Professional Documents
Culture Documents
Survival Rate of Incoming Patients With Cardiac Arrest at The Cardiology Infirmary of The Emergency Department of A Public Hospital in Greece 2019
Uploaded by
Yannis ZoldenbergOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Survival Rate of Incoming Patients With Cardiac Arrest at The Cardiology Infirmary of The Emergency Department of A Public Hospital in Greece 2019
Uploaded by
Yannis ZoldenbergCopyright:
Available Formats
Health & Research Journal
Vol. 5, 2019
Survival rate of incoming patients with cardiac
arrest at the cardiology infirmary of the emergency
department of a public hospital in Greece
Papadopoulou Styliani RN, MSc, Emergency
Department, General
Hospital of Piraeus
«ΤΖΑΝΕΙΟ»
Konstantakopoulou Olympia Economist, MSc, PhD(c),
Research Fellow, Center for
Health Services
Management and Evaluation
(CHESME), Department of
Nurs-ing, National and
Kapodistrian University of
Athens
Kalogianni Antonia Assistant Professor, Nursing
Department, University of
West Attica
Kelesi-Stavropoulou Martha Professor, Nursing
Department, University of
West Attica
Kapadohos Theodore Lecturer, Nursing
Department, University of
West Attica
http://dx.doi.org/10.12681/healthresj.20871
Copyright © 2019 Health & Research Journal
To cite this article:
Papadopoulou, S., Konstantakopoulou, O., Kalogianni, A., Kelesi-Stavropoulou, M., & Kapadohos, T. (2019). Survival
rate of incoming patients with cardiac arrest at the cardiology infirmary of the emergency department of a public hospital
in Greece. Health & Research Journal, 5(2), 53-65. doi:http://dx.doi.org/10.12681/healthresj.20871
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
RESEARCH ARTICLE
SURVIVAL RATE OF INCOMING PATIENTS WITH CARDIAC ARREST AT THE CARDIOLO-
GY INFIRMARY OF THE EMERGENCY DEPARTMENT OF A PUBLIC HOSPITAL IN GREECE
Styliani Papadopoulou1, Olympia Konstantakopoulou2, Antonia Kalogianni3, Martha Kelesi-Stavropoulou4, Theodore Ka-
padohos5
1. RN, MSc, Emergency Department, General Hospital of Piraeus «ΤΖΑΝΕΙΟ», Greece
2. Economist, MSc, PhD(c), Research Fellow, Center for Health Services Management and Evaluation (CHESME), Department of Nurs-
ing, National and Kapodistrian University of Athens, Greece
3. Assistant Professor, Nursing Department, University of West Attica, Greece
4. Professor, Nursing Department, University of West Attica, Greece
5. Lecturer, Nursing Department, University of West Attica, Greece
DOI:
Abstract
Introduction: Cardiac arrest is an urgent situation that, despite the improved resuscitation capabilities, the survival rate of out-of-
hospital cardiac arrest victims remains low.
Aim: Τo investigate the survival rate of the incoming patients with cardiac arrest in the cardiology infirmary of the emergency depart-
ment of a public hospital.
Material-Method: The study included 210 patients who were transferred pulseless and breathless at the cardiology infirmary of the
emergency department of “Tzaneio” Hospital, Piraeus, during the period April 2017 - November 2018. Data was collected from the Na-
tional Center of Emergency Dispatch's printed forms, as well as from the patients’ admission book of the emergency department.
Results: More than 10% (11.9%) of patients with cardiac arrest returned to spontaneous circulation in the emergency department, of
which 16% was discharged. Patients with known cardiac history, (p=0.002), with a shockable rhythm (p<0.001), and especially ventricu-
lar fibrillation (p<0.001) upon arrival at the emergency room, and patients who were defibrillated at the ambulance during admission
and at the emergency room, were more likely to survive (p<0.001). No statistically significant correlation was found between the factors
studied and survival after cardiac arrest, in the group of patients that were discharged.
Conclusions: The survival rate of the incoming patients with cardiac arrest at the emergency department of “Tzaneio” Hospital, Piraeus,
was low. As for most health systems, this issue constitutes a fairly complex public health problem. Cardiopulmonary resuscitation and
corresponding guidelines require further improvement in order for the survival rates of out-of-hospital cardiac arrest patients to in-
crease.
Key words: : Cardiac arrest, resuscitation, survival, emergency department.
Corresponding Author: Kapadohos Theodore, Fleming 1, P. Faliro, PC 17563, Tel. 6993161680, E-mail: kapadohos@uniwa.gr
Cite as: Papadopoulou, S., Konstantakopoulou, O., Kalogianni, A., Kelesi-Stavropoulou, M., Kapadohos, T. (2019). Survival rate of incoming patients with
cardiac arrest at the cardiology infirmary of the emergency department of a public hospital in Greece. Health and Research Journal,5(2), –
https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
Papadopoulou et al. 53 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
INTRODUCTION as well as their stay time until their discharge. In particular,
Cardiac arrest is considered worldwide, one of the most serious Galatianou et al. reported a 15.5% of patients who came at the
and most important causes of sudden death, and is defined as Emergency Department and returned to systemic circulation,
the cessation of mechanical activity of the heart, which is con- entered the intensive care unit and remained on average 6.7 ±
firmed by the absence of central pulse and normal breathing.1 4.9 days.21 Subsequently, Karagiannis et al., in a research study
As an incident, cardiac arrest occurs mainly outside the hospi- they carried out at the Nicosia General Hospital of Cyprus, re-
tal. For most health systems, it is a fairly complex public health
2
ported a 44% return of victims to automatic circulation in the
problem, and despite developments in both urgent treatment Emergency Department, after cardiac arrest.22 The survival rates
and improvement of guidelines, the survival rate of out-of- of the two surveys differ, although both are low, as well as at a
hospital cardiac arrest patients still remains low.3 Both surviving global level. However, there is no Greek study recording surviv-
and death rate is high enough, resulting in poor neurological al rates at the Emergency Department, in relation to the times
prognosis, and reduced neurological benefits for the sufferers.4 of arrest and resuscitation, both for shockable and non-
The Emergency Department staff conducts coordinated and shocable rhythms.
