Professional Documents
Culture Documents
Cytokines
Uploaded by
Mohamed Mido0 ratings0% found this document useful (0 votes)
7 views10 pagesCytokines and acute phase reactants play important roles in the immune response. Cytokines include tumor necrosis factors, interferons, chemokines, and interleukins that help coordinate immune cell communication and activity. The liver produces acute phase reactants like C-reactive protein, serum amyloid A, complement proteins, alpha1-antitrypsin, haptoglobin, fibrinogen, and ceruloplasmin in response to cytokines released during infection or injury to help clean up dead/damaged cells, recruit immune cells, and promote healing.
Original Description:
acute phase protein
Original Title
5. Cytokines
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCytokines and acute phase reactants play important roles in the immune response. Cytokines include tumor necrosis factors, interferons, chemokines, and interleukins that help coordinate immune cell communication and activity. The liver produces acute phase reactants like C-reactive protein, serum amyloid A, complement proteins, alpha1-antitrypsin, haptoglobin, fibrinogen, and ceruloplasmin in response to cytokines released during infection or injury to help clean up dead/damaged cells, recruit immune cells, and promote healing.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views10 pagesCytokines
Uploaded by
Mohamed MidoCytokines and acute phase reactants play important roles in the immune response. Cytokines include tumor necrosis factors, interferons, chemokines, and interleukins that help coordinate immune cell communication and activity. The liver produces acute phase reactants like C-reactive protein, serum amyloid A, complement proteins, alpha1-antitrypsin, haptoglobin, fibrinogen, and ceruloplasmin in response to cytokines released during infection or injury to help clean up dead/damaged cells, recruit immune cells, and promote healing.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 10
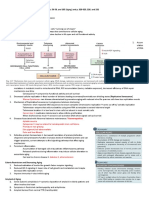
Unit 1: Nature of the Immune System
Part 3: Cytokines and Acute Phase Reactants
Cytokines
1. Tumor necrosis factors (TNF) named because they induced
lysis in tumor cells; many types with diverse biological
functions, including vasodilation and increased
vasopermeability
2. Interferons named because they interfere with viral
replication; first line of defense against viruses – tries to keep
it localized; activate NK cells
3. Chemokines (also known as a chemotaxin) family that
enhances motility and promotes migration of WBC toward
the chemokine source via a process known as chemotaxis
4. Colony stimulating factors (CSF) stimulate hematopoiesis
to replenish various cell populations when needed
5. Interleukins (IL) secreted by leukocytes and mainly act on
other leukocytes (WBC-to-WBC communication); IL1-IL38
Acute-Phase Reactants
□ Defined: normal serum constituents that increase rapidly
because of infection, injury, or trauma to tissues
□ In response to injury local inflammatory cells (neutrophils,
granulocytes and macrophages) secrete a number of cytokines
into the bloodstream, most notable of which are the
interleukins
□ The liver responds by producing a large number of
acute-phase reactants
C-Reactive Protein
□ Increases rapidly within 4-6 hours of infection
or injury
□ Returns to normal rapidly once condition
subsides
□ Non-specific, but very sensitive
□ Used to monitor healing and has also
increased in usefulness in diagnosing
myocardial infarction (heart attack)
Serum Amyloid A
□ Major protein secreted during the acute phase
of inflammation
□ Has several roles, including
■ Removes cholesterol from cholesterol-filled
macrophages at site of injury – clean up
■ Recruitment of immune cells to inflammatory
sites
■ Thought to play a role in cholesterol metabolism
Complement
□ A series of serum proteins involved in
mediation of inflammation but also involved
in
1. Opsonization
2. Chemotaxis
3. Cell lysis
Alpha1-Antitrypsin
□ Increases during acute inflammation
□ Protects tissues from enzymes of inflammatory cells,
especially elastase (a protease)
□ When the lungs do not have enough
alpha1-antitrypsin, elastase is free to destroy lung
tissue
□ As a result, the lungs lose some of their ability to
expand and contract (elasticity). This leads to
emphysema and sometimes makes breathing
difficult.
