Professional Documents
Culture Documents
COVID-19 Associated Cranial Nerve Neuropathy: A Systematic Review
COVID-19 Associated Cranial Nerve Neuropathy: A Systematic Review
Uploaded by
Demah AlAyadhiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COVID-19 Associated Cranial Nerve Neuropathy: A Systematic Review
COVID-19 Associated Cranial Nerve Neuropathy: A Systematic Review
Uploaded by
Demah AlAyadhiCopyright:
Available Formats
NEW AND EMERGING
BJBMS REVIEW ARTICLE MEDICAL ENTITIES
COVID-19 associated cranial nerve neuropathy:
A systematic review
Josef Finsterer¹*, Fulvio Alexandre Scorza², Carla Alexandra Scorza², Ana Claudia Fiorini³
ABSTRACT
The involvement of cranial nerves is being increasingly recognized in COVID-19. This review aims to summarize and discuss the recent advances
concerning the clinical presentation, pathophysiology, diagnosis, treatment, and outcomes of SARS-CoV-2 associated cranial nerve mononeu-
ropathies or polyneuropathies. Therefore, a systematic review of articles from PubMed and Google Scholar was conducted. Altogether 36
articles regarding SARS-CoV-2 associated neuropathy of cranial nerves describing 56 patients were retrieved as per the end of January 2021.
Out of these 56 patients, cranial nerves were compromised without the involvement of peripheral nerves in 32 of the patients, while Guillain-
Barre syndrome (GBS) with cranial nerve involvement was described in 24 patients. A single cranial nerve was involved either unilaterally or
bilaterally in 36 patients, while in 19 patients multiple cranial nerves were involved. Bilateral involvement was more prevalent in the GBS group
(n = 11) as compared to the cohort with isolated cranial nerve involvement (n = 5). Treatment of cranial nerve neuropathy included steroids (n
= 18), intravenous immunoglobulins (IVIG) (n = 18), acyclovir/valacyclovir (n = 3), and plasma exchange (n = 1). The outcome was classified as
“complete recovery” in 21 patients and as “partial recovery” in 30 patients. One patient had a lethal outcome. In conclusion, any cranial nerve
can be involved in COVID-19, but cranial nerves VII, VI, and III are the most frequently affected. The involvement of cranial nerves in COVID-
19 may or may not be associated with GBS. In patients with cranial nerve involvement, COVID-19 infections are usually mild. Isolated cranial
nerve palsy without GBS usually responds favorably to steroids. Cranial nerve involvement with GBS benefits from IVIG.
KEYWORDS: Cranial nerves; nerve conduction; neuropathy, SARS-CoV-2; COVID-19; Guillain Barre syndrome
INTRODUCTION of PNS involvement in the infection include neuropathy of
cranial nerves, neuropathy of peripheral nerves, Guillain
Since the outbreak of the SARS-CoV-2 pandemic in Barre syndrome (GBS) with all its subtypes (acute, inflam-
December 2019 increasing evidence accumulated that not matory demyelinating polyneuropathy, acute, motor, axonal
only the central nervous system (CNS) but also the peripheral neuropathy, acute, motor and sensory, axonal neuropathy,
nervous system (PNS) can be involved in this viral infection Miller-Fisher syndrome, pharyngo-cervico-brachial variant,
most frequently manifesting as lung disease (COVID-19) [1,2]. Bickerstaff encephalitis), myasthenia, myasthenic syndrome,
CNS involvement in COVID-19 includes viral meningitis, viral myositis, and rhabdomyolysis [2,3]. Involvement of cranial
encephalitis, immune encephalitis, limbic encephalitis, acute, nerves may occur as mono-neuropathy or polyneuritis cra-
hemorrhagic, necrotizing encephalitis, acute, disseminated nialis, unilaterally or bilaterally, together with or without the
encephalomyelitis, transverse myelitis, multiple sclerosis, involvement of peripheral nerves, and with or without CNS
cerebral vasculitis, ischemic stroke, sinus venous thrombosis, involvement. In the majority of cases with CNS/PNS involve-
cerebral vasoconstriction syndrome, intracerebral bleeding, ment, cerebrospinal fluid (CSF) investigations for SARS-
or non-aneurysmatic subarachnoid bleeding. Manifestations CoV-2 RNA are negative, suggesting that immunological reac-
tions are the most common pathophysiological mechanism
1
Clinic Landstrasse, Messerli Institute, Vienna, Austria behind CNS/PNS involvement in COVID-19. Figures about
²Department of Neuroscience, Federal University of São the frequency of CNS/PNS involvement in COVID-19 are
Paulo/Paulista School of Medicine
3
Department of Speech Therapy, Pontifical Catholic University of São hardly available. This review aims to summarize and discuss
Paulo, Paulista School of Medicine/Federal University of São Paulo, previous and recent advances in the clinical presentation,
São Paulo, Brazil
pathophysiology, diagnosis, treatment, and outcome of SARS-
*Corresponding author: Joseph Finsterer, Clinic Landstrasse,
Messerli Institute, Vienna, Austria. E-mail: fifigs1@yahoo.de CoV-2 associated neuropathies of cranial nerves.
DOI: https://doi.org/10.17305/bjbms.2021.6341
Submitted: 24 July 2021/Accepted: 05 August 2021/ MATERIALS AND METHODS
Published Online: 11 August 2021
Conflict of interest: The authors declare no conflicts of interest.
A literature review in the databases PubMed and Google
Funding: The author(s) received no specific funding for this work.
Scholar using the search terms “neuropathy,” “cranial nerves,”
©The Author(s) (2022). This work is licensed under a Creative
Commons Attribution 4.0 International License “optic nerve,” “olfactory nerve,” “oculomotor nerve,” “trochlear
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
nerve,” “trigeminal nerve,” “abducens nerve,” “facial nerve,” were bilaterally involved. Bilateral involvement was more
“acoustic nerve,” “vestibulo-cochlear nerve,” “glossopharyngeal prevalent in the GBS group as compared to the cohort with
nerve,” “vagal nerve,” “accessory nerve,” “hypoglossal nerve,” isolated cranial nerve involvement. Cerebral imaging was car-
and “nerves” together with “SARS-CoV-2,” “COVID-19,” and ried out in 38 patients and cranial nerve lesions were found in
“coronavirus” was conducted. In addition, reference lists 20 of them (Table 1). Cerebral lesions were found in only two
were checked for further articles meeting the search criteria. patients of whom one also had a cranial nerve lesion (Table 1).
Included were articles which met the search criteria, reported Cerebral imaging was normal in 17 patients (Table 1). Cranial
original data (cases, case series), and were available as full nerve I was involved in three patients (Table 2), but several
articles. Excluded were articles available only as an abstract, patients with anosmia were not included as the cause of anos-
proceedings, or review articles. Articles were also excluded mia remained elusive. Cranial nerve II was involved in seven
because of limited data or absence of original data. Only arti- patients, interestingly in none of the GBS group (Table 1).
cles in English were considered. Cranial nerve III was compromised in 15 patients (Table 2).
