Professional Documents
Culture Documents
Cardiovascular Assessment Guide
Uploaded by
Mary Joy Anne Lucas0 ratings0% found this document useful (0 votes)
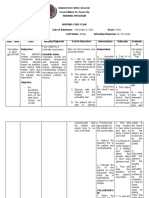
92 views9 pages1. The document outlines the steps of a cardiovascular assessment, including inspection, palpation, and auscultation of the neck vessels, heart, and peripheral vascular system.
2. Key steps include assessment of the jugular veins, carotid arteries, heart sounds and location of the apical impulse, and pulses in the upper and lower extremities.
3. Normal findings are provided and include no distention of jugular veins, no bruits heard on auscultation of carotid arteries, regular heart rate and rhythm with normal heart sounds, and symmetrically warm extremities with palpable pulses.
Original Description:
CARDIOVASCULAR Return Demonstration Script
Original Title
Cardiovascular RD Script
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. The document outlines the steps of a cardiovascular assessment, including inspection, palpation, and auscultation of the neck vessels, heart, and peripheral vascular system.
2. Key steps include assessment of the jugular veins, carotid arteries, heart sounds and location of the apical impulse, and pulses in the upper and lower extremities.
3. Normal findings are provided and include no distention of jugular veins, no bruits heard on auscultation of carotid arteries, regular heart rate and rhythm with normal heart sounds, and symmetrically warm extremities with palpable pulses.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
92 views9 pagesCardiovascular Assessment Guide
Uploaded by
Mary Joy Anne Lucas1. The document outlines the steps of a cardiovascular assessment, including inspection, palpation, and auscultation of the neck vessels, heart, and peripheral vascular system.
2. Key steps include assessment of the jugular veins, carotid arteries, heart sounds and location of the apical impulse, and pulses in the upper and lower extremities.
3. Normal findings are provided and include no distention of jugular veins, no bruits heard on auscultation of carotid arteries, regular heart rate and rhythm with normal heart sounds, and symmetrically warm extremities with palpable pulses.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 9
PRE INTRODUCTORY PHASE
1. 1st is to review the client’s medical record as well as the
doctor’s order for the assessment needed to perform.
2. Determine the scope of assessment and prepare the
necessary equipment. The following are the equipment
needed; Penlight, rectangular card, ruler, stethoscope)
THIS IS TO CONSERVE TIME AND ENERGY
3. Perform hand hygiene and wear gloves and observe
other appropriate infection prevention procedures. THIS
IS TO PREVENT THE SPREAD OF MICROORGANISMS.
INTRODUCTORY PHASE
4. Greet the client politely as well as his/her companion if
around. Introduce self and verify the client’s identity
using the agency protocol. Ask how the client would like
to be called during the assessment. Establish rapport.
Good day ma’am! I am your student nurse for today, my
name is Mary Joy Anne Guarin. Can you state your name
and birthday? How would you like to be called during the
assessment ma’am? Okay, ma’am Shai. How are you
feeling today?
5. Explain the procedure to the client and how he/she can
participate during the assessment. Provide the client’s
opportunity to ask for clarification or raise any concerns.
Ma’am Shai, for today, I am going to assess your
cardiovascular system which includes your neck vessels,
your heart, and your peripheral vascular system. I would
like to ask for your full participation that I might ask you
to stand, sit, or bend later. Do you have any questions or
clarifications so far ma’am?
6. Ensure the client’s comfort, privacy, and confidentiality.
Drape the client’s body as needed throughout the
assessment. Ma’am Shai, are you okay with your sit?
How about the air conditioning? So, I’m going to close
the door and the curtain to make sure of your privacy
ma’am Shai. So, let me inform you that your information
for today’s assessment is confidential which is our
priority.
7. Inquire if the client has any existing history of
cardiovascular problems, as well as lifestyle h
8. abits that are risk factors for cardiac problems. Do you
have any specific complaints such as neck pain or chest
pain? Or in any of your extremities? Have you experience
shortness of breath, dizziness, or headache? Do you have
a history of hypertension or coronary heart disease? Do
you smoke? What are your daily activities? Do you
exercise?
WORKING PHASE
ASSESSMENT OF NECK VESSELS
Assessment of Jugular Veins
9. Stood on the right side of the patient and position
him/her supine with the head of the bed elevated
between 30 and 45degrees, make sure that the head and
torso are on the same plane.
