Professional Documents
Culture Documents
Skillsexam
Uploaded by
Anna Nana0 ratings0% found this document useful (0 votes)
43 views5 pagesOriginal Title
skillsexam
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
43 views5 pagesSkillsexam
Uploaded by
Anna NanaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Parts of the Patient’s Chart (Documenting) Legal Documentation- Is a legal document
and is usually admissible in court as
Legally owned by the hospital
evidences.
Accurate and concise patient charting is an
important part of a nurse’s job. Health care Analysis- Information from
Through charting, nurses communicate vital records may assist health care planners to
information to the entire healthcare team. identify agency needs, such as overutilized
A patient chart is also a legal document that and underutilized hospital services.
describes all aspects of a patient’s care,
Components of Patient’s Chart/ Medical Chart
A discussion is an informal consideration of
a subject by two or more health care Admission Sheet/ Top/ Face Sheet-
personnel to identify a problem or establish information include legal name, birth
strategies to resolve a problem. details (date, year, place), age, gender,
A report is oral, written, or computer- based address, contact number, parent’s basic
communication intended to convey information, marital status, date, time
information to others and admitting diagnosis, admitting
A record is written or computer based. diagnosis, name of admitting and
A clinical record, also called a chart or client attending physician
record, is a formal, legal document that Consent for Admission/ Management
provides evidence of a client’s care. Sheet - This page contains that the
patient or relatives allowing the
Purposes of Client Records
medical institution to take care their
Communication- The record serves as the patient (full decided) whether the
vehicle by which different health possible risk beyond on the process of
professionals who interact with a client treatment course
communicate with each other. Patient’s Right Sheet - discusses the
patient’s right during the entire process
Planning Client Care- Each health of medical treatment.
professional uses data from the client’s Clinical History- contains initial history,
record to plan care for the client review of systems, and physical
Auditing Health Agencies- An audit is a assessment
review of client records for quality- Vital Signs Graphic Chart- contains of
assurance purposes every shift 5 cardinal vital signs of the
patient
Research- The information contained in a Physician’s Order and Progress Notes-
record can be a valuable source of data for Medical orders (diagnostics,
research therapeutics and other health
management). Medical Observations,
Education- Students in health disciplines
treatments, client progress (Progress
often use client records as records as
Notes usually on the right corner side
educational tool
of this sheet)
Reimbursement- For a facility to obtain Medication and Treatment Record-
payment through Medicare, name, dosage, frequency of the
medication and treatment on regular
intervals.
PRN/ Premeds/ Nebulization- Important data
separated sheet from the medication
Vital signs must be recorded accurately and
and treatment record. As needed
promptly to provide continuous and current
medications, Pre medications (pre-
documentation.
operative, pre- blood transfusion) and
nebulization and inhalation A record of a client’s vital signs helps
medications. providers diagnose and respond to the
Venoclysis- documented on this sheet client’s changing condition.
all the Intravenous Fluids administered
to the patient. The nurse needs to know the format for
Vital Signs Monitoring- in detailed vital documenting vital signs in his or her agency.
signs monitoring of the patient (it Steps for recording vital signs in the paper
depends on the order of the physician, record include
or during blood transfusion monitoring Temperature - 36.5 – 37.5
[per ANSAP protocol on blood
transfusion management]) hyperthermia hypothermia
Intake and Output Sheet- all routes of
Blood pressure – 120/60 mmhg (90/60)
fluid intake and all routes of fluid loss
of output are measured and recorded
on this form. hypertension hypotension
Laboratory Reports- all blood, urine
Pulse rate – 60 - 100 bpm
and stool exam results are attached on
this sheet. (
Nurses Notes- pertinent assessment of tachycardia bradycardia
client. Specific nursing care including Radial, brachial, popliteal, dorsalis
teaching and client’s responses.
Respiratory rate – 12 – 20 bpm/cpm
Consent for Procedures- all invasive
procedures prior to do so, must have a
written consent in relation that patient tachypnea bradypnea
and relatives able to understand the
O2 – 95% - 100%
purpose of that procedure/s.
