Professional Documents
Culture Documents
8721 1nh7pex
Uploaded by
Deepak JainOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8721 1nh7pex
Uploaded by
Deepak JainCopyright:
Available Formats
Open Access Original
Article DOI: 10.7759/cureus.32218
Efficacy and Safety of Inhalation of Nebulized
Ethanol in COVID-19 Treatment: A Randomized
Review began 11/22/2022
Clinical Trial
Review ended 12/01/2022
Published 12/05/2022 Ali Amoushahi 1 , Elham Moazam 2 , Amin Reza Tabatabaei 3 , Golnaz Ghasimi 3 , Ian Grant-Whyte 4 , Pietro
Salvatori 5 , Ahmed Ragab Ezz 6
© Copyright 2022
Amoushahi et al. This is an open access
article distributed under the terms of the 1. Anesthesiology and Intensive Care Unit, Isfahan University of Medical Sciences, Isfahan, IRN 2. Cancer Prevention
Creative Commons Attribution License CC- Research Center, Isfahan University of Medical Sciences, Isfahan, IRN 3. Internal Medicine, Isabn-e-Maryam Hospital,
BY 4.0., which permits unrestricted use, Isfahan University of Medical Sciences, Isfahan, IRN 4. Family Medicine, Retired, Pointe-Claire, CAN 5.
distribution, and reproduction in any
Otolaryngology, Humanitas San Pio X, Milano, ITA 6. Anesthesiology, Mansoura University, Mansoura, EGY
medium, provided the original author and
source are credited.
Corresponding author: Pietro Salvatori, 3356645502@tim.it
Abstract
Background: Coronavirus disease 2019 (COVID-19) is a pandemic caused by the SARS-CoV-2 virus. Many
efforts have been made and are currently being made to prevent and treat this global disease.
Objectives: This study was designed to evaluate the efficacy and safety of nebulized ethanol (EtOH) in
treating COVID-19.
Methods: A randomized clinical trial (RCT) of 99 symptomatic and real-time polymerase chain reaction (RT-
PCR)-positive patients admitted to a hospital receiving remdesivir-dexamethasone was conducted. They
were randomly assigned to receive distilled water spray (control group (CG)) or 35% EtOH spray
(intervention group (IG)). Both groups inhaled three puffs of spray (nebulizer) every six hours for a week.
The primary outcome included Global Symptomatic Score (GSS) between the two groups at the first visit and
on days three, seven, and 14. Secondary outcomes included the Clinical Status Scale (CSS; a seven-point
ordinal scale ranging from death to complete recovery) and readmission rate.
Results: A total of 44 and 55 patients were enrolled in the IG and CG, respectively. Although there was no
difference at admission, the GSS and CSS improved significantly in the IG (p = 0.016 and p = 0.001,
respectively). The IG readmission rate was considerably lower (0% vs. 10.9%; p = 0.02).
Conclusions: Inhaled-nebulized EtOH is effective in rapidly improving the clinical status and reducing
further treatment. Due to its low cost, availability, and absent/tolerable adverse events, it could be
recommended as an adjunctive treatment for moderate COVID-19. Further research on curative effects in
more serious cases and in prevention is advisable.
Categories: Infectious Disease, Pulmonology, Public Health
Keywords: nebulized ethanol, coronavirus disease, coronavirus disease 2019, sars-cov-2, nebulizer, inhalation,
ethanol, covid-19
Introduction
The in vitro antiviral effects of ethanol (EtOH) on solving the fat layer [1] and destroying the glycoprotein of
coronavirus have already been established [2]. The antiviral effects of EtOH on extracellular surfaces have
been demonstrated previously [3]. Immunological studies have shown that acute administration of ethanol
can have immunomodulatory effects on the innate immune system mediated by tumor necrosis factor-α
(TNF-α) mRNA protein and mitogen-activated protein kinase, and can reduce cytokine storm by reducing
inflammatory factors such as toll-like receptor (TLR), toll-like receptor 9 (TLR9), and interleukin-6 [4,5]. It
also helps in the chemotaxis of bronchoalveolar macrophages [6]. Other demonstrated effects of ethanol
include virus replication by inhibition of RNA-dependent polymerase [7], bronchial dilation by relaxing
involuntary smooth muscles [8], sedation and relaxation of the patient [9], and muscular analgesic effects
[10]. Ethanol administration has previously been reported to treat methanol poisoning [11], fat embolism
[12], prevention of preterm labor [13], preeclampsia [14], and pulmonary edema [15]. The histological safety
of inhalation ethanol therapy in the lungs and respiratory tracts of rodents has been demonstrated by
Castro-Balado et al. [16]. The Food and Drug Administration approved ethanol. Cytokine storms cause many
deaths due to the coronavirus disease 2019 (COVID-19) [17]. Given the actions of ethanol on virus wall
destruction, inhibition of proliferation, and inhibition of immune hyperactivity, the question now is, "Can
ethanol inhalation therapy be effective in controlling COVID-19?" There is no knowledge about inhaled
ethanol therapy for COVID-19. This idea was first suggested and published one month after Iran's COVID-
19 pandemic (February 2020) [18,19]. Later, a study dealing with the rationale for ethanol use in this field
was presented [20]. A randomized clinical trial (RCT) evaluating the combined administration of dimethyl
How to cite this article
Amoushahi A, Moazam E, Tabatabaei A, et al. (December 05, 2022) Efficacy and Safety of Inhalation of Nebulized Ethanol in COVID-19
Treatment: A Randomized Clinical Trial. Cureus 14(12): e32218. DOI 10.7759/cureus.32218
sulfoxide and ethanol recently showed considerable COVID-19 prevention in healthcare providers [21]. To
try to find the answer, we conducted a randomized clinical trial aimed at evaluating the effectiveness of
ethanol therapy on the clinical status and prognosis of a defined set of patients. The study was approved by
the Research and Ethics Committee of the School of Medicine, Isfahan University of Medical Sciences, and
registered at the Iranian Registry of Clinical Trials (https://irct.ir/trial/58201).
This article was previously posted to the medRxiv preprint server on June 23, 2022.
