Professional Documents
Culture Documents
Original Research: Video-Based Motion Analysis Use: A National Survey of Orthopedic Physical Therapists
Uploaded by
Agus TinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Original Research: Video-Based Motion Analysis Use: A National Survey of Orthopedic Physical Therapists
Uploaded by
Agus TinaCopyright:
Available Formats
Original Research
Video-Based Motion Analysis Use: C.P. Hensley, PT, DPT, Department of
Physical Therapy and Human
Movement Sciences, Northwestern
A National Survey of Orthopedic University Feinberg School of
Medicine, Chicago, Illinois.
Physical Therapists D. Millican, PT, DPT, Department of
Physical Therapy and Human
Movement Sciences, Northwestern
Craig P. Hensley, Devyn Millican, Nida Hamilton, Amy Yang, University Feinberg School of
Jungwha Lee, Alison H. Chang Medicine, Chicago, Illinois.
N. Hamilton, PT, DPT, Department of
Physical Therapy and Human
Objectives. Motion analysis is performed by physical therapists to assess and improve
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
Movement Sciences, Northwestern
movement. Two-dimensional video-based motion analysis (VBMA) is available for smart- University Feinberg School of
phones/tablets and requires little to no equipment or cost. Research on VBMA use in Medicine, Chicago, Illinois.
clinical practice is limited. The purpose of this study was to examine the current use of
A. Yang, MSc, Department of
VBMA in orthopedic physical therapist practice. Preventive Medicine, Northwestern
University Feinberg School of
Methods. Members of the Academy of Orthopaedic Physical Therapy completed an Medicine, Chicago, Illinois.
online survey. Questions examined frequency of VBMA use, reasons for use, facilita- J. Lee, PhD, Department of Preventive
tors/barriers, device/apps used, practice patterns, other certificates/degrees, and demo- Medicine, Northwestern University
graphic information. Feinberg School of Medicine,
Chicago, Illinois.
Results. Among the final analysis sample of 477 respondents, 228 (47.8%) use VBMA. Of A.H. Chang, PT, DPT, Department of
228 VBMA users, 91.2% reported using it for ≤25% of their caseload, and 57.9% reported Physical Therapy and Human
using their personal device to capture movement. Reasons for using VBMA included visual Movement Sciences, Northwestern
feedback for patient education (91.7%), analysis of movement (91.2%), and assessment of University Feinberg School of
progress (51.8%). Barriers to use included lack of device/equipment (48.8%), lack of space Medicine, 645 N Michigan Avenue,
(48.6%), and time restraint (32.1%). Those with ≤20 years of clinical experience (odds ratio #1100, Chicago, IL 60611 (USA).
Address all correspondence to Dr
[OR] = 1.83, 95% CI = 1.21–2.76), residency training (OR = 2.49, 95% CI = 1.14–5.43),
Chang at: hsini@northwestern.edu.
and fellowship training (OR = 2.97, 95% CI = 1.32–6.66), and those from the West region
[Hensley CP, Millican D, Hamilton N,
of the United States (OR = 1.66, 95% CI = 1.07–2.56) were more likely to use VBMA.
Yang A, Lee J, Chang AH. Video-based
motion analysis use: a national survey
Conclusions. More than 50% of surveyed orthopedic physical therapists do not use of orthopedic physical therapists. Phys
VBMA in clinical practice. Future research should be directed toward assessing reliability Ther. 2020;100:1759–1770.]
and validity of VBMA use by smartphones, tablets, and apps and examining whether VBMA
© The Author(s) 2020. Published by
use enhances treatment outcomes. Data security, patient confidentiality, and integration
Oxford University Press on behalf of
into the electronic medical record should be addressed. the American Physical Therapy
Association. All rights reserved. For
Impact. This study is the first to our knowledge to describe the use of VBMA permissions, please e-mail:
in orthopedic physical therapist practice in the United States. It is the first step in journals.permissions@oup.com
understanding how VBMA is used and might be used to enhance clinical assessment and Published Ahead of Print:
treatment outcomes. July 31, 2020
Accepted: May 4, 2020
Submitted: November 1, 2019
Post a comment for this
article at:
https://academic.oup.com/ptj
2020 Volume 100 Number 10 Physical Therapy 1759
Video-Based Motion Analysis
T
“ ransforming society by optimizing movement research on VBMA use in clinical practice is currently
to improve the human experience” is the vision limited.
statement for the physical therapy profession put
forth by the American Physical Therapy Association.1 Given the importance of assessing and improving human
Physical therapists are experts in the movement system. movement in physical therapist practice and the potential
Interventions are designed to improve movement benefits of VBMA, it is critical to know how and why
effectiveness and safety based on examination and VBMA is used, what types of VBMA are used, and what
evaluation findings.2,3 By identifying pathomechanics that factors influence VBMA use. The objectives of this study
may drive nociceptive input or overload tissues and are to (1) examine patterns of VBMA use; (2) identify
monitoring movement pattern changes throughout the barriers to and reasons for VBMA use; and (3) determine
episode of care, physical therapists address underlying demographic, clinical, and educational factors associated
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
movement dysfunction to enhance treatment outcome and with VBMA use in orthopedic physical therapist practice.
performance. Motion analysis, when coupled with a robust
clinical reasoning process, is a useful tool for clinicians to Methods
efficiently assess and improve movement. Traditionally, This was a cross-sectional observational study using a
movement has been analyzed using either simple visual survey. The Northwestern University Institutional Review
observation in the clinic or equipment-intensive, Board approved the study.
quantitative motion capture systems in a laboratory.
Although providing reliable kinematic information, the Participants
benchmark laboratory-based quantitative motion capture An e-mail invitation was sent to members of the Academy
system is neither always practical nor efficient for clinical of Orthopaedic Physical Therapy (AOPT) at the study’s
practice due to its high cost and space, equipment/ onset. Inclusion criteria were licensed physical therapists
software, and time requirements. On the other end of the practicing at least 4 h/wk treating primarily
spectrum, visual observation is easy, quick, and requires orthopedic-related injuries. Each participant gave
little to no equipment. Movement analysis by direct visual informed consent prior to taking the survey.
observation may be limited by the observer’s experience
and visual acuity and the speed of the analyzed Survey Design
movement. As joint angular velocities increase, dynamic The survey questions underwent a series of iterations to
visual acuity deteriorates.4,5 Patient fatigue or pain best capture respondents’ characteristics, behaviors, and
exacerbation related to repetitive performance of the same experience with VBMA use. The initial version was drafted
movement may also limit the use of direct visual by 2 physical therapists, each with ≥10 years of
observation. Finally, the observation is transitory in nature experience in musculoskeletal practice, and 4 Doctor of
with no record to refer to or reflect on. Thus, Physical Therapy students. Next, a survey expert at
observational analysis without video may lack accuracy Northwestern University critically reviewed and revised
and fail to detect pathological movement patterns.6,7 each question and corresponding response choices for
These limitations pose a need for a more consistent, utility, specificity, clarity, and brevity; pruned immaterial
practical, and valid measurement tool. items; and structured question order and branching. To
further reduce response bias and improve relevance and
With recent advances in smartphone/tablet video comprehensiveness, we empaneled a nationwide focus
recording capabilities (eg, capturing up to 240 frames per group of 11 orthopedic physical therapists representing
second in slow-motion video mode) and developments of different age groups, years of experience, and sexes. After
numerous smartphone/tablet apps for 2-dimensional (2-D) test-taking the survey, each focus group member provided
video-based motion analysis (VBMA), more nuanced feedback during an online discussion. Questions were
movement analysis can be performed requiring little to no further modified and arranged to improve the survey.
