
from up to 100 treatments. The new EVLT laser generator
itself also appears more compact and lightweight for
portable office use (Figure 2).
The CoolTouch CTEV (CoolTouch, Inc., Roseville, CA) is a
1,320-µm Nd:YAG laser with an absorption length of 300 µm
to 500 µm in tissue. The device obtained FDA clearance for
treatment of both GSV and SSV. The chromophore for this
laser is water (main component of collagen), resulting in a
shorter absorption length than diode lasers. Specific
absorption of energy only by the vein wall and not the
hemoglobin results in a more controlled depth of vein
coagulation. Furthermore, the fiber is coupled with an
automatic pullback device preset at 1 mm/s. Other advan-
tages of this system are the availability of a number of fiber
sizes (600 mm, 273 mm, and the 2.5-F SaphFire
Figure 3. The CoolTouch automatic pullback device. [CoolTouch]) and the disposability of the fibers; each can
74 I ENDOVASCULAR TODAY I 2007 BUYER’S GUIDE
2007 BUYER’S GUIDE
be used up to five times after sterilization. The newly intro- (San Jose, CA); Dan Stempel, Director, EVLT Marketing
duced SaphFire 2.5-F fiber can be inserted through a small- Diomed, Inc., (Andover, MA); and Leslie Newman,
er and less-invasive 4-F microintroducer and, in many CoolTouch, Inc. (Roseville, CA).
instances, can be passed without the need for a sheath; it
1. Elias S, Almeida JI, Gloviczki P, et al. Successful endovenous ablation. Endovasc Today.
travels a tortuous vein with relative ease due to the pro- 2006;5(9):28-40.
tected, smooth tip, it is more echogenic than other fibers, 2. Kalra M, Gloviczki P. Fifteen years ago laser was supposed to open arteries, now it is supposed to
close veins: what is the reality behind the tool? Perspect Vasc Surg Endovasc Ther. 2006;18:3-8.
and has excellent handling characteristics (Figure 3). 3. Puggioni A, Kalra M, Carmo M, et al. Endovenous laser therapy and radiofrequency ablation of
Potential advantages of 1,320-µm wavelength are efficacy the great saphenous vein: analysis of early efficacy and complications. J Vasc Surg. 2005;42:488-
493.
equal to the diode lasers with less damage to the surround- 4. Lurie F, Creton D, Eklof B, et al. Prospective randomized study of endovenous radiofrequency
obliteration (closure procedure) versus ligation and stripping in a selected patient population
ing tissues. Several investigators reported a significant (EVOLVeS Study). J Vasc Surg. 2003;38:207-214.
reduction of pain and bruising with the use of this wave- 5. Lurie F, Creton D, Eklof B, et al. Prospective randomised study of endovenous radiofrequency
obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc
length.23-25 A lack of vein wall perforations may account for Endovasc Surg. 2005;29:67-73.
decreased laser damage of perivenous tissues and 6. Rautio T, Ohinmaa A, Perala J, et al. Endovenous obliteration versus conventional stripping oper-
ation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the
decreased rate of side effects after 1,320-µm laser therapy. costs. J Vasc Surg. 2002;35:958-965.
7. Hinchliffe RJ, Ubhi J, Beech A, et al. A prospective randomized controlled trial of VNUS closure
versus surgery for the treatment of recurrent long saphenous veins. Eur J Vasc Endovasc Surg.
CONCLUSION 2006;31:212-218.
8. Merchant RF, Pichot O. Long-term outcomes of endovenous radiofrequency obliteration of saphe-
The results of case series and registries on endovenous nous reflux as a treatment for superficial venous insufficiency. J Vasc Surg. 2005;42:502-509.
thermal therapy of the incompetent saphenous veins in 9. Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of saphenous vein reflux: long-term
results. J Vasc Interv Radiol. 2003;14:991-996.
patients with varicosity and advanced venous insufficien- 10. Perkowski P, Ravi R, Gowda RC, et al. Endovenous laser ablation of the saphenous vein for treat-
ment of venous insufficiency and varicose veins: early results from a large single-center experience.
cy (some with follow-up data of 5 to 7 years) are reassur- J Endovasc Ther. 2004;11:132-138.
ing, with high occlusion rates, few side effects, and low 11. Bush RG, Shamma HN, Hammond KA. 940-nm laser for treatment of saphenous insufficiency:
histological analysis and long-term follow-up. Photomed Laser Surg. 2005;23:15-19.
recurrence rates. Prospective randomized studies com- 12. Min RJ. Laser ablation of the great saphenous vein: 5-year data. Vascular. 2006;14:S29-30.
paring RFA and stripping demonstrate earlier return to 13. Kabnick LS. Endovenous laser system (980 nm) for the treatment of saphenous vein insuffi-
ciency:7611 limbs. Presented at the ACP 19th annual conference in San Francisco, California,
work, less pain, and improved quality of life after endove- November 10-13, 2005.