Materials And Methods
Study design and oversight
This study is a randomized, double-blind, clinical trial with a control group and parallel design that was
conducted at the Isabn-e-Maryam Hospital at the Medical University of Isfahan, Iran, in September 2021
(Figure 1). The patients were randomly assigned in a 1:1 ratio. The study was originally intended for patients
admitted to the hospital; however, due to amending the country's policy of setting up respiratory clinics in
hospitals and prescribing remdesivir and dexamethasone to patients with moderate COVID-19, the study
was conducted in this clinic. Physicians of hospitalized patients were informed about the patient's referral to
the respiratory clinic and this study.
FIGURE 1: Study flowchart
Patients
The study population consisted of polymerase chain reaction (PCR)-positive SARS-CoV-2 patients. They had
moderate COVID-19 based on the national guideline for COVID-19 management, i.e., oxygen saturation =
90-94% or lung involvement [22], referred to the respiratory clinic of the hospital. Inclusion criteria were as
follows: agreeing to implement the plan in the form of informed consent, age over 12 years, no pregnancy,
no history of asthma, alcoholism, or epilepsy, no contraindications to ethanol, and use of drugs that interact
with ethanol. Exclusion criteria were intolerance to inhaled ethanol and partial or incomplete treatment. An
ethanol patch skin test was used to detect possible alcohol allergies. In this experiment, a drop of ethanol
was placed on a gauze pad and attached to the patient's arm. After approximately seven minutes, symptoms,
such as redness, swelling, or itching of the skin, were observed. These symptoms indicate the possibility of
allergy or intolerance to alcohol.
Intervention
Both the control group (CG) and intervention group (IG) were enrolled in the standard treatments based on
the national clinical guidelines of Iran [21]. The national standard treatment included intramuscular
dexamethasone 8 mg/day for five days, and 200 mg of remdesivir intravenously on day one, followed by 100
mg of remdesivir once daily for four days, infused over 30-60 minutes. In addition to the standard
treatment, patients were randomly assigned to either the CG (distilled water spray) or the IG (35% ethanol
spray). Two sets of 100 ml spray were provided and delivered according to randomization. All patients were
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 2 of 11
instructed to spray the mask three times a day (every six to eight hours) and take deep breaths. We
emphasized that this protocol had to be repeated for seven days, depending on the persistence of symptoms.
Patients were taught by nurses until they were able to manage the procedure and were then allowed to do it
on their own. Patient compliance was assessed at all referrals and follow-up appointments. Failure to adhere
to the protocol (spray not used or irregularly used) resulted in withdrawal from the study.
Clinical and laboratory monitoring
The data collection sheet consisted of two sections: demographic and clinical information. Demographic
information was obtained from the patient's records and the data collection checklist was completed by a
trained nurse based on clinical symptoms, clinical results, and clinical examination. Data related to research
variables, including blood oxygen saturation in pulse oximetry, need for adjunctive treatment or
readmission in the hospital, and clinical symptoms in both groups, were collected until discharge.
Study outcomes
Primary Outcomes
The Global Symptomatic Score (GSS) is considered an indicator of the clinical status of patients and
is achieved by calculating the cumulative scores of clinical signs and symptoms, including fever, headache,
body aches, sore throat, runny nose, chills, cough, shortness of breath, anorexia, loss of smell, and loss of
taste. This index was designed to summarize clinical symptoms in the form of one index.
Oxygenation status was monitored and recorded daily using a pulse oximeter. The pulse oximeter was fixed,
and the patient was breathing room air at the time of measurement without supplemental
oxygen. Inflammatory status was defined as the variation in serum C-reactive protein (CRP) levels.
Secondary Outcomes
A modified seven-point ordinal scale was used to assess clinical conditions on day 14 of the treatment period
related to research [23]. This scale includes seven indices: (1) death; (2) hospitalized, on invasive mechanical
ventilation; (3) hospitalized, non-invasive ventilation or high-flow oxygen devices; (4) hospitalized,
requiring low-flow supplemental oxygen; (5) hospitalized, for whatever reason, requiring ongoing medical
care (related to COVID-19 or otherwise), requiring supplemental oxygen at home; (6) continued signs or
symptoms of COVID-19 without requiring supplemental oxygen, no longer require ongoing medical care;
(7) complete recovery and any possible side effects were reported and treated in both groups. The need for
hospitalization in the intensive care unit, drug side effects, clinical symptoms, and mortality of the research
samples were recorded and monitored in both groups. The final follow-up was performed on the 14th day of
the disease. The last follow-up was performed on the 14th day of the disease. During follow-up, physical
examinations, history, telephone calls, review of patient records, and hospital information system
documents were used. Side effects were recorded after obtaining informed consent. We have made some
changes to the primary endpoints. This was because of the limitations that occurred at the same time as the
peak of the disease in Iran with the implementation of this study, and patients who needed to be
hospitalized were followed up on an outpatient basis in the respiratory clinic. We provided a detailed account
of the changes in the protocol to the sponsor and the institutional review board. The main predicted
outcome was the length of stay. During the surge, all moderate patients were treated on a five-day schedule;
therefore, this index was replaced with a more comprehensive clinical status.
Sampling
Sampling was performed using an easy random sampling method. A computerized random number table was
used for random assignment. One nurse determined the sequence of random allocations. She kept the
randomization list private and allocated each person if they were eligible and consented to the trial. Another
nurse filled the sprays (nebulizer) one by one with 100 ml of diluted distilled water or ethanol (35%) and
labeled them with the numbers coming out of the list one by one. Each spray was delivered to one of the
participants, and their family or companion was instructed on how to use it. Clinicians, nurses, and analysts
performed blinding.
