Professional Documents
Culture Documents
Dementia 2011 Saunders 1471301211421187
Dementia 2011 Saunders 1471301211421187
Uploaded by
Tamta NagervadzeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dementia 2011 Saunders 1471301211421187
Dementia 2011 Saunders 1471301211421187
Uploaded by
Tamta NagervadzeCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/254085813
The discourse of friendship: Mediators of communication among dementia
residents in long-term care
Article in Dementia · May 2012
DOI: 10.1177/1471301211421187
CITATIONS READS
26 292
4 authors:
Pamela Saunders Kate de Medeiros
Georgetown University Miami University
35 PUBLICATIONS 546 CITATIONS 103 PUBLICATIONS 1,139 CITATIONS
SEE PROFILE SEE PROFILE
Patrick J Doyle Amanda Mosby
Bowling Green State University University of Maryland, Baltimore
17 PUBLICATIONS 202 CITATIONS 6 PUBLICATIONS 80 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
one of several book reviews--not working on now View project
Language and Dementia View project
All content following this page was uploaded by Kate de Medeiros on 05 October 2016.
The user has requested enhancement of the downloaded file.
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Article
Dementia
The discourse of friendship: 0(0) 1–15
! The Author(s) 2011
Mediators of communication Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
among dementia residents DOI: 10.1177/1471301211421187
dem.sagepub.com
in long-term care
Pamela A. Saunders
Georgetown University, USA
Kate de Medeiros
Miami University, USA
Patrick Doyle
University of Maryland, USA
Amanda Mosby
University of Maryland, USA
Abstract
One the most difficult challenges experienced by people with dementia and their caregivers is
their communication. The ability to communicate is essential to creating and maintaining social
relationships. Many individuals who suffer from dementia experience increased agitation and
diminished social interaction in the long-term care living setting. This paper demonstrates how,
through language, they construct social relationships. As part of The Friendship Study, which is an
ethnographic observation of persons with dementia living in a long-term care setting, we analyzed
transcripts from video- and audio-taped data and performed a discourse analysis of conversations
to show how persons with dementia who live in a long-term care setting use language to create
friendships. These analyses show that friendships are constructed using concepts such as
conversational objects, discourse deixis, indexicality, and alignment among speakers.
Keywords
alignment, Alzheimer’s disease, dementia, discourse, friendship, indexicality, social relationships
Corresponding author:
Pamela A. Saunders, PhD, Departments of Neurology and Psychiatry, Georgetown University, School of Medicine,
Washington, DC 20057, USA
Email: saunderp@georgetown.edu
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
2 Dementia 0(0)
Introduction
Communication problems are among the most difficult faced by people with dementia and
their caregivers (Orange & Colton-Hudson, 1998), contributing to an increase in stress,
mortality, and decreased quality of life for both persons with dementia and their
caregivers (Dunn et al., 1994; Mittelman, Ferris, & Steinberg, 1993; Mobily, Maas,
Buckwalter, & Kelley, 1992; Schulz & O’Brien, 1994; Wright, 1993). A variety of studies
of communication-related stress show that caregivers perceive communication breakdown to
be a major problem in coping with the disease (Clark, 1995; Gurland, Toner, Wilder, Chen,
& Lantigua, 1994; Orange, 1991; Richter, Roberto, & Bottenberg, 1995; Williamson
& Schulz, 1993). For example, Williamson and Schulz (1993) found that communication
problems increase the risk of early institutionalization of the person with dementia. Better
understanding of the processes of communication used by persons with dementia in creating
and maintaining relationships in the long-term care setting might reduce the negative
impacts of communication problems (Orange, 1991). The present paper is part of a larger
ethnographic project, The Friendship Study, examining social interactions of persons with
dementia who live in the long-term care setting.
Background
In the last three decades, most of the research regarding dementia has focused on the
neurobiologic or the neuropsychological processes of the disease (Harris, 2002) and has
made efforts to link these findings with the presentation of symptoms. The aim of
treatment has been almost exclusively to improve cognition and to manage undesirable
behaviors through pharmacologic and behavioral efforts, as well as by the manipulation
of the physical environment. There is a growing body of literature studying psychosocial
dimensions of persons with dementia (Clare, 2002, 2003; Clare, Goater, & Woods, 2006;
Clare & Pearce, 2006; Downs, 1997; Harman & Clare, 2006; Hughes, Louw, & Sabat, 2006;
Keady & Nolan, 1995; Keady, Nolan, & Gilliard, 1995; Kontos, 2006; Leibing & Cohen,
2006; Pearce, Clare, & Pistrang, 2002; Sabat, 2001; Van Dijkhuizen, Clare, & Pearce, 2006;
Cotrell & Schulz, 1993). This current project broadens this body of research by examining
how persons with dementia living in a long-term care setting interact socially and suggests
ways that formal and informal caregivers may learn from these interactions.
Starting with the personhood movement, Kitwood and colleagues (Kitwood, 1993, 1997;
Kitwood & Benson, 1995; Kitwood & Bredin, 1992) have attempted to bring to the forefront
the person-centered approach to dementia research and care. In this approach, the person
with dementia is viewed and treated under the assumption that she or he retains an identity
with which to construct and maintain a self through usual types of social interaction. This
approach views a person with dementia as being the same as any other to the extent that her
or his ‘selfhood’ is publicly manifested in various discursive practices such as telling
autobiographical stories, taking on the responsibility for one’s actions, expressing doubt,
declaring an interest in care, decrying the lack of fairness in a situation (Sabat & Harré,
1992). Our paper examines the language of persons with dementia to show how they
establish social relationships with their conversational partners in the institutional setting.
Kitwood (1993) developed a person-centered approach to evaluating dementia care in
formal settings, called Dementia Care Mapping. He examined the viewpoint of the person
with dementia, using both empathy and observational skills. Working within this
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 3
framework, Phinney (2002) described the different ways persons with dementia talk about
living with the disease. She pointed out that to understand the symptoms, as people who
actually have the illness experienced and articulated them, provides a richer understanding of
the whole person. In addition, she suggested that intervention strategies are available only by
paying attention to the communicative behaviors of persons with dementia. For example,
persons in the early stages of dementia often fall silent in conversations. It may be because
they are having trouble keeping up with the pace of the conversation. This is a salient issue
for conversations between persons with dementia in the institutional setting. Conversational
partners may limit conversation because they have difficulty keeping pace or understanding
the semantic content. Knowing this, one conversational partner might try to slow down,
making extra effort to repeat or rephrase previous comments and to ensure that the person
with dementia is following along. If the partner has cognitive impairment, there may be
problems accommodating the conversational needs of the other.
Discourse studies of persons with dementia
Social psychologists and sociolinguists have a long tradition of examining the
communicative experiences of persons with dementia. Sabat and Harré (1992) suggested
that it was common to perceive strategies used by persons with dementia as symptoms of
the disease rather than as attempts to maintain selfhood. Communicative behaviors are a
relevant example of this phenomenon. For example, data collected by the present author
(Saunders, 1998a) include a conversation excerpt from the clinical setting between a
physician and a person diagnosed with dementia. When the physician asked the patient,
‘Who is the president of the United States?’, the patient responded, ‘Oh, he was forgettable’.
