Professional Documents
Culture Documents
Dietary Management - Cardiovascular Diseases
Uploaded by
Reanne Mae AbreraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dietary Management - Cardiovascular Diseases
Uploaded by
Reanne Mae AbreraCopyright:
Available Formats
NCM 211 NUTRITION AND DIET THERAPY (LECTURE)
Father Saturnino Urios University
Prepared by: REANNE MAE C. ABRERA SN
—————————————————————————————————————————————————————————————————————————————————————
CARDIOVASCULAR DISEASE
❖ It is a collective term referring to a group of diseases affecting the heart and blood
vessels.
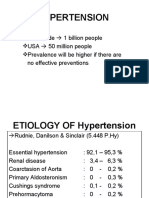
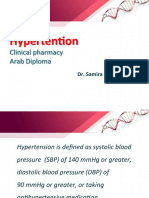
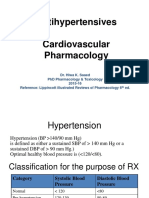
HYPERTENSION (HPN/HTN)
❖ Sustained arterial blood pressure (BP) is equal or greater than 130/80.
❖ It is not a disease, but a symptom. Less than or increased cardiac output and increased
resistance of blood vessel walls to blood flow.
❖ It may occur at any age but most frequently in persons over 40 years old.
❖ Smoking and emotional stress may elevate blood pressure (BP).
❖ There are two (2) types of Hypertension (HPN/HTN):
1. Primary Hypertension → Idiopathic; more common type occurring in 85% to 90%
of all HPN cases.
2. Secondary Hypertension → due to a clearly defined cause.
RISKS OF HYPERTENSION ROLES OF SELECTED DIETARY FACTORS IN HYPERTENSION
1. Formation of atheroma’s ❖ Sodium → Normally found in the ECF (blood plasma and interstitial fluid or extracellular
2. Coronary Artery Disease fluid) but may cross cell walls into ICF (water, electrolytes, protein or intracellular fluid)
3. Cardiac failure causing edema and elevated blood pressure.
4. Aneurysm of the aorta ❖ Sodium → It lowers blood pressure.
5. Acute vascular necrosis ❖ Magnesium → It reduces ICF (intracellular fluid) sodium which decreases blood pressure.
6. Hemorrhagic stroke ❖ Calcium → Some studies show that Ca (calcium) have beneficial effects on the blood
7. Metabolic problems pressure.
❖ Cadmium → Implicated for hypertensives; found in shellfish, kidney meats, grain cereals,
vegetables, and packed fruit juices
❖ N-3 polyunsaturated fats (in fish oils) → It promotes synthesis of prostaglandins for Na
(sodium) and K (potassium) excretion.
❖ Alcohol → High intakes causes vasoconstriction which increases blood pressure.
DIETARY MANAGEMENT: HYPERTENSION (HPN/HTN)
❖ Calories → it depends on the weight’s status or weight goal
❖ Sodium → Restricted (250mg, 500mg, 1g, 2g, 4g, and etc.)
❖ Fluids and Roughage → prevents constipation which hinders absorption of
antihypertensive drugs
❖ The DASH Diet → dietary approach to stop hypertension
➢ Effective with 14 days of initiation
➢ High quantities of fruits, vegetables, low-fat dairy products, whole grains, poultry,
fish, and nuts
❖ Alcohol → avoid high intake; the excessive levels can cause hypertriglyceridemia,
CORONARY HEART DISEASE (CHD)
elevated LDL, arrhythmia, cardiac enlargement, and heart failure
❖ It is a disease involving the network of blood vessels surrounding and serving the heart.
❖ Calories → sufficient to maintain/achieve DBW
❖ It is manifested in clinical end points of myocardial infarction and sudden deaths.
THERAPEUTIC LIFESTYLE CHANGES DIET (TLC)
❖ Pathological events leading to coronary heart disease (CHD):
1. Injury to coronary arteries ❖ It is one of the several heart-healthy diets that can lower cholesterol and help lower the
2. Fibrous plaque formation (Arteriosclerosis) risk of heart disease or stroke.
3. Thrombosis and heart attack ❖ Eating less fat and changing the types of fats to eat.
❖ Eating fewer foods that have cholesterol.