equipment at minimal to no cost.8 Recorded videos can be Finally, after evaluating questions and responses, an
reviewed with patients to achieve shared decision-making, experienced biostatistician built the data collection form
improve understanding and adherence, and motivate and using Research Electronic Data Capture (REDCap) tools
encourage self-management. Additionally, visual feedback hosted by Northwestern University. REDCap is a
of impaired movement patterns through recorded videos web-based application designed to support data capture
can potentially enhance patient motor learning. The and management for research.
primary physical therapist can also consult with
colleagues across the globe using such technology. The final survey contained a maximum of 18 questions
Despite the emphasis on movement in the physical across 6 pages (Appendix). Each page covered 2 to 5
therapy profession, recent development of questions. Adaptive questioning was used to reduce
smartphones/tablets/apps for VBMA, and an accumulating number and complexity depending on how participants
body of literature regarding VBMA application in responded. Using closed-ended questions, the survey
therapy, injury prevention, and sports performance,9–11 queried VBMA use frequency, types, barriers, and reasons
1760 Physical Therapy Volume 100 Number 10 2020
Video-Based Motion Analysis
for use. The survey also contained questions examining throughout the United States representing a range of age
potential predictors of use, including age, years of groups, years of experience, practice settings, and
experience as a physical therapist, number of patients certifications/degrees. Respondents were predominantly
seen per week, practice hours per week, practice setting, Doctors of Physical Therapy (340, 71.3%), practicing in
time spent with patients, frequency of delegation to private practice (222, 46.5%) or outpatient hospital-based
physical therapist assistants and physical therapy aides, (203, 42.6%) settings, and treating patients for 31 hours or
and other certificates/degrees. A free-text box for write-in more per week (329, 69.0%). The majority of respondents
answers was provided when respondents selected “other”; spent at least 45 minutes for new evaluations (329, 69.0%),
for example, respondents could select “other” when their at least 30 minutes for return visits (354, 74.2%), and did
certificates/degrees were not listed as options. Items were not delegate to physical therapist assistants (265, 55.6%)
presented in the same order for all respondents. Respon- or physical therapy aides (357, 74.8%). Additionally,
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
dents were allowed to review and change answers using a respondents reported whether they had earned any other
“back” button. It took approximately 5 to 10 minutes to certificates/degrees and were allowed to select more than
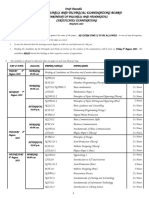
complete the survey. Those completing the survey were 1 category. The Figure shows the number of respondents
entered into a raffle for a $100 Amazon gift card. in each certificate/degree category. For example, 210
(44.0%) were board-certified orthopedic clinical specialists
Data Collection (OCS), and 143 (30.0%) did not have any
The survey invitation, consisting of a recruitment letter certificate/degree.
inviting participation, an informed consent statement, and
a short survey description, was sent electronically from Frequency of VBMA Use
the AOPT to members in January 2018. The invitation Of those who met the inclusion criteria (N = 477), 228
briefly described the study objectives and estimated time (47.8%) reported using VBMA to some extent. As shown
to complete the survey. Interested participants clicked the in Table 2, the majority of VBMA users (208/228, 91.2%)
electronic link connecting them to more detailed study reported VBMA use for only ≤25% of their caseload.
instructions and eligibility criteria. Access to the survey
was granted after selecting “yes” to informed consent to Device/Method Used to Capture VBMA
participate. No participant identifying information was In VBMA users (N = 228), most (132, 57.9%) used their
collected; thus, participation was completely anonymous. personal device to capture VBMA (Tab. 3). One hundred
Survey responses were collected on REDCap over nineteen (52.2%) reported using a single video camera on
3 months, January to March 2018. Per AOPT policy, no a tablet/phone as the primary method for capturing
follow-up survey reminders were sent. VBMA, followed by 103 (45.2%) using an app, and 6
(2.6%) using 3-dimensional motion analysis. The top 2
Data Analysis apps for VBMA were Hudl Technique (47/103, 45.6%) and
Descriptive statistics, such as number (%) and mean (SD), Coach’s Eye (23/103, 22.3%) (Tab. 3).
summarized the characteristics for the overall sample and
by VBMA use (yes vs no). To assess univariate associations Reasons for Use and Barriers
between individual factors and VBMA use, chi-squared Among VBMA users (N = 228), the commonly cited
tests were conducted for categorical variables and reasons for use included visual feedback (209, 91.7%),
independent t tests for continuous variables. When the analysis of movement (208, 91.2%), and assessment of
expected cell count was <5, Fisher’s exact tests were used progress (118, 51.8%) (Tab. 4). Of 477 respondents, the
instead. Factors with a P value ≤.20 in the univariate commonly reported barriers included lack of
comparisons were considered for inclusion in the final device/equipment (233, 48.8%), lack of space (232,
multivariable logistic regression models. Results were 48.6%), and time restraint (153, 32.1%) (Tab. 4).
reported as odds ratios (ORs) and associated 95%
confidence intervals (CIs); a 95% CI that excludes 1.0 is Factors Associated With VBMA Use
considered to be statistically significant. ORs > 1.0 Table 1 compares demographic and professional
indicated increased likelihood and <1.0 indicated factors between VBMA users and non-users. Because
decreased likelihood. All analyses were performed using age and years of experience as a physical therapist
SAS V9.4 (Cary, NC, USA). were highly correlated, only years of experience were
included in the final logistic regression models. For
other certificates/degrees, respondents could select
Results more than 1 answer; we applied hierarchical grouping to
Survey Respondents form 5 mutually exclusive subgroups.12 For example, the
A total of 567 survey responses were recorded; 477 OCS subgroup included those having only OCS (N = 163);
respondents met inclusion criteria. Demographics and the manual therapy fellowship subgroup included those
professional characteristics of respondents are earning fellowship with or without OCS or residency
summarized in Table 1. Respondents were distributed training (N = 34); the orthopedic residency subgroup
2020 Volume 100 Number 10 Physical Therapy 1761
Video-Based Motion Analysis
Table 1.