The trochlear nerve was involved in a single patient. The tri-
RESULTS geminal nerve was compromised in 6 patients. Cranial nerve
VI was involved in 17 patients (Table 2). The facial nerve was
Altogether 36 articles about SARS-CoV-2 associated compromised in 29 patients. Cranial nerve VIII was dam-
neuropathy of cranial nerves describing 56 patients were aged in two patients. Cranial nerves IX and X were injured
retrieved as per the end of January 2021 (Figure 1) [4-39]. In in five patients each. Involvement of cranial nerve XI has not
32 patients only cranial nerves without the involvement of been reported. The hypoglossal nerve was compromised in
peripheral nerves were affected (Table 1). In 24 patients GBS 4 patients (Table 2). Treatment of cranial nerve neuropathy
with involvement of cranial nerves were described (Table 1). was reported in 52 cases and included steroids (n = 18), intra-
Age, reported in 55 patients, ranged from 5 to 76 years venous immunoglobulins (IVIG) (n = 18), acyclovir/valacy-
(Table 1). Thirty-two patients were male and 23 were female clovir (n = 3, two in combination with steroids), and plasma
(Table 1). In one patient gender was not reported (Table 1). exchange (n = 1). Supportive measures were applied in four
There was female preponderance in the cohort with isolated patients. Ten patients did not receive any treatment (Table 1).
cranial nerve involvement and vice versa male preponder- Therapy was not reported in four patients. The outcome
ance in the GBS cohort (Table 1). In 36 patients, a single cra- was classified as “complete recovery” (complete resolution
nial nerve was involved in 19 patients multiple cranial nerves of cranial nerve impairment at the time of discharge or last
were affected. In a single patient, the nerve involved was not follow-up) in 21 patients and as “partial recovery” (incom-
specified (Table 1). In 15 patients one or more cranial nerves plete function of the compromised cranial nerve at the time
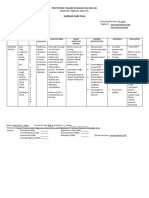
FIGURE 1. Flow chart detailing the search protocol and the results after application of inclusion and exclusion criteria.
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
TABLE 1. COVID-19 patients manifesting with involvement of a single or multiple cranial nerves
Age Sex SOC SCT ACN CSF Imaging STC OCNN Reference
Without GBS
41 F Mild NR I NR CNL None Anosmia [4]
27 F Mild NR II NR CNL Steroids PR [4]
25 F Mild NR VI, VII NR Pons lesion Steroids CR [4]
30 F Mild NR VII NR CNL Steroids CR [4]
33 M Mild NR VII bil NR CNL Steroids CR [4]
44 M Mild NR II bil Normal CNL Steroids CR [5]
24 F Mild CLQ, AZM III NR Not done None CR [6]
58 M Mild RDV, steroids V, VII, IX, X NR Normal Valacyclovir PR [7]
5 M NR NR VII bil, XII NR CNL NR NR [8]
32 F Mild AZM, steroids II, III Normal Not done Steroids CR [9]
43 F Mild NR VII NR Normal Steroids PR [10]
25 F Mild NR VII Normal Normal Steroids, ACV CR [10]
33 F Mild NR VII NR Not done Steroids, ACV PR [10]
26 F Mild NR VII Normal CNL Steroids CR [10]
50 F Mild NR VII Normal Normal Steroids PR [10]
38 F Mild NR VII Normal Normal Supportive CR [10]
39 F Mild NR VII Normal Normal Steroids CR [10]
34 M Mild NR VII Normal Normal Steroids CR [10]
69 M Severe TLM, MV V, VII, IX, X, XII NR Normal Rehabilitation PR [11]
15 M Mild NR II, NMO Normal CNL Steroids PR [12]
60 F Mild CLQ, LPV II NR Not done Steroids PR [13]
~45 F NR NR VIII NR NR NR NR [14]
35 F Mild Favipiravir VII Normal Not done Maoto CR [15]
~55 F Mild NONE II NR Normal None CR [16]
54 M Severe MV I NR Not done NR Death [17]
71 F Mild CLQ VI Normal CNL None PR [18]
20 M Mild NR VII bil Normal Not done Steroids PR [19]
43 F Mild NR VI NR Normal None NR [20]
52 M Mild NR VI NR Not done None CR [20]
NR NR Mild CLQ VI NR CNL None CR [21]
32 M Mild CLQ VI NR CNL None PR [22]
26 M Mild NR II bil 55/3 CNL, WML Steroids PR [23]
With GBS
65 M Mild NR VII bil, GBS DCA CNL IVIG PR [4]
9 M NR NR III, VI bil, VII, VIII, NR CNL NR NR [8]
GBS
36 M Mild NR III, VI bil, GBS NR CNL IVIG PR [18]
58 M Mild AZM, CTA VII bil, GBS DCA CNL IVIG PR [24]
~65 F mild NR VII bil, GBS DCA CNL IVIG PR [14]
72 M Severe CLQ, MV, TLM, oseltamivir, VII, GBS DCA Not done IVIG PR [25]
darunavir, steroid
49 F Mild CLQ, steroids, LPV, RTN III, V, VI, VII, GBS DCA Not done IVIG PR [25]
76 M Mild CLQ, TLM, oseltamivir, darunavir, VII, GBS DCA Not done IVIG PR [25]
steroid
36 M NR CLQ III, MFS NR CNL IVIG PR [21]
50 M Mild NR I, III, V, VII, MFS DCA Normal IVIG PR [26]
39 M Mild NR VI bil, MFS DCA Normal Acetaminophen CR [26]
61 M Mild CLQ. LPV, RTN VII bil, MFS NR Normal Steroids CR [27]
36 M Mild CLQ III, VI, MFS NR CNL IVIG PR [28]
51 F Mild NR VI, VII bil, GBS DCA Not done IVIG PR [29]
45 M Severe MV III, IV, VI, GBS Normal Normal IVIG PR [30]
55 M Mild NR MFS Normal Not done IVIG PR [31]
49 M Severe CLQ, RTV, LPV, MV VII, IX, X, XII, PCB DCA Normal None PR [32]
63 M Mild None III bil, VI bil, MFS DCA Normal None CR [33]
61 M Mild None III, VI, MFS DCA Not done IVIG CR [34]
21 M Mild NR VII bil, GBS NR CNL Plasma exch CR [35]
55 M Severe CLQ, LPV, RTN, MV III, V, IX, X, XII, GBS OCB Not done IVIG PR [36]
54 M Mild AZM, steroids, CLQ, MV III bil, VI bil, VII bil, GBS NR Not done IVIG PR [37]
50 M Severe MV III, IV, VI, IX, X, MFS DCA Normal IVIG PR [38]
50 F Mild CLQ, LPV, RTN III, V, MFS DCA Not done IVIG CR [39]
ACN: Cranial nerve involved; CAN: Acyclovir; AZM: Azithromycin; CLQ: Chloroquine; CNL: Cranial nerve lesion; CR: Complete recovery;
CSF: Cerebrospinal fluid abnormalities; CFTA: Ceftriaxone; DCA: Dissociation cyto-albuminique; GBS: Guillain-Barre syndrome; IVIG: Intravenous
immunoglobulins; LPV: Lopinavir; MFS: Miller Fisher syndrome; MV: Mechanical ventilation; NMO: Neuromyelitis optica; NR: Not reported;
OCB: Positive oligoclonal bands; OCNN: Outcome of cranial nerve neuropathy; PCB: Pharyngeal-cervical-brachial variant of Guillain Barré
syndrome; PR: Partial recovery; RDV: Remdesivir; RTN: Ritonavir; SCT: Specific treatment of COVID-19; SOC: Severity of the COVID-19 infection
(asymptomatic; mild; non-invasive ventilation; mechanical ventilation); STC: Specific treatment of cranial nerve neuropathy; TLM: Tocilizumab;
WML: White matter lesion
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
TABLE 2. Number of COVID-19 patients with isolated cranial frequently achieve partial recovery as compared to complete
nerve involvement and GBS with cranial nerve involvement for recovery.
