Professional Documents
Culture Documents
Types and Features of Inflammation
Uploaded by
Andrew Bonus0 ratings0% found this document useful (0 votes)
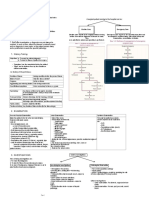
7 views2 pagesThis chapter discusses types of inflammation and features of chronic inflammation. It outlines the molecular and cellular events in acute inflammation, including vascular changes that cause increased permeability and blood flow, and leukocyte extravasation and phagocytosis. Systemic inflammatory response is also described, involving endocrine, metabolic and immune alterations mediated by cytokines. Chronic inflammation is characterized by mononuclear cell infiltration, macrophages and giant cells, tissue necrosis, and fibrosis. It can be nonspecific or chronic specific inflammation where the causative agent forms characteristic granulomas.
Original Description:
Types of inflammation, Acute, Chronic, Treatments
Original Title
2. Inflammation
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis chapter discusses types of inflammation and features of chronic inflammation. It outlines the molecular and cellular events in acute inflammation, including vascular changes that cause increased permeability and blood flow, and leukocyte extravasation and phagocytosis. Systemic inflammatory response is also described, involving endocrine, metabolic and immune alterations mediated by cytokines. Chronic inflammation is characterized by mononuclear cell infiltration, macrophages and giant cells, tissue necrosis, and fibrosis. It can be nonspecific or chronic specific inflammation where the causative agent forms characteristic granulomas.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views2 pagesTypes and Features of Inflammation
Uploaded by
Andrew BonusThis chapter discusses types of inflammation and features of chronic inflammation. It outlines the molecular and cellular events in acute inflammation, including vascular changes that cause increased permeability and blood flow, and leukocyte extravasation and phagocytosis. Systemic inflammatory response is also described, involving endocrine, metabolic and immune alterations mediated by cytokines. Chronic inflammation is characterized by mononuclear cell infiltration, macrophages and giant cells, tissue necrosis, and fibrosis. It can be nonspecific or chronic specific inflammation where the causative agent forms characteristic granulomas.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Chapter 2
(1) Discuss types of inflammation.
(2) Outline molecular and cellular events in inflammation.
(3) Discuss systemic inflammatory response.
(4) Discuss pathological types and features of chronic inflammation.
(1) Acute Inflammation
a. Short duration. Repair with early body reaction.
Chronic Inflammation
a. Longer duration, over 6 months. Either caused by agent or the stimulus.
Signs of inflammation
1. Redness Rubor
2. Heat Calor
3. Swelling Tumor
4. Pain Dolor
5. Loss of Function (Functio laesa)
(2) Acute Inflammation
I. Vascular Events
b. Increased vascular permeability:
a. Changes in vascular flow and caliber
During inflammation, endothelium lining of microvasculature
• Transient vasoconstriction for a few seconds.
becomes more leaky resulting in escape of protein
• Progressive vasodilatation involving mainly arterioles.
rich fluid into the interstitial compartment and this
Increase blood flow heat and redness.
fluid is known as exudate.
• Progressive vasodilatation hydrostatic pressure transudation.
• Next occurs slowing or stasis of microcirculation. Increased hydrostatic pressure increased vascular permeability edema
(transudation) (exudation).
Lewis’s triple response
- The flush appears immediately following stroking as
a dull red line and is due to capillary dilatation.
- The flare is a bright red irregular surrounding
due to arteriolar dilatation.
- The wheal is a swelling or edema of surrounding
skin occurring due to transudation of fluid into
extravascular space.
II. Cellular Events
a. Leukocyte extravasation b. Phagocytosis
a. Leukocyte extravasation b. Phagocytosis
escape
Leukocytes the interstitial tissue Inflammation It is the process by which polymorphs and macrophages ingest
(from the lumen of microvasculature) microorganisms and other foreign particles.
Steps of leukocyte extravasation include: It is similar to feeding process of amoeba and involves
following steps:
- Stasis of blood and changes in axial flow of blood. - Recognition and attachment.
- Margination of leukocytes and pavementing. - Engulfment.
- Rolling and adhesion to endothelium. - Killing and degradation.
- Emigration through inter-endothelial gaps by ameboid movements into
extravascular space.
- Red cells also escape by passive movements (Diapedesis).