organized actions based on a specific protocol, following the
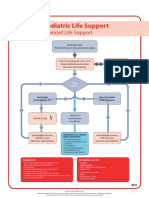
algorithm of Advanced Cardiopulmonary Resuscitation, with AIM
the main objective of resuscitating the victim and treating the The aim of this study was to investigate the survival rate of
possible reversible causes of the arrest.5 Van de Glind and his patients who were transferred to the emergency cardiology
colleagues showed a survival rate of patients with a rate of infirmary of a public hospital due to cardiac arrest, and also to
arrest ranging from 0% to 20%, which has not improved over explore possible correlations between demographics, time
the past 30 years.6 Additionally, Houssein Youness et al. in their periods of cardiac arrest-transfer time-resuscitation time and
own research study, revealed a survival rate of 5% of patients survival rates.
transferred at the Emergency Department with out-of-hospital
cardiac arrest.7 MATERIAL
A large number of scientists have investigated the survival rate The studied population consisted of 227 patients who came
of patients coming to the Emergency Department after a cardi- sequentially in the Emergency Cardiology Infirmary of the
ac arrest outside the hospital, over the last five years (2012- Emergency Department of the "Tzaneio" General Hospital of
2017), with most analysis showing a low survival rate following Piraeus, where they were transferred due to cardiac arrest, be-
a cardiac arrest incident. In particular, in most of the published tween April 2017 and November 2018.
research studies, there is evidence of good quality of chest Of the 227 patients, seventeen cases (7.5%) were excluded
compressions, the presence of witnesses in cardiac arrest inci- from the study because they were transported exclusively for
dent, airway management, the use of an automatic external the purpose of asserting death in the infirmary without the use
defibrillator and the known history of heart disease, in conjunc- of resuscitation during transfer or at the Emergency Depart-
tion with the improved survival rate after the arrest.8-19 In 2014, ment. The final sample of the study consisted of 210 patients.
Kuocw et al. in their research study, which involved 712 pa-
tients with out-of-hospital cardiac arrest, showed a 17.8% who METHOD
returned to systemic circulation, a 16.3% surviving during their A specially formatted registration form was used to collect the
incoming to the Emergency Department, and only 1.4% who data, which included data from the National Emergency Center
managed to get discharged from the hospital.20 Rescuers' Form, the hospitalization book of the cardiology in-
In Greece, two studies dealt with the survival rate of the incom- firmary of the Emergency Department, as well as the Secretari-
ing patients at the Emergency Department with rates of arrest, at of the Cardiology Unit and the Cardiology Clinic.
Papadopoulou et al. 54 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
The questionnaire consisted of five parts. First, the demograph- quantitative variable and a dichotomous variable (when the
ic characteristics of the study population were recorded (gen- quantitative variable followed normal distribution) and a quan-
der and age). The second part included data on the patient's titative variable and a dichotomous variable (when the quanti-
history, where whether the patient had a known heart disease tative variable did not follow normal distribution), respectively.
and its type were recorded. Time periods in relation to the pro- The two-sided level of statistical significance was set equal to
cess of resuscitation as well as the transfer of the patients were 0,05. Data analysis was performed with IBM SPSS 20.0 (Statisti-
recorded in the third part. Specifically, the time of the onset of cal Package for Social Sciences).
the arrest, the time of the onset of the resuscitation, the time
of the patient’s transfer to the Emergency Department and the RESULTS
end of the resuscitation period were recorded on a 24-hour 1. Demographic characteristics of patients incoming with cardiac
basis (00:00 - 23:59). From the recorded time points, the time arrest in the Emergency Department
from the detection of the arrest to the end of resuscitation, the The study population consisted of 210 consecutive cases of
time of the resuscitation in the ambulance, the resuscitation patients who were transferred with cardiac arrest at the Emer-
time in the infirmary and the total resuscitation time (both in gency Department. Seventy one percent (n = 149) of the
the ambulance and the hospital) were calculated in minutes. patients were males. The average age of the patients was 66,6
The fourth part included data on the cardiac arrest and in par- years (SD = 15,4), with the largest age group being 61 to 70
ticular the arrest rhythm on admission to the Emergency De- years old (n = 51, 24,3%) (Table 1).
partment, if defibrillation was given during the transfer, if de-
fibrillation was given to the Emergency Department and how 2. History of heart disease
many times. In the fifth part, data on the outcome of the pa- Twenty nine point five percent (n = 62) of the patients had a
tients was recorded. In particular, whether the patients survived known history of heart disease, most of whom had coronary
the arrest, whether they eventually died or got discharged from artery disease (n = 41, 19,5%) (Table 2).
the hospital, as well as the total survival time until the dis-
charge or the death (in days) were recorded. 3. Data in relation to the cardiac arrest
Ninety eight point one percent (n = 206) of the patients were
ETHICS transferred to the hospital by National Emergency Center. In
All ethical rules and anonymity of the participants were re- the majority of participants, the rate of arrest was asystole (n =
spected during the data collection and process. The study was 183, 87,1%). Defibrillation in the ambulance was given to the
carried out with the written approval of the Scientific Council of 7,1% of patients, while in the Department it was given to the
the hospital (approval number: 38 / 2-5-2017). 7,6%. The total number of defibrillations and the average times
of transfer and resuscitation are recorded in Table 3.