Statistical analysis
We calculated that 88 patients (44 in each group) would provide greater than 90% power to detect an odds
ratio of 3 for the ethanol group versus the placebo group using a two-sided significance level of 0.05. Based
on the "treatment-on" or "per-protocol" strategy, analysis was limited to participants who, according to the
study protocol and inclusion criteria, received full interventions and informed the outcomes. Quantitative
and qualitative variables were reported as descriptive statistics, including means, standard deviations, and
numbers (%). Qualitative variables were compared between the two groups using the chi-square test, and
comparisons between oxygen saturation (SpO2) values and GSS on days one, three, seven, and 14 were
performed using a mixed model. The mean changes in baseline values were measured using repeated-
measures analysis. The sphericity hypothesis was rejected with the help of Mauchly's statistics, and the
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 3 of 11
Geisser-Greenhouse correction was used for this purpose. The proportion of patients who needed additional
medical care after 14 days was tested in the two groups using the χ2 test, which was performed at zero,
three, seven, and 14 days after the intervention, and cumulative odds ordinal logistic regression with
proportional odds was used to compare clinical status between the two groups on day 14. An odds ratio
greater than 1 indicated changes in clinical status across all categories toward category seven for the
intervention group vs. the standard care group. For clinical status, if a patient recovered, the ordinal score
was recorded as 7 on the day of recovery and all subsequent days unless the patient was hospitalized for
COVID-19-related reasons or others. All statistical analyses were performed using SPSS version 22 (IBM
Corp., Armonk, NY), and p < 0.05 was considered significant. The patient's gender variable was controlled in
the outcome indicators.
Results
Patient characteristics
In this study, 150 patients from the COVID-19 respiratory outpatient clinic of Isabn-e-Maryam Hospital of
Isfahan University of Medical Sciences were evaluated for inclusion based on the positive result of the real-
time polymerase chain reaction (RT-PCR) test, from September to November 2021. Two patients did not
meet the inclusion criteria and 24 patients did not agree with the study. The remaining 124
patients were randomly assigned into two groups (intervention and control). Twenty-five patients
were then excluded from the study, due to intolerance to ethanol inhalation (six patients); hiccups, eye
irritation, cough, shortness of breath, sneezing, and the unpleasant smell of alcohol were the main reasons
for their intolerance. On the other hand, 19 patients (10 in the IG and nine in the CG) were excluded from
the study due to irregularity or not following the recommended method. Finally, 99 patients entered the
analysis: 44 patients in the IG and 55 patients in the CG.
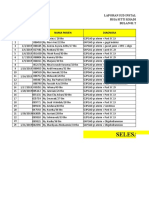
Table 1 shows the demographic and baseline characteristics of patients in the two groups. The male/female
ratio was 43/56 patients (42.4/56.6%). The mean age of patients was 46.4 years. Thirty-eight patients had
comorbidities. The most common underlying disease in both groups was diabetes mellitus: four (7%) in the
CG and six (14.3%) in the IG. Seven patients had hypertension and seven patients had other cardiovascular
problems. The two groups did not have significant differences in terms of mean age, weight, level of
education, and the number of risk factors.
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 4 of 11
Intervention group (N = 44, 44.4%) Control group (N = 55, 55.6%)
Age (years), mean (±SD) 45.91 (±12.58) 46.15 (±13.15)
BMI, N (%)
Normal weight 9 (20.5) 16 (29.1)
Overweight 22 (50) 25 (45.5)
Obesity 10 (22.7) 10 (20)
Excessive obesity 3 (6.8) 3 (5.5)
Gender, N (%)
Female 19 (43.2) 37 (67.3)
Male 25 (56.8) 18 (32.7)
Education level, N (%)
Illiterate and elementary 8 (16.3) 3 (5.4)
Secondary 7 (14.3) 8 (14.3)
Diploma 16 (32.7) 28 (50)
Bachelor-higher 16 (30.6) 16 (26.8)
Unknown 3 (6.1) 2 (3.6)
Risk factors for disease, N (%)
None 38 (69.1) 23 (52.3)
1 risk factor 12 (21.8) 19 (43.2)
2 risk factors 4 (7.3) 2 (4.5)
3 risk factors 1 (1.8) 0
TABLE 1: Demographics
Clinical signs and symptoms at the time of admission
Patients also did not differ significantly in the time distance between the onset of symptoms and admission,
pulmonary involvement, and early clinical signs and symptoms at baseline. The basic characteristics of the
patient's clinical signs and symptoms are given in Table 2.
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 5 of 11
Intervention group (N = 44, 44.4%) Control group (N = 55, 55.6%)
Delay from symptoms onset to treatment, mean (±SD) 8.50 (±3.52) 9.36 (±5.13)
Pulmonary involvement (CT scan)
Less than 30% 19 (43.2) 22 (40)
30-49% 15 (34.1) 25 (45.5)
50% or more 2 (4.5) 2 (3.6)
Unknown 8 (18.2) 6 (10.9)
Fever 25 (56.8) 21 (38.2)
Chills 30 (68.2) 35 (63.6)
Cough 41 (95.3) 49 (89.1)
Headache 30 (68.2) 35 (63.6)
Short breath 24 (54.5) 37 (67.3)
Sore throat 16 (36.4) 27 (49)
Rhinorrhea 9 (20.5) 18 (32.7)
Body pain 36 (65.5) 36 (65.5)
Anorexia 29 (65.9) 38 (69.1)
Anosmia 26 (59.1) 39 (70.9)
Lack of taste 27 (61.4) 32 (58.2)
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 6 of 11
Global Symptomatic Score (GSS) 6.72 (2.07) 6.67 (2.09)
TABLE 2: Baseline signs and symptoms, risk factors, and laboratory values
The primary clinical symptoms in the IG were cough, body aches, chills, and headaches. Cough, olfactory
disturbance, and anorexia were more common in the CG. No significant difference was observed in
symptoms.
Global symptomatic score
The GSS at the beginning of treatment and after three, seven, and 14 days of treatment was assessed in two
groups. The results are shown in Figure 2.
FIGURE 2: Comparison of mean Global Symptomatic Score (GSS)
between the intervention and the control groups at admission, and days
three, seven, and 14 after admission
Statistical analysis showed that the GSS of the two groups was the same at the beginning of the study, but in
the IG, the clinical symptoms decreased more than in the placebo group and more rapidly. This difference
was statistically significant (p = 0.016).
Blood oxygen saturation
There was no significant difference in blood oxygen saturation between the two groups at the time of the
study (92.07 ± 4.6 in the CG vs. 91.56 ± 3.39 in the IG). As can be seen in Figure 3, blood oxygenation
improved in both groups and the slope of oxygenation was higher in the ethanol group. Although, this
difference is not statistically significant (p = 0.097).
