Professional Documents
Culture Documents
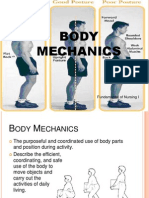
Body Mechanics
Uploaded by
Janelle LasalaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Body Mechanics
Uploaded by
Janelle LasalaCopyright:
Available Formats
BODY MECHANICS BASE OF SUPPORT – An are on which an object rests.
The feet are the base of support when a person is in
Is the efficient, coordinated and safe use of the body standing position.
to produce motion and maintain balance during
activities. THINGS TO CONSIDER BY THE NURSE WHEN
Essential to both clients and nurses to prevent strain, MOVING CLIENTS AND OBJECTS
injury and fatigue.
LEVER – a rigid piece that transmit or modify motion
PURPOSES or force
FORCE – The energy or power required to accomplish
It facilitates safe and efficient use of the appropriate movement
groups of muscles. FRICTION – Force that opposes the motion of an
It reduces the energy required to move and maintain object as it is slid.
balance. FULCRUM – a fixed point at which a lever moves.
It reduces fatigue. When a person moves, the center of gravity shifts
To prevent or decrease the risk of strain, injury and continuously in the direction of the moving body
fatigue for both nurses and clients. parts. Balance depends on the interrelationship of the
NEW RESEARCH ON BODY MECHANICS center of gravity, the line of the gravity, and the
base of support.
Training nurses in body mechanics alone will not The closer the line of gravity is to the center of the
prevent job-relation injuries. base of support, the greater the person’s stability.
Back belts are like not effective in reducing back The closer the line of gravity is to the edge of the
injury. base of support, the more precarious the balance.
Nurses who are physically fit are at no less risk of If the line of gravity falls outside the base of support,
injury. the person falls.
The average nurse should not lift more than 51 The broader the base of support and the lower the
pounds and only under very controlled center of gravity, the greater the stability and
circumstances. balance.
Nurses are encourage to support “NO MANUAL LIFT” o By widening the base of support
and “NO SOLO LIFT” policies. In their work places. o Lowering the center of gravity, bringing it
Long term benefits of proper equipment (mechanical closer to the base of support.
lifts) far outweigh cost related to injuries. The base of support is easily widened by spreading
the feet farther apart.
Staff will use equipment when they participate in the
decision-making process for purchasing the Two movements to avoid because of their potential:
equipment. TWISTING and STOOPING
Undesirable twisting of the back can be prevented by
CONCEPT squarely facing the direction of movement, whether
pushing, pulling or sliding, and moving the objects
GRAVITY – Force that pulls objects towards the
directly toward or away from one’s center of gravity.
center of the earth.
CENTER OF GRAVITY – Point at which the mass of an LIFTING
object is centered.
o That is, the COG of a standing person is the Nurses should not lift more than 51 pounds without
center of the pelvis and about halfway assistance from proper equipment and/ or persons.
between the umbilicus and the pubic bone. It’s always necessary to us proper body mechanics,
BALANCE – Steady weight of the person even though they do not guarantee freedom from
LINE OF GRAVITY – Imaginary vertical line that passes injury.
through the center of gravity When a person lifts or carries an object, a suitcase,
o That is, the LOG in a standing person is a the weight of an object becomes part of the person’s
straight line from the head to the feet body weight.
through the center of the body.
The weight affects the location of the person’s center 8. Before moving an object, contract your gluteal,
of gravity, which is displaced in the direction of the abdominal, leg, and arm muscles to prepare them for
added weight. action.
To counteract this potential imbalance, body parts 9. Avoid working against gravity. Pull, push, roll, or turn
(arm and trunk) move in a direction away from the objects instead of lifting them.
weight. In this way, the center of gravity is 10. Use your gluteal and leg muscles rather than
maintained over the base of support. sacrospinal muscles of your back to exert an upward
By holding the lifted object as close as possible to the thrust when lifting.
body’s center of gravity, the lifter avoids undue 11. Distribute the workload between both arms and legs
displacement of the center of gravity and achieves to prevent back strain.
greater stability. 12. When pushing an object, enlarge the base of support
by moving the front foot forward.