This statement is open to a variety of interpretations. Clinicians may call this a
circumlocution (i.e. words and phrases substituted for intended word) and view it as a
symptom of the disease, or as a way to save face (a form of semiotic, or meaning-driven,
behavior) in a humorous way, given the speaker’s inability to recall the name of the
president. To interpret this response as also a socially acceptable communication behavior
is to appreciate it as a way to present oneself as a humorous person who has certain opinions
or political views.
Sociolinguistic studies also examine the language and conversational discourse of persons
with dementia in a naturalistic setting. The goal of these studies is to understand social and
psychological interactions through a linguistic analysis. In an important early study,
Hamilton (1994) described a nursing home resident, Elsie, who maintained the ability to
ask and answer questions into advanced stages of dementia. Elsie describes her own memory
loss by saying, ‘I’ve had so many names. . . sometimes they are hard to get’. Ramanathan
(1997) examined the coherence of the speech of people with dementia, noting that
interlocutors frequently ‘take over’ the conversation, reducing opportunities for subjects
to contribute to the conversation. Previous research by the author, Saunders (1998a,
1998b) analyzed the accounts (i.e., explanations) employed by persons with dementia
regarding their memory loss as a means through which to construct personal identity.
For instance, an example of a memory account is shown here:
Clinician: What floor are we on right now?
Patient: I don’t know because I wasn’t paying attention (ha ha).
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
4 Dementia 0(0)
Sociolinguistic studies as referenced above examine language as an analytical unit used by
persons with dementia. These studies shed light on how we understand social relationships of
people with dementia.
Friendships in persons with dementia in long-term care
Research on social relationships within dementia special care units examined dementia
residents’ relationships with staff members (Cohen-Mansfield & Marx, 1992), residents’
friendships related to agitated behaviors (Kutner, Brown, Stavisky, Clark, & Green,
2000), and staff members’ perceptions of residents’ characteristics and successful
social placement (Wood, Cooper, Richardson, & Forbes, 1992). Specifically, Cohen-
Mansfield and Marx (1992) studied relationships between residents with dementia and
‘outsiders’ (e.g. family, friends not living in the nursing home) but not social
relationships among residents. They found increased agitation was associated with
fewer outside social contacts. Kutner et al. (2000) studied friendship and agitated
behaviors among 59 residents of a dementia care unit. Like Cohen-Mansfield and
Marx (1992), Kutner and colleagues found an association between friendship and
lack of agitated behavior. However, these authors did not investigate qualities that
contribute to the formation of friendships, or characterize those friendships, such as
communicative ability, cognition, and physical function (Astell & Ellis, 2006; Chen,
Ryden, Feldt, & Savik, 2000).
Wood et al. (1992) investigated whether residents’ characteristics (specifically
cognition, affect, and mood and/or behavior) influenced staff members’ perceptions of
the residents’ successful placement in a care facility, and found that negative affect and
depressed mood, rather than cognitive function or behavior, were linked with residents’
being labeled ‘unsuccessfully placed’. These authors did not investigate social
interactions among residents but rather whether or not individual residents ‘fit in’ at
the facility.
Even fewer published studies to date have explored friendships specifically among people
with dementia in long-term care. Diaz Moore (1999) conducted participant observation, as
part of his study of social interaction in the dining room of a specialized dementia long-term
care unit, and described three types of social relationships between residents: (1) ‘congenial
friendships’ based on equality of the participants; (2) the ‘clique’ based on similarity or
power of personality; and (3) ‘confidants’ based on asymmetry. Diaz Moore also
characterized staff/resident negotiations as: ‘befriending’, a positive negotiation in which a
staff member is friendly and sociable with a resident; ‘suggesting’, a negotiation technique in
which staff attempts to convince the residents to do something; and ‘invading,’ a strategy in
which staff occupies residents’ space to socialize among themselves. Diaz Moore’s work
provides important insights into how to examine the types of friendships or social
interactions that may exist.
The above studies examine the discourse of persons with dementia using
frameworks that highlight the discourse and language used by persons with
dementia. The current study illustrates examples of social relationships that are
constructed and maintained through language and discourse among residents in the
long-term care setting.
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 5
Methods
The Friendship Study takes place at Cedar Hill, which is a 20-bed, assisted-living, residential,
care unit for people with moderate to severe dementia. The dementia diagnoses were
determined by the clinical team and confirmed through scores on the Mini-Mental Status
Examination (Folstein, Folstein, & McHugh, 1975). The research team collected data from
residents to characterize their cognition, language, communicative ability, and depression at
Cedar Hill (see the companion article by de Medeiros et al. in this issue). Cedar Hill is a
pseudonym to protect the privacy of the staff and resident participants of this study. The
Institutional Review Board of the Johns Hopkins University School of Medicine reviewed
and approved this study. Resident participants were recruited by first contacting their legally
authorized representative (LAR), then obtaining written informed consent from both LAR
and research participant, and then gaining oral assent from residents again at the time of
data collection (Black, Kass, Fogarty, & Rabins, 2007). Staff participants were recruited
through staff meetings where the research team described the study. Staff participants also
signed informed consent documents. The following sections describe in detail both
participant samples.
Participants
Residents. A total of 31 residents (21 women, 10 men) participated in the study over the
course of the 6-month period. Two participants described their race/ethnicity as African
American; the remainder (n ¼ 29) were European American. Years of education ranged from
8 to 20 years (mean 14 years, SD 3.6 years); see the companion article by de Medeiros, et al
in this issue for full details of the subject sample.
Staff. The staff participants (n ¼ 10) were from three Cedar Hill departments: activities
(n ¼ 3), social work (n ¼ 2), and nursing (n ¼ 5). The nursing staff included certified
nursing assistants and medication aids. Staff had to be employed for at least 1 month at
Cedar Hill with a weekly workload of at least 10 hours to be included in the study.
Ethnographic observations
This study conducted ethnographic observations of residents at Cedar Hill for 10 hours per
week for 24 weeks (6 months). The research team members sat quietly in background areas
and took field notes on interactions between residents, the general social environment, and
other overall impressions. The researchers were instructed to be as unobtrusive as possible to
avoid influencing the interaction between residents more than necessary. When possible, to
capture non-verbal data such as facial expressions, physical position, ‘body language,’ and
other cues to communication, the researchers obtained videotaped footage of residents.
Video-taping was limited to common, public areas of the assisted living wing (e.g., dining
room, television lounge, hallways). Residents’ assent to video-taping and/or audio-taping
was obtained at the start of each observational session. Members of the research team
conducted this additional assent process as extra protection for the residents with
dementia to ensure they were willing to be taped each time. Only written notes were used
if residents did not assent to taping or if residents, staff members, or visitors were present for
whom consent had not been obtained. If participating residents did not assent to taping, the
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
6 Dementia 0(0)
researcher took hand-written ethnographic notes. Multi-modal transcription techniques
used to transcribe videotapes include non-verbal communication such as images and
gestures (Baldry & Thibault, 2006; Iedema, 2003). Verbatim transcriptions (Du Bois,
1991) were made of audiotapes.
Most of the interactions reported in this study occurred in the dining room, which served
as the main social space for Cedar Hill residents. Since residents are free to sit in the dining
room at anytime during the day, often they lingered prior to and after meals. They would
walk through this centrally locating dinning space to their rooms and to reach the activity
rooms and other areas of the assisted-living wing. The doors of each wing were open for
residents to move freely between them.