14. Navarro L, Min RJ, Bone C. Endovenous laser: a new minimally invasive method of treatment for
nous procedures when compared to open surgery. No varicose veins—preliminary observations using an 810 nm diode laser. Dermatol Surg.
randomized studies are currently available for EVLT. Strict 2001;27:117-122.
15. Proebstle TM, Krummenauer F, Gul D, et al. Nonocclusion and early reopening of the great
adherence to suggested guidelines and progress in tech- saphenous vein after endovenous laser treatment is fluence dependent. Dermatol Surg. 2004;30(2 Pt
nology will further decrease the low incidence of throm- 1):174-178.
16. Timperman PE, Sichlau M, Ryu RK. Greater energy delivery improves treatment success of
botic complication rates, perioperative pain, and pares- endovenous laser treatment of incompetent saphenous veins. J Vasc Interv Radiol. 2004;15:1061-
1063.
thesias. Although these procedures are clearly less inva- 17. Mundy L, Merlin TL, Fitridge RA, et al. Systematic review of endovenous laser treatment for vari-
sive then conventional open surgery, level-1 evidence for cose veins. Br J Surg. 2005;92:1189-1194.
18. Mekako AI, Hatfield J, Bryce J, et al. A nonrandomised controlled trial of endovenous laser ther-
long-term superiority over other techniques used for apy and surgery in the treatment of varicose veins. Ann Vasc Surg. 2006;20:451-457.
treatment of varicose veins is not available. ■ 19. Hingorani AP, Ascher E, Markevich N, et al. Deep venous thrombosis after radiofrequency abla-
tion of greater saphenous vein: a word of caution. J Vasc Surg. 2004;40:500-504.
20. Kabnick LS. Complications of endovenous therapies: statistics and treatments. Vascular.
2006;14:S31-32.
Peter Gloviczki, MD, is from the Division of Vascular 21. Mozes G, Kalra M, Carmo M, et al. Extension of saphenous thrombus into the femoral vein: a
Surgery, Gonda Vascular Center, Mayo Clinic, Rochester, potential complication of new endovenous ablation techniques. J Vasc Surg. 2005;41:130-135.
22. Labropoulos N, Bhatti A, Leon L, et al. Neovascularization after great saphenous vein ablation.
Minnesota. He has disclosed that he holds no financial Eur J Vasc Endovasc Surg. 2006;31:219-222.
interest in any product or manufacturer mentioned herein. 23. Weiss RA, Weiss MA. Controlled radiofrequency endovenous occlusion using a unique
radiofrequency catheter under duplex guidance to eliminate saphenous varicose vein reflux: a 2-year
Varicose Veins
Dr. Gloviczki may be reached at (507) 284-3407; follow-up. Dermatol Surg. 2002;28:38-42.
24. Proebstle TM, Moehler T, Gul D, et al. Endovenous treatment of the great saphenous vein using
gloviczki.peter@mayo.edu. a 1,320 nm Nd:YAG laser causes fewer side effects than using a 940 nm diode laser. Dermatol Surg.
Alessandra Puggioni, MD, is from Maimonides Medical 2005;31:1678-1683; discussion 1683-1684.
25. Goldman MP, Mauricio M, Rao J. Intravascular 1320-nm laser closure of the great saphenous
Center, Brooklyn, New York. She has disclosed that she vein: a 6- to 12-month follow-up study. Dermatol Surg. 2004;30:1380-1385.
holds no financial interest in any product or manufacturer 26. Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux a multi-
center study. J Vasc Surg. 2002;35:1190-1196.
mentioned herein. Dr. Puggioni may be reached at (718) 27. Pichot O, Kabnick LS, Creton D, et al. Duplex ultrasound scan findings two years after great
saphenous vein radiofrequency endovenous obliteration. J Vasc Surg. 2004;39:189-195.
