Professional Documents
Culture Documents
Intensive Care Unit (ICU) Manual 2020-21
Uploaded by
anithaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intensive Care Unit (ICU) Manual 2020-21
Uploaded by
anithaCopyright:
Available Formats
INTENSIVE CARE
MANUAL
Edition
Revised and reprinted
Approved by Assistant Director medical services
Reviewed by Critical care In charge
Quality Steering Committee
Annual Review of Manual
Amendments:
Additions:
Admission& Discharge criteria added for COVID Extension
Insulin sliding scales has been added
Intensive Care Manual Controlled Copy Quality Department 1
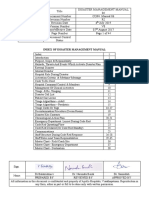
S.NO CONTENTS PAGE NO.
1. ICU ADMISSION, DISCHARGE AND TRIAGE 3
2. TRIAGE FOR ICU 28
3. BED SHORTAGE POLICY 31
4. INFECTION CONTROL IN ICU 32
5. GUIDELINES TO MEDICAL STAFF 33
6. CLINICAL PROCEDURES 37
7. DRUGS AND INFUSIONS 63
8. FLUIDS AND ELECTROLYTES 93
9. METABOLIC DISTURBANCES 105
10. ACID BASE DISTURBANCE IN ICU 110
11. SPECIAL CONSIDERATIONS 116
12. CRITICAL CARE IN PREGNANCY 124
13. MICROBIOLOGY PROTOCOLS 133
14. APPENDIX 141
Intensive Care Manual Controlled Copy Quality Department 2
ADMISSION, DISCHARGE & TRIAGE
ADMISSION CRITERIA
Intensive Care Unit (ICU) admission criteria select patients who are likely to benefit from ICU
care. Each ICU admits patients with the following diagnosis respectively.
ADMISSION & DISCHARGE CRITERIA - ADVANCED CRITICAL CARE UNIT (ACCU)
ADMISSION CRITERIA
Patients are admitted to this unit for evaluation and treatment of illness that may lead to death
or acute organ failure, that are amenable to treatment, and that require intensive monitoring
(including intravascular pressure monitors), frequent evaluation (including laboratory tests),
continuous medication infusions, and/or intensive nursing care. Admission decisions are made
based on complete evaluation of the patient’s medical and nursing requirements. Paediatric
patients as well as adults are provided admission to this unit. In case of bed shortage, other
specialty patients may also be admitted.
A. Respiratory System
Acute respiratory failure Pao2 less than 50 mm Hg; Paco2>60 mm Hg requiring
ventilator support. (Invasive or non-invasive support).
Chronic respiratory failure with altered sensorium.
Patients who are demonstrating respiratory deterioration.
Require frequent tracheal suctioning or chest physiotherapy.
Acute airway obstruction.
Massive haemoptysis.
Pulmonary embolism with hemodynamic instability.
B. Cardiovascular system
Hemodynamic instability
Acute coronary syndrome
Congestive heart failure
C. Gastrointestinal system
Acute upper or lower GI tract haemorrhage causing orthostatic hypotension or
blood loss requiring multiple transfusions.
Hepatic dysfunction causing encephalopathy.
Inflammatory bowel disease causing ileus or peritonitis.
Severe acute pancreatitis
Intensive Care Manual Controlled Copy Quality Department 3
D. Renal system
Acute kidney injury
Acute or Chronic kidney disease
Patients requiring dialysis support like CRRT, Peritoneal dialysis.
E. Endocrine system
Diabetic ketoacidosis
Thyroid storm or myxoedema coma
Hyperosmolar coma
Adrenal crisis with hemodynamic instability or other endocrinal problems with
hemodynamic instability.
Hypo or hypernatremia with seizure, altered mental function.
Hypo or hyperkalaemia with dysrhythmias or muscular weakness.
Severe hypocalcaemia/ severe hyperkalaemia with altered mental status or
requiring hemodynamic monitoring.
Hypo or Hyper magnesium with hemodynamic or respiratory compromise or
dysrhythmias.
F. Haematology system
Thrombocytopenia with active bleeding
Coagulopathy with active bleeding
G. Infectious /Environmental agents
Severe sepsis and sepsis shock
Acute meningitis with neurological abnormalities
Acute poisoning with depressed level of consciousness or airway compromised,
hemodynamic instability or cardiac arrhythmias.
Acute drug withdrawal syndromes with hemodynamic instability.
Environmental injuries (lightening, near drowning, hypo-hyperthermia)
Scorpion, snake bite with hemodynamic and respiratory dysfunction
H. Post-operative
Patients requiring ICU care postoperatively
I. Relative physiologic indications for admission to the ICU
New onset persistent oliguria (urine output<0.5ml/kg/hour)
Intensive Care Manual Controlled Copy Quality Department 4
Severe dehydration or severe sepsis with systolic BP<90mmHg.
GCS 8 or less than 8, if GCS>8 with rapid worsening.
Haemoglobin <7 grams/dl at presentation to hospital.
DISCHARGE CRITERIA
Patients are discharged from the ICU when their acute illness is treated, their medical
condition has stabilized, and they do not require any form of life support, frequent evaluation
(including laboratory tests), medication infusions, and /or intensive nursing care.
Discharge decisions are made based on complete evaluation of the patient’s medical and
nursing requirements.
A. Respiratory system
Treatment of respiratory failure with stable haemodynamic
B. Cardiovascular system
Blood pressure within acceptable range without inotropic support.
Symptomatic Bradycardia or tachycardia reversed.
Not requiring continuous infusions of vasoactive drugs or antiarrhythmic agents.
Physiological admission Criteria
S.N Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
o. condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
C. Gastrointestinal system
Intensive Care Manual Controlled Copy Quality Department 5
No orthostatic hypotension and haematocrit stable for previous 24 hours.
Stable or improving hepatic encephalopathy.
Ileus or peritonitis resolving.
D. Renal system
Oliguria corrected or stable on haemodialysis.
E. Endocrine system
Correction of diabetic emergencies with treatment stabilizing blood sugar for 24
hrs.
F. Haematology system
Control of bleeding and correction of thrombocytopenia
Correction of INR with control of bleeding
Stable haematocrit for 24 hrs
G. Infectious/Environmental agents
Resolving Sepsis with acceptable blood pressure.
Stable or improving neurological function with resolving acute meningitis.
Stable with airway protection with resolving acute poisoning, without need for
further monitoring.
H. Relative physiologic indications for discharge from the ACCU
Parameter Adults Paediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree F +/-1.5
Heart rate Heart rate- >40 beats per 80-140 Beats/minute
minute, <130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, 90-100 +/-10 mm Hg
Systolic BP </= 200 mmhg.
Respiratory rate >14 breaths/min and 20-30 Breaths/minute
Respiratory rate <35 breaths /
min
Intensive Care Manual Controlled Copy Quality Department 6
SpO2 >95% on room air>/= 90% on 90-95% on room air
4lit/min of oxygen.
1. Resolution of primary disease, (as per treating / ICU team)
2. Able to protect airway on his/her own or with a tracheostomy tube.
3. Overall GCS of >/= 13/15
4. No fresh Neurological deficits in the last 12 hours, or no worsening of existing deficits.
5. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit, Potassium > 3
mmol/lit.)
6. Post op wound status- healthy with drains less than 50% of container.
7. Not requiring any form of organ support for at least more than 24 hours (Ventilator, Bi Pap
Etc.)
8. Stable hemodynamic parameters without any inotropic requirement for at least 24 hours,
ADMISSION AND DISCHARGE CRITERIA - CARDIO THORACIC, HEART & LUNG
TRANSPLANT ICU (CTPOST)
The Cardio- Thoracic, Heart transplant ICU provides comprehensive 24-hour patient care for
adult patients requiring intensive care for the following conditions:
ADMISSION CRITERIA
1. All adult cases who have undergone Cardiac surgery in the CTVS operation theatre for post-
operative care with Pump /Off Pump support
2. All adult cases who have undergone Thoracic surgery in the Operating room for post-
operative care
3. All adult patients who have received a cardiac transplant from a donor for post-operative
care and stabilization
4. Adult pre cardiac surgery cases who are hemodynamically unstable and need ionotropic
support to be stabilized before surgery.
5. Adult post-cardiac surgery cases who are hemodynamically unstable or have arrhythmias
and need ionotropic support or antiarrhythmic drugs to be stabilized before discharge
Intensive Care Manual Controlled Copy Quality Department 7
DISCHARGE CRITERIA
I. Relative physiologic indications for discharge from the CTPOST
9. Resolution of primary disease, (as per treating / ICU team)
10. Able to protect airway on his/her own or with a tracheostomy tube.
11. Overall GCS of >/= 13/15
12. No fresh Neurological deficits in the last 12 hours, or no worsening of existing
deficits.
13. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit,
Potassium > 3 mmol/lit.)
14. Post op wound status- healthy with drains less than 50% of container.
15. Not requiring any form of organ support for at least more than 24 hours (Ventilator,
Bi Pap Etc.)
16. Stable hemodynamic parameters without any inotropic requirement for at least 24
hours,
Diastolic BP >/= 90 mmhg, Systolic BP </= 200 mmhg.
Heart rate- >40 beats per minute, <130 beats/ minute
17. Respiratory rate >14 breaths/min and Respiratory rate <35 breaths / min
18. O2 saturations- >/= 90% on 4lit/min of oxygen.
19. No major cardiac arrhythmias in the last 24 hours
20. Not requiring temporary external pacemaker
Physiological admission Criteria
S.N Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
o. condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
Intensive Care Manual Controlled Copy Quality Department 8
21. Able to walk a few steps with assistance
Physiological discharge criteria :
Parameter Adults Paediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree F +/-1.5
Heart rate Heart rate- >40 beats per minute, 80-140 Beats/minute
<130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, Systolic 90-100 +/-10 mm Hg
BP </= 200 mmhg.
Respiratory rate >14 breaths/min and Respiratory 20-30 Breaths/minute
rate <35 breaths / min
SpO2 >95% on room air>/= 90% on 90-95% on room air
4lit/min of oxygen.
PHYSIOLOGICAL ADMISSION AND DISCHARGE CRITERIA - TICU (Transplant ICU)
Liver Transplant:
Post Liver Transplant care is a highly specialized service that is provided for the patients.
Admission criteria:
Patients are shifted to the ICU following liver transplantation surgery and multi visceral
transplantation. Rarely patients who are liver transplant recipients and multi visceral transplant
recipients may also be admitted to ICU for treatment of post operative complications.
Discharge criteria:
1. Vitas signs within normal limits
2. Good trend of liver function tests
3. Haemodynamically stable
SBP 85 -180 mmHg
DBP 45-110 mmHg
HR 45-120 beats per minute
Spo2 >90%
GCS>13
The Patient Must Be:
Oriented to the person, time, and place
Intensive Care Manual Controlled Copy Quality Department 9
Tolerating oral feeds
Ambulatory
The Patient Must Not Have:
Nausea or Vomiting
Bleeding
Pain score should be >4
Written instruction for post-operative period and follow up on a regular basis are done
Immunosuppressant medication has been optimised
Admission & Discharge Criteria
(Medical Intensive Care Unit)
ADMISSION CRITERIA
Patients are admitted to this unit for evaluation and treatment of illness that may lead to acute
organ failure or may progress to death, that are amenable to treatment, and that require
various forms of life support (like mechanical ventilation) intensive monitoring (including
intravascular pressure monitors), frequent evaluation (including laboratory tests), continuous
medication infusions, and/or intensive nursing care. Admission decisions are made based on
complete evaluation of the patient’s medical and nursing requirements. Paediatric patients as
well as adults are provided admission to this unit. In case of situation like bed shortages, other
specialty patients may also be admitted.
J. Respiratory System:
Acute respiratory failure, (type 1 or type 2), Pao2 less than 50 mm Hg; Paco2>60
mm Hg requiring ventilator support. (Invasive or non invasive support).
Chronic respiratory failure with altered sensorium.
Patients who are need monitoring to assess and treat respiratory deterioration.
Require monitoring / protection of airway patency.
Require frequent tracheal suctioning or chest physiotherapy.
Acute airway obstruction.
Massive hemoptysis.
Pulmonary embolism with hemodynamic instability.
K. Cardiovascular system
Hemodynamic instability
Acute coronary syndrome
Congestive heart failure
Intensive Care Manual Controlled Copy Quality Department 10
L. Gastrointestinal system
Acute upper or lower GI tract haemorrhage causing orthostatic hypotension or
blood loss requiring multiple transfusions.
Hepatic dysfunction causing encephalopathy.
Inflammatory bowel disease causing ileus or peritonitis.
Severe acute pancreatitis.
M. Renal system
Acute kidney injury.
Acute or Chronic kidney disease.
Patients requiring dialysis support like CRRT, Peritoneal dialysis.
N. Endocrine system
Diabetic ketoacidosis.
Thyroid storm or myxoedema coma.
Hyperosmolar coma.
Adrenal crisis with hemodynamic instability or other endocrinal problems with
hemodynamic instability.
Hypo or hypernatremia with seizure, altered mental function.
Hypo or hypernatremia with dysrhythmias or muscular weakness.
Severe hypocalcaemia/ severe hyperkalaemia with altered mental status or
requiring hemodynamic monitoring.
Hypo or Hyper magnesium with hemodynamic or respiratory compromise or
dysrhythmias.
O. Haematology system
Thrombocytopenia with active bleeding
Coagulopathy with active bleeding
P. Infectious /Environmental agents
Severe sepsis and sepsis shock
Acute meningitis with neurological abnormalities
Acute poisoning with depressed level of consciousness or airway compromised,
hemodynamic instability or cardiac arrhythmias.
Acute drug withdrawal syndromes with hemodynamic instability.
Environmental injuries (lightening, near drowning, hypo-hyperthermia)
Scorpion, snake bite with hemodynamic and respiratory dysfunction
Intensive Care Manual Controlled Copy Quality Department 11
Note: Hemodynamic instability is defined as-
Pulse rate less than 50 beats/min or more than 150 beats/minute.
Systolic blood pressure (SBP) less than 90mm Hg or 40 mm Hg drop of systolic Blood
pressure.
Diastolic blood pressure more than 120mm Hg.
Mean arterial pressure less than 60 mm Hg.
DISCHARGE CRITERIA
Patients are discharged from the ICU when their acute illness is treated, their medical
condition has stabilized, and they do not require frequent evaluation (including laboratory
tests), continuous medication infusions, and/or intensive nursing care.
Discharge decisions are made based on complete evaluation of the patient’s medical and
nursing requirements.
J. Respiratory system
Treatment and reversal of respiratory failure with stable haemodynamic
K. Cardiovascular system
Physiological admission Criteria
S.N Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
o. condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
Blood pressure within acceptable range without inotropic support.
Symptomatic Bradycardia or tachycardia reversed.
Not requiring continuous infusions of vasoactive drugs or antiarrhythmic agents.
L. Gastrointestinal system
No orthostatic hypotension and haematocrit stable for previous 24 hours.
Stable or improving hepatic encephalopathy.
Ileus or peritonitis resolving.
M. Renal system
Oliguria corrected or stable on haemodialysis.
Intensive Care Manual Controlled Copy Quality Department 12
N. Endocrine system
Correction of diabetic emergencies with treatment stabilizing blood sugar for 24
hrs.
O. Haematology system
Control of bleeding and correction of thrombocytopenia
Correction of INR with control of bleeding
Stable haematocrit for 24 hrs.
P. Infectious/Environmental agents
Resolving Sepsis with acceptable blood pressure.
Stable or improving neurological function with resolving acute meningitis.
Stable with airway protection with resolving acute poisoning, without need for
further monitoring.
Q. Relative physiologic indications for discharge from the MICU I and MICU II
22. Resolution of primary disease, (as per treating / ICU team)
23. Able to protect airway on his/her own or with a tracheostomy tube.
24. Overall GCS of >/= 13/15
25. No fresh Neurological deficits in the last 12 hours, or no worsening of existing
deficits.
26. Critical lab parameters within satisfactory range, (E.g.- Sodium- >130 mmol/lit,
Potassium > 3 mmol/lit.)
27. Post op wound status- healthy with drains less than 50% of container.
28. Not requiring any form of organ support for at least more than 24 hours (Ventilator,
Bi Pap Etc.)
29. Stable hemodynamic parameters without any inotropic requirement for at least 24
hours
Parameter Adults Paediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree F +/-1.5
Heart rate Heart rate- >40 beats per 80-140 Beats/minute
minute, <130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, 90-100 +/-10 mm Hg
Systolic BP </= 200 mmhg.
Intensive Care Manual Controlled Copy Quality Department 13
Respiratory rate >14 breaths/min and 20-30 Breaths/minute
Respiratory rate <35 breaths /
min
SpO2 >95% on room air>/= 90% on 90-95% on room air
4lit/min of oxygen.
ADMISSION AND DISCHARGE CRITERIA SICU (Surgical Intensive Care Unit)
ADMISSION CRITERIA
All patients from general surgery besides from ENT, Head and Neck Surgery, Gynecology,
Urology, Surgical Gastroenterology, Surgical Oncology, Plastic, Pediatric surgery and Orthopedic
Surgery for whom ICU Care is required. Pediatric patients as well as adults are provided
admission to this unit. In case of bed shortage, other specialty patients may also be admitted.
A. Criteria for Admission to the SICU.
Peri operative acute respiratory failure
Treatment of hemodynamic instability status
Intubated patients requiring ventilator support
Patient in severe sepsis and septic shock
B. Relative physiologic indications for admission to the SICU.
Severe tachycardia (Heart Rate > 130beats/minute) or bradycardia (Heart rate <
40beats/minute)
Respiratory distress (Respiratory Rate > 30breaths/minutes, SPO2 < 88%, PaO2/FiO2
ratio <300)
New onset persistent oliguria (urine output < 0.5ml/kg/hour)
Severe dehydration of severe sepsis with systolic Blood Pressure <90mm Hg
Glasgow Coma Scale 8 or less than 8, if Glasgow Coma Scale > 8 with rapid worsening.
Hemoglobin < 7 grams/dl at presentation to hospital.
Septic shock – MAP < 65 mm of Hg.
Intensive Care Manual Controlled Copy Quality Department 14
Physiological admission Criteria
S.No. Sudden deterioration in Greater Than (>) Lesser Than (<)
patient’s condition as
evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
DISCHARGE CRITERIA
The following will include absolute criteria necessary for discharge and relative physiologic
criteria to be used in guidelines for discharge.
A. Absolute Criteria
Patients must be off mechanical ventilation
Patients must be hemodynamically stable and not in respiratory distress before
discharge from the ICU
B. Relative physiologic indications for discharge.
30. Resolution of primary disease, (as per treating / ICU team)
31. Able to protect airway on his/her own or with a tracheostomy tube.
32. Overall GCS of >/= 13/15
33. No fresh Neurological deficits in the last 12 hours, or no worsening of existing
deficits.
34. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit,
Potassium > 3 mmol/lit.)
35. Post op wound status- healthy with drains less than 50% of container.
36. Not requiring any form of organ support for at least more than 24 hours (Ventilator,
Bi Pap Etc.)
Intensive Care Manual Controlled Copy Quality Department 15
Stable vitals : Adults Pediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree +/- 1.5
Heart rate 80-120 Beats/minute 80-140 Beats/Minute
BP 120/80 +/- 20 mmHg 90-100 +/- 10 systolic
mmHg
Respiratory rate 18-20 Breaths /minute 20-30 Breaths/minute
SPO2 >95% on room air 90-95% on room air
CICU (Cardiac Intensive Care Unit)
ADMISSION AND DISCHARGE CRITERIA CICU (CARDIAC INTENSIVE CARE UNIT)
Pediatric patients as well as adults from Cardiology services are provided admission to this unit.
In case of bed shortage, other specialty patient may also be admitted
ADMISSION CRITERIA
Cardiovascular System
Acute Coronary Syndrome ( STEMI ), NSTEMI , Unstable Angina .
Primary PTCA, Elective Angiogram and stenting.
Complex arrhythmias requiring close monitoring and intervention
Acute congestive heart failure with respiratory failure and / or requiring hemodynamic
support
Hypertensive emergencies
Acute MI related complication ( Pul;monary edema,VSD, MVR , Cordae Suphex
)particularly with dysrhythmias, hemodynamic instability, or persistent chest pain.
Pulmonary Embolism
Cardiac arrest
ASD Closure
Intensive Care Manual Controlled Copy Quality Department 16
Physiological admission Criteria
S.N Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
o. condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
Cardiac Tamponade or constriction with hemodynamic instability
Dissecting aortic aneurysms.
Correction of hy[potension ? hypertension
Correction of bradycardia
Complete heart block requiring Interventions.
Absence of life-threatening arrhythmias after observation?
Post PPI ,AICD Implantation ,TAVI ?
DISCHARGE CRITERIA
Cardiovascular system
Correction of hypotension / hypertension
Correction of bradycardia / tachycardia
Absence of life - threatening arrhythmia after observation
Not requiring continuous infusions of vasoactive drugs or antiarrhythmic agents
Pericardial tamponade resolved
Hemodynamic stability
Intensive Care Manual Controlled Copy Quality Department 17
Transfer / discharge will be based on the following criteria :
Stable hemodynamic parameters
Stable respiratory status (patient extubated with stable arterial blood gases) and airway
patency
Minimal oxygen requirements that do not exceed patient care unit guidelines
Intravenous inotropic support, vasodilators, and antiarrhythmic drugs are no longer
required
Cardiac dysrhythmias are controlled
Removal of all hemodynamic monitoring catheters
Discontinuation of peritoneal or hemodialysis with resolution of critical illness
Patients with tracheostomies who no longer require excessive suctioning.
B. Relative physiologic indications for Discharge.
37. Resolution of primary disease, (as per treating / ICU team)
38. Able to protect airway on his/her own or with a tracheostomy tube.
39. Overall GCS of >/= 13/15
40. No fresh Neurological deficits in the last 12 hours, or no worsening of existing
deficits.
41. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit,
Potassium > 3 mmol/lit.)
42. Post op wound status- healthy with drains less than 50% of container.
43. Not requiring any form of organ support for at least more than 24 hours (Ventilator,
Bi Pap Etc.)
44. Stable hemodynamic parameters without any inotropic requirement for at least 24
hours,
Diastolic BP >/= 90 mmhg, Systolic BP </= 200 mmhg.
Heart rate- >40 beats per minute, <130 beats/ minute
45. Respiratory rate >14 breaths/min and Respiratory rate <35 breaths / min
46. O2 saturations- >/= 90% on 4lit/min of oxygen.
Intensive Care Manual Controlled Copy Quality Department 18
Physiological discharge criteria :
Parameter Adults Pediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree F +/-1.5
Heart rate Heart rate- >40 beats per 80-140 Beats/minute
minute, <130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, 90-100 +/-10 mm Hg
Systolic BP </= 200 mmhg.
Respiratory rate >14 breaths/min and 20-30 Breaths/minute
Respiratory rate <35 breaths /
min
SpO2 >95% on room air>/= 90% on 90-95% on room air
4lit/min of oxygen.
NEURO ICU 1 and 2. (Neurology Intensive Care Unit)
Admission & Discharge criteria Neuro ICU (Neurology intensive care unit)
Pediatric patients as well as adults from Neurology and Neurosurgical services are provided
admission to this unit. In case of bed shortage, other specialty patients may also be admitted.
Admission Criteria (Neurological systems )
Fall in Glasgow com score less than 8 or a fall of more than 2 within 24 hours with need
for continuous monitoring.
Uncontrolled seizures.