10. Instruct the client to turn the head slightly to the left
and shine tangential light source onto the neck,
suprasternal notch, and area around the clavicles to
observe for pulsations and shadows
11. If jugular distention is noted, assess the jugular
venous pressure by locating the highest visible point of
distention of the internal jugular vein. Emphasize the
distention with tangential lighting. NOTE! The jugular
vein should not be distended, bulging, or protruding at 45
degrees or greater. If so, it may indicate right-sided heart
failure.
12. As deemed necessary, raised or lowered the head of
the bed (30, 45, 60, and 90 degrees) until the highest
visible point of distention of the jugular vein is observed
13. Measure the vertical distance in centimeters above
the sternal angle by extending a long rectangular object
or card horizontally from this point and a centimeter
ruler vertically from the sternal angle making an exact
right angle.
14. Repeat on the other side
NORMAL- VEINS NOT VISIBLE WHICH INDICATES THAT
THE RIGHT SIDE OF HEART IS FUNCTIONING NORMALLY
Assessment of Carotid Arteries
15. With head of the bed still slightly elevated at
30degrees, positioned the client’s head slightly towards
the side being examined. Palpate the carotid artery
avoiding too much pressure or massaging the area.
16. Repeat the steps of the other side
NORMAL- SYMMETRIC PULSE VOLUMES
- FULL PULSATION
- ELASTIC ARTERIAL WALL
17. Turn the client’s head slightly away from the side
being examined. Placed the bell of the stethoscope over
the carotid artery, and ask the client to hold his/her
breath for a moment and auscultate the carotid artery
listening for bruit.
18. Repeat steps on the other side
NORMAL- NO SOUND HEARD ON AUSCULTATION
(NEITHER BRUIT NOR THRILL)
ASSESSMENT OF THE HEART (PERICARDIUM)
Inspection and Palpation
19. Begin with a general inspection of the chest wall.
Looking for any pulsations, symmetry of movement,
retraction or heaves. For women, kept the right chest
draped, and gently lift the breast with the left hand or
ask your client to do this for assistance. Stood at the right
side of the client with the head of the bed elevated at 30
degrees and look for any abnormal pulsations.
NORMAL- CHEST MOVEMENT IS SYMMETRICAL, NO
RETRACTIONS
20. Simultaneously inspect the pericardium for
pulsations while palpating all four anatomic sites: aortic,
pulmonic, tricuspid, and apical.
21. Palpate for heaves and lifts using the palm and/or
hold finger pads flat or obliquely against the chest
22. For thrills, pressed the ball of the hand firmly on the
chest to check for a buzzing or vibratory sensation caused
by underlying turbulent flow.
23. Palpate impulses using finger pads flatly or obliquely
on the body surface from the four anatomic sites: aortic,
pulmonic, tricuspid, and apicalError! Hyperlink reference
not valid.
NORMAL- NO PULSATIONS, NO LIFT OR HEAVE
24. Palpate the apical impulse using the palmar surfaces
of two to three middle fingers. For a finer assessment,
palpate with one finger alone to confirm characteristics
of the apical impulse noting for location, diameter, and
amplitude.
25. If unable to palpate the apical impulse with the
patient in a supine position, reposition the patient to roll
partly in the left lateral side. Palpate again, using the
palmar surfaces of several fingers. If still not able to
palpate, ask the patient to exhale fully and stop
breathing for a few seconds and palpate again while
he/she maintains to be partly facing left side.
NORMAL- PULSATIONS VISIBLE IN 50% OF ADULTS AND
PALPABLE IN MOST
- DIAMETER OF 1-2CM
- NO LIFT OR HEAVE
26. Inspect and palpate the epigastric area at the base
of the sternum for abdominal aortic pulsations.
Auscultation
27. Assess heart rate and rhythm by placing the
diaphragm of the stethoscope at the apex and listening
closely to the rate and rhythm of the apical impulse.
Count the heartbeat for a full minute. (If an irregular
rhythm was detected, assess for a pulse rate deficit)
28. Using the diaphragm of the stethoscope first, then
the bell, auscultate the heart in all four anatomic sites
aortic, pulmonic, tricuspid, and apical (mitral) for heart
sounds, extra heart sounds, and murmurs. Then, ask the
client to breathe regularly while auscultating
29. Repeat the steps while the patient is in left lateral
position them at sitting position, leaning forward and
briefly stop after exhalation
NORMAL- Heart rate is _ per minute and have a regular
rhythm
ASSESSMENT OF THE PERIPHERAL VASCULAR SYSTEM
Examining Upper Extremities
30. Assess each arm for size, symmetry, skin color and
temperature from finger tips to shoulder. Note for any
presence of edema, lesion, changes in skin texture and
hair distribution
31. Inspect the peripheral veins in the arm for the arms
for the presence and/or appearance of superficial veins
when limbs are dependent and when limps are elevated.