283-7957; apuggioni@maimonidesmed.org. 28. Merchant RF, Pichot O, Myers KA. Four-year follow-up on endovascular radiofrequency oblitera-
Manju Kalra, MD, is from the Division of Vascular tion of great saphenous reflux. Dermatol Surg. 2005;31:129-134.
29. Nicolini P, Closure Group. Treatment of primary varicose veins by endovenous obliteration with
Surgery, Gonda Vascular Center, Mayo Clinic, Rochester, the VNUS closure system: results of a prospective multicentre study. Eur J Vasc Endovasc Surg.
Minnesota She has disclosed that she holds no financial 2005;29:433-439.
30. Sadick NS, Wasser S. Combined endovascular laser with ambulatory phlebectomy for the treat-
interest in any product or manufacturer mentioned herein. ment of superficial venous incompetence: a 2-year perspective. J Cosmet Laser Ther. 2004;6:44-49.
31. Timperman PE. Prospective evaluation of higher energy great saphenous vein endovenous laser
Dr. Kalra may be reached at (507) 284-3407; treatment. J Vasc Interv Radiol. 2005;16:791-794.
kalra.manju@mayo.edu. 32. Kavuturu S, Girishkumar H, Ehrlich F. Endovenous laser ablation of saphenous vein is an effec-
tive treatment modality for lower extremity varicose veins. Am Surg. 2006;72:672-675.
33. Myers K, Fris R, Jolley D. Treatment of varicose veins by endovenous laser therapy: assessment
The authors acknowledge Brian Farley, President and of results by ultrasound surveillance. Med J Austral. 2006;185:199-202.
34. Ravi R, Rodriguez-Lopez JA, Trayler EA, et al. Endovenous ablation of incompetent saphenous
Chief Executive Officer VNUS Medical Technologies, Inc. veins: a large single-center experience. J Endovasc Ther. 2006;13:244-248.
76 I ENDOVASCULAR TODAY I 2007 BUYER’S GUIDE
You might also like
- Indiabulls PILDocument64 pagesIndiabulls PILPGurus100% (1)
- Applying The WALANT Technique To Surgical Treatment of Distal Radius FracturesDocument6 pagesApplying The WALANT Technique To Surgical Treatment of Distal Radius Fracturesdaniel saucedoNo ratings yet
- Quiz 1 - Domain Modeling With Answer KeyDocument5 pagesQuiz 1 - Domain Modeling With Answer Keyprincess100267% (3)
- 2010 01 19 - 14 18 57 - VV - Flyer PDFDocument1 page2010 01 19 - 14 18 57 - VV - Flyer PDFAstro LogicalNo ratings yet
- Ulcera EndovascDocument4 pagesUlcera EndovascGustavo DolinskyNo ratings yet
- EJVES VF Watanabe April 2020Document4 pagesEJVES VF Watanabe April 2020Francisco Álvarez MarcosNo ratings yet
- Varicose Veins Endovenous Laser TreatmentDocument17 pagesVaricose Veins Endovenous Laser TreatmentaillNo ratings yet
- Varicose Vein Treatment Tips and Trick - Ablation or GlueDocument30 pagesVaricose Vein Treatment Tips and Trick - Ablation or GlueNata NakamuraNo ratings yet
- Radiofrequency Ablation Therapy For Varicose VeinsDocument7 pagesRadiofrequency Ablation Therapy For Varicose VeinsFauziah Nurul LailiNo ratings yet
- Endovenous Laser Treatment of Varicose Veins EVLTDocument18 pagesEndovenous Laser Treatment of Varicose Veins EVLTCTAFDocuments100% (1)
- JDattaMegheInstMedSciUniv162235-4959576 134635Document5 pagesJDattaMegheInstMedSciUniv162235-4959576 134635shyampanga2No ratings yet
- Randomized Foam TrialDocument10 pagesRandomized Foam TrialrachiddellarNo ratings yet
- Randomized Clinical Trial of Mechanochemical and Endovenous Thermal Ablation of Great Saphenous Varicose VeinsDocument7 pagesRandomized Clinical Trial of Mechanochemical and Endovenous Thermal Ablation of Great Saphenous Varicose VeinsAmade DeaNo ratings yet
- Articulo en InglesDocument4 pagesArticulo en InglesNatalia Gonzalez PerezNo ratings yet