Progressive muscle weakness involving respiratory muscles.
Intracranial masses associated with acute or progressive neurologic dysfunction.
Recent non-traumatic subarachnoid hemorrhage and intracranial bleeding.
Recent cerebral infarction associated with diminished level of consciousness of
progressive focal deficits.
Coma, Metabolic, toxic or anoxic.
Patients in com from acute structural brain disease or injury but who do not have an
acute intracranial mass.
Post operative craniotomies.
Post operative intracranial stereotactic biopsies.
Post-operative extra cranial cerebrovascular cases.
Post-operative laminectomies with an unusual risk of hematoma.
Meningitis with altered mental status or respiratory compromise.
Intensive Care Manual Controlled Copy Quality Department 19
Physiological admission Criteria
S.No. Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >30 / Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <90% @6Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
Discharge Criteria
Seizures controlled on stable medical regimen after observation.
Patients must have a stable GCS.
Patient shoulder have a mental status that has stabilized and an ability to protect the
airway either by a level of consciousness or a tracheostomy tube.
Improving level of consciousness.
Stabilization of focal deficits.
Following acute spinal cord injury, no progression of deficit with stable respiratory and
hemodynamic status.
Following post-operative laminectomy, no deficit or progression of deficit after
observation.
A. Relative physiologic indications for admission to the NEURO ICU 1 and 2.
Severe dehydration of severe sepsis with systolic BP < 90 Hg.
GCS 8 or less than 8, if GCS > 8 with rapid worsening.
Hemoglobin < 7 grams/dl at presentation to hospital.
Transfer / discharge will be based on the following criteria:
Stable hemodynamic parameters, systolic blood pressure > 90 mmHg.
Stable respiratory status respiratory rate < 30 breaths/minute (patient extubated with
stable arterial blood gases) and airway patency.
Minimal oxygen requirements (< 2 liters/min) that do not exceed patient care unit
guidelines.
Intravenous inotropic support, vasodilators, and antiarrhythmic drugs are no longer
required.
Cardiac dysrhythmia’s are controlled.
Intensive Care Manual Controlled Copy Quality Department 20
Neurologic stability with control of seizures.
Removal of all hemodynamic monitoring catheters.
Discontinuation of peritoneal of hemodialysis with resolution of critical illness.
Patients with tracheostomies who no longer require excessive suctioning.
B. Relative physiologic indications for discharge.
47. Resolution of primary disease, (as per treating / ICU team)
48. Able to protect airway on his/her own or with a tracheostomy tube.
49. Overall GCS of >/= 13/15
50. No fresh Neurological deficits in the last 12 hours, or no worsening of existing deficits.
51. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit, Potassium > 3
mmol/lit.)
52. Post op wound status- healthy with drains less than 50% of container.
53. Not requiring any form of organ support for at least more than 24 hours (Ventilator, Bi Pap
Etc.)
54. Stable hemodynamic parameters without any inotropic requirement for at least 24 hours,
Parameter Adults Paediatric
Temperature 98.6 degree F +/- 1.5 98.6 degree F +/-1.5
Heart rate Heart rate- >40 beats per 80-140 Beats/minute
minute, <130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, 90-100 +/-10 mm Hg
Systolic BP </= 200 mmhg.
Respiratory rate >14 breaths/min and 20-30 Breaths/minute
Respiratory rate <35 breaths /
min
SpO2 >95% on room air>/= 90% on 90-95% on room air
4lit/min of oxygen.
Admission & Discharge Criteria PICU (Pediatric Intensive Care Unit)
ADMISSION CRITERIA :
Physiological criteria for mandatory admission :
1. Any child with unstable airway or need for artificial airway
2. Any child with moderate to severe respiratory distress or respiratory failure.
Intensive Care Manual Controlled Copy Quality Department 21
3. Any child with unstable or potentially unstable circulation despite adequate fluid
resuscitation.
( SBP less than 5th percentile for the given age and sex)
4. Child with acutely diminished level of consciousness or a decreasing level of consciousness.
5. Child with status epilepticus or in post-octal state.
6. Children requiring acute renal support or having complication of rental failure like oliguria ,
acute dyselectrolytemia.
7. Children with fulminant hepatic failure requiring intensive monitoring.
8. Some children who appear to be stable but have the potential to rapidly decompensated (
Eg;
Toxic ingestions , major electrolyte disturbances, severe DKA)
Procedural categories for mandatory admission :
9. All pediatric ( up to 16 years ) post -operative patients after cardiothoracic surgery
10. All neonates for post -operative care.
11. All children with major surgeries like neurosurgery and major abdmonial surgeries requiring
intense monitoring.
12. All children after liver transplant for post - operative care.
DISCHARGE CRITERIA :
Absolute criteria :
1. Child with partial or complete resolution of the physiological indication for admission into
PICU and stable hemodynamics.
2. Child who is maintaining spo2 95 % with 5 litres of o2 through face mask (or) 2 laters of o2
through nasal cannula with stable hemodynamics.
Transfer /Discharge shall be based on the following:
1. Stable hemodynamics
2. Stable respiratory status (stable gas exchange)
3. Minimal oxygen requirements that do not exceed patient care unit guidelines
4. Intravenous ionotropicsupport,vasodilators and anti-arrhythmic drugs are no longer
required
5. No life threatening electrolyte imbalances
6. Removal of all hemodynamic monitoring catheters
7. Patient with mature artificial airways (tracheostomies) who no longer require excessive
Suctioning
Intensive Care Manual Controlled Copy Quality Department 22
ADMISSION & DISCHARGE CRITERIA (COVID 19 ICU)
ADMISSION CRITERIA
All the patients who are admitted to this unit are tested positive for RTPCR for SARS CoV2 and
should be less than or equal to 14 days from positive test. Patients are admitted to this unit for
evaluation and treatment of illness that may lead to acute organ failure or may progress to
death, that are amenable to treatment, and that require various forms of life support (like
mechanical ventilation) intensive monitoring (including intravascular pressure monitors),
frequent evaluation (including laboratory tests), continuous medication infusions, and/or
intensive nursing care. Admission decisions are made based on complete evaluation of the
patient’s medical and nursing requirements. Paediatric patients as well as adults are provided
admission to this unit. In case of situation like bed shortages, other specialty patients may also
be admitted.
Q. Respiratory System:
Severe Covid 19 patients whose respiratory rate is more than 24, Spo2 is less than 94
%, requiring more than 4 litres/min.
Acute respiratory failure, (type 1 or type 2), Pao2 less than 50 mm Hg; Paco2>60
mm Hg requiring ventilator support. (Invasive or non-invasive support).
Chronic respiratory failure with altered sensorium.
Patients who are need monitoring to assess and treat respiratory deterioration.
Require monitoring / protection of airway patency.
Require frequent tracheal suctioning or chest physiotherapy.
Acute airway obstruction.
Massive haemoptysis.
Pulmonary embolism with hemodynamic instability.
Perioperative respiratory failure
R. Cardiovascular system
Hemodynamic instability
Systolic blood pressure less than 90 mmHg within last 24 hours and who require
vasopressors.
Acute coronary syndrome
Primary PTCA, Elective Angiogram and stenting.
Complex arrhythmias requiring close monitoring and intervention
Acute congestive heart failure with respiratory failure and / or requiring
hemodynamic support
Intensive Care Manual Controlled Copy Quality Department 23
Hypertensive emergencies
Unstable angina, particularly with dysrhythmias, hemodynamic instability, or
persistent chest pain.
Cardiac arrest
Cardiac Tamponade or constriction with hemodynamic instability
Dissecting aortic aneurysms.
S. Gastrointestinal system
Acute upper or lower GI tract haemorrhage causing orthostatic hypotension or
blood loss requiring multiple transfusions.
Hepatic dysfunction causing encephalopathy.
Inflammatory bowel disease causing ileus or peritonitis.
Severe acute pancreatitis.
T. Renal system
Acute kidney injury.
Acute or Chronic kidney disease.
Patients requiring dialysis support like CRRT, Peritoneal dialysis.
U. Endocrine system
Diabetic ketoacidosis.
Thyroid storm or myxoedema coma.
Hyperosmolar coma.
Adrenal crisis with hemodynamic instability or other endocrinal problems with
hemodynamic instability.
Hypo or hypernatremia with seizure, altered mental function.
Hypo or hypernatremia with dysrhythmias or muscular weakness.
Severe hypocalcaemia/ severe hypercalcemia with altered mental status or
requiring hemodynamic monitoring.
Hypo or Hyper magnesium with hemodynamic or respiratory compromise or
dysrhythmias.
V. Haematology system
Thrombocytopenia with active bleeding
Coagulopathy with active bleeding
W. Infectious /Environmental agents
Severe sepsis and sepsis shock
Acute meningitis with neurological abnormalities
Intensive Care Manual Controlled Copy Quality Department 24
Acute poisoning with depressed level of consciousness or airway compromised,
hemodynamic instability or cardiac arrhythmias.
Acute drug withdrawal syndromes with hemodynamic instability.
Environmental injuries (lightening, near drowning, hypo-hyperthermia)
Scorpion, snake bite with hemodynamic and respiratory dysfunction
Neurological system:
Fall in Glasgow com score less than 15 within 24 hours with need for continuous
monitoring.
Uncontrolled seizures.
Progressive muscle weakness involving respiratory muscles.
Intracranial masses associated with acute or progressive neurologic dysfunction.
Physiological admission Criteria
S.N Sudden deterioration in patient’s Greater Than (>) Lesser Than (<)
o. condition as evidenced by :
1 Heart Rate >130 / Min <40 / Min
2 Respiratory Rate >24/ Min
3 Systolic Blood Pressure >200 mmHg <90 mmHg
4 Oxygen Saturation - <94% @ more than
4Lt/min
5 Urine Output - <50 cc over 4 hours
6 Random Blood Sugar - <60 mg%
7 Neurological Nature:
1 Sudden Deterioration in the Level of consciousness(GCS fall of >2)
2. Repeated prolonged seizures
Recent non-traumatic subarachnoid hemorrhage and intracranial bleeding.
Recent cerebral infarction associated with diminished level of consciousness of
progressive focal deficits.
Coma, Metabolic, toxic or anoxic.
Patients in com from acute structural brain disease or injury but who do not have an
acute intracranial mass.
Post operative craniotomies.
Intensive Care Manual Controlled Copy Quality Department 25
Post operative intracranial stereotactic biopsies.
Post operative extracranial cerebrovascular cases.
Post operative laminectomies with an unusual risk of hematoma.
Meningitis with altered mental status or respiratory compromise
Note: Hemodynamic instability is defined as-
Pulse rate less than 50 beats/min or more than 150 beats/minute.
Systolic blood pressure (SBP) less than 90mm Hg or 40 mm Hg drop of systolic Blood
pressure.
Diastolic blood pressure more than 120mm Hg.
Mean arterial pressure less than 60 mm Hg.
DISCHARGE CRITERIA
Any patient with COVID19 who is being transferred to Non covid units of hospital (either ICU
or Ward) has to complete more than 14 days after the positive RTPCR test for SARS Cov2.
ICU Patients with Covid 19 and who has not completed 14 days of isolation will be shifted to ID
ward after meeting physiological criteria for discharge from ICU.
Patients with Covid 19 are discharged from the ICU when their acute illness is treated, their
medical condition has stabilized, and they do not require frequent evaluation (including
laboratory tests), continuous medication infusions, and/or intensive nursing care.
Discharge decisions are made based on complete evaluation of the patient’s medical and
nursing requirements.
R. Respiratory system
Treatment and reversal of respiratory failure with stable haemodynamics
S. Cardiovascular system
Blood pressure within acceptable range without inotropic support.
Symptomatic Bradycardia or tachycardia reversed.
Not requiring continuous infusions of vasoactive drugs or antiarrhythmic agents.
T. Gastrointestinal system
No orthostatic hypotension and hematocrit stable for previous 24 hours.
Stable or improving hepatic encephalopathy.
Ileus or peritonitis resolving.
U. Renal system
Oliguria corrected or stable on hemodialysis.
V. Endocrine system
Intensive Care Manual Controlled Copy Quality Department 26
Correction of diabetic emergencies with treatment stabilizing blood sugar for 24
hrs.
W. Hematology system
Control of bleeding and correction of thrombocytopenia
Correction of INR with control of bleeding
Stable hematocrit for 24 hrs
X. Infectious/Environmental agents
Resolving Sepsis with acceptable blood pressure.
Stable or improving neurological function with resolving acute meningitis.
Stable with airway protection with resolving acute poisoning, without need for
further monitoring.
Y. Relative physiologic indications for discharge from the COVID 19 ICU
55. Resolution of primary disease, (as per treating / ICU team)
56. Able to protect airway on his/her own or with a tracheostomy tube.
57. Overall GCS of 15/15
58. No fresh Neurological deficits in the last 12 hours, or no worsening of existing
deficits.
59. Critical lab parameters within satisfactory range, (Eg- Sodium- >130 mmol/lit,
Potassium > 3 mmol/lit.)
60. Post op wound status- healthy with drains less than 50% of container.
61. Not requiring any form of organ support for at least more than 24 hours (Ventilator,
Bi Pap Etc.)
62. Stable hemodynamic parameters without any inotropic requirement for at least 24
hours
Parameter Adults
Temperature 98.6 degree F +/- 1.5
Heart rate Heart rate- >40 beats per minute, <130 beats/ minute.
BP Diastolic BP >/= 90 mmhg, Systolic BP </= 200 mmhg.
Intensive Care Manual Controlled Copy Quality Department 27
Respiratory rate >14 breaths/min and Respiratory rate <35 breaths / min
SpO2 >95% on room air>/= 90% on 4lit/min of oxygen.
2. TRIAGE FOR ICU
Under ideal conditions patients shall be admitted or discharged strictly on their potential to
benefit from ICU care. Unfortunately, in many instances the number of potential ICU patients
exceeds the available beds. A method of prioritizing or triaging patients is necessary. Initial
triage or patients may follow the guidelines given in the prioritization model. In an environment
where ICU admissions are rigorously screened for benefit and discharge is ongoing and
continuous, the need for triage is minimized. Triage decisions are made explicitly, and without
bias. Ethnic origin, race, sex social status, sexual preference or financial status is never
considered in triage decisions.
Prioritization Model
This system defines those that shall benefit most from the ICU (Priority 1) to those that shall
not benefit at all (Priority 4) from ICU admission.
Priority 1: These are critically ill, unstable patients in need of intensive treatment and
monitoring that cannot be provided outside of the ICU. Usually, these treatments include
ventilator support, continuous vasoactive drug infusions, etc. Priority 1 patients generally have
no limits placed on the extent of therapy they are to receive. Examples of these patients may
include post-operative or acute respiratory failure patients requiring mechanical ventilatory
support and shock or hemodynamically unstable patients receiving invasive monitoring and/or
vasoactive drugs.
Priority 2: These patients require intensive monitoring and may potentially need immediate
intervention. No therapeutic limits are generally stipulated for these patients. Examples include
patients with chronic comorbid conditions who develop acute severe medical or surgical illness.
Priority 3: These unstable patients are critically ill but have a reduced likelihood of recovery
because of underlying disease or nature or their acute illness. Priority 3 patients may receive
intensive treatment to relieve acute illness but limits on therapeutic efforts may be set such as
no intubation or cardiopulmonary resuscitation. Examples include patients with metastatic
malignancy complicated by infection, cardiac tamponade, or airway obstruction.
Intensive Care Manual Controlled Copy Quality Department 28
Priority 4: These are patients who are generally not appropriate for ICU admission. Admission
of these patients shall be on an individual basis, under unusual circumstances. These patients
can be placed in the following categories:
A. Little or no anticipated benefit from ICU care based on low risk of active intervention that
could not safely be administered in a non-ICU setting (too well to benefit from ICU care).
Examples include patients with peripheral vascular surgery; hemodynamically stable diabetic
ketoacidosis, mild congestive heart failure, conscious drug overdose, etc.
B. Patients with terminal and irreversible illness facing imminent death (too sick to benefit
from ICU care). For example: severe irreversible multi-organ system failure, metastatic cancer
unresponsive to chemotherapy and/or radiation therapy (unless the patient is on a specific
treatment protocol), patients with decision-making capacity who decline intensive care and/or
invasive monitoring and who receive comfort care only, brain dead non-organ donors, patients
in persistent vegetative state, patients who are permanently unconscious, etc.
2. PERFORMANCE REVIEW
The performance evaluation and review of an ICU shall include its admission/ discharge/triage
policy. A multi-professional team shall review performance at least annually. In order to
adequately review performance as it relates to admission, outcome, and the decision-making
process.
Administrative Recommendations to Facilitate Appropriate Admissions, Discharges and
Delivery of Intensive Care Units
The ICU Coordinator shall be appointed on the basis of training, interest, type of practice, and
availability and who can give clinical, administrative and educational direction to the Intensive
Care Unit.
The ICU Coordinator shall assume responsibility for assuring the quality, safety, and
appropriateness of care in the Intensive Care Unit.
The ICU Coordinator shall work collaboratively with the Coordinators of other areas in the
institution so that patient care, triage, and patient flow are effective and efficient.
Intensive Care Manual Controlled Copy Quality Department 29
Following indices (but not restricted to) shall be regularly monitored to review the
performance of each ICU:
VAP
CLBSI
CAUTI
Needle stick injuries
Patient falls
Compliance to IPSG
The first three shall be visually tracked also using a green star which shall be displayed in every
ICU.
The data shall be collected and analyzed regularly.
The data shall also be presented in Infection control committee by the respective ICU in-
charges on a monthly basis.
Quality improvement projects shall be based on incidents reported, data trends and other
reported issues/ feedback. Monthly review of the data shall be done with the CEO as part of the
centre of excellence activity in critical care. Annual reviews will also happen to review the
requirements and other improvements.
Intensive Care Manual Controlled Copy Quality Department 30
3. BED SHORTAGE POLICY
SUBJECT: Contingency plan for handling a shortage of Intensive Care Beds in Intensive Care
Units
PURPOSE
This policy issuance sets forth a contingency plan for handling a shortage of intensive care beds
in any of the ICUs.
POLICY
1. When no bed is available in a given ICU for a patient needing admission to that ICU, and
when, in the opinion of the Consultant, no patient presently occupying a bed in that ICU can
be moved to a general patient care unit, physicians in that ICU may seek to locate a bed in
the other ICU.
2. If a bed is available in an alternate unit, the patient may be admitted to that unit only with
the consent of its Consultant. Responsibility for medical care of the patient shall rest with
the staff of the unit to which the patient has been admitted.
3. Consultants of the two ICUs agree to allow other units’ Consultant to admit and care for a
critically ill patient in their unit, when shortages as outlined here arise, unless there are
medical contraindications. Aside from those exceptions, one ICU group shall be allowed to
“borrow” an ICU bed in another unit with the understanding that this represents a
temporary admission, and that the patient shall promptly be returned to the appropriate
ICU as soon as a bed is available.
4. Because a bed shortage may occur at any hour of the day or night, each ICU coordinator
shall have ultimate responsibility for deciding which patient, if any, may be moved from that
ICU to make room for a case more urgently in need of specialized care.
BED BOOKING
Each ICU maintains a bed booking register. Patients’ status is to be indicated in the register. In
case of two or more patients requiring the same bed, patient with the higher priority category
shall get preference. The second patient is to be relocated to another ICU.
Intensive Care Manual Controlled Copy Quality Department 31
4. INFECTION CONTROL IN ICU
A. Prevention and containment of Hospital Associated Infections (HAI) / nosocomial infection
is a fundamental principle of effective medical practice.
B. The critically ill patient is highly vulnerable to nosocomial infection, which results in
significant morbidity, prolonged length of hospital stay, increased cost and attribute
mortality.
C. It is the responsibility of every member of the health care team to ensure compliance with
hospital and unit infection control policies. This may include reminding senior colleagues or
visiting teams to conform to basic issues such as hand washing or barrier nursing measures.
D. If you are reminded by a colleague to conform to these policies (for example hand-washing
after examining a patient), then this shall not be regarded as a criticism, but rather as
responsible practice.
E. Hand-washing remains the only established method of effective infection control and shall
be religiously performed by all members or the health care team.
1. Compulsory before and after entering a patient’s cubicle for
a. Physical examination of the patient
b. Manipulation of patient’s environment including respiratory equipment, infusion
pumps, dressings, drains, linen or bedding.
c. Inspection or handling or the patient chart, case notes etc. when these are placed
inside the cubicle.
d. Following all procedures, even if aseptic techniques are used.
2. This may be performed by washing for a minimum of 01 minute using Micro shield
hand cleanser (at the basin closest to, or within the patient’s cubicle) (or by soap and
water or by alcohol based hand rubs, For example AHD 2000/Sterilium)
F. Gloves
1. Disposable gloves shall be worn for all contracts with patient’s body fluids, dressings
and wounds.
2. The use of gloves is not a substitute for hand washing before and after patient
contact.
3. Gloves shall be disposed of in appropriate waste disposal containers.
G. Barrier nursing measures
The following patients are regarded as infective risks requiring barrier nursing.
1 Infection or colonization with
(a) Methicillin Resistant Staphylococcus Aureus
(b) Vancomycin Resistant Enterococcus
(c) Multiresistant Gram Negatives
Intensive Care Manual Controlled Copy Quality Department 32
(d) Toxin A Producing Clostridium Difficile.
2. Burns
3. Febrile Neutropenia
4. High risk immunosuppressed patients as directed by Infection Control Team.
H. Aseptic technique
Aseptic technique is to be used for all patients undergoing major invasive
procedures (refer to procedures section). This includes:
a. Hand disinfection: surgical scrub with Chlorhexidine / Povidone Iodine for more
than 1 minute.
b. Sterile barrier: full gown, mask, disposable caps, gloves and sterile drapes.
c. Skin preparations with chlorhexidine.
d. Proper sharps disposal.
e. The person performing the procedure is responsible for disposal of all sharps
(needles, blades) using the sharp disposal containers.
f. Nursing staff is not responsible for cleaning-up sharps after a medical procedure.
I. “Traffic control”
1. Movement of people through the Unit shall be kept to a minimum. This
applies equally to visiting clinicians and large numbers of relatives.
2. All visitors are expected to conform to the above infection control measures and are
to be tactfully reminded or instructed about these issues.
3. All the visitors are advised to wash their hands before leaving the ICU.
4. All the visitors to the ICU shall be instructed (by the nursing staff) regarding the
infection control policies.
5. GUIDELINES TO MEDICAL STAFF
A. Admitting a new patient
1. Obtain as much information as possible from relatives and referring physicians.
2. Primary survey
a. Ensure adequate airway, breathing and place patient on highest FiO2 if needed.
b. Check circulation and venous access
3. Secondary survey fully examine patient
a. Document essential orders
i. Ventilation
ii. Sedation / analgesia
iii. Drugs, infusions
iv. Fluids
4. Outline plan to nursing staff.
5. Secure appropriate basic monitoring/ procedures
a. SpO2
b. ECG
c. Arterial line, if needed
Intensive Care Manual Controlled Copy Quality Department 33
d. Nasogastric tube
e. CVP monitoring if needed
6. Basic investigations
a. Routine biochemistry, blood picture and coagulation studies.
b. Microbiology as indicated.
c. Arterial blood gas as indicated.
d. CXR
7. Assess the need for advanced investigations CT, angiography, MRI, etc.
8. Advanced monitoring where indicated for example, PA catheter, ICP, SjvO2
9. Document the details in case notes.
10. Inform and counsel relatives.
B. Daily management
1. Daily investigations
a. Routine blood tests (Biochemistry and Hematology) are ordered on the physician
Order Sheet. Drug levels or other tests are requested as required.
b. The night duty nurses or phlebotomist shall take the bloods at 0600h.
c. The junior medical staff is responsible for taking blood samples when the nursing
staff request assistance.
d. Chest x-rays are ordered before 0800h
e. Handover ward rounds are at 0900h and 1700h. These are brief business rounds
to handover essential information to the next team (either day or night) and are
attended by the unit residents, registrars and nurses.
f. Complex investigations (for example, CT, MRI scans) and procedures shall be
authorized by the Senior Consultants.