32. Palpate for radial pulse, ulnar pulse, and brachial
pulse individually and bilaterally
33. Assess for capillary refill
34. Perform Allen Test
35. Repeat the steps on the other side
NORMAL- ARMS ARE BILATERALLY SYMMETRIC WITH
MINIMAL VARIATION IN SIZE AND SHAPE. NO EDEMA
AND LESIONS. SKIN TEMPERATURE IS WARM AND
CAPILLARY REFILL IS GOOD. RADIAL PULSE, ULNAR AND
BRACHIAL PULSE ARE BILATERALLY STRONG AND HAVE A
NORMAL RHYTHM. UPON ALLEN TEST, WHEN YOU WERE
OPENING AND CLOSING YOUR HANDS, THE RESULT IS
NORMAL.
Examining Lower Extremities
36. At the supine position, assess each leg for size,
symmetry, skin color and temperature from groin to toes.
So, I’m looking for any ulcerations, edema or swelling,
venous pattern or varicosities. Note for any presence of
lesion, changes in skin texture and hair distribution
37. Inspect the peripheral veins in the legs for the
presence and/or appearance of superficial veins when
limbs are dependent and when limbs are elevated
38. Palpate for a femoral pulse, popliteal pulse, dorsalis
pedis, and posterior tibialis individually and bilaterally
39. Assess the peripheral leg veins for veins signs of
ulcerations, varicosities, and thrombophlebitis:
Inspect the calves for ulcerations, varicosities, redness
and swelling over vein sites
40. Palpate the calves for firmness or tension of the
muscles, the presence of edema over the dorsum of the
foot, and areas of localized warmth. Push the calves from
side to side for tenderness
41. Firmly dorsiflexed the client’s foot while supporting
the entire leg in extension (Homans’ test) or had the
client stand or walk
42. Assess for capillary refill for both legs and repeat
steps with the other leg
NORMAL- UPON EXAMINING YOUR LEGS: HAIR IS
EVENLY DISTRIBUTED, SKIN TEMPERATURE IS WARM, NO
EDEMA, NO LESIONS AND NO SWELLING. FEMORAL
PULSE, POPLITEAL PULSE, DORSALIS PEDIS, AND
POSTERIOR TIBIALIS ARE NORMAL: EQUALLY STRONG
AND HAVE A NORMAL RHYTHM
SUMMARY AND CLOSING
43. Inform the client that the assessment was done. If
deemed, assist client to change clothes. Reposition the
client comfortably sitting on a chair.
44. Summarize the information obtained during the
working phase and discuss findings to the client. Discuss
the possible plans to resolve health concern. Assess for
client’s understanding of the plan and the need for
further teaching. Provide the client the opportunity to
clarify, raise any concern.
45. Thank the client for her cooperation and ended the
assessment politely. Done aftercare. Perform hand
hygiene.
46. Document findings in client record using printed or
electronic forms or checklists supplemented by narrative
notes when appropriate.