- Lessons Learned After 366 Thermoablated VeinsDocument5 pagesLessons Learned After 366 Thermoablated VeinsAlexandre Campos Moraes AmatoNo ratings yet
- Ajum 13 37Document9 pagesAjum 13 37Nurhanief KamalNo ratings yet
- NCMA113 - Finals LABORATORY Part 2Document9 pagesNCMA113 - Finals LABORATORY Part 2KYLE MITZIE SENGCONo ratings yet
- Standard Varicose Vein Surgery: J M T PerkinsDocument8 pagesStandard Varicose Vein Surgery: J M T PerkinsimherestudyingNo ratings yet
- Us Guided Upper Limb BlocksDocument5 pagesUs Guided Upper Limb BlockskeerthiNo ratings yet
- Lnvaginated Axial Stripping and Stab Avulsion (Hook) Phlebectomy: A Definitive Outpatient Procedure For Primary Varicose VeinsDocument9 pagesLnvaginated Axial Stripping and Stab Avulsion (Hook) Phlebectomy: A Definitive Outpatient Procedure For Primary Varicose VeinsAbrar SabawiNo ratings yet
- Multi-Case Review of Various Applications of Vascular Plugs in Embolization of High Flow Vascular LesionsDocument8 pagesMulti-Case Review of Various Applications of Vascular Plugs in Embolization of High Flow Vascular LesionsBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Endoscopic Versus No-Touch'' Saphenous Vein Harvesting For Coronary Artery Bypass Grafting: A Trade-Off Between Wound Healing and Graft PatencyDocument13 pagesEndoscopic Versus No-Touch'' Saphenous Vein Harvesting For Coronary Artery Bypass Grafting: A Trade-Off Between Wound Healing and Graft PatencyMissing ManNo ratings yet
- 2013 Phlebology EliasDocument5 pages2013 Phlebology EliasronnyNo ratings yet
- AAOS Paperchapter With Jupiter and AmadioDocument11 pagesAAOS Paperchapter With Jupiter and AmadioreyNo ratings yet
- Khairy 2017Document7 pagesKhairy 2017Beby Dwi Lestari BajryNo ratings yet
- Aneurysmorrhaphy (Eng)Document14 pagesAneurysmorrhaphy (Eng)Harlan IdrisNo ratings yet
- Peripheral Intravenous Cannulation 2Document4 pagesPeripheral Intravenous Cannulation 2valecharapova11No ratings yet
- AnnCardAnaesth15154-6423638 175036Document10 pagesAnnCardAnaesth15154-6423638 175036ElenaCondratscribdNo ratings yet
- Endovasc VV MXDocument9 pagesEndovasc VV MXdrrochanNo ratings yet
- Kjtcs043 06 09Document7 pagesKjtcs043 06 09정윤형No ratings yet
- The Clinical Outcomes of Endovenous Microwave and Laser Ablation For Varicose VeinsDocument6 pagesThe Clinical Outcomes of Endovenous Microwave and Laser Ablation For Varicose VeinsMalekseuofi مالك السيوفيNo ratings yet
- Malgor 2013Document4 pagesMalgor 2013vas25No ratings yet
- AVF NewDocument81 pagesAVF NewBasit AliNo ratings yet
- Endovenous Laser Treatment of Saphenous Vein Reflux: Long-Term ResultsDocument6 pagesEndovenous Laser Treatment of Saphenous Vein Reflux: Long-Term ResultsOberdan Duarte da SilvaNo ratings yet
- Technology Assessment Status Evaluation Endoscopic Band Ligation of VaricesDocument3 pagesTechnology Assessment Status Evaluation Endoscopic Band Ligation of VaricesElmer PalaciosNo ratings yet
- 0068KJR - KJR 12 481Document6 pages0068KJR - KJR 12 481Indra dig DrNo ratings yet
- Iranjradiol 14 03 21742Document5 pagesIranjradiol 14 03 21742AisahNo ratings yet
- Nasser Et Al. - 2013 - Use of Transoesophageal Echocardiography in Endovascular Stenting For Superior Vena Cava SyndromeDocument3 pagesNasser Et Al. - 2013 - Use of Transoesophageal Echocardiography in Endovascular Stenting For Superior Vena Cava SyndromeflashjetNo ratings yet
- Shaggy 18Document2 pagesShaggy 18Eghet SilviuNo ratings yet
