Professional Documents
Culture Documents
(2010) Rehabilitation in Semantic Dementia. Effectiveness of Reacquisition in Three Patients
Uploaded by
Gabriel Jesus Morales MoralesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(2010) Rehabilitation in Semantic Dementia. Effectiveness of Reacquisition in Three Patients
Uploaded by
Gabriel Jesus Morales MoralesCopyright:
Available Formats
Dement Neuropsychol 2010 December;4(4):306-312 Original Article
Rehabilitation in semantic dementia
Study of the effectiveness of lexical
reacquisition in three patients
Mirna Lie Hosogi Senaha1, Sonia Maria Dozzi Brucki2, Ricardo Nitrini3
Abstract – Although language rehabilitation in patients with primary progressive aphasia (PPA) is recommended,
rehabilitation studies in this clinical syndrome are scarce. Specifically, in relation to semantic dementia (SD), few
studies have shown the possibility of lexical relearning. Objective: To analyze the effectiveness of rehabilitation
for lexical reacquisition in SD. Methods: Three SD patients were submitted to training for lexical reacquisition
based on principles of errorless learning. Comparisons between naming performance of treated items (pre and
post-training) and non-treated items of the Boston Naming Test (BNT) were made. Results: All patients improved
their performance in naming treated words after intervention. However, decline in performance in naming of
non-treated items was observed. Case 1 named zero items at baseline while her performance post-training was
29.4% correct responses without cueing, and 90.7% correct with and without cueing. Case 2 named 6.9% of items
correctly at baseline and his performance in post-training was 52.9% without cueing and 87.3%, with and without
cueing. Case 3 named zero items at baseline and his performance in post-training was 100% correct responses
without cueing. Considering the performance in naming the non-treated items of the BNT, the percentages of
correct responses in the first evaluation and in the re-evaluation, respectively were: 16.7% and 8.3% (case 1; 14
month-interval); 26.7% and 11.6% (case 2; 18 month-interval) and 11.6% and 8.3% (case 3; 6 month-interval).
Conclusions: The reacquisition of lost vocabulary may be possible in SD despite progressive semantic deterioration.
Key words: semantic dementia, semantic memory, primary progressive aphasia, rehabilitation; lexical reacquisition.
Reabilitação na demência semântica: estudo da eficácia da reaquisição lexical em três pacientes
Resumo – Apesar de recomendada reabilitação da linguagem na afasia progressiva primária (APP), há poucos
estudos sobre reabilitação nesta síndrome. Especificamente, quanto à demência semântica (DS), os poucos estudos
têm mostrado possibilidade de reaprendizado lexical. Objetivo: Analisar a eficácia da reabilitação para reaquisição
lexical na DS. Métodos: Três pacientes com DS foram submetidos à reabilitação para reaquisição lexical baseada
nos princípios do aprendizado sem erro. Comparações entre desempenhos na nomeação de itens treinados (pré
e pós-tratamento) e de itens não-treinados do Teste de Nomeação de Boston (TNB) foram realizadas. Resultados:
Os pacientes obtiveram melhor desempenho na nomeação das palavras treinadas após intervenção. Por outro lado,
houve declínio no desempenho dos itens não-treinados. O caso 1 não nomeou nenhum item na linha de base (pré-
tratamento) e seu desempenho após o tratamento foi de 29,4% de acertos sem pistas e 90,7% com e sem pistas. O
caso 2 nomeou corretamente 6,9% na linha de base e sua performance, pós-treinamento, foi de 52,9% sem pistas
e 87,3%, com e sem pistas. O caso 3 não nomeou nenhum item na linha de base e após o treinamento nomeou
100% dos itens sem pista. Considerando a nomeação dos itens lexicais não-treinados do TNB, as porcentagens de
acertos na primeira e segunda avaliações foram respectivamente: 16,7% e 8,3% (caso 1; 14 meses de intervalo);
26,7% e 11,6% (caso 2; 18 meses de intervalo) e 11,6% e 8,3% (caso 3; 6 meses de intervalo). Conclusões:
A reaquisição do vocabulário perdido pode ser possível na DS apesar da progressiva deterioração semântica.
Palavras-chave: demência semântica, memória semântica, afasia progressiva primária, reabilitação, reaquisição
lexical
1
PhD, Speech pathologist, Member of Behavioral and Cognitive Neurology Unit of Department of Neurology, University of São Paulo School of Medicine, São
Paulo, Brazil. 2MD, Neurologist, Member of Behavioral and Cognitive Neurology Unit of Department of Neurology, University of São Paulo School of Medi-
cine, São Paulo, Brazil. 3MD, PhD, Neurologist, Associate Professor, Department of Neurology, University of São Paulo School of Medicine, São Paulo, Brazil.
Mirna Lie Hosogi Senaha – Rua Montesquieu, 371 / 62 - 04116-190 São Paulo SP - Brazil. E-mail: senaha@uol.com.br
Disclosure: The authors report no conflicts of interest.
Received March 10, 2010. Accepted in final form August 11, 2010.
306 Rehabilitation in semantic dementia Senaha MLH, et al.
Dement Neuropsychol 2010 December;4(4):306-312
Primary Progressive Aphasia (PPA) is a neurodegen- mended.7,9-14 Rehabilitation plays a very important role in
erative clinical syndrome in which progressive language minimizing the impact of the linguistic disturbance in dai-
impairment occurs in parallel with relative preservation ly life. Although rehabilitation is recommended, published
of other cognitive abilities. PPA was firstly defined by Me- studies addressing rehabilitation in this clinical syndrome
sulam in 1982 by means of his description of patients who are scarce.