Pain scale – 0 – 10
Other Parts of Patient Chart (Per condition)
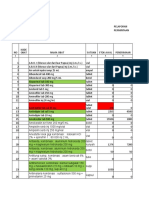
Plotting Vital Signs
CBG monitoring sheet
Patient’s discharge summary Time to Assess Vital Signs
Discharge clearance
Home against medical advice On admission to health care agency to
obtain baseline data
Newborn Additional Parts When a client has a change in health status
or report symptoms such as chest pain, or
Immunization slip card
feeling hot or faint
Newborn rooming and discharge checklist
Before and after surgery or an invasive
Newborn record
procedure
EINC monitoring sheet
Before and/ or after the administration of a
Vital Signs medication that could affect the respiratory
or cardiovascular systems, for example, PPD (Purified Protein Derivative) is used
before giving a digitalis preparation Route of administration: Intradermal
Before and after any nursing intervention Read 48 to 72 hours after injection
that could affect the vital signs (ambulating (+) Mantoux test is induration of 10mm
a client who has been on bed rest) or more
For HIV positive clients, induration of
The Graphic Record
5mm is considered positive
The graphic record is a flow sheet used (+) Mantoux signifies exposure to
to easily document large amounts of Mycobacterium tubercle bacilli
information for all members of the Mantoux test will be positive for clients
healthcare team to read. who have received BCG
Usually, the graphic record documents
CHEST RADIOGRAPHY/ CHEST X-RAY
measurements of vital signs, fluid
intake and output (I&O), weight, and In chest radiography, X-rays or
bowel movements, assessed at regular electromagnetic waves penetrate the
intervals. chest and cause an image to form on
specially sensitized film.
Recording Vital Signs
Air appears radiolucent, whereas
a. Locate the current date on the graphic record. normal tissue, bone, and abnormalities
— such as infiltrates, foreign bodies,
b. Record temperature by making a dot on the scale
fluids, and tumors appear as densities
parallel to the temperature value under the
on the film.
designated time. Connect the dot to the previous
A chest X-ray is most useful when
reading with a short line. (In many facilities using a
compared with previous films to detect
paper record, the temperature and pulse are
changes
graphed in different color inks.)
BRONCHOGRAPHY/ BRONCHOGRAM
c. Record pulse rate by making a dot on the scale
parallel to the pulse rate under the designated time. A radiopaque medium is instilled
Connect the dot to the previous reading with a short directly into the trachea and bronchi
line. and the entire bronchial tree or
selected areas may be visualized
d. Record respiratory rate at the bottom of the graph
through x-ray
with numbers.
e. Record BP with written numbers (e.g., 120/80) or
graph the numbers in a manner similar to that used NURSING INTERVENTIONS BEFORE BRONCHOGRAM
for the temperature graph.
Secure written consent
f. Record other information, such as weight, bowel Check for allergies to sea foods or
movements, and the totals for I&O, with written iodine or anesthesia
numbers in the spaces provided. NPO for 6 to 8 hours
Pre- op Medications: Atropine Sulfate
and Valium, topical anesthesia sprayed
Diagnostic Studies and Therapies into the throat; followed by local
anesthetic injected to the larynx
SKIN TEST: MANTOUX TEST
Have oxygen and antispasmodic agents LUNG SCAN
ready
Following injection of a radioisotope,
NURSING INTERVENTIONS AFTER BRONCHOGRAM scans are taken with a scintillation
camera.