STATISTICAL ANALYSIS Indicatively, as recorded in the study, the average time from
Categorical variables are presented as absolute (n) and relative the detection of arrest to the end of resuscitation was 54,6
(%) frequencies, while quantitative variables are presented as minutes (SD = 19,9), while the median overall resuscitation
mean value (standard deviation) or as median (interquartile time (ambulance + hospital) was 40,5 minutes (IR = 21,0).
range). The Kolmogorov-Smirnov test and normality plots were
used to test for normal distribution of quantitative variables. 4. Outcome
X2 test (chi-square test), t test (student's t-test) and Mann- Eleven point nine percent (n = 25) of the patients survived the
Whitney test were used in order to investigate the existence of arrest, of which 16% (n = 4) got discharged from the hospital,
the relationship between two categorical variables, between a 68% (n = 17) died and 16% (n = 4) was transferred to another
Papadopoulou et al. 55 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
hospital (Table 4). cases of cardiac arrest outside hospital, only 5,5% survived.23
Similarly, Fan et al. showed a low survival rate in Hong Kong
5. Correlations after a cardiac arrest incident, which mounted 2,3% and only
5.1. Survival from the arrest 1,5% with good neurological benefits.24
Following the bivariate analysis a statistically significant rela- From the results of the statistical analysis, in the present study,
tionship occurred at the level of 0,05 (p <0,05) between the five statistically significant factors related to the survival from
survival from the arrest and 5 independent variables (Table 5): the arrest were found: The known history of heart disease, the
− Most of the patients who survived had known history of defibrillation rate, ventricular fibrillation as the rate of arrest
heart disease, while the majority of patients who did not and the out-of-hospital and in the Emergency Department
survive the arrest had no known history of heart disease defibrillation.
(p = 0,002). In particular, patients who came to the Emergency Department
− Most of the patients who survived the arrest had a shock- with a known history of heart disease, were more likely to sur-
able rhythm, while the majority of patients who did not vive than those without known heart disease (p = 0,002). In
survive the arrest had no shockable rhythm (p <0,001). Boyce et al. research, it was shown that the survival rate after
− The majority of the patients who survived had ventricular cardiac arrest could rise to 43%, taking into account factors
fibrillation as a rhythm of arrest, while the majority of pa- such as immediate onset of Cardiopulmonary Resuscitation by
tients who did not survive the arrest had asystole (p witnesses in the event, early defibrillation, and the known his-
<0,001). tory of heart disease. It was also found that 76% of cardiac
− Of all patients who received defibrillation, the largest per- arrest victims were of cardiological origin, with a known history
centage survived the arrest, while of all patients who did of heart disease.25 Respectively, Lee et al., in the research study
not receive defibrillation, the majority did not survive the which they carried out in 7 Asian countries from 2009 to 2012,
arrest (p <0,001). found a correlation between the known history of heart disease
− Most of the patients who survived the arrest received de- - as a single factor in their statistical analysis - and the increase
fibrillation during resuscitation in the Department, while in survival rates following cardiac arrest. However, when this
the majority of patients who did not survive the arrest did factor was associated with age and chronic health problems,
not receive defibrillation during the resuscitation in the the survival rate was low.26
Department (p <0,001). In the results of this study it was also found that the majority of
5.2 Survival and discharge from the hospital the patients who survived cardiac arrest had a shockable
None of the independent variables showed a statistically signif- rhythm, unlike those who did not (p <0,001). This finding is
icant correlation with survival and discharge from the hospital. consistent with a relative study of Blom et al., who correlating
the improvement of survival rate following cardiac arrest with
DISCUSSION the use of an automatic external defibrilator, showed an in-
Based on the results of this study, the percentage of patients creased survival rate with good neurological benefits in pa-
with return of circulation after the arrest was low (n=25, 11,9%). tients with shockable rhythms, unlike with those who had no
The percentage of patients who recovered from cardiac arrest shockable rhythms.27 Strömsöe et al. also came to a similar
and got discharged from the hospital (n=4, 1,9%) was lower, result, in Sweden, where they found an increased rate of sur-
while it was not possible to determine survival with discharge vival and return of spontaneous circulation in patients trans-
for patients transferred to other hospitals (n=4, 1,9%). Similar ferred to the Emergency Department with a shockable rhythm
results of low survival rates were reported by El Sayed et al., in versus patients with non-shockable rhythm.28
their own research study in Lebanon, where in a total of 205 According to this study, the majority of patients who survived,
Papadopoulou et al. 56 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
had ventricular fibrillation as an arrest rhythm, while the ma- store spontaneous circulation and improve survival rate. In
jority of patients who did not survive the arrest had asystole particular, at the initial stage of an evolving infarction, shocka-
(p<0,001). Bhandari et al. concluded in their study that the ble rhythms, as pathological electrical activities, are due to
shockable rhythms, such as ventricular fibrillation, shows a transient arrhythmogenic effects in ischemic and occlusive tis-