DIETARY MANAGEMENT: CORONARY HEART DISEASE (CHD)
❖ Maintain desirable body weight.
❖ Total Fat → not more than 30% of TER (total energy requirement)
❖ Manage stress.
❖ SFA (saturated fatty acids) → Approximately 10% of TER (total energy requirement) or
❖ Small frequent feedings are indicated.
10% of TER; reduces plasma LDL (low density lipoproteins)
❖ Adequate dietary fiber and fluid intake.
❖ PUFA (polyunsaturated faty acids) → Approximately 10% of TER (total energy
❖ Initially, full liquid diet is done to promote rest and danger in aspiration.
requirement); reduce plasma LDL;
❖ Caffeine intake is reduced (less than 3 cups per day) to prevent potential arrhythmias.
➢ N-6 PUFA (e.g. linoleic acid) promotes prostaglanding synthesis which promotes
❖ Sodium is restricted.
arterial dilatation and heart muscle contractility;
❖ Fluid intake is individualized depending on the fluid status of the patient.
➢ N-3 PUFA of O3 FA reduces blood pressure, inflammation, platelet aggregation,
❖ Low in saturated fats or cholesterol.
fibrinogen, and severity of arrhythmia
❖ Small frequent feedings to reduce cardiac workload.
❖ MUFA (monounsaturated fatty acids) → as effective as PUFA but DOES NOT LOWER
❖ Adequate calcium, potassium, and magnesium is needed.
HDL, less susceptible to oxidation, less thrombogenic potential, does not raise serum TGC
ANGINA AND PRE-INFARCTION ANGINA
(triglycerides)
❖ Cholesterol → not more than 200mg/day; reduce LDL ❖ Pain is caused by demand on the heart when inadequately supplied with blood.
❖ Sodium → moderate intake ❖ It is a type of temporary chest pain, pressure, or discomfort.
❖ Carbohydrates → depends on severity of hyperlipoproteinemias ❖ There is a presence of a narrowed artery which causes ischemia as the heart muscle is
not receiving enough oxygen.
❖ Pain is precipitated by exertion. ❖ Sub-acute Phase
❖ The etiology of angina is atherosclerosis. ➢ 1000kcal to 1200kcal (20% CHON, 45% CHO, 35% FAT) in order to meet REE
(resting energy expenditure??)
DIETARY MANAGEMENT: ANGINA AND PRE-INFARCTION ANGINA
➢ 300mg to control blood cholesterol
❖ Small Meals → To reduce cardiac workload
➢ Soft, low fiber, free of gastric irritants to avoid indigestion and flatus
❖ Avoidance of Gas-Forming Foods → Prevent abdominal distention which may add
➢ Coffee and tea in moderation to avoid stimulation
pressure to the heart
➢ Sodium restriction to prevent or correct edema
❖ Low Calorie for the Obese → To attain DBW (desired body weight)
➢ Small, frequeny feeding to reduce possibility of postprandial dyspnea or pain
❖ Low Cholesterol, Total Fat → To lower cholesterol and TGC (triglycerides) in the serum
■ Postprandial means after eating dinner or lunch, or usually a meal
❖ Alcohol → in moderation; may induce arrhythmias and in large amounts, depresses
❖ Rehabilitative Phase
cardiac function
➢ Calories are adjusted to maintain optimal weight so as to avoid obesity which
ACUTE MYOCARDIAL INFARCTION increases cardiac workload
➢ Fat-controlled diet to control blodo lipid levels so as to lessen the risk for another
❖ It is also known as coronary occlusion or thrombosis.
infarction
❖ It is the destruction of a position of the myocardium due to an interruption of blood
➢ Avoidance of excessive roughage, gas forming and spice foods for easy digestion
supply resulting to formation of localized necrotic areas.
and preventing distention
❖ The etiology can be atherosclerosis.
➢ Limit stimulants
DIETARY MANAGEMENT: ACUTE MYOCARDIAL INFARCTION
➢ Sodium restriction when necessary in case of edema
❖ Acute Phase
CONGESTIVE HEART FAILURE
➢ 500kcal to 800kcal in order to avoid gagging and aspiration of solid foods
❖ It is a disorder of the cardiovascular system caused by the failure of the heart as a pump.
