Professional Documents
Culture Documents
Chapter 6 Wounds
Uploaded by
Andrew BonusCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 6 Wounds
Uploaded by
Andrew BonusCopyright:
Available Formats
Chapter 6 Wounds
(1) Define wound. What are types of surgical wound.
(2) Classify wounds. Discuss each of them briefly.
(3) Describe phases of wound healing.
(4) What are factors affecting wound healing?
(5) Describe wounds in medicolegal aspect.
(6) Outline management of facial wounds.
(7) What are complications of wound healing?
1. Wound
Break in continuity of lining surface epithelium is defined as wound. Wound is seen in a wide variety of situations, e.g. after an accident, assault, surgery
and even self-inflicted wound. Wounds are classified into tidy and untidy wounds.
Types of surgical wounds
i. Clean Wound of elective surgery where hollow viscera* are not entered, e.g. lymph node biopsy.
ii. Clean contaminated Wound where hollow viscera* are entered with minimal contamination.
iii. Contaminated Wound where hollow viscera* are entered with uncontrolled spillage.
iv. Dirty Wound with pus in operative field, e.g. abscess drainage.
*Hollow viscera—gut, respiratory tract, genitourinary tract
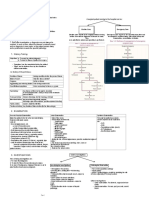
2. Classification of wounds
From practical point of view
Tidy Wounds Untidy Wounds
These are clean wounds caused by sharp Soiled wounds caused by crushing and avulsion injuries. The
instruments and can be closed primarily. If underlying underlying structures (nerves, vessels, etc.) are crushed to
structures (nerves, vessels, etc.) are damaged, they variable extent. They cannot be closed primarily because in
can be repaired at the same sitting before wound presence of foreign bodies and devitalized tissues. High
closure. chances of wound infection, wound dehiscence, septicemia
and even death. Tx - wound toilet and excision of all dead
tissues so that it gets converted to a tidy
TYPES OF WOUND
Abrasion Irregular tearing of only superficial layers of skin as body skids on a rough surface.
Severe pain(Exposed Bleeding points and sensitive nerve endings)
Dirt gets embedded in the wound.
Wound toilet, dressing for management.
Abrasions of face may be left uncovered. Healing occurs in about 10 day’s time.
In case of infection full thickness skin loss may occur.
Contusion • Skin surface remains intact and subcutaneous bleeding occurs, leading to swelling and
skin discoloration.
• The color- red, gradually > blue > black, fades > greenish yellow > normal skin color.
• No treatment is required
Hematoma • More severe injury leading to collection of large volume of blood in tissue planes.
• Large hematomas need intervention -
• requires incision and drainage (Abscess formation)
• can be aspirated with a wide bore needle to liquefied hematoma(a cystic swelling (seroma))
• A large hematoma producing pressure effects (e.g. intracranial hematoma) > Surgery
• A hematoma in a muscle may organize into fibrous tissue producing a very firm swelling.
may be replaced by calcifying osteoid tissue (myositis ossificans), quadriceps femoris muscle
Incised wound • caused by sharp knife, metal and glass.
• Clean wounds and injury occurs along the track of penetration.
• Ideal for primary closure if done within 6 hours of injury.
Lacerated wound • irregular and untidy wounds caused by crushing and tearing forces
• Contusion and abrasion of surrounding area.
• Nerves and vessels may be stretched and torn rather than cleanly divided.
• Grossly contaminated with dust and foreign materials, rapid proliferation of bacteria in dead
and devitalized tissues > infection.
• Tx - wound toilet, excision of dead tissue, primary closure within 6 hours.
• If delayed, the wound should be left open and repaired after a few days when edema and inflammation has subsided.
Punctured wound • Deeper than their length, caused by stabbing action of a long, thin weapon
• A punctured wound can be:
• Penetrating wound: It is an entry wound only.
• Perforating wound: It has both entry and exit wound.