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 7 of 11
FIGURE 3: Comparison of mean blood oxygen saturation (SpO2)
between the intervention and the control groups at admission, and days
three, seven, and 14 after patient admission
Inflammatory factor (CRP)
Multiple measurements and statistical analysis of the two groups showed that CRP had a decreasing trend
(Figure 4), but in the IG, the rate of reduction was more rapid and intense, in a significant way (p = 0.05).
FIGURE 4: Comparison of C-reactive protein between the intervention
and control groups at admission and three days after patient admission
Clinical status scale
CSS based on the modified seven-point ordinal scale was compared in two groups. On day 14, the odds of the
IG having better CSS were 5.7 times higher (95% CI: 2.47-13.19) than that of the CG, with a statistically
significant effect: Wald χ2 (1) = 16.67 and p = 0.001. Details are shown in Table 3.
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 8 of 11
Intervention (N = Control (N =
Characteristic and score, N (%)
44) 55)
Death 0 0
Hospitalized, on invasive mechanical ventilation 0 0
Hospitalized, on non-invasive ventilation or high-flow oxygen devices 0 0
Hospitalizations for any reason and need oxygen 0 2 (3.63)
Requiring ongoing medical care or supplemental oxygen at home 2 (4.54) 10 (18.18)
Continue signs or symptoms without requiring supplemental oxygen - no longer requires ongoing
13 (29.54) 29 (52.72)
medical care
Complete recovery 29 (65.90) 14 (25.45)
TABLE 3: Clinical Status Scale (CSS) on day 14 from admission
After the end of the treatment period in the CG, six patients (10.9%) were readmitted to receive additional
treatment or hospitalization. In the ethanol group, none of the patients were readmitted (p = 0.02).
Adverse events and safety
Six out of 50 patients in the ethanol group (12%) stopped using it because of adverse events at the onset of
inhalation and we excluded them from the study. No more than one case was observed for each side effect
and that side effect disappeared after stopping ethanol use. Adverse events included hiccups, eye irritation,
cough, shortness of breath, sneezing, and an unpleasant odor of alcohol.
Discussion
In this clinical trial, patients with positive RT-PCR test, moderate clinical symptoms, and suitable for
remdesivir and dexamethasone treatment (according to the Iran Ministry of Health protocol) were included
and the effect of adding nebulized inhalation was studied. The rationale for using EtOH in COVID-19 has
been extensively treated [20].
Experimental and clinical data leave no doubt about the effect of ethanol on destroying or inactivating
SARS-CoV-2, even at concentrations as low as 30% v/v and for a short time (30 seconds)
[24]. The EtOH viricidal properties rely on the dissolution of the virus fat layer and subsequent inhibition of
its proliferation. In addition, EtOH has been shown to mitigate the hyperactivity of the immune system
during COVID-19. Ethanol is likely ineffective against intracellular viruses.
Since viral replication occurs in 48-72 hours, followed by cellular death and shedding, it is important to
prolong ethanol inhalation for at least three days. Moreover, thanks to its non-specificity, ethanol is
intrinsically effective on any SARS-CoV-2 variant and other “enveloped” viruses.
Worse outcomes in ICU patients were related to the abnormal presence of Mycoplasma salivarium in the
lower tract or Clostridia absence in the upper tract [25]. Interestingly, it should be noted that Mycoplasma
and SARS-CoV-2 are completely inactivated by ethanol [26]. Moreover, certain Clostridia strains produce
endogenous ethanol [27]. Hypothetically, the absence of nasopharyngeal Clostridia could lead to a lack of
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 9 of 11
local ethanol production and therefore reduced/absent inactivation of SARS-CoV-2 at this level, thus
allowing the virus to spread to the lower respiratory tract.
Concerns about the mucosal damage that inhaled ethanol could induce locally have been frequently and
strongly raised. The meticulous work of Castro-Balado et al. [16] seems to have definitively eliminated these
concerns.
When evaluating methods, it should be highlighted that spraying into the mask reduces the nebulized
liquid's dispersion and evaporation, leading to a longer-lasting action, and maintaining its efficacy. A
possible unavoidable bias is derived from the two solutions' distinct odors. However, as the patients did not
know the real substance in the spray, they could only be aware that one spray was different from the other. In
other words, the drug could have been in an odorless spray. The COVID-19 standard treatment
includes intramuscular dexamethasone and remdesivir [22]. A recent study has shown no benefit on the 30-
day mortality from adding early antibiotic treatment for COVID-19 pneumonia [28]. Contrary to
expectations [29,30], the authors [28] did not find significant vaccine effectiveness in lowering disease
severity and mortality among patients with COVID-19 pneumonia.
Our results showed that in the IG, the GSS decreased more than in the control group, and these data reached
a statistically significant level (p = 0.016).
The benefits of nebulized EtOH inhalation were also significantly evident (p = 0.05) in reducing the
inflammatory status, as measured by CRP. This finding confirms the beneficial effects of EtOH on the
immune system [3].
On the other hand, in the IG, blood oxygenation improved faster, and the slope of oxygen was higher than
that in the CG. However, there was no statistically significant difference between the two groups (p = 0.097).
About CSS, the response of the IG was better than that of the CG because no patient was readmitted, against
the need to repeat the standard treatment or to be hospitalized, which occurred in six patients (10.8%) in the
CG. These findings support the EtOH virucidal power.
One of the limitations of this trial was that the patients were far from our strict control and switched to
other therapies. In addition, unpleasant alcohol consumption and the possibility of non-inhaled alcohol
consumption are limiting concerns of the healthcare system. Among others, this study is limited by
confounding factors (due to an imbalance in gender distribution), chance (due to the small sample size), and
insufficient power. A per-protocol analysis breaks the randomization sequence and introduces bias into the
study.