Side- lying position
Measures blood perfusion through the
NPO until cough and gag reflexes return
lungs
Cough and deep breathe client
Confirms pulmonary embolism or other
Low grade fever is common blood- flow anomalies
BRONCHOSCOPY Instruct the client to remain still during
the procedure
The direct inspection and observation
of the larynx, trachea and bronchi SPUTUM COLLECTION
through a bronchoscope
To assess for gross appearance of the
DIAGNOSTIC USES sputum
Sputum C and S (Culture and
To collect secretions Sensitivity Test)- this is done to detect
To determine location of pathologic the actual microorganisms causing
process and collect specimen for biopsy respiratory infection
THERAPEUTIC USES AFB Staining (Acid Fast Bacillus Stain)-
to detect PTB
To remove aspirated foreign objects
PROPER COLLECTION OF SPUTUM
To excise small lesions
Early morning sputum specimen is to be
NURSING INTERVENTIONS BEFORE BRONCHOSCOPY
collected
Informed consent Advise the client to rinse mouth with plain
Atropine and Valium pre- procedure as water
prescribed; topical anesthesia sprayed Use sterile container
into the throat followed by local Sputum specimen for C and S is collected
anesthesia injected into larynx before the first dose on antimicrobial
NPO for 6 to 8 hours For AFB staining, collect sputum specimen
Remove dentures, prostheses, contact for 3 consecutive mornings
lenses
BIOPSY OF LUNG
NURSING INTERVENTIONS AFTER BRONCHOSCOPY
Transbronchoscopic biopsy- done
Side- lying position during bronchoscopy
Check for return of cough and gag Percutaneous Needle Biopsy- done
reflex before giving fluids with the use of aspiration needle
Watch out for cyanosis, hypotension, Open Lung Biopsy- done during surgery
tachycardia, arrythmias, hemoptysis, Lymph Node Biopsy- scalene or
dyspnea cervicomediastinal- to assess
metastasis of lung cancer
ARTERIAL BLOOD GAS STUDIES
To assess ventilation and acid- base
balance
Radial artery is the common site for
withdrawal of blood specimen
Allen’s test is done to assess for
adequacy of collateral circulation of the
hands
Use 10 ml pre- heparinized syringe to
draw blood specimen.
Place the specimen in a container with
ice
PULSE OXIMETRY
To determine oxygen saturation in the
blood
95% to 100%- normal range
The pulse oximeter sensor is placed in
the index finger or ear lobe
The sensor should be covered with
opaque material. The reading can be
affected by sunlight
THORACENTESIS
Aspiration of fluid or air from the
pleural space
NURSING INTERVENTIONS BEFORE THORACENTESIS
Secure written consent
take initial vital signs
Position: upright, leaning on overbed
table
Instruct the client to remain still, avoid
coughing during insertion of needed
Turn the client on unaffected side
Bed rest
Check for expectoration of blood
Monitor vital signs
You might also like
- Health Information System Developmen T (Medical Records)Document21 pagesHealth Information System Developmen T (Medical Records)skidz137217100% (10)
- Week 13 Documentation in Psychiatric Mental Health Nursing PracticeDocument69 pagesWeek 13 Documentation in Psychiatric Mental Health Nursing PracticeJeff MalinisNo ratings yet
- Documenting and Reporting: CommunicationDocument5 pagesDocumenting and Reporting: CommunicationDanielle Cachero100% (1)
- Newman's Certified Electronic Health Records Technician Study GuideFrom EverandNewman's Certified Electronic Health Records Technician Study GuideNo ratings yet
- Patient's Medical Chart PDFDocument2 pagesPatient's Medical Chart PDFHydieNo ratings yet
- Histrionic Personality DisorderDocument2 pagesHistrionic Personality DisorderRodeneNo ratings yet
- DocumentationDocument15 pagesDocumentationAra- Cvsu Francisco100% (2)