PIVOTING 13. When pulling an object, enlarge the base of support
by either moving the rear leg back facing away from
A technique in which the body is turned in a way that
the object.
avoids twisting of the spine.
14. When moving or carrying objects, hold them as close
To pivot, place one foot ahead of the other, raise the as possible to your center of gravity.
heels very slightly and put the weight of the body on 15. Use the weight of the body as a force for pulling or
the balls of the feet. pushing, by rocking on the feet or leaning forward or
Keeping the body aligned, turn about 90 degrees in backward.
the desired position. The foot that was forward will 16. Alternate rest periods with periods of muscles to
now be behind. help prevent fatigue.
GUIDELINES TO PROPER BODY MECHANICS
1. Plan the move or transfer carefully. Free the
surrounding area of obstacle and move required
equipment near the head or foot of the bed.
2. Obtain the assistance of other people or use
mechanical devices to move objects that are too
heavy. Encourage client to assist as much as possible
by pushing or pulling themselves to reduce muscular
effort.
3. Adjust the working area to waist level, and keep the
body close to the area. Elevate adjustable beds and
overbed tables or lower the side rails of beds to
prevent stretching and reaching.
4. Provide a firm, smooth dry bed foundation before
moving a client in bed or use a pull sheet.
5. Always face the direction of the movement.
6. Start any body movement with proper alignment.
Stand as close as possible to the object to be moved.
Avoid stretching, reaching, and twisting, which may
place the line of gravity outside the base of support.
7. Before moving an object, increase your stability by
widening your stance and flexing your knees, hips and
ankles
Common or Concerning Symptoms of the Neck Palpate in sequence the following nodes:
Swollen Lymph nodes 1. Preauricular in front of the ear
Enlarged Thyroid Glands 2. Posterior auricular – superficial to the mastoid
Hoarseness process
3. Occipital – at the base of the skull posteriorly
Ask “Have you noticed any swollen glands or lump in the 4. Tonsillar – at the angle of the mandible
neck?” 5. Submandibular – midway between the angle and the
Onset: When was you first notice it? tip of the mandible. These nodes are usually smaller
Location: How long have you had the lump? and smoother than the lobulated submandibular
Duration: How long have you had the lump? glands against which they lie
6. Submental – in the midline a few centimeters behind
Characteristics symptoms: Size, tenderness, drainage,
the tip of the mandible
shape, consistency, change in size
7. Superficial cervical – superficial to the sternomastoid
Associated Manifestations: Ask for difficulty of
8. Posterior cervical – along the anterior edge of the
swallowing, any recent infection, trauma, radiotion,
trapezius
surgery, history of smoking, drinking alcohol, chewing
9. Deep cervical chain – deep to the sternomastoid and
tobacco?
often inaccessible to examination. Hook thumb and
Relieving factor: Ask if anything makes the lump
fingers around either side of the sternomastoid
smaller
muscle to find them.
Treatment: Ask for any treatment or if have been to
10. Supraclavicular – deep in the angle formed by the
health care provider
clavicle and the sternomastoid
THYROID GLAND
Assess thyroid function and any evidence on enlarged
thyroid gland
To evaluate thyroid function: Ask about temperature
intolerance or sweating
o Ask for the preferred weather, hot or cold?
o Ask if they perspire more or less than others
o Ask for palpitations and change in weight
With goiter thyroid function may be increased,
decreased or normal
Intolerance to cold, preference for warm clothing and
decreased sweating suggest Hypothyroidism
The opposite symptoms, palpitations and involuntary
weight loss suggest Hyperthyroidism
PHYSICAL EXAMINATION OF THE NECK TRACHEA
Inspect for
Observe the skin, note for its color, pigmentation, any
texture, thickness, hair distribution, and any lesions deviation
Inspect and note for asymmetry, any mass or scars from the
Look for enlargement of the parotid or usual
submandibular glands and any visible lymph nodes. midline
Palpate the lymph nodes - using the pads of the index position
and middle fingers, move the skin over the underlying Feel for any
tissues in each area in circular motion deviation
Patient should be relax, with neck flexed slightly Place finger
forward and if needed slightly toward the side of along one
being examined. side of the
trachea and note the space between it and Displace the trachea to the right with fingers of the
sternomastoid left hand; with the right hand finger, palpate laterally
The space should be symmetric for the right lobe of the thyroid in the space between
the displaced trachea and the relaxed sternomastoid.