- Chemotaxis: It is movement of leukocytes towards the site of injury and is
defined as locomotion oriented along a chemical gradient.
(3) SYSTEMIC INFLAMMATORY RESPONSE
Involves neuroendocrine, immunological and metabolic alterations.
Endocrine Response Metabolic Response Immune Response
There is increased release of i. There is increased lipolysis resulting in elevated i.Innate Response ii. Acquired Response
hormones namely: ACTH, levels of plasma fatty acids and glycerol.
cortisol, growth hormone, epinephrine, ii. There is increased nitrogen excretion leading to Occurs early and is Occurs later after antigen processing
norepinephrine,glucagon, renin rise in blood urea levels. not antigen specific. It and clonal expansion of T- and B-cells.
and aldosterone. iii. There is increased production and decreased depends on It is antigen specific.
utilization of glucose by tissues leading to functioning of natural
hyperglycemia. killer (NK) cells.
During innate response to injury, mediators release Cytokines.(small proteins or lipids)
Cytokines appear very rapidly after injury, influence by proinflammatory or anti-
inflammatory response.
systemic inflammatory response syndrome(SIRS)- fever, tachycardia,
leukocytosis(by Cytokines)
Pre-existing cytokine production multiple organ failure (MOF) and mortality.
General Surgery Page 1
Various cytokines related to inflammatory response are: Tumor Necrosis Factor-alpha (TNF-α) (most potent mediator of inflammation)
Interleukin-1 (IL-1) (extremely potent mediator of inflammation)
IL-6, IL-8, IL-11 (other proinflammatory cytokines)
IL-4, IL-10 and IL-13 ( anti-inflammatory cytokines produced by T-helper cells )
Interferon-γ (IFN-γ ) ( central role in innate immune response to microbial invasion)
Inducible Nitric Oxide Synthase (NOS-2) and Cyclooxygenase-2 (COX-2)
(4) I. Pathological Features of Chronic Inflammation
- Infiltration by mononuclear cells.
- Presence of tissue macrophages, epithelioid cells (modified macrophages) and multinucleated giant cells.
- Tissue necrosis, e.g. central caseation necrosis in tuberculosis.
- Proliferation of granulation tissue comprising blood vessels and fibroblasts.
- Collagen formation and healing by fibrosis.
II. Types of Chronic Inflammation Chronic Specific Inflammation
Chronic Nonspecific Inflammation
When the causative agent leads to characteristic
When irritant substance produces nonspecific inflammation histological tissue response like ‘granuloma formation’.
with formation of granulation tissue and healing It is also called as chronic granulomatous inflammation.
by fibrosis, e.g. chronic osteomyelitis. The granuloma is a circumscribed tiny lesion about 1 mm
in diameter. It consists of epithelioid cells, lymphoid cells and giant cells
along with necrosis and fibrosis. Examples are: tuberculosis, leprosy,
syphilis, actinomycosis. (Details in Chapter 4, Specific
infections).
General Surgery Page 2
You might also like
- Inflammation: Causes, Types and MediatorsDocument81 pagesInflammation: Causes, Types and Mediatorssaloni singhNo ratings yet
- Session 08 Acute InflammationDocument40 pagesSession 08 Acute Inflammationkasper mkNo ratings yet
- Pathology ReviewDocument26 pagesPathology ReviewSafiya James100% (1)
- Acute InflammationDocument47 pagesAcute InflammationAjit Metake-DeshmukhNo ratings yet
- Inflammation and Repair-2021Document93 pagesInflammation and Repair-2021Manav VyasNo ratings yet
- 2.acute & Chronic Inflammation, S1Document90 pages2.acute & Chronic Inflammation, S1LennyOctaviaNo ratings yet