Results
What is the motivation for people with dementia living in long-term care settings to talk to
one another? In the dining room, the present authors observed conversations around
mealtimes. These conversations resembled what one might expect to hear in any dining
room regardless of the diagnosis of the participants. The research team considered this an
important issue of inquiry: who talks to whom and why? Does it depend on similar personal
attributes of the residents, ambulatory function, language ability, or cognitive status?
One finding of the current study was that often the impetus for a conversation involved a
person or an object in the immediate surroundings. These ‘conversational objects’ were
animate items, inanimate items, and abstract concepts in the local surroundings serving to
promote interaction. Apart from the research team’s equipment (e.g., tape recorder), these
objects were part of the everyday décor at Cedar Hill. See Table 1 for a taxonomy of
conversational objects. An animate object includes people and animals. Inanimate objects
include physical or non-living objects that might be found in a home or office environment.
Conversations also focused on topics that are abstract concepts, such as ideas, feelings, or
sounds. Persons with dementia experience anomia (i.e., word-finding problems) and tend to
use function words (e.g., pronouns, determiners) more frequently than content words (e.g.,
nouns and verbs) as their disease progresses. Hence, the ways in which they referenced
conversational objects may be somewhat non-specific. The following examples will
illustrate the use of conversational objects using pronominal reference.
In the following example, Anna, a resident, is sitting with Mary, a staff member, at the
dining table. Anna initiates a conversation by indexing (i.e., pointing to) a tape recorder,
sitting in the center of the dining table. This tape recorder (an inanimate object) serves as a
conversational object. Example 1 begins with Anna’s reaching for the tape recorder and
Mary’s moving it out of Anna’s reach.1
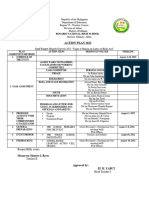
Table 1. Taxonomy of conversational objects.
Animate Inanimate Abstract
People Plants, Trees, Flowers, Activities
(Staff, Residents) Books, Food, Equipment, (Baking, Outings)
Animals (Dogs) Toys, Musical Instruments, Furniture
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 7
Example 1
1 Anna: (Reaches for tape recorder)
2 Mary: Mm mm- That’s- That can’t be touched. Bet-
3 Anna: But that- it’s mine
4 Mary: No ma’am, it’s not yours. Not yours
5 Anna: I- I put one away like that she tells me
6 Laura: Alright S¼
7 Anna: ¼Like mine¼
8 Laura: ¼I’ll get you it, OK?
9 Anna: Ok, thank you
10 Laura: You’re welcome (Laura brings Anna a glass of water) (pause)
11 Here you go Anna. That one is yours
Anna starts the conversation about a novel object sitting on the dining table. Tape
recorders do not usually appear on the lunch table; thus, its presence is a reasonable
conversation starter. Mary, the staff person, knows the tape recorder belongs to the
research team and tries to keep Anna from touching it. On line 3, Anna claims it belongs
to her by saying, ‘that’s mine’; but Mary disagrees. Anna continues by insisting she had one
in her possession and constructs her story using indefinite terms ‘one’ and ‘that’. In addition,
she supports her story with the report of a third party ‘she tells me’.
Much of the talk in this example is punctuated with discourse deixis, which is the use of
pronouns to refer to people, places, and things (Levinson, 1983). Deictic pronouns are a way
of pointing to things in the environment (Lyons, 1977) using indefinite pronouns (e.g., that,
it). On line 3, Anna refers to the tape recorder with the pronouns, ‘that’ and ‘it’. The use of
non-content words, such as pronouns, is common in the speech of persons with dementia
since anomia is a symptom of the disease. Anna makes herself very clear, as this example
shows by Mary’s response on line 4. The use of pronominal reference allows the person with
dementia to feel that she has made herself clear and initiated a conversation. Such feeling is
an important part of being a social actor in any environment.
Moving from the textual level to the discourse level, Example 1 shows that Anna’s use of
deictic pronouns functions to create cohesion and coherence. Cohesion is what makes a text
semantically meaningful and is achieved through syntactic features, such as deictic,
anaphoric and cataphoric elements2 or a logical tense structure, as well as
presuppositions and implications connected to general world knowledge (Halliday &
Hasan, 1976). Coherence is a broader interpretation by interlocutors regarding the
understandability of the interaction. Anna and Laura together achieve cohesion and
coherence through the sequence of turn taking in which they accept and make sense of
each other’s utterances.
Up to a point, the conversation in Example 1 appears still to be about a tape recorder.
Then, on lines 6 and 8, Laura, another staff member who is serving lunch, says, ‘All right, I’ll
get you it’ and offers Anna a glass of water. Now the textual cohesion is complicated by
another interlocutor. It is unclear whether Laura is trying to distract Anna by offering her a
glass of water or if Laura perceives Anna’s claim ‘that’s mine’ to refer to a glass of water. In
line 9, Anna accepts Laura’s offer and her reinterpretation of the conversational object in
question. This re-framing (Goffman, 1974) is a technique used by caregivers to minimize
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
8 Dementia 0(0)
behavioral disturbances. Was Laura aware of her re-framing? Is this a conversational
diversion on the part of the staff member? The present authors suggest that Laura applied
her knowledge of the resident’s ambiguous discourse and found a solution to the issue of
tape recorder ownership.
In the following excerpt, Liz, a physical therapist at Cedar Hill, has just brought Bob, a
resident, back to the dining room after his therapy session. She assists Bob in navigating
the tables and chairs with his walker and then bids him goodbye. When Bob sits down, he
is joining John, another resident, who is already seated. The conversation with Liz,
the therapist, is included to contextualize the conversation that ensues between Bob
and John.
Example 2
1 Liz: You’re welcome. Thank you: Oops be careful of your walker.
Have a good lunch
2 Bob: OK
3 Liz: I’ll see you I’ll see you on Monday, ok?
4 Bob: OK
5 Liz: We’re going to work on this (points to walker) again
6 Bob: Today (speaks to John sitting across the table from him)
7 John: Shakes his head. I’m not even sure. I don’t know what day it is
8 Bob: No I said¼
9 John: ¼Oh¼
10 Bob: ¼She said, I’ll see you on Monday,
I said ‘today’ (smiles and laughs) (pause)
11 Takes me back about six years ago
12 Haha (Bob starts eating lunch)
13 John: (coughs)
This example illustrates the use of indexicality to create linguistic and social meaning. An
indexical behavior or utterance points to (or indicates) some state of affairs. Indexicality is a
phenomenon far broader than language, one that, independently of interpretation, points to
something, such as smoke as an index of fire (Peirce, 1932). In discourse analysis, indexicality
functions to show how speaker-meaning can be viewed on the sentence level and on the
discourse or interactional level.
In Example 2 on line 6, when Bob said ‘today’, he means he would rather not wait
until Monday to see the physical therapist. Then he addresses his comments to John in
an attempt to start conversation. Liz, the therapist, is the conversational object. The
presence of an attractive young woman serves as a way for one gentleman to initiate
conversation with another. The conversational object is indexed by the word3 ‘today’
and points backward to Liz’s comment on line 3 as well as forward to the present
moment of the lunch table with his dining companion. In pointing backward, Bob
uses an indexical to create meaning and continuity in his discourse. At the same time,
he uses an indexical to point forward. First, he points forward by moving the
conversational center to a new interlocutor, John, and second he points forward by
talking about himself. On line 11, he recalls himself in the past. From this example,
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 9
we see Bob using language to create coherence in his discourse along a time continuum
from present to past. Bob’s cognitive status of being diagnosed with dementia in the
mild stages as defined by clinical criteria does not interfere with his ability to construct
his own identify as a gentleman who notices ladies and recalls himself as a younger man.