- Multimodal Tretment of Intracranial Aneurysm: A. Chiriac, I. Poeata, J. Baldauf, H.W. SchroederDocument10 pagesMultimodal Tretment of Intracranial Aneurysm: A. Chiriac, I. Poeata, J. Baldauf, H.W. SchroederApryana Damayanti ARNo ratings yet
- Dural Arteriovenous Fistulas: A Review of The Literature and A Presentation of A Single Institution's ExperienceDocument9 pagesDural Arteriovenous Fistulas: A Review of The Literature and A Presentation of A Single Institution's Experiencejan lester LaingoNo ratings yet
- Varicose Vein TreatmentDocument22 pagesVaricose Vein TreatmentRavi GuptaNo ratings yet
- 23824-Brain AVM With OnyxDocument6 pages23824-Brain AVM With OnyxCut FadmalaNo ratings yet
- Solid-State Mid-Infrared Laser Facilitated Coronary Angioplasty: Clinical and Quantitative Coronary AngiographicDocument13 pagesSolid-State Mid-Infrared Laser Facilitated Coronary Angioplasty: Clinical and Quantitative Coronary Angiographicfriiday.qNo ratings yet
- (10920684 - Neurosurgical Focus) Transvenous Embolization of Brain Arteriovenous Malformations - A Review of Techniques, Indications, and OutcomesDocument7 pages(10920684 - Neurosurgical Focus) Transvenous Embolization of Brain Arteriovenous Malformations - A Review of Techniques, Indications, and Outcomesns52h22pvzNo ratings yet
- Endovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and LimitationsDocument10 pagesEndovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and Limitationsafso afsoNo ratings yet
- Varicose Veins of The Lower Extremities Treatment ForDocument17 pagesVaricose Veins of The Lower Extremities Treatment ForsalinasjulioNo ratings yet
- The Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionDocument10 pagesThe Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionRobert ChristevenNo ratings yet
- Ecmo Cannula Size JournalDocument9 pagesEcmo Cannula Size Journalbreaking nurseNo ratings yet
- Outcomes After Onyx Embolization As Primary Treatment For Cranial Dural Arteriovenous Fistula in The Past DecadeDocument9 pagesOutcomes After Onyx Embolization As Primary Treatment For Cranial Dural Arteriovenous Fistula in The Past DecadeRafika Ayu NadiaNo ratings yet
- White 2015Document6 pagesWhite 2015Muhammad AdithiaNo ratings yet
- Supratentorial Arteriovenous MalformationsDocument4 pagesSupratentorial Arteriovenous MalformationsMorteza Mazloom Farsi BafNo ratings yet
- Ophthalmology 8 1079Document3 pagesOphthalmology 8 1079Raúl Plasencia SaliniNo ratings yet
- In-Human Robot-Assisted Retinal Vein Cannulation, A World FirstDocument10 pagesIn-Human Robot-Assisted Retinal Vein Cannulation, A World Firstjhorman bulaNo ratings yet
- Cobb - Endoscopic Carpal Tunnel ReleaseDocument8 pagesCobb - Endoscopic Carpal Tunnel ReleaseJohnny WangNo ratings yet
- Endovenous Radiofrequency Ablation of The Saphenous Vein The VNUS Closure ProcedureDocument26 pagesEndovenous Radiofrequency Ablation of The Saphenous Vein The VNUS Closure ProcedureMichael ChandraNo ratings yet
- Comerota 2010Document5 pagesComerota 2010Jade GomitaNo ratings yet
- Diagnosis and Treatment of Radiation ProctitisDocument2 pagesDiagnosis and Treatment of Radiation ProctitispatNo ratings yet
- Rosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NerveDocument4 pagesRosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NervedanielpohlmanNo ratings yet
- Computer-Assisted Transcatheter Heart Valve Implantation in Valve-in-Valve ProceduresDocument8 pagesComputer-Assisted Transcatheter Heart Valve Implantation in Valve-in-Valve ProceduresrédaNo ratings yet