Then examine the left.
Note the size, shape, and consistency of the gland
and identify any nodules or tenderness.
They are harder to feel than the isthmus.
HYPERTHYROIDISM HYPOTHYROIDISM
Symptoms: Symptoms:
Nervousness Fatigue, lethargy
Weight loss despite Modest weight gain
increased appetite with anorexia
Excessive sweating Dry, coarse skin and
and heat intolerance cold intolerance
Palpitations Swelling of face,
THYROID GLAND
Frequent BM hands and legs
Inspect the neck for thyroid gland Muscular weakness of Constipation
Tilt patients head back a bit and inspect the region the proximal type and Weakness, muscle
below the cricoid cartilage tremor cramps, arthralgia,
Ask the patient to swallow and watch for the most paresthesia, impaired
memory and hearing
important physical sign – a thyroid gland moves up
during deglutition.
Signs: Signs:
This us due to the fact that thyroid gland is fixed to
Warm, smooth, moist Dry, coarse, cool skin,
the larynx
skin with nonpitting
Such movement of the thyroid becomes greatly With Grave’s disease, edema and loss of
limited when it is fixed by an inflammation or eye signs such as hair
malignant infiltration. stare, lid lag and Periorbital puffiness
The thyroid cartilage, cricoid cartilage, and thyroid exophthalmos Decreased systolic
gland all rise with swallowing and then fall to their Increased systolic and and increased
resting position. decreased diastolic diastolic pressure
pressure Bradycardia, in late
Tachycardia or atrial stage hypothermia
fibrillation Impaired memory,
Tremor and proximal mixed hearing loss,
muscle weakness peripheral neuropathy
STEPS FOR PALPATION OF THE THYROID GLAND
Ask the patient to flex the neck slightly forward to
relax the sternomastoid muscles
Place the fingers of both hands on the patient’s neck CULTURE AND ETHINICITY Assessment
so that the index fingers are just below the cricoid
cartilage Definition of Culture
Ask the patient to sip and swallow water. Feel for the
thyroid isthmus rising up under the finger pads
Purnell & Paulanka – “The totality of socially 3. To assess the client’s health relative to disease
transmitted behavioral patterns, arts, beliefs, values, prevalent in specific cultural group
customs, lifeways and all other products of human
work and thought characteristics of a population of
CULTURAL BELIEFS AND VALUES TO ASSESS
people that guide their worldview and decision Value orientation – principles of what values and
The system shared ideas, rules and meanings that behaviors are considered right or wrong by a group or
influence how we view the world, experience it an individual
emotionally, and behave in relation to other people Beliefs about human nature – natural way of thinking,
PATIENTS do not live in isolation… they are part of feeling and acting of a person
families, communities, cultures, race and countries Beliefs about purpose of life
Nurses must assess them in context of this Beliefs about health, illness and healing – health care
background to fully understand them. beliefs, causes of illness, culture-based treatments
CULTURE determines interpersonal communication Beliefs about what causes disease
style, as well as health beliefs, values and practices Beliefs about health care – pregnancy and
childbearing, blood products, transfusions and organ
ASPECT OF CULTURE RELEVANT TO HEALTH
donation, diet and nutrition, death rituals
ASSESSMENT
Beliefs about who serves in the role of healer or what
1. Communication and language practices brings about the healing
2. Kinship and social networks Beliefs about the meaning of suffering and pain
3. Educational background and learning style
4. Nutrition
SPIRITUALITY AND RELIGIOUS PRACTICE
5. Child-bearing and child-rearing practices Assessment
6. High risk behavior Spirituality and religion are important factors in
7. Health Care beliefs and practices health and can influence health decision and
8. Health Care practitioners outcomes
9. Spirituality
TERMS RELATED TO SPIRITUALITY
CULTURAL HUMILITY: another approach for caring for
patients from culturally diverse backgrounds. RELIGION: rituals, practices, and experiences involving a
search for the sacred that are shared within a group
A process that requires humility as individuals
continually engage in self- reflection and self- critique Characteristics:
as lifelong learners and reflective practitioners
Formal
THREE DIMENSIONS OF CULTURAL HUMILITY Organized
Group oriented
a. Self-awareness: learn about your own biases Ritualistic
b. Respectful communication: work to eliminate Objective
assumptions about what is “normal” ; learn directly
from your patient – they are experts on their culture SPIRITUALITY: a search for meaning and purpose in
and illness life, which seek to understand life’s ultimate
c. Collaborative partnership: build your patients questions in relation to the sacred
respect and mutually acceptable plans
Characteristics:
CULTURAL ASSESSMENT
Informal
Purpose and Scope No organized
Self-reflective
1. To learn about the client’s beliefs and usual behaviors
May involve spiritual experience
associated with health and illness
2. To compare and contrast the client’s beliefs and Subjective
practices to standard health care
SPIRITUAL ASSESSMENT: active and ongoing What lifestyle activities or practices does your religion
conversation that assesses the spiritual needs of the encourage, discouraged or forbid?