• potentially lethal
• High velocity bullets create shock waves while passing through the tissues,
causes widespread tissue destruction due to cavitational effect
General Surgery Page 1
Avulsion wound • Caused by shearing force that detaches the skin from its underlying structures.
• The raised skin flap may remain attached at one edge; degloving injury.
(separation is between subcutaneous fat and deep fascia)
• Tx - thorough cleansing of the wound, excision of obvious dead tissues and
reposition of skin flap with a few stitches.
• Risk - devascularized skin flap will slowly necrose and become dead.
• Skin flap is completely detached and crushed > wound requires skin grafting after
thorough toilet and debridement of dead tissues.
Crushed wound • Severe blunt injury to the tissues leading to inflammation, edema and bleeding within closed fascial compartments.
• Rise in interstitial pressure leading to decreased blood flow and muscle ischemia that further adds to interstitial edema
• a vicious cycle starts leading to progressive ischemia of muscles and nerves and then limb loss
(Compartment syndrome), can cause acute renal failure.
• Tx - urgent fasciotomy. Longitudinal incisions are given on skin and deep fascia, compressed muscles are released
and restored circulation.
3. Phases of wound healing
- If wound edges are approximated as is done in a clean incised wound, called as healing by primary intention.
- If wound edges cannot be approximated due to presence of devitalized tissue, called as healing by secondary intention.
1. Phase of inflammation (Day 1-4) • “Lag phase”
• Bleeding d/t injury contact with collagen tissue and activates kinins, complement cascade,
clotting factors activated and platelets aggregate. (blood clot formation)
• RBC and WBC escape into the wound ( capillary permeability)
• Polymorphs remove dead tissues during initial 48 hrs.(as scavengers)
• Monocytes act as scavengers.(3rd to 5th day)
• 5th day, capillary budding and fibroblast proliferation starts granulation tissue formation.
2. Phase of granulation tissue (Day 5-20) • The granulation tissue is rich in fibroblasts that secrete collagen and ground substance.
• The fibroblasts protocollagen (immature form) collagen (mature form), hydroxylation.
• mature collagen fiber gives strength to the tissues
• Ground substance = a thin gel like binding agent (binds the collagen fibers)
3. Phase of scar formation (Day 20 onwards) • haphazardly arranged collagen fibers takes place
• New collagen fibers synthesized in an orderly fashion along lines of tension in the scar.
• Vascularity becomes less and ingrowth of nerve fibers and lymphatics takes place.
• imperceptible scar remodeling and gain in strength continues up to 2 years
• scar revision for cosmetic reasons should not be done before 1 year.
4. Factors affecting wound healing
General factors Local factors
Old age Wound hematoma
Anemia Wound infection
Hypoproteinemia Necrotic tissue in wound
Uremia Foreign material in wound
Diabetes Poor blood supply
Jaundice Tension on suture line
Malignancy Faulty wound closure
Chemotherapy Lack of rest to the sutured area
Steroids Local radiotherapy
Immunodeficiency
(HIV infection)
5. Wounds in medicolegal aspect
First examine the patient as a whole and look for vital signs—pulse, blood pressure, respiration, consciousness level, temperature, etc.
Examine the wound
General Surgery Page 2
Examine structures deep to the wound viz:
In limbs Look for major vessel injury by feeling peripheral pulses.
Look for tendon injury by testing movements.
Look for nerve injury by testing sensations and movements.
Look for any fractured bones
In head Look for injuries to skull, brain, eyes and ears.
In chest Look for injuries to lungs, heart and great vessels.
In abdomen Look for injury to solid and hollow viscus.
6. Management of facial wounds
Facial wounds bleed profusely due to high vascularity.
Facial artery can be tied safely without ischemic tissue damage (rich collateral circulation).
Careful clinical examination
Examine inside of the mouth
X-ray is indicated
Ragged skin edges need minimum trimming
Deep tissues are repaired with absorbable sutures
Skin is accurately approximated with several, fine, non-absorbable sutures.