each of the 12 cranial nerves
The pathophysiology of cranial nerve involvement remains
Cranial
Isolated Bilateral GBS Bilateral Total Bilateral elusive but it can be speculated that involvement of a cranial
nerve
I 2 0 1 0 3 0 nerve results from the uptake of the virus into the intracellu-
II 7 2 0 0 7 2 lar space of neurons at a distal location followed by retrograde
III 2 0 13 2 15 2
transport of the virus particles to the brain. An argument
IV 0 0 1 0 1 0
V 2 0 4 0 6 0
for this hypothesis is that in an autopsy study of 43 patients
VI 6 0 11 5 17 5 deceased from COVID-19 SARS-CoV-2 viral proteins were
VII 16 3 13 7 29 10 detected in cranial nerves originating from the lower brain-
VIII 1 0 1 0 2 0 stem and in isolated brainstem cells [40]. Furthermore, virus
IX 2 0 3 0 5 0
particles have been repeatedly found in neurons but also axons
X 2 0 3 0 5 0
XI 0 0 0 0 0 0 of cranial nerves in other autopsy studies [17]. Experimental
XII 2 0 2 0 4 0 studies indicate that SARS-CoV-2 indeed migrates retro-grad-
GBS: Guillain-Barre syndrome ually within axons of cranial nerves to the CNS [41].
Whether anosmia/hyposmia and ageusia/hypogeusia are
of discharge or last follow-up) in 30 patients. Only a single truly attributable to the involvement of cranial nerves I, VII,
patient died. In four patients, the outcome was not reported. IX, and X, respectively, in each case is unknown, since only
An illustrative case of cranial nerve involvement in a small portion of these patients undergoes investigations
COVID-19 was recently reported by Gogia et al. [7]. A 58-years- of cranial nerve involvement and since it is conceivable that
old male with mild COVID-19 developed left facial numbness, ageusia or anosmia results rather from the affection of appro-
left facial dribbling, and mild “dysphagia” 4 days after onset of priate receptors in mucous membranes than of the nerve.
the viral infection [7]. Clinical exam revealed hypoesthesia However, if the virus goes intercellularly, it is quite likely that
in the distribution of the left trigeminal nerve and left facial the cranial nerves most frequently involved in COVID-19 are
palsy but excluded involvement of cranial nerves IX and X [7]. cranial nerves I, VII, IX, and X, as the prevalence of hypos-
Cerebral MRI with contrast medium was non-informative. mia/anosmia and hypogeusia/ageusia is high in several stud-
The patient refused CSF investigations. Facial and trigeminal ies. Anyhow, as long as anosmia and hypogeusia are not con-
nerve impairment partially resolved under valacyclovir during firmed by MRI or other means, they may not be classified as
7 days (Table 1) [7]. involvement of appropriate cranial nerves. Involvement of
cranial nerves I should be diagnosed only if imaging demon-
DISCUSSION strates affection of the olfactory bulb or the fila olfactoria or
if autopsy demonstrates the virus within olfactory neurons. If
This review shows that involvement of cranial nerves retrograde migration of the virus along olfactory or gustatory
in the setting of COVID-19 infection is not rare and may pathways can be confirmed, the frequency of cranial nerves I,
be associated with GBS. Cranial nerves most frequently VII, IX, and X needs to be re-assessed.
involved are cranial nerves VII, VI, and III manifesting A second hypothesis explaining cranial nerve involve-
as hypogeusia/ageusia, facial palsy, or ophthalmoparesis. ment relies on the assumption that immunological reactions
COVID-19 in patients with associated cranial nerve involve- against the virus secondarily affect neuronal structures due to
ment is usually mild but in patients with severe COVID-19 epitope mimicry as in GBS. Arguments in favor of the radicu-
requiring mechanical ventilation, involvement of cranial litis hypothesis are that cranial nerve involvement frequently
nerves, and in particular GBS, may be missed. CSF investiga- occurs in patients with GBS and that patients with GBS and
tions are usually normal in COVID-19 patients with isolated cranial nerve involvement may present with DCA or pos-
involvement of cranial nerves but show dissociation cyto-al- itive OCB on CSF investigations. An argument against the
buminique (DCA) or positive oligoclonal bands (OCB) in radiculitis hypothesis, however, is that imaging studies hardly
patients with GBS and concomitant cranial nerve involve- revealed impairment of proximal portions of cranial nerves
ment (Table 1). The majority of cases with isolated cranial clinically involved in COVID-19. Interestingly, patients have
nerve involvement benefit from steroids, whereas GBS cases been reported in whom MRI revealed enhancement of cra-
with cranial nerve involvement benefit from IVIG. The nial nerves without corresponding clinical abnormalities [8].
outcome in isolated cases is usually fair with more patients Absence of cranial nerve II involvement in GBS patients
reaching complete recovery than partial recovery. On the could be explained by classification of the optic nerve as part
contrary, GBS patients with cranial nerve involvement more of the CNS and not as cranial nerve. Whether involvement
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
of the optic nerve in COVID-19 favours the development of delineation between cranial nerve involvement plus GBS or
demyelinating disease remains elusive but several cases with only cranial nerve involvement is not feasible.
SARS-CoV-2 associated optic neuritis have been reported
since the end of January 2021. Long-term evaluation of these CONCLUSION
patients is crucial to assess if SARS-CoV-2 triggers multiple
sclerosis or neuromyelitis optica. As soon as a cranial nerve This review shows that all cranial nerves can be involved
lesion becomes evident on a clinical exam in a patient with in COVID-19 but most frequently cranial nerves VII, VI,
COVID-19 cerebral imaging is mandatory. and III. Involvement of cranial nerves in COVID-19 may go
A third hypothesis explaining the involvement of cranial along with or without GBS. As per the end of January 2021,
nerves in COVID-19 relies on the assumption that drugs given 32 patients with isolated cranial nerve involvement and
to treat COVID-19 could exhibit neurotoxic side effects par- 24 patients with GBS and involvement of cranial nerves were
ticularly damaging cranial nerves. Drugs known to cause neu- reported. Cerebral imaging in patients with cranial nerve
ropathy and frequently given to COVID-19 patients include involvement is crucial as it may demonstrate a lesion not
daptomycin [42], linezolid [43], lopinavir [44], ritonavir [45], only in clinically affected but also clinically unaffected cranial
hydro-chloroquine [46], cisatracurium [47], clindamycin nerves. In patients with cranial nerve involvement COVID-19
[48], tocilizumab [49], and glucocorticoids [50]. An argument infections are usually mild. Isolated cranial nerve palsy with-
in favor of hypothesis three is that linezolid can cause optic out GBS usually responds favorably to steroids. GBS with cra-
and auditory nerve neuropathy [51, 52]. An argument against nial nerve involvement benefits from IVIG.
hypothesis three, however, is that COVID-19 in patients with
cranial nerve involvement is usually mild and does not require REFERENCES
aggressive treatment with any of the neurotoxic compounds.