client What meaning does these practices and restrictions
have for you?
Characteristics:
To what extent have you followed these guidelines
Formal or informal
I – Implication for Medical Care
Respectful
Nonbiased Are there specific elements of medical care that your
religion discourages or forbids? To what extent have
SPIRITUAL CARE: addressing the spiritual needs of the
you followed these guidelines?
client as they unfold through spiritual assessment
What aspect of your religion would you like me to
Characteristics: keep in mind as I care for you?
What knowledge or understanding would strengthen
Individualized
our relationship as nurse and patient?
Client oriented
Are there barriers to our relationship based on
Collaborative
religious or spiritual issues?
TAKING SPIRITUAL HISTORY (S.P.I.R.I.T) Would you like to discuss religious implications of
health care?
S – Spiritual Belief System
T – Terminal Events Planning
Do you have a formal religious affiliation? Can you
describe it? Are there particular aspects of medical care that you
Do you have spiritual life that is important to you? wish to forgo or have withheld because of your
What is your clearest sense of meaning of your life at spirituality?
this time? Are there religious practices or rituals that you would
like to have available in the hospital or home?
P – Personal Spirituality Are there religious practices that you wish to plan for
regarding time of death, or the period following
Describe the beliefs and practices of your religion that
death?
you personally accept
From what sources do you draw strength in order to
Describes those beliefs and practices that you do not
cope with this illness?
accept or follow
For what in your life do you still feel gratitude even
In what ways is your spirituality/ religion meaningful
though your ill?
to you?
When you are afraid or in pain, how do you find
How is your spirituality important to you in daily life?
comfort?
I – Integration with Spiritual Community As we plan for your medical care near the end of life,
in what ways will your religion and spirituality
Do you belong to any religious or spiritual groups or influence your decision?
communities?
How do you participate in this group? What is your
role?
What importance does this group have for you?
In what ways is this group a source of support for
you?
What type of support and help does this group
provide for you in dealing with health issues?
R – Ritualized Practices and Restrictions
What specific practices do you carry out as a part of
your religious and spiritual life?