Haptoglobin
□ Binds irreversibly to free hemoglobin to
protect kidneys from damage and prevent loss
of iron by urinary excretion
□ Haptoglobin/hemoglobin complex removed
by RES, mainly spleen
□ Used to monitor hemolysis
Fibrinogen
□ A coagulation factor integral to clot formation
which serves as a barrier to prevent spread of
microorganisms further in the body
□ Levels increase with tissue inflammation or
tissue destruction
Ceruloplasmin
□ Principal copper transporting protein in plasma, plays a role
in iron metabolism and histamine regulation
□ Stimulates the immune system to fight infections, repair
injured tissues and promote healing
□ Depletion found in Wilson’s disease, causes the body to
absorb and retain excessive amounts of copper
■ Copper deposits in the liver, brain, kidneys, and the eyes
■ The deposits of copper cause tissue damage, necrosis
(death of the tissues), and scarring, which causes
decreased functioning of the organs affected
■ Liver failure and damage to the central nervous system
(brain, spinal cord) are the most predominant, and the
most dangerous, effects of the disorder
You might also like
- Inflammation PPT - OdpDocument82 pagesInflammation PPT - OdpBhanu PraseedhaNo ratings yet
- Drugs Acting On The Immune SystemDocument162 pagesDrugs Acting On The Immune SystemKrizelle Varona100% (1)
- Chapter 2.3Document37 pagesChapter 2.3Clare MercadoNo ratings yet
- Patho Unit 4.1Document20 pagesPatho Unit 4.1Lily ChouNo ratings yet
- SirsDocument49 pagesSirsJesca MgegelaNo ratings yet
- Drugs Acting On The Immune SystemDocument6 pagesDrugs Acting On The Immune Systembeautifuljade_16100% (2)
- Drugs Acting On The Immune SystemDocument11 pagesDrugs Acting On The Immune SystemloiselleilanoNo ratings yet
- Drugs Acting On The Immune SystemDocument16 pagesDrugs Acting On The Immune SystemRellie Castro0% (2)
- Inflammation and HealingDocument44 pagesInflammation and HealingAncy VarkeyNo ratings yet
- Sistem ImunologiDocument41 pagesSistem ImunologidesydewiNo ratings yet
- 12 The Nonspecific Defense Mechanism 1-19-17 1Document38 pages12 The Nonspecific Defense Mechanism 1-19-17 1isa masiasNo ratings yet
- Biochemistry of InflamationDocument45 pagesBiochemistry of Inflamationmichot feleguNo ratings yet
- Inflammatory ResponseDocument7 pagesInflammatory Responseᵇᵅᵇᵞ Anden GonzagaNo ratings yet
- Chapter 1 Basic Immunology Ppts DZ 2010Document39 pagesChapter 1 Basic Immunology Ppts DZ 2010malake.a13cj7No ratings yet
- ImmunologyDocument9 pagesImmunologyRamadhan Dwi AnggoroNo ratings yet
- Module 4 Chronic InflammationDocument34 pagesModule 4 Chronic InflammationAllan SigangaNo ratings yet
- Cell Injury, Adaptation, and DEATHDocument31 pagesCell Injury, Adaptation, and DEATHagungNo ratings yet
- Session 11 Outcomes of InflammationDocument22 pagesSession 11 Outcomes of InflammationGodfrey GeorgeNo ratings yet
- InflammationDocument54 pagesInflammationPoco PocoNo ratings yet
- Inflammatory CellsDocument5 pagesInflammatory CellsFahad KhanNo ratings yet
- Inflammation and Tissue RepairDocument55 pagesInflammation and Tissue RepairSingitan SiyoumNo ratings yet
- Inflammation: Benito K. Lim Hong III, M.DDocument70 pagesInflammation: Benito K. Lim Hong III, M.DCoy NuñezNo ratings yet
- Fish and Shellfish Diseases U 2 C 1Document24 pagesFish and Shellfish Diseases U 2 C 1Thakur VeeruNo ratings yet
- Pathophysiology Notes 1-4Document24 pagesPathophysiology Notes 1-4Scotty Banks100% (3)
- Clinical CaseDocument25 pagesClinical CaseRussell Talan CilotNo ratings yet
- Week 1.3 Defense MechanismsDocument39 pagesWeek 1.3 Defense MechanismsDio Rafael DeynataNo ratings yet
- Surgery NotesDocument9 pagesSurgery NotesClaire MayNo ratings yet
- NCM 104 - ImmunologyDocument102 pagesNCM 104 - ImmunologyfaithopeloveNo ratings yet
- Scenario 3.3.1Document18 pagesScenario 3.3.1Unarine MudauNo ratings yet
- Cytokine StormDocument16 pagesCytokine StormParulNo ratings yet
- Unit 4.1Document8 pagesUnit 4.1Bloody MarieNo ratings yet