- Decoding Cardiac Electrophysiology: Understanding the Techniques and Defining the JargonFrom EverandDecoding Cardiac Electrophysiology: Understanding the Techniques and Defining the JargonAfzal SohaibNo ratings yet
- Materi Basic Safety #1Document32 pagesMateri Basic Safety #1Galih indrahutama100% (1)
- FFA Test CHP INV and 16Document8 pagesFFA Test CHP INV and 16zainabNo ratings yet
- 2008 Almocera vs. OngDocument11 pages2008 Almocera vs. OngErika C. DizonNo ratings yet
- 14.quality of Life in Patients With Recurrent AphthousDocument7 pages14.quality of Life in Patients With Recurrent AphthousCoste Iulia RoxanaNo ratings yet
- Rules and Regulations Governing Private Schools in Basic Education - Part 2Document103 pagesRules and Regulations Governing Private Schools in Basic Education - Part 2Jessah SuarezNo ratings yet
- FINA 3780 Chapter 6Document33 pagesFINA 3780 Chapter 6roBinNo ratings yet
- Topic: Matrix Addition and SubtractionDocument6 pagesTopic: Matrix Addition and SubtractionAnonyNo ratings yet
- Lua ApiDocument176 pagesLua Apiyaotl albores tecuautzinNo ratings yet
- Soal Dan Jawaban Audit IIDocument22 pagesSoal Dan Jawaban Audit IIsantaulinasitorusNo ratings yet
- Is Your Money Safe With Builders Indulging in Criminal Disreputation Management - Story of Navin Raheja & Raheja Developers in GurgaonDocument44 pagesIs Your Money Safe With Builders Indulging in Criminal Disreputation Management - Story of Navin Raheja & Raheja Developers in Gurgaonqubrex1No ratings yet
- Raghad Kamel's ResumeDocument7 pagesRaghad Kamel's ResumeMostafa Mohamed GamalNo ratings yet
- MT7605B DSDocument7 pagesMT7605B DSVishal dtuNo ratings yet
- Complaint - Burhans & Rivera v. State of New York PDFDocument34 pagesComplaint - Burhans & Rivera v. State of New York PDFpospislawNo ratings yet
- Lesson 2. WHAT IS AGROTECHNOPRENEURSHIPDocument23 pagesLesson 2. WHAT IS AGROTECHNOPRENEURSHIPRhea Jane DugadugaNo ratings yet
- United States v. Lavaris Perry, 4th Cir. (2014)Document3 pagesUnited States v. Lavaris Perry, 4th Cir. (2014)Scribd Government DocsNo ratings yet
- Economics: PAPER 1 Multiple ChoiceDocument12 pagesEconomics: PAPER 1 Multiple ChoiceigcsepapersNo ratings yet
- Financial Ratio Analysis FormulasDocument4 pagesFinancial Ratio Analysis FormulasVaishali Jhaveri100% (1)
- C&DS Lab Manual UpdatedDocument182 pagesC&DS Lab Manual UpdatedJesmin MostafaNo ratings yet
- Krishna Yadav Cell#+91-9540308010: BjectiveDocument6 pagesKrishna Yadav Cell#+91-9540308010: BjectiveIssac JohnNo ratings yet
- GSM Controlled RobotDocument33 pagesGSM Controlled RobotAbhishek KunalNo ratings yet
- HboDocument126 pagesHboKunal ChaudhryNo ratings yet
- k90mcc6 PDFDocument381 pagesk90mcc6 PDFTammy JohnsonNo ratings yet
- Plewa2016 - Reputation in Higher Education: A Fuzzy Set Analysis of Resource ConfigurationsDocument9 pagesPlewa2016 - Reputation in Higher Education: A Fuzzy Set Analysis of Resource ConfigurationsAlice ChenNo ratings yet
- JD Data Analyst CapgeminiDocument2 pagesJD Data Analyst CapgeminiShivansh KansalNo ratings yet
- Forging 2Document17 pagesForging 2Amin ShafanezhadNo ratings yet
- 2019 - All Heads of Bureaus & Offices - Disconnection of Old Dti Telephone Lines - 64562Document8 pages2019 - All Heads of Bureaus & Offices - Disconnection of Old Dti Telephone Lines - 64562dannalauraNo ratings yet
- Full Download Test Bank For Accounting Information Systems Hall 8th Edition PDF Full ChapterDocument36 pagesFull Download Test Bank For Accounting Information Systems Hall 8th Edition PDF Full Chapterfluiditytrenail7c8j100% (16)
- Cryo CarDocument21 pagesCryo CarAnup PatilNo ratings yet