C. Documentation
The following guidelines are designed to facilitate the recording of clear, relevant
information that is essential for continuity of care, audit and medico legal review.
Entries shall establish a balance, being concise but still accurately recording all relevant
information and events.
1. Documentation by ICU registrars includes
a. Admission note for all patients admitted to ICU and HDU
b. Daily entry in case notes
c. Discharge Summary
d. Death Certificate
e. In-house Transfer Summary
f. Physical Restraint Form.
2. ICU Admission Note
a. All patients admitted to the ICU shall have an admission summary
Intensive Care Manual Controlled Copy Quality Department 34
b. The Senior Consultant shall be notified and invited to record an admission
summary for patients admitted directly to ICU.
c. The admission note shall incorporate all relevant aspects of the patient’s medical
history, clinical examination and results of appropriate investigations.
3. Daily Progress Note in ICU
a. A daily entry shall be made in the case notes
i. Notes are most efficiently recorded after the 1000h ward round so that
current results and management plans are recorded.
ii. Notes shall mention plan of care, pain assessment, effect of medication,
patient and family education.
b. Additional notes shall be made for the following
i. Significant changes in physical condition necessitating changes in
management, for example, renal failure requiring dialysis.
ii. Major procedures, for example, laparotomy, tracheostomy.
iii. Results of specific investigations or test, for example, CT scans, endocrine
tests.
iv. Changes in policy, e.g. non-escalation of treatment, advance directives.
4. In-House Transfer Forms
a. All patients transferred out of ICU require an In-House Transfer form to be
completed.
b. This is a single page document outlining all relevant transfer information.
c. The reverse side of the form is a nursing transfer summary, which shall be
completed by the attending nurse.
d. The duty registrar on day of transfer is responsible for completing the form.
Incomplete or missing summaries shall be forwarded to the responsible registrar
for completion.
5. Consent in ICU
a. Competent patients
i. All competent patients undergoing invasive procedure in ICU shall have
Consent for Procedure completed and signed by the patient.
b. Incompetent patients (sedation, coma or encephalopathy)
i. Third party consent will be taken for routine ICU procedures, these include.
(a) Endotracheal lines
(b) Arterial lines
(c) Central venous lines
(d) Pulmonary artery catheters
(e) Transvenous pacing wires
(f) Underwater seal drains
(g) Intra-aortic balloon Counterpulsation
(h) Bronchoscopy
Intensive Care Manual Controlled Copy Quality Department 35
ii. However, relatives shall be informed prior to the procedure if present and
the indications, conduct and complications of the procedure shall be clearly
documented in the case notes.
iii. Major invasive procedures such as percutaneous tracheostomy, coronary
angiography, permanent pacemaker insertion or acute surgical procedures
require completion of a consent form.
(a) Emergency procedures are done by informing the patient attender if not
present at the ICU and signature taken once they come to ICU.
(b) Non-urgent procedures by third party consent (next-of-kin)
iv. Ultimate responsibility for consent lies with the operator performing the
procedure, however junior medical staff shall ensure appropriate consent is
obtained.
v. Relatives shall always be informed of any procedures and the consent issue
explained.
D. ICU Ward Round.
1. The daily ICU 10 00h ward round is an integral feature of the running of the Unit. It is
the forum to openly discuss management issues and is a useful teaching forum.
2. Junior medical staff is expected to present their allocated patients at this round and to
actively participate in the discussion. Presentations at this round shall be of a standard
suitable for a fellowship examination.
3. The ward round is attended by
a. ICU consultants, registrars and residents
b. Nursing staff
4. Presentation at ward round
Presentation shall take no more than 5-10 minutes
Emphasize the relevant and pertinent issues only
a. Patient details and demographics
b. State day of ICU admission (for example, Day 6 ICU)
c. Diagnosis or major problems
d. Relevant pre-morbid history pertinent to this admission
e. Relevant progress and events in ICU (deterioration/ improvement, procedures,
investigations)
f. Current clinical status (system by system)
g. Outline features on daily basis for Pathology and Radiology
h. Current plan of management
i. Medications
j. Further investigations / procedures
k. Discharge / Prognosis
Intensive Care Manual Controlled Copy Quality Department 36
5. Laboratory results
Biochemistry, hematology and coagulation results for the 10.00hr ward round will be
collected if not shall be obtained by the ICU Secretary, either by phone or via the
computer terminals in each nursing station.
E. Hospital Emergencies
1. In case of any emergency, inform the concerned authorities, state nature and location
of emergency. (Following The Safety Manual / The Red Book)
2. Fire (follow the Safety Manual)
a. A copy of the hospital Safety Manual (fire, smoke, and bomb-threat) is kept in all
nursing stations.
b. The Fire Officer is the overall controller during a fire or smoke emergency (Code
Brown).
c. Become familiar with the location of fire exits, extinguishers and blankets in the unit.
i. Unless a fire is small and easily contained do not attempt to fight the fire
yourself.
ii. Remove yourself from the immediate vicinity of the fire, alerting other staff
members as indicated.
iii. Wait for the arrival of the Fire Officer and assist in any patient movement/
evacuation only as indicated by the Fire Officer.
iv. In the event of a significant fire / smoke hazard, staff shall only re-enter the
danger zone in the immediate company of a fire fighter, with appropriate
breathing apparent.
6. CLINICAL PROCEDURES
I. Introduction
1. Junior medical staff is encouraged to become proficient in all intensive care procedures.
2. Invasive procedures shall only be authorized by the Senior Consultant.
3. Adequate familiarization and supervision with unfamiliar procedures is essential there is
always someone available to help.
4. The relative risk vs. benefit of all procedures shall be carefully considered
5. Do not persist if you are having difficulty with the procedure: call for help
6. Consent for procedures: * refer to Hospital Policies
a. Competent patients undergoing invasive procedures shall have the Consent Form
completed and signed by the patient.
b. Third party consent is necessary for incompetent patients undergoing routine ICU
procedures.
c. Major ICU procedures such as percutaneous tracheostomy or enterogastrostomy
require third party, or two-doctor consent.
Intensive Care Manual Controlled Copy Quality Department 37
7. Indications, conduct and any complications of the procedure shall be clearly
documented in the case notes in addition to a consent form if this is completed.
8. Discuss the planned procedure with the ICU nursing staff and allow sufficient time for
setting up of trays and equipment. Remember: the nursing staff has extensive
experience with these procedures.
9. It is the responsibility of the operator to discard all sharps used in the procedure and to
ensure that they are placed in a sharps disposal container as per protocol.
II. Procedures
1. Junior medical staff is expected to become proficient in all routine procedures.
2. Specialized procedures are done by the Consultant or strictly under Consultant
supervision.
3. Protocols for the under mentioned routine and specialized procedures are outlined in
the following sections.
Routine ICU procedures
1. Endotracheal intubation
2. Central venous catheterization
3. Arterial cannulation
4. Urinary catheterization
5. Lumbar puncture
6. Epidural catheterization
7. Underwater seal drain insertion
8. Pleurocentesis
9. Peritoneocentesis
10. Nasogastric tube insertion.
Specialized ICU procedures
1. Fiber-optic bronchoscopy
2. Transvenous pacing
3. Pericardiocentesis
4. Esophageal tamponade tube insertion
5. Intra-aortic balloon counterpulsation.
A. PERIPHERAL IV CATHETERS
1. Indications
a. All ICU patients require IV access
b. Stable ICU patients where a CVC is no longer necessary.
2. Management protocol
Remove all resuscitation lines inserted in unsterile conditions as soon as possible.
Local Anesthesia in awake patients while placing IV catheter
Intensive Care Manual Controlled Copy Quality Department 38
Aseptic technique
- Hand wash and gloves
- Skin preparation.
Dressing: adhesive Non-occlusive
Change / remove all peripheral lines after 48 hours.
a. COMPLICATIONS
Infection
Thrombophlebities
Extravasation in tissues
B. ARTERIAL CANNULAE
a. INDICATIONS
Patients in severe hypotension requiring continuous monitoring of arterial blood
pressure
Multiple blood gas and laboratory analysis
b. MANAGEMENT PROTOCOL
Remove and replace lines inserted in unsterile conditions as soon as possible.
Brachial and ulnar arterial lines should be changed as soon as Radial or femoral
arteries are available.
Aseptic technique:
- Hand wash and gloves.
- Skin preparation with 5% Betadine/ chlorhexidine
Local anesthesia in awake patients.
Sites: (in order of preference): Femoral, Radial, Ulnar, dorsalis pedis and brachial.
The Femoral artery may be the sole option in the acutely shocked patient.
Dressing: Occlusive transparent dressing
There is no optimal time for an arterial line to be removed or changed.
Intra-arterial Cannula is changed/removed only in the following settings:
- Distal ischemia
Intensive Care Manual Controlled Copy Quality Department 39
- Mechanical failure (over damped waveform, inability to aspirate blood)
- Evidence of unexplained systemic or local infection
- Invasive pressure measurement or frequent blood sampling is no longer
necessary.
Measurement of pressure
- Transducers should be 'zeroed' at the mid-axillary line in the 4th intercostal space.
(phlebostatic axis)
Maintenance of lumen patency
- Heparinised Saline flush (1u/ml) – 3ml/hr
c. COMPLICATIONS
Infection
Thrombophlebities
Digital ischemia
Vessel damage / aneurysm
HIT ( Heparin induced thromocytopenia)
C. CENTRAL VENOUS CATHETERS
Note: Registrars shall be familiar with the interpretation and limitation of haemodynamic
variables derived from central catheters (CVC and PAC) in critically ill patients.
a. INDICATIONS
- Fluid administration
- TPN, hypertonic solutions.
- Vasopressors/ ionotropes infusions
- Monitoring of right atrial pressure (CVP)
Venous access for:
- Pulmonary artery catheterization (PAC)
- Continuous renal replacement therapy, plasmapheresis.
- Transvenous pacing.
Intensive Care Manual Controlled Copy Quality Department 40
b. MANAGEMENT PROTOCOL (APPLIES TO ALL TYPES OF CVC)
- SITES
- Internal jugular is the preferred site for routine stable patients, followed by
subclavian vein cannulation.
- Femoral access is preferable where:
a. Limited IV access (burns, multiple previous CVC’s),
b. Thoracic approach is considered hazardous:
Severe respiratory failure with high PEEP.
Hyper expanded lung fields (severe asthma, bullous lung disease)
- Uncontrolled Coagulopathy (use Femoral approach or PlCC)
TECHNIQUE POLICY
- Local anesthesia in .awake patients.
- Strict aseptic technique at insertion:
a. Hand disinfection: Surgical scrub with Chlorhexidine or 5%betadine for
more than 1 minute
b. Sterile barrier: gown, glove, cap and mask and sterile drapes.
c. Skin preparation with chlorhexidine or 5%betadine
- Seldinger technique only.
- Suture all lines
- Dressing: non-occlusive dressing
- Flush all lumens with Heparinised Saline
- Check CXR prior to use.
MAINTENANCE
- Daily inspection of the insertion site and clinical examination for infection
irrespective of duration of insertion.
- Catheters are left in place as long as clinically indicated changed when:
a. Evidence of systemic infection
o New, unexplained fever
Intensive Care Manual Controlled Copy Quality Department 41
o Unexplained rise in WBC
o Deterioration in organ function
b. Evidence of local infection - inflammation or pus at the insertion site.
c. Central line blood stream infections will be described later
- Guide wire exchanges are actively discouraged. They may be indicated in the
following situations
a. Mechanical problems in the existing catheter (leaks or kinks)
b. Difficulty in the access
- Maintenance oflumen patency
a. Central venous catheters.
o Withdraw 2ml and discard,
o Flush with 2ml normal saline.
o Flush 2ml solution of Hepsaline.
c. COMPLICATIONS
- At insertion
a. Arterial puncture
o Hematoma with mass effect
o Arterial thrombosis/embolism
b. Pneumothorax, Hemothorax, Chylothorax
c. Neural injury (Phrenic, Brachial Plexus, Femoral Nerve)
- Passage of wire/catheter
a. Arrhythmias
b. Perforation of SVC, RA, Tamponade
- Presence of catheter
a. Catheter infection: rates increase under the following conditions
o Size of catheter - thicker catheters (Pulmonary Artery catheters)
o Site of catheter - Femoral more often than Internal Jugular, more than
Subclavian sites
o Increased number oflumens
Intensive Care Manual Controlled Copy Quality Department 42
- Nature of fluid through catheters –
a. TPN requires dedicated lumen
b. Dextrose / normal saline , hypertonic solutions.
Complications
a Thrombosis
b Catheter/Air embolism
c. Knotting of catheters (especially PAC)
d. Pulmonary infarct I arterial rupture (PAC)
e. HIT
NOTE: Where insertion ofa CVC presents "significant risk" in a non-urgent situation,
consider insertion ofa PICC line as an alternative.
D. URINARY CATHETER
1. Standard in all ICU patients
2. Management protocol
a. Aseptic technique at insertion
i. Hand disinfection: surgical scrub with Chlorhexidine for more than 1 minute
ii. Sterile barrier: gloves and sterile drapes
iii. Skin preparation: Chlorhexidine 1%
b. Local anesthesia gel in all patients
c. Foley catheters can be changed to Silastic if prolonged catheterization is anticipated.
d. Remove catheters in anuric patients and perform intermittent catheterization
weekly, or as indicated.
E. EPIDURAL CATHETERS
INDICATIONS
- Postoperative pain relief
- Analgesia in chest trauma, trauma to abdomen, acute pancreatitis, lower limb
crush injuries.
MANAGEMENT PROTOCOL
- Notify the Anesthetist of any epidural to be placed
Intensive Care Manual Controlled Copy Quality Department 43
- Strict aseptic technique at insertion.
- Daily inspection of the insertion site. The catheter should not be routinely
redressed, except under the advice of the Anesthetist.
- Leave in for a maximum of 5 days and then remove.
- Remove if not in use for more than 24 hours or clinical evidence of unexplained
sepsis
- Heparin / Warfarin, LMWH follow guidelines
COMPLICATIONS
- Hypotension from sympathetic blockade / relative hypovolemia
-This usually responds to adequate intravascular volume replacement
- Pruritis, nausea and vomiting, or urinary retention (Opioid effects)
- Post-dural puncture headache
- Infection: epidural abscess
- Pneumothorax
- Total spinal anesthesia
F. PULMONARY ARTERY CATHETER
POLICY
- Insertion of PA catheters should be authorized by the Senior Consultant.
- Become familiar with the theory of insertion, indications, interpretation and
complications of PACs
- Insertion of PA catheters should never delay resuscitation of shocked patients.
- Allow sufficient time for nursing staff to set up insertion trays and transducer
manifolds.
- Remove catheters once they are not being routinely used
INDICATIONS
- Hemodynamic measurement (cardiac output, stroke volume, SVR)
a. Diagnostic assessment of shock states (cardiogenic, hyperdynamic hypovolemia)
b. Assessment of response to treatment in the above
Intensive Care Manual Controlled Copy Quality Department 44
- Measurement of right heart pressures (RAP, PAP):
a. Acute pulmonary hypertension
b. Pulmonary embolism
c. Cardiac Tamponade
- Estimation of preload / left heart filling (P AOP)
a. lntravascular volume status
b. LVF
c. Response to fluid loading
MANAGEMENT PROTOCOL
- Insertion protocol as per CVC
- Specific features of PACs
- Insertion protocol
a. Sheath introducer (8.5 Fr) with side port, haemostatic valve and plastic
contamination shield.
b. Shared transducer forRAP (proximal) and PAP (distal) Lumens
c. Check competence of balloon and concentric position
d. Ensure all lumens are flushed with Heparinised Saline prior to insertion
e. Ensure adequately zeroed system and appropriate scale (0-40mmHg) on monitor
prior to insertion.
f. Insert catheter using changing waveforms (RA, R V, P A) on monitor with balloon
inflated and locked until catheter displays Pulmonary Artery occlusion tracing:
usually 50cm on catheter in most patients using Subclavian and left internal
jugular approach; right internal jugular 40 cm.
g. Deflate balloon and ensure adequate PAP trace. Adjust catheter depth until a P
AOP trace appears with I - 1.5ml air in balloon.
h. Suture introducer and attach contamination shield to the hub of the introducer.
o Apply a non-occlusive dressing.
o Ensure an adequate P A tracing is on the monitor at all times
o "Wedged" tracings should be corrected as soon as possible:
Intensive Care Manual Controlled Copy Quality Department 45
a) Flush distal lumen with 2ml normal saline
b) Withdraw the catheter until a P A trace is visible
o Measurement of pressures:
a) Reference pressures to the mid axillary line
b) Measure at end-expiration of the respiratory cycle
c) Do not disconnect ventilated patients to measure pressures.
d) Measurement of PAOP
(1) End expiration
(2) Use the "electronic cursor" on monitors after 2-3 respiratory cycles
o Hemodynamic measurements
(a) These are routinely performed by the nursing staff, however junior
medical staff should become familiar with the procedure.
COMPLICATIONS
- Related to CVC cannulation (see CVC section)
- Related to insertion/use of a PAC
a. Tachyarrhythmias
b. RBBB
c. Cardiac perforation
d. Thromboembolism
e. Pulmonary infarction (secondary persistent wedging) - 0- 1.4%
f. Pulmonary artery rupture - 0.06-0.2% (mortality 50%)
g. Catheter related sepsis
h. Endocarditis
i. Pulmonary valve insufficiency
j. Catheter knotting
k. Balloon fragmentation/embolism
Intensive Care Manual Controlled Copy Quality Department 46
F. PLEURAL DRAINAGE
1. INDICATIONS
- Pneumothorax
- Tension Pneumothorax may require urgent needle thoracostomy
- Haemothorax
- pneumothorax on ventilator
- Large symptomatic pleural effusion or suspected infected pleural effusion with
patient on ventilator
MANAGEMENT PROTOCOL
- 16G cannula placed in mid clavicular line, 2nd intercostal space
- Alwaysplace an UWSD following this procedure
a. PLEUROCENTESIS: (PLEURAL EFFUSION)
o Local anesthesia and sterile technique
o Cannula technique
(a) 3 way tap attached to 12 - 14 G IV cannula, syringe and rubber hose
(closed system)
(b) Remove needle from cannula and aspirate pleural effusion.
o Record volume removed and sends forinvestigations required
o Check CXR Post – procedure
b. UNDERWATER SEAL DRAINAGE (USWD)
o Local Anesthesia in awake patients.
o Strict aseptic technique at insertion: i e. full gown/glove/mask and cap:
o skin preparation with 5% betadine
o Site: mid axillary line, 3rd- 4th intercostal space
o CCU patients need large drains: 28F catheter or larger
o ICD catheter with trochar can be used for insertion of2-3 cm skin incision
parallel to the ribs
o Blunt dissection to and through intercostal space with index finger or
Howard Kelly forceps until within pleural space.
Intensive Care Manual Controlled Copy Quality Department 47
o Insert finger into pleural space to enlarge hole and insert tube directly into
pleural space or with forceps.
o Connect to underwater seal apparatus
o Insert 2 purse string sutures: 1) to fasten the tube 2) to close the incision on
removal.'
o Dressing: occlusive dressing
o Check CXR.
o Maintenance
(a) Remove or replace drains inserted in unsterile conditions as soon as
possible.
(b) Leave drain in situ until radiological resolution, no further bubbling, or
drainage (less than 150 ml/24 hours).
(c) Surgically placed drains (i.e. intraoperative placement) are the
responsibility of the surgeon
(d) If ICD catheter is blocked then remove and place a new catheter
COMPLICATIONS (minimized using the blunt technique)
- Incorrect placement (extra pleural, intrapulmonary, sub diaphragmatic)
- Pulmonary laceration (hemorrhage, fistula)
- Pneumothorax
- Bleeding
a. Local incision, intercostal vessels
b. Lung
c. IMA (with anterior placement)
d. Great vessels (rare)
- Infection: Empyema.
- Mechanical (kinking, luminal obstruction)
Intensive Care Manual Controlled Copy Quality Department 48
G. ENDOTRACHEAL INTUBATION
POLICY
- Endotracheal intubation in ICU patients is a high risk but vital procedure:
a. Usually an emergency procedure, with limited 'time.
b. It is also done as electively
c. Usually indicated for acute respiratory failure, or associated with limited
respiratory reserve.
d. Patients may have cardiovascular instability and significant co morbidities
e. Patients may have cervical spine injuries, oropharyngeal trauma/surgery
f. Patients are at risk of vomiting and aspirating
g. Positioning is difficult.
- Familiarization with the intubation trolleys, equipment and drugs is essential.
- Intubation should ideally not be done as a sole operator procedure skilled
assistance should always be sought.
- In difficult airway situations anesthesiologist help is taken
- The majority of CCU patients require rapid sequence induction.
INDICATIONS
- Institution of mechanical ventilation
- To maintain an airway
a. Upper airway obstruction
b. Patient transportation
- To protect an airway
a. Patients at risk of aspiration
b. Altered conscious state
c. Loss of glottic reflexes
- Tracheal toilet
TECHNIQUES
- Orotracheal intubation is the standard method of intubation in this unit.