Descriptive Summary of Factors Related to Use of VBMA (Univariate Comparisons)a
Factor Total N VBMA Use (N = 228) No VBMA Use (N = 249) Pb
Mean age in years (SD) 40.6 (11.2) 43.2 (12.4) .014
Years of physical therapist practice .003
≤20 y 326 171 (75.0%) 155 (62.2%)
>20 y 151 57 (25.0%) 94 (37.8%)
Certificates/degreesc .007
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
OCS 163 79 (34.6%) 84 (33.7%)
Orthopedic residency graduate 36 24 (10.5%) 12 (4.8%)
Fellow (FAAOMPT) 34 23 (10.1%) 11 (4.4%)
Other 101 43 (18.9%) 58 (23.3%)
None 143 59 (25.9%) 84 (33.7%)
Time spent in direct patient care (h/wk) .556
4–10 29 16 (7.0%) 13 (5.2%)
11–20 45 18 (7.9%) 27 (10.8%)
21–30 74 33 (14.5%) 41 (16.5%)
31–39 184 86 (37.7%) 98 (39.4%)
≥40 145 75 (32.9%) 70 (28.1%)
Geographic region .183
Midwest 140 60 (26.3%) 80 (32.1%)
West 117 67 (29.4%) 50 (20.1%)
Northeast 100 48 (21.1%) 52 (20.9%)
Southeast 89 39 (17.1%) 50 (20.1%)
Southwest 31 14 (6.1%) 17 (6.8%)
Terminal physical therapy degree .218
DPT 340 170 (74.6%) 170 (68.3%)
MPT 72 33 (14.5%) 39 (15.7%)
PT 65 25 (11.0%) 40 (16.1%)
Practice setting .325
Private practice 222 114 (50.0%) 108 (43.4%)
Outpatient hospital-based 203 92 (40.4%) 111 (44.6%)
Otherd 52 22 (9.6%) 30 (12.0%)
Time spent with initial evaluations (min) .389
<30 25 9 (3.9%) 16 (6.4%)
30–44 123 60 (26.3%) 63 (25.3%)
45–59 244 113 (49.6%) 131 (52.6%)
≥60 85 46 (20.2%) 39 (15.7%)
Time spent with return patients (min) .300
<15 4 1 (0.4%) 3 (1.2%)
15–29 119 58 (25.4%) 61 (24.5%)
30–44 223 114 (50.0%) 109 (43.8%)
45–59 106 42 (18.4%) 64 (25.7%)
≥60 25 13 (5.7%) 12 (4.8%)
(Continued)
1762 Physical Therapy Volume 100 Number 10 2020
Video-Based Motion Analysis
Table 1.
Continued
Factor Total N VBMA Use (N = 228) No VBMA Use (N = 249) Pb
Frequency of delegation to physical .879
therapist assistants (%)
0 265 131 (57.5%) 134 (53.8%)
1–25 116 54 (23.7%) 62 (24.9%)
26–50 75 35 (15.4%) 40 (16.1%)
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
51–75 16 6 (2.6%) 10 (4.0%)
76–100 5 2 (0.9%) 3 (1.2%)
Frequency of delegation to physical .307
therapy aides (%)
0 357 162 (71.1%) 195 (78.3%)
1–25 94 51 (22.4%) 43 (17.3%)
26–50 20 12 (5.3%) 8 (3.2%)
>50 6 3 (1.3%) 3 (1.2%)
a
FAAOMPT = Fellow of American Academy of Orthopaedic Manual Physical Therapists; MPT = Master of Physical Therapy; OCS = board-certified orthopaedic
clinical specialist; DPT = Doctor of Physical Therapy; PT = Physical Therapy; VBMA = video-based motion analysis.
b
P values comparing VBMA use ≤ .20 are bolded.
c
Because respondents could select more than 1 answer, we applied hierarchical grouping to form 5 mutually exclusive subgroups. The OCS subgroup
included those having only OCS; the manual therapy fellowship subgroup included those earning fellowship with or without OCS or residency training;
the orthopedic residency subgroup included those completing residency training with or without OCS or fellowship; the “other” subgroup consisted of those
with certificates/degrees other than OCS, fellowship, or residency; and the “none” subgroup comprised those without any certificates/degrees.
d
“Other” included practice settings of state/federal government, workplace/occupational environment, wellness/prevention/sports/fitness, and research center.
Figure.
The number of respondents in each certificate/degree category (N = 477). Respondents may select ≥1 category. ATC = certified athletic
trainer; DSc = Doctor of Science; FAAOMPT = Fellow of American Academy of Orthopaedic Manual Physical Therapists; MDT = mechanical
diagnosis and therapy; OCS = board-certified orthopaedic clinical specialist; SCS = board-certified sports clinical specialist.
2020 Volume 100 Number 10 Physical Therapy 1763
Video-Based Motion Analysis
Table 2.
Percentage of Physical Therapist Caseload Using VBMAa
Caseload VBMA Used Respondents (N = 477)
0% 249 (52.2%)
1–25% 208 (43.6%)
26–50% 17 (3.6%)
51–75% 2 (0.004%)
76–100% 1 (0.002%)
a
VBMA = video-based motion analysis.
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
Table 3.
Devices and Apps Used to Capture VBMAa
Device Used to Capture VBMA Respondents Who Use VBMA (N = 228)
Personal device 132 (57.9%)
Patient device 98 (43.0%)
Clinic-issued device 90 (39.5%)
Other 9 (4.0%)
App Used to Capture VBMA b
Respondents Who Use App (N = 103)
Hudl Technique 47 (45.6%)
Coach’s Eye 23 (22.3%)
Dartfish 15 (14.6%)
Slowmo 6 (5.8%)
KCapture 2 (1.9%)
CMV 2 (1.9%)
V1 Golf 1 (1.0%)
Runmatic 1 (1.0%)
Other 6 (5.8%)
a
Respondents were able to choose ≥1 answer. VBMA = video-based motion analysis.
b
Manufacturer information: Hudl Technique (Agile Sports Technologies Inc, Lincoln, NE, USA; Coach’s Eye (TechSmith Corporation, Okemos, MI, USA;
Dartfish (Alpharetta, GA, USA); KCapture (video-capturing app); CMV (CoachMyVideo, https://www.coachmyvideo.mobi); V1 Golf (V1 Sports, Novi, MI,
USA); Runmatic (https://apps.apple.com/us/app/runmatic/id1075902287).
included those completing residency training with or therapy aides, practice setting, or terminal physical
without OCS or fellowship (N = 36); the “other” subgroup therapy degree were not associated with VBMA use.
consisted of those with certificates/degrees other than
OCS, fellowship, or residency (N = 101); and the “none”
subgroup comprised those without any certificates/degrees Discussion
(N = 143). As shown in Table 5, physical therapists with To our knowledge, this is the first study to examine
≤20 years of experience, graduates from an orthopedic descriptive and predictive factors associated with VBMA
residency program (vs physical therapists without use in physical therapy practice. Results show that more
any other certificates/degrees), Fellows of the American than 50% of orthopedic physical therapists do not use
Academy of Orthopaedic Manual Physical Therapists (vs VBMA. Among VBMA users, approximately 90% use it for
physical therapists without any other certificates/degrees), 25% or less of their caseload. The limited use of VBMA
and those from the West geographic region were among orthopedic physical therapists may be attributed to
each more likely to use VBMA. Other certificates/degrees, a number of factors. As highlighted in Table 4, lack of
weekly hours in patient care, patients seen per equipment, lack of space, time restraint, cost, and patient
week, time spent with patients for initial or return visits, privacy were among the top 5 barriers to using VBMA in
delegation to physical therapist assistants or physical orthopedic practice.
1764 Physical Therapy Volume 100 Number 10 2020
Video-Based Motion Analysis
Table 4.
Reasons for and Barriers to Using VBMAa
Reasons for Using Respondents Who Use VBMA (N = 228)
Visual feedback for patient education 209 (91.7%)
Analysis of movement 208 (91.2%)
Assessment of progress 118 (51.8%)
Quantification of movement 82 (36.0%)
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
Other 10 (2.1%)
Barriers to Using Respondents (N = 477)
Lack device/equipment 233 (48.8%)
Lack of space 232 (48.6%)
Time restraint 153 (32.1%)
Cost 137 (28.7%)
Other 104 (21.8%)
Patient privacy 93 (19.5%)
No barriers 62 (13.0%)
Difficult to use 29 (6.1%)
Do not find it benefits patients 24 (5.0%)
Unfamiliar 19 (4.0%)
Not allowed 18 (3.8%)
Lack internet access 11 (2.3%)
a
Respondents were able to choose ≥1 answer. VBMA = video-based motion analysis.
Table 5.