➢ No extreme in temperature to prevent possible precipitation of arrhythmias
❖ The characteristics are:
➢ No coffee or tea as it may stimulate and increase heart rate
1. Weakening of the heart muscles leads to increased blood supply to the body.
➢ Parenteral Feeding → for those unwilling to consume a liquid diet
2. Pooling of blood in the venous system which leads to increased venous pressure
➢ Restriction of Na (sodium) in order to prevent or correct edema.
resulting to edema.
3. RAAS (renin, angiotensin, aldosterone system) is active and responsible for
regulating blood pressure (BP).
4. Low renal blood flow causes Na (sodium) retention which results in edema.
5. Release of vasopressin causes water absorption.
6. Dyspnea, anorexia, nausea and vomiting.
DIETARY MANAGEMENT: CONGESTIVE HEART FAILURE
❖ Low Calorie → reduce weight; decrease workload of the heart
❖ Moderate Protein → maintenance of N (nitrogen) balance
❖ Sodium Restriction → 500mg initially, 1000mg later to control edema
❖ Small Frequent Feeding → decrease circulatory and cardiac workload
❖ Fluid as desired
CARDIAC CACHEXIA
❖ A syndrome of malnutrition that occurs in up to half of patients with moderate to severe
heart failure.
DIETARY MANAGEMENT: CARDIAC CACHEXIA
❖ Cachexia, also known as wasting syndrome, is loss of weight, muscle atrophy, fatigue,
weakness, and significant loss of appetite in someone who is not actively trying to lose ❖ Sodium Restriction → approximately 2400mg/day
weight. It is a common complication of congestive heart failure (CHF) or due to other ❖ Fluid Restriction → 500 - 2000ml/day, typically only during hospitalization
cardiac diseases.
You might also like
- Group 4 Dietary Management of Cardiovascular Disease 2Document72 pagesGroup 4 Dietary Management of Cardiovascular Disease 2Princess IlaNo ratings yet
- Cardiovascular Agents Group 1 Parmacology ReportingDocument415 pagesCardiovascular Agents Group 1 Parmacology ReportingMajestic RavenNo ratings yet
- Nutrition Therapy For Cardiovascular DiseasesDocument43 pagesNutrition Therapy For Cardiovascular DiseasesChelo Jan GeronimoNo ratings yet
- 5 Nutrition Therapy For Cardiovascular DiseasesDocument74 pages5 Nutrition Therapy For Cardiovascular Diseaseskarinablanca adranedaNo ratings yet
- Cardiac DrugsDocument4 pagesCardiac DrugsIbrahem Al100% (2)
- Congestive Heart Failure: Mary Triana xh/26Document14 pagesCongestive Heart Failure: Mary Triana xh/26i make hamburgersNo ratings yet
- Heart Disease2Document34 pagesHeart Disease2mahmoudayman201571No ratings yet
- Hypertension NotesDocument7 pagesHypertension Notesapi-3697326100% (3)
- LTC CHF Case PresentationDocument8 pagesLTC CHF Case Presentationapi-650480818No ratings yet
- CHN Non Communicable Diseases and OthersDocument90 pagesCHN Non Communicable Diseases and OthersEllenare Racion100% (1)
- Cardio PPT BasedDocument17 pagesCardio PPT Basedgindie ceraNo ratings yet
- PBL 2 Session 2 PresentationDocument44 pagesPBL 2 Session 2 PresentationElisaNo ratings yet
- Pathophysiology of HypertensionDocument11 pagesPathophysiology of HypertensionThenmozhi SureshNo ratings yet
- Nursing Management OF A Patient With HypertensionDocument39 pagesNursing Management OF A Patient With HypertensionJEEJANo ratings yet
- ICM 5 Cases 1 - 12Document76 pagesICM 5 Cases 1 - 12oyim sNo ratings yet