Intensive Care Manual Controlled Copy Quality Department 49
- Nasotracheal intubated patients were managed in SICU with maxillofacial
surgeries
- Methods
a. Direct visualization under rapid sequence induction
b. Fibreoptic bronchoscopic awake intubation
ENDOTRACHEAL TUBES
- Standard tube: low pressure, high volume PVC oral tube.
a. Males 8- 8.5mm: secure at 21-23cm to incisors
b. Females 7-7.5 mm: secure at 19-21cm to incisors
- Double lumen tubes rarely indicated in lCU
a. Unilateral lung isolation for bronchopulmonary fistula, abscess or hemorrhage
b. These tubes should be inserted as a temporary maneuver prior to a definitive
procedure.
c. Allow differential lung ventilation
- Intubated patients from theatre may have the following tubes that are not
recommended for prolonged intubation. These tubes should be changed if
intubation anticipated more than 48 hours if safe and feasible.
a. Plain PVC tubes: change to standard EVAC translaryngeal tube
b. Armored tubes: problems:
o High pressure, low volume cuff
o Once kinked, remain kinked: beware in patients who bite tubes.
c. RAE tubes: problems
o Difficulty in suction due to bend
o Fixed length from bend: frequently advance down right main bronchus
o High pressure, low volume cuff
PROTOCOL FOR ENDOTRACHEAL INTUBATION IN CCU
- Personnel: Intubation is a 4-person procedure; skilled assistance is mandatory:
a. “Top end" incubator who coordinates the intubation
b. One person to administer drugs
Intensive Care Manual Controlled Copy Quality Department 50
c. One person to apply Cricoid Pressure once induction commences:
o This is recommended as a routine for emergency intubations
o The incubator should direct the person who is applying Cricoid pressure so
that pressure is correctly applied and removed if distortion of the Larynx
or difficulty in intubation occurs as a result.
o CP is considered safe even in the presence of suspected spinal injury.
d. Manual in line cervical spine immobilization in patients with spinal cord
injuries
- Secure adequate IV access
- Equipment kept in intubation trolleys
Ensure the following equipment is available and functional
a. Adequate light
b. Oropharyngeal airways
c. Working suction with a rigid (Yankauer) sucker
d. Bains circuit and mask
e. 100% Oxygen, i.e. working flow meter at 15 l/min
f. 2 working laryngoscopes
g. Magill forceps
h. Malleable introducer and gum elastic bougie
i. 2 endotracheal tubes
o Normal size and 1 size smaller
o Check cuff competence
j. Access to difficult intubation equipment. .
o Be aware of failed Intubation.
o Cricothyroidotomy equipment (#15 scalpel I #6.0 cuffed ETT)
- Monitoring (on all patients)
a. Pulse oximetry
b. Electrocardiography
Intensive Care Manual Controlled Copy Quality Department 51
c. Blood pressure
- Drugs
a. Induction agent (Thiopentone, Fentanyl, Ketamine, Midazolam)
b. Suxamethonium (1-2 mg/kg) is the muscle relaxant of choice.
o Contraindicated in:
(a) Burns more than 3 days
(b) Chronic spinal injuries (i.e. spastic plegia)
(c) Chronic neuromuscular disease (for example; Guillain Barre syndrome,
Motor Neurone disease)
(d) Hyperkalaemic states. (Potassium more than 5.5)
o Consider Rocuronium (1-2 mg/kg)if Suxamethonium contraindicated
c. Atropine (0.6 - 1.2 mg) if indicated
- Procedure: Rapid sequence induction and Orotracheal intubation
a. Pre oxygenate with 100% oxygen for 3-4 minutes.
b. Preload with 250-500ml crystalloid intravenously
c. Induction agent, Suxamethonium is used if necessary
d. Cricoid pressure applied
e. Direct visualization of vocal cords and tracheal intubation
f. Inflation of cuff until sealed
g. chest auscultation with manual ventilation
h. Check B / L air entry equal
i. Cricoid pressure released
j. Secure tube at correct length
k. Connect patient to ventilator (check for ventilator parameters before
connecting )
l. Ensure adequate sedation and muscle relaxant if required
m. Chest X-ray
n. Blood gas analysis as required
- Sedation post intubation
Intensive Care Manual Controlled Copy Quality Department 52
a. None if comatose or hemodynamically unstable
b. Morphine,Midazolam, Propofol, Fentanyl, Diazepam as indicated by the clinical
scenario.
MAINTENANCE OF ENDOTRACHEAL TUBES
- Tapes: Secure tubes firmly in place with adhesive tape and tube fixator.
- Cuff checks
a. Volumetric tests are done following insertion and whenever a leak is detected
with a manual hyperinflation once per nursing shift.
b. Seal is assessed by checking ventilatory parameters during normal ventilation.
- Persistent cuff leaks
a. Tubes requiring more than 5ml of air to obtain a seal or if there is a persistent
cuff leak should be examined by direct laryngoscope as soon as possible even
if the tube appears to be taped at the correct distance at the teeth.
b. Ensure that:
o The cuff has not herniated above the cords
o Tube has not ballooned inside the oral cavity and "pulled' the cuff above
the cords.
c. High -risk patients for cuff leaks
o Facial swelling (burns, facial trauma)
o Patients requiring high airway pressures during ventilation
ENDOTRACHEAL TUBE CHANGE PROTOCOL
- Ensure adequate skilled assistance, equipment, drugs and monitoring as for
denovo intubation.
- Procedure
a. Set the FI02 at 1.0 and change spontaneous modes to CMV.
b. Ensure sufficient anesthesia and muscle relaxation
c. Perform laryngoscopy and carefully identify patency of upper airway after
suction, anatomy of Larynx, degree of laryngeal exposure and swelling.
Intensive Care Manual Controlled Copy Quality Department 53
d. Clear view of Larynx and no or minimal laryngeal swelling
o Application of Cricoid pressure by assistant and careful, graded extubation
under direct laryngoscopic vision.
o Maintain laryngoscopy and replace tube under direct vision.
e. Impaired visualization of Larynx:
o Use bougie
o Place bougie through tube under direct vision and insert to a length that
would be just distal to the end of the ETT (approximately 30cm from end of
tube)
o Have an assistant control the bougie so that it does not move during
movement of the endotracheal tube
o Application of Cricoid pressure by assistant and careful, graded extubation
o Maintain laryngoscopy and ensure bougie is through the cords on
extubation
o Replace tube over bougie and guide through larynx under available vision.
f. Inflate cuff, auscultation, expired tidal volume and then release Cricoid
pressure.
g. Secure tube with tape.
Readiness to test for SBT (spontaneous breathing trail)
- Patient should be conscious, follows commands, primary disease resolving, PEEP less
than 8, Fio2 less than 0.6, PF ratio >200, heart rate <140/min, no ongoing myocardial
ischemia.
- Tidal Volume (VT) 4–6 mL/kg
- Respiratory Rate (RR) 30–38 bpm
- Total Ventilation (VE) 10–15 L/min
- RR/VT Ratio (RSBI) 60–105/L
Give a spontaneous breathing trail (SBT) once the above criteria is met
SBT is of 1) T piece 2) Pressure support ventilation 3) CPAP
Intensive Care Manual Controlled Copy Quality Department 54
Give SBT for 30minutes to 2hours
If the patient tolerates SBT well then plan for extubation
If SBT is not tolerated the look for the causes like Excessive load may be imposed by
the endotracheal tube, heat and moisture exchange devices and valves.
Intrinsic factors such as increased airways resistance, increased dynamic
hyperinflation
• Critical illness neuromyopathy, hypothyroidism, adrenal insufficiency, malnutrition.
• Cardiac dysfunction (CAD)
• Elevated B-type natriuretic peptide (BNP)
• Positive fluid balance
• Calcium, magnesium, phosphorous, potassium.
• Pleural effusion, ascites, IAP
• Overfeeding
EXTUBATION PROTOCOL
- Ensure equipment, monitoring and adequate assistance as for intubation
o Allpatients should receive supplemental Oxygen post extubation
Extubation failure- defined as reintubation within the subsequent 24–72 h.
Incidence 5–20% of patients.
Risk is greatest for medical and neurologic patients.
Reintubated patients experience increased hospital mortality, prolonged ICU and
hospital stays, and greater need for tracheostomy
Inability to protect the airway and manage respiratory secretions.
Cuff leak test can be done if suspected laryngeal oedema
I. FIBREOPTIC BRONCHOSCOPY
1. Policy
a. This is only to be used by skilled personnel and authorized by the Senior Consultant.
2. Indications
a. Difficult intubation (trained staff only): can be used as aid to failed intubation
Intensive Care Manual Controlled Copy Quality Department 55
b. Persistent lobar collapse that is refractory to physiotherapy
c. Foreign bodies
d. Diagnostic bronchoalveolar lavage (BAL)
3. Protocol for fibreoptic intubation
a. Indication as per endotracheal intubation
b. Procedure
i. All equipment, drugs and monitoring as for any intubation
ii. Supplemental Oxygen shall be given via a mask and may also be given via the
suction channel of the bronchoscope.
iii. Usually performed nasally: preparation of the nasal mucosa with topical 10%
Lignocaine.
iv. Anaesthetize pharynx with viscous Lignocaine and Larynx with transtracheal
injection, direct application through the scope or nerve blockade.
v. Check tube cuff
vi. Place warmed appropriately sized tube (7-7.5 mm tube for either sex) into
posterior nasal space.
vii. Insert scope through tube under direct vision
viii. Advance the scope into trachea under vision.
ix. Advance tube over scope into trachea and then remove scope.
x. Confirm ETT placement by ETCO2, auscultation an CXR.
4. Protocol for BAL
a. Diagnosis of nosocomial pneumonia in selected patients
i. Determination of colonization vs. infection in chronically ventilated patients.
ii. These patients shall ideally be off antibiotics for 24-48 hours
iii. Sufficient reserve to tolerate procedure.
(a) Ideally PaO2 more than 70 and FiO2 less than 0.7
(b) BAL shall commonly result in a 10% reduction in PaO2 for up to 24 hours after
procedure
b. Procedure
i. Ensure sufficient sedation.
ii. Place patient on 100% Oxygen
iii. Select lobe to be lavaged from morning CXR
iv. Local anesthetic gel is contra-indicated (interferes with culture media)
v. If possible, do not suction through scope prior to lavage (upper airway bacterial
contamination).
iii. Pass scope directly into the selected lobe
iv. Wedge scope as far as possible – ideally to third generation bronchi
v. Lavage with 4-6 x 20-40 ml Aliquot’s of sterile normal saline
viii. Aspirate between Aliquot’s and label Aliquot’s accordingly
xi. Send aspirates for quantitative culture and atypical pneumonia screening as
directed.
Intensive Care Manual Controlled Copy Quality Department 56
J. PERICARDIOCENTESIS
1. Policy
a. This procedure shall be authorized by the Senior Consultant and performed by the
junior medical staff under supervision, or Cardiology.
b. Confirmation of pericardial effusion or tamponade shall be made with
echocardiography prior to procedure. Liaison with Cardiology is essential.
2. Indications
a. Symptomatic pericardial effusion (tamponade)
3. Procedure
a. Strict aseptic technique
b. Local anaesthetic infiltration if awake patient.
c. This procedure is greatly facilitated using echocardiography guidance
d. Technique: Sedlinger technique and insertion of a pigtail catheter
i. Small incision under Xiphisternum
ii. Insert needle on syringe at 45 degree from the horizontal axis and aim for tip
of left Sheller
iii. Advance slowly and aspirate until confirmation by aspirating blood or serous
fluid.
iv. Insert catheter using Sedlinger technique over guidewire
v. Confirm placement by aspiration and / or echocardiography
vi. Check CXR (Pneumothorax)
vii. Suture and occlusive dressing if leaving for more than 24 hours.
4.Complications
a. Arrythmias
b. Cardiac tamponade
c. Myocardial laceration
d. Pneumothorax, pneumopericardium
e. Liver laceration
K. INTRA-AORTIC BALLOON PULSATION
POLICY
- The decision to insert an IABP is made in conjunction with the duty Cardiologist
and authorized by the Senior Consultant.
INDICATIONS
- As a mechanical bridge prior to and following myocardial revascularization or
transplant
Intensive Care Manual Controlled Copy Quality Department 57
- lschaemic heart disease
a. Low cardiac output states following cardiac surgery
b. Cardiogenic shock in association with angiography and revascularisation
(PTCA, stent or CABG)
c. Acute Mitral incompetence (Papillary Muscle rupture), VSD following AMI
pending operative repair.
d. Myocardial disease
o Severe myocardial contusion
o Severe myocarditis
o Cardiomyopathy
o Severe Alpha Blocker overdose.
CONTRA-INDICATIONS
- Aortic regurgitation
- Aortic dissection
- Severe peripheral vascular disease
PROCEDURE PROTOCOL
- Strict aseptic technique
- Check IABP function prior to insertion:
a. Adequate Helium cylinder volume
b. Arterial pressure manifold: referenced to mid auxiliary line in the 4th
intercostal space and correctly zeroed
c. Dedicated 5 lead ECG connected to IABP
d. Turn on and leave in standby mode
e. Initial settings
o ECG / arterial sense: 1:2 ratio
o Augmentation: minimum
o Inflate and deflate times zero
- Insertion procedure
a. Local anesthesia in awake patients
Intensive Care Manual Controlled Copy Quality Department 58
b. Scrubbed assistant recommended
c. Select size (by patient's height)
o Less than 165 cm: 34ml balloon
o More than 165 cm: 40ml balloon
d. Femoral Artery approach: Sedlinger technique and insertion of a 12F
introducer.
e. The correct length for insertion should be checked prior to insertion using
the Angle of Louis (level of T 4) as the surface landmark. Insert the balloon to
the level of T4. The double black marker on the balloon catheter should be
visible this indicates that the balloon has fully exited the sheath.
f. Connect to pressure transducer and pump, then press "lAB fill" button to fill
the balloon. When balloon fill is complete, press "assist/standby" button to
start the pump. Start on minimal augmentation and increase to maximum
NB: subsequent augmentation should not be set below 50%
g. Suture in place and cover with an occlusive dressing.
h. Set timing
o Check balloon inflation against pressure wave set to peak of the Dicrotic
notch.
o Check balloon deflation against ECG: prior to QRS Complex and observe
decrease in end diastolic pressure.
o Check diastolic augmentation on pressure wave
o Select augmentation ratio: *standard = 1: 1
- Maintenance
a. Systemic Heparinisation (APTT = 50-80s).
b. Check CXR post insertion: Tip of IABP below T4- (carina) = below the origin of
the Left Subclavian artery
c. Neurovascular observation of insertion site, lower limbs and left arm hourly
d. Document pumps timing (ratio) and adequacy of augmentation.
e. Assess hemodynamic response: CI, MAP, SVR, filling pressures, CXR.
Intensive Care Manual Controlled Copy Quality Department 59
f. Ensure clear balloon tubing is exposed,' to monitor condensation (due to
rapid Helium shuttling) or blood in tubing (balloon rupture).
- Timing during arrhythmias
a. Ectopics: keep on ECG trigger, system should automatically deflate on ectopic
b. Tachycardia more than 160/min
o Reduce augmentation (equal to patient systole)
o Decrease ratio to 1:2 if reducing augmentation is not adequate
c. Atrial fibrillation: move deflate slide to extreme right to deflate on R wave or
synchronize with arterial wave form
d. VT or VF: defibrillate or cardioversion as required, the IABP is isolated
e. weaning
o Commence when patient's hemodynamics have improved.
o IABP is generally removed within 72 hours.
o Methods.
(a) Reducing ratio from 1: 1 to 1:2 to 1:3
(b) Reduce augmentation. Note: minimum balloon inflation 50%
f. Removal of catheter
o Notify cardiac vascular surgeons
o Cease Heparin 3 hours prior to removal
o Disconnect IABP tubing: do not aspirate the balloon.
o Use local pressure immediately on Catheter removal
COMPLICATIONS
- Limb ischemia - thrombotic or embolic
- Bleeding at the insertion site or systemically
- Infection
- Aortic dissection
- Occlusion of origins of Aortic arch vessels if too high.
- Occlusion of Renal/ Splanchnic vessels if too low
Intensive Care Manual Controlled Copy Quality Department 60
- Thrombocytopenia
- Balloon rupture: gas embolism
L . CARDIAC PACING
POLICY
- The decision to use Transvenous pacing (TVP) is made in conjunction with the
duty Cardiologist and authorized by the Senior Consultant.
- Become familiar with the theory of insertion, indications, interpretation and
complications of TVP.
INDICATIONS
- Medical pacing with Adrenaline or transthoracic pacing may be adequate to treat
many symptomatic bradycardia.
- Any sustained symptomatic bradycardia, which does not respond to medical
treatment, or predisposes to a malignant ventricular arrhythmia.
Note: Pacing is indicated by the hemodynamic consequences of the rhythm, not
the arrhythmia per se.
- Ventricular Tachycardia (especially polyphasic) may respond to overdrive
suppression pacing.
- Following cardiac surgery in high-risk patients (epicardial leads)
- Valve replacement / repair: Especially Mitral.
- VSD repair / Papillary Muscle rupture.
- Acute Myocardial Infarction.
TYPES
- Bipolar pacing lead (VVI): insert under image intensification
- Balloon flotation leads: may be inserted under ECG or pressure guidance
- Pace port P A catheters: these have little utility.
Intensive Care Manual Controlled Copy Quality Department 61
- Epicardial leads
a. Placed during cardiac surgery in high risk patients
b. Usually unipolar ventricular, but may be bipolar, atrial or ventricular: check the
operative note and liaise with the surgeon.
PROCEDURE PROTOCOL (VVI LEAD)
- Strict aseptic technique
- Image intensification
- Local anesthesia where appropriate
- Insertion protocol
a. 6F peel away sheath or PAC introducer
b. Right IJ Vein is the preferred route, then Left Subclavian.
NB: if permanent pacing is likely then avoid Subclavian placement.
c. feed the wire through the RA until the tip just stops on the right ventricular
wall
d. Connect to the control box (switched off)
e. Set output and sense to their minimum value, and rate 20 bpm faster than
the patient's own rate (or 70bpm, whichever is greater).
f. Turn the generator on and gradually increase the output while watching the
ECG for capture.
g. If there is no capture or a high output is required:
o Place on demand mode
o Turn output right down, advance or reposition the wire slightly
o Try to capture again. An ideal capture setting is ~ 2 mA
o Ensure wires are not exposed and tape both sides
h. Suture the wire and apply an occlusive dressing
i. Arrange a post-insertion CXR.
- Daily check
a. Battery strength
Intensive Care Manual Controlled Copy Quality Department 62
b. Capture: set the output 2x higher than threshold for safety.
M. FLOATATION CATHETER INSERTION
a. These may be inserted either “blind”, under ECG guidance (standard
recommendation), or via pressure guidance for catheters having an infusion
lumen (cf. PA catheter insertion).
b. Aseptic technique and local anesthesia where appropriate.
c. Insertion protocol
i. 6F peel away sheath, do not use a PAC introducer as these shall leak
ii. Attach V5 lead of an ECG to the distal electrode of catheter and monitor
iii. Note P and then QRS waveform changes as the catheter advances to the RV
iv. Advance catheter another 2 cm, deflate the balloon and advance 1 cm
v. Connect to the pulse generator (switched off)
vi. Set output and sense to their minimum value, and rate 20 bpm faster than
the patient’s own rate.
vii. Turn the generator on and gradually increase output while watching the ECG
for capture.
viii. If there is no capture or a high output is required – see (4 d.vii) above
ix. Suture the wire and apply an occlusive dressing
x. Arrange a post-insertion CXR.
7. DRUGS AND INFUSIONS
A. Policy
1. Patients admitted to ICU shall have all old and current medications reviewed. Only
medications that are applicable to the current admission shall be transcribed to the
Drug Chart.
2. All drugs, infusions and fluids are reviewed and written up daily
3. All subsequent changes or additions to drug and fluid orders shall be written and signed
for on the Drug Chart. Nursing staff shall be notified of these changes or additions as
soon as charted. Verbal orders alone are neither sufficient nor legal.
Intensive Care Manual Controlled Copy Quality Department 63
4. Vasoactive or hypertonic infusions (for example, TPN) shall be administered through
dedicated lumens of a central venous catheter.
5. The concentration of infusions shall not be changed (i.e. ‘double strength’) from the
Unit infusion protocols outlined below. Standardization of infusion concentrations is an
essential quality control exercise to prevent confusion and potentially dangerous drug
mishaps.
6. Charting of drugs and infusions is only to be done by Intensive Care medical staff.
7. Patients discharged from ICU shall have appropriate drugs, infusions and fluids written
up on standard hospital forms.
8. Notify the Anesthesia Department about patients discharged under their care (i.e.
epidurals, PCA).
B. Principles of drug prescription in Intensive Care.
1. Ideally, drugs shall only be prescribed where proven benefit has been demonstrated.
2. Drugs shall be prescribed according to protocols and guidelines.
3. Ensure that the drug doses are correct: Check the Formulary if unsure.
4. The risk and benefit of starting any drug shall be carefully considered. Critically ill
patients have altered pharamcokinetics and pharmacodynamics with the potential for
toxicity and drug interactions.
5. Where possible:
a. Use drugs that can be titrated or prescribed to an easily measured endpoint.
b. Use drugs that can be measured to monitor therapeutic drug levels.
c. Avoid drugs with narrow therapeutic indices (For example, Digoxin, Theophylline),
particularly in patients with associated Hepatic or Renal dysfunction.
d. Cease a drug if there is no apparent benefit.
e. If two drugs are of equal efficacy, choose the cheaper drug (For example,
Pancuronium Vs. Vecuronium) as the cost of drugs in ICU is significant.
C. CARDIOVASCULAR DRUGS
I. INOTROPES
Inotropes are the most frequently used cardiotropic drugs in cardiac Intensive Care
and less frequently used in other ICU.
General principles
a. Maintenance of cardiac output in critically ill patients forms the basis of
hemodynamic resuscitation and organ perfusion.
b. The main indication for inotropes is to increase myocardial contractility for a
Intensive Care Manual Controlled Copy Quality Department 64
given preload and after load.
c. These agents have variable effects on heart rate and peripheral vascular
resistance (systemic and pulmonary).
d. Hypovolemia is the most common cause of hypotension and low cardiac output
in critically ill patients should be assiduously monitored and corrected.
e. No single inotrope (or mixture of inotropes) has been shown to be superior to
another.
f. There is marked inter-individual variation in the response to inotropes. This is
partly due to qualitative and quantitative changes in adrenergic receptor kinetic
in acute illness. Similarly, prolonged exposure to catecholamine infusions may
produce adrenergic receptor down-regulation.
g. The clinical implications are
h. Infusions should be started at a low rate (3-5 g/kg/min) and increased until a
satisfactory clinical response occurs
(a) Improvement in peripheral perfusion and CO
(b) No significant increase in HR or development of arrhythmias
(c) Maintenance or increase in urine output
1. Primarily a vasodilator, weak
250mg/50ml
inotropic action
Dobutamine 5% Dextrose
2. Used in cardiogenic shock or low
(ml/hr approx g/kg/min)
output, high after load states
II Vasopressor agents
a. General principles
Apart from the Catecholamines, which have variable effects on the peripheral vasculature,
vasopressor usually act directly on the peripheral vasculature and are primarily used to
acutely elevate blood pressure.
The most common cause of hypotension in Intensive Care patients is hypovolaemia.
Vasopressor agents shall not be used as an alternative to fluid resuscitation.
Intensive Care Manual Controlled Copy Quality Department 65
b. Indications (in ICU)
i. Septic shock
ii. Cardiogenic shock, hypotension following sympathetic block (For example,
Epidural anesthesia).
Noradrenaline is the drug of choice for septic shock.
c. Complications
i. Rebound hypertension
ii. Vagal response
iii. Tachyphylaxis.
Agent Standard infusion Uses
1. Cardiopulmonary resuscitation
2. Severe sepsis syndrome, septic shock
3. Cardiogenic shock
6 mg/ 100 ml 5%
4. Acute severe asthma
Adrenaline Dextrose
5. Anaphylaxis
(ml/hr = µg / min)
6. Maintenance of cerebral perfusion
pressure
7. Medical pacing (1st line drug)
6 mg/ 100 ml 5% 1. Vasodilated (vasoplegic) states eg septic
Noradrenaline Dextrose shock (although adrenaline is equally as
(ml/hr = µg / min) effective)
1. No advantage over Adrenaline /
400 mg/ 100 ml 5%
Noradrenaline
Dextrose
Dopamine 2. Produces more Tachycardia than
(ml/hr approx µg/kg
Adrenaline
/ min)
3. “Real dose” Dopamine is not used
20 units / 20 ml 5% 1. Vasodilated (vasoplegic) states eg.,
Dextrose septic shock (although adrenaline is
Vasopressin
2.4 ml / hr (0.04 equally as effective)
µ/min)
6 mg/ 100 ml 5% 1. Vasodilator, chronotrope (rarely used)
Isoprenaline Dextrose 50 2. Medical pacing (2nd line after
(ml/hr = µg / min) Adrenaline)
Intensive Care Manual Controlled Copy Quality Department 66
III. Antihypertensive agents
a. General principles
i. The most common cause of hypertension in Intensive Care patients is
sympathetic drive due to pain agitation or delirium. This shall be treated with
adequate sedation and analgesia.
ii. Patients in the recovery phase of acute renal failures are other hypertensive and
as such do not need treatment.
iii. Similarly, neurogenic hypertension is frequent following head injury or
intracerebral hemorrhage and is generally self-limiting and does not require
treatment. The use of vasodilators in this setting is relatively contraindicated.
iv. Antihypertensive shall be titrated against the patient’s premorbid blood
pressure.
b. Indications
i. Acute
(a) Acute perioperative control of hypertension after cardiac, carotid, or
Cerebrovascular surgery, or for patients with critical myocardial ischemia.