presented gradual deterioration of language in the absence More specifically, in relation to the patients with SD,
of generalized dementia, and associated to enlargement of the few intervention studies available have shown the pos-
the sylvian fissure in the left cerebral hemisphere.1 sibility of lexical relearning despite progressive semantic
The label “semantic dementia” (SD) was given by Neary deterioration. To date, only 12 SD patients submitted to
et al. (1989) following the reporting of three patients who lexical reacquisition rehabilitation have been reported.15-24
presented progressive semantic disturbance, evidenced by Snowden & Neary (2002) studied two cases with SD, each
difficulty in naming and understanding the meanings of submitted to different experiments, and showed the pos-
words and objects.2 The patients presented fluent verbal sibility of relearning of lost words.15 According to the au-
production, but anomic and difficulties in semantic com- thors, the study showed the importance of medial temporal
prehension, despite the preservation of syntactic compre- lobe structures for the acquisition of semantic facts. Gra-
hension. Later in 1992, Hodges and colleagues character- ham et al. discussed the reacquisition of vocabulary from
ized the cognitive and linguistic profile for SD in detail, and self-training carried out by patient D.M. with SD.16-17 These
associated this clinical syndrome to temporal lobe atrophy.3 authors compared this case with another (A.M.) who did
In 1998, a consensus on clinical diagnostic criteria for fron- not enjoy the same success in lexical reacquisition. Frat-
totemporal lobar degeneration (FTLD) was published. In tali (2004) described a case in which the process of lexical
this consensus, Neary et al.4 proposed that SD, as one of relearning of a list of nouns and verbs was carried out in
the three most frequent clinical syndromes in FTLD, be conversational situations.19 The patient presented improve-
defined as “semantic aphasia associated to the associative ment after the period of therapy, but had not retained the
agnosia”. Adlam et al. (2006)5 subsequently suggested the gains at the next follow-up (three months). Jokel et al.
redefinition of associative agnosia issues in SD, pointing (2006) studied a treatment program (home practice) in
out that the non-verbal semantic impairment tends to be only one case with SD and evidenced the benefit of the
much less prominent than the verbal semantic deficit. The program for trained lexical items.18 In 2009, Heredia et al.
researchers proposed the substitution of the use of term published the case study of patient C.U.B., and found, in
“associative agnosia” to characterize SD, by “impairment contrast to the other cases, a possibility of generalization
on tests of non-verbal associative knowledge”. of lexical relearning.22 In addition, the authors had also
Recently, Rogalski & Mesulam and Mesulam & Wein- observed the maintenance of relearning despite intense de-
traub published a new revision of the diagnostic criteria terioration of semantic memory. Jokel et al. (2010) pub-
for PPA, outlining the core, ancillary and exclusionary cri- lished another SD case which was successfully submitted to
teria for PPA.6,7 According to the authors, the clinical pro- treatment for anomia based on principles of the errorless
file of PPA can be defined as “an aphasic dementia where learning approach using a computer program.20 Newhart
the language impairment emerges in relative isolation and et al (2009) compared the benefits of rehabilitation in two
is the major determinant in the limitation of daily living PPA cases, one with logopenic progressive aphasia, and the
activities. Perception, memory, personality are relatively another with SD. Both presented improvement in naming,
preserved during the initial 1-2 years”. Specifically, in rela- but the generalization was evidenced only in the patient
tion to the different subtypes of PPA, the authors suggested with logopenic progressive aphasia.21 Robinson et al. (2009)
classification into three main clinical subtypes as proposed verified the effectiveness of treatment for object naming,
by Gorno-Tempini et al.:8 agrammatic subtype, logopenic definition and object use in two SD cases. Both patients
progressive aphasia, and semantic subtype. These variants showed improvement, but only one had retained the im-
are the main subtypes, but other clinical manifestations of provement at the follow up.23 Bier et al. (2009) studied the
PPA are described in the literature. According to Mesulam method of formal-semantic therapy (which focuses on
and Weintraub,7 the semantic subtype fits the criteria for restoring lost concepts and discriminating between these
semantic dementia redefined by Adlam et al.5. concepts) used in non-degenerative fluent aphasics com-
Considering that PPA patients present selective impair- bined with the spaced retrieval method in an SD case. The
ment and are independent regarding daily living activities, authors observed the possibility of improvement in nam-
except in situations which rely heavily on linguistic abili- ing performance, but with limitations.24
ties, cognitive-linguistic rehabilitation has been recom- Considering the few studies on intervention in SD and
Senaha MLH, et al. Rehabilitation in semantic dementia 307
Dement Neuropsychol 2010 December;4(4):306-312
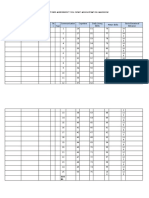
the fact that most of these display some benefits for the Table 1. Demographic data of semantic dementia patients.
patients, we can conclude that rehabilitation contributes Case 1 Case 2 Case 3
toward minimizing linguistic difficulties, and may conse- Age 55 77 56
quently postulate that rehabilitation can also contribute
Age of onset 53 76 54
to improving the life quality of patients and their relatives.
Gender F M M
Given the importance of rehabilitation in SD and the
Educational level 11 16 16
lack of studies in the literature, the present study sought
to report the lexical relearning training of three SD cases
submitted to language rehabilitation. The therapeutic ap-
proach was based on previous studies that showed the
Methods
possibility of lexical reacquisition in SD patients. In other
Subjects
words, the purpose of this study was to analyze the effec-
Three SD patients were submitted to cognitive-linguis-
tiveness of rehabilitation for lexical reacquisition in three
patients with SD. tic rehabilitation. The demographic data of these cases are
We raised two hypotheses, the first based on previous presented in Table 1. The group comprised two men and
studies that patients with SD have the capacity to reacquire one woman aged between 55 and 77, with an educational
lost lexical items. The second hypothesis was that patients level greater than 11 years. Table 2 shows the performanc-
will present improvement only on the reacquisition of es of the three patients on language tests and semantic
trained lexical items, and this would not be generalized memory tasks. Some of these tasks had been described in
for non-treated lexical items. This notion was based on a previous study.25,26 As expected for the profile of SD clini-
the characteristics of the semantic disturbance of SD: the cal syndrome, all the cases presented low performance in
anomia in SD occurs mainly due to semantic degradation visual confrontation naming (Boston Naming Test - BNT),
and this leads to systematic semantic errors. difficulties on the word definition task and oral word com-
Table 2. Performance on language and semantic memory tasks.