He uses this identity construction in his discourse and to construct his social
relationships.
The next example illustrates an inanimate item as the conversational object and highlights
the use of function words for indexing a social relationship. Here two residents were
sitting down for lunch when a staff member interrupts the conversation to offer a cup of
coffee.
Example 3
1 Bob: How are you doing?
2 Clara: OK.
3 Staff: Would you like a hot cup of coffee?
4 Bob: Yes, I would. [getting ready to sit down]
5 These things don’t move on the carpet at all. [Bob tries to move table]
6 Clara: Not too much. [laughing]
7 Bob: Not at all. [Bob begins to eat and silence returns to the table]
This is an example of a typical interaction between two residents. The conversational
object introduced on line 5, refers to the lunch table. The conversation is short and
punctuated by staff interjections as seen on line 3 when the staff member offers Bob a
cup of coffee. Bob and Clara align themselves with each other using linguistic devices such
as indefinite nouns as in line 5, when Bob says, ‘these things don’t move’. Alignment, as
described by Goffman (1974), is the way we position ourselves in a social interaction. This
may be done by shifting our footing, stance, or the positions that interlocutors take up in
relation to one another and their utterances. Shifts in footing can affect task, tone, social
roles, and interpersonal alignments (Goffman, 1981). Bob is constructing conversational
cohesion through his linguistic usage. Clara’s response ‘Not too much’ serves to support
the construction of coherence in that she agrees with Bob’s assessment that the table does
not move too much on the carpet. Bob continues to align himself with Clara when he
completes the interaction with a repetition of Clara’s statement on line 6, ‘Not too much’.
Indexicality, as a discursive component of the social relationship, is being co-constructed
by Bob and Clara when they align themselves using function words, adverbs, and
prepositions.
Despite the limited verbal exchanges of persons with dementia in long-term care settings,
repeatedly the data revealed that residents aligned themselves to their conversational
partners. Sometimes the work of making friendly conversation can be challenging when
staff members and meal logistics interrupt. Because these conversational interactions can
be so brief, staff members may overlook them and thus may not recognize them as examples
of friendships being created and maintained.
In the next example, two residents are engaged in a conversation that is recognizable as a
friendly interaction based on the topic of food and caring for others.
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
10 Dementia 0(0)
Example 4
1 Lilly: Listen, you better go get something for yourself to eat.
2 Anna: I am not hungry.
3 Lilly: You are very foolish.
4 Anna: My stuff can sit there.
5 If I get hungry
6 I can get it myself.
7 Lilly: You’re not at home now.
8 Anna: I am.
Here Lilly urged Anna to get something to eat and the conversational object is food, an
inanimate item. Lilly expressed, in line 1, her concern for Anna’s state of hunger. Caring for
one another is what friends do for each other. Anna disputed Lilly’s concern, ‘I am not
hungry’ and informed Lilly on line 4 what her plans are if she gets hungry. While Lilly and
Anna seemed to disagree on one level, this author proposes that the indexical behaviors
reveal friendship or, at least, caring between the speakers. Each line is similar in length,
about four or five words. The structure of the sentence follows a similar syntactic pattern
(subject–verb–object). The repetition of pronouns shows alignment. On lines 1, 2, and 5 Lilly
repeats the second person pronoun, ‘you’. Anna matches this pattern by responding
consistently on lines 2, 5, 6, 8 with the first person pronoun, ‘I’. This example illustrates
the concept of indexicality in that the speakers align themselves using language and syntax
that is synchronous and at the same time indexes their social identities: Lilly as the caregiver
and Anna as the self-sufficient.
Discussion
The conversations among persons with dementia reveal many of the elements of
conversation that one would expect in the conversation of non-impaired adults. The
topics chosen to talk about related to their environment: the food, the furniture, and the
people around them. Their discourse serves socially to construct the residents’ identities as
well as their social relationships. While staff members may subscribe to a person-centered
philosophy, may thoughtfully design the physical environment (Brawley, 2006; Briller &
Calkins, 2000), and may plan activities accordingly (Davis, Byers, Nay, & Koch, 2009),
even still, they may not then be aware of the ways in which language in conversational
interaction functions in the social relationships among persons with dementia.
Conversational interactions reveal that residents with dementia in long-term care do
develop and maintain relationships. These relationships focus on the mundane (e.g., the
furniture) as well as personal (e.g., taking care of oneself). The construction of these
relationships is revealed through the discourse: the use of conversational objects and
linguistic elements that show alignment between friends.
Conversational objects are indexed using definite and indefinite pronouns. Residents with
moderate to severe dementia use their linguistic resources to communicate with staff and
other residents, and this use of language is well within their conversational skill set. A
conversational object is an analytical tool to identify the start of a conversation. While
this study highlights the conversational discourse between residents, this same analytical
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 11
tool can easily be applied to the conversations between resident and staff members. The
identification of conversational objects allows for the analysis of coherent conversations, as
well as of misunderstandings, as seen in Example 2, with Bob and John’s conversation about
the staff member. Bob is doing his best to have a friendly conversation with John about his
memories of himself at a younger age. John in turn is trying to make sense of what John was
saying. This misunderstanding reveals much about how persons with dementia communicate
despite cognitive impairments. That is, they communicate using indefinite linguistic reference
and use alignment of social identities (old self versus young self) thus revealing how social
relationships are constructed in this setting. That is, there may be misunderstandings, and
yet the relationship still perseveres as relationships do among non-diagnosed people who
experience misunderstandings in conversation.
While staff communication was not itself examined here, it was inevitable that it would
appear as part of the communicative interaction in the long-term care setting (Small, Gutman,
Makela, & Hillhouse, 2003). Between staff members and residents, conversational objects
motivate conversation and smooth interaction. In Example 1, the conversational object
starts out as a tape recorder. However, as the conversation ensued Laura, another staff
member, interprets the conversational object to be something else. While it is not clear
whether re-framing is a conscious move on Laura’s part, there was some resolution to the
issue when Anna accepted the glass of water. Vasse, Vernooij-Dassen, Spijker, Rikkert, and
Koopmans (2010) reviewed the literature on staff interventions designed to improve
communication strategies among residents in long-term care facilities. While the meta-
analysis found no overall effects, several of the single-task session interventions with
residents (e.g., life review) and one-on-one tasks embedded in activities of daily living
showed improved communication. Future studies of intervention should include
information for staff members about how persons with dementia use language to construct
their social relationships. In addition, such training should emphasize how the role of the staff
members themselves influences social interaction among residents and how such influence can
be improved further.
Conclusion
While research on the subjective experience of dementia is a growing field (Pearce et al.,
2002; Sabat, 2001; Woods, 2001; Clare, Rowlands, Bruce, Surr & Downs, 2008), additional
research is necessary to understand how the person diagnosed copes with the difficulties (the
realities of their) everyday life. The Friendship Study used both ethnographic and
neuropsychological assessments to explore communication and social relationships among
persons with dementia in the long-term care setting, as well as to examine individual views of
friendship (see the companion article be de Medeiros et al. in this issue), all while keeping the
perspective and the experience of the persons with dementia as a focus of this research.