- Membrane Phospholipids & Inflammatory Mediators: Dr. Salar A. AhmedDocument21 pagesMembrane Phospholipids & Inflammatory Mediators: Dr. Salar A. AhmedJoo Se HyukNo ratings yet
- 101 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eDocument20 pages101 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eRizky Angga PerdanaNo ratings yet
- Pharma Reviewer MidtermDocument21 pagesPharma Reviewer Midtermjana whiteNo ratings yet
- Chronic InflammationDocument24 pagesChronic InflammationTommys100% (1)
- Brief History of Veterinary Immunology: Chapter 1 - The Defense of The BodyDocument9 pagesBrief History of Veterinary Immunology: Chapter 1 - The Defense of The BodyZoe Alea MartinezNo ratings yet
- Systemic Response To Injury: Janneth T. Tan, MDDocument38 pagesSystemic Response To Injury: Janneth T. Tan, MDkira santosNo ratings yet
- Mast Cells and Allergy.Document7 pagesMast Cells and Allergy.coolcat92011hotmail.comNo ratings yet
- Acute and Chronic InflammationDocument36 pagesAcute and Chronic Inflammationibnbasheer89% (18)
- Drugs Acting On The Immune System: Retchel-Elly D. Dapli-AnDocument60 pagesDrugs Acting On The Immune System: Retchel-Elly D. Dapli-AnJoshua MendozaNo ratings yet
- Inflammation Lecture 3 Chemical Mediators and Regulators of IflammationDocument30 pagesInflammation Lecture 3 Chemical Mediators and Regulators of Iflammationtareqhaddad123No ratings yet
- Chronic InflammationDocument38 pagesChronic InflammationMarium AliNo ratings yet
- Mediators of Inflammation: DR - Djumadi Achmad, Sppa (K)Document33 pagesMediators of Inflammation: DR - Djumadi Achmad, Sppa (K)Elearning FK UnhasNo ratings yet
- New InflammationDocument135 pagesNew Inflammation77 Weam AliNo ratings yet
- Shock EmergenciesDocument19 pagesShock Emergenciesjinopic306No ratings yet
- 4.chronic InflammationDocument29 pages4.chronic Inflammationyaqeenallawi23No ratings yet
- Review InflamasiDocument61 pagesReview InflamasiRival d'SloversNo ratings yet
- Acute Inflammation, Cell Derived and Plasma Protein Derived Mediators, MorphologyDocument66 pagesAcute Inflammation, Cell Derived and Plasma Protein Derived Mediators, MorphologyJ Ta RaNo ratings yet
- لقطة شاشة ٢٠٢٣-١١-٠٩ في ٨.٥٣.٥٠ صDocument7 pagesلقطة شاشة ٢٠٢٣-١١-٠٩ في ٨.٥٣.٥٠ صmo44hh44No ratings yet
- BLOOD LECTURE 4 2017 Immunity 1Document38 pagesBLOOD LECTURE 4 2017 Immunity 1Philip Abayomi VincentNo ratings yet
- NewGeneral Pathology2Document305 pagesNewGeneral Pathology2Tahir AzizNo ratings yet
- InflammationDocument28 pagesInflammationMasum ShahriarNo ratings yet
- 2 - Hypersensitvity ReactionsDocument55 pages2 - Hypersensitvity ReactionsSafa TaweelNo ratings yet
- VfyggdbDocument33 pagesVfyggdbBibek RajNo ratings yet
- General Pathology and CytologyDocument110 pagesGeneral Pathology and CytologyJustine Nicole Clavel LachicaNo ratings yet
- Inflammation: Course Teacher: Imon RahmanDocument21 pagesInflammation: Course Teacher: Imon RahmanDaksh SabharwalNo ratings yet
- Lesson 1 - Cell InjuryDocument69 pagesLesson 1 - Cell InjuryAY 700No ratings yet
- Lecture Note For Colleges of Health Technology by - M.A. JiyaDocument21 pagesLecture Note For Colleges of Health Technology by - M.A. JiyaDaniel DendaNo ratings yet
- Unit 1: Nature of The Immune System: Part 5: Antigens and AntibodiesDocument27 pagesUnit 1: Nature of The Immune System: Part 5: Antigens and AntibodiesMohamed MidoNo ratings yet
- Basic Immunoassay PrinciplesDocument22 pagesBasic Immunoassay PrinciplesMohamed MidoNo ratings yet
- Adaptive ImmunityDocument34 pagesAdaptive ImmunityMohamed Mido100% (1)
- Basic Principles and Practice of Clinical Chemistry Part 1Document34 pagesBasic Principles and Practice of Clinical Chemistry Part 1Mohamed MidoNo ratings yet
- IntroductionDocument32 pagesIntroductionMohamed MidoNo ratings yet
- Body FluidsDocument24 pagesBody FluidsMohamed MidoNo ratings yet
- The Role of Iron: Ahmad Sh. Silmi MSC Haematology, FIBMSDocument66 pagesThe Role of Iron: Ahmad Sh. Silmi MSC Haematology, FIBMSMohamed MidoNo ratings yet