- 6.-NCDs Part II (Cardiovascular Diseases (CVDS) )Document36 pages6.-NCDs Part II (Cardiovascular Diseases (CVDS) )Nathaniel OrtegaNo ratings yet
- Case Presentation On Ischemic Cardiomyopathy & Ccf-1-1Document18 pagesCase Presentation On Ischemic Cardiomyopathy & Ccf-1-1Maliha aliNo ratings yet
- Lesson 1 Antihypertensive AgentsDocument8 pagesLesson 1 Antihypertensive AgentsVincent Joshua TriboNo ratings yet
- Oncology EmergencyDocument41 pagesOncology Emergencyomad pendaftaranPPDS100% (2)
- Atrial Fibrillation-OfFICIALDocument13 pagesAtrial Fibrillation-OfFICIALChristelleMaeNo ratings yet
- HypertensionDocument20 pagesHypertensiondocbayNo ratings yet
- Cardiovascular DiseasesDocument47 pagesCardiovascular DiseasesAngie LorenzoNo ratings yet
- Case Study: Congestive Heart FailureDocument7 pagesCase Study: Congestive Heart FailureXI-E / 21 / MARY TRIANANo ratings yet
- Hipertensión Septiembre UMD 2023Document82 pagesHipertensión Septiembre UMD 2023Roberto TicasNo ratings yet
- Vetteth Chronic Kidney DiseaseDocument35 pagesVetteth Chronic Kidney DiseaselmdeboniNo ratings yet
- 5,6.heart FailureDocument12 pages5,6.heart FailureKUMUTHA MALAR A/P PARMESWARANNo ratings yet
- Dietary Management of Congestive Cardiac Failure and DementiaDocument77 pagesDietary Management of Congestive Cardiac Failure and DementiaAgboola SeyiNo ratings yet
- Diagnosis and Management of HypertensionDocument55 pagesDiagnosis and Management of HypertensionDanaTyastriNo ratings yet
- Cardiovascular FunctionDocument157 pagesCardiovascular FunctionJonnabelle PadillaNo ratings yet
- Medical Nutrition Therapy For Cardiovascular Disease 2013Document30 pagesMedical Nutrition Therapy For Cardiovascular Disease 2013ashry909100% (1)
- HTN Dr. Samira BelkheirDocument47 pagesHTN Dr. Samira BelkheirkalfNo ratings yet
- SPLE Clinical PharmaDocument72 pagesSPLE Clinical PharmaSEIYADU IBRAHIMNo ratings yet
- CA ReviewerDocument16 pagesCA ReviewerJheanAlphonsineT.MeansNo ratings yet
- Hypertensiveemergencies RullDocument60 pagesHypertensiveemergencies RullagustinaNo ratings yet
- Report JajaDocument17 pagesReport JajaAlleyah LorenzoNo ratings yet
- Hypertension Walker JNC 8Document10 pagesHypertension Walker JNC 8John TecsonNo ratings yet
- Chronic Kidney Disease: Pathophysiology Review: Stages in CKDDocument17 pagesChronic Kidney Disease: Pathophysiology Review: Stages in CKDAjie ZamNo ratings yet
- Assignment: Applied MedicineDocument8 pagesAssignment: Applied MedicineKhadija BakhtawarNo ratings yet
- Assignment: Applied MedicineDocument8 pagesAssignment: Applied MedicineKhadija BakhtawarNo ratings yet
- Based On Your Possible Final Diagnosis, What Are The Treatment Plans For Our Patient?Document63 pagesBased On Your Possible Final Diagnosis, What Are The Treatment Plans For Our Patient?Kita kitaNo ratings yet
- Coronary Atherosclerosis: Cardiovascular System: Coronary Vascular Disease Topics Discussed Here AreDocument6 pagesCoronary Atherosclerosis: Cardiovascular System: Coronary Vascular Disease Topics Discussed Here AreKamx MohammedNo ratings yet
- Hypertension: SubobjectiveDocument34 pagesHypertension: Subobjectivesotharysok629No ratings yet
- Drugs Acting On The KidneysDocument56 pagesDrugs Acting On The Kidneysbetu tufaNo ratings yet
- Nutrition Therapy 2Document16 pagesNutrition Therapy 2Cariel BunyiNo ratings yet
- Cardiovascular Diseases: Factors Affecting CVDDocument7 pagesCardiovascular Diseases: Factors Affecting CVDManu MustafaNo ratings yet