(b) Hypertensive emergency, urgency
(c) Pre-eclampsia / Eclampsia
(d) Pheochromocytoma
ii. Other indications for vasodilators
(a) Reduction of afterload in cardiac ischemia and failure.
(b) Adjunct to passive warming in hypothermia.
iii. Chronic
a. Reflex tachycardia
b. Hypotension (especially in Hypovolumic patients)
c. Tachyphylaxis
d. Pulmonary vasodilatation causing shunt and hypoxia
e. Cyanide toxicity (SNP)
Agent Standard infusion Uses
1. Mainly venodilation: useful in cardiac
25µgm/ 50 ml 5%
ischemia
Glyceryl Dextrose
2. Less predictable control of hypertension
trinitrate (Non PVC Bottle and
3. Tachyphylaxis develops within 24-48 h;
(GTN) giving set)
shall need additional agents for persistent
range 2-2.5 ml/hr
hypertension
Intensive Care Manual Controlled Copy Quality Department 67
1. Rapid control of hypertensive crises.
Sodium 50 mg/ 250 ml 5% 2. Tachyphylaxis and metabolic acidosis may
Nitroprusside Dextrose Range 3-40 imply Cyanide toxicity (total dose more
(SNP) ml/hr than 1.5 mg/kg/24 hrs)
10 mg/ 10 ml 5% Dextrose 1. Pure alpha blockage, short acting
Phentolamine
titrate antihypertensive
1. Short to medium term parenteral
antihypertensive
10-20 mg as bolus
Hydrallazine 2. Often use with alpha blockers for reflex
20-40 mg 6-8 hourly
tachycardia
3. Useful in renovascular hypertension
1. Long acting oral Calcium antagonist.
Amlodipine 5-10 mg oral bd
2. Caution in Renal failure.
1. Treatment of hypertension
Start low dose ~3-6.25 mg 2. Left ventricular dysfunction, especially
upto 50 mg orally 8 hourly post- MI
Captopril Syrup: 5mg/ml or tablets 3. Left ventricular failure
Acute hypertension: 6.25- 4. Diabetic nephropathy
25 mg sublingually prn 5. Caution in Reno vascular disease and
Renal failure
1. Treatment of hypertension
2. Left ventricular dysfunction, especially
post -MI
Start 2.5 mg daily
Enalapril 3. Left ventricular failure
Up to 20mg bd orally
4. Diabetic nephropathy
5. Caution in Reno vascular disease and
Renal failure
Oral: 10mg/day until 1. Long acting Alpha Blocker
postural hypotension 2. Preoperative preparation of
Phenoxy- IV: 1 mg/kg/day (dilute to Phaeochromocytoma
benzamine 200-500 ml) : 1/3 dose 3. Idiosyncratic hypotension may occur
over 1/24, 2/3 dose over
1/24
1. Alpha - blocker
Start with 0.5 mg, and
2. Potent antihypertensive agent
Prazosin increase up to 5 mg bd
3. Beware first does effect, especially fin
orally
under filled
1. Used in high sympathetic drive states:
neurogenic hypertension
1-2 mg IV bolus (up to 10
2. All grades of hypertension, including Reno
Atenolol mg)
vascular
Oral: 25-100 mg bd
3. Cardiac ischemia
4. Control of reflex Tachycardia with
Intensive Care Manual Controlled Copy Quality Department 68
vasodilators
5. Thyroid crisis
6. Caution in poor LV function, asthma
7. Renal excretion; virtually no Hepatic
metabolism
1. As for Atenolol
Metoprolol Oral: 25-100 mg bd
2. Mainly eliminated by Hepatic metabolism
1. Ultra short acting Alpha-blocker
Loading dose 0.5 mg/kg 2. Useful as trial for patients with poor LV
Esmolol Infuse 100mg/10ml and function
titrate 3. Adjunct to vasodilators post cardiac
surgery
1. Acute, centrally mediated hypertension.
2. Useful post cardiac surgery
Start 25ug @ 150 ug IV
3. Withdrawal states
Clonidine Oral : 75 ug bd
4. Care with Hepatic or Renal dysfunction
Upto 150-300 ug tds.
5. May cause rebound hypertension with
chronic use.
1. Third line drug for chronic hypertension,
especially if intolerant of ACEI
250-2g/day oral bd 2. Pregnancy induced hypertension
Methyldopa
125 mg-250mg IV bolus 3. May require diuretic / ACEI
4. IV useful in centrally mediated
hypertension
40-60mg /kg (or 4 g) 1. Pre-eclampsia/ eclampsia
Magnesium loading , Infuse at 2-4 g/hr 2. Phaeochromocytoma
Sulphate to maintain 3. Sympathetic overdrive in Tetanus
Mg level > 1.5 – 2 mmol/l
0.25mg/kg slow IV at 1. As for Atenolol
Labetolol
2 ml/minute 2. Mainly eliminated by Hepatic metabolism
IV. Antiarrhythmics
a. General principles
i. Prior to administration of antiarrhythmic agents, optimize correction of the
following
a. Hypovolaemia
b. Metabolic abnormalities (Decreased Calcium, Magnesium and Biphosphate
leading to alkalosis)
c. Myocardial ischemia or cardiac failure (especially post cardiac surgery)
d. Sepsis
e. Pain and agitation.
Intensive Care Manual Controlled Copy Quality Department 69
ii. All antiarrhythmic drugs shall be regarded as pro-arrhythmic
iii. Virtually all depress myocardial contractility.
iv. Antiarrhythmics drugs are indicated when the arrhythmia causes
haemodynamic compromise (hypotension or prolonged Tachycardia more
than 120-130 /min) or in susceptible patients with Myocardial Ischemia
b. Indications
i. Termination of an acute arrhythmia
ii. Prophylaxis for recurrence
Agent Standard infusion Uses
1. Effective in treatment and prophylaxis of
Rapid atrial flutter/fibrillation or MAT
complicating acute illness, especially
sepsis
(Monomorphic ventricular Tachycardia)
Acute use: 2. Generally does not suppress contractility
Amiodarone 300mg bolus over 5minutes 3. Can cause acute hypotension of given too
followed by 1mg/min for rapidly
6hours followed by 0.5mg/min 4. Less proarrhythmic potential than most
over 18hours other drugs
Chronic use: 5. Causes QT, but rarely Torsade de points
200-400 mg IV / oral daily 6. Renal excretion is minimal – no need to
change dose in Renal failure
7. Long term side effects rare in short term
use
8. Interference with Digoxin kinetics and
assay
9. Interference with Thyroid function tests.
Magnesium 5-10 mmol IV slow bolus 1. Acts principally as a Calcium blocker
infuse at 2-5 mmol/hr 2. Useful in atrial fibrillation and Torsade –
de-Pointes
Verapamil 1. Conversion atrial flutter SR
5-10 mg IV slow bolus
2. SVT – 2nd line to Adenosine
1. Ventricular rate control in rapid AF (usually
2nd line to amiodarone in critically ill)
2. Narrow therapeutic index especially in
Rapid digitalization: 0.5 – 1 mg Renal failure and metabolic abnormalities
IV (Decreased Potassium, Magnesium,
Digoxin Maintenance: 62.5 –250 g Phosphates, alkalosis)
IV / oral daily 3. Proarrhythmic potential high in critically ill
(levels 0.6 –2.3 nmol/l) patients
4. Minimal inotropic effect in critically ill
patients
5. Hypokalaemia potentiates effect
Intensive Care Manual Controlled Copy Quality Department 70
Atenolol 1. Used in high sympathetic drive
states: neurogenic hypertension
2. Control of reflex Tachycardia with
1-2mg IV bolus (upto 10 mg)
vasodilators
25-100 mg oral bd
3. Caution in poor LV function, asthma
4. Renal excretion: virtually no Hepatic
metabolism`
Adenosine 1. Diagnosis / Conversion of SVT
6-12 mg rapid IV push
(Prolonged AV conduction)
Lignocaine 1. Sustained, recurrent VT (2nd line drug after
Amiodarone)
0.4% solution = 4 mg /ml 2. No longer routinely used for prophylaxis
60ml/hr (4mg/min) for 1-2 hrs for VT
45 ml/hr for 2-4 hrs 3. VF resistant to defibrillation (now
30ml/hr 2-4 hrs questioned)
4. Potent negative inotrope, causes
convulsion’s
Phenytoin 15mg /kg loading / 1 hr 1. Digoxin toxicity
300 mg /day 2. Tricyclic induced malignant arrhythmias
(Level 40-80 mmol/l)
V. ACUTE CORONARY SYNDROME (ACS)
Any of the 2 criteria should be met of the 3 to diagnose ACS
1) chest pain or equivalent symptom 2) ECG changes 3) biomarkers
ACS is of a) unstable angina b) NSTEMI c) STEMI
ST ELEVATION MI (STEMI)
- ECG evidence of acute infarction:
Raised ST segment 2mm in two (or more) chest leads
Raised ST segment 1mm in two adjacent limb leads, or
New onset LBBB
Posterior infarction (Raised R in V1)
- Morphine sulfate (2 to 4 mg IV with increments of 2 to 8 mg IVrepeated at 5- to
15-minute intervals) is the analgesic of choice.
- Patients routinely taking NSAIDs (except for aspirin), bothnonselective as well as
COX-2 selective agents, before STEMIshould have those agents discontinued at the
time of presentation with STEMI because of the increased risk of
mortality,reinfarction, hypertension, heart failure, and myocardial
ruptureassociated with their use.
Intensive Care Manual Controlled Copy Quality Department 71
- Oral beta-blocker therapy should be initiated in the first 24 hours for patients who
do not have any of the following: 1) signs of heart failure, 2) evidence of a low
output state, 3) increased risk for cardiogenic shock, or 4) other relative
contraindications tobeta blockade (PR interval greater than 0.24 seconds, second-
or third-degree heart block, active asthma, or reactive airway disease).
- STEMI patients presenting to our hospital with PCI will be treated with primary PCI
within 90 minutes of first medical contact .
- Patients undergoing reperfusion with fibrinolytics should receive anticoagulant
therapy for a minimum of 48 hours and preferably for the duration of
hospitalization up to 8 days.
Anticoagulant regimens with established efficacy include:
UFH (initial intravenous bolus 60 U per kg [maximum 4000 U]) followed by an
intravenous infusion of 12 U per kg per hour (maximum 1000 U per hour) initially,
adjusted to maintain the activated partial thromboplastin time at 1.5 to 2.0 times
control
Enoxaparin for patients less than 75 years of age, an initial 30 mg intravenous bolus is
given, followed 15 minutes later by subcutaneous injections of 1.0 mg per kg every 12
hours; for patients at least 75 years of age, the initial intravenous bolus is eliminated
and the subcutaneous dose is reduced to 0.75 mg per kg every 12 hours. Maintenance
dosing with enoxaparin should be continued for the duration of the index
hospitalization, upto 8 days.
Fondaparinux (provided the serum creatinine is less than 3.0 mg per dL): initial dose 2.5
mg intravenously; subsequently subcutaneous injections of 2.5 mg once daily.
Maintenance dosing with fondaparinux should be continued for the duration of the
index hospitalization, up to 8 days.
Clopidogrel 75 mg per day orally should be added to aspirin (aspirin 300mg stat dosage
followed by 75mg per day) in patients with STEMI regardless of whether they undergo
reperfusion with fibrinolytic therapy or do not receive reperfusion therapy.
Treatment with clopidogrel should continue for at least 14 days.
In patients taking clopidogrel for whom CABG is planned, the drugshould be withheld
for at least 5 days and preferably for 7 daysunless the urgency for revascularization
outweighs therisks of excess bleeding.
ACE inhibitors should be started and continued indefinitely in all patients recovering
from STEMI with LVEF less than or equal to 40% and for those with hypertension,
diabetes, or chronic kidney disease, unless contraindicated.
Statins to be added
Role of use of abciximab in patients for PCI has established role
Intensive Care Manual Controlled Copy Quality Department 72
THROMBOLYTIC THERAPY
If the initial ECG is not diagnostic of STEMI but the patient remains Symptomatic,
and there is a high clinical suspicion for STEMI, serial ECGs at 5- to 10- minute intervals or
continuous 12-lead ST-segment monitoring should be performed to detect the potential
development of ST elevation.
- Indications
- STEMI
Contraindications
Absolute contraindications
a)Any prior ICH
b) Known structural cerebral vascular lesion (e.g., arteriovenousmalformation)
c) Known malignant intracranial neoplasm (primary or metastatic)
d) Ischemic stroke within 3 months except acute ischemic strokewithin 3 hours
e)Suspected aortic dissection
f)Active bleeding or bleeding diathesis (excluding menses)
g)Significant closed-head or facial trauma within 3 months.
Relative contraindications
a) Severe uncontrolled hypertension on presentation (SBP greaterthan 180 mm Hg or DBP
greater than 110 mmHg)
b)History of prior ischemic stroke greater than 3 months, prolonged (greater than 10 minutes)
CPR or major surgery (less than 3 weeks)Recent (within 2-4 weeks) internal bleeding, Non-
compressible vascular punctures
c) For streptokinase prior exposure (more than 5 daysago) or prior allergic reaction to these
agents
d)Pregnancy Active peptic ulcer
Laboratory Evaluations for Management of STEMI
Serum biomarkers for cardiac damage (do not wait for results before implementing
reperfusion strategy)
CBC with platelet count, PT, INR ,aPTT, serum lipids Electrolytes ,magnesium, BUN
,Creatinine, Glucose
- Routine follow-up
a. ECG at 1 and 4 hours. post STK/TNK
b. Cardiac enzymes 6, 12 and 24 hours post infusion if required
Intensive Care Manual Controlled Copy Quality Department 73
Standard Uses
Infusion/Dose
1. 300 mg Aspirin prior to therapy
then daily 75mg od
1.5 million units/ 100mls
Streptokinase STK Normal Saline, over 60
minutes via syringe pump
Tissue plasminogen 15mg bolus followed by
activator(alteplace) 85mg over 90minutes
ANTIPLATELET AGENTS
Agent Standard Uses
Infusion/Dose
Bolus: 0.25mg/kg Only to be ordered by Cardiology Binds
IV over 1 min, 10 to Platelet Glycoprotein IIb/IIIa receptor,
mins before PTCA inhibiting platelet aggregation and
Reo Pro
Infusion: 0.125 thrombus formation
Abciximab)
g/kg/min IV for Primarily used with PTCA
12 hrs. (max rate=
10g/min)
Bolus: Blocks Platelet Glycoprotein IIb/IIIa
0.4g/kg/min for receptor.
30 mins Short half-life (1.4-1.8hrs)
Maintenance: Uses: unstable angina, non-Q wave MI
Intensive Care Manual Controlled Copy Quality Department 74
0.1g/kg/min for Continue through angiography,
at least 48 hrs and for 12-24 hrs post –PTCA.
Tirofiban NB: reduce doses Check platelet count 6 hrs post
by 50% with bolus, then at least daily bleeding
severe renal in (major 1.4%), thrombocytpenia,
sufficiency. (for fever
example,
Creatinine
clearance less
than 30 ml/min)
References: American heart association guidelines for MI 2004, 2007.
VI. RESPIRATORY DRUGS
1. Nebulised bronchodilators
a. General Principles
i. These agents are the mainstay of treatment for bronchospasm in Intensive Care
(including acute severe asthma)
ii. They are not routinely used in all ventilated patients.
iii. Once commenced, they shall be reviewed daily regarding efficacy. This is
assessed by improvements in audible wheeze, lung compliance, respiratory rate
and blood gases.
b. Indications
i. Pre-existing asthma/ chronic airflow obstruction (CAO)
ii. Acute severe asthma
iii. Acute bronchospasm secondary to infection, aspiration or during mechanical
ventilation.
iv. Acute exacerbation of CAO
2. Parenteral therapy
a. Indications
i. Adjunctive therapy for acute severe asthma in patients not responding to nebulised
agents
ii. Selected patients who are difficult to wean from ventilation (usually due to CAO)
iii. Maintenance in patients with chronic airflow obstruction
b. Complications
i. Hypokalaemia, metabolic alkalosis
ii. Arrhythmias (Theophylline)
iii. Intercurrent infection (steroids)
Intensive Care Manual Controlled Copy Quality Department 75
iv. Polyneuropathy (steroids)
Agent Standard infusion / dose Uses
Salbutamol Nebulised in Normal Saline 1. First line
(nebulised) (1ml:1ml) bronchodilator
continuously, 2 or 4 hourly 2. Used in severe
hyperkalemia
Ipratroprium Nebulised in addition to 1. Chronic airflow
Bromide Salbutamol (1ml: 1ml) obstruction (CAO)
2. Asthma
Budesonide Nebulised 1 mg bd 1. Steroid dependent
(nebulised steroid) (CAO)
2. Acute exacerbation of
CAO
Adrenaline 6mg / 100ml 5% Dextrose 1. Acute severe asthma
(IV) (ml/hr = g/min) 2. Rapid onset and offset
of action
3. Titrate until
demonstrate pressor
response (may require
upto 100 g.
Salbutamol 6mg/100ml 5% Dextrose 1. Acute severe asthma
(IV) (ml/hr = g/min) 2. Longer duration of
action
Methylprednisolone 40mg iv od 7days 1. Acute exacerbation of
CAO
2. Acute severe asthma
(methyprednisolone 40mg
TID x 48hrs and wean)
Theophylline 1000mg/100ml 5% 1. No longer 1 st line drug
dextrose 2. May improve
loading 5-7 mg/kg, respiratory drive in
infuse 2-4 ml/hr (1gm/day) CAO
levels : 55-110 mol/l 3. Narrow therapeutic
index: Proarrhythmic
VII. Sedation, analgesia and muscle relaxants
1. Sedatives and analgesics
a. Adequate analgesia and anxiolysis are primary goals in the management of the
critically ill patient.
Intensive Care Manual Controlled Copy Quality Department 76
b. Pain and anxiety are associated with significant adverse physiological responses:
i. Hypertension, Tachycardia with significant adverse physiological responses:
ii. Gastric erosion
iii. Intracranial hypertension
iv. Persistent catabolism
c. Sedatives and analgesics in ICU are also associated with adverse effects
i. Respiratory depression
ii. Emergence delirium and sympathetic overdrive, accidental extubation and
removal of lines
iii. Hypotension due to unmasked hypovolaemia
iv. Gastro paresis, ileus
- Sedation protocol for Intensive Care patients.
a. Sedation should be given whenever required
b. Patients with Renal, Hepatic or associated encephalopathy may require lower
doses.
c. Interruption of sedation is required daily for all patients except with patients
on high ventilatory support and neuro patients.
d. Bolus doses of sedation are better when compared with continuous infusions
e. Sedation assessed as per the scale given below.
Modified Ramsay Scale for sedation
1. Anxious and agitated or restless, or both
2. Cooperative, orientated, and tranquil
3. Drowsy, but responds to commands
4. Asleep, brisk response to light glabellar tap or loud auditory stimulus
5. Asleep, sluggish response to light glabellar tap or loud auditory stimulus
6. Asleep and unarousable
Current guidelines recommend routine monitoring of sedation and the use of
protocols to guide sedation can decrease the time spent on mechanical ventilation .
The goal of sedation in the ICU is a patient who is calm but easily arousable ( score of 3). The
use of a sedation scale will allow you to achieve and maintain this goal with the lowest possible
dose of a sedative agent and with the lowest possible risk of harm to your patient.
Intensive Care Manual Controlled Copy Quality Department 77
Pain assessment in intubated patients
Behaviour pain assessment (BPS) scores range from 3 (no pain) to 12 (maximal pain) . The BPS
has a maximal acceptable pain score of 5. Intervention is required if pain score more than 5.
Agent Standard Uses
Infusion/Dose
1. Haemodynamic stability
100-200 g IV bolus
Fentanyl 2. Potent medium acting narcotic
Infusion: 50-200 g/hr
3. Useful for CCU procedures.
10mg/ml (neat 1. Short term sedation of intubated
Propofol solution), start and ventilated patients.
at 3 ml/hr and 2. Do not use in patients where
Intensive Care Manual Controlled Copy Quality Department 78
titrate Against prolonged ventilation is anticipated,
effect except where repeated neurological
assessment is required, or in the
presence of Hepatic or Renal failure.
3. hypotension more common
4. No analgesic effect
Fentanyl 5g/ml and 1. Standard epidural analgesic regimen
Bupivacaine 0.125% 2. Maximal duration 4 days unless
Rate : age indicated
Epidural
related doses
(as per APS
protocols)
1. First line major tranquillizer, use for
Haloperidol 2.5-5mg IV pm delirium, and agitation as in Opioid /
Benzodiazepine withdrawal.
Lorazepam Used in Status Epilepticus and as an
anxiolytic in pre – anesthetic medicine,
prolonged ventilation
Midazolam 20 Only for Ventilated patients.
mg and - watch out for Hypotension
3 to 5 ml/hr
Fentanyl 300
g in 50 ml NS
Intensive Care Manual Controlled Copy Quality Department 79
References
1) Guidelines for use of sedative and analgesics in critically ill patients Crit Care Med 2002, vol
30,no1.
2) Payen JF, Bru O, Bosson JL, Lagrasta A, Novel E, Deschaux I, Lavagne P, Jacquot C: Assessing
pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med
2001,29:2258-2263.
2. Muscle relaxants
a. General principles
i. The use of muscle relaxants for the critically ill patient is different to patients
undergoing elective anesthesia
ii. These agents have a limited role in Intensive Care and shall not be used unless the
patient is adequately sedated and if required.
iii. Non-depolarizing agents (except Rocuronium) shall not be used for emergency
(rapid sequence induction) endotracheal intubation
b. Indications
i. Depolarizing: Suxamethonium
(a) First line relaxant for emergency endotracheal intubation
ii. Non-depolarising : Pancuronium, Vecuronium, Atracurium
(a) Acute control of ventilation post intubation
(b) Patient transport post intubation
(c) Selected patients with poor lung complications
(d) Acute procedures: tracheostomy, bronchoscopy if required.
c. Complications
i. Hyperkalemia, Bradycardia (Suxamethonium)
ii. Polyneuropathy and myopathy (especially with concomitant use of steroids)
iii. Sympathetic overdrive, particularly in under-sedated patients
iv. Adverse outcome in head injury when used as a measure to control ICP
Relaxant Dose Comment
Suxamethonium 100-200 mg 1. 1st line agent in Rapid Sequence
or Induction (RSI)
1-2 mg/kg 2. Consider pre-treatment with atropine
(0.6- 1.2 mg) if potential Bradycardia
3. Contraindicated in burns (More than 3
days), chronic spinal and neuromuscular
disease, hyperkalemic states
(Potassium more than 5.5)
Rocuronium 0.6 mg/kg 1. First line non-depolarizing agent in ICU
1.0 mg/kg 2. Rapid onset (60 secs) 2nd line agent in
Intensive Care Manual Controlled Copy Quality Department 80
for RSI RSI-used as alternative to
Suxamethonium
3. Duration of action 30-40 minutes
Pancuronium 2-4 mg IV prn 1. 2nd line non-depolarizing agent in ICU
2. Long duration of action
3. Tachycardia rarely a problem in ICU
patients
VIII. Anticoagulants
1. General principles
a. Anticoagulants are potentially dangerous drugs.
b. All patients on systemic anticoagulation shall have an APTT, INR and CBP performed
daily.