Using discourse analysis, the conversational examples in this paper illustrate how persons
with dementia use specific linguistic behaviors to construct and maintain relationships with
their fellow residents. These conversational interactions are evidence of how these
individuals construct their own social identities and, in so doing, their social relationships.
Using language, these individuals align themselves with each other to form social bonds at
the conversational level. At the same time, using language in their daily conversations, they
indexically construct social meaning and social relationships with their table-mates. The
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
12 Dementia 0(0)
individuals observed herein are very capable of forming and maintaining friendships, or
pleasant social relationships despite their cognitive or physical impairments. Future
studies will examine interventional strategies with staff and family caregivers to improve
social interaction in long-term care settings.
Acknowledgment
This research was supported by a grant from the Alzheimer’s Association (NIRG-08-91764).
Many thanks are given to Philip A. Saunders for thoroughly proof-reading this and many
other manuscripts.
Conflict of interest statement
The authors declare no conflicts of interest in preparing this article.
Notes
1. Transcription conventions are modified from Du Bois (1991).
2. Anaphora is an instance of one expression referring to another. A cataphoric reference is used to
describe an expression that co-refers with a later expression in the discourse.
3. ‘Today’ in this context may be analyzed as a noun or an adverb depending on the completion of
the sentence. Assuming the rest of the sentence was ‘Today I would like to have another
appointment’, then it would be an adverb modifying time.
References
Astell, A. J., & Ellis, M. P. (2006). The social function of limitation in severe dementia. Infant and Child
Development, 15, 311–319.
Baldry, A., & Thibault, P. J. (2006). Multimodal transcription and text analysis: A multimodal toolkit
and coursebook with associated on-line course. London: Equinox Publishing.
Black, B. S., Kass, N. E., Fogarty, L. A., & Rabins, P. V. (2007). Informed consent for dementia
research: The study enrollment encounter. IRB: Ethics and Human Research, 29(4), 7–14.
Brawley, E. (2006) Design Innovations for Aging and Alzheimer’s: Creating Caring Environments. New
York: Wiley-Blackwell.
Briller and Calkins (2000) Conceptualizing care settings as home, resort or hospital. Alzheimer’s Care
Quarterly, 1(1), 17–23.
Chen, Y., Ryden, M., Feldt, K., & Savik, K. (2000). The relationship between social interaction and
characteristics of aggressive, cognitively impaired nursing home residents. American Journal of
Alzheimer’s Disease, 15, 10–17.
Clare, L. (2002). We’ll fight it as long as we can: Coping with the onset of Alzheimer’s disease. Aging
and Mental Health, 6, 139–148.
Clare, L. (2003). Managing threats to self: The construction of awareness in early-stage Alzheimer’s
disease. Social Science and Medicine, 57, 1017–1029.
Clare, L., Goater, T., & Woods, B. (2006). Illness representations in early-stage dementia:
A preliminary investigation. International Journal of Geriatric Psychiatry, 21, 761–767.
Clare, L., Rowlands, J., Bruce, E., Surr, C., & Downs, M. (2008). The experience of living with
dementia in residential care: An interpretative phenomenological analysis. The Gerontologist, 48,
711–720.
Clark, L. W. (1995). Intervention for persons with Alzheimer’s disease: Strategies for maintaining and
enhancing communicative success. Topics in Language Disorders, 15, 47–66.
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 13
Cohen-Mansfield, J., & Marx, M. S. (1992). The social network of the agitated nursing home resident.
Research on Aging, 14, 110–123.
Cotrell, V., & Schulz, R. (1993). The perspective of the patient with Alzheimer’s disease: A neglected
dimension of dementia research. The Gerontologist, 33, 205–211.
Davis, S., Byers, S., Nay, R., & Koch, S. (2009). Guiding design of dementia friendly environments in
residential care settings: Considering the living experiences. Dementia, 8, 185–203.
Diaz Moore, K. (1999). Dissonance in the dining room: A study of social interaction in a special care
unit. Qualitative Health Research, 9, 133–155.
Downs, M. (1997). The emergence of the person in dementia research. Ageing and Society, 17, 597–607.
Du Bois, J. W. (1991). Transcription design principles for spoken discourse research. Pragmatics, 1,
71– 106.
Dunn, L. A., Rout, U., Carson, J., & Ritter, S. A. (1994). Occupational stress amongst care staff
working in nursing homes: An empirical investigation. Journal of Clinical Nursing, 3, 177–183.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: A practical method for
grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Goffman, E. (1974). Frame analysis. New York: Harper & Row.
Goffman, E. (1981). Forms of talk. Philadelphia, PA: University of Pennsylvania Press.
Gurland, B., Toner, J., Wilder, D., Chen, J., & Lantigua, R. (1994). Impairment of communication and
adaptive functioning in community-residing elderly with advanced dementia. Alzheimer Disease and
Associated Disorders, 8, 230–241.
Hamilton, H. (1994). Conversations with an Alzheimer’s patient: An interactional examination of
questions and responses. New York: Cambridge.
Harman, G., & Clare, L. (2006). Illness representations and lived experience in early-stage dementia.
Qualitative Health Research, 16, 484–502.
Halliday, M. A. K., & Hasan, R. (1976). Cohesion in English. London: Longman.
Harris, P. B. (Ed.) (2002). The person with Alzheimer’s disease: Pathways to understanding the
experience. Baltimore, MD: Johns Hopkins University Press.
Hughes, J., Louw, S. J., & Sabat, S. (Eds.) (2006). Dementia: Mind, meaning, and the person. Oxford:
Oxford University Press.
Iedema, R. (2003). Multimodality, resemioticization: Extending the analysis of discourse as a
multisemiotic practice. Visual Communication, 2, 29–57.
Kitwood, T. (1993). Towards a theory of dementia care: The interpersonal process. Aging and Society,
13, 51–67.
Kitwood, T. (1997). Dementia Reconsidered: The person comes first. Rethinking Aging. Buckingham:
Open University Press.
Kitwood, T., & Benson, S. (1995). The new culture of dementia care. London: Hawker Publications.
Kitwood, T., & Bredin, K. (1992). Towards a theory of dementia care: Personhood and well-being.
Ageing Society, 12, 269–287.
Kutner, N. G., Brown, P. J., Stavisky, R. C., Clark, W. S., & Green, R. C. (2000). ‘‘Friendship’’
interactions and expression of agitation among residents of a dementia care unit: Six-month
observational data. Research on Aging, 22, 188–205.
Keady, J., & Nolan, M. (1995). IMMEL: Assessing coping responses in the early stages of dementia.
British Journal of Nursing, 4, 309–314.
Keady, J., Nolan, M. R., & Gilliard, J. (1995). Listen to the voices of experience. Journal of Dementia
Care, 3(May–June), 15–17.
Kontos, P. C. (2006). Embodied selfhood: An ethnographic exploration of Alzheimer’s disease.
In A. Leibing, & L. Cohen (Eds.), Thinking about dementia: Culture, loss, and the anthropology
of senility (pp. 195–217). New Brunswick, NJ: Rutgers University Press.