- Inflammation: Presenter: Priyanka Shah Junior Resident Department of Pedodontics and Preventive DentistryDocument73 pagesInflammation: Presenter: Priyanka Shah Junior Resident Department of Pedodontics and Preventive DentistryBibek RajNo ratings yet
- Acute InflammationDocument76 pagesAcute InflammationOmor faruk HridoyNo ratings yet
- Acute Inflammation: A Guide to the Protective ResponseDocument82 pagesAcute Inflammation: A Guide to the Protective ResponseBhanu PraseedhaNo ratings yet
- 01.inflammation 1Document30 pages01.inflammation 1Shameena KnNo ratings yet
- Acute InflammationDocument55 pagesAcute InflammationMohammad_Islam8790% (10)
- SHS 301 Lect-05Document44 pagesSHS 301 Lect-05AAZEEN ALINo ratings yet
- Patologi AnatomiDocument26 pagesPatologi AnatomiNia AnestyaNo ratings yet
- InflammationDocument8 pagesInflammationGhazi Uddin AhmedNo ratings yet
- Harsh Mohan Quick Review InflammationDocument23 pagesHarsh Mohan Quick Review InflammationTanaya PujareNo ratings yet
- Inflammation overviewDocument10 pagesInflammation overviewYaff DthNo ratings yet
- Inflammation and RepairDocument5 pagesInflammation and RepairDENILLE AIRA NOGOYNo ratings yet
- INFLAMAATIONDocument6 pagesINFLAMAATIONSabbir AhmedNo ratings yet
- Inflammation Seminar OverviewDocument19 pagesInflammation Seminar OverviewDrGurinder Kanwar100% (1)
- Chapter 2 - Acute and Chronic InflammationDocument12 pagesChapter 2 - Acute and Chronic InflammationAgnieszka WisniewskaNo ratings yet
- A Inflammation For NursingDocument47 pagesA Inflammation For NursingSintayehu MulatuNo ratings yet
- Basic mechanisms of inflammation and repairDocument23 pagesBasic mechanisms of inflammation and repairdhanashriNo ratings yet
- Lecture 3Document56 pagesLecture 3w2tz2qrqxdNo ratings yet
- Inflammation and Healing: Inflammation "Local Response of Living Mammalian Tissues To Injury Due To Any Agent"Document121 pagesInflammation and Healing: Inflammation "Local Response of Living Mammalian Tissues To Injury Due To Any Agent"Bharath GowdaNo ratings yet
- Inflammation and Tissue Repair: July 2021Document54 pagesInflammation and Tissue Repair: July 2021EdenNo ratings yet
- Inflammation PDFDocument70 pagesInflammation PDFinamNo ratings yet
- Inflammation and Wound Healing Guide: Causes, Signs, Types, and StagesDocument46 pagesInflammation and Wound Healing Guide: Causes, Signs, Types, and StagesVijetha RaiNo ratings yet
- Acute vs Chronic Inflammation: Causes, Types & ProcessesDocument12 pagesAcute vs Chronic Inflammation: Causes, Types & Processeskarthikeyan rajeevNo ratings yet
- 2 - PATHOLOGY - Inflammation and Repair LectureDocument66 pages2 - PATHOLOGY - Inflammation and Repair Lectureregeti bhargavNo ratings yet
- 07 InflammationDocument69 pages07 InflammationSangameswaran B.BNo ratings yet
- InflammationDocument93 pagesInflammationbekaluNo ratings yet
- GPHT1 InflammationDocument5 pagesGPHT1 InflammationRachel ManaloNo ratings yet
- InflammationDocument26 pagesInflammationjoppaNo ratings yet
- Group No 3Document19 pagesGroup No 3محمد نعیم اقبالNo ratings yet
- inflammation and tissue repairDocument55 pagesinflammation and tissue repairSingitan SiyoumNo ratings yet
- Handouts - 6BIOM002W.2 - Inflammation 2018-9 PDFDocument66 pagesHandouts - 6BIOM002W.2 - Inflammation 2018-9 PDFFatima HusseinNo ratings yet
- Inflammation & Immune ResponseDocument68 pagesInflammation & Immune ResponseAgata Krisensia Putri100% (1)
- Inflammation & Immune ResponseDocument68 pagesInflammation & Immune Responsesuday sunday100% (1)