To which degree tocilizumab contributed to the development [1] Cabañes-Martínez L, Villadóniga M, González-Rodríguez L,
Araque L, Díaz-Cid A, Ruz-Caracuel I, et al. Neuromuscular
of cranial nerve palsies in the three patients who received it involvement in COVID-19 critically ill patients. Clin Neurophysiol
[11,25], remains speculative. 2020;131(12):2809-16.
https://doi.org/10.1016/j.clinph.2020.09.017.
Treatment of cranial nerve involvement relies on the
[2] Paliwal VK, Garg RK, Gupta A, Tejan N. Neuromuscular presenta-
application of anti-COVID-19 drugs and more specifically tions in patients with COVID-19. Neurol Sci 2020;41(11):3039-56.
on the application of steroids, particularly in patients with https://doi.org/10.1007/s10072-020-04708-8.
[3] Maury A, Lyoubi A, Peiffer-Smadja N, de Broucker T, Meppiel E.
isolated cranial nerve involvement, of IVIG, particularly in Neurological manifestations associated with SARS-CoV-2 and
patients with GBS and cranial nerve involvement, and of other coronaviruses: A narrative review for clinicians. Rev Neurol
plasma exchange in single cases with GBS and cranial nerve (Paris) 2020;2002:30732-3.
https://doi.org/10.1016/j.neurol.2020.10.001.
involvement. In single cases virostatics, such as acyclovir or [4] Corrêa DG, da Cruz LC Jr., Lopes FC, Rangel CC, de Araújo
valacyclovir, were tried with limited effect. Recently, stimula- Henriques Tessarollo AL, Coelho KC, et al. Magnetic resonance
tion of cranial nerves was suggested to be used for therapeutic imaging features of COVID-19-related cranial nerve lesions.
J Neurovirol 2021;27(1):171-7.
purposes of COVID-19 [53]. In patients with severe COVID- https://doi.org/10.1007/s13365-020-00934-0.
19 under mechanical ventilation, transcutaneous, non-inva- [5] Sawalha K, Adeodokun S, Kamoga GR. COVID-19-induced acute
bilateral optic neuritis. J Investig Med High Impact Case Rep
sive vagal nerve stimulation has been shown to improve lung
2020;8:2324709620976018.
functions [53]. https://doi.org/10.1177/2324709620976018.
Limitations of the review were that detailed individual [6] Belghmaidi S, Nassih H, Boutgayout S, El Fakiri K, El Qadiry R,
Hajji I, et al. Third cranial nerve palsy presenting with unilateral dip-
data from several studies were not available. In a retrospective lopia and strabismus in a 24-year-old woman with COVID-19. Am
study of 50 COVID-19 patients, five patients with ophthal- J Case Rep. 2020;21:e925897.
moparesis and two patients with facial palsy were reported. https://doi.org/10.12659/ajcr.925897.
[7] Gogia B, Guevara AG, Rai PK, Fang X. A case of COVID-19 with
Unfortunately, no detailed individual data were provided multiple cranial neuropathies. Int J Neurosci2020;2020:1-3.
for these patients, why they were not included in the pres- [8] Lindan CE, Mankad K, Ram D, Kociolek LK, Silvera VM,
ent evaluation [54]. In a retrospective study of 841 COVID- Boddaert N, et al. Neuroimaging manifestations in children with
SARS-CoV-2 infection: A multinational, multicentre collaborative
19 patients, optic neuritis was reported in a single patient [55]. study. Lancet Child Adolesc Health 2020;2020:30362-X.
For this particular patient, no individual data were provided. [9] Raharimanantsoa OL, Razakarivony FA, Andriamiadanalisoa AO,
Rajaona RA, Rakotoarisoa R, Randrianarimanana SE, et al.
Lin et al. reported four patients with olfactory bulb abnormali-
Multinévrite oculaire dans le cadre d’une infection COVID-19
ties on MRI but did not present details required to be included Multiple infectious cranial nerve palsies in COVID-19. J Fr
in Table 1 [21]. The patient with anosmia and motor deficits Ophtalmol 2020;43(10):e351-3.
https://doi.org/10.1016/j.jfo.2020.08.001.
reported by Aragão et al. (patient-2) [56] was not included as [10] Lima MA, Silva MT, Soares CN, Coutinho R, Oliveira HS, Afonso L,
a work-up for GBS, respectively, neuropathy is missing and et al. Peripheral facial nerve palsy associated with COVID-19.
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
J Neurovirol 2020;26(6):941-4. Pedro-Murillo E, Bermejo-Guerrero L, Gordo-Mañas R, et al.
https://doi.org/10.1007/s13365-020-00912-6. Miller Fisher syndrome and polyneuritis cranialis in COVID-19.
[11] Cavalagli A, Peiti G, Conti C, Penati R, Vavassori F, Taveggia G. Neurology 2020;95(5):e601-5.
Cranial nerves impairment in post-acute oropharyngeal dys- https://doi.org/10.1212/wnl.0000000000009619.
phagia after COVID-19: A case report. Eur J Phys Rehabil Med [27] Caamaño DS, Beato RA. Facial diplegia, a possible atypical variant
2020;56(6):853-7. of Guillain-Barré syndrome as a rare neurological complication of
https://doi.org/10.23736/s1973-9087.20.06452-7. SARS-CoV-2. J Clin Neurosci 2020;77:230-2.
[12] de Ruijter NS, Kramer G, Gons RA, Hengstman GJ. Neuromyelitis https://doi.org/10.1016/j.jocn.2020.05.016.
optica spectrum disorder after presumed coronavirus (COVID-19) [28] Lantos JE, Strauss SB, Lin E. COVID-19-associated Miller Fisher syn-
infection: A case report. Mult Scler Relat Disord 2020;46:102474. drome: MRI findings. AJNR Am J Neuroradiol 2020;41(7):1184-6.
https://doi.org/10.1016/j.msard.2020.102474. https://doi.org/10.3174/ajnr.a6609.
[13] Benito-Pascual B, Gegúndez JA, Díaz-Valle D, Arriola-Villalobos P, [29] Reyes-Bueno JA, García-Trujillo L, Urbaneja P, Ciano-Petersen NL,
Carreño E, Culebras E, et al. Panuveitis and optic neuritis as a Postigo-Pozo MJ, Martínez-Tomás C, et al. Miller-Fisher syndrome
possible initial presentation of the novel coronavirus disease 2019 after SARS-CoV-2 infection Eur J Neurol 2020;27(9):1759-61.
