Professional Documents
Culture Documents
Ob Topic 3 - Multiple Pregnancy - NCP
Uploaded by
Thelly MargalloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ob Topic 3 - Multiple Pregnancy - NCP
Uploaded by
Thelly MargalloCopyright:
Available Formats
Successful Delayed-Interval Delivery In Monochorionic Diamniotic Twin Pregnancy: A Case Report
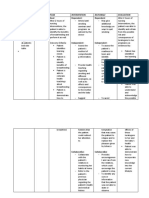
Assessment Nursing Rationale Planning Nursing Rationale Evaluation
Diagnosis Interventions
Objective data: Readiness for Readiness for Goal: Assess the patient This gives the After nurse-patient
• G2P1 enhanced enhanced • As many weeks and family’s level nurse information interaction, the
• Monochorionic, therapeutic therapeutic regimen AOG as the fetus of knowledge of as to what extent patient:
diamniotic regimen management refers and the patient can the treatment. do the patient and • Understands
pregnancy management to a pattern of sustain, the patient her family the whole
• Preterm related to regulating and will be able to understand the process of DID
premature delayed- integrating into daily deliver her fetus treatment. • Understands
rupture of interval living a program for safely and with less the importance
membranes at delivery treatment of illness complications. Explain and Making them of every
20 weeks AOG method and its sequelae Long-term objectives: supplement the understand the component of
• AFI satisfactory secondary to that is sufficient for • After days of nurse knowledge of the treatment more the treatment
• Close outpatient PPROM in meeting health- – patient patient and her promotes regimen
monitoring at 22 monochorionic related goals and interaction, the family regarding participation and • Proactively
weeks AOG diamniotic can be patient and her the treatment. adherence to the participates in
o On regular pregnancy strengthened. Since family will be able interventions. the treatment
fetal the occurrence of to demonstrate regimen
monitoring PPROM at 20 proactive Accept the This promotes • Is able to get
o On regular weeks AOG, the participation in: patient’s sense of self- rest periods and
serum patient has o Monitoring the evaluation of her esteem and relaxation while
inflammatory undergone several well-being of the strengths and confidence to on treatment
markers and measures to ensure mother and the weaknesses while continue efforts. It
rotating that the twins are baby working together also promotes
antibiotics well and safe o Adhering to the to improve her positivity which
• With threatened despite the early treatment and capabilities. contributes to
preterm labor at rupture of management in better outcomes
23 weeks and 2 membranes. Now preparation to of the treatment.
days AOG that she has already second delivery
• Delivered 555-g delivered her first Short-term objectives: Acknowledge the This provide
female infant by twin at 23 weeks, • Within 8 hours of patient and positive
spontaneous options have been the shift, the patient family’s efforts in reinforcement and
vaginal breech discussed with her and the family will participating in the encourages
delivery and her family and be able to: treatment. cooperation in the
they have decided treatment.
• Umbilical cord to go for DID for the o Verbalize Encourage the Rest periods and
was ligated high second twin in understanding of patient to get rest relaxation
in the vagina anticipation of DID method and and relaxation reserves the
• The family was improved and better its process while on patient’s energy
counselled outcomes. This o Verbalize treatment. and prevent any
regarding the indicates that the understanding of complications that
options for the family, especially importance of might disrupt the
second twin the patient, is ready every flow of the
Subjective data: and open for the component of treatment regimen
• The patient, with option of DID for her the treatment like infection.
the family, opted second twin. o Identify
for delayed- measures that Collaborate with This helps modify
interval delivery promote safety the health care and improve the
(DID) and improved team regarding treatment regimen
outcomes for the the patient and the for the well-being
treatment. fetus’ responses of the mother and
to the treatment. the fetus.
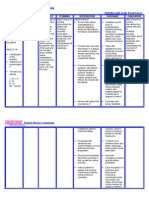
Administer These
medications as medications help
ordered. the mother and
the fetus sustain
the delay in the
interval of the
delivery of the
second twin.
Reference:
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2008). Nurses pocket guide: diagnoses, prioritized interventions, and rationales (11th ed.).
Philadelphia: F.A. Davis.