You might also like
- Illuminism - The Occult Force Behind Globalization - by Wes PenreDocument98 pagesIlluminism - The Occult Force Behind Globalization - by Wes Penrebreiard100% (1)
- Health and Safety Plan TranslationDocument17 pagesHealth and Safety Plan TranslationEvaristo MudenderNo ratings yet
- Assessing The Thorax and LungsDocument4 pagesAssessing The Thorax and LungsLorenz Jude Cańete100% (2)
- Jenkins Lab Guide: 172-172, 5th Floor Old Mahabalipuram Road (Above Axis Bank-PTC Bus Stop) Thuraipakkam Chennai 600097Document45 pagesJenkins Lab Guide: 172-172, 5th Floor Old Mahabalipuram Road (Above Axis Bank-PTC Bus Stop) Thuraipakkam Chennai 600097thecoinmaniac hodlNo ratings yet
- Checklist of Thorax and Lungs Students'Document5 pagesChecklist of Thorax and Lungs Students'Rosette Malenab de AsisNo ratings yet
- Assurance Question Bank 2013 PDFDocument168 pagesAssurance Question Bank 2013 PDFIan RelacionNo ratings yet
- Unit 06 Assessment of Thorax and LungDocument55 pagesUnit 06 Assessment of Thorax and Lunghuma100% (1)
- #3 - 2nd Day NCM 01 - Lab - Reviewer PrelimDocument20 pages#3 - 2nd Day NCM 01 - Lab - Reviewer PrelimNurse TinNo ratings yet
- Bekkersdal Business Hive Close Out ReportDocument19 pagesBekkersdal Business Hive Close Out ReportMichael Benhura100% (2)
- Understanding Cirrhosis of the LiverDocument16 pagesUnderstanding Cirrhosis of the LiverAmanda ScarletNo ratings yet
- Overcoming ChallengesDocument28 pagesOvercoming ChallengesDeutsche Mark CuynoNo ratings yet
- Assessing Apical Pulse 29 3Document4 pagesAssessing Apical Pulse 29 3Maria Angelika Bughao100% (1)
- Self - Transcendence Theory in NursingDocument20 pagesSelf - Transcendence Theory in NursingRaveesh Kaimal100% (1)
- Obtaing Subjective & Objective Data On Assessing Breast and Lymphatic SystemDocument8 pagesObtaing Subjective & Objective Data On Assessing Breast and Lymphatic SystemKathlyne Jhayne100% (1)
- Madeleine LeiningerDocument38 pagesMadeleine LeiningerCharina AubreyNo ratings yet
- Communication in PsychiatricDocument27 pagesCommunication in PsychiatricRobert Edwards100% (1)
- Critical Thinking Skills Vital for NursesDocument4 pagesCritical Thinking Skills Vital for Nursesgabrielle magdaraogNo ratings yet
- DiscussDocument2 pagesDiscussruthlessly_inloveNo ratings yet
- Evaluating the Teaching ProgramDocument5 pagesEvaluating the Teaching ProgramPerly joy SeguraNo ratings yet
- First Aid EssayDocument1 pageFirst Aid Essayadrian lozanoNo ratings yet
- TFN-MIDTERMS-AND-SEMIS Bat Exam ReviewerDocument59 pagesTFN-MIDTERMS-AND-SEMIS Bat Exam ReviewerPrince D. JacobNo ratings yet
- RLE-level-2-packet-week-12-requirement (SANAANI, NUR-FATIMA, M.)Document26 pagesRLE-level-2-packet-week-12-requirement (SANAANI, NUR-FATIMA, M.)Nur SanaaniNo ratings yet
- WEEK 1 - OVERVIEW OF HEALTH ASSESSMENTDocument4 pagesWEEK 1 - OVERVIEW OF HEALTH ASSESSMENTDharyn KhaiNo ratings yet
- CU 11. Ethico Moral and Legal Foundations of Client EducationDocument5 pagesCU 11. Ethico Moral and Legal Foundations of Client Educationcloe blancaNo ratings yet
- Assessing General Status Vital Signs 1Document20 pagesAssessing General Status Vital Signs 1Geylla FaeldoniaNo ratings yet
- Health Education Prelims TopicsDocument36 pagesHealth Education Prelims TopicsAmiel Francisco ReyesNo ratings yet
- The Nurse As An EducatorDocument4 pagesThe Nurse As An EducatorAlbean DelojeroNo ratings yet
- NCM 104 - RleDocument25 pagesNCM 104 - RleAbigael Patricia GutierrezNo ratings yet
- Nursing as an Academic DisciplineDocument20 pagesNursing as an Academic DisciplineJules Antonette RNNo ratings yet
- TFN Final ExamDocument2 pagesTFN Final ExamJamoi Ray VedastoNo ratings yet
- Assisting in Catherization IDocument6 pagesAssisting in Catherization IGrezilmay MeninguitoNo ratings yet