You might also like
- Anatomical PositionsDocument36 pagesAnatomical PositionsrlinaoNo ratings yet
- Body MechanicsDocument7 pagesBody MechanicssophiaellainemarcosNo ratings yet
- Nursing Funda Manual NewDocument420 pagesNursing Funda Manual Newharold smithNo ratings yet
- Body MechanicsDocument2 pagesBody MechanicsCrazy StrangerNo ratings yet
- Body MechanicsDocument4 pagesBody Mechanicsjulietaira quibilanNo ratings yet
- Fundamentals of Nursing Module 2 Mobility: TitleDocument8 pagesFundamentals of Nursing Module 2 Mobility: Titlesharahcatherine romanaNo ratings yet
- Nursing Guide to Preventing Patient FallsDocument17 pagesNursing Guide to Preventing Patient FallsmonabertNo ratings yet
- Essential Body Mechanics Principles for Healthcare WorkersDocument22 pagesEssential Body Mechanics Principles for Healthcare Workerscrisferd labajoNo ratings yet
- Body Mechanics: Marlon A. de Guzman, PTRP, MOHDocument36 pagesBody Mechanics: Marlon A. de Guzman, PTRP, MOH력강No ratings yet
- Body Mechanics BrochureDocument2 pagesBody Mechanics BrochureRizka KhaerNo ratings yet
- Lesson Notes - Body MechanicsDocument9 pagesLesson Notes - Body MechanicsNicole Marin-ChingNo ratings yet
- Chapter 1 Body Mechanics: DefinitionDocument25 pagesChapter 1 Body Mechanics: DefinitionCyeonjNo ratings yet
- Procedure in Turning Client To Side-Lying PositionDocument1 pageProcedure in Turning Client To Side-Lying PositioncrrfrncNo ratings yet
- Balance, Posture and Body AlignmentDocument6 pagesBalance, Posture and Body AlignmenthahahahaaaaaaaNo ratings yet
- Proper Body Mechanics for Safe Patient HandlingDocument35 pagesProper Body Mechanics for Safe Patient HandlingAslea Aubrey ZorillaNo ratings yet
- Assingment Human Anatomy ReviseDocument24 pagesAssingment Human Anatomy RevisekrubanNo ratings yet
- Body Mechanics ChecklistDocument7 pagesBody Mechanics ChecklistPrincess ZantuaNo ratings yet
- Body MechanicsDocument18 pagesBody MechanicsMelody LandichoNo ratings yet
- BACK SAFETY AND MANUAL HANDLING TIPSDocument24 pagesBACK SAFETY AND MANUAL HANDLING TIPSKama EfendiyevaNo ratings yet
- Body MechanicsDocument27 pagesBody MechanicsJURY LEIGH SALUQUENNo ratings yet
- Transfer and AmbulationDocument108 pagesTransfer and AmbulationGladys YaresNo ratings yet
- Maintaining Proper Body Mechanics for NursesDocument60 pagesMaintaining Proper Body Mechanics for NursesMargarette AfanNo ratings yet
- Body MechPos Mob Dev.Document3 pagesBody MechPos Mob Dev.Alyssa Jade GolezNo ratings yet
- Body Mechanics Brochure PDFDocument2 pagesBody Mechanics Brochure PDFAbdul Rahman YusofNo ratings yet
- Lafarge Construction Ergonomics in The WorkplaceDocument48 pagesLafarge Construction Ergonomics in The WorkplacehksNo ratings yet
- Assist With Client or Patient MovementDocument88 pagesAssist With Client or Patient Movementmihret gashayeNo ratings yet
- Ms .Sheetal More Clinical InstructorDocument18 pagesMs .Sheetal More Clinical InstructorMangesh PoteNo ratings yet
- HDC Lesson 1 Body Mechanics NPCI Jan. 2021Document2 pagesHDC Lesson 1 Body Mechanics NPCI Jan. 2021cherryNo ratings yet
- Body Mechanics and Transferring PatientDocument57 pagesBody Mechanics and Transferring PatientRhenier S. Ilado100% (2)
- Body Posture & Lifting-8Document89 pagesBody Posture & Lifting-8Shafiq Mohd NorNo ratings yet
- Procedure in Moving The Patient Up in The BedDocument2 pagesProcedure in Moving The Patient Up in The Bedcrrfrnc0% (2)
- Mecanica CorporalDocument1 pageMecanica CorporalXiomara EspinelNo ratings yet