double survival rate after cardiac arrest, which reaches the 46%, sue, such as abnormal automatic function, triggered activity
over non-shockable rhythms, such as asystole, which has a and reentry circuits generated by the heterogeneous conduc-
survival rate of about 20%. 29
Subsequently, Boyce et al. in a tion and repolarization of ischemic cells. The sooner the cur-
relative survey, showed a correlation between the known histo- rent is given, by defibrillation, to the abnormal cells contrib-
ry of heart disease and the shockable rhythms, while they con- uting to the mechanism of arrhythmogenesis, the higher the
cluded that 52% of patients who had been transferred with rate of return to an organized rhythm with cardiac output. On
ventricular fibrillation as an arrest rhythm, had an improved the other hand, the more delayed the defibrillation delivery,
survival rate.25 Accordingly, Capucci et al. were led to the con- the lower the rates of success of return to an organized rhythm
clusion that shockable rhythms such as ventricular fibrillation, with cardiac output.34
do not only improve survival rates, but also neurological defi-
cits following an incident of arrest.18 Limitations
Another finding was with regard to the administration of defib- Despite attempts to minimize the limitations of the present
rillation in the ambulance. It appeared that most of the patients research, however they could not be eliminated. The sample
survived the arrest, in contrast to the patients who did not re- number is not particularly large so as to enable safe conclu-
ceive defibrillation in the ambulance (p <0,001). A similar con- sions to be drawn for the survival rate in the general popula-
clusion was reached by the research study of Hasegawa et al. tion, despite the fact that it is consistent with the international
where they showed survival rate for one month in arrest victims rates of other surveys. The small sample number also did not
who received 2 or less pre-hospital defibrillations, which allow for possible correlations of the studied factors with sur-
reached 34,48%.30 In the same conclusion came Garcia et al., in vival rates discharged from the hospital. The studied sample
a study which they carried out at international airports of derived from a single public hospital and specifically from the
France and Spain. They highlighted the importance of early cardiology infirmary, where all the cases of cardiac arrests were
pre-hospital defibrillation in order to improve the survival rate transferred in order to be treated. Finally, it was not possible to
in the Emergency Departments with good neurological bene- find information related to the discharge survival rate when
fits.
31
patients have been transferred to other hospitals of Attica (n =
Finally, according to the results of the present study, the arrest 4), after their return to spontaneous circulation.
victims who were defibrillated in the Emergency Department
showed a higher possibility of survival, as opposed to the pa- FUNDING
tients who did not receive any defibrillation in the hospital (p No funding. The operating expenses were covered by the prin-
<0,001). Both the American Cardiological Association, as well cipal researcher.
as the study by Pan et al. converge to the fact that during the
advanced cardiopulmonary resuscitation in Emergency De- CONCLUSIONS
partment, a defibrillation by a biphasic defibrillator, the use of The survival rate of the incoming patients with cardiac arrest at
energy <200J and the defibrillation prior to cardiopulmonary the emergency department of “Tzaneio” Hospital, Piraeus, was
resuscitation, improve the rate of return to spontaneous circu- low. The known cardiac history, the presence of a shockable
lation.32,33 The pathophysiology of shockable rhythms explains rhythm, ventricular fibrillation as a rhythm of arrest, defibrilla-
how direct current delivery to a cardiac arrest victim can re- tion at the ambulance and at the Emergency Department were
Papadopoulou et al. 57 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
strongly correlated with return of spontaneous circulation. Emerg Med. 2016;34(11):2101-6.
None of the studied factors was found to correlate with surviv- 9. Ha TS, Yang JH, Cho YH, Chung CR, Park CM, Jeon K, et al.
al and discharge from the hospital. As for most health systems, Clinical outcomes after rescue extracorporeal cardiopul-
this issue constitutes a fairly complex public health problem. monary resuscitation for out-of-hospital cardiac arrest.
Cardiopulmonary resuscitation and corresponding guidelines Emerg Med J. 2017;34(2):107-11.
require further improvement in order for the survival rates of 10. Fouche PF, Jennings PA. Physician presence at out-of-
out-of-hospital cardiac arrest patients to increase. hospital cardiac arrest is not necessarily the cause of im-
proved survival. Scand J Trauma Resusc Emerg Med.
2016;24(1):88.
REFERENCES 11. Sugiyama A, Duval S, Nakamura Y, Yoshihara K, Yannopou-
1. Kapadohos T. Cardiac Arrest. In: Marvaki Ch, Kotanidou A, los D. Impedance Threshold Device Combined With High-
Papageorgiou D, Kalogianni A (authors). Emergency Nurs- Quality Cardiopulmonary Resuscitation Improves Survival
ing (Book written in Greek). Athens: Konstantaras Medical With Favorable Neurological Function After Witnessed
Books; 2015. Pages 131-49. Out-of-Hospital Cardiac Arrest. Circ J. 2016;80(10):2124-
2. McCoy MA, Schultz AM. Exploring Strategies to improve 32.
cardiac arrest survival. United States of America: The 12. Girotra S, van Diepen S, Nallamothu BK, Carrel M, Vellano K,
Ntional Academies of press; 2017. Anderson ML, et al. Regional Variation in Out-of-Hospital
3. Ewy GA. The cardiocerebral resuscitation protocol for Cardiac Arrest Survival in the United States. Circulation.
treatment of out-of-hospital primary cardiac arrest. Scand 2016;133(22):2159-68.