Factors Associated with Use of VBMA: Multivariate Logistic Regressiona
Factor Odds ratio 95% CI Pb
Physical therapist experience
≤20 vs >20 y as physical therapist 1.83 1.21–2.76 .004
Certificates or advanced degrees vs no certificates or advanced degrees
OCS 1.34 0.84–2.12 .217
Orthopedic residency graduate 2.49 1.14–5.43 .022
Fellow (FAAOMPT) 2.97 1.32–6.66 .008
Other certificates 1.19 0.70–2.02 .514
Geographic region
West vs other regions 1.66 1.07–2.56 .023
a
FAAOMPT = Fellow of American Academy of Orthopaedic Manual Physical Therapists; OCS = board-certified orthopedic clinical specialist; VBMA = video-based
motion analysis.
b
Factors with P ≤ .20 in the univariate comparisons (see Table 1) were included in the multivariate logistic regression models.
2020 Volume 100 Number 10 Physical Therapy 1765
Video-Based Motion Analysis
Barriers to Performing VBMA some may argue that observation without technology
Lack of equipment was the most common barrier to suffices to identify pathomechanics, it could be
performing VBMA. For those who do not want to use a challenging for clinicians to identify variables contributing
personal device, “lack of equipment” could be perceived to the movement problem, especially during fast
as a barrier. Some respondents may not have access to a movements. VBMA has the advantages of repeated
clinic-owned device (eg, phone or tablet) to capture video. viewings, slowed motion analysis, zooming on a specific
Finally, free text comments suggested that the inability to region of interest, still frame at a particular movement
upload video to Electronic Medical Record (EMR) event, and side-by-side comparison with another
discourages VBMA use. This could be interpreted as “lack recording. Visual feedback of movement (real-time or
of equipment.” Lack of space and time restraint were post-performance) provided to the patient may serve as
frequently cited barriers. Tasks that require a larger area, powerful immediate input to improve movement
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
such as sprinting, may be difficult to capture in smaller execution and performance and can be universally
clinics. Recording long-distance running on a treadmill applied to patients who move at all speeds.18 ,19 Over 50%
could consume valuable patient encounter time. To of respondents selected assessment of progress as a
overcome these barriers, patients could share videos reason to use VBMA. Anecdotally, we have found this to
captured outside clinic to maximize efficiency. Recording be valuable in tracking movement pattern change over
and analyzing movement may initially require more time, time, from both the clinician’s and patient’s perspective.
but it will enable clinicians to quickly identify key Visual feedback of improvement may potentially further
pathomechanics and may save time and cost and reduce facilitate a patient’s engagement and treatment adherence.
patient visits. Nearly 30% of respondents selected cost as a
barrier. While most VBMA apps are free for basic
Device, Methods for Capturing VBMA
packages, some, as part of their premium packages,
A single camera on a smartphone/tablet was more
require monthly subscription fees. Concerns over lack of
commonly used than an app or 3-dimensional motion
insurance reimbursement and uncertainty about
analysis in clinical practice. This is expected given that
VBMA-related Current Procedural Terminology coding
most smartphones/tablets come with preinstalled video
may also be perceived as a cost-related barrier. Around
cameras. Although some of the VBMA apps are free, they
20% of physical therapists reported patient privacy as a
require extra steps to download and additional time to
barrier. Capturing information by smartphones/tablets
learn. They also may occupy a large amount of storage on
poses a risk for confidentiality and Health Insurance
devices. These drawbacks may discourage some physical
Portability and Accountability Act violations. In a survey of
therapists from using apps. Hudl Technique and Coach’s
dermatologists, 30% reported storing patient photographs
Eye were the 2 most frequently used VBMA apps. Both
on personal smartphones; 48% of these were not secured
are downloadable for Android and iOS and incorporate
or encrypted.13 Unintentional privacy breaches could also
features of video playback up to 240 frames per second;
occur when other patients’ or staffs’ voices or images are
slowed motion at one-half, one-quarter, and one-eighth
captured in the recording without knowledge or consent.
speeds; angle and line drawings; and side-by-side
Care must be taken to document consent and record only
comparison of pre- and post-videos. The basic version of
what is necessary. Future policies and guidelines relating
Hudl Technique is free, while a fee applies to Coach’s
to patient consent; recording procedures; recording device
Eye.8 ,15 ,20 ,21 Interestingly, the majority of our respondents
use; data storage, security, and encryption; and integration
used their own personal devices to capture video, likely
with EMR should be developed to ensure confidentiality
due to familiarity with and access to one’s own device at
and privacy protection. Approximately 6% reported
any time. In light of potential confidentiality and Health
“difficult to use” and 4% reported “unfamiliar” as barriers
Insurance Portability and Accountability Act violations,
to VBMA use. It is unknown how motion analysis is
physical therapists are advised to obtain consent prior to
incorporated in physical therapy curriculum. If students
capturing patient information on their personal devices.
are not exposed to a framework of systematic analysis of
Alternatively, recording on patients’ devices could
movement and VBMA, they may find it difficult to use in
potentially mitigate this risk but at the expense of limited
clinical practice. Physical therapy educators may consider
access for the clinician.
integrating frameworks for structured movement analysis14
or VBMA application10,15,16 into their curriculum.
Factors Associated With VBMA Use
Those with 20 years or less experience as a physical
Facilitators to Performing VBMA therapist were more likely to use VBMA. One possible
The top reasons for VBMA use were visual feedback for explanation is that younger individuals are more familiar
patient education (91.7%) and analysis of movement with recent advances in digital technology and
(91.2%). A recent systematic review concluded that visual smartphone use. This is consistent with what has been
feedback, in conjunction with other methods of feedback reported in medicine. Medical students (85%) and
and intervention, should be incorporated when addressing residents (95%) used their smartphones for
injury-contributing pathomechanics for runners.17 While communicating with other medical staff and for quick
1766 Physical Therapy Volume 100 Number 10 2020
Video-Based Motion Analysis
access to information more frequently than their faculty orthopedic clinical practice. Recall bias could have
mentors (65%).22 Additionally, less experienced physical occurred when responding to survey items. At the time of
therapists may be more inclined to rely on survey distribution in January 2018, there were
smart/electronic technologies for accuracy given their approximately 19,000 AOPT members. Due to the
limited experience and confidence in movement electronic distribution methods and anonymous nature of
analysis.6,23,24 Additional training in orthopedic residency the survey, we are unable to account for e-mails that were
or fellowship in orthopaedic manual physical therapy undelivered, unopened, or received in duplicate by
each increased the likelihood of use. These individuals members. Further, we were unable to account for
may have been introduced to VBMA during their members who opted out of e-mail communications. Thus,
structured advanced training. In theory, pursuing a true response rate is undetermined. However, the
post-graduate training may signal interest and number of recorded returns and sample characteristics in
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
commitment to expert practice, in part characterized by a our study are comparable with those in a recent survey
central focus on movement assessment linked to patient that employed the same method of e-mail invitation to
function and by a clinical reasoning process that is AOPT members.31 No identifying information was
embedded in a collaborative, problem-solving venture collected regarding each respondent, which may have
with the patient.25 This focus on patient-centered allowed some to access and respond to the survey more
movement analysis and use of technology to engage than once if they wished to do so.