- Martha Rogers: Presented By: Lyndsi Byers, Geena Griffin, Chelsea Hoy and Mallory ShepardDocument18 pagesMartha Rogers: Presented By: Lyndsi Byers, Geena Griffin, Chelsea Hoy and Mallory ShepardChelsea Hoy100% (2)
- Florence Nightingale's Environmental Theory: Josephine Ann J. Necor, RNDocument38 pagesFlorence Nightingale's Environmental Theory: Josephine Ann J. Necor, RNBheru LalNo ratings yet
- Models of Health and WellnessDocument5 pagesModels of Health and WellnessGlory GloryNo ratings yet
- NCMA112: History of Health EducationDocument11 pagesNCMA112: History of Health EducationAngelica LegaspiNo ratings yet
- Case Scenario - NebulizationDocument2 pagesCase Scenario - NebulizationHilario. Hayascent.Reign.M.No ratings yet
- Hospital Organizational ChartDocument1 pageHospital Organizational ChartAnonymous tDXlfJxNo ratings yet
- Research Paper DiabetesDocument8 pagesResearch Paper Diabetesapi-359023534No ratings yet
- Filipino Culture, Values and Practices in Relation To Health Care of Individual and FamilyDocument15 pagesFilipino Culture, Values and Practices in Relation To Health Care of Individual and Familyfatima dasalNo ratings yet
- 2 A Healthy CommunityDocument12 pages2 A Healthy CommunityJmarie Brillantes PopiocoNo ratings yet
- Module 6 - Environmental Sanitation Revised Dec 18Document76 pagesModule 6 - Environmental Sanitation Revised Dec 18mgllacuna0% (2)
- Professional Developmental PlanDocument2 pagesProfessional Developmental Planapi-509382617No ratings yet
- Head and Neck Assessment FindingsDocument4 pagesHead and Neck Assessment FindingsCiara Manguiat100% (1)
- Unit 1: Macromolecules: Food Tests: Outu - Be/Slp8Dcnwnj GDocument4 pagesUnit 1: Macromolecules: Food Tests: Outu - Be/Slp8Dcnwnj GManan PatelNo ratings yet
- Critical Care in NursingDocument16 pagesCritical Care in NursingFUZNA DAHLIA MUDZAKIROH 1No ratings yet
- 1 - Civic Responsibilities & Rights As CitizensDocument28 pages1 - Civic Responsibilities & Rights As CitizensAbdul Rahman SaniNo ratings yet
- Health Assessment SAS Session 13 PDFDocument8 pagesHealth Assessment SAS Session 13 PDFMaria Jub MangrubanNo ratings yet
- Patient Positioning: Complete Guide For Nurses: Marjo S. Malabanan, R.N.,M.NDocument43 pagesPatient Positioning: Complete Guide For Nurses: Marjo S. Malabanan, R.N.,M.NMercy Anne EcatNo ratings yet
- Framework For Maternal and Child Health NursingDocument18 pagesFramework For Maternal and Child Health NursingKristil ChavezNo ratings yet
- Nursing As A ProfessionDocument6 pagesNursing As A Professionreyl MercadejasNo ratings yet
- 2 - Concept of Health Education - 04!08!2023Document8 pages2 - Concept of Health Education - 04!08!2023Israt SadiaNo ratings yet
- Cu 2 Issues & Trends in HeDocument4 pagesCu 2 Issues & Trends in HeMichelle Gliselle Guinto MallareNo ratings yet
- NCM 113 Midterm Lec Mod 5Document17 pagesNCM 113 Midterm Lec Mod 5desteen klaire montefalcoNo ratings yet
- Cellular Aberrations NotesDocument22 pagesCellular Aberrations NotesH50% (2)
- My SHN CompilationDocument57 pagesMy SHN Compilationapi-3718174100% (2)
- Fowler's Stages of Faith Development SummaryDocument18 pagesFowler's Stages of Faith Development SummaryErin RedNo ratings yet
- 10 Key Characteristics of a Great NurseDocument6 pages10 Key Characteristics of a Great NurseAzhin O MuhammadNo ratings yet
- Pcip-Ncmh 2016Document38 pagesPcip-Ncmh 2016Carissa De Luzuriaga-BalariaNo ratings yet
- Comfort Theory Kolcaba EnglishDocument4 pagesComfort Theory Kolcaba EnglishRahayu SavitriNo ratings yet
- Safe Patient Transfers: Bed to StretcherDocument3 pagesSafe Patient Transfers: Bed to StretcherRoxas CedrickNo ratings yet
- Community Health NursingDocument105 pagesCommunity Health NursingKBDNo ratings yet
- Prelim Exam NCM 103Document10 pagesPrelim Exam NCM 103Zhyraine Iraj D. CaluzaNo ratings yet