2. Indications
a. Acute systemic anticoagulation
i. Heparin infusion titrated to a therapeutic APTT is used in critically ill patients.
This allows monitoring and the provision for reversal if indicated (for example,
procedures, bleeding complications).
ii. High dose Enoxaparin (for example, 1 mg/kg bd s/c) is as effective, difficult to
monitor and reverse its effect but easy to administer.
a. Proven venous or arterial thromboembolism
b. Myocardial infarction: as sole therapy or with following PA
a. Prosthetic heart valves
1. Prior to commitment of oral anticoagulants
2. During an acute illness, where oral anticoagulation is relatively
contraindicated.
b. AF in patients complicated by emboli less than 70 years.
c. AF for more than 48 hours, in which cardio version is being considered
d. Extracorporeal circuits. For example, CVVHDF
e. IABP
b. Partial anticoagulation (low dose IV Heparin (500 u/hr)
c. Oral anticoagulants (INR 2-4: rarely used in ICU)
i. Prosthetic valves (Mitral more than Aortic valves)
ii. Previous thromboembolism
iii. Maintenance of thromboprophylaxis in high risk patients (fracture pelvis)
Intensive Care Manual Controlled Copy Quality Department 81
PROTOCOL FOR DVT PROPHYLAXIS SUBCUTANEOUS ENOXAPARIN
- Routine monitoring is not necessary.
- Indications:
Level of Risk
Low risk
Minor surgery in patients less than 40 yr with no additional risk factors
Moderate risk
Minor surgery in patients with additional risk factors
Surgery in patients aged 40–60 yr with no additional risk factors
High risk
Surgery in patients more than 60 yr with additional risk factors (prior VTE, cancer, molecular
hypercoagulability)
Highest risk
Surgery in patients with multiple risk factors (age more than 40 yr, cancer, prior VTE)
Hip or knee arthroplasty
Major trauma; Spinal cord injury
- Contraindications
a. Young, short stay patients (less than 24hours) For example, drug overdoses
b. Post neurosurgery/eye surgery
c. Acute head injury with parenchymal lesions
d. Intracranial hemorrhage
e. Active bleeding, coagulopathy
f. Thrombocytopenia
g. Previous documented HIT
- In patients who cannot receive subcutaneous Heparin
a. TED stockings
b. Mechanical compression devices
For removal of epidural catheters heparin and LMWH should be withheld for 6 and
12 hrs respectively and recommence Heparin and LMWH after 4hrs.
Check platelet count no later than 5 days post commencement of Heparin then
Intensive Care Manual Controlled Copy Quality Department 82
weekly thereafter. If more than 50% fall hold Heparin
Prophylaxis Regimens
Unfractionated heparin, 5,000 units SC every 12 hr
Enoxaparin 1mg/kg SC once daily, or dalteparin, 2,500 units SC once dailydose adjustments to
be done in renal failure
RECOMMENDATIONS FOR PERIOPERATIVE ANTICOAGULATION IN PATIENTS ON
WARFARIN
- Heparin infusion remains the first choice in CCU, as the effect is more readily
monitored and reversed.
- Therapeutic Enoxaparin should not be used in this setting (unless Heparin is
contraindicated).
PROTOCOL FOR HEPARIN INDUCED THROMBOCYTOPENIA SYNDROME (HIT)
- GENERAL PRINCIPLES
a. Occurs in 1-5% patients
o 7-10 days after starting Heparin or on the 2nd day if the patient already
received heparin in the last 100 days.
o Autoimmune mediated platelet aggregation with thrombosis
o Not dose related
- SUSPECTED HIT: unexplained thrombocytpenia and/or thrombosis in a patient
receiving Heparin
Consider other causes of thrombocytopenia
Cease all Heparin (including flushing bags)
If anticoagulation is necessary, two direct thrombin inhibitors are available
1) lepirudin and
2) argatroban .
These agents inhibit clot-bound thrombin, and they do not cross-react with heparin
antibodies.
Intensive Care Manual Controlled Copy Quality Department 83
Fondaparinaux can be used in HIT
o Hemodialysis to be done by citrate anticoagulation.
o Document Heparin allergy in case notes.
IX. RENAL DRUGS
GENERAL PRINCIPLES for use of diuretics in ICU
- Oliguria in acutely ill patients is frequently a manifestation of hypovolaemia,
decreased cardiac output, direct renal toxicity, or a combination of these factors.
Therapy shall be directed toward these factors.
- Urine output, in the absence of diuretic use, represents one of the best markers of
end-organ perfusion and is a useful guide to clinical management.
- Diuretics should not be used in renal failure as it increases in hospital mortality
and non-recovery of renal function
INDICATIONS
- Symptomatic fluid overload
Pulmonary edema
Congestive cardiac. Failure
- Diuretic dependent-Renal function
- Ascites
CONTRAINDICATIONS
- Hypovolemia and/or Sodium depleted states
COMPLICATIONS
- Hypovolemia
- Hyperosmolar states due to inappropriate diuresis in hypovolemia
- Potentiation of Renal failure secondary to hypovolemia
- Electrolyte disturbance especially decreased Potassium, Magnesium, phosphate,
metabolic alkalosis
- Naturesis and Kaliuresis should alter urine electrolytes and osmolality for 24-48
hours post dose.
Intensive Care Manual Controlled Copy Quality Department 84
Drug Dose Indications
1 to 2 1. First line, potent loop diuretic
Frusemide mg/k 2. Doses may be increased in diuretic dependence
g IV
1. Carbonic anhydrase inhibitor: alkaline diuresis with
250-
Acetazolami HCO3 excretion
500m
de 2. Used for severe metabolic alkalosis after correction
g IV
of hypovolemia: K+,Mg,PO4
Reference- Role of diuretics in AKI. JAMA 2002
8. FLUIDS AND ELECTROLYTES
A.PRINCIPLES OF FLUID MANAGEMENT
- All fluids, infusions are reviewed daily and rewritten.
- Assessment of volume status/and fluid balance involves all of the following:
a. Clinical markers
o Skin turgor, mucous membranes
o Pulse, blood pressure,
o Peripheral perfusion, capillary refill
o RAP, PAOP if required
o CXR
b. Biochemical markers
o Serum Sodium, Chlorides, osmolality
o Urea / Creatinine ( ratio)
o Bicarbonate
o Hematocrit
Intensive Care Manual Controlled Copy Quality Department 85
c. Charted fluid balance
o Total intake including drug/infusion volumes
o Total output including urine output, drains, NG losses, blood loss
o Insensible losses due to pyrexia, transcellular shifts, etc.
Fluids should be considered in two components:
- Maintenance fluids
o Usually crystalloids, (according to Sodium):
(a) Normal Saline
(b) 1/2 Normal Saline
(c) 5% Detrose normal saline.
o Usual volumes: 1.5- 2 ml/kg/hour
- Replacement,resuscitation fluids
o Both crystalloids and colloids can be used for resuscitation
(a) 5% albumin can be used, Albumin 20% increases renal failure and
mortality
(b) Gelofusin and 6% hetastarch can be used
o Blood and blood component therapy as indicated
o Crystalloid replacement is usually used for excessive Renal, Enteric and
burns losses.
Reference. Use of hyperoncotic fluids in resuscitation Intensive care medicine
2008 vol 34 page2160.
B.ENTERAL NUTRITION
a. Enteric feeding is the preferred mode of nutritional support and should be
considered in all patients as soon as possible after admission to ICU.
b. Advantages
o Early enteral feeding in trauma patients has been associated with improved
outcome
o Use of the gut decreases mucosal atrophy, which may reduce bacterial
Intensive Care Manual Controlled Copy Quality Department 86
translocation thereby reducing the incidence and duration of sepsis.
o The incidence and severity of gastric erosions and stress ulceration may be
reduced.
o Cheaper than TPN v. Complications of central vascular access (especially
infection) are reduced or avoided.
c. Disadvantages
Regurgitation / aspiration
diarrhea (other causes are more likely than enteral feed)
Nutrition Protocol
o Traditional nutrition assessment tools (albumin, prealbumin, and
anthropometry) are not validated in critical care. Before initiation of
feedings, assessment should include evaluation of weight loss and previous
nutrient intake prior to admission, level of disease severity, comorbid
conditions, and function of the gastrointestinal (GI) tract.
o EN is the preferred route of feeding over parenteral nutrition (PN) for the
critically ill patient who requires nutrition support therapy.
o Enteral feeding should be started early within the first 24-48 hours following
admission. The feedings should be advanced toward goal over the next 48-72
hours.
o In the setting of hemodynamic compromise EN should be withheld until the
patient is fully resuscitated and/or stable.
o In the ICU patient population, neither the presence nor absence of bowel
sounds nor evidence of passage of flatus and stool is required for the
initiation of enteral feeding.
o Either gastric or small bowel feeding is acceptable in the ICU setting. Critically
ill patients should be fed via an enteral access tube placed in the small bowel
if at high risk for aspiration or after showing intolerance to gastric feeding.
Withholding of enteral feeding for repeated high gastric residual volumes
Intensive Care Manual Controlled Copy Quality Department 87
alone may be sufficient reason to switch to small bowel feeding .
o If early EN is not feasible or available the first 7 days following admission to
the ICU, no nutrition support therapy should be provided. In the patient who
was previously healthy prior to critical illness with no evidence of protein
calorie malnutrition, use of PN should be reserved and initiated only after the
first 7 days of hospitalization.
o If there is evidence of protein-calorie malnutrition on admission and EN is
not feasible, it is appropriate to initiate PN as soon as possible following
admission and adequate resuscitation.
o If a patient is expected to undergo major upper GI surgery and EN is not
feasible, PN should be provided under very specific conditions:
1. If the patient is malnourished, PN should be initiated 5-7 days preoperatively
and continued into the postoperative period.
2. PN should not be initiated in the immediate postoperative period but should
be delayed for 5-7 days.
3. PN therapy provided for a duration of <5-7 days would be expected to have
no outcome effect and may result in increased risk to the patient. Thus, PN
should be initiated only if the duration of therapy is anticipated to be ≥7
days.
o The target goal of EN should be determined and clearly identified at the time
of initiation of nutrition support therapy.
o Energy requirements may be calculated either through simplistic formulas
(25-30 kcal/kg/d), published predictive equations
o Efforts to provide >50%-65% of goal calories should be made in order to
achieve the clinical benefit of EN over the first week of hospitalization
o If unable to meet energy requirements (100% of target goal calories) after 7-
10 days by the enteral route alone, consider initiating supplemental PN.
Initiating supplemental PN prior to this 7-10 day period in the patient already
receiving EN does not improve outcome and may be detrimental to the
Intensive Care Manual Controlled Copy Quality Department 88
patient. protein requirements should be in the range of 1.2-2.0 g/kg actual
body weight per day, and may likely be even higher in burn or multi-trauma
patients.
o In the critically ill obese patient, permissive underfeeding or hypocaloric
feeding with EN is recommended. For all classes of obesity where BMI is >30,
the goal of the EN regimen should not exceed 60%-70% of target energy
requirements (or 22-25 kcal/kg ideal body weight per day). Protein should be
provided in a range ≥2.0 g/kg ideal body weight per day for (BMI 30-40),
≥2.5 g/kg ideal bodyweight per day (BMI ≥ 40).
o Feeding schedule
o Start 25 ml / hour for 4hrs and give a gap of 1hour and aspirate, if gastric
residue (GR) < 200 ml return GR to the patient then increase 25 ml per hour,
if GR > 200 ml discard GR and continue the same feed rate, if GR >300 then
decrease the feed rate and to start prokinetics, if GR >500 stop the feed and
try the feed after 6hrs gap, take medical gastroenterology opinion to place
duodenal tube
o EN visible in mouth, vomiting, aspiration then stop EN. Total feedings 16hrs
per day.
o Holding EN for gastric residual volumes <500 mL in the absence of other signs
of intolerance should be avoided.
o Use of enteral feeding protocols increases the overall percentage of goal
calories provided and should be implemented.
o Patients placed on EN should be assessed for risk of aspiration. Steps to
reduce risk of aspiration should be employed.
o In all intubated ICU patients receiving EN, the head of the bed should be
elevated 30°-45°.
o For high-risk patients or those shown to be intolerant to gastric feeding,
delivery of EN should be switched to continuous infusion. Agents to promote
motility such as prokinetic drugs (metoclopramide) should be initiated
Intensive Care Manual Controlled Copy Quality Department 89
where clinically feasible. Diverting the level of feeding by post-pyloric tube
placement should be considered.
o Blue food coloring and glucose oxidase strips, as surrogate markers for
aspiration, should not be used in the critical care setting.
o Development of diarrhea associated with enteral tube feedings warrants
further evaluation for etiology
o Immune-modulating enteral formulations (supplemented with agents such as
arginine, glutamine, nucleic acid, ω-3 fatty acids, and antioxidants) should be
used for the appropriate patient population (major elective surgery, trauma,
burns, head and neck cancer, and critically ill patients on mechanical
ventilation), with caution in patients with severe sepsis.
o Patients with ARDS and severe acute lung injury(ALI) should be placed on an
enteral formulation characterizedby an anti-inflammatory lipid profile (i.e.,
ω-3 fish oils, borage oil) and antioxidants.
o If there is evidence of diarrhea, soluble fiber containing or small peptide
formulations may be utilized.
o Specialty high-lipid low-carbohydrate formulations designed to manipulate
the respiratory quotient and reduce CO2 production are not recommended
for routine use in ICU patients with acute respiratory failure.
o Serum phosphate levels should be monitored closely and replaced
appropriately when needed.
o EN is the preferred route of nutrition therapy in ICU patients with acute
and/or chronic liver disease.
o Nutrition regimens should avoid restricting protein in patients with liver
failure.
o Standard enteral formulations should be used in ICU patients with acute and
chronic liver disease.
o Branched chain amino acid formulations (BCAA) should be reserved for the
rare encephalopathy patient who is refractory to standard treatment with
Intensive Care Manual Controlled Copy Quality Department 90
luminal acting antibiotics and lactulose.
Reference. A.S.P.E.N. and SCCM recommendations. J Parenter Enteral Nutr 2009; 33; 277.
C. PARENTERAL NUTRITION
a. General principles
o There is considerable evidence now available that TPN is harmful in critically
ill patients.
o TPN is usually ordered by the Consultants
o IV access may be via a CVC or PICC line.
o A dedicated lumen for the TPN is required
b. Indications for TPN are
o GIT failure for more than 7-10 days.
(a) Prolonged post-operative ileus
(b) Malnourished at presentation to ICU and contraindicated for enteral
feed.
c. Complications of TPN
o Depression of immune function, especially in cancer patients
o Gut villous atropy
o Metabolic imbalance
(a) Electrolyte disturbances (K +, HP04- Mg -++)
(b) Glucose intolerance: hyperglycemia and glycosuria
(c) Hyperosmolar dehydration syndrome
(d) Rebound hypoglycemia on cessation of TPN
(e) Hyperbilirubinaemia
(f) CO2 production
o Fluid imbalance
o Trace element and vitamin deficiencies
o Central venous access complications
d. Protocol
o On commencement
Intensive Care Manual Controlled Copy Quality Department 91
(a) Check CVC/PICC line with X-Ray
(b) Commence TPN solution at a lower rate (40ml/hr) in starved because
of refeeding syndrome. It is due to the ICF movement of K and P04
with refeeding.
(c) Prescribe the balance of fluid according to the patient's serum
Chemistry and fluid requirements.
o Daily
a. Review the patient, CVC site, Biochemistry, and fluid balance.
b. These bags are pre-prepared and should not be altered, i.e. no further additives.
Patients requiring Potassium, Phosphates etc. above the quantities provided
should receive these in a separate line/infusion.
c. Some patients on TPN exhibit poor glycemic control. This places the patient at
significant risk of complications and should be managed actively.
d. Trace elements are to be added to the patients only on TPN.
e. Average daily requirements
Water 30-40 ml/kg/day
Calories 30-40 kcal/kg /day 1. Glucose: 2 g/kg/day at 4.1
kcal/g
2. Fat: 2 g/kg/day @ 9 kcal / g
Protein 0.5 –1.0 g/kg/day 1. 2:5 essential: total amino acids
2. 150: 1 Kcal: g N2 (non-nitrogen
kcal)
Sodium 1.0 mmol/kg/day
Potassium 1.0mmol/kg/day Dependent on Renal function
Phosphate 0.2 mmol/kg/day Dependent on Renal function
Vitamins B groups daily Trace elements as required
B12, Folate, A, D,E,K weekly
Replacement 1. Urine 1. ½ Normal saline ±10ml KCI/liter
Solutions 2. Nasogastric/ Ileostomy 2. ½ Normal saline ±10ml KCI/liter
3. Pancreatic/biliary fistulae 3. Ringer’s Lactate
Intensive Care Manual Controlled Copy Quality Department 92
D. Hemotherapy:
Refer to Blood Bank Policies in Hospital Policy Manual
E. ELECTROLYTE MANAGEMENT
I. General principles
a. Total body water (60% total body weight):
i. Intracellular fluid: predominant ions : K+, PO4
ii. Extracellular fluid:
a. 75% interstitial fluid: predominant ions: Na+, Cl-
b. 25% plasma volume (PV)
b. Osmotic equilibrium is maintained by Na+/K+ pump
i. ECF ions therefore reflect total osmolality
ii. Magnesium is a cofactor for this pump
c. Most electrolyte disturbances in critically ill patients relate to changes in the
distribution and concentrations of the predominant ECF and ICF ions.
d. As a general rule, changes in one ion shall be reflected in the associated cation or
anion.
e. Electrolyte disturbances shall be considered in terms of the following groups:
i. Erroneous results
a. Lab error
b. Bloods taken from a drip arm
c. Haemolysed specimen- traumatic (old IA lines), delayed samples
ii. Decreased or increased intake
iii. Decreased or increased losses: usually
a. Renal
b. Extra renal: GIT, skin losses
iv. Transcellular shifts:
f. Treatment shall be directed at the underlying cause.
g. Rapid correction of electrolyte disturbances may be deleterious
h. The following paragraphs outline the common electrolyte disturbances.
II. Hyponatraemia:
Sodium less than 130 mmol/l
a. Aetiology / classification
i. Hyperosmolar: measured osmolality more than 290
a. Hyperglycaemia
b. Mannitol
c. Ethanol, Methanol, Ethylene, Glycol
ii. Isoosmolal: measured osmolality 270-290
a. Hyperlipidaemia
Intensive Care Manual Controlled Copy Quality Department 93
b. Hyperproteinaemia not seen with ion-specific electrodes
c. IVT arm sample
iii. Hypo-osmolal: measured osmolality is less than 270
a. Hypovolaemia (Sodium depletion)
1. Renal
i. Diuretics
ii. Addison’s
iii. Polyuric Renal failure
2. Extra renal
i. GIT
ii. Burns
3. Transcellular water loss
b. Hypervolaemia (Water excess)
1. Extra renal
i. Excessive intake (IV 5% Dextrose)
ii. Oedematous states – CCF, cirrhosis, Nephrotic syndrome decreased
Albumin
2. Renal
i. Acute Renal failure, CRF
c. Normovolumia
1. Psychogenic polydipsia
2. SIADH
3. Hypothyroidism
Hyponatremia (serum sodium less than 135mEq/L) has been reported in 50% of
hospitalized patients with neurologic disorders.
Hyponatremic patients can have twice the mortalityrate of patients with a normal
plasma sodium.
Pseudohyponatremia
Extreme elevations in plasma lipids or proteins will increase the volume of the non-
aqueous phase of plasma.
The measured plasma sodium concentration can be significantly lower than the actual
sodium concentration.
Each 100mg/dl increase in blood sugars the sodium is decreased by 1.6meq/l.
Hypotonic Hyponatremia
True or hypotonic hyponatremia represents an increase in free water relative to sodium
in the extracellular fluids.
The ECV can be low, normal, or high in patients with hyponatremia.
Intensive Care Manual Controlled Copy Quality Department 94
Hypovolemic Hyponatremia
This condition is characterized by fluid losses combined with volume replacement using
a fluid that is hypotonic to the lost fluid.
The concentration of sodium in a random (spot) urine sample can sometimes help
determine if the sodium loss is renal or extrarenal in origin.
Site of Sodium Loss Urine Sodium
Renal >20 mEq/L
Extra renal <10 mEq/L
Renal sodium losses would be seen in diuretic overuse, adrenal insufficiency and in
cerebral salt-wasting syndrome. Extrarenal sodium losses can occur with diarrhea and
persistent vomiting.
Isovolemic Hyponatremia
Isovolemic hyponatremia is characterized by a small gain in free water, but not enough
to be clinically detected.
In this situation, the major disorders to consider are inappropriate release of ADH and
acute waterintoxication (psychogenic polydipsia).
The urine sodium and urine osmolality will help distinguish between these two
disorders.
Clinical Disorder Urine Sodium, Urine Osmolality
The inappropriate release of ADH is characterized by an inappropriately concentrated
urine (urine osmolality above 100 mOsm/kg in the face of a hypotonic plasma plasma
tonicity below 290 mOsm/kg H2O). This condition is known as the syndrome of
inappropriate ADH (SIADH).
In SIADH fluid restriction increases serum sodium.
In cerebral salt wasting syndrome fluid resuscitation to be done.
Serum uric acid is low in SIADH.
Hypervolemic hyponatremia
It represents an excess of sodium and water, with the water gain exceeding the sodium gain. In
this situation, the urine sodium can sometimes help identify the source of the problem.
Common Causes Urine Sodium
Heart failure < 20 mEq/L
Renal failure >20 mEq/L
Hepatic failure < 20 mEq/L
Intensive Care Manual Controlled Copy Quality Department 95
Management of hyponatremia
The management of hyponatremia is determined by the state of the ECV (i.e., low,
normal, or high) and by the presence or absence of neurological symptoms.
Symptomatic hyponatremia requires more aggressive corrective therapy than
asymptomatic hyponatremia.
To limit the risk of a demyelinating encephalopathy, the rate of rise in plasma sodium
should not exceed 0.5 mEq/L per hour and the final plasma sodium concentration
should not exceed 130 mEq/L.
The general management strategies based on the ECV are as follows:
Low ECV: Infuse hypertonic saline (3% NaCl) in symptomatic patients, and isotonic saline
in asymptomatic patients.
Normal ECV: Infusion of hypertonic saline in symptomatic patients or isotonic saline in
asymptomatic patients. Diuretics can be used in symptomatic patients.
High ECV: Use furosemide-induced diuresis in symptomatic patients. In symptomatic
patients, combine furosemide diuresis with judicious use of hypertonic saline.
Sodium Replacement
The sodium replacement therapy can be guided by the calculated sodium deficit.
The normal TBW is 60% of the lean body weight (in kg) in men, and 50% of the lean
body weight in women.
E.g. A 60 kg woman with a plasma sodium of 120 mEq/L, the sodium deficit will be 0.5 × 60 ×
(130 - 120) = 300 mEq. (130 is the target sodium). 3% sodium chloride contains 513 mEq of
sodium per liter, the volume of hypertonic saline needed to correct a sodium deficit of 300 mEq
will be 300/513 = 585 mL. Maximum rate of rise of 0.5 mEq/L per hour for the plasma sodium
the sodium concentration deficit of 10 mEq/L. The sodium deficit of 10 mEq/L in the previous
example should be corrected over at least 20 hours. The maximum rate of hypertonic fluid
administration will be 585/20 = 29 mL/hour.