J Trauma Resusc Emerg Med. 2012;20:65. 13. Benson-Cooper KA. Therapeutic hypothermia is inde-
4. Ogawa Y, Shiozaki T, Hirose T, Ohnishi M, Nakamori Y, pendently associated with favourable outcome after re-
Ogura H, et al. Load-distributing-band cardiopulmonary suscitation from out-of-hospital cardiac arrest: a retro-
resuscitation for out-of-hospital cardiac arrest increases spective, observational cohort study. N Z Med J.
regional cerebral oxygenation: a single-center prospective 2015;128(1427):33-7.
pilot study. Scand J Trauma Resusc Emerg Med. 14. Ageron FX, Debaty G, Gayet-Ageron A, Belle L, Gaillard A,
2015;23:99. Monnet MF, et al. Impact of an emergency medical dis-
5. Mangla A, Daya MR, Gupta S. Post-resuscitation care for patch system on survival from out-of-hospital cardiac ar-
survivors of cardiac arrest. Indian Heart J. 2014;66 Suppl rest: a population-based study. Scand J Trauma Resusc
1:S105-12. Emerg Med. 2016;24:53.
6. van de Glind EM, van Munster BC, van de Wetering FT, 15. Funada A, Goto Y, Maeda T, Teramoto R, Hayashi K, Yamag-
van Delden JJ, Scholten RJ, Hooft L. Pre-arrest predictors ishi M. Improved Survival With Favorable Neurological
of survival after resuscitation from out-of-hospital cardiac Outcome in Elderly Individuals With Out-of-Hospital Car-
arrest in the elderly a systematic review. BMC Geriatr. diac Arrest in Japan- A Nationwide Observational Cohort
2013;13:68. Study. Circ J. 2016;80(5):1153-62.
7. Youness H, Al Halabi T, Hussein H, Awab A, Jones K, Ked- 16. Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg
dissi J. Review and Outcome of Prolonged Cardiopulmo- J, Nordberg P, et al. Early cardiopulmonary resuscitation
nary Resuscitation. Crit Care Res Pract. in out-of-hospital cardiac arrest. N Engl J Med.
2016;2016:7384649. 2015;372(24):2307-15.
8. Jeong S, Ahn KO, Shin SD. The role of prehospital ad- 17. Oman G, Bury G. Use of telephone CPR advice in Ireland:
vanced airway management on outcomes for out-of- Uptake by callers and delays in the assessment process.
hospital cardiac arrest patients: a meta-analysis. Am J
Papadopoulou et al. 58 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
Resuscitation. 2016;102:6-10. after out-of-hospital cardiac arrest and possible associa-
18. Capucci A, Aschieri D, Guerra F, Pelizzoni V, Nani S, Villani tion with improvements in every link in the chain of sur-
GQ, et al. Community-based automated external defibril- vival. Eur Heart J. 2015;36(14):863-71.
lator only resuscitation for out-of-hospital cardiac arrest 29. Bhandari S, Doan J, Blackwood J, Coult J, Kudenchuk P,
patients. Am Heart J. 2016;172:192-200. Sherman L, et al. Rhythm profiles and survival after out-
19. Kitamura T, Kiyohara K, Matsuyama T, Izawa J, Shimamoto of-hospital ventricular fibrillation cardiac arrest. Resuscita-
T, Hatakeyama T, et al. Epidemiology of Out-of-Hospital tion. 2018;125:22-7.
Cardiac Arrests Among Japanese Centenarians: 2005 to 30. Hasegawa M, Abe T, Nagata T, Onozuka D, Hagihara A. The
2013. Am J Cardiol. 2016;117(6):894-900. number of prehospital defibrillation shocks and 1-month
20. Kuo CW, See LC, Tu HT, Chen JC. Adult out-of-hospital car- survival in patients with out-of-hospital cardiac arrest.
diac arrest based on chain of survival in Taoyuan County, Scand J Trauma Resusc Emerg Med. 2015;23:34.
northern Taiwan. J Emerg Med. 2014;46(6):782-90. 31. Garcia EL, Caffrey-Villari S, Ramirez D, Caron JL, Mannhart P,
21. Galatianou I, Karlis G, Apostolopoulos A, Intas G, Chalari E, Reuter PG, et al. [Impact of onsite or dispatched automat-
Gulati A, et al. Body mass index and outcome of out-of- ed external defibrillator use on early survival after sudden
hospital cardiac arrest patients not treated by targeted cardiac arrest occurring in international airports]. Presse
temperature management. Am J Emerg Med. Med. 2017;46(3):e63-e8.