patients may have explained why those with advanced
training were more likely to use VBMA. This survey is, to our knowledge, the first to describe the
use of VBMA in orthopedic physical therapist practice in
Compared with the rest of the United States, those from the United States. Results indicate that the majority of
the West region were more likely to use VBMA. Regional orthopedic physical therapists do not use VBMA in clinical
variance in health care practice is frequently observed.26 practice. In VBMA users, approximately 90% utilize it for
Given that western states have statistically higher 25% or less of their caseload. Those practicing for 20 years
smartphone and tablet usage rates than the national or less or those from the West region are more likely to
average,27 it is plausible that clinicians in this region are use VBMA. Being Fellows of the American Academy of
more attuned and open to adopting available technology Orthopaedic Manual Physical Therapy or orthopedic
that may enhance clinical practice. residency graduates each predicted VBMA use. Future
research should be directed toward better assessing
Recent advances in smartphone/tablet video recording reliability and validity of VBMA use through
capabilities and relative ease of capturing movement smartphones/tablets/apps; investigating whether VBMA is
kinematics using automated apps/software have motivated superior to commonly used clinical assessment tools (eg,
renewed interest in examining the reliability and validity goniometry); developing educational programs of VBMA
of using 2-D video analysis to assess functional tasks. application for clinicians; and examining whether the use
Moderate to excellent intra- and inter-rater reliability has of VBMA enhances treatment outcomes. Data security,
been reported when analyzing lower extremity kinematics patient confidentiality, and integration into EMR should
during functional tasks, such as walking, running, also be addressed.
squatting, and landing tasks.9,28– 30 Investigations into the
validity of 2-D video analysis have shown mixed results in
two recent systematic reviews9,29 reporting very low to
low article quality.9 Both reviews, nonetheless, Author Contributions and Acknowledgments
emphasized that 2-D analysis could be informative in
Concept/idea/research design: C.P. Hensley, D. Millican,
identifying those with pathomechanics at risk for injury.
N. Hamilton, J. Lee, A.H. Chang
Writing: C.P. Hensley, D. Millican, N. Hamilton, J. Lee, A.H. Chang
Several limitations to this study should be recognized. We Data collection: C.P. Hensley, D. Millican, N. Hamilton, A. Yang,
made every attempt to ensure clarity and accurate A.H. Chang
interpretation of survey items by iterative survey Data analysis: D. Millican, A. Yang, J. Lee, A.H. Chang
development/refinement that involved experts and Project management: C.P. Hensley, A.H. Chang
stakeholders (eg, 11 nationwide practicing orthopedic Consultation (including review of manuscript before submitting):
physical therapists). However, the final survey A. Yang
questionnaire was not further pilot tested; varied The authors thank the survey respondents and Dr Stephen Reischl
individual interpretation of questions/answers may exist. for providing feedback to improve the manuscript.
All survey respondents were AOPT members; among
them, 44% were OCSs. This may limit generalizability of
our results to other non-AOPT members and/or those Ethics Approval
without clinical specialization that provide care for
patients with musculoskeletal dysfunction. It is possible This study was approved by the Institutional Review Board at
that these findings may overestimate the use of VBMA in Northwestern University.
2020 Volume 100 Number 10 Physical Therapy 1767
Video-Based Motion Analysis
Funding 19 Abujaber S, Pozzi F, Zeni J Jr. Influence of weight bearing
visual feedback on movement symmetry during sit to stand
There are no funders for this study. task. Clin Biomech (Bristol, Avon). 2017;47:110–116.
20 Hudltechnique. https://www.hudl.com/products/technique.
Disclosures Accessed May 7, 2020.
21 Coach’s Eye. https://www.coachseye.com/product/coachseye?
The authors completed the ICMJE Form for Disclosure of Potential package=individual. Accessed May 7, 2020.
Conflicts of Interest and reported no conflicts of interest. 22 Wallace S, Clark M, White J. ‘It’s on my iPhone’: attitudes to
the use of mobile computing devices in medical education, a
DOI: 10.1093/ptj/pzaa125 mixed-methods study. BMJ Open. 2012;2:e001099.
23 Viehweger E, Zurcher Pfund L, Helix M et al. Influence of
clinical and gait analysis experience on reliability of
observational gait analysis (Edinburgh gait score reliability).
Ann Phys Rehabil Med. 2010;53:535–546.
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
References 24 Toro B, Nester CJ, Farren PC. Inter- and intraobserver
repeatability of the Salford gait tool: an observation-based
1 American Physical Therapy Association. Vision statement for clinical gait assessment tool. Arch Phys Med Rehabil.
the physical therapy profession and guiding principles to 2007;88:328–332.
achieve the vision. https://www.apta.org/vision/. Updated
September 25, 2019. Accessed May 7, 2020. 25 Jensen GM, Gwyer J, Shepard KF. Expert practice in
physical therapy. Phys Ther. 2000;80:28–43; discussion
2 Sahrmann SA. The human movement system: our professional 44–52.
identity. Phys Ther. 2014;94:1034–1042.
26 Deyo RA, Mirza SK. Trends and variations in the use of spine
3 Voight ML, Hoogenboom BJ. What is the movement system surgery. Clin Orthop Relat Res. 2006;443:139–146.
and why is it important? Int J Sports Phys Ther. 2017;12:1–2.
27 Ryan C. Computer and internet usage in the United States:
4 Brown B. Dynamic visual acuity, eye movements and 2016. American Community Survey Reports website. https://
peripheral acuity for moving targets. Vision Res. www.census.gov/content/dam/Census/library/
1972;12:305–321. publications/2018/acs/ACS-39.pdf. 2017. Accessed May 7,
5 Aznar-Casanova JA QL, Sinnet S. The effects of drift and 2020.
displacement motion on dynamic visual acuity. Psicologica. 28 Harris-Hayes M, Steger-May K, Koh C, Royer NK, Graci V,
2005;26:75–92. Salsich GB. Classification of lower extremity movement
6 Toro B NC, Farren PC. A review of observational gait patterns based on visual assessment: reliability and
assessment in clinical practice. Physiother Theory Pract. correlation with 2-dimensional video analysis. J Athl Train.
2003;19:137–149. 2014;49:304–310.
7 Ekegren CL, Miller WC, Celebrini RG, Eng JJ, Macintyre DL. 29 Lopes TJA, Ferrari D, Ioannidis J, Simic M, Micolis de Azevedo
Reliability and validity of observational risk screening in F, Pappas E. Reliability and validity of frontal plane
evaluating dynamic knee valgus. J Orthop Sports Phys Ther. kinematics of the trunk and lower extremity measured with
2009;39:665–674. 2-dimensional cameras during athletic tasks: a systematic
review with meta-analysis. J Orthop Sports Phys Ther.
8 Mills K. Motion analysis in the clinic: there’s an app for that. J 2018;48:812–822.
Physiother. 2015;61:49–50.
30 Pipkin A, Kotecki K, Hetzel S, Heiderscheit B. Reliability of a
9 Parks MT, Wang Z, Siu KC. Current low-cost video-based qualitative video analysis for running. J Orthop Sports Phys
motion analysis options for clinical rehabilitation: a systematic Ther. 2016;46:556–561.
review. Phys Ther. 2019;99:1405–1425.
31 Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ.
10 Souza RB. An evidence-based videotaped running Rehabilitation practice patterns following anterior cruciate
biomechanics analysis. Phys Med Rehabil Clin N Am. ligament reconstruction: a survey of physical therapists. J
2016;27:217–236. Orthop Sports Phys Ther. 2018;48:801–811.
11 Knudson DV. Qualitative Diagnosis of Human Movement:
Improving Performance in Sport and Exercise. 3rd ed.
Champaign, IL, USA: Human Kinetics, Inc; 2013.
Appendix.