Leibing, A., & Cohen, L. (Eds.) (2006). Thinking about dementia: Culture, loss, and the anthropology of
senility. New Brunswick, NJ: Rutgers University Press.
Levinson, S. C. (1983). Pragmatics. Oxford: Cambridge University Press.
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
14 Dementia 0(0)
Lyons, J. (1977). Deixis, space and time. Semantics, 2, 636–724.
Mittelman, M. S., Ferris, S. H., & Steinberg, G. (1993). An intervention that delays institutionalization
of Alzheimer’s disease patients: treatment of spouse-caregivers. The Gerontologist, 33, 730–740.
Mobily, P. R., Maas, M. L., Buckwalter, K. C., & Kelley, L. S. (1992). Staff stress on an Alzheimer’s
unit. Journal of Psychosocial Nursing in Mental Health Services, 30, 25–31.
Orange, J. B. (1991). Perspectives of family members regarding communication changes.
In R. Lubinski (Ed.), Dementia and Communication (pp. 168–186). Philadelphia, PA: Mosby.
Orange, J. B., & Colton-Hudson, A. (1998). Enhancing communication in dementia of the Alzheimer’s
type. Topics in Geriatric Rehabilitation, 14(2), 56–75.
Pearce, A., Clare, L., & Pistrang, N. (2002). Managing sense of self: Coping in the early stages of
Alzheimer’s disease. Dementia, 1, 173–192.
Peirce, C. S. (1932). Division of signs. In Collected Papers of Charles Sanders Peirce. Cambridge:
Cambridge University Press.
Phinney, A. (2002). Living with the symptoms. In P. B. Harris (Ed.), The person with Alzheimer’s
disease (pp. 49–76). Baltimore, MD: The Johns Hopkins University Press.
Ramanathan, V. (1997). Alzheimer Discourse: Some Sociolinguistic Dimensions. Mahwah, NJ:
Lawrence Erlbaum Associates.
Richter, J. M., Roberto, K., & Bottenberg, D. J. (1995). Communicating with persons with
Alzheimer’s disease: Experiences of family and formal caregivers. Archives of Psychiatric Nursing,
9, 279–285.
Sabat, S. R. (2001). The experience of Alzheimer’s disease: Life through a tangled veil. Oxford:
Blackwell.
Sabat, S. R., & Harré, R. (1992). The construction and deconstruction of self in Alzheimer’s disease.
Aging and Society, 12, 443–461.
Saunders, P. A. (1998a). ‘‘You’re out of your mind!’’ An analysis of humor as a face saving strategy for
patients and clinicians during neuropsychological examinations. Health Communication, 10,
357–372.
Saunders, P. A. (1998b). ‘‘My brain’s on strike’’: The construction of identity through memory
accounts by dementia patients. Research on Aging, 20, 65–90.
Schulz, R., & O’Brien, A. T. (1994). Alzheimer’s disease caregiving: An overview. Seminars in Speech
and Language, 15, 185–194.
Small, J. A., Gutman, G., Makela, S., & Hillhouse, B. (2003). Effectiveness of communication
strategies used by caregivers of persons with Alzheimer’s disease during activities of daily living.
Journal of Speech, Language, and Hearing Research, 46, 353–367.
Van Dijkhuizen, M., Clare, L., & Pearce, A. (2006). Striving for connection: Appraisal and coping
among women with early-stage Alzheimer’s disease. Dementia, 5(1), 73–94.
Vasse, E., Vernooij-Dassen, M., Spijker, A., Rikkert, M. O., & Koopmans, R. (2010). A systematic
review of communication strategies for people with dementia in residential and nursing homes.
International Psychogeriatrics, 22(02), 189.
Williamson, G. M., & Schulz, R. (1993). Coping with specific stressors in Alzheimer’s disease
caregiving. The Gerontologist, 33, 747–755.
Wood, K. A., Cooper, J. A., Richardson, K., & Forbes, A. (1992). Affective behaviour and success of
EMI community home placement. International Journal of Geriatric Psychiatry, 7, 351–356.
Woods, R. T. (2001). Discovering the person with Alzheimer’s disease: Cognitive, emotional, and
behavioral aspects. Aging and Mental Health, 5, 7–S16.
Wright, L. W. (1993). Alzheimer’s Disease and Marriage. Newbury Park, CA: Sage Publications.
Pamela A. Saunders, PhD, is an Associate Professor in the Departments of Neurology and
Psychiatry at Georgetown University School of Medicine. Her research focuses on the
identity, and the preserved, communicative abilities of persons with dementia. In addition,
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
XML Template (2011) [3.11.2011–3:08pm] [1–15]
K:/DEM/DEM 421187.3d (DEM) [PREPRINTER stage]
Saunders et al. 15
she teaches medical students how to communicate in clinical settings. She is the author of
multiple articles on language, communication, and dementia as well as in the arena of
medical education.
Kate de Medeiros, PhD, is Assistant Professor of Gerontology in the Department of
Sociology and Gerontology, Miami University, Oxford, Ohio. Her research focuses
broadly on the construction of selfhood in old age and includes work on friendships and
self expression/performance through autobiographical writing for a variety of older
populations. She has published work on the complementary self in old age, narrative
explorations of selfhood, neuropsychiatric symptoms in dementia, and the meaning of
suffering.
Patrick Doyle, MA, is a doctoral candidate in Gerontology at the University of Maryland,
Baltimore County. His research has focused on how caregiving practices, physical
environments, and social interactions influence the lived experience of people with
dementia residing in long-term care settings. In his dissertation research, he is examining
how a person-centered model of care is interpreted and applied by various stakeholders
within a dementia-specific long-term care setting.
Amanda Mosby graduated from Indiana University with a master’s degree in social and
cognitive psychology. She has directed a variety of research studies that have focused on
sociological, behavioral, and public health issues including memory performance in older
adults and the concept of generativity in childless older women. She is currently a research
associate at the University of Maryland Baltimore County in the Department of Sociology
and Anthropology.