- Chapter 31 HypertensionDocument3 pagesChapter 31 HypertensionVen SemillaNo ratings yet
- Nutrition For Cardiovascular Diseases 2012Document80 pagesNutrition For Cardiovascular Diseases 2012Miftachul JannahNo ratings yet
- Hypertension KLP 10Document16 pagesHypertension KLP 10Tri ArdiyaniNo ratings yet
- HYPERTENSIONDocument10 pagesHYPERTENSIONChelsea Faith SarandiNo ratings yet
- Antihypertensives Cardiovascular PharmacologyDocument52 pagesAntihypertensives Cardiovascular PharmacologyAlan LealNo ratings yet
- Hypertension Definition:: Nitric OxideDocument5 pagesHypertension Definition:: Nitric OxideAnonymous bbeAZHxZNo ratings yet
- Peripheral Vascular DisordersDocument4 pagesPeripheral Vascular DisordersDawnmurph Dharlene Wag-eNo ratings yet
- Lesson 5 Hypertension Notes White BGDocument15 pagesLesson 5 Hypertension Notes White BGWaliid Khan 5SNo ratings yet
- Hypertension: by Krikor Jabourian Nakhleh Nehmeh Yara YounesDocument33 pagesHypertension: by Krikor Jabourian Nakhleh Nehmeh Yara YounesHamza DibNo ratings yet
- Case Study 4Document10 pagesCase Study 4api-440408997No ratings yet
- A Simple Guide to Hypertension and Heart DiseasesFrom EverandA Simple Guide to Hypertension and Heart DiseasesRating: 5 out of 5 stars5/5 (1)
- Topic 8 - The NewbornDocument16 pagesTopic 8 - The NewbornReanne Mae AbreraNo ratings yet
- Topic 7 - Perineal and Abdominal ExercisesDocument3 pagesTopic 7 - Perineal and Abdominal ExercisesReanne Mae AbreraNo ratings yet
- Topic 1 - Introduction To PharmacologyDocument4 pagesTopic 1 - Introduction To PharmacologyReanne Mae AbreraNo ratings yet
- Topic 10 - The Schooler and The FamilyDocument18 pagesTopic 10 - The Schooler and The FamilyReanne Mae AbreraNo ratings yet
- Topic 2.1 - Pharmacokinetics and PharmacodynamicsDocument10 pagesTopic 2.1 - Pharmacokinetics and PharmacodynamicsReanne Mae AbreraNo ratings yet
- Topic 3.2 - Philippine Drug Regulations and LegislationsDocument3 pagesTopic 3.2 - Philippine Drug Regulations and LegislationsReanne Mae AbreraNo ratings yet
- Dietary Management - Renal DisordersDocument8 pagesDietary Management - Renal DisordersReanne Mae AbreraNo ratings yet
- Topic 11 - Respiratory AgentsDocument5 pagesTopic 11 - Respiratory AgentsReanne Mae AbreraNo ratings yet
- Dietary Management - Diabetes MellitusDocument9 pagesDietary Management - Diabetes MellitusReanne Mae AbreraNo ratings yet
- Dietary Management - Gastrointestinal ProblemsDocument14 pagesDietary Management - Gastrointestinal ProblemsReanne Mae AbreraNo ratings yet
- Topic 13 - Reproductive AgentsDocument8 pagesTopic 13 - Reproductive AgentsReanne Mae AbreraNo ratings yet
- Topic 10 - Cardiovascular AgentsDocument8 pagesTopic 10 - Cardiovascular AgentsReanne Mae AbreraNo ratings yet
- Topic 14 - Dermatologic AgentsDocument4 pagesTopic 14 - Dermatologic AgentsReanne Mae AbreraNo ratings yet
- Topic 12 - Endocrine AgentsDocument7 pagesTopic 12 - Endocrine AgentsReanne Mae AbreraNo ratings yet
- Picco Technology Clinical Evidence Brochure en Non - UsDocument25 pagesPicco Technology Clinical Evidence Brochure en Non - UsRichard DaiNo ratings yet
- NCLEX Review Question in Cardiovascular System Part 7Document5 pagesNCLEX Review Question in Cardiovascular System Part 7Rochelle Ricafrente100% (2)
- Assessment of Left AtriumDocument68 pagesAssessment of Left Atriumadh30No ratings yet