Conclusions
All over, adding inhaled nebulized ethanol to the standard treatment (remdesivir + dexamethasone)
significantly improves recovery from moderate COVID-19. Considering the low cost, availability, and lack of
significant adverse events associated with ethanol, it could be recommended as an adjunctive treatment for
moderate COVID-19. Further research on curative effects in more serious cases and in prevention is
advisable.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Ethics Committee of
School of Medicine, Isfahan University of Medical Sciences issued approval IR.MUI.MED.REC.1400.506.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the
following: Payment/services info: All authors have declared that no financial support was received from
any organization for the submitted work. Financial relationships: All authors have declared that they have
no financial relationships at present or within the previous three years with any organizations that might
have an interest in the submitted work. Other relationships: All authors have declared that there are no
other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
Data are available on reasonable request. Our thanks go to consultation and scientific relations with
scientists from other countries especially Professor Tsumoru Shintake (Okinawa Institute of Science and
Technology Graduate University, Okinawa, Japan), Thomas Manning (Ph.D. Professor of Chemistry in
Valdosta University), Dr. Steven Stogner (Pulmonologist, Forrest General Hospital in Mississippi), Dr. Ali
Shahshahan (Internist, Hattiesburg Clinic, Mississippi), and Annemarie Padmos (Master of Advanced
Nursing Practice, Netherlands). We are also grateful to our co-workers Dr. MR Nazer (Infection Disease
Specialist) and Dr. S. Abbasi (Intensivist) and other nurses in the ethanol therapy project in Isfahan.
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 10 of 11
References
1. Singh D, Joshi K, Samuel A, Patra J, Mahindroo N: Alcohol-based hand sanitisers as first line of defence
against SARS-CoV-2: a review of biology, chemistry and formulations. Epidemiol Infect. 2020, 148:e229.
10.1017/S0950268820002319
2. Lai MM, Cavanagh D: The molecular biology of coronaviruses . Adv Virus Res. 1997, 48:1-100.
10.1016/S0065-3527(08)60286-9
3. Moorer WR: Antiviral activity of alcohol for surface disinfection . Int J Dent Hyg. 2003, 1:138-42.
10.1034/j.1601-5037.2003.00032.x
4. Mörs K, Hörauf JA, Kany S, et al.: Ethanol decreases inflammatory response in human lung epithelial cells
by inhibiting the canonical NF-kB-pathway. Cell Physiol Biochem. 2017, 43:17-30. 10.1159/000480313
5. Chandrasekar A, Heuvel FO, Palmer A, et al.: Acute ethanol administration results in a protective cytokine
and neuroinflammatory profile in traumatic brain injury. Int Immunopharmacol. 2017, 51:66-75.
10.1016/j.intimp.2017.08.002
6. Boé DM, Nelson S, Zhang P, Bagby GJ: Acute ethanol intoxication suppresses lung chemokine production
following infection with Streptococcus pneumoniae. J Infect Dis. 2001, 184:1134-42. 10.1086/323661
7. Berres ME, Garic A, Flentke GR, Smith SM: Transcriptome profiling identifies ribosome biogenesis as a
target of alcohol teratogenicity and vulnerability during early embryogenesis. PLoS One. 2017, 12:e0169351.
10.1371/journal.pone.0169351
8. Sakihara C, Jones KA, Lorenz RR, Perkins WJ, Warner DO: Effects of primary alcohols on airway smooth
muscle. Anesthesiology. 2002, 96:428-37. 10.1097/00000542-200202000-00031
9. Acevedo SF, Peru y Colón de Portugal RL, Gonzalez DA, Rodan AR, Rothenfluh A: S6 kinase reflects and
regulates ethanol-induced sedation. J Neurosci. 2015, 35:15396-402. 10.1523/JNEUROSCI.1880-15.2015
10. Arout CA, Perrino AC Jr, Ralevski E, et al.: Effect of intravenous ethanol on capsaicin-induced hyperalgesia
in human subjects. Alcohol Clin Exp Res. 2016, 40:1425-9. 10.1111/acer.13095
11. Ekins BR, Rollins DE, Duffy DP, Gregory MC: Standardized treatment of severe methanol poisoning with
ethanol and hemodialysis. West J Med. 1985, 142:337-40.
12. Myers R, Taljaard JJ: Blood alcohol and fat embolism syndrome. J Bone Joint Surg Am. 1977, 59:878-80.
13. Haas DM, Morgan AM, Deans SJ, Schubert FP: Ethanol for preventing preterm birth in threatened preterm
labor. Cochrane Database Syst Rev. 2015, 2015:CD011445. 10.1002/14651858.CD011445.pub2
14. Teran E, Racines-Orbe M, Vivero S, Escudero C, Molina G, Calle A: Preeclampsia is associated with a
decrease in plasma coenzyme Q10 levels. Free Radic Biol Med. 2003, 35:1453-6.
10.1016/j.freeradbiomed.2003.08.004
15. Gootnick A, Lipson HI, Turbin J: Inhalation of ethyl alcohol for pulmonary edema . N Engl J Med. 1951,
245:842-3. 10.1056/NEJM195111292452202
16. Castro-Balado A, Mondelo-García C, Barbosa-Pereira L, et al.: Development and characterization of inhaled
ethanol as a novel pharmacological strategy currently evaluated in a phase II clinical trial for early-stage
SARS-CoV-2 infection. Pharmaceutics. 2021, 13:342. 10.3390/pharmaceutics13030342
17. Hu B, Huang S, Yin L: The cytokine storm and COVID-19 . J Med Virol. 2021, 93:250-6. 10.1002/jmv.26232
18. A suggestion on ethanol therapy in COVID-19 . (2020).
https://www.researchgate.net/publication/342077930_A_suggestion_on_Ethanol_therapy_in_COVID-19.
19. Ezz AR, Amoushahi A, Rashad A: Disinfection of SARS-COV-2 (COVID-19) in human respiratory tract by
controlled ethanol vapor inhalation combined with aspirin. J Vaccines Vaccin. 2021, 12:454.
20. Salvatori P: The rationale of ethanol inhalation for disinfection of the respiratory tract in SARS-CoV-2-
positive asymptomatic subjects. Pan Afr Med J. 2021, 40:201. 10.11604/pamj.2021.40.201.31211
21. Hosseinzadeh A, Tavakolian A, Kia V, et al.: Combined application of dimethyl sulfoxide and ethanol nasal
spray during COVID-19 pandemic may protect healthcare workers: a randomized controlled trial. Iran Red
Crescent Med J. 2022, 24:8. 10.32592/ircmj.2022.24.8.1640
22. Rahmanzade R, Rahmanzadeh R, Hashemian SM, Tabarsi P: Iran's approach to COVID-19: evolving
treatment protocols and ongoing clinical trials. Front Public Health. 2020, 8:551889.