Downloaded from dem.sagepub.com at Miami University Libraries on October 5, 2016
View publication stats
You might also like
- Savage Worlds MLP EditionDocument66 pagesSavage Worlds MLP EditionCarsten_Curren_7854100% (8)
- Introvert Extrovert QuestionnaireDocument2 pagesIntrovert Extrovert QuestionnaireJustin Oliver Hautea67% (3)
- Maiorescu 2017Document25 pagesMaiorescu 2017Ligia-Elena StroeNo ratings yet
- Comparision of Banking System of Us, Europe, India-1Document36 pagesComparision of Banking System of Us, Europe, India-1Rashmeet Kaur100% (2)
- Purpose of Summons in Action in Rem and Quasi in RemDocument4 pagesPurpose of Summons in Action in Rem and Quasi in Remjane100% (2)
- Miller 2014Document17 pagesMiller 2014dantealtighieriNo ratings yet
- Final Thesis PaperDocument24 pagesFinal Thesis PaperJessa D. SabudNo ratings yet
- Tomenyetal.2017 RIDD PreprintDocument35 pagesTomenyetal.2017 RIDD Preprintsanskriti gautamNo ratings yet
- AAC Interventions For Individuals With Autism Spectrum Disorders - State of The Science and Future Research DirectionsDocument13 pagesAAC Interventions For Individuals With Autism Spectrum Disorders - State of The Science and Future Research DirectionsLiamariasabauNo ratings yet
- Public Display of AffectionDocument2 pagesPublic Display of AffectionMicca MitraNo ratings yet
- Div Class Title Socioemotional Profiles of Autism Spectrum Disorders Attention Deficit Hyperactivity Disorder and Disinhibited and Reactive Attachment Disorders a Symptom Comparison and Network Approach DiDocument10 pagesDiv Class Title Socioemotional Profiles of Autism Spectrum Disorders Attention Deficit Hyperactivity Disorder and Disinhibited and Reactive Attachment Disorders a Symptom Comparison and Network Approach DiArnau Miquel CosNo ratings yet
- Everyday Conversation in Dementia A Review of The Literature To Inform Research and PracticeDocument15 pagesEveryday Conversation in Dementia A Review of The Literature To Inform Research and Practicexyang105No ratings yet
- Dissociation, Dissociative Disorders, and PTSD: January 2015Document17 pagesDissociation, Dissociative Disorders, and PTSD: January 2015Jorge LusagaNo ratings yet
- AJSLP BradyDocument14 pagesAJSLP BradygiselleprovencioNo ratings yet
- Morgan - Students' Perceptions of The Effect (AAM) 2016Document39 pagesMorgan - Students' Perceptions of The Effect (AAM) 2016Tarun SoniNo ratings yet
- Fears Article CCR 2012 April Dwyer DavidsonDocument11 pagesFears Article CCR 2012 April Dwyer DavidsonaachecheutautautaNo ratings yet
- Channels of Computer-Mediated Communication and Satisfaction in Long-Distance RelationshipsDocument17 pagesChannels of Computer-Mediated Communication and Satisfaction in Long-Distance RelationshipsgabbymacaNo ratings yet
- Wrzus Etal2017friendship AdulthoodDocument17 pagesWrzus Etal2017friendship AdulthoodRheivita Mutiara FawzianNo ratings yet
- ContentserverDocument18 pagesContentserverapi-406956380No ratings yet
- The Benefit of Contact For Prejudice-Prone Individuals: The Type of Stigmatized Outgroup MattersDocument14 pagesThe Benefit of Contact For Prejudice-Prone Individuals: The Type of Stigmatized Outgroup MattersSiti SurtiNo ratings yet
- Personality and Individual Di FferencesDocument6 pagesPersonality and Individual Di FferencesJefri ansyahNo ratings yet
- This Is Me: Evaluation of A Boardgame To Promote Social Engagement, Wellbeing and Agency in People With Dementia Through Mindful Life-StorytellingDocument23 pagesThis Is Me: Evaluation of A Boardgame To Promote Social Engagement, Wellbeing and Agency in People With Dementia Through Mindful Life-StorytellingNatalia Francisca ValdésNo ratings yet
- Marquardt Et Al 2014 Impact of The Design of The Built Environment On People With Dementia An Evidence Based ReviewDocument31 pagesMarquardt Et Al 2014 Impact of The Design of The Built Environment On People With Dementia An Evidence Based Reviewyfive soneNo ratings yet
- J DENT RES-2015-Schwendicke-10-8Document9 pagesJ DENT RES-2015-Schwendicke-10-8Tahir AliNo ratings yet
- Willingness To Communicate in A Second Language THDocument21 pagesWillingness To Communicate in A Second Language THBaihaqi Zakaria MuslimNo ratings yet
- Is Public Speaking Really More Feared Than Death?: Communication Research Reports April 2012Document11 pagesIs Public Speaking Really More Feared Than Death?: Communication Research Reports April 2012Gilang NugrahaNo ratings yet
- Navigating Thin' Dating Markets: Mid-Life Repartnering in The Era of Dating Apps and WebsitesDocument17 pagesNavigating Thin' Dating Markets: Mid-Life Repartnering in The Era of Dating Apps and WebsitescutkilerNo ratings yet
- 2020-InfluenceTraumaSymptomsonAlliance JCD1 PDFDocument13 pages2020-InfluenceTraumaSymptomsonAlliance JCD1 PDFIsaac AkakyinsimiraNo ratings yet
- When Online Meets Offline The Effect of Modality Switching On Relational CommunicationDocument25 pagesWhen Online Meets Offline The Effect of Modality Switching On Relational CommunicationAbdul WahabNo ratings yet
- Edwards Bybee Frost Harvey Navarro 2017Document24 pagesEdwards Bybee Frost Harvey Navarro 2017polandpoplawskaNo ratings yet
- Article - Evaluating The Efficacy of Drama Therapy in Teaching Social Skills To Children With Autism Spectrum DisordersDocument20 pagesArticle - Evaluating The Efficacy of Drama Therapy in Teaching Social Skills To Children With Autism Spectrum DisordersDespina Kalaitzidou100% (3)
- Sibling Relationship and Friendship in Adolescents With AutismDocument10 pagesSibling Relationship and Friendship in Adolescents With AutismNobodyNo ratings yet
- A Multi-Study Examination of Attachment and Implicit Theories of Relationships in Ghosting ExperiencesDocument24 pagesA Multi-Study Examination of Attachment and Implicit Theories of Relationships in Ghosting ExperiencesAquina Case SaymanNo ratings yet
- Love OnlineDocument14 pagesLove Onlineferrerkale13No ratings yet
- Intergroup Contact, Social Dominance and Environmental Concern: A Test of The Cognitive-Liberalization HypothesisDocument64 pagesIntergroup Contact, Social Dominance and Environmental Concern: A Test of The Cognitive-Liberalization HypothesisAbdülkadir IrmakNo ratings yet
- 3 - Acquiescence-Response-Styles - A-Multilevel-Model-Exp - 2017 - Personality-and-InDocument5 pages3 - Acquiescence-Response-Styles - A-Multilevel-Model-Exp - 2017 - Personality-and-InbelenNo ratings yet
- The Best PDF Ever Download It NowDocument7 pagesThe Best PDF Ever Download It Nowchiquinho.gaviao231No ratings yet
- Annotated Bibliography SampleDocument9 pagesAnnotated Bibliography SampleIan Paul Hurboda DaugNo ratings yet
- Wan Muelleretal - gpsdementiaCareAcademia-Industryperspective ToCHI2016Document37 pagesWan Muelleretal - gpsdementiaCareAcademia-Industryperspective ToCHI2016Mharits FadhillaNo ratings yet