- Acute and Chronic InflammationDocument69 pagesAcute and Chronic InflammationJac mswimaNo ratings yet
- InflammationDocument48 pagesInflammationTewodros TeshomeNo ratings yet
- Inflamation: Drh. M. Arfan Lesmana, M.Sc. Fakultas Kedokteran Hewan, Universitas Brawijaya EmailDocument55 pagesInflamation: Drh. M. Arfan Lesmana, M.Sc. Fakultas Kedokteran Hewan, Universitas Brawijaya EmailalrezaNo ratings yet
- Patogenesis Infeksi Bakteri, Infeksi Lokal, Dan SepsisDocument52 pagesPatogenesis Infeksi Bakteri, Infeksi Lokal, Dan SepsisNia AnestyaNo ratings yet
- 1 Acute InflammationDocument6 pages1 Acute InflammationNauzaina IjazNo ratings yet
- Inflammation and Repair OverviewDocument10 pagesInflammation and Repair OverviewMiguel Cuevas DolotNo ratings yet
- II Inflam-PatoDocument27 pagesII Inflam-Patozenitha firdausNo ratings yet
- 2.4 2.5 Radang Akut Kronik Dan MorfologiDocument51 pages2.4 2.5 Radang Akut Kronik Dan MorfologimeNo ratings yet
- Immunology of Inflammation - SlidesDocument22 pagesImmunology of Inflammation - SlidesEssington BeloNo ratings yet
- InflammationDocument17 pagesInflammationNajwa AbdualgaderNo ratings yet
- Inflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDocument26 pagesInflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDavid Cahyo WibisonoNo ratings yet
- Mechanism of Inflammation (DRG Hesti) PPTDocument27 pagesMechanism of Inflammation (DRG Hesti) PPTTifani Cita DewiNo ratings yet
- Pathology 2 PDFDocument18 pagesPathology 2 PDFfadoNo ratings yet
- Inflammation's Link to Genetic DiseasesDocument23 pagesInflammation's Link to Genetic DiseasesSaraNo ratings yet
- INFLAMMATION & HEALING: THE CARDINAL SIGNSDocument93 pagesINFLAMMATION & HEALING: THE CARDINAL SIGNS숭숩No ratings yet
- Dr. Manella Joseph Senior Lecturer/Consultant PathologistDocument41 pagesDr. Manella Joseph Senior Lecturer/Consultant PathologistNipun Shamika100% (1)
- Histopathology - c3 - Acute and Chronic Inflammation - MasterDocument28 pagesHistopathology - c3 - Acute and Chronic Inflammation - MasterGhinescu AdrianNo ratings yet
- Chronic Inflammation and HemodynamicsDocument7 pagesChronic Inflammation and HemodynamicsKaty RosNo ratings yet
- WaaazzzzzzDocument21 pagesWaaazzzzzzSydjad Karl Ursal MiraflorNo ratings yet
- Physiology: Anatomy LectureDocument4 pagesPhysiology: Anatomy Lecturewesrdftyghuijkol wasedrftgyhuijkolNo ratings yet
- Chapter 10 Care of The Acutely InjuredDocument3 pagesChapter 10 Care of The Acutely InjuredAndrew BonusNo ratings yet
- Chapter 8 HemorrhageDocument4 pagesChapter 8 HemorrhageAndrew BonusNo ratings yet
- Chapter 7 Surgical Asepsis and Antiseptic MeasuresDocument2 pagesChapter 7 Surgical Asepsis and Antiseptic MeasuresAndrew BonusNo ratings yet
- Chapter 6 WoundsDocument3 pagesChapter 6 WoundsAndrew BonusNo ratings yet
- InfectionDocument3 pagesInfectionAndrew BonusNo ratings yet
- Sinus and FistulaDocument3 pagesSinus and FistulaAndrew BonusNo ratings yet
- General Surgery IntroductionDocument1 pageGeneral Surgery IntroductionAndrew BonusNo ratings yet
- Infectious Diseases and TreatmentsDocument5 pagesInfectious Diseases and TreatmentsAndrew BonusNo ratings yet
- Pyoderma Gangrenosum - A Guide To Diagnosis and Management: Authors: Christina GeorgeDocument5 pagesPyoderma Gangrenosum - A Guide To Diagnosis and Management: Authors: Christina GeorgeTasyaIndrianiRcisNo ratings yet
- 2 CELL INJURY AND CELL DEATH Reviewer 2Document4 pages2 CELL INJURY AND CELL DEATH Reviewer 2manuelNo ratings yet