Case 1 Case 2 Case 3
Syntactic comprehension
– Simple and complex sentences* 37/38 38/38 38/38
Semantic comprehension
– Words+ 56/90 58/90 68/90
Repetition
– Words and non-words* 25/25 25/25 25/25
– Sentences (high frequency)§ 7/8 8/8 7/8
– Sentences (low frequency)§ 3/8 7/8 4/8
Reading aloud 86/110 109/110 96/110
– Words and non-words|| surface dyslexia semantic dyslexia surface dyslexia
Writing to dictation 28/46 70/110 62/110
– Words and non-words|| surface dysgraphia surface dysgraphia surface dysgraphia
Visual confrontation naming
– Pictures¶ 10/60 16/60 7/60
Verbal fluency
– Animals 5 6 6
– FAS (total) 20 13 17
Word definition+ 2/13 4/13 3/13
Visual sorting+ 137/168 150/168 155/168
*Beta MT-8630; +Semantic memory battery; §Boston Diagnostic Aphasia Examination31; ||HFSP protocol32; ¶Boston Naming Test33.
308 Rehabilitation in semantic dementia Senaha MLH, et al.
Dement Neuropsychol 2010 December;4(4):306-312
Figure 1. Examples of structural imaging (MRI) of cases 1 and 3. [A] Case 1. Anterior temporal lobe atrophy, more prominent
on right side; [B] Case 3. Anterior temporal lobe atrophy, more prominent on left side.
prehension (word-picture matching task), preserved syn- lexical difficulties faced in their daily lives; [3] through in-
tactic comprehension, surface dysgraphia and impairment formation supplied by the relatives.
on tests of non-verbal associative knowledge. The diagnosis Using the selection of the words to be trained, cards
of SD was confirmed by experienced cognitive neurologists were assembled containing figures, photos or written de-
and was based on clinical history, neurological examina- scriptions on one side of the cards while the back of each
tion, neuropsychological and language evaluation, and card contained a written graphic cue that induced the
neuroimaging data. Results on neuroimaging examination correct naming of each stimulus. With the training and
(MRI) were consistent with diagnoses of SD. All the cases progression in correct answers in the naming with the aid
presented temporal lobe atrophy. Case 1 presented anterior of the cues, the letters of the graphic cues were gradually
temporal lobe atrophy, which was more prominent on the removed as shown in Figure 2 (vanishing cues).
right side whereas cases 2 and 3 presented temporal lobe The sessions of this lexical reacquisition intervention
atrophy predominantly in the left hemisphere (Figure 1) were carried out once or twice a week. All the patients were
instructed to carry out daily home self-training. Despite
Stimulation for lexical reacquisition the recommendation of daily training, case 2 carried out
The patients were submitted to language rehabilitation the training only once or twice a week.
individually. One of the principle focuses was the stimula- For the analysis of the effectiveness of the training of
tion for lexical reacquisition since the main complaint of lexical reacquisition, comparisons between naming of the
the patients and their relatives was related to verbal seman- treated items (pre and post-training) and of non-treated
tic impairment (anomia and word comprehension impair- items (BNT) were carried out for each case. The length of
ment), the most evident characteristics in SD. the training and the number of treated lexical items varied
The stimulation for the lexical reacquisition carried for each patient (case 1: 119 treated items, 14 months of
out was based on principles of the errorless learning ap- intervention; case 2: 87 treated items, 18 months of inter-
proach.27-29 For the training of lexical reacquisition, it was vention; case 3: 65 treated items, 6 months of interven-
necessary to carry out a selection of words for stimulation. tion). The assessment of non-treated items of BNT - first
The selection of words to be trained was personalized, tak- evaluation and re-evaluation - occurred in parallel at the
ing into account the difficulties and particular needs of beginning and end of the lexical stimulation in each case.
each patient and their relevance to daily life.
The selection of the words occurred in a dynamic way Results
and in several different manners: [1] from the observa- The results of the patients’ performances on the naming
tion of the patients’ lexical problems in situations involv- of non-treated lexical items and treated items are depicted
ing spontaneous speech; [2] through information and in Figure 3. Each sub item of Figure 3 shows the results
complaints provided by the patients who wrote down the for each patient displayed on two graphs: the first graph
Senaha MLH, et al. Rehabilitation in semantic dementia 309
Dement Neuropsychol 2010 December;4(4):306-312
A CASE 1
Non-treated items Treated items
100% 100%
90.7%
80% 80%
60% 60%
40% 40%
29.4%
23.3%
20% 16.7% 15% 20%
8.3%
0%
0% 0%
BNT - 1st evaluation BNT - 2nd evaluation Pre-training Post-training
Rehabilitation lenght: 14 months Treated items: 119 words
Correct response (without cueing) Correct response (without cueing and with phonemic cues)
B CASE 2
Non-treated items Treated items
100% 100%
87.3%
80% 80%
60% 60% 52.9%
40% 40%
31.7%
26.7%
20% 18.3% 20%
11.6%
6.9%
0% 0%
BNT - 1st evaluation BNT - 2nd evaluation Pre-training Post-training
Rehabilitation lenght: 18 months Treated items: 87 words
Correct response (without cueing) Correct response (without cueing and with phonemic cues)
C CASE 3
Non-treated items Treated items
Figure 2. Cards samples for training of lexical reacquisition. 100% 100%
100%
80% 80%
60% 60%
shows the comparison of the performances on the naming
40% 40%
of non-treated items (Boston Naming Test) for the first and 28.3%
23%
the second evaluations that occurred at the beginning and 20%
11.6%
8.3%
20%
end of the stimulation of lexical reacquisition. The second 0%
BNT - 1st evaluation BNT - 2nd evaluation
0%
0%
Pre-training Post-training
graph shows the comparison of the performances on the
naming of the treated items (pre and post-training). Rehabilitation lenght: 6 months Treated items: 65 words
All three patients presented a decline in performances in
Correct response (without cueing) Correct response (without cueing and with phonemic cues)
naming non-treated items between the first evaluation and
the re-evaluation yet presented improvement in the perfor- Figure 3. Comparison of patient’s performance in the naming of
mances in naming of treated items (pre and post-training). non-treated and treated lexical items.