12 Ward JH. Hierarchical grouping to optimize an objective
function. J Am Stat Assoc. 1963;58:236–244. Survey
13 Anyanwu CO, Lipoff JB. Smartphones, photography, and Thank you for agreeing to take part in this important survey
security in dermatology. J Am Acad Dermatol. regarding physical therapist use of video-based motion analysis
2015;72:193–195. in clinical practice. This survey should take 5–10 minutes to
14 Hedman LD, Quinn L, Gill-Body K et al. White paper: complete. All the answers you provide will be completely
movement system diagnoses in neurologic physical therapy. J
Neurol Phys Ther. 2018;42:110–117. anonymous.
15 Weiler R. Ubersense coach app for sport medicine? Slow
motion video analysis (mobile app user guide). Br J Sports Section 1
Med. 2016;50:255–256.
1) Do you currently see patients at least 4 hours per
16 Finkbiner MJ, Gaina KM, McRandall MC et al. Video
movement analysis using smartphones (ViMAS): a pilot study. week?
J Vis Exp. 2017;121:e54659.
• Yes
17 Agresta C, Brown A. Gait retraining for injured and • No
healthy runners using augmented feedback: a systematic
literature review. J Orthop Sports Phys Ther. 2015;45:
576–584. 2) Are you a licensed physical therapist?
18 Millington PJ, Myklebust BM, Shambes GM. Biomechanical • Yes
analysis of the sit-to-stand motion in elderly persons. Arch • No
Phys Med Rehabil. 1992;73:609–617.
1768 Physical Therapy Volume 100 Number 10 2020
Video-Based Motion Analysis
3) Do most of your patients have orthopedic and/or • Lack of space availability
sports-related injury? • Time restraint
• Unfamiliar with the use of video-based motion
• Yes
• No analysis
• Other (please specify)
Section 2
8) What is the primary method you use to perform
4) Approximately how many patients do you see per video-based motion analysis in your clinical practice?
week? (Check all that apply)
• Between 1–10
• • Single video camera, smartphone, tablet, other video
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
Between 11–25
• Between 26–40 method
• • App on smartphone/tablet
Between 41–59
• • 3d motion analysis cameras
More than 60
8b) (If answered B to 8) What video-based motion analysis app
5) How many hours per week do you provide direct
do you use most frequently?
patient care?
• Between 4–10
• Video-based Motion Analysis Applications (Apps): Apps available
Between 11–20
• for android, iPhone, and iPad that record video and still frames to
Between 21–30
• assist with movement analysis using various features of
Between 31–39
• frequency, timing, angles, posture grids, Borg scales, and slow
40 or more
motion. Examples include Hudl/Technique, Coach’s Eye, Dartfish
6) What percentage of your patient caseload do you use Express, and PostureScreen.
video-based motion analysis in clinical practice?
• Hudl/Technique
• 0% • Sports Motion Analyzer HD
• 1%–25% • Coach’s Eye—Video Analysis
• 26%–50% • Dartfish Express
• 51%–75% • PostureScreen
• 76%–100% • VStrator
• KCapture
6b) (If response to 6 was other than 0%) Which of the following • SKLZ Cam
devices do you use to capture video-based motion analysis in • Slowmo
clinical practice? (Select all that apply) • CMV—Slow Frame Video Analysis
• Simi Move
• • Coach Video Analyzer
Your own personal device
• • V1 Golf—2D video
A hospital/clinic-issued device
• • Runmatic
Patient device
• • Other (please list)
Other (free text)
9) What barriers, if any, keep you from using
7) What barriers, if any, keep you from using video-based motion ANALYSIS APPS in your clinical
video-based motion ANALYSIS in your clinical practice? (Choose all that apply).
practice? (Select all that apply).
• No barriers to use • No barriers to use
• Cost • Cost
• Difficult to use • Difficult to use
• Discouraged/not allowed in clinic by • Discouraged/not allowed in clinic by
supervisor/manager/boss/institution supervisor/manager/boss/institution
• Do not find that it benefits me or my patients • Do not find that it benefits me or my patients
• Lack internet access • Lack internet access
• Lack of equipment/device to use video-based • Lack of equipment/device to use video-based
motion analysis motion analysis
• Patient privacy/lack of patient consent/data security • Patient privacy/private room
2020 Volume 100 Number 10 Physical Therapy 1769
Video-Based Motion Analysis
• Lack of patient consent or others in the clinic • 0%
• Time restraint • 1–25%
• Unfamiliar with the use of video-based motion • 26–50%
analysis • 51–75%
• Other (please specify) • 76–100%
10) How do you use video-based motion-analysis in your 13b) What percentage of your patient caseload do you delegate to
practice? Select all that apply. physical therapy AIDES?
• Analysis/evaluation of movement • 0%
• Assessment of progress • 1–25%
Downloaded from https://academic.oup.com/ptj/article/100/10/1759/5875771 by guest on 02 February 2023
• Visual feedback for patient education in clinic • 26–50%
and/or at home • 51–75%
• Quantification of movement patterns (ie, knee • 76–100%
flexion ROM during a squat)
• Other (please specify)
14) What is your current age?
15) What is the primary state you practice in?
11) What is your primary practice setting? 16) How many years have you been working as a
licensed physical therapist?
• Outpatient hospital-based clinic
• Private practice • Under 5 years
• Wellness/Prevention/Sports/Fitness • 5–10 years
• Workplace, or Other Occupational Environments • 11–15 years
• State/Federal Government • 16–20 years
• Research Center • Over 20 years
• Other
17) Please list any additional certifications/education you
12) During an initial evaluation, how much time (on currently hold (ie, board certification, fellow, manual
average) do you spend with a patient? therapy, aquatics, myofascial release, kinesiotape,
etc.) Select all that apply.
• Less than 30 minutes • None
• 30–44 minutes • OCS
• 45–59 minutes • SCS
• 60 minutes or more • FAAOMPT
• Other APTA board certification
13) During return visits, how much time (on average) do • Graduated from APTA orthopedic residency program
you spend one-on-one (not including time with • Graduated from APTA sports residency program
physical therapy assistant or aide) with a • PhD
patient? • DHS
• DsC
• • ATC
15 minutes or less •
• 16–29 minutes MDT
• • Other free text
30–44 minutes
• 45–59 minutes
• 60 minutes or more 18) What is your terminal physical therapy degree?
13a) What percentage of your patient caseload do you delegate to
• PT
physical therapy ASSISTANTS?