- 7 Laboratory SafetyDocument26 pages7 Laboratory SafetyMohamed MidoNo ratings yet
- Osmometry ElectrochemistryDocument25 pagesOsmometry ElectrochemistryMohamed MidoNo ratings yet
- Iron OverloadDocument37 pagesIron OverloadMohamed MidoNo ratings yet
- Introduction To ImmunologyDocument10 pagesIntroduction To ImmunologyArvi MandaweNo ratings yet
- Immunology ModuleDocument42 pagesImmunology ModuleAhmed KerAtyNo ratings yet
- Spondiloartritis Diagnosis 2017 222234456Document40 pagesSpondiloartritis Diagnosis 2017 222234456Alexandra BalanNo ratings yet
- Disorders of Granulocytes and MonocytesDocument45 pagesDisorders of Granulocytes and Monocytesswathi bsNo ratings yet
- Immunology of Fish: Advanced ArticleDocument9 pagesImmunology of Fish: Advanced ArticleMd. Forshed DewanNo ratings yet
- S1 Spike Protein Causes PASC, Cytokine Storm, & Long COVIDDocument115 pagesS1 Spike Protein Causes PASC, Cytokine Storm, & Long COVIDAnthony DocKek PenaNo ratings yet
- TEAS 6 Science by KellyDocument22 pagesTEAS 6 Science by KellyLily Garcia100% (1)
- Tyrosine Kinase Receptors in Oncology: Molecular SciencesDocument48 pagesTyrosine Kinase Receptors in Oncology: Molecular SciencesAnuradha Monga KapoorNo ratings yet
- Test Bank For Textbook of Diagnostic Microbiology 6th Edition MahonDocument13 pagesTest Bank For Textbook of Diagnostic Microbiology 6th Edition MahonNorma Elliot97% (29)
- Prof. Dr. Dr. Banundari Rachmawati SPPK (K) - Diabetes Mellitus. A Risk Factor For The Progression of COVID-19.Webinar PT Gandasari. 10022021Document48 pagesProf. Dr. Dr. Banundari Rachmawati SPPK (K) - Diabetes Mellitus. A Risk Factor For The Progression of COVID-19.Webinar PT Gandasari. 10022021Irene Halim SubrataNo ratings yet
- 3-d Immune Colored LectureDocument33 pages3-d Immune Colored LecturerohitNo ratings yet
- Immunology: 'S CompanionsDocument74 pagesImmunology: 'S CompanionsRoahit RajanNo ratings yet
- The Roles of B-Cell, T-Cells, and Antigens in The Immune SystemDocument5 pagesThe Roles of B-Cell, T-Cells, and Antigens in The Immune SystemSam MansfieldNo ratings yet
- Lecture 5.1: TISSUES - Human Biology (FSM)Document166 pagesLecture 5.1: TISSUES - Human Biology (FSM)Selaina NawadraNo ratings yet
- Pathology Lecture 11 Scientific TeamDocument34 pagesPathology Lecture 11 Scientific TeammikiyaskayleNo ratings yet
- Systemic Enzyme TherapyDocument10 pagesSystemic Enzyme TherapyAndrei GabrielNo ratings yet
- Periradicular Lesions (Chapter 5)Document28 pagesPeriradicular Lesions (Chapter 5)revlieeNo ratings yet
- Type 1 Diabetes Pathogenesis Genetics and ImmunotherapyDocument670 pagesType 1 Diabetes Pathogenesis Genetics and ImmunotherapyMihaela PurcaruNo ratings yet
- Obesity PathophysiologyDocument23 pagesObesity PathophysiologykotraeNo ratings yet
- Budwig Cancer GuideDocument108 pagesBudwig Cancer GuideasoboohbahNo ratings yet
- Mediators of InflammationDocument43 pagesMediators of InflammationNatasha Baloch100% (2)
- Introduction To ImmunologyDocument21 pagesIntroduction To Immunologysaeed5220020% (1)
- Destruction of Red Blood CellsDocument2 pagesDestruction of Red Blood CellsakosibusayNo ratings yet
- Robbins Inflammation and HemodynamicsDocument44 pagesRobbins Inflammation and HemodynamicsJustine HungNo ratings yet
- Nanotechnology and Nanoparticles PDFDocument103 pagesNanotechnology and Nanoparticles PDFApple TakishimaNo ratings yet
- Stevens (Science) Med TechDocument31 pagesStevens (Science) Med TechnotsoninjaninjaNo ratings yet
- Immunology: Overview (Moses Franklyn Dumbuya)Document69 pagesImmunology: Overview (Moses Franklyn Dumbuya)Moses DumbuyaNo ratings yet
- Immune System Dysfunction in The ElderlyDocument16 pagesImmune System Dysfunction in The ElderlyLiya AnjelinaNo ratings yet
- Boundless Lecture Slides: Available On The Boundless Teaching PlatformDocument132 pagesBoundless Lecture Slides: Available On The Boundless Teaching PlatformFoday S MansarayNo ratings yet
- Chapter 21 - ImmunityDocument77 pagesChapter 21 - ImmunityAk62442100% (1)