- A Drug Study On Evening Primrose OilDocument5 pagesA Drug Study On Evening Primrose OilAlexis Khalyl Y. MontejoNo ratings yet
- CD RationalizationDocument19 pagesCD RationalizationAnastasya Gishella RorongNo ratings yet
- BIOREGULATORY MEDICINE 19 March 2022 Low MemDocument115 pagesBIOREGULATORY MEDICINE 19 March 2022 Low Memantudwo33No ratings yet
- 6 A-Hot ToothDocument14 pages6 A-Hot ToothYadnesh DondulkarNo ratings yet
- Ccid 8 239Document10 pagesCcid 8 239Marfatul ArifahNo ratings yet
- DR Sarah Ballantyne Immune Health Ebook PDFDocument36 pagesDR Sarah Ballantyne Immune Health Ebook PDFMay IshiiNo ratings yet
- TOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Document25 pagesTOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Waiwit KritayakiranaNo ratings yet
- Eva-Detko 4-Week ProgramDocument25 pagesEva-Detko 4-Week ProgramVeronika Solntseva100% (3)
- Nanocolloids For Nanomedicine and Drug DeliveryDocument274 pagesNanocolloids For Nanomedicine and Drug Deliveryenock-readersNo ratings yet
- How To Manage Coagulopathies in Critically Ill Patients: ReviewDocument18 pagesHow To Manage Coagulopathies in Critically Ill Patients: ReviewDaniel Balderas Anzures100% (2)
- Tocilizumab (Actemra)Document17 pagesTocilizumab (Actemra)dr. FAPNo ratings yet
- Asthma Concept MapDocument7 pagesAsthma Concept Mapshehada bondad100% (2)
- Evaluation of H 2 - Receptor Antagonists - Cimetidine, Ranitidine and Famotidine in An In-Vivo Gingivitis Model A.G. Snider, J.P. Ebel, H.M. Pickrum, R.E. SingerDocument2 pagesEvaluation of H 2 - Receptor Antagonists - Cimetidine, Ranitidine and Famotidine in An In-Vivo Gingivitis Model A.G. Snider, J.P. Ebel, H.M. Pickrum, R.E. Singer2288RNo ratings yet
- Patho QuestDocument4 pagesPatho QuestRosel Ann BontiaNo ratings yet
- Pancreatitis: (Alterations in Metabolic and Endocrine Functions)Document7 pagesPancreatitis: (Alterations in Metabolic and Endocrine Functions)Jorie Roco0% (1)
- Hijama Cupping PDFDocument16 pagesHijama Cupping PDFMuhammad Khalid JavedNo ratings yet
- Study Guide To The Six Tissue States PDFDocument34 pagesStudy Guide To The Six Tissue States PDFNick Max100% (6)
- Anemia in Renal DiseaseDocument59 pagesAnemia in Renal DiseaseShephali SharmaNo ratings yet
- زياد ٤Document43 pagesزياد ٤Ibrahim RamizNo ratings yet
- 1340 FullDocument9 pages1340 FullAkma RahaNo ratings yet
- Metformina y Estrés Oxidativo en Pacientes DiabéticosDocument14 pagesMetformina y Estrés Oxidativo en Pacientes DiabéticosJesus D. Hernandez GuitianNo ratings yet
- Basic Principles of Wound Healing - UpToDateDocument8 pagesBasic Principles of Wound Healing - UpToDateNguyễn TrangtrangNo ratings yet
- 1921 7826 3 PBDocument9 pages1921 7826 3 PBLeilybadryaNo ratings yet
- Chemical Composition and Anti-Arthritic Activity of Anacyclus Valentinus Extract On Adjuvant-Induced Arthritis in RatsDocument8 pagesChemical Composition and Anti-Arthritic Activity of Anacyclus Valentinus Extract On Adjuvant-Induced Arthritis in RatsIJEAB JournalNo ratings yet
- 22 - Ectoin - Natural - Factsheet - Bitop AG - 44pDocument44 pages22 - Ectoin - Natural - Factsheet - Bitop AG - 44pMihaela Simona IsacNo ratings yet
- White Blood Cell WBC Differential PDFDocument15 pagesWhite Blood Cell WBC Differential PDFStefan SuhartoNo ratings yet
- Cupping For Patients With Inflammatory CDocument2 pagesCupping For Patients With Inflammatory CPatryk StowaszewskiNo ratings yet
- Topnotch Surgery Supplement HandoutDocument85 pagesTopnotch Surgery Supplement HandoutSarah Michelle NiduaNo ratings yet