- Body Mec and Bed MakingDocument95 pagesBody Mec and Bed Makingloise100% (1)
- Rle - Mid WK 1Document3 pagesRle - Mid WK 1cheryl.c.miguelNo ratings yet
- Body MechanicsDocument2 pagesBody MechanicsKarLo TabuzoNo ratings yet
- Moving and Handling Elearning TheoryDocument44 pagesMoving and Handling Elearning TheoryAdam wizNo ratings yet
- Body MechanicsDocument7 pagesBody MechanicsKristine CustodioNo ratings yet
- Body Mechanics and Positioning EssentialsDocument66 pagesBody Mechanics and Positioning Essentialsbevzie datuNo ratings yet
- Body Mechanics PDFDocument13 pagesBody Mechanics PDFAny Andriani100% (1)
- Body Mechanics: Ms. Francisca Achaliwie AND Ms. Mabel Apaanye AvaneDocument22 pagesBody Mechanics: Ms. Francisca Achaliwie AND Ms. Mabel Apaanye AvaneAmfo Baffoe FrederickNo ratings yet
- Body Mechanics: Fundamental of Nursing IDocument55 pagesBody Mechanics: Fundamental of Nursing Irlinao100% (3)
- NURS 04 RLE - Bed To WheelchairDocument1 pageNURS 04 RLE - Bed To WheelchairayresNo ratings yet
- Principles of Body Mechanics: By: Angeluz Fernandez-GarciaDocument34 pagesPrinciples of Body Mechanics: By: Angeluz Fernandez-Garciadear_angel2003No ratings yet
- Activity and ExerciseDocument27 pagesActivity and Exercisehannah soledadNo ratings yet
- Body Mechanics for NursesDocument3 pagesBody Mechanics for NursesKERL RAMANo ratings yet
- II Body MechanicsDocument2 pagesII Body MechanicsTuTit0% (1)
- Principles For Proper Body Mechanics: Self-Study GuideDocument8 pagesPrinciples For Proper Body Mechanics: Self-Study GuideSLCNtc100% (1)
- Movement Activity 2Document94 pagesMovement Activity 2pizzyray640No ratings yet
- Body Posture and LiftingDocument88 pagesBody Posture and LiftingShafiq Mohd NorNo ratings yet
- Basic Body MechanicsDocument83 pagesBasic Body MechanicsCyrille Aira AndresaNo ratings yet
- Body MechanicsDocument41 pagesBody MechanicsPaul ReynaldoNo ratings yet
- Proper Body Mechanics For NursesDocument3 pagesProper Body Mechanics For NursesRaquel RamalNo ratings yet
- BSBWHS501A AnswerDocument21 pagesBSBWHS501A AnswerPrashikshan UlakNo ratings yet
- LogrollingDocument1 pageLogrollingLoren MisticaNo ratings yet
- Principles of Body MechanicsDocument2 pagesPrinciples of Body MechanicsKhie-An Ocampo100% (2)
- What Is Posture?: Phclab Phclab Phclab PhclabDocument8 pagesWhat Is Posture?: Phclab Phclab Phclab PhclabMaria Theresa UyNo ratings yet
- FUNDA RLE SAS 4 Zabate Samantha Kaye A PDFDocument7 pagesFUNDA RLE SAS 4 Zabate Samantha Kaye A PDFgekkonoojiNo ratings yet
- Body Mechanics and Transfer TechniquesDocument90 pagesBody Mechanics and Transfer TechniquesTina Talmadge100% (1)
- Reproductive SystemDocument3 pagesReproductive SystemJanelle LasalaNo ratings yet
- Thorax Breast and Lymphatic System AssesmentDocument106 pagesThorax Breast and Lymphatic System AssesmentJanelle LasalaNo ratings yet
- Stress and AdaptationDocument2 pagesStress and AdaptationJanelle LasalaNo ratings yet
- Death and DyingDocument2 pagesDeath and DyingJanelle LasalaNo ratings yet
- COMFORT, PAIN, REST and SLEEPDocument11 pagesCOMFORT, PAIN, REST and SLEEPJanelle LasalaNo ratings yet
- Endocrine System BrochureDocument2 pagesEndocrine System BrochureAldrin CortezNo ratings yet
- Endocrinology 2015-2016 CM 377Document45 pagesEndocrinology 2015-2016 CM 377Daniel ArseniNo ratings yet
- Hypothyroidism: Brief Definition Prevalence Risk FactorsDocument8 pagesHypothyroidism: Brief Definition Prevalence Risk FactorsJennifer BeguinwaNo ratings yet