2017;35(9):1247-51. 32. Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP,
22. Karagiannis C, Georgiou M, Kouskouni E, Iacovidou N, Xan- Moitra VK, et al. Part 7: Adult Advanced Cardiovascular
thos T. Association of lactate levels with outcome after in- Life Support: 2015 American Heart Association Guidelines
hospital cardiac arrest. Resuscitation. 2012;83(8):e175-6. Update for Cardiopulmonary Resuscitation and Emergen-
23. El Sayed MJ, Tamim H, Nasreddine Z, Dishjekenian M, Kazzi cy Cardiovascular Care. Circulation. 2015;132(18 Suppl
AA. Out-of-hospital cardiac arrest survival in Beirut, Leba- 2):S444-64.
non. Eur J Emerg Med. 2014;21(4):281-3. 33. Pan J, Zhu JY, Kee HS, Zhang Q, Lu YQ. A review of com-
24. Fan KL, Leung LP, Siu YC. Out-of-hospital cardiac arrest in pression, ventilation, defibrillation, drug treatment, and
Hong Kong: a territory-wide study. Hong Kong Med J. targeted temperature management in cardiopulmonary
2017;23(1):48-53. resuscitation. Chin Med J (Engl). 2015;128(4):550-4.
25. Boyce LW, Vliet Vlieland TP, Bosch J, Wolterbeek R, Volker 34. Podrid J, Ganz I. Pathogenesis of ventricular tachycardia
G, van Exel HJ, et al. High survival rate of 43% in out-of- and ventricular fibrillation during acute myocardial infarc-
hospital cardiac arrest patients in an optimised chain of tion. UpToDate. Waltham, MA: UpToDate; [Από:
survival. Neth Heart J. 2015;23(1):20-5. https://www.uptodate.com/contents/pathogenesis-of-
26. Lee MH, Fook-Chong S, Wah W, Shin SD, Nishiuchi T, Ko ventricular-tachycardia-and-ventricular-fibrillation-
PC, et al. Effect of known history of heart disease on sur- during-acute-myocardial-infarction
vival outcomes after out-of-hospital cardiac arrests.
Emerg Med Australas. 2018;30(1):67-76.
27. Blom MT, Beesems SG, Homma PC, Zijlstra JA, Hulleman M,
van Hoeijen DA, et al. Improved survival after out-of-
hospital cardiac arrest and use of automated external de-
fibrillators. Circulation. 2014;130(21):1868-75.
28. Stromsoe A, Svensson L, Axelsson AB, Claesson A, Gorans-
son KE, Nordberg P, et al. Improved outcome in Sweden
Papadopoulou et al. 59 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
ANNEX
TABLE 1. Demographic characteristics of incoming victims with cardiac arrest to Emergency Department
Characteristic Ν (%)
Gender
Female 61 (29,0)
Male 149 (71,0)
Agea 66,6 (15,4)
Age Groups
<51 years old 38 (18,1)
51-60 years old 29 (13,8)
61-70 years old 51 (24,3)
71-80 years old 50 (23,8)
>80 years old 42 (20,0)
Values are expressed as absolute (N) and relative (%) frequency unless stated otherwise.
a Mean
value (standard deviation)
Papadopoulou et al. 60 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
TABLE 2. Characteristics according to the history of heart disease of incoming patients with cardiac arrest to the Emergency Depart-
ment
Characteristic Ν (%)
Known history of heart disease
No 148 (70,5)
Yes 62 (29,5)
Type of heart disease
Coronary Disease 41 (19,5)
Heart Failure 11 (5,2)
Acute myocardial infarction 9 (4,3)
Valvulopathy 1 (0,5)
Unknown history of heart disease 148 (70,5)
Values are expressed as absolute (N) and relative (%) frequency
Papadopoulou et al. 61 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
TABLE 3: Data in relation to the arrest
Characteristic Ν (%)
Transfer by National Emergency Center
No 4 (1,9)
Yes 206 (98,1)
Arrest rhythm at the arrival at Emergency Department
Ventricular fibrillation 11 (5,2)
Abdominal Tachycardia without pulse 5 (2,4)
Asystole 183 (87,1)
Electrical Activity without pulse 11 (5,2)
Shockable rhythm
No 194 (92,4)
Yes 16 (7,6)
Defibrilation in the ambulance
No 195 (92,9)
Yes 15 (7,1)
Defibrilation in the Emergency Department
No 194 (92,4)
Yes 16 (7,6)
Number of total defibrillations at the Emergency Department
1 3 (1,4)
2 12 (5,7)
7 1 (0,5)
They didn’t receive defibrilation 194 (92,4)
Time from detecting the arrest until the end of resuscitation 54,6 (19,9) / 51,0 (21,0)
(minutes)a/b
Time of resuscitation in the ambulance (minutes)a/b 31,8 (115,7) / 18,0 (13,0)
Time of resuscitation in the hospital (minutes) a/b
22,7 (12,8) / 20,0 (14,0)
Total time of resuscitation (ambulance+hospital) (minutes)a/b 54,5 (117,6) / 40,5 (21,0)
Values are expressed as absolute (N) and relative (%) frequency unless stated otherwise.
a/b
Mean value (standard deviation) / Median (interquartile range)
Papadopoulou et al. 62 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
TABLE 4: Outcome
Characteristic Ν (%)
Survival from the arrest
No 185 (88,1)
Yes 25 (11,9)
Survival and discharge from the hospital
No 17 (8,1)
Yes 4 (1,9)
We don’t know (they were transferred to other hospital) 4 (1,9)
The rates are expressed as absolute N frequency and relative frequency (%).