Reference 1) Text book of Irwin rippe 2007
2) Text book of Fink 2008
Hypernatraemia:
Sodium more than 145 mmol/I
a. Aetiology / classification: always hyperosmolar
i. Hypovolaemic H2O loss > Na+ (most body fluids have a [Na+] < plasma net water
loss)
a. Renal
1. Diuretics, glucosuria
2. ARF/CRF, partial obstruction
3. Diabetes Insipidus
b. GIT losses: Diarrhea, vomiting, fistulae, SBO
c. Respiratory –IPPV with dry gases
Intensive Care Manual Controlled Copy Quality Department 96
d. Skin losses
1. Fever, high ambient temperature
2. Thyrotoxicosis
3. Vasodilatory states
4. Exfoliative skin disorders, burns
ii. Iso-hypovolaemic “pure water” less (plasma osmotic pressure, tends to maintain
intravascular volume mild-moderate decrease in ECF and ICF)
iii. Iso-hypervolaemic Na+ gain > H2O gain (plasma osmality ADH secretion ECFV,
with subsequent renal escape, thus Oedema in this group is rare)
a. Iatrogenic (major cause): NaHCO3, feeding formulate, TPN
b. Mineralocorticoid excess: usually has 1-3 of excess TBW
1. Conn’s, Cushing’s syndromes
2. Steroid excess
b. Management of hypernatremia
i. Hypovolaemic states
a. Restore volume according to clinical markers: BP, HR, urine output, RAP
1. Colloid: initial resuscitation, severe Hypovolaemic states.
2. Hartman’s solution- slightly hypo-osmolar
ii. Slow sodium correction: 2mmol/l/hr
a. Water deficit:- ~ (Na + - 140)/ 140 X (70 x 0.6) ~ 6.0 liters, 1 liter water
replacement shall raise Na+ 3-4mmol/l
b. In addition to basal fluid requirements and ongoing losses
c. Replace over a 24-48 hour period with 5% Dextrose
d. Monitor Sodium regularly
e. Manage etiological causes
f. Cease causal drugs and inappropriate IVT
g. DDAVP for central DI
III. Hypokalaemia:
Potassium less than 3.0 mmol/l
a. Etiology / Classification
i. Transcellular shift
a. Alkalemia pH~ 0.1 [K+}pl~0.5 mmol/l
b. Catecholamines / Salbutamol
c. Insulin
d. Familial periodic paralysis
e. Anabolism – refeeding effect
f. Hypomagnesaemia – ICF Potassium depletion
ii. Reduced intake
a. Starvation
b. TPN
iii. Increased clearance
Intensive Care Manual Controlled Copy Quality Department 97
a. Renal
1. Diuretics leading to raised distal tubular flow
i. PT agents – Acetazolamide, Mannitol
ii. Loop agents – Frusemide, Bemutanide
iii. Early DT- Thiazides
2. Steroids / Mineralocorticoid excess
3. Anionic drugs
i. Antibiotics (Penicillins)
ii. Amphotericin
4. Hypomagnesaemia, Hypocalcaemia
5. Lithium
6. RTA I,II
b. Non-renal
1. GIT
i. Villous Adenoma
ii. Ureterosigmoidostomy
iii. Fistulae, malabsorption syndromes
iv. Diarrhea, Laxatives
2. Skin losses
b. Management of hypokalemia
i. Treat underlying cause
ii. Correct hypovolaemia: volume contraction shall potentiate both alkalosis and
hypokalemia
iii. Always add Magnesium: normomagnesemia is essential for correction of
hypokalaemia
iv. Causes and treatment of hypophosphataemia same as decreased Potassium
v. Potassium preparations
a. KCL: 10 ml = 1g= 13.4 mmol/l
b. KH2PO4: 10ml = 10 mmol/l
c. K-acetate: 10ml at 5 mmol/ml 50 mmol K+ +50 mmol acetate.
d. K-acetate: 10ml at 5 mmol/ml 50 mmol K ++50 mmol acetate.
(Bicarbonate)
IV. Hyperkalaemia:
Potassium more than 5.0 mmol/l
a. Aetiology / Classification
i. Artefactual
a. Drip arm specimen
b. Tourniquet / Haemolysed (extravascular)
c. Thrombocytosis (more than 750,000)
d. Leucocytosis more than 50,000
Intensive Care Manual Controlled Copy Quality Department 98
ii. Transcellular exchange
a. Acidosis breakdown
b. Tissue breakdown
c. Rhabdomyolysis, haemolysis (intravascular), ischemia / reperfusion
d. Severe burns
e. Tumour Lysis Syndrome
f. Leukaemia
g. Familial periodic paralysis
h. Suxamethonium paralysis
i. Insulin deficiency: DKA
NB: Normo-or hypokalaemia in the presence of severe DKA is associated with a marked
total body potassium deficit, which shall be addressed prior to correction of the
acidaemia.
j. Increased ECF tonicity: movement of water from cells the [K+] ICF and passive
diffusion seen with large doses of Mannitol given rapidly (1.5-2.0 g/kg),
Hyperkalaemia of DKA is due to this in addition to the acidaemia and Insulin
deficiency.
k. Beta blockers
iii. Increased intake- rarely a problem unless impaired Renal function.
a. Direct IV / oral
b. Drugs (Penicillins)
c. Transfusion
iv. Reduced clearance
a. Acute Renal failure
1. Any cause for decreased distal tubular flow, or decreased distal NaCl delivery
2. Hypoaldosteronism (Mineralocorticoid deficiency, Addison’s) – K+ is
multifactorial (K+ ICF K+ ECF, distal tubular flow and DT Aldosterone effect)
b. Type IV RTA
c. Potassium sparing diuretics
1. Aldosterone antagonists - Spironolactone
2. Distal Sodium channel inhibitors- Amiloride, Triamterene
b. Management of hyperkalemia
Calcium.
Calcium directly antagonizes the myocardial effects of hyperkalemia without lowering
Plasma potassium.Calcium is beneficial even in patients who are normocalcemic.
The recommended dose is 10 mL intravenous over 10 mins. The onset of action is 3
mins.
The ECG should be monitored continuously. The dose may be repeated in 5 mins if there
is no improvement in the EKG.
Insulin.
Intensive Care Manual Controlled Copy Quality Department 99
Insulin reliably lowers Plasma potassium in patients with end-stage renal disease
confirming its effect to shift Kinto cells. An intravenous dose of ten units of regular
insulin given as a bolus along with an intravenous bolus of dextrose ( 25% solution)
Bicarbonate.
Sodium bicarbonate should be given for hyperkalemic patientwith metabolic acidosis
Hypertonic Saline. Intravenous hypertonic sodium chloride has been shown to reverse
the EKG changes of hyperkalemia in patients with concurrent hyponatremia.This effect
seems to be mediated by a change in the electrical properties of cardiomyocytes rather
than by a reduction in Plasma potassium.
Enhanced Renal Elimination
Loop-acting diuretics alone or in combination with a thiazide diuretic will induce a
kaliuresis and will be beneficialin the volume expanded patient.
Diuretic induced volume contraction must be avoided since this will lead to decreased
distal nephron flow and reduced K excretion.
Exchange Resin.
Sodium polystyrene sulfonate (SPS, Kayexalate, Kionex) is a cation-exchange resin that
is prepared in the sodium phase but has a higher affinity for potassium than sodium.
Dialysis.
Hemodialysis is the method of choice for removal of potassium from the body.
Intensive Care Manual Controlled Copy Quality Department 100
References. Management of severe hyperkalemia.Crit Care Med 2008; 36:3246 –3251
V. Other Electrolyte Abnormalities
1. Calcium
Calcium is required for muscle contraction, nerve impulse transmission, hormone
secretion, blood clotting, cell division, cell motility, and wound healing. Effective calcium
levels are best assessed by using ionized calcium measurements, if available. If
treatment decisions are based on total serum calcium, the albumin concentration must
be considered. In general, for each increase or decrease in serum albumin of 1 g/dL, the
serum calcium increases or decreases by 0.8 mg/dL (0.2 mmol/L). However, the
relationship between albumin and serum calcium is less reliable in critically ill patients.
a. Hypocalcemia (Total Calcium <8.5 mg/dL [<2.12mmol/L], Ionized Calcium <1.0
mmol/L)
Hypocalcemia is common in critically ill patients and results from impairment of the
parathyroid and / or vitamin D systems (Table 12-5). Cardiovascular abnormalities,
the most common clinical manifestations of hypocalcemia in critically ill patients,
include hypotension, bradycardia, arrhythmias, heart failure, cardiac arrest, digitalis
insensitivity, and QT interval and ST segment prolongation. Neuromuscular
manifestations include weakness, muscle spasm, laryngospasm, hyperreflexia,
seizures, tetany, and paresthesias.
Causes of hypocalcemia
Hypoparathyroidism Malabsorption
Sepsis Liver disease
Burns Renal disease
Rhabdomyolysis Calcium chelators
Pancreatitis Hypomagnesemia
Massive transfusion
Treatment is aimed at correcting the underlying disease process and any concomitant
electrolyte abnormalities, and administering calcium. Mild hypocalcemia is well
tolerated, and aggressive treatment may result in tissue injury (especially during
Ischemic and septic states). If the hypocalcemia is severe or if the patient is
symptomatic, administer 100 mg calcium intravenously over 5 to 10 minutes (3 to 4 mL
of 10% calcium chloride, 10mL of 10% calcium gluconate), followed by 0.3 to 2.0
mg/kg/hr. Calcium preparations vary in the content of calcium: 10% calcium chloride 1 g
= 10 mL = 272 mg of calcium; 10% calcium may be replaced via the Enteral rout (i.e.,500
to 1000 mg every 6 hours).
Intensive Care Manual Controlled Copy Quality Department 101
Monitor ionized or total calcium levels frequently during treatment, and adjust repletion
to maintain calcium in the lower normal range, so as not to suppress parathyroid gland
function. If calcium replacement alone fails to maintain the circulating calcium level,
consider administration of vitamin D and magnesium. Adverse effects of calcium
administration include Hypercalcemia, bradycardia, nausea/vomiting flushing, tissue
calcium precipitation, and digitals toxicity.
Critically ill newborns are particularly prone to hypocalcemia because these
patients experience a sudden withdrawal from a high rate of calcium intake
associate with normal maternal-to-fetal transfer of calcium during gestation. The
following doses should be used to correct life-threatening hypocalcemia in
children:
Calcium gluconate (10%), 0.5 to 1.0 mL/Kg
Calcium chloride (10%), 0.1 to 0.2 mL/kg
b. Hypercalcemia (Total Calcium > 11 mg/dl [>2.75 mmol/L], Ionized Calcium > 1.3
mmol/L)
The most common causes of Hypercalcemia are the result of calcium release from bone.
The clinical manifestations of Hypercalcemia relate primarily to the cardiovascular and
neuromuscular systems and include hypertension, cardiac ischemia, arrhythmias,
bradycardia, conduction abnormalities, digitalis toxicity, dehydration, hypotension,
weakness, depressed mentation, coma, seizures, and sudden death. Gastrointestinal
manifestations include nausea/vomiting, anorexia, abdominal pain, constipation,
Pancreatitis, and ulcer disease. Nephrogenic diabetes insipidus with polyuria may occur
and when present contributes to volume depletion. Renal stones, nephrocalcinosis, and
renal failure are also encountered.
Causes of Hypercalcemia
Hyperparathyroidism Excess vitamin A or D intake
Malignancy Thyrotoxicosis
Immobilization Ganulomatous disease
Treatment of Hypercalcemia is aimed at controlling the underlying disease, rehydrating
the patient, rehydrating the patient, and lowering the calcium level. The circulating
calcium level frequently needs to be lowered while the primary disease is being
evaluated and treated. Intravascular volume should be restored with normal saline to
assure adequate tissue perfusion and renal blood flow (urine output 2 to 3 mL/kg/hr).
Saline also decreases renal tubular calcium reabsorption. Diuresis with a loop diuretic
further increases renal calcium loss. In patients with renal failure or life-threatening
Hypercalcemia, calcium levels may be lowered with dialysis. After initial stabilization,
therapy with calcitonin, mithramycin, or diphosphonates can be considered.
Intensive Care Manual Controlled Copy Quality Department 102
For Pediatric Patients
Hypercalcemia is rare in the pediatric population. Treatment is similar to that
described for adults: saline infusion + furosemide (1 to 2 mg/kg every 6 to 12
hours)
c. Hypophosphatemia (Phosphate < 2.5 mg/dl [0.81 mmol/L])
Phosphate is important in cellular energy metabolism. Hypophosphatemia results from
transcellular shifts, renal loss, gastrointestinal loss, or inadequate intake. Phosphate
depletion primarily affects the neuromuscular and central nervous systems. Clinical
manifestations include muscle weakness, respiratory failure,(difficulty in weaning the
patient) Rhabdomyolysis, paresthesias, lethargy, disorientation, obtundation, coma,
and seizures. Other manifestations include impaired renal tubular function, impaired
pressor responses, hepatic dysfunction, immune dysfunction, impaired protein
synthesis, hemolysis, impaired platelet function, and impaired oxygen offloading from
hemoglobin.
Causes of hypophosphatemia
Gastrointestinal Decreased
Transcellular Shift Renal Loss
Loss Intake
Acute alkalosis Hypoparathyroidism Malabsorption Malnutrition
Carbohydrate Diuretic use Diarrhea Parenteral
administration nutrition
Drugs (insulin, Hypokalemia Intestinal fistulas
epinephrine)
Hypomagnesemia Antacids
Steroids
Treatment of hypophosphatemia consists of controlling the underlying disease,
removing offending drugs, correcting electrolyte abnormalities, and replacing
phosphate. Phosphate levels < 1 mg/dl (<0.32 mmol/L) associated with symptoms are
considered life-threatening and require immediate treatment. For emergency
treatment, administer phosphate at 0.6 to 0.9 mg/kg/hr intravenously. When circulating
phosphate levels are stable, maintenance replacement of phosphate is 1000 mg/day
Intensive Care Manual Controlled Copy Quality Department 103
intravenously plus excess losses (i.e., in urine or stool). Phosphate is not available as
intravenous injections so given as phosphate containing enema and amount to be given
and its absorption and increase in serum levels are unpredictable.
Serum phosphate should be monitored during repletion and therapy adjusted to
achieve a circulating level of 3 to 4 mg/dL (0.97 to 1.29 mmol/L). Adverse effects of
phosphate administration include hyperphosphatemia, hypocalcemia, tissue calcium
precipitation, renal injury, and diarrhea (enteral phosphate).
For Pediatric Patients
Hypophosphatemia is relatively uncommon in children and is usually associated
with malnutrition or malabsorption syndromes. Life-threatening
hypophosphatemia in children can be treated with 5mg/kg phosphate
intravenously as sodium or potassium phosphate.
d. Hypomagnesemia (Magnesium < 1.8 mg/dL or 1.5 mEq/dL [<0.75 mmol/L])
Magnesium is important to the body for energy transfer and electrical stability. Causes
of hypomagnesemia are listed in Table.
Clinical manifestations of hypomagnesemia overlap those of hypokalemia and
hypocalcemia. These manifestations include cardiovascular abnormalities (e.g. QT
interval prolongation, arrhythmias, vasospasm, ischemia), neuromuscular abnormalities
(i.e., weakness, tremor, seizures, tetany, obtundation, coma), and electrolyte
abnormalities (e.g., hypokalemia, hypocalcemia).
Causes of hypomagnesemia
Gastrointestinal
Renal Loss Transcellular shift Decreased intake
Loss
Renal tubular Malabsorption Refeeding Malnutrition
dysfunction Diarrhea Recovery from Alcoholism
Diuresis Nasogastric hypothermia Parenteral
suction nutrition
Hypokalemia Drugs
(aminoglycosides,
amphotericin etc.)
Treatment of hypomagnesemia consists of treating the underlying disease,
discontinuing problematic drugs, correcting concomitant electrolyte abnormalities, and
replenishing magnesium. For emergency treatment of hypomagnesemia (e.g.,
arrhythmias), administer 1 to 2 g magnesium sulfate intravenously over 5 to 10 minutes.
Magnesium sulfate can be administered over a longer interval (10 to 60 minutes) in less
Intensive Care Manual Controlled Copy Quality Department 104
urgent situations. Depending on the clinical situation, subsequent intravenous
replacement ranges from 1 to 2 g magnesium sulfate every 4 to 6 hours. Once serum
magnesium levels stabilize, intravenous maintenance doses are 0.1 to 0.2 mmol /kg/day
(1 g magnesium sulfate = 8 mmol). Maintenance magnesium may also be administered
enterally. The dose of magnesium should be reduced if renal failure is present..
Magnesium levels should be monitored during repletion.
Manifestation Serum Magnesium
Hyporeflexia >4 mEq/L
1st° AV Block >5 mEq/L
Complete Heart Block >10 mEq/L
Cardiac Arrest >13 mEq/L
Hypomagnesemia in children is commonly associated with malnutrition or
malabsorption syndromes and with poor gut function in critically ill infants
receiving prolonged intravenous fluid administration. Life-threatening
hypomagnesemia may be treated with magnesium sulfate (25 to 50 mg/kg
intravenously over 5 to 15 minutes)
9. METABOLIC DISTURBANCES
A. ACUTE ADRENAL INSUFFICIENCY
Lack of specific signs and symptoms makes early recognition of acute adrenal
insufficiency difficult. Adrenal insufficiency may result from failure of the adrenal glands
(e.g., autoimmune disease, granulomatous disease, human immunodeficiency virus
[HIV] infection, adrenal hemorrhage, meningococcemia, ketoconazole) or failure of the
hypothalamic/pituitary axis (e.g., withdrawal from glucocorticoid therapy). Primary
adrenal gland failure results in loss of both glucocorticoid and mineralocorticoid
secretion, whereas secondary adrenal gland failure causes only glucocorticoid
deficiency.
Clinical manifestations suggestive of acute adrenal insufficiency include weakness,
nausea/vomiting, abdominal pain, orthostatic hypotension, hypotension refractory to
volume or vasopressor agents, and fever. Suggestive laboratory findings include
hyponatremia, hyperkalemia, acidosis, hypoglycemia, and prerenal azotemia.
Emergent treatment is indicated in critically ill patients , even if the diagnosis is not
established. High-risk patients include those with the acquired immune deficiency
syndrome (AIDS), disseminated tuberculosis, sepsis, or acute anticoagulation, as well as
postcoronary artery bypass grafting patients and patients from whom glucocorticoid
therapy was withdrawn within the past 12 months. When dexamethasone is used
Intensive Care Manual Controlled Copy Quality Department 105
initially for emergent steroid replacement, a short adrenocorticotropic hormone (ACTH)
stimulation test can be performed for diagnosis after resuscitative therapy is instituted
because this corticosteroid does not interfere with serum cortisol assay. The treatment
steps for acute adrenal insufficiency are as follow:
Obtain baseline blood samples for cortisol, electrolytes, etc.
Infuse D5 normal saline to support blood pressure.
Administer dexamethasone 4 mg intravenously, then 4 mg intravenously
every 6 hours.
Perform short adrenocorticotropic hormone stimulation test if needed for
diagnosis.
If the diagnosis of adrenal insufficiency is confirmed, hydrocortisone 100 mg
intravenously every 8 hours can be administered. Some physicians prefer
administration of hydrocortisone as a continuous infusion, 300 mg over 24
hours.
Treat precipitating conditions.
For pediatric patients
Adrenal insufficiency in children may be increasing in frequency as a result of
adrenal suppression from therapeutic steroids. In addition, a unique cause of
adrenal insufficiency in infants is congenital adrenal hyperplasia, the result of an
inborn abnormality in adrenal cortical enzymes. The symptoms (e.g., vomiting,
enlarged phallus) develop gradually during the first month of life. Treatment
includes saline infusion to correct circulatory failure, mineralocorticoid
administration with deoxycorticoid acetate (1 mg intramuscularly), and
glucocorticoid replacement with hydrocortisone (25 mg intravenously, followed by
50 mg/m2/24 hour) as a constant infusion. Symptomatic sodium and potassium
abnormalities should be treated as described above for electrolyte abnormalities.
B. HYPERGLYCEMIC SYNDROMES
Serious metabolic complications of diabetes result from a relative or absolute lack of insulin
coupled with increased production of counter regulatory hormones such as glucagon,
catecholamines, and others. Life-threatening hyperglycemic syndromes include diabetic
ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS).
Clinical manifestations result from hyperglycemia and excess ketone production.
Hyperglycemia causes hyperosmolality, osmotic diuresis, fluid and electrolyte loss,
dehydration, and volume depletion. Ketones (DKA) cause acidosis and osmotic diuresis.
Clinical features of hyperglycemic syndromes include weakness, dehydration, polydipsia,
altered mental status, coma, tachycardia, arrhythmias, hypotension, anorexia,
Intensive Care Manual Controlled Copy Quality Department 106
nausea/vomiting, ileus, abdominal pain, hyperpnea, and fruity odor to the breath (DKA).
Laboratory investigation reveals hyperglycemia, hyperosmolality (more common in HHS),
glucosuria, ketonemia/ketonuria (DKA), anion gap metabolic acidosis (DKA), hypokalemia,
hyphosphatemia, hypomagnesemia, leukocytosis, azotemia, and elevated amylase and
creatine phosphokinase.
The goals of treatment of hyperglycemic syndromes are to restore the fluid and electrolyte
balance, provide insulin, and identify precipitating factors (e.g., infection, stroke, myocardial
infarction, pancreatitis, corticosteroids). Volume deficits correlate with the severity of
hyperglycemia and are usually greater in HHS. Normal saline should be used to replenish
intravascular volume and restore hemodynamic stability and renal perfusion (i.e., 1 liter in
the first hour, then 250 to 500 mL/hr as need). After administration of 1 to 2 L of normal
saline, fluids with less chloride (e.g., 0.45% saline) should be used to avoid or minimize the
development of hyperchloremic metabolic acidosis. The corrected serum sodium [measured
sodium + (1.6 x glucose/100)] should also be used to guide fluid selection. Urine output
should be maintained at 1 to 3 mL/kg/hr to ensure adequate tissue perfusion and clearance
of glucose. Invasive hemodynamic monitoring (e.g., arterial catheter and central venous
catheter ) may be required in patients with underlying cardiovascular disease.
Priorities in initial resuscitation of diabetic ketoacidosis
1. Institute crystalloid resuscitation, initially with normal saline
2. Institute insulin bolus (0.1 to 0.15 U/kg) and infusion at 0.1 U/kg/hr.
3. Consider bicarbonate only if pH < 7.0
4. Look for precipitating cause of DKA (infection, myocardial infarction,
pancreatitis, trauma, etc)
5. Add potassium chloride to IV fluids when serum potassium is known or
expected to be low or normal, and urine output is documented.
6. Add glucose to crystalloid infusion when serum glucose is 250 to 300
mg/dL (13.9 to 16.7mmol/L). Do not decrease insulin infusion rate.
Administer 10% dextrose if necessary to maintain serum glucose > 150
mg/dL (>8.3 mmol/L).
7. Continue insulin infusion until ketosis is cleared (negative serum ketones
with correction of increased anion gap).
Give 0.1 to 0.15 U/kg regular human insulin intravenously as a loading dose in DKA,
followed by 5 to 10 units of regular insulin per hour (0.1 U/kg/hr). The intravenous route
Intensive Care Manual Controlled Copy Quality Department 107
is the most reliable and easiest to titrate. Because of the short half-life of intravenous
insulin, a continuous infusion,we will follow protocolised sliding sclaes A&B depending
on the patient conditions and treating physicial preference,(Annexure A&B attached),is
necessary with serial monitoring of the blood glucose and electrolyte concentrations.