(COVID-19). Ocul Immunol Inflamm 2020;28(6):922-5. https://doi.org/10.1111/ene.14383.
https://doi.org/10.1080/09273948.2020.1792512. [30] Lowery MM, Malik MT, Seemiller J, Tsai CS. Atypical variant of
[14] Klironomos S, Tzortzakakis A, Kits A, Öhberg C, Kollia E, Guillain Barre syndrome in a patient with COVID-19. J Crit Care
Ahoromazdae A, et al. Nervous system involvement in coronavirus Med (Targu Mures) 2020;6(4):231-6.
disease 2019: Results from a retrospective consecutive neuroimag- https://doi.org/10.2478/jccm-2020-0038.
ing cohort. Radiology 2020;297(3):E324-34. [31] Garnero M, Del Sette M, Assini A, Beronio A, Capello E, Cabona C,
https://doi.org/10.1148/radiol.2020202791. et al. COVID-19-related and not related Guillain-Barré syndromes
[15] Homma Y, Watanabe M, Inoue K, Moritaka T. Coronavirus dis- share the same management pitfalls during lock down: The experi-
ease-19 pneumonia with facial nerve palsy and olfactory distur- ence of Liguria region in Italy. J Neurol Sci 2020;418:117114.
bance. Intern Med 2020;59(14):1773-5. https://doi.org/10.1016/j.jns.2020.117114.
https://doi.org/10.2169/internalmedicine.5014-20. [32] Liberatore G, De Santis T, Doneddu PE, Gentile F, Albanese A,
[16] Selvaraj V, Sacchetti D, Finn A, Dapaah-Afriyie K. Acute vision loss Nobile-Orazio E. Clinical reasoning: A case of COVID-19-
in a patient with COVID-19. R I Med J (2013) 2020;103(6):37-8. associated pharyngeal-cervical-brachial variant of Guillain-Barré
https://doi.org/10.1101/2020.06.03.20112540. syndrome. Neurology 2020;95(21):978-83.
[17] Bulfamante G, Chiumello D, Canevini MP, Priori A, Mazzanti M, https://doi.org/10.1212/wnl.0000000000010817.
Centanni S, Felisati G. First ultrastructural autoptic findings of SARS [33] Ray A. Miller Fisher syndrome and COVID-19: Is there a link? BMJ
Cov-2 in olfactory pathways and brainstem. Minerva Anestesiol Case Rep 2020;13(8):e236419.
2020;86(6):678-9. https://doi.org/10.1136/bcr-2020-236419.
https://doi.org/10.23736/s0375-9393.20.14772-2. [34] Senel M, Abu-Rumeileh S, Michel D, Garibashvili T, Althaus K,
[18] Dinkin M, Gao V, Kahan J, Bobker S, Simonetto M, Wechsler P, et al. Kassubek J, et al. Miller-Fisher syndrome after COVID-19:
COVID-19 presenting with ophthalmoparesis from cranial nerve Neurochemical markers as an early sign of nervous system involve-
palsy. Neurology 2020;95(5):221-3. ment. Eur J Neurol 2020;27(11):2378-80.
https://doi.org/10.1212/wnl.0000000000009700. https://doi.org/10.1111/ene.14473.
[19] Muras AC, Carmona-Abellán MM, Fernández AC, Valiente JM, [35] Hutchins KL, Jansen JH, Comer AD, Scheer RV, Zahn GS,
Méndez LA, García-Moncó JC. Bilateral facial nerve palsy asso- Capps AE, et al. COVID-19-associated bifacial weakness with
ciated with COVID-19 and Epstein-Barr virus co-infection. Eur J paresthesia subtype of Guillain-Barré syndrome. AJNR Am J
Neurol 2021;28(1):358-60. Neuroradiol 2020;41(9):1707-11.
https://doi.org/10.1111/ene.14561. https://doi.org/10.3174/ajnr.a6654.
[20] Greer CE, Bhatt JM, Oliveira CA, Dinkin MJ. Isolated cranial nerve [36] Assini A, Benedetti L, Di Maio S, Schirinzi E, Del Sette M. New
6 palsy in 6 patients with COVID-19 infection. J Neuroophthalmol clinical manifestation of COVID-19 related Guillain-Barrè syn-
2020;40(4):520-2. drome highly responsive to intravenous immunoglobulins: Two
https://doi.org/10.1097/wno.0000000000001146. Italian cases. Neurol Sci 2020;41(7):1657-8.
[21] Lin E, Lantos JE, Strauss SB, Phillips CD, Campion TR Jr., Navi BB, https://doi.org/10.1007/s10072-020-04484-5.
et al. Brain imaging of patients with COVID-19: Findings at an aca- [37] Rana S, Lima AA, Chandra R, Valeriano J, Desai T, Freiberg W, et al.
demic institution during the height of the outbreak in New York Novel coronavirus (COVID-19)-associated Guillain-Barré syn-
city. AJNR Am J Neuroradiol 2020;41(11):2001-8. drome: Case report. J Clin Neuromuscul Dis 2020;21(4):240-2.
https://doi.org/10.3174/ajnr.a6793. https://doi.org/10.1097/cnd.0000000000000309.
[22] Falcone MM, Rong AJ, Salazar H, Redick DW, Falcone S, [38] Kajani S, Kajani R, Huang CW, Tran T, Liu AK. Miller Fisher syn-
Cavuoto KM. Acute abducens nerve palsy in a patient with the drome in the COVID-19 era a novel target antigen calls for novel
novel coronavirus disease (COVID-19). J AAPOS 2020;24(4):216-7. treatment. Cureus 2021;13(1):e12424.
https://doi.org/10.1016/j.jaapos.2020.06.001. https://doi.org/10.7759/cureus.12424.
[23] Zhou S, Jones-Lopez EC, Soneji DJ, Azevedo CJ, Patel VR. Myelin [39] Manganotti P, Pesavento V, Stella AB, Bonzi L, Campagnolo E,
oligodendrocyte glycoprotein antibody-associated optic neuritis Bellavita G, et al. Miller Fisher syndrome diagnosis and treatment
and myelitis in COVID-19. J Neuroophthalmol 2020;40(3):398-402. in a patient with SARS-CoV-2. J Neurovirol 2020;26(4):605-6.
https://doi.org/10.1097/wno.0000000000001049. https://doi.org/10.1007/s13365-020-00858-9.
[24] Chan JL, Ebadi H, Sarna JR. Guillain-Barré syndrome with facial [40] Matschke J, Lütgehetmann M, Hagel C, Sperhake JP, Schröder AS,
Diplegia related to SARS-CoV-2 infection. Can J Neurol Sci Edler C, et al. Neuropathology of patients with COVID-
2020;47(6):852-4. 19 in Germany: A post-mortem case series. Lancet Neurol
https://doi.org/10.1017/cjn.2020.106. 2020;19(11):919-29.