- Cardio Report (Mi)Document9 pagesCardio Report (Mi)Tifanie Cyrine MerneloNo ratings yet
- Re Ca VADocument9 pagesRe Ca VAmanudanuNo ratings yet
- CVS Examination PSC2021Document2 pagesCVS Examination PSC2021علي 707No ratings yet
- Preparing A Patient For Cardiac Catheterization.4Document1 pagePreparing A Patient For Cardiac Catheterization.4Quality PmnhNo ratings yet
- Acrocyanosis: Acrocyanosis Is Persistent Blue or CyanoticDocument5 pagesAcrocyanosis: Acrocyanosis Is Persistent Blue or CyanoticFamilia Macovei Haralambie-AndreeaNo ratings yet
- 22 Blood Supply of The Ear - DoneDocument7 pages22 Blood Supply of The Ear - DoneosamaeNo ratings yet
- (Modified Essay Question) ADIC 510302: Managing Critically Ill Patient IDocument2 pages(Modified Essay Question) ADIC 510302: Managing Critically Ill Patient Isembakarani thevagumaranNo ratings yet
- Pathophysiology of Native Coronary, Vein Graft, and In-Stent Atherosclerosis PDFDocument20 pagesPathophysiology of Native Coronary, Vein Graft, and In-Stent Atherosclerosis PDFJorge Arturo Bustos MartinezNo ratings yet
- Anaesthetic Considerations in Cardiac Patients Undergoing Non Cardiac SurgeryDocument7 pagesAnaesthetic Considerations in Cardiac Patients Undergoing Non Cardiac Surgerysatria wibawaNo ratings yet
- Limb IschaemiaDocument40 pagesLimb Ischaemiaqaaneta bint-e-najafNo ratings yet
- Stroke: Joan Marie Amamio BSN IV Report byDocument35 pagesStroke: Joan Marie Amamio BSN IV Report byAnjo Marie AmamioNo ratings yet
- Nursing Care Plan Pregnancy Induced Hypertension (PIH Preeclampsia and Eclampsia)Document2 pagesNursing Care Plan Pregnancy Induced Hypertension (PIH Preeclampsia and Eclampsia)deric91% (78)
- Anatomical and Histological Description of The Right Atrioventricular Valve of The Canine Heart (Canis Lupus Familiaris)Document7 pagesAnatomical and Histological Description of The Right Atrioventricular Valve of The Canine Heart (Canis Lupus Familiaris)Esteban SchenckeNo ratings yet
- 13 Calibration WassertheurerDocument7 pages13 Calibration WassertheurerYasmine AbbaouiNo ratings yet
- Varicose VeinsDocument19 pagesVaricose VeinsnadiaNo ratings yet
- CH 19 Transport in HumanDocument49 pagesCH 19 Transport in HumanRay PeramathevanNo ratings yet
- LP Stemi PujaDocument25 pagesLP Stemi PujaPuja Oktavia100% (1)
- Liver Vascular Anatomy - A RefresherDocument10 pagesLiver Vascular Anatomy - A Refresherilham nugrohoNo ratings yet
- Transport System Question and AnswersDocument12 pagesTransport System Question and Answerskumara guruparanNo ratings yet
- Excellup Class TenDocument3 pagesExcellup Class TenHemant KumarNo ratings yet
- The Human Heart: Presentation By: Zuhaib FayyazDocument22 pagesThe Human Heart: Presentation By: Zuhaib Fayyazfdrz200887No ratings yet
- Idiopathic Postural HvpotensionDocument5 pagesIdiopathic Postural HvpotensionGonzalo ReitmannNo ratings yet
- Thorax - BRS Gross Anatomy NOTESDocument8 pagesThorax - BRS Gross Anatomy NOTESJustyna PoznanskaNo ratings yet
- Redo Cardiac Surgery in AdultsDocument202 pagesRedo Cardiac Surgery in AdultsJaime ArroyoNo ratings yet
- My CV in PDF File LDocument115 pagesMy CV in PDF File LMohamed Omar ElfarokNo ratings yet
- AortographyDocument31 pagesAortographyWendy Escalante100% (1)
- 11 The Pericardium and The HeartDocument39 pages11 The Pericardium and The HeartJeff D'erique Ozil TettehNo ratings yet