Wounds crossing linear features must accurately approximated (e.g. lips)
A wound inside mouth should be sutured first
Skin sutures are removed on 4th day since wound heals (rich blood supply and less cross marks)
7. Complications of wound healing
Wound infection • complains of throbbing pain
• the wound is tense and inflamed
• The skin sutures need to be removed, wound laid open to allow free drainage of pus
• Pus culture sensitivity, wound dressed regularly, antibiotics
• secondary suturing
Hypertrophic scar • The stages in formation of scar-
• Healing (0-4 weeks): The scar is fine, soft, not contracted and not strong.
• Remodeling (4-12 weeks): The scar is red, raised, itchy, tender and starts contracting.
• Maturation (12-40 weeks): The scar becomes soft, supple and white and tends to
relax.
• If the scar remains in remodeling stage for a longer time, it is called as hypertrophic scar
Keloid (like a Claw) • Excessive growth of the scar tissue
• spreads like a claw into adjoining normal tissues
• itching, erythematous and spreading margins.
• continues to grow even after 1 year or 5-10 years
• Treatment is extremely difficult.
• Use of pressure garments and intralesional injection of triamcenolone with hyalase
(Control Growth)
Skin pigmentation • Pigments
Contractures • final scar is always shorter than original wound.
• The scar should be placed parallel to the line of wrinkle (looks like another wrinkle)
• On face and neck, the lines of wrinkles are at right angles to the direction of fibers of
underlying muscles
• Linear scars cutting the lines of wrinkles, can restrict mobility
• More common if healing occurs with secondary intention, e.g. post-burn contractures.
• The treatment is by doing plastic procedures like Z plasty, Y-V plasty or scar excision with
skin grafting.
Marjolin’s ulcer • Squamous cell carcinoma developing in long-standing scar is called as Marjolin’s ulcer
General Surgery Page 3
You might also like
- WoundDocument31 pagesWoundEnos ErastusNo ratings yet
- Wound Healing and Its Complication: DR - Bile MDocument33 pagesWound Healing and Its Complication: DR - Bile Mzack ian yazinNo ratings yet
- Wound and HealingDocument16 pagesWound and HealingRisav GhoshNo ratings yet
- Wound HealingDocument36 pagesWound HealingShahenda El-falkyNo ratings yet
- Wound HealingDocument36 pagesWound Healingkiran kcNo ratings yet
- Woundhealingseminar 150216070848 Conversion Gate02Document103 pagesWoundhealingseminar 150216070848 Conversion Gate02mohan100% (1)
- Wounds & UlcerDocument15 pagesWounds & UlcerVirendra K. GajbhiyeNo ratings yet
- Unit 1msn Last PartDocument11 pagesUnit 1msn Last PartSusmita BeheraNo ratings yet
- Wound RepairDocument100 pagesWound RepairVergel John ErciaNo ratings yet
- Healing RepairDocument39 pagesHealing RepairRakeesh VeeraNo ratings yet
- 06 Repair2Document23 pages06 Repair2Shameena KnNo ratings yet
- Tissue Healing Processes: Primary vs Secondary IntentionDocument12 pagesTissue Healing Processes: Primary vs Secondary Intentionjyoti kunduNo ratings yet
- Wound Healing-1Document63 pagesWound Healing-1sunday danielNo ratings yet
- L10 Wound HealingDocument26 pagesL10 Wound HealingAnggi HimranNo ratings yet
- GMS511Document29 pagesGMS511Mahmoud NafeaNo ratings yet