- Urology Resident Handbook3380 PDFDocument65 pagesUrology Resident Handbook3380 PDFKeserovic AdmirNo ratings yet
- Manual for Iv Therapy Procedures & Pain Management: Fourth EditionFrom EverandManual for Iv Therapy Procedures & Pain Management: Fourth EditionNo ratings yet
- Unit 1 Documentation-and-ReportingDocument39 pagesUnit 1 Documentation-and-ReportingMs.V. Mahesha Asst. Prof.No ratings yet
- 1 Patient-Chart PDFDocument32 pages1 Patient-Chart PDFAira Gene MenesesNo ratings yet
- Maintenance of Records and ReportsDocument81 pagesMaintenance of Records and ReportsSanjna Kumari (SNSR Senior Tutor/Lecturer)100% (1)
- Definition of Terms Purposes of Documentation in The Nursing Practice 1. CommunicationDocument37 pagesDefinition of Terms Purposes of Documentation in The Nursing Practice 1. CommunicationMARIA STEPHANY DELA CRUZNo ratings yet
- Documentation: Basic Nursing: Foundations of Skills & Concepts DocumentationDocument8 pagesDocumentation: Basic Nursing: Foundations of Skills & Concepts DocumentationJona GarzonNo ratings yet
- Patients Medical ChartDocument25 pagesPatients Medical ChartErlyn EnocNo ratings yet
- Transcribing Doctors OrderDocument6 pagesTranscribing Doctors OrderMarielle Chua100% (1)
- Hospital Design: Flow Chart of DepartmentsDocument15 pagesHospital Design: Flow Chart of DepartmentsAbirami80% (5)
- NICU Documentation: Gama Hospital Al Khobar K.S.ADocument8 pagesNICU Documentation: Gama Hospital Al Khobar K.S.ALucian CaelumNo ratings yet
- Kaplan, R.-Anna O Being Bertha PappenheimDocument8 pagesKaplan, R.-Anna O Being Bertha PappenheimNico ChurchuNo ratings yet
- Kode Pintar Icd 10Document48 pagesKode Pintar Icd 10Glory Stephanie Tesalonika Supit100% (2)
- Nursing ProcessDocument52 pagesNursing ProcessDzon LornaNo ratings yet
- Computed Tomography Radiation Safety Issues in OntarioDocument71 pagesComputed Tomography Radiation Safety Issues in Ontariopebbles18950% (2)
- Hospitals in Coimbatore PDFDocument24 pagesHospitals in Coimbatore PDFSACHIDANANDA SNo ratings yet
- Komunikasi Efektif Dan Keselamatan Pasien - Bahan Bu TikaDocument44 pagesKomunikasi Efektif Dan Keselamatan Pasien - Bahan Bu TikaZara Yuliani PutriNo ratings yet
- Transcribing Doctors OrderDocument6 pagesTranscribing Doctors OrderLiza SoberanoNo ratings yet
- Medical RecordsDocument331 pagesMedical Recordssgekara cyberNo ratings yet
- (Nursing English) DIYAH AHADYATUNNISADocument10 pages(Nursing English) DIYAH AHADYATUNNISAdiyah hansuNo ratings yet
- 9 3 2012 Charting and DocumentationDocument44 pages9 3 2012 Charting and DocumentationMacrossBalaNo ratings yet
- Medical Procedures Reviewer G5 7Document8 pagesMedical Procedures Reviewer G5 7jilliantrcieNo ratings yet
- Group11 MOPDocument5 pagesGroup11 MOPjilliantrcieNo ratings yet
- Week 6 Group 3Document6 pagesWeek 6 Group 3Art Jay DelfinNo ratings yet
- KLP 2 (10-18) - Kelas Ners A - English Medical RecordDocument22 pagesKLP 2 (10-18) - Kelas Ners A - English Medical RecordKusumadewi WidiarsaNo ratings yet
- Medical Record Documentation Standards For Practitioners: Aetna Better Health® of West VirginiaDocument3 pagesMedical Record Documentation Standards For Practitioners: Aetna Better Health® of West VirginiaMkamal MosaNo ratings yet
- Documentation System Focus ChartingDocument26 pagesDocumentation System Focus ChartingneehoshiNo ratings yet
- Risk 201008 Medical Records and You PDFDocument4 pagesRisk 201008 Medical Records and You PDFFitra PringgayudaNo ratings yet
- Documentation: VN230 Vocational Nursing Spring 2007Document44 pagesDocumentation: VN230 Vocational Nursing Spring 2007brendz_pontelaNo ratings yet