10.3389/fpubh.2020.551889
23. Spinner CD, Gottlieb RL, Criner GJ, et al.: Effect of remdesivir vs standard care on clinical status at 11 days
in patients with moderate COVID-19: a randomized clinical trial. JAMA. 2020, 324:1048-57.
10.1001/jama.2020.16349
24. Kratzel A, Todt D, V'kovski P, et al.: Inactivation of severe acute respiratory syndrome coronavirus 2 by
WHO-recommended hand rub formulations and alcohols. Emerg Infect Dis. 2020, 26:1592-5.
10.3201/eid2607.200915
25. Sulaiman I, Chung M, Angel L, et al.: Microbial signatures in the lower airways of mechanically ventilated
COVID-19 patients associated with poor clinical outcome. Nat Microbiol. 2021, 6:1245-58. 10.1038/s41564-
021-00961-5
26. Eterpi M, McDonnell G, Thomas V: Decontamination efficacy against Mycoplasma . Lett Appl Microbiol.
2011, 52:150-5. 10.1111/j.1472-765X.2010.02979.x
27. Ruuskanen MO, Åberg F, Männistö V, et al.: Links between gut microbiome composition and fatty liver
disease in a large population sample. Gut Microbes. 2021, 13:1-22. 10.1080/19490976.2021.1888673
28. Choi YJ, Song JY, Hyun H, et al.: Prognostic factors of 30-day mortality in patients with COVID-19
pneumonia under standard remdesivir and dexamethasone treatment. Medicine (Baltimore). 2022,
101:e30474. 10.1097/MD.0000000000030474
29. Lopez Bernal J, Andrews N, Gower C, et al.: Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca
vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: test
negative case-control study. BMJ. 2021, 373:n1088. 10.1136/bmj.n1088
30. Tenforde MW, Self WH, Adams K, et al.: Association between mRNA vaccination and COVID-19
hospitalization and disease severity. JAMA. 2021, 326:2043-54. 10.1001/jama.2021.19499
2022 Amoushahi et al. Cureus 14(12): e32218. DOI 10.7759/cureus.32218 11 of 11
You might also like
- Mycoses - 2023 - Kato - A Systematic Review and Meta Analysis of Efficacy and Safety of Isavuconazole For The Treatment andDocument10 pagesMycoses - 2023 - Kato - A Systematic Review and Meta Analysis of Efficacy and Safety of Isavuconazole For The Treatment andc gNo ratings yet
- COVID-19: A global problem for modern civilization.: Transactions of the International Academy of Science H&E.From EverandCOVID-19: A global problem for modern civilization.: Transactions of the International Academy of Science H&E.No ratings yet
- Skin and Soft Tissue Injuries & InfectionsDocument221 pagesSkin and Soft Tissue Injuries & InfectionsMario Espinosa100% (1)
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-455378107No ratings yet
- Efficacy of A Polyphenolic, Standardized Green Tea Extract For The Treatment of COVID-19 Syndrome: A Proof-of-Principle StudyDocument11 pagesEfficacy of A Polyphenolic, Standardized Green Tea Extract For The Treatment of COVID-19 Syndrome: A Proof-of-Principle StudyFrankNo ratings yet
- International ImmunopharmacologyDocument6 pagesInternational ImmunopharmacologyMarvin Huanca MartinezNo ratings yet
- Pone 0165942Document15 pagesPone 0165942rastiNo ratings yet
- Ipt 2Document9 pagesIpt 2PPDS ANAK FK USUNo ratings yet
- Etm 20 6 9260 PDFDocument7 pagesEtm 20 6 9260 PDFLina UkagoNo ratings yet
- Referensi 2Document5 pagesReferensi 2ilomurtalaNo ratings yet
- 1 s2.0 S1201971221007980 MainDocument6 pages1 s2.0 S1201971221007980 MainDarshan GandhiNo ratings yet
- Covid 19'Document3 pagesCovid 19'Bella FebriantiNo ratings yet
- 1 s2.0 S0048969720328473 MainDocument10 pages1 s2.0 S0048969720328473 MainExcelsis VallejoNo ratings yet
- Combined Metabolic Activators Accelerates Recovery in Mild-to-Moderate COVID-19Document16 pagesCombined Metabolic Activators Accelerates Recovery in Mild-to-Moderate COVID-19alicia dawnNo ratings yet
- Impétigo Revisión SistemáticaDocument21 pagesImpétigo Revisión SistemáticaDanielNo ratings yet
- Ijo 33 229Document7 pagesIjo 33 229Agung wibisonoNo ratings yet
- La Ivermectina No Previene La Hospitalización Por Coronavirus, Según EstudioDocument11 pagesLa Ivermectina No Previene La Hospitalización Por Coronavirus, Según EstudioEl Informador Santa MartaNo ratings yet
- Allergy - 2020 - Pfaar - Placebo Effects in Allergen Immunotherapy An EAACI Task Force Position PaperDocument19 pagesAllergy - 2020 - Pfaar - Placebo Effects in Allergen Immunotherapy An EAACI Task Force Position PaperKohinoorKohinoorNo ratings yet
- Corresponding Author Dr. Nicola Luigi BragazziDocument47 pagesCorresponding Author Dr. Nicola Luigi BragazziSusana PaçoNo ratings yet
- Rheumatol Q-1-1-EnDocument5 pagesRheumatol Q-1-1-EnSalmiyah HasibuanNo ratings yet
- Co Vid 19Document5 pagesCo Vid 19MonicaNo ratings yet
- Effect of Tocilizumab Vs Standard Care On Clinical Worsening in Patients Hospitalized With COVID-19 Pneumonia A Randomized Clinical TrialDocument8 pagesEffect of Tocilizumab Vs Standard Care On Clinical Worsening in Patients Hospitalized With COVID-19 Pneumonia A Randomized Clinical TrialNimas NimasNo ratings yet
- COVID 19 Influences Lung Microbiota Dynamics and Favors The 2021 Journal ofDocument3 pagesCOVID 19 Influences Lung Microbiota Dynamics and Favors The 2021 Journal ofJosé Carlos Bernaola ZevallosNo ratings yet