- Basic Pathology of Wound Healing and RepairDocument36 pagesBasic Pathology of Wound Healing and Repairaimi BatrisyiaNo ratings yet
- Trauma (Wound & Burn Injury) : Dr. Onarisa Ayu, SpotDocument79 pagesTrauma (Wound & Burn Injury) : Dr. Onarisa Ayu, SpotDini YulidarNo ratings yet
- Hassib Surgery, Volume IV - PDF @AUDatabotDocument49 pagesHassib Surgery, Volume IV - PDF @AUDatabotKhaled OmarNo ratings yet
- 09 Surgical Asepsis & Wound CareDocument44 pages09 Surgical Asepsis & Wound CareBobet ReñaNo ratings yet
- Wound Healing and Its DisordersDocument39 pagesWound Healing and Its Disordersmahdi aljamalNo ratings yet
- Wound Healing: WOUND - It Is A Circumscribed Injury Which Is Caused by External Force and ItDocument5 pagesWound Healing: WOUND - It Is A Circumscribed Injury Which Is Caused by External Force and ItKarolina DoskoczNo ratings yet
- Skin Integrity and Wound CareDocument47 pagesSkin Integrity and Wound CareCHALIE MEQUNo ratings yet
- Wound Healing & BurnsDocument232 pagesWound Healing & BurnsdillaNo ratings yet
- Wound Healing Stages and ManagementDocument10 pagesWound Healing Stages and ManagementAhmed H. Itsh IINo ratings yet
- Drainage harus bersih, tidak berdarah- Ukur volume cairan yang keluar- Perhatikan warna dan bau cairan- Laporkan jika banyak dan berdarah- Lepas setelah sesuai indikasi dokterDocument57 pagesDrainage harus bersih, tidak berdarah- Ukur volume cairan yang keluar- Perhatikan warna dan bau cairan- Laporkan jika banyak dan berdarah- Lepas setelah sesuai indikasi dokterDadek PradnyanaNo ratings yet
- NCMA 219 RLE Laboratory Unit 11bDocument7 pagesNCMA 219 RLE Laboratory Unit 11bJeeduu frostNo ratings yet
- Group 3 Das Souvik (15) David Mahima (16) Deshpande Manaswi (17) Dhulla Pratik (18) Dudhare Shashikant (19) Elango Purnima (20) FAIZANDocument40 pagesGroup 3 Das Souvik (15) David Mahima (16) Deshpande Manaswi (17) Dhulla Pratik (18) Dudhare Shashikant (19) Elango Purnima (20) FAIZANvishnu SNo ratings yet
- Nursing Care For Patient With Wound Nursing Care For Patient With WoundDocument48 pagesNursing Care For Patient With Wound Nursing Care For Patient With Woundayu triaNo ratings yet
- Healing and RepairDocument59 pagesHealing and RepairDyuti SikdarNo ratings yet
- SKIN INTEGRITYDocument2 pagesSKIN INTEGRITYKristine KrisNo ratings yet
- Skin Injury: Dr. Imam FirmansyahDocument28 pagesSkin Injury: Dr. Imam FirmansyahVanquish VeinNo ratings yet
- 4.wound Care IDocument46 pages4.wound Care Iamir aizatNo ratings yet
- Chapter 48 - Skin Integrity and Wound CareDocument13 pagesChapter 48 - Skin Integrity and Wound CareHaji Raji100% (1)
- Wound and Wound HealingDocument18 pagesWound and Wound HealingGopikrishnansNo ratings yet
- Module five: Wound care and dressingDocument40 pagesModule five: Wound care and dressingZahraJaneANo ratings yet
- Tissue Repair & Wound Healing GuideDocument21 pagesTissue Repair & Wound Healing GuideVikash ChoudharyNo ratings yet
- Wounds and Wound Healing: DR Jithin MDocument73 pagesWounds and Wound Healing: DR Jithin Mshruthy rakeshNo ratings yet
- 08 Wound HealingDocument107 pages08 Wound HealingzzmasterNo ratings yet
- Wound Healing and Its Complications - 2Document28 pagesWound Healing and Its Complications - 2Devanand KumarNo ratings yet