[25] Manganotti P, Bellavita G, D’Acunto L, Tommasini V, Fabris M, https://doi.org/10.1016/s1474-4422(20)30308-2.
Sartori A, et al. Clinical neurophysiology and cerebrospinal [41] Baig AM. Covert pathways to the cranial cavity: Could these be
liquor analysis to detect Guillain-Barré syndrome and polyneu- potential routes of SARS-CoV-2 to the brain? ACS Chem Neurosci
ritis cranialis in COVID-19 patients: A case series. J Med Virol 2020;11(20):3185-7.
2021;93(2):766-74. https://doi.org/10.1021/acschemneuro.0c00604.
https://doi.org/10.1002/jmv.26289. [42] Kushlaf HA. Emerging toxic neuropathies and myopathies. Neurol
[26] Gutiérrez-Ortiz C, Méndez-Guerrero A, Rodrigo-Rey S, San Clin 2011;29(3):679-87.
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
Josef Finsterer, et al.: SARS-CoV-2 associated cranial nerve neuropathy
https://doi.org/10.1016/j.ncl.2011.05.009. Mod Rheumatol 2009;19(2):199-203.
[43] Pilania RK, Arora A, Agarwal A, Jindal AK, Aggarwal K, Krishnan G, https://doi.org/10.3109/s10165-008-0132-2.
et al. Linezolid-induced mitochondrial toxicity presenting as retinal [50] Zorowitz RD. ICU-acquired weakness: A rehabilitation perspec-
nerve fiber layer microcysts and optic and peripheral neuropathy tive of diagnosis, treatment, and functional management. Brust
in a patient with chronic granulomatous disease. Retin Cases Brief 2016;150(4):966-71.
Rep 2021;15(3):224-9. [51] Xerri, O., Lemaire, B., Nasser, G., Rousseau-Huvey, B.,
https://doi.org/10.1097/icb.0000000000000777. Labetoulle, M., & Rousseau, A. (2015). Neuropathie optique toxique
[44] Khanlou H, Valdes-Sueiras M, Farthing C. Peripheral neuropathy grave liée au linézolide [Severe linezolid-induced toxic optic neu-
induced by Lopinavir-Saquinavir-ritonavir combination therapy in ropathy]. Journal francais d’ophtalmologie, 38(3), e55–e58.
an HIV-infected patient. J Int Assoc Physicians AIDS Care (Chic) https://doi.org/10.1016/j.jfo.2014.05.020
2007;6(3):155. [52] Brennan, K., Jones, B. L., & Jackson, L. (2009). Auditory
https://doi.org/10.1177/1545109707302756. nerve neuropathy in a neonate after linezolid treat-
[45] Lorber M. A case of possible darunavir/ritonavir-induced periph- ment. The Pediatric infectious disease journal, 28(2), 169.
eral neuropathy: Case description and review of the literature. J Int https://doi.org/10.1097/INF.0b013e31818fd8f5
Assoc Provid AIDS Care 2013;12(3):162-5.
[53] Bara GA, de Ridder D, Maciaczyk J. Can neuromodulation support
https://doi.org/10.1177/2325957412471993.
the fight against the COVID19 pandemic? Transcutaneous non-in-
[46] Becerra-Cuñat JL, Coll-Cantí J, Gelpí-Mantius E, Ferrer-Avellí X,
vasive vagal nerve stimulation as a potential targeted treatment of
Lozano-Sánchez M, Millán-Torné M, et al. Miopatía y neuropatía
fulminant acute respiratory distress syndrome. Med Hypotheses
inducida por cloroquina: tetraparesia progresiva con arreflexia
2020;143:110093.
que simula una polirradiculoneuropatía. A propósito de dos casos
Chloroquine-induced myopathy and neuropathy: Progressive tetra- https://doi.org/10.1016/j.mehy.2020.110093.
paresis with areflexia that simulates a polyradiculoneuropathy. Two [54] Pinna P, Grewal P, Hall JP, Tavarez T, Dafer RM, Garg R, et al.
case reports. Rev Neurol 2003;36(6):523-6. Neurological manifestations and COVID-19: Experiences from a
https://doi.org/10.33588/rn.3606.2002407. tertiary care center at the Frontline. J Neurol Sci 2020;415:116969.
[47] Fodale V, Praticò C, Girlanda P, Baradello A, Lucanto T, Rodolico C, https://doi.org/10.1016/j.jns.2020.116969.
et al. Acute motor axonal polyneuropathy after a cisatracurium [55] Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-
infusion and concomitant corticosteroid therapy. Br J Anaesth Larsen Á, Layos-Romero A, García-García J, et al. Neurologic
2004;92(2):289-93. manifestations in hospitalized patients with COVID-19: The
https://doi.org/10.1093/bja/aeh040. ALBACOVID registry. Neurology 2020;95(8):e1060-70.
[48] Thomas RJ. Neurotoxicity of antibacterial therapy. South Med J https://doi.org/10.1212/wnl.0000000000009937.
1994;87(9):869-74. [56] Aragão MF, Leal MC, Filho OQ, Fonseca TM, Valença MM.
[49] Sugiura F, Kojima T, Oguchi T, Urata S, Yuzawa Y, Sakakibara A, Anosmia in COVID-19 associated with injury to the olfactory bulbs
et al. A case of peripheral neuropathy and skin ulcer in a patient evident on MRI. AJNR Am J Neuroradiol 2020;41(9):1703-6.
with rheumatoid arthritis after a single infusion of tocilizumab. https://doi.org/10.3174/ajnr.a6675.