- Research Paper Outline On Down SyndromeDocument4 pagesResearch Paper Outline On Down Syndromeegw4qvw3100% (1)
- Computers in Human Behavior: Brendan Dempsey, Kathy Looney, Roisin Mcnamara, Sarah Michalek, Eilis HennessyDocument9 pagesComputers in Human Behavior: Brendan Dempsey, Kathy Looney, Roisin Mcnamara, Sarah Michalek, Eilis HennessyFulaneto AltoNo ratings yet
- Brand Loewenstein Spiegel Dispelling Myths DIDTreatment 2014Document23 pagesBrand Loewenstein Spiegel Dispelling Myths DIDTreatment 2014Inna RiegoNo ratings yet
- The Art of Breaking Up - Ending Romantic RelationshipsDocument45 pagesThe Art of Breaking Up - Ending Romantic Relationshipspaul tNo ratings yet
- Article 5Document24 pagesArticle 5syamimiNo ratings yet
- Can Digital Technology Enhance Social Connectedness Among Older Adults? A Feasibility StudyDocument24 pagesCan Digital Technology Enhance Social Connectedness Among Older Adults? A Feasibility Studydena dgNo ratings yet
- Disclosure of Stuttering and Quality of Life in People Who StutteDocument11 pagesDisclosure of Stuttering and Quality of Life in People Who Stuttephelie2008No ratings yet
- Annotated BibliographyDocument5 pagesAnnotated Bibliographyapi-259529340No ratings yet
- New Nomenclature DementiaDocument7 pagesNew Nomenclature DementiaFernando lazzarettiNo ratings yet
- DEMTEC Health Care ProfessionalsDocument28 pagesDEMTEC Health Care ProfessionalsrajasinguNo ratings yet
- Decision Making Styles East and West Is It Time ToDocument9 pagesDecision Making Styles East and West Is It Time ToSharrme ChandranNo ratings yet
- 1.) Fear of Public Speaking - Perception of College Students and Correlates - ScienceDirectDocument6 pages1.) Fear of Public Speaking - Perception of College Students and Correlates - ScienceDirectwakinn lezgoNo ratings yet
- 1Document134 pages1ghizlane berradaNo ratings yet
- Loneliness Being AloneDocument17 pagesLoneliness Being AloneAsri PutriNo ratings yet
- DospertDocument12 pagesDospertAndreea LixandruNo ratings yet
- Comm Research Final PaperDocument19 pagesComm Research Final Paperapi-528626923No ratings yet
- Do You Have Anything To Hide Infidelity-Related BeDocument33 pagesDo You Have Anything To Hide Infidelity-Related BeDewwii AmbarwatiiNo ratings yet
- 2022 Duker - ReviewDocument19 pages2022 Duker - Reviewfabian.balazs.93No ratings yet
- Different Types of Internet Use, Depression, and Social Anxiety: The Role of Perceived Friendship QualityDocument16 pagesDifferent Types of Internet Use, Depression, and Social Anxiety: The Role of Perceived Friendship QualityTom ArrolloNo ratings yet
- Research On NarcissismDocument46 pagesResearch On NarcissismBen ApawNo ratings yet
- Trans and Family Therapy Edwards2018Document17 pagesTrans and Family Therapy Edwards2018Francisca Nilsson RodríguezNo ratings yet
- Lanzi Burshnic Bourgeois 2017Document15 pagesLanzi Burshnic Bourgeois 2017DivyaChettyNo ratings yet
- Workplace Relationships, Stress, and Verbal Rumination in OrganizationsDocument12 pagesWorkplace Relationships, Stress, and Verbal Rumination in OrganizationsHany A AzizNo ratings yet
- Mrug 09Document10 pagesMrug 09Savio RebelloNo ratings yet
- Fast Facts: Dementia and Augmentative and Alternative Communication: Supporting conversationsFrom EverandFast Facts: Dementia and Augmentative and Alternative Communication: Supporting conversationsNo ratings yet
- A Corpus Based Analysis of William BlakeDocument20 pagesA Corpus Based Analysis of William BlakeTamta NagervadzeNo ratings yet
- WS ARTIST Final Conference CUN Siol EilksDocument35 pagesWS ARTIST Final Conference CUN Siol EilksTamta NagervadzeNo ratings yet
- Speaking and Listening Skills DevelopmentDocument37 pagesSpeaking and Listening Skills DevelopmentTamta NagervadzeNo ratings yet
- Yesterday? I Walk To SchoolDocument6 pagesYesterday? I Walk To SchoolTamta NagervadzeNo ratings yet
- The Application of Translation Strategies and Predicate Transformations in Teaching Written TranslationDocument13 pagesThe Application of Translation Strategies and Predicate Transformations in Teaching Written TranslationTamta NagervadzeNo ratings yet
- A Critical Discourse Analysis of The Power RelatioDocument6 pagesA Critical Discourse Analysis of The Power RelatioTamta NagervadzeNo ratings yet
- Book Review by Azhar Kaz MiDocument3 pagesBook Review by Azhar Kaz Miappu kundaNo ratings yet
- Petition For Change of NameDocument44 pagesPetition For Change of NameLenNo ratings yet
- Case Study 4: Brothers MowersDocument2 pagesCase Study 4: Brothers MowersRayan HafeezNo ratings yet
- unit5-MB 0001Document12 pagesunit5-MB 0001yogaknNo ratings yet
- Somebody To LoveDocument3 pagesSomebody To LoveIksan PutraNo ratings yet
- Circulatory SystemDocument5 pagesCirculatory SystemMissDyYournurse100% (1)
- Universal Network Solutions IncDocument15 pagesUniversal Network Solutions IncChandu NsaNo ratings yet
- UOI V Indian Navy Civilian Design Officers Association & AnrDocument6 pagesUOI V Indian Navy Civilian Design Officers Association & Anrkhyati vermaNo ratings yet
- HRM WordDocument7 pagesHRM WordShaishav BhesaniaNo ratings yet
- IC5 L1 WQ U15to16 PDFDocument2 pagesIC5 L1 WQ U15to16 PDFRichie Ballyears100% (1)
- How To Use ArticlesDocument7 pagesHow To Use Articlescrazy about readingNo ratings yet
- Chemistry CrosswordDocument1 pageChemistry CrosswordHanifan Al-Ghifari W.No ratings yet
- WFDDocument97 pagesWFDajay WaliaNo ratings yet
- Lesson PlansDocument7 pagesLesson Plansapi-316237434100% (1)
- FPEBb6 Hadji Nabel FPE MidtermDocument5 pagesFPEBb6 Hadji Nabel FPE MidtermNadhif Radiamoda Hadji NabelNo ratings yet
- Chapter 2 Solution 1Document4 pagesChapter 2 Solution 1Pragya PandeyNo ratings yet
- Action Plan - Brigada Eskwela 2022Document1 pageAction Plan - Brigada Eskwela 2022Anna Lou R. retubaNo ratings yet
- Mapping Toolbox GuideDocument1,710 pagesMapping Toolbox GuideAaron RampersadNo ratings yet
- Fantastics English Monday Letter Writing Powerpoint 41973Document17 pagesFantastics English Monday Letter Writing Powerpoint 41973Aryan KyathamNo ratings yet
- Fulltext 01Document54 pagesFulltext 01Shafayet UddinNo ratings yet
- Daily Painting and Observations On Art, Nature and Life, by Stefan BaumannDocument122 pagesDaily Painting and Observations On Art, Nature and Life, by Stefan BaumannStefan BaumannNo ratings yet
- Lecture Planner - Mathematics - LAKSHYA JEE 2022 PLANNER - MathematicsDocument5 pagesLecture Planner - Mathematics - LAKSHYA JEE 2022 PLANNER - MathematicsprekshaNo ratings yet
- UAS Pre ExerciseDocument2 pagesUAS Pre Exerciserain maker100% (2)
- English PunctuationDocument157 pagesEnglish Punctuationayman.barghash9635No ratings yet
- Secretary of Justice v. LantionDocument53 pagesSecretary of Justice v. LantionKristinaCuetoNo ratings yet
- Lesson 4 Activity CrashingDocument17 pagesLesson 4 Activity CrashingMuhammad Syahir BadruddinNo ratings yet