- Cmca Rle L1 DocumentationDocument23 pagesCmca Rle L1 DocumentationJay EstrellaNo ratings yet
- NC State University Veterinary Teaching Hospital Medical Records Documentation GuideDocument14 pagesNC State University Veterinary Teaching Hospital Medical Records Documentation GuideTriwanti TiagaNo ratings yet
- Nursing Documentation and Recording Systems of Nursing CareDocument7 pagesNursing Documentation and Recording Systems of Nursing CaredesianabsNo ratings yet
- Skills in Documenting and ReportingDocument9 pagesSkills in Documenting and ReportingcjNo ratings yet
- ID - DocumentationDocument4 pagesID - DocumentationDharylle CariñoNo ratings yet
- Records and ReportDocument4 pagesRecords and ReportAnusikta PandaNo ratings yet
- CLINPHARM Lab Act 1Document8 pagesCLINPHARM Lab Act 1ezzaNo ratings yet
- Hospital Forms and Postpartum ExercisesDocument8 pagesHospital Forms and Postpartum ExercisesVincent Paul PagulayanNo ratings yet
- Pharm Info LecDocument5 pagesPharm Info LecTrixie Nichole LaraNo ratings yet
- Med Record Auditor - Sample PagesDocument5 pagesMed Record Auditor - Sample PagesDaniel O. FernandezNo ratings yet
- A The Health RecordDocument6 pagesA The Health Recordbusinge innocentNo ratings yet
- Chapter 02Document44 pagesChapter 02Carlos ChuNo ratings yet
- Chapter 1 - Introduction To Health Record ManagementDocument18 pagesChapter 1 - Introduction To Health Record ManagementLalita A/P AnbarasenNo ratings yet
- Wm. Jennings Bryan Dorn VAMC Patient Safety TrainingDocument39 pagesWm. Jennings Bryan Dorn VAMC Patient Safety Trainingkamnasharma0907No ratings yet
- Computer Assignment1Document9 pagesComputer Assignment1AlizaNo ratings yet
- Nabh Tertiary CareDocument7 pagesNabh Tertiary CareGold PANDINo ratings yet
- Documentation: Written Evidence ofDocument30 pagesDocumentation: Written Evidence ofAnggraeni Prameswari PutriNo ratings yet
- Ipd Documentation Jr'sDocument12 pagesIpd Documentation Jr'sQuality AIIMSUdrNo ratings yet
- Documenting and ReportingDocument5 pagesDocumenting and ReportingElla LobenariaNo ratings yet
- ED Doc PolicyDocument4 pagesED Doc PolicyAlyssa AzucenaNo ratings yet
- Medical Records DepartmentDocument20 pagesMedical Records DepartmentPrasidha PrabhuNo ratings yet
- COP 1 and 2Document16 pagesCOP 1 and 2Kristel Jane QuitoNo ratings yet
- Relevance of Nursing Documentation and Its Legal ImplicationsDocument8 pagesRelevance of Nursing Documentation and Its Legal ImplicationsGeorge AyiteyNo ratings yet
- Binder 1Document5 pagesBinder 1Walid YoussefNo ratings yet
- Charter of Patients Rights ResponsibilitiesDocument12 pagesCharter of Patients Rights ResponsibilitiesSuhas KandNo ratings yet
- Fact Sheet: Providing Patients in Ambulatory Care Settings With A Clinical Summary of The Office VisitDocument3 pagesFact Sheet: Providing Patients in Ambulatory Care Settings With A Clinical Summary of The Office VisitAnonymous ZbY0QisHKNo ratings yet
- Learning Module NUMBER 1 The Health Record From Paper To ElectronicDocument28 pagesLearning Module NUMBER 1 The Health Record From Paper To ElectronicKahfi NzeelNo ratings yet
- HCM Module 5Document10 pagesHCM Module 5HisanaNo ratings yet
- Patient Assessment PolicyDocument7 pagesPatient Assessment Policysyed ishan ahmedNo ratings yet
- Chapter 26: Documentation and Informatics Mistakes in Documentation That Commonly Results in MalpracticeDocument9 pagesChapter 26: Documentation and Informatics Mistakes in Documentation That Commonly Results in MalpracticejoanneNo ratings yet
- Fluids and ElectrolytesDocument19 pagesFluids and ElectrolytesAnna NanaNo ratings yet
- Nursing Care in The HomeDocument4 pagesNursing Care in The HomeAnna NanaNo ratings yet
- LRDRDocument2 pagesLRDRAnna NanaNo ratings yet