You might also like
- Patient's Profile:: Delivery Room Case 3 Labor & DeliveryDocument8 pagesPatient's Profile:: Delivery Room Case 3 Labor & DeliveryDanica Yen PagalNo ratings yet
- NCP Mod9Document3 pagesNCP Mod9Francis ChloeNo ratings yet
- Nursing Care Plan: Angeles University Foundation College of NursingDocument2 pagesNursing Care Plan: Angeles University Foundation College of NursingRey Ann PangilinanNo ratings yet
- Case Study PIHDocument26 pagesCase Study PIHChen OmbrosaNo ratings yet
- Readiness For Enhanced Nutrition: Subjective: Short Term: Independent: Short TermDocument4 pagesReadiness For Enhanced Nutrition: Subjective: Short Term: Independent: Short TermPrincess GarciaNo ratings yet
- NCP Def KnowwwwDocument11 pagesNCP Def KnowwwwCarey Jamille YadanNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care PlanAngeline MacarioNo ratings yet
- Subjective: Goal: Dependent: Dependent:: Assessment Diagnosis Plan Intervention Rationale EvaluationDocument2 pagesSubjective: Goal: Dependent: Dependent:: Assessment Diagnosis Plan Intervention Rationale EvaluationTrisha Cayabyab100% (1)
- Objective: Short Term Objectives: Diagnostic: Sto: Partially MET, TheDocument2 pagesObjective: Short Term Objectives: Diagnostic: Sto: Partially MET, TheWayne LoriaNo ratings yet
- Sample TCP - GraceGuitguitenDocument4 pagesSample TCP - GraceGuitguitenLauren JalandoniNo ratings yet
- NURSING CARE PLAN - Breast CancerDocument2 pagesNURSING CARE PLAN - Breast Cancerderic100% (3)
- Nursing-Care-Plan Case 1 LaquihonDocument2 pagesNursing-Care-Plan Case 1 LaquihonRuby Jane LaquihonNo ratings yet
- Assessment Nursing Diagnosis Outcome Identification Planning Nursing Intervention Evaluation IndependentDocument7 pagesAssessment Nursing Diagnosis Outcome Identification Planning Nursing Intervention Evaluation IndependentQueenie Silva100% (1)
- NCP CHNN Case PresDocument3 pagesNCP CHNN Case PresKhristine EstosoNo ratings yet
- Acute PainDocument4 pagesAcute PainRuffy AbdulazisNo ratings yet
- Family Nursing Process 1Document6 pagesFamily Nursing Process 1Khristine EstosoNo ratings yet
- DR-RLE-NCP-AND-DRUG-STUDY-Ambrosio 3Document6 pagesDR-RLE-NCP-AND-DRUG-STUDY-Ambrosio 3Ambrosio, Jasmin G.No ratings yet
- CHN Implementing Family Care PlanDocument2 pagesCHN Implementing Family Care PlanCharlie Abagon100% (1)
- NCPDocument3 pagesNCPeun kyung shinNo ratings yet
- NCP Cystic Fibrosis (Example)Document3 pagesNCP Cystic Fibrosis (Example)Lizet QuiamcoNo ratings yet
- Adherence Scientific Basis Nursing InterventionsDocument2 pagesAdherence Scientific Basis Nursing InterventionsKathleen AngNo ratings yet
- NCP Readiness UTI 1Document5 pagesNCP Readiness UTI 1Mary Grace AgataNo ratings yet
- DAVAO DOCTORS COLLEGE NURSING CARE PLAN FOR GDMDocument3 pagesDAVAO DOCTORS COLLEGE NURSING CARE PLAN FOR GDMkkd nyleNo ratings yet
- Balisi, Vener Vince D. Nursing Care PlanDocument2 pagesBalisi, Vener Vince D. Nursing Care PlanVince BalisiNo ratings yet
- Marjorie ncp8Document2 pagesMarjorie ncp8Jovel CortezNo ratings yet
- NCP Template 1Document6 pagesNCP Template 1SHIELOU LOMODNo ratings yet
- AP NCP by Garcia, p.-1Document4 pagesAP NCP by Garcia, p.-1Princess GarciaNo ratings yet
- Nursing Care Plan: Dizon, Patricia Ellyne T. Patient Apple 08 Female 04-20-2021Document3 pagesNursing Care Plan: Dizon, Patricia Ellyne T. Patient Apple 08 Female 04-20-2021Patricia Ellyne DizonNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planjonaa2564No ratings yet
- Prognosis and Discharge Plan - MaiaDocument12 pagesPrognosis and Discharge Plan - Maiajia88100% (1)