- Saint Paul University Philippines Nursing Student Biographical DataDocument7 pagesSaint Paul University Philippines Nursing Student Biographical DataStephNo ratings yet
- Carmencita Abaquin's PREPARE ME Theory for Cancer PatientsDocument2 pagesCarmencita Abaquin's PREPARE ME Theory for Cancer PatientsBSN-2F Neutral Axis SiazonNo ratings yet
- Healthcare Reflections, Insights, and Lessons: Proactive/ReactiveFrom EverandHealthcare Reflections, Insights, and Lessons: Proactive/ReactiveNo ratings yet
- Cardiovascular Assessment - RDDocument2 pagesCardiovascular Assessment - RDANGELICA CLAIRE BARECUATRONo ratings yet
- Davao Doctors College Nursing AssessmentDocument9 pagesDavao Doctors College Nursing AssessmentMary Joy Anne LucasNo ratings yet
- GUARIN NCP Module 8Document4 pagesGUARIN NCP Module 8Mary Joy Anne LucasNo ratings yet
- Final Najud Simulation ScriptDocument13 pagesFinal Najud Simulation ScriptMary Joy Anne LucasNo ratings yet
- Guarin NCPDocument4 pagesGuarin NCPMary Joy Anne LucasNo ratings yet
- Dabe Drug StudyDocument3 pagesDabe Drug StudyMary Joy Anne LucasNo ratings yet
- Civil Engineering Softwares and Their ImplementationsDocument13 pagesCivil Engineering Softwares and Their ImplementationsADITYANo ratings yet
- Ruibal & Shoemaker 1984 - Osteoders in AnuransDocument17 pagesRuibal & Shoemaker 1984 - Osteoders in AnuransRuivo LucasNo ratings yet
- FNCP Family Nursing Care Plan 1 Poor Environmental Sanitation Health ThreatDocument2 pagesFNCP Family Nursing Care Plan 1 Poor Environmental Sanitation Health Threatbraceceeem03No ratings yet
- ADP Pink Diamond Investment Guide 2023Document47 pagesADP Pink Diamond Investment Guide 2023sarahNo ratings yet
- Jerome KaganDocument5 pagesJerome KaganMandeep morNo ratings yet
- B2 - PlatoDocument1 pageB2 - PlatoVeda Leigh SyNo ratings yet
- Between Empire and GlobalizationDocument5 pagesBetween Empire and Globalizationazert yuiopNo ratings yet
- Guided Reading Activity: The Reach of ImperialismDocument2 pagesGuided Reading Activity: The Reach of ImperialismevertNo ratings yet
- Robbins OB15GE Inppt16Document31 pagesRobbins OB15GE Inppt16Nida IsrarNo ratings yet
- Detroit Cathedral Program Final 4-17-12Document2 pagesDetroit Cathedral Program Final 4-17-12Darryl BradleyNo ratings yet
- Papadaki 2017Document7 pagesPapadaki 2017Teresa MataNo ratings yet
- 3D Solar System With Opengl and C#Document4 pages3D Solar System With Opengl and C#Shylaja GNo ratings yet
- FulfillerDocument8 pagesFulfillermanojeil1No ratings yet
- A Meta Analysis of Effectiveness of Interventions To I - 2018 - International JoDocument12 pagesA Meta Analysis of Effectiveness of Interventions To I - 2018 - International JoSansa LauraNo ratings yet
- CS/CS/SB 1550: Prescription DrugsDocument49 pagesCS/CS/SB 1550: Prescription DrugsBrandon HoganNo ratings yet
- Csir - CimfrDocument31 pagesCsir - Cimfrshravan kumarNo ratings yet
- From Verse Into A Prose, English Translations of Louis Labe (Gerard Sharpling)Document22 pagesFrom Verse Into A Prose, English Translations of Louis Labe (Gerard Sharpling)billypilgrim_sfeNo ratings yet
- Anatomija Za Umetnike PDFDocument4 pagesAnatomija Za Umetnike PDFДанило ВујачићNo ratings yet
- February 2023Document2 pagesFebruary 2023rohitchanakya76No ratings yet
- GH Bhandara RTPCR Reports From Aiims Nagpur 05.05.2023Document15 pagesGH Bhandara RTPCR Reports From Aiims Nagpur 05.05.2023Aditi NadangeNo ratings yet
- 2019 AhmadDocument73 pages2019 Ahmadaateka02No ratings yet
- China VS1-24 Series Indoor High Voltage Vacuum Circuit Breaker Factory and Manufacturers - GhoritDocument6 pagesChina VS1-24 Series Indoor High Voltage Vacuum Circuit Breaker Factory and Manufacturers - GhoritKalidass BackNo ratings yet
- Soal Bing XiDocument9 pagesSoal Bing XiRhya GomangNo ratings yet
- Iit Ashram: Guj - Board Pattern Test-7Document6 pagesIit Ashram: Guj - Board Pattern Test-7rult007No ratings yet