Discussion
All the patients showed improved performance in nam- These results confirm the two hypotheses put forward
ing treated items after rehabilitation, in spite of decline in initially: firstly, that SD patients have the capacity to relearn
performance on non-treated items. This data indicates the lost lexical items, and secondly that the reacquisition only
effectiveness of the lexical stimulation without generaliza- occurs for treated lexical items, without generalization for
tion. Despite the absence of generalization, the possibility non-treated lexical items.
of patients using the reacquired lexical items functionally, In SD, anomia occurs principally due to semantic de-
i.e. in “extra-training” situations, was demonstrated in terioration rather than lexical access impairment. For this
spontaneous speech situations. reason and because of the type of therapeutic intervention
310 Rehabilitation in semantic dementia Senaha MLH, et al.
Dement Neuropsychol 2010 December;4(4):306-312
used for lexical reacquisition, generalization of the lexical 3. Hodges JR, Patterson K, Oxburry S, Funnell E. Semantic de-
relearning of non-treated items did not occur. This non- mentia. Progressive fluent aphasia with temporal lobe atro-
generalization for non-treated lexical elements was also phy. Brain 1992;1151783-1806.
evidenced in other studies.16-18,21 4. Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lo-
The benefits of the rehabilitation process involving the bar degeneration. A consensus on clinical diagnostic criteria.
lexical reacquisition of our three patients varied from case Neurology 1998;51:1546-1554.
to case. Case 3 was the patient who presented the greatest 5. Adlam ALR, Patterson K, Rogers TT, et al. Semantic dementia
gain as he was able to name all treated items without cues and fluent primary progressive aphasia: two sides of the same
after the intervention. In this study, it was not possible to coin? Brain 2006;129:3066-3080.
associate the intensity of the therapeutic benefit to factors 6. Rogaslki E, Mesulam MM. Clinical Trajectories and biologi-
such as age, gender, rehabilitation time and severity of the cal Features of primary progressive aphasia (PPA). Curr Al-
disturbance. Case 3 had the greatest gain but presented the zheimer Res 2009;6:331-336.
lowest performance on the Boston Naming Test in the first 7. Mesulam M, Weintraub S. Primary progressive aphasia and
evaluation and underwent less rehabilitation in terms of kindred disorders. Handb Clin Neurol 2008;89:573-587.
time. 8. Gorno-Tempini ML, Dronkers NF, et al. Cognition and anat-
The success of the therapeutic intervention, even omy in three variants of primary progressive aphasia. Ann
with limitations in neurodegenerative disease such as SD, Neurol 2004;55:335-346.
is relevant to patients and their relatives when minimizing 9. Henry, ML, Beeson, PM, Rapcsak, SZ. Treatment for anomia
linguistic difficulties. Moreover, it serves as a motivational in semantic dementia. Semin Sppech Lang 2008;29:60-70.
stimulus, as patients and relatives have the opportunity to 10. Mesulam MM. Primary progressive aphasia a 25-year retro-
experience the possibility of relearning, reinforcing one spective. Alzheimer Dis Assoc Disord 2007;21:S8-S11.
of the characteristics of PPA - the presence of a selective 11. Mesulam MM. Primary progressive aphasia: a language-based
disturbance along with relative preservation of other dementia. N Engl J Med 2003;349:1535-1542.
cognitive abilities. 12. Mesulam MM. Primary progressive aphasia. Ann Neurol
The personalized selection of words to be trained was 2001;49:425-432.
important, by considering the difficulties and particular 13. Murray LM. Longitudinal treatment of primary progressive
needs of each patient and relevance in their daily lives. aphasia: a case study. Aphasiology 1998;12:651-672.
Akin to previous studies on non-pharmacological in- 14. Weintraub S, Rubin NP, Mesulam MM. Primary progressive
tervention in SD, the present study has the limitation of a aphasia: longitudinal course, neuropsychological profile, and
small number of cases in the sample. Another important language features. Arch Neurol 1990;47:1329-1335
issue is, although the training for the three patients had the 15. Snowden JS, Neary D. Relearning of verbal labels in semantic
same theoretical principles of errorless learning, there was dementia. Neuropsychologia 2002;40:1715-1728.
no strict use of the same lexical items or number of sessions 16. Graham KS, Patterson K, Pratt KH, Hodges JR. Relearning and
for the three cases. In contrast to other studies, we chose to subsequent forgetting of semantic category exemplars in a cast
personalize the selection of words to be trained according of semantic dementia. Neuropsychology 1999;13:359-380.
to the particular needs of each patient. This option can be 17. Graham KS, Patterson K, Pratt KH, Hodges JR. Can repeat-
viewed as a disadvantage for the comparison of variables ed exposure to “forgotten” vocabulary help alleviate word-
and those involved in the effectiveness of the treatment finding difficulties in semantic dementia? An illustrative case
study. However, we believe this to be important for reach- study. Neuropsychol Rehabil 2001;11:429-454.
ing the individuals’ needs and for motivational aspects. 18. Jokel R, Rochon E, Leonard C. Treating anomia in semantic
In spite of these limitations, the results have proven the dementia: improvement, maintenance, or both? Neuropsy-
effectiveness of the intervention for lexical reacquisition in chol Rehabil 2006;16:241-256.
the three SD cases, despite progressive semantic deteriora- 19. Frattali C. An errorless learning approach to treating dysno-
tion, thus demonstrating the ability of lexical relearning mia in frontotemporal dementia. J Med Speech Lang Pathol
in SD patients. 2004;12:11-24.
20. Jokel R, Rochon E, Anderson ND. Errorless learning of com-
References puter-generated words in a patient with semantic dementia.
1. Mesulam MM. Slowly progressive aphasia without general- Neuropsychol Rehabil 2010;20:16-41.
ized dementia. Ann Neurol 1982;11:592-598. 21. Newhart M, Davis C, Kannan V, Heidler-Gary J, Cloutman
2. Snowden JS, Goulding PJ, Neary D. Semantic dementia: a form of L, Hillis AE. Therapy for naming deficits in two variants of
circumscribed cerebral atrophy. Behav Neurol 1989;2:167-182. primary progressive aphasia. Aphasiology 2009;23:823-834.