Papadopoulou et al. 63 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
Table 5: Bivariate correlations between demographic and other characteristics and the survival from the arrest
Survival from the arrest
Characteristic Rate p
No Yes
Gender 0,729a
Female 53 (28,6) 8 (32,0)
Male 132 (71,4) 17 (68,0)
Ageb 66,2 (15,5) 69,5 (14,4) 0,315c
Known history of heart disease 0,002a
No 137 (74,1) 11 (44,0)
Yes 48 (25,9) 14 (56,0)
Type of heart disease 0,249d
Coronary Disease 33 (68,8) 8 (57,1)
Heart Failure 9 (18,8) 2 (14,3)
Acute myocardial infarction 6 (12,5) 3 (21,4)
Valvulopathy 0 (0,0) 1 (7,1)
Transfer by National Emergency Center 0,070e
No 2 (1,1) 2 (8,0)
Yes 183 (98,9) 23 (92,0)
Defibrilating rate <0,001e
No 182 (98,4) 12 (48,0)
Yes 3 (1,6) 13 (52,0)
Arrest rate at the arrival at Emergency Department <0,001d
Ventricular fibrillation 2 (1,1) 9 (36,0)
Abdominal Tachycardia without pulse 1 (0,5) 4 (16,0)
Asystole 175 (94,6) 8 (32,0)
Electrical Activity without pulse 7 (3,8) 4 (16,0)
Defibrilation in the ambulance <0,001e
No 180 (93,3) 13 (6,7)
Yes 4 (26,7) 11 (73,3)
Defibrilation during resuscitation in the Emergency De-
<0,001e
partment
No 182 (98,4) 12 (48,0)
Yes 3 (1,6) 13 (52,0)
Number of total defibrilations at the Emergency De-
2,0 (0,0) 2,0 (0,0) 0,638g
partment f
Time from detecting the arrest until the end of resusci-
54,3 (18,9) 57,3 (26,6) 0,587c
tation (minutes)b
Time of resuscitation in the ambulance (minutes)f 13,0 (0,0) 14,0 (12,3) 0,632g
Papadopoulou et al. 64 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
(2019), Volume 5, Issue 2
Time of resuscitation in the hospital (minutes)f 41,0 (0,0) 20,5 (5,5) 0,532g
Total time of resuscitation (ambulance+hospital)
57,0 (0,0) 35,5 (18,0) 0,937g
(minutes)f
Values are expressed as n (%) unless stated otherwise.
a
X2 test
b
Mean value (standard deviation)
c
t test
d
Monte-Carlo exact test
e Fisher’s exact test
f
Median (interquartile range)
g
Mann-Whitney test
Papadopoulou et al. 65 https://ejournals.epublishing.ekt.gr/index.php/HealthResJ
http://epublishing.ekt.gr | e-Publisher: EKT | Downloaded at 01/12/2019 10:39:55 |
Powered by TCPDF (www.tcpdf.org)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Trends in Survival After In-Hospital Arrest During Nights and Weekends 2018Document10 pagesTrends in Survival After In-Hospital Arrest During Nights and Weekends 2018Yannis ZoldenbergNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Vettius Valens EntireDocument172 pagesVettius Valens Entirecobalt_cannonNo ratings yet
- Location of In-Hospital Cardiac Arrest in The United States 2016Document8 pagesLocation of In-Hospital Cardiac Arrest in The United States 2016Yannis ZoldenbergNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- MasteringChemistry ConstantsDocument3 pagesMasteringChemistry ConstantsYannis ZoldenbergNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Out-Of-hospital Cardiac Arrest Survival in Athens 2019Document5 pagesOut-Of-hospital Cardiac Arrest Survival in Athens 2019Yannis ZoldenbergNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Brentons Mcat GuideDocument20 pagesBrentons Mcat GuideYannis ZoldenbergNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- @anesthesia Books 2011 PracticalDocument254 pages@anesthesia Books 2011 PracticalSuci RamadhaniKhairiNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Chap. 2. Water (Part B) : TopicsDocument25 pagesChap. 2. Water (Part B) : TopicsSamyaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Mrocwal 1Document133 pagesMrocwal 1Yannis ZoldenbergNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Chap. 2. Water (Part B) : TopicsDocument25 pagesChap. 2. Water (Part B) : TopicsSamyaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- s15 Miller Chap 2a LectureDocument19 pagess15 Miller Chap 2a LectureYannis ZoldenbergNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Life SupportDocument1 pageLife SupportYannis ZoldenbergNo ratings yet
- Perceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesDocument6 pagesPerceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesYannis ZoldenbergNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- s15 Miller Chap 2 ProblemsDocument11 pagess15 Miller Chap 2 ProblemsYannis ZoldenbergNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A01628 CH19Document36 pagesA01628 CH19Yannis ZoldenbergNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 2007 Monitoring in The Intensive Care Unit PDFDocument326 pages2007 Monitoring in The Intensive Care Unit PDFYannis ZoldenbergNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- 2009 PiCCO Advanced Hemodynamic Monitoring PDFDocument15 pages2009 PiCCO Advanced Hemodynamic Monitoring PDFYannis ZoldenbergNo ratings yet