- Case Study 2Document2 pagesCase Study 2Gemina Leah MaeNo ratings yet
- Strat4 Tool 1 IDEAL CHKLST DischargeDocument7 pagesStrat4 Tool 1 IDEAL CHKLST DischargeNurbaitiNo ratings yet
- Discharge Plan: Patient'S Outcome Criteria Nursing OrderDocument2 pagesDischarge Plan: Patient'S Outcome Criteria Nursing OrdergaeLtorvzNo ratings yet
- Nutrition Knowledge GainDocument4 pagesNutrition Knowledge GainTrisha CayabyabNo ratings yet
- Prenatal Care NCPDocument10 pagesPrenatal Care NCPAlex AntipordaNo ratings yet
- Prenatal Care NCPDocument10 pagesPrenatal Care NCPAlex AntipordaNo ratings yet
- AssessmentDocument3 pagesAssessmentLOUISE JOSEL TACLAYNo ratings yet
- Nursing Care Plan for Smoking CessationDocument1 pageNursing Care Plan for Smoking CessationPatrick Renz TibayanNo ratings yet
- Prelim Reviewer 2023Document83 pagesPrelim Reviewer 2023jakexsanchez1515No ratings yet
- Nursing Care Plan for Alcohol Withdrawal AnxietyDocument5 pagesNursing Care Plan for Alcohol Withdrawal Anxietykuro hanabusaNo ratings yet
- After 2 Hours of Nursing Intervention, The Mother Will Verbalized The Understanding of The Condition, Process, and TreatmentDocument3 pagesAfter 2 Hours of Nursing Intervention, The Mother Will Verbalized The Understanding of The Condition, Process, and TreatmentJelly Yanquiling DumlaoNo ratings yet
- Trans NCM 207 MCNDocument41 pagesTrans NCM 207 MCNJianne CaloNo ratings yet
- NCP Disturbed Sleep Pattern and Hypothermia (Care of Older Adult Issues)Document4 pagesNCP Disturbed Sleep Pattern and Hypothermia (Care of Older Adult Issues)Jenny AjocNo ratings yet
- Shaina RDocument6 pagesShaina RSHAINAR KIM VILLACORTANo ratings yet
- ncp3-health-teachingDocument2 pagesncp3-health-teachingjardinanbalagsojoweeNo ratings yet
- NCPDocument1 pageNCPEve DelosoNo ratings yet
- Barangay Putik (Report)Document26 pagesBarangay Putik (Report)Shareen AbdusalamNo ratings yet
- 4 Phases of Health Care: RehabilitationDocument56 pages4 Phases of Health Care: RehabilitationmayangernszNo ratings yet
- BSN 3e Duropan Ncp-Knowledge DeficitDocument12 pagesBSN 3e Duropan Ncp-Knowledge DeficitJane DuropanNo ratings yet
- Introduction To MCN Prof. Dymphna Casquejo: Framework For Maternal and Child NursingDocument4 pagesIntroduction To MCN Prof. Dymphna Casquejo: Framework For Maternal and Child NursingLynnelljhyen MALUBAYNo ratings yet
- Iles S. Normal Pregnancy and Antenatal Care. Essential Obstetrics and Gynaecology. 6th Ed2020. P. 82-92.Document11 pagesIles S. Normal Pregnancy and Antenatal Care. Essential Obstetrics and Gynaecology. 6th Ed2020. P. 82-92.Alhafiz KarimNo ratings yet
- FNCP - MalnutritionDocument3 pagesFNCP - MalnutritionoctoberttwentythreeNo ratings yet
- Family Nursing Care PlanDocument5 pagesFamily Nursing Care PlanMarlchiel Nathan ArregladoNo ratings yet
- Maternal and Child Nursing Care FrameworkDocument34 pagesMaternal and Child Nursing Care FrameworkBSN 1GNo ratings yet
- Postpartum Care PlanDocument6 pagesPostpartum Care Planallie-jones-6489100% (27)
- Related Literary RiviewDocument6 pagesRelated Literary RiviewVal Gillian BranzuelaNo ratings yet
- Spray and Stretch TechDocument2 pagesSpray and Stretch TechrahulphysioNo ratings yet
- Textbook of Medical Physiology, 11th Edition: Guyton & HallDocument21 pagesTextbook of Medical Physiology, 11th Edition: Guyton & HallPatricia Denise Orquia100% (2)
- Newborn Calf ManagmentDocument17 pagesNewborn Calf ManagmentCarolyn ParsonsNo ratings yet
- (Current Clinical Psychiatry) Oliver Freudenreich - Psychotic Disorders - A Practical (2020) PDFDocument479 pages(Current Clinical Psychiatry) Oliver Freudenreich - Psychotic Disorders - A Practical (2020) PDFMatías Correa-Ramírez100% (7)