- 2 .Bone Fracture ManagementDocument48 pages2 .Bone Fracture Managementcctmt5rpphNo ratings yet
- Wound Healing PhasesDocument27 pagesWound Healing PhasesAnil BasnetNo ratings yet
- Wound HealingDocument4 pagesWound HealingyayassssssNo ratings yet
- Surgical Wound, Surgical Site Infection and AbxDocument53 pagesSurgical Wound, Surgical Site Infection and AbxvimalNo ratings yet
- Wound HealingDocument44 pagesWound HealingSorin Niky MocanuNo ratings yet
- Tissue RepairDocument9 pagesTissue RepairSakidu LegionNo ratings yet
- wound healing in surgeryDocument77 pageswound healing in surgerychguduruNo ratings yet
- ContusionsDocument35 pagesContusionsSARVESH MAWALE100% (1)
- Wound Healing and Burn Care ProcessDocument3 pagesWound Healing and Burn Care ProcessCharmaine PilacNo ratings yet
- Soft Tissue InjuriesDocument25 pagesSoft Tissue InjuriesNgô Duy LongNo ratings yet
- SMNR - 4... Wound HealingDocument62 pagesSMNR - 4... Wound HealingDrAmar GillNo ratings yet
- WOUND HEALING AND CLASSIFICATIONDocument48 pagesWOUND HEALING AND CLASSIFICATIONBenita Janet AppajiNo ratings yet
- Wound Care Guide for Skin Integrity & HealingDocument4 pagesWound Care Guide for Skin Integrity & HealingLiane BartolomeNo ratings yet
- Wound Dressing: Anatomy, Classification, Healing and Debridement Methods/TITLEDocument43 pagesWound Dressing: Anatomy, Classification, Healing and Debridement Methods/TITLENik FatihahNo ratings yet
- WoundDocument19 pagesWoundVasanth RksNo ratings yet
- Copy1-Wounds and Wound HealingDocument44 pagesCopy1-Wounds and Wound Healingfodayskamara67No ratings yet
- Acute and Chronic WoundDocument69 pagesAcute and Chronic Woundaufar isytaharNo ratings yet
- WoundDocument14 pagesWoundHetvi ParmarNo ratings yet
- 3-0 Wound Healing Basic ScienceDocument42 pages3-0 Wound Healing Basic ScienceProfesseur Christian Dumontier100% (2)
- HEALING ORAL WOUNDSDocument47 pagesHEALING ORAL WOUNDSnarmaNo ratings yet
- Skin Wounds And Wound Healing, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSkin Wounds And Wound Healing, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Chapter 8 HemorrhageDocument4 pagesChapter 8 HemorrhageAndrew BonusNo ratings yet
- Chapter 10 Care of The Acutely InjuredDocument3 pagesChapter 10 Care of The Acutely InjuredAndrew BonusNo ratings yet
- Chapter 7 Surgical Asepsis and Antiseptic MeasuresDocument2 pagesChapter 7 Surgical Asepsis and Antiseptic MeasuresAndrew BonusNo ratings yet
- InfectionDocument3 pagesInfectionAndrew BonusNo ratings yet
- Sinus and FistulaDocument3 pagesSinus and FistulaAndrew BonusNo ratings yet
- Infectious Diseases and TreatmentsDocument5 pagesInfectious Diseases and TreatmentsAndrew BonusNo ratings yet
- General Surgery IntroductionDocument1 pageGeneral Surgery IntroductionAndrew BonusNo ratings yet
- Types and Features of InflammationDocument2 pagesTypes and Features of InflammationAndrew BonusNo ratings yet
- FV10 Excel Flux Tutorial en 2Document36 pagesFV10 Excel Flux Tutorial en 2Ahcene BouzidaNo ratings yet
- Material Safety Data Sheet: Chemtherm 550Document6 pagesMaterial Safety Data Sheet: Chemtherm 550Javier vaca villalbaNo ratings yet
- Air Sentry - Energy Statement App 3 Dessicant and Filters PDFDocument20 pagesAir Sentry - Energy Statement App 3 Dessicant and Filters PDFEsteban Fernando Meza IbacetaNo ratings yet