Senaha MLH, et al. Rehabilitation in semantic dementia 311
Dement Neuropsychol 2010 December;4(4):306-312
22. Heredia CG, Sage K, Lambon-Ralph MA, Berthier ML. Re- Linden DEJ. Goal-oriented cognitive rehabilitation for an in-
learning and retention of verbal labels in a case of semantic dividual with Mild Cognitive Impairment: Behavioural and
dementia. Aphasiology 2009;23:192-209. neuroimaging outcomes. Neurocase 2009;15:318-331.
23. Robinson S, Druks J, Hodges JR, Garrard P. The treatment of 28. Clare L, Jones RSP. Errorless learning in the rehabilitation of
object naming, definition and object use in semantic demen- memory impairment: a critical review. Neuropsychol Review
tia: the effectiveness of errorless learning. Aphasiology 2009; 2008;18:1-23.
23:749-775. 29. Clare L, Wilson BA, Carter G, Roth I, Hodges JR. Relearning
24. Bier N, Macoir J, Gagnon L, Van der Linden M, Louveaux S, of face-name associations in early Alzheimer’s disease. Neu-
Desrosiers J. Known, lost, and recovered: Efficacy of formal- ropsychology 2002;16:538-547.
semantic therapy and spaced retrieval method in a case of 30. Nespoulous JL, Lecours AR, Lafond D, Parente MAMP. Pro-
semantic dementia. Aphasiology 2009;23:210-235. tocole Montréal-Tolouse MT-86 d’examen linguistique de
25. Senaha MLH, Caramelli P, Porto CS, Nitrini R. Semantic de- l’aphasie-version Beta. Laboratoire Théophile-Alajouanine,
mentia Brazilian study of nineteen cases. Dement Neuropsy- Montréal; 1986.
chol 2007;1:366-373. 31. Goodglass H, Kaplan E. The Assessment of Aphasia and Relat-
26. Senaha MLH, Caramelli P, Porto CS, Nitrini R. Verbal and ed Disorders. 2nd ed., Philadelphia, PA: Lea & Febiger; 1983.
non-verbal semantic impairment: from fluent primary pro- 32. Parente MAMP, Hosogi ML, Delgado AP, Lecours AR. Proto-
gressive aphasia to semantic dementia. Dement Neuropsychol colo de Leitura para o projeto H.F.S.P.;São Paulo; 1992.
2007;1:203-211 33. Kaplan E, Goodglass H, Weintraub S. The Boston Naming
27. Clare L, Van Paasschen J, Evans SJ, Parkinson C, Woods RT, Test. Philadelphia: Lea & Febiger; 1983.
312 Rehabilitation in semantic dementia Senaha MLH, et al.
You might also like
- "What I Mean Is..." A Structured Program to Improve Mild to Moderate Retrieval/Fluency Problems 3rd EditionFrom Everand"What I Mean Is..." A Structured Program to Improve Mild to Moderate Retrieval/Fluency Problems 3rd EditionRating: 5 out of 5 stars5/5 (1)
- California Verbal Learning Test: Performance by Patients With Focal Frontal and Non-Frontal LesionsDocument11 pagesCalifornia Verbal Learning Test: Performance by Patients With Focal Frontal and Non-Frontal LesionsAngela Bibiana Cañon OrtizNo ratings yet
- 2011 Acta Lambon&cols PDFDocument18 pages2011 Acta Lambon&cols PDFMaca Martínez-CuitiñoNo ratings yet
- Effects of Phonomotor Treatment On The Reading Abilities of Individuals With Aphasia and Phonological AlexiaDocument7 pagesEffects of Phonomotor Treatment On The Reading Abilities of Individuals With Aphasia and Phonological Alexiamary engNo ratings yet
- Adlam Et Al., 2006Document15 pagesAdlam Et Al., 2006Axel MayartNo ratings yet
- Cognition AphasiaDocument16 pagesCognition AphasiaKarolina SantiagoNo ratings yet
- Decreasing Cues For A Dynamic List of Noun and Verb Naming Targets: A Case-Series Aphasia Therapy StudyDocument25 pagesDecreasing Cues For A Dynamic List of Noun and Verb Naming Targets: A Case-Series Aphasia Therapy StudyUTKARSH SHUKLANo ratings yet
- 2013 Evaluacion Del Entrenamiento de La Atencion y Facilitacion Metacognitiva para Mejorar La Lectura en La Comprension AfasicaDocument18 pages2013 Evaluacion Del Entrenamiento de La Atencion y Facilitacion Metacognitiva para Mejorar La Lectura en La Comprension AfasicaAlba Sueiro DominguezNo ratings yet
- Dislexia FonológicaDocument9 pagesDislexia FonológicaBrenda BorgesNo ratings yet
- A Systematic Review of Treatment OutcomeDocument19 pagesA Systematic Review of Treatment OutcomeDayna DamianiNo ratings yet
- " The Effectiveness of Verbal-Gestural Treatment On Verb Naming in Acute Inpatient Rehabilitation" Journal Article ReviewDocument6 pages" The Effectiveness of Verbal-Gestural Treatment On Verb Naming in Acute Inpatient Rehabilitation" Journal Article Reviewapi-709202309No ratings yet
- Tratamiento en APP 2013Document34 pagesTratamiento en APP 2013Mauricio EtchegarayNo ratings yet
- Rest Primary Progressive Aphasia: A Tale of Two Syndromes and TheDocument10 pagesRest Primary Progressive Aphasia: A Tale of Two Syndromes and TheDranmar AhmedNo ratings yet
- Artigo para população brasileira - idososDocument5 pagesArtigo para população brasileira - idososDayanne SilvaNo ratings yet
- Murray2014 2 PDFDocument20 pagesMurray2014 2 PDFJaviera Cortés MoralesNo ratings yet
- Neuropsychologia: Jade Dignam, David Copland, Alicia Rawlings, Kate O 'Brien, Penni Burfein, Amy D. RodriguezDocument12 pagesNeuropsychologia: Jade Dignam, David Copland, Alicia Rawlings, Kate O 'Brien, Penni Burfein, Amy D. RodriguezFrancisco Beltrán NavarroNo ratings yet