• MPT
• DPT
1770 Physical Therapy Volume 100 Number 10 2020
You might also like
- Radiomics and Its Clinical Application: Artificial Intelligence and Medical Big DataFrom EverandRadiomics and Its Clinical Application: Artificial Intelligence and Medical Big DataNo ratings yet
- Articulo FisioterapiaDocument10 pagesArticulo FisioterapiaMonica LopezNo ratings yet
- Artificial Intelligence Will Soon Change The Landscape of Medical PhysicsDocument3 pagesArtificial Intelligence Will Soon Change The Landscape of Medical Physicsxiwevi4103No ratings yet
- 2019 - Zhou - Caregiver-Delivered Stroke Rehabilitation in Rural ChinaDocument6 pages2019 - Zhou - Caregiver-Delivered Stroke Rehabilitation in Rural ChinaWarsi MaryatiNo ratings yet
- Graham 2006Document18 pagesGraham 2006Sii Odong OdongNo ratings yet
- Teori-Teori Perubahan PerilakuDocument13 pagesTeori-Teori Perubahan PerilakuihsanNo ratings yet
- Stroke Disability and Physiotherapy Interventions: A Quantitative Evaluation of Physiotherapy Treatment Approaches' in ZambiaDocument9 pagesStroke Disability and Physiotherapy Interventions: A Quantitative Evaluation of Physiotherapy Treatment Approaches' in ZambiaPaulomds1991No ratings yet
- A Study to Assess the Effectiveness of Structured Teaching Programme on Knowledge Regarding Body Mechanics in Reducing Low Back Pain Among Staff Nurse at Selected Department of Sharda Hospital of Greater Noida, Uttar PradeshDocument7 pagesA Study to Assess the Effectiveness of Structured Teaching Programme on Knowledge Regarding Body Mechanics in Reducing Low Back Pain Among Staff Nurse at Selected Department of Sharda Hospital of Greater Noida, Uttar PradeshInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Physical Therapy Following Cervical Spine Surgery For Degenerative Spine Disorders: A Systematic ReviewDocument17 pagesThe Impact of Physical Therapy Following Cervical Spine Surgery For Degenerative Spine Disorders: A Systematic ReviewKyle RobinNo ratings yet
- Ethical AnalysisDocument4 pagesEthical Analysisapi-520841770No ratings yet
- SkjaervenoneDocument16 pagesSkjaervenonePrincess Edelweiss CorpuzNo ratings yet
- Interventions Used For Rehabilitation and Prevention of Patellar Tendinopathy in Athletes A Survey of Brazilian Sports Physical TherapistsDocument8 pagesInterventions Used For Rehabilitation and Prevention of Patellar Tendinopathy in Athletes A Survey of Brazilian Sports Physical TherapistsRonny Araya AbarcaNo ratings yet
- Administrative or Educational Medicine: ISPRM - June 12-16, 2011, San Juan, Puerto RicoDocument157 pagesAdministrative or Educational Medicine: ISPRM - June 12-16, 2011, San Juan, Puerto RicoAugusto FuscoNo ratings yet
- PTJ 1383Document14 pagesPTJ 1383marcus souzaNo ratings yet
- Complementary Therapies in MedicineDocument8 pagesComplementary Therapies in Medicinekhadesakshi55No ratings yet
- Attitudes and Barriers Towards Continuing Professional Development Among Physiotherapists in South-Eastern NigeriaDocument9 pagesAttitudes and Barriers Towards Continuing Professional Development Among Physiotherapists in South-Eastern Nigeriaangenicanor7No ratings yet
- The Clinical Implementation of Pain Neuroscience Education: A Survey StudyDocument13 pagesThe Clinical Implementation of Pain Neuroscience Education: A Survey Studycookiepower54321No ratings yet
- Physical Function in Hospice Patients and Physiotherapy Interventions: A Profile of Hospice PhysiotherapyDocument8 pagesPhysical Function in Hospice Patients and Physiotherapy Interventions: A Profile of Hospice PhysiotherapyAnggita Setya LudtianingmaNo ratings yet
- 0849BA768880Document9 pages0849BA768880angenicanor7No ratings yet
- Pzaa 180Document10 pagesPzaa 180Ajeeta KulkarniNo ratings yet
- Moss 2009Document7 pagesMoss 2009Natalia López Aliaga UndaNo ratings yet
- Morley PT Resume 5Document3 pagesMorley PT Resume 5api-422030113No ratings yet
- Critical Appraisal - Research and Evidence: Maisie Sheahan (21215414)Document5 pagesCritical Appraisal - Research and Evidence: Maisie Sheahan (21215414)Jan MackeyNo ratings yet
- An Online Survey of NursingDocument10 pagesAn Online Survey of NursingwilmaNo ratings yet
- Effects of Distraction On Children's Pain and Distress During Medical Procedures A Meta-AnalysisDocument4 pagesEffects of Distraction On Children's Pain and Distress During Medical Procedures A Meta-AnalysisMiguel TuriniNo ratings yet
- Saudi SurveyDocument12 pagesSaudi SurveyNaveen KumarNo ratings yet
- PTJ 20080139Document13 pagesPTJ 20080139Martina SimangunsongNo ratings yet
- Fuentes 2010Document22 pagesFuentes 2010RodrigoAndresVenegasGodoyNo ratings yet
- Bennell. JAMA, 2014Document11 pagesBennell. JAMA, 2014Santiago CerfogliNo ratings yet
- Intensive & Critical Care Nursing: Research ArticleDocument7 pagesIntensive & Critical Care Nursing: Research ArticleEviNo ratings yet
- Knowledge Attitudes and Barriers Towards Evidence Ba - 2017 - Hong Kong PhysioDocument9 pagesKnowledge Attitudes and Barriers Towards Evidence Ba - 2017 - Hong Kong PhysioAnuj ShandilyaNo ratings yet
- Management of Plantar Heel Pain. A Best Practice Guide Informed by A Systematic Review, Expert Clinical Reasoning and Patient ValuesDocument14 pagesManagement of Plantar Heel Pain. A Best Practice Guide Informed by A Systematic Review, Expert Clinical Reasoning and Patient ValuesJesusNavarrete97No ratings yet
- A Systematic Review of Treatments For Mild Traumatic Brain InjuryDocument3 pagesA Systematic Review of Treatments For Mild Traumatic Brain InjurySergio Machado NeurocientistaNo ratings yet
- Listening Is Therapy Patient Interviewing From A Pain Science PerspectiveDocument13 pagesListening Is Therapy Patient Interviewing From A Pain Science PerspectiveDuvan CarvajalNo ratings yet
- Critical Appraisal of EvidenceDocument5 pagesCritical Appraisal of EvidenceLADY JOWAHER ALLASNo ratings yet
- Evaluation of Psychiatric Morbidity in The Community Through Application of Schedule For Clinical Assessment in Neuropsychiatry (Scan)Document6 pagesEvaluation of Psychiatric Morbidity in The Community Through Application of Schedule For Clinical Assessment in Neuropsychiatry (Scan)Dhrubajyoti BhuyanNo ratings yet
- Management of Plantar Heel Pain: A Best Practice Guide Informed by A Systematic Review, Expert Clinical Reasoning and Patient ValuesDocument14 pagesManagement of Plantar Heel Pain: A Best Practice Guide Informed by A Systematic Review, Expert Clinical Reasoning and Patient ValuesMaximiliano LabraNo ratings yet
- FMS Squat Assessment and 2D Video Motion Analysis As Screening inDocument12 pagesFMS Squat Assessment and 2D Video Motion Analysis As Screening inAgus TinaNo ratings yet
- AAEMS Webinar 5 June 2020Document1 pageAAEMS Webinar 5 June 2020John DoeNo ratings yet