- of The Blessedness of God.Document3 pagesof The Blessedness of God.itisme_angelaNo ratings yet
- Foundation of EducationDocument31 pagesFoundation of EducationM T Ząřřąř100% (1)
- Mathematical Structures of The UniverseDocument228 pagesMathematical Structures of The UniverseMaki MajomNo ratings yet
- Path Loss Models and Wireless Propagation EffectsDocument17 pagesPath Loss Models and Wireless Propagation EffectsAhsan RafiqNo ratings yet
- Simply Supported Beam ReactionsDocument4 pagesSimply Supported Beam ReactionsRushi TutorNo ratings yet
- Tutorial - DGA AnalysisDocument17 pagesTutorial - DGA Analysisw automationNo ratings yet
- Wemco Depurator 2003Document2 pagesWemco Depurator 20031mmahoneyNo ratings yet
- 4.2 - Traditional Double-Walled HapaDocument25 pages4.2 - Traditional Double-Walled HapaThakur VeeruNo ratings yet
- Solar Collectors Final WordDocument14 pagesSolar Collectors Final WordVaibhav Vithoba NaikNo ratings yet
- Kant On Religion and ScienceDocument21 pagesKant On Religion and ScienceEduardo CharpenelNo ratings yet
- Orac Charts - BuenisimoDocument92 pagesOrac Charts - BuenisimosanthigiNo ratings yet
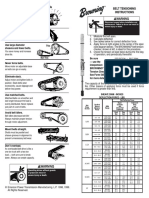
- Browning Belt Tension GaugeDocument2 pagesBrowning Belt Tension GaugeJasperken2xNo ratings yet
- DM3xxx Accessory List LeafletDocument2 pagesDM3xxx Accessory List LeafletAdvantec SrlNo ratings yet
- 2024 Drik Panchang Telugu Calendar v1.0.1Document25 pages2024 Drik Panchang Telugu Calendar v1.0.1Sreekara GsNo ratings yet
- Biomass and Bioenergy: Z.N. Akhlisah, R. Yunus, Z.Z. Abidin, B.Y. Lim, D. KaniaDocument20 pagesBiomass and Bioenergy: Z.N. Akhlisah, R. Yunus, Z.Z. Abidin, B.Y. Lim, D. KaniaPutri sinagaNo ratings yet
- MUSCULAR SYSTEM WORKSHEET Slides 1 To 4Document4 pagesMUSCULAR SYSTEM WORKSHEET Slides 1 To 4kwaiyuen ohnNo ratings yet
- PR900 Operator ManualDocument21 pagesPR900 Operator ManualAlan TanNo ratings yet
- Shadows On The Moon by Zoe Marriott ExtractDocument20 pagesShadows On The Moon by Zoe Marriott ExtractWalker Books100% (1)
- Blackmer Pump Parts ListDocument2 pagesBlackmer Pump Parts ListFelipe Ignacio PaillavilNo ratings yet
- Fitness RX For Women - December 2013Document124 pagesFitness RX For Women - December 2013renrmrm100% (2)
- Whirlpool - Service Information Frontloader Washing Machine AWO/D 43115Document53 pagesWhirlpool - Service Information Frontloader Washing Machine AWO/D 43115amandialopes50% (2)
- C32 MOTOR CAT Electronic Unit Injector - TestDocument2 pagesC32 MOTOR CAT Electronic Unit Injector - TestFreddy Villegas100% (1)
- Line Pack Presentation - Dec 2018Document7 pagesLine Pack Presentation - Dec 2018Goran JakupovićNo ratings yet
- HymssheetDocument4 pagesHymssheettoby_wardmanNo ratings yet
- SE 276B Syllabus Winter 2018Document2 pagesSE 276B Syllabus Winter 2018Manu VegaNo ratings yet
- A Drop of Blood: Casting Time Range Components Duration Casting Time Range Components DurationDocument6 pagesA Drop of Blood: Casting Time Range Components Duration Casting Time Range Components DurationCristobal RencoretNo ratings yet
- Reading Test 7 - PassageDocument12 pagesReading Test 7 - PassageĐinh Quốc LiêmNo ratings yet