- Addressing Cognitive Skills in Aphasia Therapy? A Primer For CliniciansDocument1 pageAddressing Cognitive Skills in Aphasia Therapy? A Primer For CliniciansFelipeAndresPradenaMenesesNo ratings yet
- Hardy2015 Linguagem e DftDocument13 pagesHardy2015 Linguagem e DftLuciana CassimiroNo ratings yet
- Striking Loss of Second Language in Bilingual Patients With Semantic Dementia (Journal of Neurology) (2019)Document10 pagesStriking Loss of Second Language in Bilingual Patients With Semantic Dementia (Journal of Neurology) (2019)fandomstwentyoneNo ratings yet
- Alexia Central ArtDocument15 pagesAlexia Central Artsandra patricia monterrey gomezNo ratings yet
- Generalization and Maintenance of Treatment Gains in Primary Progressive Aphasia (PPA) : A Systematic ReviewDocument18 pagesGeneralization and Maintenance of Treatment Gains in Primary Progressive Aphasia (PPA) : A Systematic ReviewBrian CasasnovasNo ratings yet
- Brain and Language: Eun Jin Paek, Laura L. Murray, Sharlene D. NewmanDocument13 pagesBrain and Language: Eun Jin Paek, Laura L. Murray, Sharlene D. NewmanCamila BarreraNo ratings yet
- Tips - Habib 2Document2 pagesTips - Habib 2Michel HabibNo ratings yet
- Doctoral Thesis Subtypes of DevelopmentaDocument300 pagesDoctoral Thesis Subtypes of DevelopmentaИрина МокракNo ratings yet
- Immediate List Recall As A Measure of Short-Term Episodic Memory: Insights From The Serial Position Effect and Item Response TheoryDocument11 pagesImmediate List Recall As A Measure of Short-Term Episodic Memory: Insights From The Serial Position Effect and Item Response TheoryRomina BoldasuNo ratings yet
- Long-Term Maintenance of Anomia Treatment Effects inDocument26 pagesLong-Term Maintenance of Anomia Treatment Effects inHarumy NakayamaNo ratings yet
- Treatment of Primary Progressive Aphasia: Donna C. Tippett, MPH, Ma Argye E. Hillis, MD, Ma Kyrana Tsapkini, PHDDocument11 pagesTreatment of Primary Progressive Aphasia: Donna C. Tippett, MPH, Ma Argye E. Hillis, MD, Ma Kyrana Tsapkini, PHDKomputer BossquNo ratings yet
- 701 Bhavika Agarwal Cog AssignmentDocument9 pages701 Bhavika Agarwal Cog AssignmentTA701 Bhavika AgarwalNo ratings yet
- Can Non Linguistic Cognitive Stimulation Enhance The Cognitive and Linguistic Functions of People With Aphasia Receiving Conversation TherapyDocument29 pagesCan Non Linguistic Cognitive Stimulation Enhance The Cognitive and Linguistic Functions of People With Aphasia Receiving Conversation TherapyUTKARSH SHUKLANo ratings yet
- Action (Verb Naming) Uency As An Executive Function Measure: Convergent and Divergent Evidence of ValidityDocument5 pagesAction (Verb Naming) Uency As An Executive Function Measure: Convergent and Divergent Evidence of ValiditySandy KOLBASINo ratings yet
- Effective Music Therapytechniquesfor Aphasia Tomaino 2012Document7 pagesEffective Music Therapytechniquesfor Aphasia Tomaino 2012אהרון גור אריהNo ratings yet
- Da Cunha Pereira 2017Document7 pagesDa Cunha Pereira 2017Pablo Andrés Sánchez MonsalveNo ratings yet
- Efectos de La Terapia en Disfonia Musculotensional.2017Document7 pagesEfectos de La Terapia en Disfonia Musculotensional.2017Jenith Karem Paredes GonzalezNo ratings yet
- Neuropsychological Evaluation in Patients With Eating DisordersDocument6 pagesNeuropsychological Evaluation in Patients With Eating DisordersSabri Lozada MonfortNo ratings yet
- Sentence Comprehension in Parkinson's DiseaseDocument6 pagesSentence Comprehension in Parkinson's DiseaseKarina Andrea Torres OcampoNo ratings yet
- Recovery in AphasiaDocument6 pagesRecovery in Aphasiakeihoina keihoinaNo ratings yet
- WORKING MEMORY, SECOND LANGUAGE ACQUISITION AND LOW EDUCATED SECOND LANGUAGE AND LITERACY LEARNERS: Alan JuffsDocument16 pagesWORKING MEMORY, SECOND LANGUAGE ACQUISITION AND LOW EDUCATED SECOND LANGUAGE AND LITERACY LEARNERS: Alan JuffsAnindita PalNo ratings yet
- APP Comprensión Palabra en Área de WernickeDocument11 pagesAPP Comprensión Palabra en Área de WernickeBazarCasiopeaNo ratings yet
- The Effects of Oral Motor Exercises On Diadochokinetic RatesDocument23 pagesThe Effects of Oral Motor Exercises On Diadochokinetic RatesNicole GrayNo ratings yet
- HVLTDocument19 pagesHVLTVicente Cáceres100% (3)
- Evolution of Phonemic Word Fluency PerformanceDocument25 pagesEvolution of Phonemic Word Fluency PerformancecharlesamaralsNo ratings yet
- Treatment of Wernicke'S Aphasia With Jargon: A Case StudyDocument11 pagesTreatment of Wernicke'S Aphasia With Jargon: A Case StudyIvanaNo ratings yet
- Semantic fluency definitionDocument7 pagesSemantic fluency definitioncapereh11No ratings yet
- WRAML CVLTfinalDocument29 pagesWRAML CVLTfinallaajimi olfaNo ratings yet
- NeuropsychologiaDocument11 pagesNeuropsychologiaJaqueline AlvarezNo ratings yet
- 2021 - Ajslp 20 00265Document9 pages2021 - Ajslp 20 00265Luis.fernando. GarciaNo ratings yet