- DR Bruce West's Health Alert Newsletter - Find Information On Heart Health, Diabetes, Prostate, Alternative Health Care, Holistic Medicine and Much More!Document7 pagesDR Bruce West's Health Alert Newsletter - Find Information On Heart Health, Diabetes, Prostate, Alternative Health Care, Holistic Medicine and Much More!cafjnk43% (7)
- Hypothyroidism DiagnosisDocument4 pagesHypothyroidism DiagnosisWan Razin Wan HassanNo ratings yet
- PosterDocument32 pagesPosterBeny RiliantoNo ratings yet
- Clinical Pathology MCQDocument14 pagesClinical Pathology MCQhshshhsjsjsbxxhNo ratings yet
- HipertiroidDocument42 pagesHipertiroidCoass XII BonamNo ratings yet
- Oral Manifeststions of Endocrine DisorderDocument8 pagesOral Manifeststions of Endocrine DisorderpratheeparamkumarNo ratings yet
- Thyroid Panel Results for 40-Year-Old FemaleDocument1 pageThyroid Panel Results for 40-Year-Old FemaleDeeptha AravamudhanNo ratings yet
- Management of The Medically Compromised Dental PatientDocument40 pagesManagement of The Medically Compromised Dental PatientabodyzizoNo ratings yet
- Thyroid Stimulating Hormone Test and Its Effect On The Human BodyDocument4 pagesThyroid Stimulating Hormone Test and Its Effect On The Human BodyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Surgery PDF 4TH Yr 7TH Sem Solved On The Basis of Previous Yr Paper and Books Ankit AkelaDocument25 pagesSurgery PDF 4TH Yr 7TH Sem Solved On The Basis of Previous Yr Paper and Books Ankit Akelachai rinNo ratings yet
- MRCS Clinical 3 1Document47 pagesMRCS Clinical 3 1Alexandros Megas100% (1)
- Daftar Pustaka PDFDocument13 pagesDaftar Pustaka PDFcut yura AddinaNo ratings yet
- Papillary Thyroid CarcinomaDocument17 pagesPapillary Thyroid CarcinomaEster Sibarani100% (2)
- Mindmap METENDocument1 pageMindmap METENIpulCoolNo ratings yet
- Dpa Cross Sectional Study On The Prevalence of Thyroid Disorders in The Urban Community of DelhiDocument54 pagesDpa Cross Sectional Study On The Prevalence of Thyroid Disorders in The Urban Community of DelhiGurmeet SinghNo ratings yet
- Hipertiroid Guideline, ATADocument54 pagesHipertiroid Guideline, ATAHashini VjkmrNo ratings yet
- MRCP Recall May 19Document10 pagesMRCP Recall May 19Mariam YousifNo ratings yet
- General Practitioner - Endocrinology MCQsDocument17 pagesGeneral Practitioner - Endocrinology MCQsAsif Newaz100% (2)
- Herbal Drugs For Thyroid - PDF: International Journal of Pharmacy and Biological Sciences May 2016Document10 pagesHerbal Drugs For Thyroid - PDF: International Journal of Pharmacy and Biological Sciences May 2016Sanju TkNo ratings yet
- Endocrain Systm Question 1 ST DayDocument15 pagesEndocrain Systm Question 1 ST DayJohn AjishNo ratings yet
- Acute Biologic CrisisDocument142 pagesAcute Biologic CrisisAngel VallejoNo ratings yet
- Endometab Exam 2018Document8 pagesEndometab Exam 2018teabagmanNo ratings yet
- Hypothyroidism Diagnosis and TreatmentDocument59 pagesHypothyroidism Diagnosis and TreatmentAmir Mahmoud100% (1)
- Understanding Multinodular Non-Toxic GoiterDocument58 pagesUnderstanding Multinodular Non-Toxic GoiterSeff CausapinNo ratings yet
- Thyrotoxicosis Weight Loss and Energy LevelsDocument7 pagesThyrotoxicosis Weight Loss and Energy LevelshappyhappylandNo ratings yet
- Werner & Ingbar’s The Thyroid 8th EditionDocument10 pagesWerner & Ingbar’s The Thyroid 8th Editionbyrock66No ratings yet
- Toxic multinodular goiter exam findingsDocument2 pagesToxic multinodular goiter exam findingsAngie MandeoyaNo ratings yet