Related articles published in BJBMS
1. SARS-CoV-2 infection of the nervous system: A review of the literature on neurological involvement in novel coronavirus dis-
ease (COVID-19)
Alvin Oliver Payus et al., BJBMS, 2020
2. Sustained seroprevalence of SARS-CoV-2 antibodies one year after infection: one of the first COVID-19 cluster cases in
Bosnia and Herzegovina
Božo Šušak et al., BJBMS, 2020
Bosn J Basic Med Sci. 2022;22(1):39-45 www.bjbms.org
You might also like
- Agesta Sacred Codes ListDocument22 pagesAgesta Sacred Codes Listmimigogo92% (12)
- Diabetic Foot Ulcers Prevention & ManagementDocument59 pagesDiabetic Foot Ulcers Prevention & Managementcharity kalinowsky100% (2)
- Types of PainDocument1 pageTypes of PainTracy100% (3)
- Systemic Lupus Erythematosus Disease Activity Index SELENA ModificationDocument4 pagesSystemic Lupus Erythematosus Disease Activity Index SELENA ModificationaminahrahimiNo ratings yet
- Cervicogenic Headache1Document41 pagesCervicogenic Headache1Jeetendra Soni100% (1)
- Flox Report Rev 11Document253 pagesFlox Report Rev 11azpam100% (1)
- KatirjiDocument311 pagesKatirjiEjaz MasoodNo ratings yet
- An Update On The Neuropsychiatric Complications of COVID-19: PsychiatryDocument7 pagesAn Update On The Neuropsychiatric Complications of COVID-19: PsychiatryAdrian CantemirNo ratings yet
- GBS CovidDocument10 pagesGBS Covidcristina zarzanaNo ratings yet
- Journal of The Neurological Sciences: SciencedirectDocument12 pagesJournal of The Neurological Sciences: SciencedirectBotez MartaNo ratings yet
- 12 - Evidence of Central Nervous System Infection and Neuroinvasive Routes As WellDocument11 pages12 - Evidence of Central Nervous System Infection and Neuroinvasive Routes As WellVerónica GaticaNo ratings yet
- (2020-JAMA) - Neuropathogenesis and Neurologic Manifestations of The Coronaviruses in The Age of Coronavirus Disease 2019Document10 pages(2020-JAMA) - Neuropathogenesis and Neurologic Manifestations of The Coronaviruses in The Age of Coronavirus Disease 2019Iván PérezNo ratings yet
- Multiple Sclerosis and Related DisordersDocument5 pagesMultiple Sclerosis and Related DisordersDana DumitruNo ratings yet
- Ebiomedicine: Qi Cheng, Yue Yang, Jianqun GaoDocument6 pagesEbiomedicine: Qi Cheng, Yue Yang, Jianqun Gaowedib17801No ratings yet
- Guillain Barre Syndrome As A Complication of Covid 19 A Systematic ReviewDocument11 pagesGuillain Barre Syndrome As A Complication of Covid 19 A Systematic ReviewKARLOS ALVARO ACURIO ORTIZNo ratings yet
- Neuropathogenesis in COVID-19 - Journal of Neuropathology & Experimental Neurology OXFORDDocument3 pagesNeuropathogenesis in COVID-19 - Journal of Neuropathology & Experimental Neurology OXFORDMarcos AltableNo ratings yet
- Main - CópiaDocument7 pagesMain - CópiaMariana OliveiraNo ratings yet
- Update On The Neurology of COVID 19: LettertotheeditorDocument3 pagesUpdate On The Neurology of COVID 19: Lettertotheeditorgevowo3277No ratings yet
- How Covid 19Document3 pagesHow Covid 19EkaNo ratings yet
- MiscDocument8 pagesMiscTajul TajNo ratings yet
- Journal of The Neurological Sciences: Ali A. Asadi-Pooya, Leila Simani TDocument4 pagesJournal of The Neurological Sciences: Ali A. Asadi-Pooya, Leila Simani TAmandaNo ratings yet
- 1 s2.0 S0022510X20304226 Main PDFDocument18 pages1 s2.0 S0022510X20304226 Main PDFautomationenggNo ratings yet
- 17-Neurological Infections in 2020 COVID-1takes Centre StageDocument2 pages17-Neurological Infections in 2020 COVID-1takes Centre StageVerónica GaticaNo ratings yet
- COVID-19 Related Acute Hemorrhagic Necrotizing Encephalitis: A Report of Two Cases and Literature ReviewDocument8 pagesCOVID-19 Related Acute Hemorrhagic Necrotizing Encephalitis: A Report of Two Cases and Literature Reviewrifki irsyadNo ratings yet
- Basal Ganglia Involvement and AlteredDocument8 pagesBasal Ganglia Involvement and AlteredJonnathan Quintero (tatán)No ratings yet
- Articulo Secuelas Neurologicas COVID 19Document11 pagesArticulo Secuelas Neurologicas COVID 19carolina caroNo ratings yet
- Neuro-COVID Is Not at Variance Between Children and AdultsDocument3 pagesNeuro-COVID Is Not at Variance Between Children and AdultsMaurycy RakowskiNo ratings yet
- Guillain Barr ́e Syndrome and Its Variants As A Manifestation of COVID-19: A Systematic Review of Case Reports and Case SeriesDocument11 pagesGuillain Barr ́e Syndrome and Its Variants As A Manifestation of COVID-19: A Systematic Review of Case Reports and Case Seriesmikeb92556No ratings yet
- Neurocovid Pharmacological Recommendations For Delirium Associated With COVID-19Document12 pagesNeurocovid Pharmacological Recommendations For Delirium Associated With COVID-19Abdualaziz AlmalkiNo ratings yet
- Neurological Complications of COVID-19: Underlying Mechanisms and ManagementDocument21 pagesNeurological Complications of COVID-19: Underlying Mechanisms and ManagementAngelita Torres LlacsahuangaNo ratings yet
- PIIS0140673620312824Document1 pagePIIS0140673620312824Dino AdijayaNo ratings yet
- Covid-19 Vaccination Induced Encephalitis A ReviewDocument9 pagesCovid-19 Vaccination Induced Encephalitis A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Aghagoli2020 Article NeurologicalInvolvementInCOVIDDocument10 pagesAghagoli2020 Article NeurologicalInvolvementInCOVIDEduardo MazziniNo ratings yet
- Neurology and Covid 2Document20 pagesNeurology and Covid 2Novi SeptianiNo ratings yet
- Neurological Impact of Coronavirus Disease, Practical Considerations For The Neuroscience CommunityDocument33 pagesNeurological Impact of Coronavirus Disease, Practical Considerations For The Neuroscience CommunityArtur Cordeiro100% (1)
- 3 Manifestaciones 3Document7 pages3 Manifestaciones 3Nat LesNo ratings yet
- Neurologic Complications of COVID-19Document6 pagesNeurologic Complications of COVID-19Liliann RiveraNo ratings yet
- Neurological Manifestations in COVID-19: A Systematic Review and Meta-AnalysisDocument21 pagesNeurological Manifestations in COVID-19: A Systematic Review and Meta-AnalysisAlexandra PopNo ratings yet
- Nihms 1664293Document21 pagesNihms 1664293MARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Neurobiologia Del COVID19Document25 pagesNeurobiologia Del COVID19paola coralNo ratings yet
- A Comprehensive Review of Neurologic Manifestations of COVID-19 and Management of Pre-Existing Neurologic Disorders in ChildrenDocument7 pagesA Comprehensive Review of Neurologic Manifestations of COVID-19 and Management of Pre-Existing Neurologic Disorders in ChildrenNoviaNo ratings yet
- Variability of Symptoms in Neuralgic Amyotrophy Following Infection With Sars-Cov-2Document5 pagesVariability of Symptoms in Neuralgic Amyotrophy Following Infection With Sars-Cov-2Guido Alfonso Fierro PortoNo ratings yet