- The Effectiveness of Transcranial Direct Current Stimulation (TDCS) With Broad-Frontal Montages On Improving Working Memory and Reading Skills in Dyslexic Children A Randomized Clinical Trial.Document8 pagesThe Effectiveness of Transcranial Direct Current Stimulation (TDCS) With Broad-Frontal Montages On Improving Working Memory and Reading Skills in Dyslexic Children A Randomized Clinical Trial.Hossein AsgarianNo ratings yet
- PeterDocument5 pagesPeterErsya MuslihNo ratings yet
- Mecanismos Betabolicos de Fadiga VocalDocument11 pagesMecanismos Betabolicos de Fadiga VocalIsabel Monteiro GomesNo ratings yet
- 3 Rehabilitation of AphasiaDocument10 pages3 Rehabilitation of AphasiaMatthew PhillipsNo ratings yet
- Effects of Impairment Based Individual and Socially Oriented Group Therapies On Verb Production in AphasiaDocument19 pagesEffects of Impairment Based Individual and Socially Oriented Group Therapies On Verb Production in AphasiaConcepcion NeulingNo ratings yet
- Effectiveness of Twice-Weekly Rapid Syllable Transitions Treatment for Childhood Apraxia of SpeechDocument14 pagesEffectiveness of Twice-Weekly Rapid Syllable Transitions Treatment for Childhood Apraxia of SpeechFernanda FreitasNo ratings yet
- Maximising Recovery From Aphasia With Central andDocument28 pagesMaximising Recovery From Aphasia With Central andHarumy NakayamaNo ratings yet
- NEOLOGISMODocument6 pagesNEOLOGISMOMarcela MercadoNo ratings yet
- U07d1 Memory SystemDocument3 pagesU07d1 Memory Systemarhodes777No ratings yet
- 10.1016@j.neuropsychologia.2016.07.009 Neuropsychol 91 (October 2016) 36-49 Brain mechanisms of recovery from pure alexiaDocument35 pages10.1016@j.neuropsychologia.2016.07.009 Neuropsychol 91 (October 2016) 36-49 Brain mechanisms of recovery from pure alexiastephane.chenardNo ratings yet
- The Hopkins Verbal Learning Test An in Depth Analysis of Recall PatternsDocument22 pagesThe Hopkins Verbal Learning Test An in Depth Analysis of Recall PatternsChrisNo ratings yet
- Journal of Neurolinguistics: ArticleinfoDocument17 pagesJournal of Neurolinguistics: ArticleinfoMarilyn BucahchanNo ratings yet
- Pwas and Pbjs Language For Describing A Simple ProcedureDocument8 pagesPwas and Pbjs Language For Describing A Simple Proceduremary engNo ratings yet
- Fulton 2013Document12 pagesFulton 2013Cecilia AgostNo ratings yet
- Rev. Valentina VargasDocument3 pagesRev. Valentina VargasGabriel Jesus Morales MoralesNo ratings yet
- Unit 1, Week 1Document10 pagesUnit 1, Week 1Gabriel Jesus Morales MoralesNo ratings yet
- (2011) Loss of Basic Lexical Knowledge in Old AgeDocument9 pages(2011) Loss of Basic Lexical Knowledge in Old AgeGabriel Jesus Morales MoralesNo ratings yet
- Zimmerman 1990Document16 pagesZimmerman 1990Gabriel Jesus Morales MoralesNo ratings yet
- Unit 2, Week 1Document12 pagesUnit 2, Week 1Gabriel Jesus Morales MoralesNo ratings yet
- Explore the Arts in English Workshop 2Document10 pagesExplore the Arts in English Workshop 2Gabriel Jesus Morales MoralesNo ratings yet
- Rev. Valentina VargasDocument3 pagesRev. Valentina VargasGabriel Jesus Morales MoralesNo ratings yet
- (2011) Longitudinal Detection of Dementia Through Lexical and Syntactic Changes in WritingDocument27 pages(2011) Longitudinal Detection of Dementia Through Lexical and Syntactic Changes in WritingGabriel Jesus Morales MoralesNo ratings yet
- (2010) Lexical, Semantic and Action Verbal Fluency in Parkinsons Disease With and Without DementiaDocument10 pages(2010) Lexical, Semantic and Action Verbal Fluency in Parkinsons Disease With and Without DementiaGabriel Jesus Morales MoralesNo ratings yet
- (1998) The Discourse of Self in DementiaDocument27 pages(1998) The Discourse of Self in DementiaGabriel Jesus Morales MoralesNo ratings yet
- (2008) Lexical and Articulatory Aspects of Speech Production in Cognitive DeclineDocument54 pages(2008) Lexical and Articulatory Aspects of Speech Production in Cognitive DeclineGabriel Jesus Morales MoralesNo ratings yet
- (2014) Teaching Minority Indigenous Language at UniversitiesDocument7 pages(2014) Teaching Minority Indigenous Language at UniversitiesGabriel Jesus Morales MoralesNo ratings yet
- (1998) Naming Problems in Dementia. Semantic or LexicalDocument19 pages(1998) Naming Problems in Dementia. Semantic or LexicalGabriel Jesus Morales MoralesNo ratings yet
- FAAPI2015Document256 pagesFAAPI2015Gabriel Jesus Morales MoralesNo ratings yet
- Using the Language to Learn: XXXIII FAAPI Conference ProceedingsDocument181 pagesUsing the Language to Learn: XXXIII FAAPI Conference ProceedingsGabriel Jesus Morales MoralesNo ratings yet
- FAAPI2007Document147 pagesFAAPI2007Gabriel Jesus Morales MoralesNo ratings yet
- Grammatical Gender in Adult L2 Acquisition: Relations Between Lexical and Syntactic VariabilityDocument25 pagesGrammatical Gender in Adult L2 Acquisition: Relations Between Lexical and Syntactic VariabilityDelfa OtrNo ratings yet