- Immunotherapy Toxicities ESMODocument22 pagesImmunotherapy Toxicities ESMOicemoonNo ratings yet
- A Five-Day Course of Ivermectin May Reduce The DurationDocument3 pagesA Five-Day Course of Ivermectin May Reduce The DurationPaulinho CtsNo ratings yet
- TocilizumabDocument14 pagesTocilizumabTri CahyaniNo ratings yet
- Treatment With Tocilizumab or Corticosteroids For COVID 2021 Clinical MicroDocument9 pagesTreatment With Tocilizumab or Corticosteroids For COVID 2021 Clinical MicroSusanyi ErvinNo ratings yet
- (2020) Oxygen-Ozone (O2-O3) Immunoceutical Therapy For Patients With COVID-19 Preliminary Evidence ReportedDocument5 pages(2020) Oxygen-Ozone (O2-O3) Immunoceutical Therapy For Patients With COVID-19 Preliminary Evidence ReportedVu TranNo ratings yet
- Addiction - 2021 - Knuijver - Safety of Ibogaine Administration in Detoxification of Opioid Dependent Individuals A-1Document11 pagesAddiction - 2021 - Knuijver - Safety of Ibogaine Administration in Detoxification of Opioid Dependent Individuals A-1Anka StNo ratings yet
- ArticleDocument9 pagesArticleVictor ValarezoNo ratings yet
- 2021 Article 2702Document7 pages2021 Article 2702Gangga ChandraNo ratings yet
- Ijccm 24 1015 PDFDocument3 pagesIjccm 24 1015 PDFMahtosurup GodavarthyNo ratings yet
- Immunomodulation and COVID-19: Is There A Winning Combination?Document3 pagesImmunomodulation and COVID-19: Is There A Winning Combination?Mahtosurup GodavarthyNo ratings yet
- Ijccm 24 1015 PDFDocument3 pagesIjccm 24 1015 PDFMahtosurup GodavarthyNo ratings yet
- Cigarette Smoking and Asthma: Clinical Management ReviewDocument15 pagesCigarette Smoking and Asthma: Clinical Management ReviewMuhammad FikriNo ratings yet
- Budesonide Pada Serangan Asma - AJEM-3-e4Document5 pagesBudesonide Pada Serangan Asma - AJEM-3-e4Tulus Java Rimbunan S.No ratings yet
- Antimicrobial, Antioxidant, and Cytotoxic Activities of Juglans Regia L. Pellicle ExtractDocument20 pagesAntimicrobial, Antioxidant, and Cytotoxic Activities of Juglans Regia L. Pellicle ExtractBETÜL KILINÇLINo ratings yet
- IVIg For The Treatment of COVID 19Document3 pagesIVIg For The Treatment of COVID 19lalaine nadulpitNo ratings yet
- Lary 9999 0Document8 pagesLary 9999 0Niken KuncorowatiNo ratings yet
- Inhaled Corticosteroids Safety and Adverse Effects-DikonversiDocument8 pagesInhaled Corticosteroids Safety and Adverse Effects-DikonversiRachmi MerrinaNo ratings yet
- Clinical StudyDocument12 pagesClinical StudyansunNo ratings yet
- Allergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofDocument17 pagesAllergy - 2022 - Farraia - Allergen Immunotherapy For Asthma Prevention A Systematic Review and Meta Analysis ofpedrotiagosilvaNo ratings yet
- Antiviral Treatment of COVID-19: A Clinical Pharmacology Narrative ReviewDocument14 pagesAntiviral Treatment of COVID-19: A Clinical Pharmacology Narrative ReviewJack JacksonNo ratings yet
- Cytokine and Interleukin Profile in Patients With Headache and COVID-19: A Pilot, CASE-control, Study On 104 PatientsDocument11 pagesCytokine and Interleukin Profile in Patients With Headache and COVID-19: A Pilot, CASE-control, Study On 104 Patientszee zeeNo ratings yet
- Lung Abcess Childreen AnnThoracMed113191-6070308 - 014110Document6 pagesLung Abcess Childreen AnnThoracMed113191-6070308 - 014110Muchammad FahruludinNo ratings yet
- Treatment Efficacy of Lianhua Qingwen Capsules For Early Stage Covid 19Document8 pagesTreatment Efficacy of Lianhua Qingwen Capsules For Early Stage Covid 19Isaac Joshua AganonNo ratings yet
- Name: Athena Dianne B. Aguillon Block: 2-NgDocument3 pagesName: Athena Dianne B. Aguillon Block: 2-NgATHENA DIANNE BARON AGUILLONNo ratings yet
- (2020) Oxygen-Ozone Therapy As Adjuvant in The Current Emergency in Sars-Cov-2 Infection - A Clinical StudyDocument10 pages(2020) Oxygen-Ozone Therapy As Adjuvant in The Current Emergency in Sars-Cov-2 Infection - A Clinical StudyVu TranNo ratings yet
- Phytotherapy Research - 2020 - Pesce - Phytotherapics in COVID19 Why PalmitoylethanolamideDocument9 pagesPhytotherapy Research - 2020 - Pesce - Phytotherapics in COVID19 Why PalmitoylethanolamideFabiano SousaNo ratings yet
- RecentprogressinthetreatmentofLN PDFDocument12 pagesRecentprogressinthetreatmentofLN PDFHosne araNo ratings yet
- Curcumin As A Potential Target For COVIDDocument10 pagesCurcumin As A Potential Target For COVIDPathirage Kamal PereraNo ratings yet
- 20220115-8166-4705cj Ivermectin Prophylaxis Used For COVID-19Document25 pages20220115-8166-4705cj Ivermectin Prophylaxis Used For COVID-19Hansley Templeton CookNo ratings yet
- Emerging Treatment Strategies For Impetigo in Endemic and Nonendemic Settings: A Systematic ReviewDocument21 pagesEmerging Treatment Strategies For Impetigo in Endemic and Nonendemic Settings: A Systematic Reviewnurul hidayatiNo ratings yet
- Evolving Consensus For Immunomodulatory Therapy in Non-Infectious Uveitis During The COVID-19 PandemicDocument9 pagesEvolving Consensus For Immunomodulatory Therapy in Non-Infectious Uveitis During The COVID-19 PandemicSyafrial BarawasNo ratings yet