- DrugDocument5 pagesDrugAnna NanaNo ratings yet
- OpdDocument1 pageOpdAnna NanaNo ratings yet
- Ucv 1Document1 pageUcv 1Anna NanaNo ratings yet
- Discussion Activity PregnancyDocument1 pageDiscussion Activity PregnancyAnna NanaNo ratings yet
- SeptDocument3 pagesSeptAnna NanaNo ratings yet
- AnatomyDocument8 pagesAnatomyAnna NanaNo ratings yet
- Lesson Notes Sep 20 2021Document1 pageLesson Notes Sep 20 2021Anna NanaNo ratings yet
- Ob Case ScenarionDocument1 pageOb Case ScenarionAnna NanaNo ratings yet
- Nutri Lab Prelim ExamDocument2 pagesNutri Lab Prelim ExamAnna NanaNo ratings yet
- Nutri Lab Prelim ExamDocument2 pagesNutri Lab Prelim ExamAnna NanaNo ratings yet
- Ob Case ScenarionDocument1 pageOb Case ScenarionAnna NanaNo ratings yet
- Wonders of FertilizationDocument6 pagesWonders of FertilizationAnna NanaNo ratings yet
- Ob Case Scenario-Preliminary ExaminationDocument1 pageOb Case Scenario-Preliminary ExaminationAnna NanaNo ratings yet
- q2 Health - 8 M 4 Revised PDFDocument24 pagesq2 Health - 8 M 4 Revised PDFGemarie CallosaNo ratings yet
- First Aid Principles and PracticeDocument51 pagesFirst Aid Principles and PracticeGiselle KhrystineNo ratings yet
- Alternative Certificate - Foundation Competences ProtectedDocument12 pagesAlternative Certificate - Foundation Competences ProtectedFlavian Costin NacladNo ratings yet
- Written Report - PhilHealthDocument5 pagesWritten Report - PhilHealthSophia VeralloNo ratings yet
- CRE Fixed Wire Balloon Dilatation CatheterDocument2 pagesCRE Fixed Wire Balloon Dilatation CathetermaassingerNo ratings yet
- Allergies: A Protective Mechanism Out of ControlDocument29 pagesAllergies: A Protective Mechanism Out of Controlडा. सत्यदेव त्यागी आर्यNo ratings yet
- Infopia Clover A1cDocument31 pagesInfopia Clover A1cAde NasutionNo ratings yet
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementDocument10 pagesMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahNo ratings yet
- Elitrol I Elitrol Ii: Français - FR English - EN Español - ES Português - PTDocument2 pagesElitrol I Elitrol Ii: Français - FR English - EN Español - ES Português - PTYousra ZeidanNo ratings yet
- Lplpo Agustus 2017Document66 pagesLplpo Agustus 2017Selly Wijaya BermawiNo ratings yet
- NCD BrochureDocument2 pagesNCD BrochureQuỳDướiChânPhậtNo ratings yet
- Pedia-Formulas and DripsDocument6 pagesPedia-Formulas and DripsNerak LuNo ratings yet
- Antibiotik Dan Antiseptik Saluran KemihDocument29 pagesAntibiotik Dan Antiseptik Saluran KemihPutri Sari SeptirianiNo ratings yet
- LocholDocument6 pagesLocholKashif FarooquiNo ratings yet
- All About Iris Tumors Dr. Schefler1 PDFDocument2 pagesAll About Iris Tumors Dr. Schefler1 PDFTruly GracevaNo ratings yet
- A 55-Year-Old Woman With Shock and Labile Blood PressureDocument11 pagesA 55-Year-Old Woman With Shock and Labile Blood PressureMr. LNo ratings yet
- Episode ListDocument25 pagesEpisode ListhectorNo ratings yet
- FLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeDocument3 pagesFLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeAizaz ul HaqNo ratings yet
- FHTMonitoringDocument21 pagesFHTMonitoringlaarnie100% (1)
- Fiebre de Origen Desconocido NEJMDocument15 pagesFiebre de Origen Desconocido NEJMJacinto RamonNo ratings yet
- Reproductive Arranged (MedicalBooksVN - Com)Document63 pagesReproductive Arranged (MedicalBooksVN - Com)Rabooh AyashiNo ratings yet
- Anti Allergy: NO Produk Komposisi Kemasan HNA Hna + PPN KETDocument6 pagesAnti Allergy: NO Produk Komposisi Kemasan HNA Hna + PPN KETMuhammad Asri,S.Kep,NsNo ratings yet
- Vitti Labs: Our Mission in BriefDocument7 pagesVitti Labs: Our Mission in BriefvittilonghaulNo ratings yet