- PIIS2211034822003029Document7 pagesPIIS2211034822003029Johanna ValentinaNo ratings yet
- S0022510X21003014Document9 pagesS0022510X21003014shehabNo ratings yet
- Global Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19Document14 pagesGlobal Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19Tao ShenNo ratings yet
- As Sequelas Neuropsiquiátricas Crônicas de COVID-19 - Possíveis Impactos em Demências e DADocument10 pagesAs Sequelas Neuropsiquiátricas Crônicas de COVID-19 - Possíveis Impactos em Demências e DAAlberto HenriqueNo ratings yet
- Potential Neurologic Manifestations of COVID-19Document13 pagesPotential Neurologic Manifestations of COVID-19Raymond AriantoNo ratings yet
- Brain, Behavior, and Immunity: SciencedirectDocument5 pagesBrain, Behavior, and Immunity: SciencedirectJessica Malek da SilvaNo ratings yet
- Neurologic Manifestations in Hospitalized Patients With COVID-19 The ALBACOVID RegistrDocument26 pagesNeurologic Manifestations in Hospitalized Patients With COVID-19 The ALBACOVID RegistrsamuelNo ratings yet
- Neurological Manifestations of Sarscov2 A Proposed PathogenesisDocument6 pagesNeurological Manifestations of Sarscov2 A Proposed PathogenesisOmar Al-bazzaNo ratings yet
- Gillen Bare Sy PDFDocument6 pagesGillen Bare Sy PDFberinah65No ratings yet
- Complicaciones Neurologicas Covid en NiñosDocument11 pagesComplicaciones Neurologicas Covid en NiñosHéctor HerreraNo ratings yet
- Dementia and Long CovidDocument16 pagesDementia and Long CovidMaria SilvaNo ratings yet
- Neurological Cxs COVID PDFDocument19 pagesNeurological Cxs COVID PDFBirrie DeresseNo ratings yet
- Neurology TodayDocument3 pagesNeurology TodayBruno MosqueraNo ratings yet
- Fneur 13 988359Document12 pagesFneur 13 988359otakualafugaNo ratings yet
- 932 Full-2Document10 pages932 Full-2sara laadamiNo ratings yet
- Neurological Complications of COVID-19: Covid-19 in Intensive CareDocument3 pagesNeurological Complications of COVID-19: Covid-19 in Intensive CareQuốc BảoNo ratings yet
- Neurological Disorders in Patients Survivors of Covid-19Document6 pagesNeurological Disorders in Patients Survivors of Covid-19Central Asian StudiesNo ratings yet
- Subclinical Cognitive Impairment After Recovery of Mild Covid-19 23 Nov 2020Document9 pagesSubclinical Cognitive Impairment After Recovery of Mild Covid-19 23 Nov 2020yohanes suryonoNo ratings yet
- Paliwal2020 Article NeuromuscularPresentationsInPaDocument18 pagesPaliwal2020 Article NeuromuscularPresentationsInPaLina MalagonNo ratings yet
- Complicaciones Neurológicas de La COVID-19 Desde La Fisiopatología Hasta La Rehabilitación. Una Visión GeneralDocument17 pagesComplicaciones Neurológicas de La COVID-19 Desde La Fisiopatología Hasta La Rehabilitación. Una Visión GeneralB10. Oscar Alonso Díaz PintoNo ratings yet
- O7kdbu MainDocument5 pagesO7kdbu MainMariana OliveiraNo ratings yet
- Pediatric Neurology: Topical ReviewDocument17 pagesPediatric Neurology: Topical ReviewclaudyNo ratings yet
- The Altered Anatomical Distribution of ACE2 in The Brain With Alzheimer's Disease PathologyDocument8 pagesThe Altered Anatomical Distribution of ACE2 in The Brain With Alzheimer's Disease PathologyDeeksha20No ratings yet
- 1 s2.0 S2173580823000135 MainDocument6 pages1 s2.0 S2173580823000135 MainSusana MalleaNo ratings yet
- Clinical Neuroimmunology: Multiple Sclerosis and Related DisordersFrom EverandClinical Neuroimmunology: Multiple Sclerosis and Related DisordersNo ratings yet
- Asbury - Assesment of Current Diagnostic Criteria For GBSDocument4 pagesAsbury - Assesment of Current Diagnostic Criteria For GBSMarcelo BedoyaNo ratings yet
- Neuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeDocument8 pagesNeuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeNahu SteinmannNo ratings yet
- Neurological AssessmentDocument10 pagesNeurological AssessmentmatsumotoNo ratings yet
- Diabetic Autonomic NeuropathyDocument17 pagesDiabetic Autonomic NeuropathyRafael BohnenbergerNo ratings yet
- Top of The Foot Pain and Swelling TreatmentDocument13 pagesTop of The Foot Pain and Swelling TreatmentNyanLinKyawNo ratings yet
- Diabetic Foot CareDocument110 pagesDiabetic Foot CareEsi AfriyantiNo ratings yet
- JurnalDocument10 pagesJurnalZaoldyeck PutriNo ratings yet
- Fisioterapi LepraDocument13 pagesFisioterapi LepramuhammadasyamfawwazakbarNo ratings yet
- European Journal of Pain - 2017 - Arendt Nielsen - Assessment and Manifestation of Central Sensitisation Across DifferentDocument26 pagesEuropean Journal of Pain - 2017 - Arendt Nielsen - Assessment and Manifestation of Central Sensitisation Across DifferentLucas Mamud MeroniNo ratings yet
- Optic Atrophy :major Review March 2010, Kerala Journal of Ophthalmology, Devendra V. Venkatramani Et AlDocument6 pagesOptic Atrophy :major Review March 2010, Kerala Journal of Ophthalmology, Devendra V. Venkatramani Et AlNavojit ChowdhuryNo ratings yet
- Thieme E-Journals - Seminars in Neurology - Full TextDocument1 pageThieme E-Journals - Seminars in Neurology - Full TextLeandro SebastianNo ratings yet
- Vision Research: Stephanie K. Lynch, Michael D. AbràmoffDocument7 pagesVision Research: Stephanie K. Lynch, Michael D. Abràmoffanka_mihaelaNo ratings yet
- NCP PryllDocument6 pagesNCP PryllpjcolitaNo ratings yet
- Role of Jalauka in Diabetic Foot UlcerDocument12 pagesRole of Jalauka in Diabetic Foot UlcerMinakshi Gulshan SharmaNo ratings yet
- Lymphomyosot Aids Conventional Therapy in Diabetic Peripherial Neuropathy 2003Document8 pagesLymphomyosot Aids Conventional Therapy in Diabetic Peripherial Neuropathy 2003Dr. Nancy MalikNo ratings yet
- Vas & NprsDocument13 pagesVas & NprsDian Sulistya EkaputriNo ratings yet
- Approach To The Differential Diagnosis of Leg Ulcers - UpToDateDocument44 pagesApproach To The Differential Diagnosis of Leg Ulcers - UpToDatePriscillaNo ratings yet
- Baumann 2013Document184 pagesBaumann 2013sekar alifaNo ratings yet
- Polyneuritis Medical Appendix (Polyneuropathy, Multiple Neuritis, Multiple Symmetrical Peripheral Neuritis)Document4 pagesPolyneuritis Medical Appendix (Polyneuropathy, Multiple Neuritis, Multiple Symmetrical Peripheral Neuritis)Chideraa FloveraNo ratings yet
- Hydrotherapy With Massage On SerumNGFDocument43 pagesHydrotherapy With Massage On SerumNGFDr Vaishali MathapatiNo ratings yet
- Painless Diabetic Motor NeuropathyDocument12 pagesPainless Diabetic Motor NeuropathyHamza JubranNo ratings yet
- Referat GBSDocument12 pagesReferat GBSSoraya Dwi KhairunnisaNo ratings yet
- Neuromuscular DisordersDocument39 pagesNeuromuscular DisordersanibandasoNo ratings yet