- 5-2016 42 Ijmah GoniometeryDocument7 pages5-2016 42 Ijmah GoniometeryNatalie AcostaNo ratings yet
- Manual Therapy: Neil Langridge, Lisa Roberts, Catherine PopeDocument6 pagesManual Therapy: Neil Langridge, Lisa Roberts, Catherine PopeVizaNo ratings yet
- Physical Therapy in Sport: Literature ReviewDocument9 pagesPhysical Therapy in Sport: Literature ReviewPrincess Dianna SulitNo ratings yet
- Documento 4aDocument8 pagesDocumento 4aBelen SozaNo ratings yet
- Joseph Michael Pellerito, JR, MS, OTR Eds Driver RehabilitationDocument671 pagesJoseph Michael Pellerito, JR, MS, OTR Eds Driver Rehabilitationsarawu9911No ratings yet
- Asian Nursing ResearchDocument7 pagesAsian Nursing ResearchWayan Dyego SatyawanNo ratings yet
- Jsaa 086Document11 pagesJsaa 086Elías Coreas SotoNo ratings yet
- OT in The ICU. Revision de Mas de 200 ArticulosDocument8 pagesOT in The ICU. Revision de Mas de 200 ArticulosFlorencia Yael ItovichNo ratings yet
- Journal Homepage: - : IntroductionDocument8 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- BMC Pediatrics: Effectiveness of Physical Therapy Interventions For Children With Cerebral Palsy: A Systematic ReviewDocument10 pagesBMC Pediatrics: Effectiveness of Physical Therapy Interventions For Children With Cerebral Palsy: A Systematic ReviewERICKNo ratings yet
- Jiwa 1Document10 pagesJiwa 1Sa'adahNo ratings yet
- Caru2020 Article ChildrenSPhysicalActivityBehavDocument12 pagesCaru2020 Article ChildrenSPhysicalActivityBehavkaterinaNo ratings yet
- Fbe - EcuadorDocument7 pagesFbe - EcuadorJoselyn VelasquezNo ratings yet
- Evaluating Preferences For Online Psychological Interventions - 2023 - PsychiatDocument10 pagesEvaluating Preferences For Online Psychological Interventions - 2023 - Psychiattito syahjihadNo ratings yet
- Opioid Analgesics: Symposium On Pain MedicineDocument12 pagesOpioid Analgesics: Symposium On Pain Medicineyunica simanjuntakNo ratings yet
- Manipulation and Mobilization For Treating Chronic Low Back Pain: A Systematic Review and Meta-AnalysisDocument14 pagesManipulation and Mobilization For Treating Chronic Low Back Pain: A Systematic Review and Meta-AnalysisradenbagasNo ratings yet
- K Rivet Amico CV May 20 2018 v2Document27 pagesK Rivet Amico CV May 20 2018 v2api-424535213No ratings yet
- RH Del MS en ACV PDFDocument12 pagesRH Del MS en ACV PDFDiego VolattiNo ratings yet
- Physiological ParametersDocument4 pagesPhysiological ParametersBryan NguyenNo ratings yet
- 9635 34327 1 PBDocument2 pages9635 34327 1 PBTheepan ThuraiNo ratings yet
- Article 7Document9 pagesArticle 7Hamza DibNo ratings yet
- LBP2Document2 pagesLBP2Agus TinaNo ratings yet
- CTS1Document3 pagesCTS1Agus TinaNo ratings yet
- CRS 1Document3 pagesCRS 1Agus TinaNo ratings yet
- Lower Extremity Strengthening - Home Exercise Program: 1. Ankle PumpsDocument3 pagesLower Extremity Strengthening - Home Exercise Program: 1. Ankle PumpsAgus TinaNo ratings yet
- FMS Squat Assessment and 2D Video Motion Analysis As Screening inDocument12 pagesFMS Squat Assessment and 2D Video Motion Analysis As Screening inAgus TinaNo ratings yet
- Reliability and Validity of Standing Balance Measurements With A Motion Analysis SystemDocument8 pagesReliability and Validity of Standing Balance Measurements With A Motion Analysis SystemAgus TinaNo ratings yet
- Rajat Chawla: About MeDocument2 pagesRajat Chawla: About MeRajat ChawlaNo ratings yet
- Lexical AnalysisDocument38 pagesLexical Analysissaeed khanNo ratings yet
- Annual Report 2020 PDFDocument165 pagesAnnual Report 2020 PDFNRNo ratings yet
- Ansible TutorialDocument39 pagesAnsible Tutorialswathi sree100% (1)
- Text Classification To Predict Skin Concerns Over Skincare Using Bidirectional Mechanism in Long Short-Term MemoryDocument11 pagesText Classification To Predict Skin Concerns Over Skincare Using Bidirectional Mechanism in Long Short-Term MemoryCSIT iaesprimeNo ratings yet
- Mercedes Clase S S Guard 2014 INTDocument28 pagesMercedes Clase S S Guard 2014 INTShreyasNo ratings yet
- Threat HuntingDocument2 pagesThreat HuntingDrShubhamangala SunilaNo ratings yet
- Annex B: Application Information For Ampacity CalculationDocument16 pagesAnnex B: Application Information For Ampacity Calculationfa2iiNo ratings yet
- Variance and Standard DeviationDocument17 pagesVariance and Standard DeviationPuja GahatrajNo ratings yet
- Thesis-Speech Recognition MarkovDocument65 pagesThesis-Speech Recognition MarkovTuul TriyasonNo ratings yet
- Ansys Icepak Users GuideDocument1,110 pagesAnsys Icepak Users GuideEsa0% (1)
- BS 4422 2005Document84 pagesBS 4422 2005Dave WilliamsNo ratings yet
- AZ900 Exam Questions Good OneDocument172 pagesAZ900 Exam Questions Good OneShubham Bhaumik100% (1)
- Terastandard - Bsi Bs Iso 5597 267Document26 pagesTerastandard - Bsi Bs Iso 5597 267baladiroyaNo ratings yet
- Algorithm and FlowchartDocument34 pagesAlgorithm and Flowchartmd sufiyanNo ratings yet
- Sentiment Emotion RecognitionDocument6 pagesSentiment Emotion RecognitionSam RockNo ratings yet
- SAP ECC and S4 HANADocument10 pagesSAP ECC and S4 HANASoumya PandaNo ratings yet
- Begin Your Mind Map!: How To Create Mind MapsDocument13 pagesBegin Your Mind Map!: How To Create Mind MapsAnanditaKarNo ratings yet
- Business Certificate Timetable August 2023 Draft Edited 1 1pdf 1686898228811Document3 pagesBusiness Certificate Timetable August 2023 Draft Edited 1 1pdf 1686898228811Sada DahonestNo ratings yet
- Lia Aftanty - 21202241042 - Business PresentationDocument3 pagesLia Aftanty - 21202241042 - Business PresentationLia AftantyNo ratings yet
- DS PPTDocument221 pagesDS PPTanilperfectNo ratings yet
- EGA Pipa ConduitDocument2 pagesEGA Pipa ConduitDerahamaniNo ratings yet
- 11.2.4.4 Packet Tracer - Configuring Port Forwarding On A Linksys Router InstructionsDocument2 pages11.2.4.4 Packet Tracer - Configuring Port Forwarding On A Linksys Router InstructionsLiyanNo ratings yet
- Integrity of Subsea Control UmbilicalDocument11 pagesIntegrity of Subsea Control Umbilicalxinlin.cppNo ratings yet
- A Novel Method For Reconciliation - Julian Et. AlDocument12 pagesA Novel Method For Reconciliation - Julian Et. AlIgnacio UribeNo ratings yet
- PCCCR001Document7 pagesPCCCR001dennisplazaNo ratings yet
- Xerox Phaser 3635mfp - Service ManualDocument202 pagesXerox Phaser 3635mfp - Service ManualFritz BukowskyNo ratings yet
- Lawson Industries, IncDocument4 pagesLawson Industries, IncTony DiStasioNo ratings yet
- 80 High Pressure Piston CompressorDocument10 pages80 High Pressure Piston CompressorSerwis SprężarekNo ratings yet
- Creating Thematic Maps in MapInfo - Geo InformationDocument9 pagesCreating Thematic Maps in MapInfo - Geo InformationMaxim GhereaNo ratings yet