- COVID 19 Infection Prevention and Control Healthcare Settings March 2020Document10 pagesCOVID 19 Infection Prevention and Control Healthcare Settings March 2020Adrian RuxandaNo ratings yet
- The Body in Balance3 PDFDocument5 pagesThe Body in Balance3 PDFYannis ZoldenbergNo ratings yet
- Commonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFDocument12 pagesCommonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFYannis Zoldenberg100% (1)
- ΈγγραφοeDocument1 pageΈγγραφοeYannis ZoldenbergNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ΈγdfgφοDocument1 pageΈγdfgφοYannis ZoldenbergNo ratings yet
- Annual Incidence of Adult and Pediatric in Hospital Cardiac Arrest in The U.S 2019Document8 pagesAnnual Incidence of Adult and Pediatric in Hospital Cardiac Arrest in The U.S 2019Yannis ZoldenbergNo ratings yet
- T - 14.5. N.A. Pupils 9.1 PDFDocument2 pagesT - 14.5. N.A. Pupils 9.1 PDFYannis ZoldenbergNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Advanced Life Support (Training Manual)Document74 pagesAdvanced Life Support (Training Manual)Matt100% (25)
- Wisdom of The EgoDocument1,041 pagesWisdom of The EgoYannis Zoldenberg100% (1)
- Wisdom of The EgoDocument1,041 pagesWisdom of The EgoYannis Zoldenberg100% (1)
- DebusyDocument1 pageDebusyYannis ZoldenbergNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- SopernhouredDocument1 pageSopernhouredYannis ZoldenbergNo ratings yet
- Angiographic ProjectionsDocument16 pagesAngiographic ProjectionsKarren_M888No ratings yet
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- How To Choose A Medical Specialty Fifth Edition 20Document254 pagesHow To Choose A Medical Specialty Fifth Edition 20Sosakkada80% (5)
- GuidelinesDocument4 pagesGuidelinesChidambaram SeevakanNo ratings yet
- Pals Pediatric BradycardiaDocument1 pagePals Pediatric BradycardiadarlingcarvajalduqueNo ratings yet
- Cardiomegaly, RadiologyDocument20 pagesCardiomegaly, RadiologyJia LingNo ratings yet
- Polycystic Kidney DiseaseDocument15 pagesPolycystic Kidney DiseaseSabita TripathiNo ratings yet
- Anti Arrhythmic DrugsDocument22 pagesAnti Arrhythmic DrugsHarsheethaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofahmadto80No ratings yet
- Minimum Standard Requirements For 150 Admissions PDFDocument93 pagesMinimum Standard Requirements For 150 Admissions PDFimtiazNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gambaran Disfungsi Diastolik Pada Pasien 7414b2baDocument7 pagesGambaran Disfungsi Diastolik Pada Pasien 7414b2baAmelNo ratings yet
- AfDocument35 pagesAfEmman AbelardoNo ratings yet
- High Yield Cardiology Internal Medicine Shelf PDFDocument44 pagesHigh Yield Cardiology Internal Medicine Shelf PDFsaja fuadNo ratings yet
- EKG Clep TestDocument13 pagesEKG Clep TestElissa LafondNo ratings yet
- Cardiac Tamponade Management Clinical GuidelineDocument20 pagesCardiac Tamponade Management Clinical Guidelinealejandro montesNo ratings yet
- Klinik Bornmeds Stress Exercise Report: Stress ECG Analysis SystemDocument1 pageKlinik Bornmeds Stress Exercise Report: Stress ECG Analysis SystemMagenta GamingNo ratings yet
- FC62F7D4 CToDocument99 pagesFC62F7D4 CToRanda TabbahNo ratings yet
- Echocardiography PDFDocument4 pagesEchocardiography PDFDualaut AndiNo ratings yet
- RCP Consultant Physicians Working With PatientsDocument266 pagesRCP Consultant Physicians Working With PatientsalaaNo ratings yet
- Cardioembolic StrokeDocument13 pagesCardioembolic StrokeAzarel JimmyNo ratings yet
- Pemicu 1A Blok KGD - FK UNTARDocument72 pagesPemicu 1A Blok KGD - FK UNTARaindrawantoNo ratings yet
- Cardiovascular MCQs For Pharmacology ReviewDocument14 pagesCardiovascular MCQs For Pharmacology ReviewBhopesh Kadian38% (8)
- Classic Imaging Signs of Congenital Cardiovascular Abnormalities 1Document45 pagesClassic Imaging Signs of Congenital Cardiovascular Abnormalities 1adhik_deepakNo ratings yet
- Association of Serum Magnesium On Mortality in Patients Admitted To The Intensive Cardiac Care UnitDocument9 pagesAssociation of Serum Magnesium On Mortality in Patients Admitted To The Intensive Cardiac Care UnitDr Mohammed Nizam UddinNo ratings yet
- Acute Coronary SyndromesDocument8 pagesAcute Coronary Syndromesadek07No ratings yet
- Ventricular Arrythmias: Junctional TachycardiaDocument1 pageVentricular Arrythmias: Junctional TachycardiaLwin Maung Maung ThikeNo ratings yet
- Rhythm Summary Review Packet EKG CLassDocument12 pagesRhythm Summary Review Packet EKG CLassmisslhen.rn04No ratings yet
- Gravido CardiacDocument19 pagesGravido CardiacOUR LADY OF FATIMA UNIVERSITY COLLEGENo ratings yet
- Atrial FlutterDocument17 pagesAtrial FlutterEdRobertArnadNo ratings yet
- Nursing CS Acute-Kidney-Injury 04Document1 pageNursing CS Acute-Kidney-Injury 04Mahdia akterNo ratings yet