- Acute Rheumatic FeverDocument29 pagesAcute Rheumatic FeverFelix Wafula MusibiNo ratings yet
- Measuring pulse and oxygen with a pulse oximeterDocument2 pagesMeasuring pulse and oxygen with a pulse oximeterPedro TelloNo ratings yet
- TelemedicineDocument23 pagesTelemedicineNedhi Singh100% (2)
- Povidone Iodine Use in Hand Disinfectionskin Preparation and Antiseptic IrrigationDocument12 pagesPovidone Iodine Use in Hand Disinfectionskin Preparation and Antiseptic Irrigationpendekar bodohNo ratings yet
- The Common ColdDocument3 pagesThe Common ColdLalan ArdyanNo ratings yet
- Otitis Media: Prepared By: - Priyanka ThapaDocument38 pagesOtitis Media: Prepared By: - Priyanka ThapaKalo kajiNo ratings yet
- PHCL Midterms - Lesson 1 (Calculation of Doses General Consideration)Document4 pagesPHCL Midterms - Lesson 1 (Calculation of Doses General Consideration)Lazaro, Javen Andrie A.No ratings yet
- ADMINISTRATIVE SERVICES in HospitalDocument20 pagesADMINISTRATIVE SERVICES in HospitalSthitapragyan senapati100% (1)
- Finding the Right Pharmacy for Your NeedsDocument4 pagesFinding the Right Pharmacy for Your Needsprabakar VNo ratings yet
- Clonazepam Drug CardDocument1 pageClonazepam Drug CardSheri490No ratings yet
- Pox, Parvo, Adeno and Papova VirusesDocument33 pagesPox, Parvo, Adeno and Papova VirusesmicroperadeniyaNo ratings yet
- Chapter 1 - Papers PapersDocument14 pagesChapter 1 - Papers PapersJethro Floyd QuintoNo ratings yet
- Comparative Analysis of The Quantitative and Qualitative Method For Determination of D - DimerDocument4 pagesComparative Analysis of The Quantitative and Qualitative Method For Determination of D - DimerDimitar KosturkovNo ratings yet
- Clinicopathologic Conference: Tejada, Michael Leonelle A. Block 10Document14 pagesClinicopathologic Conference: Tejada, Michael Leonelle A. Block 10Michael TejadaNo ratings yet
- The Effectiveness of The Benevron BF Drug in The Treatment of Patients With Sensoneural StiffnessDocument6 pagesThe Effectiveness of The Benevron BF Drug in The Treatment of Patients With Sensoneural StiffnessCentral Asian StudiesNo ratings yet
- Refsum DiseaseDocument11 pagesRefsum DiseasechindyismailNo ratings yet
- Leap Level 1Document4 pagesLeap Level 1A Aziz Nizar DaudNo ratings yet
- Placenta PreviaDocument7 pagesPlacenta PreviaMarhina Asarabi MukimNo ratings yet
- History and Mental Status Exam GuideDocument17 pagesHistory and Mental Status Exam Guideyeney armenterosNo ratings yet
- Health Declaration Form: (Buong Pangalan) (Petsa) (Oras) (Kasa/ukuyang Tirahan) : (Numero NG Telepono)Document1 pageHealth Declaration Form: (Buong Pangalan) (Petsa) (Oras) (Kasa/ukuyang Tirahan) : (Numero NG Telepono)NICOSAT CollegesNo ratings yet
- CHARTINGDocument7 pagesCHARTINGGEN COLLANTESNo ratings yet
- The Effect of Music Therapy On Pain Level in Infusion in Children 6-12 Years of Age at Harapan Dan Doa HospitalDocument9 pagesThe Effect of Music Therapy On Pain Level in Infusion in Children 6-12 Years of Age at Harapan Dan Doa Hospitalratna purnamasariNo ratings yet
- Treatment of Pulmonary and Extra-Pulmonary Tuberculosis in AdultsDocument65 pagesTreatment of Pulmonary and Extra-Pulmonary Tuberculosis in AdultsLloyd Daniel BarrantesNo ratings yet
- Chapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and PerformanceDocument32 pagesChapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and Performanceec16043No ratings yet
- Health Problem Addressed: Umdns GMDNDocument1 pageHealth Problem Addressed: Umdns GMDNHaerul ImamNo ratings yet