- 1 s2.0 S1198743X14607667 MainDocument15 pages1 s2.0 S1198743X14607667 MainiisisiisNo ratings yet
- 2022 The Effects of Hyperbaric Oxygen Therapy (HBOT) On Coronavirus Disease-2019 (COVID-19) - A Systematic ReviewDocument12 pages2022 The Effects of Hyperbaric Oxygen Therapy (HBOT) On Coronavirus Disease-2019 (COVID-19) - A Systematic ReviewabnfojoNo ratings yet
- Antibiotics 11 01291Document8 pagesAntibiotics 11 01291semaraNo ratings yet
- Articulo 1Document7 pagesArticulo 1Adrian EspinosaNo ratings yet
- TCZ Recovery Journal 2021Document9 pagesTCZ Recovery Journal 2021dr. FAPNo ratings yet
- Atorvastatin Improves Sputum Conversion and Chest X-Ray Severity ScoreDocument6 pagesAtorvastatin Improves Sputum Conversion and Chest X-Ray Severity Scorecharmainemargaret.parreno.medNo ratings yet
- Ivermectin As An Adjunct Treatment For Hospitalized Adult COVID-19 PatientsDocument8 pagesIvermectin As An Adjunct Treatment For Hospitalized Adult COVID-19 PatientschristineNo ratings yet
- Potential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsFrom EverandPotential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsNo ratings yet
- JMCB +DJ-1Document10 pagesJMCB +DJ-1Deepak JainNo ratings yet
- ZnT8 Nature GeneticsDocument28 pagesZnT8 Nature GeneticsDeepak JainNo ratings yet
- BMJ 2021 068060.fullDocument8 pagesBMJ 2021 068060.fullDeepak JainNo ratings yet
- Efficacy of Breathox® Device Inhalation On Acute Symptoms Associated With COVID-19 (BREATH Study) European Respiratory SocietyDocument6 pagesEfficacy of Breathox® Device Inhalation On Acute Symptoms Associated With COVID-19 (BREATH Study) European Respiratory SocietyDeepak JainNo ratings yet
- Fitness JournalDocument68 pagesFitness JournalKrisztinaVágvölgyiNo ratings yet
- Mustafa CV PDFDocument22 pagesMustafa CV PDFMUSTAFA TEMEMINo ratings yet
- Understanding and Preparing For A CAtHeteRIZAtIon PRoCeDUReDocument7 pagesUnderstanding and Preparing For A CAtHeteRIZAtIon PRoCeDUReBMTNo ratings yet
- Craniofacial SyndromesDocument101 pagesCraniofacial SyndromesSaranya MohanNo ratings yet
- Unit 1: Definitions of Social Work: I. Reading ComprehensionDocument59 pagesUnit 1: Definitions of Social Work: I. Reading ComprehensionMậpp HuyyNo ratings yet
- Jdo Vol 59 New PDFDocument100 pagesJdo Vol 59 New PDFLex MNo ratings yet
- Postharvest Technology-Importance: Eufemio G. Barcelon, PHDDocument56 pagesPostharvest Technology-Importance: Eufemio G. Barcelon, PHDJohanna Amor L. AdaoNo ratings yet
- DR Norris - Good Trasfusion Practice PDFDocument27 pagesDR Norris - Good Trasfusion Practice PDFvasu_5iveNo ratings yet
- Aldomet: (Methyldopa)Document6 pagesAldomet: (Methyldopa)Riska AuliahNo ratings yet
- Health Beliefs and PracticesDocument7 pagesHealth Beliefs and Practicesapi-283426681No ratings yet
- Laporan Iud 2019Document91 pagesLaporan Iud 2019Yuli AntiNo ratings yet
- Effect of A Program of Physical Activity Motivated by Lipid Parameters of Patients With Obesity and or Overweight PDFDocument6 pagesEffect of A Program of Physical Activity Motivated by Lipid Parameters of Patients With Obesity and or Overweight PDFMarlio Andres Vargas PolaniaNo ratings yet
- Infant Tub RationaleDocument4 pagesInfant Tub RationaleAllen Kenneth PacisNo ratings yet
- House M D Rudeness and ImpolitenessDocument17 pagesHouse M D Rudeness and ImpolitenessMasroof GanieNo ratings yet
- Syba Economics Syll 20-21Document13 pagesSyba Economics Syll 20-21Saniya ShaikhNo ratings yet
- Child Welfare Trauma Training Participant GuideDocument104 pagesChild Welfare Trauma Training Participant GuideAllison PalmisanoNo ratings yet
- Gap AnalysisDocument9 pagesGap Analysisapi-706947027No ratings yet
- Epstein Barr Virus (EBV) PDFDocument33 pagesEpstein Barr Virus (EBV) PDFahmad mohammadNo ratings yet
- Advancements in The Bbutilization of Azolla Anabaena System in RelationDocument17 pagesAdvancements in The Bbutilization of Azolla Anabaena System in Relationryana_soesantieNo ratings yet
- Nso AblaparotomyDocument3 pagesNso AblaparotomyAleeya SarajanNo ratings yet
- Week 4.1 The Law of ResonanceDocument12 pagesWeek 4.1 The Law of ResonanceWim Massop100% (1)
- Assisting Delivery Name: - Grade: - Year and Section: - DateDocument5 pagesAssisting Delivery Name: - Grade: - Year and Section: - DateCrisia Jane LotaNo ratings yet
- An Atlas of Radiology of The Traumatized Dog and CatDocument566 pagesAn Atlas of Radiology of The Traumatized Dog and CatDenise Gomes de MeloNo ratings yet
- BURNS SoftDocument3 pagesBURNS SoftErlo John Asentista0% (1)
- The Myths and Truths About Transcendental MeditationDocument11 pagesThe Myths and Truths About Transcendental MeditationMeditation Fix100% (2)
- Meditation ScriptDocument9 pagesMeditation Scriptapi-361293242100% (1)
- Module 5 Nature of The Clinical LaboratoryDocument26 pagesModule 5 Nature of The Clinical LaboratoryAlexander LimNo ratings yet
- SHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)Document18 pagesSHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)wstNo ratings yet