- Guidelines Parcial 1 PDFDocument4 pagesGuidelines Parcial 1 PDFGabriel Jesus Morales MoralesNo ratings yet
- Personal-Statement-Mind-Map HDocument1 pagePersonal-Statement-Mind-Map HAhmad UsmanNo ratings yet
- (2020) ASLA History and Perspective On Practices On SLA TheoriesDocument9 pages(2020) ASLA History and Perspective On Practices On SLA TheoriesGabriel Jesus Morales MoralesNo ratings yet
- (2009) Vanderplank. A Decade of Research On Language LabsDocument38 pages(2009) Vanderplank. A Decade of Research On Language LabsGabriel Jesus Morales MoralesNo ratings yet
- (2020) A Critical Study of The Principles and Approaches To Needs AnalysisDocument17 pages(2020) A Critical Study of The Principles and Approaches To Needs AnalysisGabriel Jesus Morales MoralesNo ratings yet
- Unit 1 Test GuidelinesDocument3 pagesUnit 1 Test GuidelinesGabriel Jesus Morales MoralesNo ratings yet
- English 4 AgendaDocument1 pageEnglish 4 AgendaGabriel Jesus Morales MoralesNo ratings yet
- PRESENT PERFECT TALENTS WORKSHOPDocument11 pagesPRESENT PERFECT TALENTS WORKSHOPGabriel Jesus Morales MoralesNo ratings yet
- Lesson 1 TM15 MandarinDocument10 pagesLesson 1 TM15 MandarinHérmesNo ratings yet
- D-1 Introduction of Induction TrainingDocument23 pagesD-1 Introduction of Induction TrainingMumtaz DahriNo ratings yet
- How CBT Effectively Treats DepressionDocument52 pagesHow CBT Effectively Treats DepressionUkhtSameehNo ratings yet
- Quality and Safety Using The Qsen CompetenciesDocument34 pagesQuality and Safety Using The Qsen Competenciesapi-356391957No ratings yet
- Contemporary Philippine Arts Regional ExamDocument5 pagesContemporary Philippine Arts Regional ExamShiella PimentelNo ratings yet
- Persons Behaviors and SituationsDocument7 pagesPersons Behaviors and SituationsRhoma siregarNo ratings yet
- Boysen Company X Led EomDocument1 pageBoysen Company X Led Eomapi-341737011No ratings yet
- FSIE ScrapbookDocument5 pagesFSIE ScrapbookRea Mae LeymaNo ratings yet
- 07 Types of Managers 2Document13 pages07 Types of Managers 2bum_24No ratings yet
- ECCE 2013 Upcoming ChangesDocument12 pagesECCE 2013 Upcoming ChangesΔήμητραΓουδέλαNo ratings yet
- Jacob Stewart ResumeDocument2 pagesJacob Stewart Resumeapi-250063152No ratings yet
- Five Minute Refresher EzineDocument7 pagesFive Minute Refresher EzineMichael KaplanNo ratings yet
- Scientific Pluralism, 2006 PDFDocument279 pagesScientific Pluralism, 2006 PDFzeeshanshhd100% (1)
- Play TherapyDocument2 pagesPlay TherapyravensuichiroNo ratings yet
- Lesson Plan Unit 4: He's A HeroDocument5 pagesLesson Plan Unit 4: He's A Heromanhtrang07100% (1)
- American EducationDocument62 pagesAmerican EducationN San100% (1)
- Lesson 3 - READ BETWEEN THE LINESDocument6 pagesLesson 3 - READ BETWEEN THE LINESQueenie CervantesNo ratings yet
- A.Trebits - Phrasal Verbs in EU English - SystemDocument13 pagesA.Trebits - Phrasal Verbs in EU English - SystemehsanNo ratings yet
- Asef Hussaini: Personal InformationDocument1 pageAsef Hussaini: Personal InformationNaqi MuttaqiNo ratings yet
- The Global Open University Nagaland Sem 1 Paper IT and Systems 1, eMBADocument1 pageThe Global Open University Nagaland Sem 1 Paper IT and Systems 1, eMBAleenamyidNo ratings yet
- Daily Lesson Plan Mathematics (DLP) Year 2Document3 pagesDaily Lesson Plan Mathematics (DLP) Year 2CHONG HUI WEN MoeNo ratings yet
- A Critical Review of The Effect of Teacher Preparedness On Students' Academic Achievement: A Research AgendaDocument9 pagesA Critical Review of The Effect of Teacher Preparedness On Students' Academic Achievement: A Research AgendaAnonymous CwJeBCAXpNo ratings yet
- Anglisht Skema B PDFDocument4 pagesAnglisht Skema B PDFJolaAlimemajNo ratings yet
- Module 3 Applied EconomicsDocument6 pagesModule 3 Applied EconomicsEarl GaliciaNo ratings yet
- Position Paper EappDocument3 pagesPosition Paper EappAshlea tabitha fae AngcoNo ratings yet
- The correct answers are:Q1: a. Down SyndromeQ2: c. poor visionDocument74 pagesThe correct answers are:Q1: a. Down SyndromeQ2: c. poor visionShai MacapillarNo ratings yet
- MFAT assessment results summaryDocument3 pagesMFAT assessment results summaryMARVY VILLAMOR100% (1)
- Module 1 L1 PhilosDocument23 pagesModule 1 L1 PhilosRainier CaindoyNo ratings yet
- Cognitive Code LearningDocument3 pagesCognitive Code LearningSharon Vijaya BalakrishnanNo ratings yet
- Education Measurment and Evaluation Unit: 1 Introduction The Concept of MeasurementDocument39 pagesEducation Measurment and Evaluation Unit: 1 Introduction The Concept of MeasurementSuleman ShahNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (20)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Secure Love: Create a Relationship That Lasts a LifetimeFrom EverandSecure Love: Create a Relationship That Lasts a LifetimeRating: 5 out of 5 stars5/5 (18)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (26)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)