Smaller doses of insulin are usually adequate in HHS. Monitor glucose levels frequently,
and when glucose decreases to 250 to 300 mg/dL (13.9 to 16.7 mmol/L), switch to
glucose-containing fluids to avoid hypoglycemia. Glucose-containing fluids may be
started earlier if blood glucose cannot be monitored frequently. Administration of 10%
dextrose may be necessary to maintain glucose levels > 150 mg/dL (> 8.3 mmol/L) while
continuing insulin infusion for clearing ketones. When blood glucose is controlled,
ketonemia has cleared, and the patient is stable, the patient may be advanced to
subcutaneous insulin. An insulin sliding scale with subcutaneous administration of
regular and longer-acting preparations can be started and should be overlap with
discontinuation of the insulin infusion.
Insulin and correction of acidosis shift potassium intracellularly and may lead to
precipitous drops in serum potassium levels. Potassium deficits range from 3 to 10
mmol/kg. Potassium should be added to fluid therapy as soon as serum potassium is
recognized to be < 5.5 mmol/L and urine output is documented. Oral potassium
replacement can be considered if nausea and vomiting are not present. Potassium and
other electrolyte levels should be monitored frequently until levels stabilize and acidosis
is resolved. (eg. DKA)
Consider phosphate replacement if serum levels are low. Magnesium should be
administered if hypomagnesemia is present. Acidosis is well tolerated by patients with
DKA, and bicarbonate therapy, which is controversial, is rarely needed. Bicarbonate
administration may be considered if the arterial pH is < 7.0 (give 25 to 50 mmol
bicarbonate over 1 hour to increase pH > 7.0). Do not attempt to normalize blood pH
with bicarbonate, since acidosis resolves as ketones are metabolized.
For Pediatric Patients
A bolus of insulin is not necessary in pediatric patients with DKA, and the insulin
infusion is initiated as for adults. Bicarbonate, if needed, can be administered in a
dose of 1 to 2 mmol/kg. Careful attention should be given to dilute fluid volumes to
avoid the potential complication of cerebral edema. Cerebral edema and increased
intracranial pressure have been associated with too-rapid administration of large
volumes of dilute resuscitation fluid (>4000 mL/m2/day or 2.7 times the normal
maintenance rate). A useful guide to fluid resuscitation in children with DKA is to
follow serial measurements of the serum sodium. As ketoacidosis comes under
control and the glucose level falls, the serum sodium (previously falsely depressed
because of high glucose levels) should rise. A serum sodium level that does not rise
during fluid resuscitation suggests that too much free water is being administered.
Intensive Care Manual Controlled Copy Quality Department 108
A decrease in total fluid administration, an increase in the sodium concentration of
the resuscitation fluid, or, if the patient is symptomatic, an acute elevation of the
serum sodium may be helpful. If the patient’s neurologic status continues to
deteriorate, an evaluation for cerebral swelling and treatment should be instituted.
C. ADDITIONAL METABOLIC DISTURBANCES
I. THYROID STORM
Thyroid storm usually occurs in patients with Graves’ disease or toxic nodular goiter.
Precipitating factors include infection, surgery, labor/delivery, acute medical illness,
trauma, or emotional stress. Thyroid storm is characterized by exaggerated classic
manifestations of hyperthyroidism plus fever, CNS dysfunction (apathy, agitation, coma
etc.), congestive heart failure, arrhythmias, and gastrointestinal symptoms (vomiting,
diarrhea, jaundice).
Therapy should be initiated immediately without awaiting results of thyroid hormone
tests. An endocrinologist or critical care specialist should be consulted as soon as
possible. Supportive and specific measures are listed below.
Supportive measures:
Cooling: acetaminophen, cooling blankets (salicylates should be
avoided since salicylates affect binding of T4 and T3 to their binding
proteins)
Hydration: glucose-containing fluids
Treat the precipitating cause.
Specific measures:
Inhibit T4 synthesis: propylthiouracil 800 t0 1200 mg orally initially,
then 200 to 300 mg orally every 6 hours; or methimazole 80 to 120
mg orally or rectally initially, then 20 to 30 mg orally or rectally
every 6 hours
Inhibit adrenergic effects: Propranolol 1.0 to 10 mg intravenously
(titrated) or 40 to 120mg orally every 6 hours
Inhibit T4 release: saturated solution of potassium iodide (SSKI) 5
drops orally every 6 to 8 hours; or sodium iodine 0.5 g intravenously
every 12 hours. Initiate 1 hour after propylthiouracil or
methimazole is given.
Inhibit T4 to T3 conversion: dexamethasone 2 mg intravenously or
orally every 6 hours; sodium ipodate 0.5 to 1.0 g orally every day.
Intensive Care Manual Controlled Copy Quality Department 109
Thyroid storm is infrequent in children. Occasionally, thyroid is seen in neonates
born to mothers with hypothyroidism or circulating thyroid-stimulating
antibodies. The thyroid disease spontaneously remits in 1 to 2 months, but
treatment as listed below may be necessary during that period:
Propylthiouracil 6 to 10 mg/kg/day orally every 8 hours in
equal doses or methimazole 0.6 to 0.7 mg/kg/day orally
every 8 hours.
SSKI 0.3 mL orally every 8 hours.
Dexamethasone 0.2 mg/kg/day.
Propranolol 30 to 100 µg/kg/day intravenously (titrated),
then 0.5 to 10 mg/ kg/ day in three to four equal doses.
II. MYXEDEMA COMA
Myxedema coma (life-threatening hypothyroidism) is a rare manifestation of chronic
hypothyroidism that occurs most frequently in elderly patients during winter months.
Precipitating factors include infection, drugs (e.g. sedatives, hypnotics), surgery,
neurologic disorders (e.g., Cerebrovascular accident, seizures), acute medical illness,
trauma, and exposure to cold. Clinical manifestations are an exaggeration of less severe
hypothyroidism and result in widespread organ dysfunction. Features of life-threatening
hypothyroidism include hypothermia, obtundation/coma, bradycardia, heart failure,
hypoventilation, hyporeflexia, hyponatremia, hypoglycemia, anemia, and decreased ECG
voltage.
The diagnosis of myxedema coma is clinical, and treatment should not be delayed
pending laboratory results. Treatment with T4 is unlikely to cause harm if the diagnosis
is in error, but delay in therapy can be fatal. An endocrinologist or clinical care specialist
should be consulted as soon as possible. In addition to obtaining blood for thyroid
hormone tests, the following measures should be instituted:
Secure airway and ventilate, if necessary.
Treat hypotension with fluids
Treat precipitating cause
Provide passive warming (e.g., blankets)
Provide glucose
Treat significant hyponatremia with diuresis (e.g., loop diuretic)
Give hydrocortisone 100 mg intravenously every 8 hours, or assess adrenal
functions
Administer L-thyroxine (T4), 300 to 500 µg daily; children, 4 µg daily.
Intensive Care Manual Controlled Copy Quality Department 110
9. ACID BASE DISTURBANCE IN ICU
a. Acid base disturbances in Intensive Care are frequently mixed metabolic and respiratory
disorders.
b. Correction to these disturbances shall be directed at the underlying cause and
maintenance of cardiopulmonary homeostasis
c. Primary correction of an acid base disturbance with acid or alkali is seldom required
How to read an ABG
Stage I: Identify the Primary Acid-Base Disorder
In the first stage of the approach, the measured PaCO2 and pH are used to determine if an
acid-base disturbance is present and, if so, to identify the primary acid-base disorder.
Rule 1: An acid-base abnormality is present if either the PaCO2 or the pH is outside the
normal range.
Rule 2: If the pH and PaCO2 are both abnormal, compare the directional change. If both
change in the same direction (both increase or decrease), the primary acid-base disorder is
metabolic, and if both change in opposite directions, the primary acid-base disorder is
respiratory.
Example: Consider a patient with an arterial pH of 7.23 and a PaCO2 of 23 mm Hg. The pH
and PaCO2 are both reduced (indicating a primary metabolic problem) and the pH is low
(indicating acidemia), so the problem is a primary metabolic acidosis.
Rule 3: If either the pH or PaCO2 is normal, there is a mixed metabolic and respiratory acid-
base disorder (one is an acidosis and the other is an alkalosis). If the pH is normal, the
direction of change in PaCO2 identifies the respiratory disorder, and if the PaCO2 is normal,
the direction of change in the pH identifies the metabolic disorder.
Example: Consider a patient with an arterial pH of 7.37 and a PaCO2 of 55 mm Hg. The pH
is normal, so there is a mixed metabolic and respiratory acid-base disorder. The PaCO2 is
elevated, so the respiratory disorder is an acidosis, and thus the metabolic disorder must
be an alkalosis. Therefore, this is a combined respiratory acidosis and metabolic alkalosis.
There is no primary acid-base disorder in this situation; both disorders are equivalent in
severity (which is why the pH is normal).
Remember that the compensatory responses to a primary acid-base disturbance are
never strong enough to correct the pH, but act to reduce the severity of the change in pH.
Therefore, a normal pH in the presence of an acid-base disorder always signifies a mixed
respiratory and metabolic acid-base disorder. (It is sometimes easier to think of this
situation as a condition of overcompensation for one of the acid-base disorders.)
Stage II: Evaluate Compensatory Responses
The second stage of the approach is for cases where a primary acid-base disorder has
been identified in StageI. (If a mixed acid-base disorder was identified in Stage I, go
directly to Stage III.) The goal in Stage II is to determine if the compensatory responses are
adequate and if there are additional acid-base derangements.
Rule 4: If there is a primary metabolic acidosis or alkalosis, use the measured serum
bicarbonate concentration to identify the expected PaCO2. If the measured and expected
PaCO2 are equivalent, the condition is fully compensated. If the measured PaCO2 is higher
than the expected PaCO2, there is a superimposed respiratory acidosis.
Intensive Care Manual Controlled Copy Quality Department 111
• In Metabolic acidosis the expected PaCO2 is (1.5 × HCO3) + (8 ± 2) mm Hg.
• If the measured PaCO2 is equivalent to the expected PaCO2, then the respiratory
compensation is adequate, and the condition is called a compensated metabolic
acidosis.
Example: Consider a patient with a PaCO2 of 23 mm Hg, an arterial pH of 7.32, and a serum
HCO3 of 15 mEq/L. The pH is acidemic and the pH and PCO2 change in the same direction,
so there is a primary metabolic acidosis. The expected PCO2: (1.5 × 15) + (8 ±2) = 30.5 ± 2
mm Hg. The measured PaCO2 (23 mm Hg) is lower than the expected PaCO2, so there is an
additional respiratory alkalosis. Therefore, this condition can be described as a primary
metabolic acidosis with a superimposed respiratory alkalosis.
In metabolic alkalosis expected PaCO2 = (0.7 x HCO3-) + (21 ± 2)
• Metabolic alkalosis with a plasma HCO3 of 40 mEq/L
expected PCO2 is (0.7 × 40) + (21 ± 2) = 49 ± 2 mm Hg.
measured PaCO2 is equivalent to the expected PaCO2, then the respiratory
compensation is adequate, and the condition is called a compensated metabolic alkalosis.
Rule 5: If there is a respiratory acidosis or alkalosis, use the PaCO2 to calculate the
expected pH.
Compare the measured pH to the expected pH to determine if the condition is acute,
partially compensated, or fully compensated. For respiratory acidosis, if the measured pH is
lower than the expected pH for the acute, uncompensated condition, there is a
superimposed metabolic acidosis, and if the measured pH is higher than the expected pH
for the chronic, compensated condition, there is a superimposed metabolic alkalosis. For
respiratory alkalosis, if the measured pH is higher than the expected pH for the acute,
uncompensated condition, there is a superimposed metabolic alkalosis, and if the
measured pH is below the expected pH for
the chronic, compensated condition, there is a superimposed metabolic acidosis.
Acute respiratory acidosis: pH decrease = 0.08 x (PaCO2 - 40)
Acute respiratory alkalosis: pH increase = 0.08 x (40 - PaCO2)
Chronic respiratory acidosis: pH decrease = 0.03 x (PaCO2 - 40)
Chronic respiratory alkalosis pH increase = 0.03 x (40 - PaCO2)
Example: Consider a patient with a PaCO2 of 23 mm Hg and a pH of 7.54. The PaCO2 and
pH change in opposite directions so the primary problem is respiratory and, since the pH is
alkalemic, this is a primary respiratory alkalosis. The expected pH for an acute respiratory
alkalosis is described as
7.40 + [0.008 × (40 - 23)] = 7.54.
This is the same as the measured pH, so this is an acute, uncompensated respiratory
alkalosis. If the measured pH was higher than 7.55, this would be evidence of a
superimposed metabolic alkalosis.
Stage III: Use The “Gaps” to Evaluate Metabolic Acidosis
Intensive Care Manual Controlled Copy Quality Department 112
The final stage of this approach is for patients with a metabolic acidosis, and it involves two
determinations known as gaps. The first is the anion gap, which is an estimate of
unmeasured anions that helps to identify the cause of a metabolic acidosis. The second gap
is a comparison of the change in the anion gap and the change in the serum HCO3
concentration: the gap between the two (known as the gap-gap) can uncover mixed
metabolic disorders (e.g., a metabolic acidosis and alkalosis) that would otherwise go
undetected. These two measurements are described in the next section.
A. METABOLIC ACIDOSIS
a. Appreciation of acid base (specifically metabolic acidosis) shall be taken in the
context of the anion gap
Anion Gap = [Na + K]- [Cl + HCO3 ] ~ 12-17 mmol/l
UNMEASURED CATAIONS UNMEASURED ANION
Mg+++ ~ 1.2 mmol/l Albumin ~ 15 mEq/l
Ca++ ~ 2.2 mmol/l H2PO4- ~ 2 mmol/l
IgG Small HSO4 - ~ 1 mmol/l Organic~5mEq/l~7.0mEq/l~23 mEq/l
b. This allows classification of metabolic acidosis into raised or normal anion gap
acidosis.
NB:While this is a classical “text book” subdivision, one shall be aware that the
measurement of Chlorides in the lab is highly variable and assessment of the anion gap
shall always be viewed within the clinical context.
c. Aetiology of raised anion gap
i. Renal failure ~ H2 PO4 -, HSO4 ~ (rarely more than 23)
ii. Lactic acidosis – types A and B * normal AG does not exclude a lactic acidosis
iii. Ketoacids (Hydroxy-butyrate, Acetoacetate): Diabetes Mellitus, starvation,
alcohol
iv. Rhabdomyolysis – organic acids
v. Drugs / poisons:
a. Aspirin – Salicylate, Lactate, Ketones
b. Ethanol – Acetoacetate, lactate
c. Methanol – Formate (Formaldehyde), Lactate
d. Methanol – Formate, Acetate, Lactate, Pyruvate
e. Ethylene Glycol - Oxalate
f. Fructose – Lactate
d. Aetiology of low or normal anion gap
i. Hyperchloraemic metabolic acidosis
a. Resolving Renal failure
Intensive Care Manual Controlled Copy Quality Department 113
b. Resolving DKA
c. Renal tubular acidosis / Carbonic Anhydrase inhibitors
d. Mineralocorticoid deficiency
e. Pancreatic, enteric fistulae
f. Ureterosigmoidostomy
g. IV HCL, Ammonium Chloride, Arginine
ii. Metabolic alkalosis due to Bicarbonate gain
iii. Hypoalbuminaemia
iv. Myeloma – IgG has positive charge, Thus decreased AG
v. Increased Magnesium or Calcium (rarely)
vi. Artificially elevated Chlorides
vii. Hyperlipidaemia (questionable)
e. Management
i. High anion gap
a. Treat the underlying cause
b. No indication for Bicarbonate
ii. Normal anion gap
b. Treat underlying cause
c. Replace Bicarbonate serum level and losses
1. Approx. deficit = (24 – [HCO3]) X (Body Wt. X 0.6 ) mmol / l
2. For example, for a 70 patient with a [HCO3] = 4 mmol /l deficit = (24-
4) X (70 X 0.6 ) = 840 mmol (= ml of standard Bicarbonate solution)
replace 1/3-1/2 of this amount then remeasure blood gases.
B. METABOLIC ALKALOSIS
a. Aetiology / classification
i. Common causes:
a. Diuretics
b. Vomiting
c. Post- hypercapnia for more than 48 hours
d. Any fluid loss replaced with insufficient Sodium H+ excretion (contraction
alkalosis)
e. Commonly associated with hypovolaemia and /or hypokalaemia however,
actual causation by these is debated.
ii. Increased proton losses: acid loss is either renal or GIT
a. Renal
1. Raised sodium reabsorption (hypovolaemia, dehydration, etc)
2. Cushing’s syndrome, exogenous steroids
3. Hyperaldosteronism Primary / Secondary
4. Batter’s syndrome (JGA hyperplasia)
5. Liddle’s syndrome
6. Hypercalcemia / Hypomagnesaemia NDI
Intensive Care Manual Controlled Copy Quality Department 114
7. Drugs: steroids, diuretics, Carbenoxolone
b. GIT
1. N/G suctioning, protracted vomiting
2. Diarrhea
iii. Increased bases
a. Administration of Sodium Bicarbonate
b. Metabolism of exogenous acid anions – Citrate, Lactate, Acetate
c. Milk / alkali syndrome
d. Renal conservation of Bicarbonate (Acidosis, Hypercarbia)
iv. Factors tending to maintain an alkalosis
a. Hypovolaemia
b. Hypokalaemia
c. Hypochloraemia
d. Hypomagnesaemia
e. Chronic hypercapnia
f. Mild chronic Renal failure
b. Management
i. Correct hypovolaemia a functional ECF volume is essential for the correction of
alkalosis
ii. Inotropic support of cardiac output and GFR
iii. Correct decreased Potassium, Magnesium, Phosphate
i. Consider Acetazolamide if the alkalosis is persistent: provided the above
are corrected
C. RESPIRATORY ACIDOSIS
a. Etiology
i. Any cause of hypoventilation leading to respiratory failure
ii. May be acute or chronic in nature
b. Management
i. Restore ventilation
ii. No indication for Bicarbonate
D. Respiratory alkalosis
a. Etiology
i. Any cause of hyperventilation in ICU
ii. Early hypoxia
iii. Anxiety, hysteria
iv. Prescribed hyperventilation (rarely indicated)
v. Neurogenic hyperventilation
b. Management
i. Treat underlying cause
ii. Neurogenic hyperventilation is a marker of severity of head injury
Intensive Care Manual Controlled Copy Quality Department 115
10. SPECIAL CONSIDERATIONS
A. SEVERE GASTROINTESTINAL HEMORRHAGE
a. General Management Principles
Medications for ulcer treatment and prophylaxis have reduced the incidence of stress
gastritis and severe upper gastrointestinal (GI) bleeding. However, when present, such
bleeding can be life-threatening and requires early surgical consultation. The distinction
between upper and lower GI sources is important in determining the appropriate
diagnostic/therapeutic approach. The ligament of Treitz is the anatomic landmark that
separates the upper from the lower GI tract when discussing hemorrhage.
Typically, patients with life-threatening GI hemorrhage are older and have other chronic
organ system disease(s). Therefore, the critical consequences of GI hemorrhage,
hypotension and anemia, may be poorly tolerated and may lead to other systemic
manifestations of poor oxygen delivery, such as myocardial ischemia. Prompt
resuscitation and early diagnosis (even during resuscitation) are needed to prevent
these secondary consequences.
The AmericanCollege of Surgeons identifies four categories of acute blood loss based on
the percent loss of blood volume.
Class I. Loss of 15% or less of the total blood volume. This degree of blood loss is usually
fully compensated by transcapillary refill. Because blood volume is
maintained, clinical findings are minimal or absent.
Class II. Loss of 15 to 30% of the blood volume. The clinical findings at this stage may
include orthostatic changes in heart rate and blood pressure. However, these clinical
findings are inconsistent. Sympathetic vasoconstriction maintains blood pressure and
perfusion of vital organs, but urine output can fall to 20 or 30
mL/hr, and splanchnic flow may also be compromise.
Splanchnic hypoperfusion is a particular concern because it can lead to breakdown of
the intestinal barrier and translocation of microbes and inflammatory cytokines, setting
the stage for systemic inflammation and multiple organ failure.
Class III. Loss of 30 to 40% of the blood volume. This marks the onset of
decompensated hypovolemic shock, where the vasoconstrictor response to
hemorrhage is no longer able to sustain blood pressure and organ perfusion. The
clinical consequences include hypotension and reduced urine output (usually 5 to 15
mL/hr).
Systemic vasoconstriction may be attenuated or lost at this stage, resulting in
exaggerated hypotension.
Class IV. Loss of more than 40% of blood volume. Hypotension and oliguria are
Intensive Care Manual Controlled Copy Quality Department 116
profound at this stage (urine output may be <5 mL/hr), and these changes may be
irreversible.
Steps in rapid assessment and acute intervention include the following:
1. Verify the patient with active hematemesis has airway protective reflexes to
maintain adequate ventilation and oxygenation. This will be critical if endoscopy is
anticipated and sedation for the procedure will be used. Endotracheal intubation
may be advisable if the patient’s level of consciousness is altered, if copious or
frequent emesis is occurring, or for protection of the airway during endoscopy.
2. Obtain intravenous access by means of a large-bore peripheral catheter (preferably)
or a large central venous line. Frequently, more than one intravenous access is
needed to match the volume of resuscitation fluid to hemorrhagic losses. Isotonic
fluids (lactated Ringer’s solution or normal saline) and blood products are the
resuscitation fluids of choice.
3. Monitor availability of blood products on the basis of frequent assessment of visible
blood loss, vital signs, hemoglobin/hematocrit, and laboratory tests for coagulation
(PT, PTT, INR, platelets, fibrinogen). A hemoglobin level of 9 to 10 g/dL (90 to 100
g/L) should be maintained and coagulopathies corrected. If a reserve (e.g., 4 units
PRBC) of blood products cannot be immediately available, early patient transfer
should be planned.
4. Institute appropriate monitoring of systemic oxygenation (pulse oximetry), blood
pressure, and, if needed, central venous (or pulmonary artery occlusion) pressure.
The presence of orthostatic changes in blood pressure, tachycardia, altered level of
consciousness, and decreased urine output all suggest that significant blood loss has
already occurred.
5. Plan for rapid diagnostic evaluation, potential surgical intervention, or transfer of
the patient.
Maintain 1) Platelet count > 1lakh/mm3
2) Fibrinogen >200mg/dl
3) Normalize PT,PTT,INR
b. Severe Upper Gastrointestinal Hemorrhage
Severe upper GI hemorrhage is diagnosed by hematemesis or the presence of blood in
the gastric aspirate, although 10% to 15% of patients with duodenal ulcer may have
little or no blood in the gastric aspirate. When obtaining the patient’s history and
physical examination, special attention should be given to a history of previous upper GI
bleeding, previous ulcer disease, alcohol consumption, stigmata of cirrhosis, coagulation
disorders, and use of aspirin, nonsteroidal anti-inflammatory drugs, or anticoagulants.
Common causes of upper GI hemorrhage include duodenal ulcer, gastric ulcer,
esophageal varices, Mallory-Weiss tear, and gastritis.
For Pediatric Patients
Intensive Care Manual Controlled Copy Quality Department 117
Serous upper GI hemorrhage is unusual in children. Many of the causes,
including esophageal varices, are similar to the causes of upper GI hemorrhage
in adults.
Endoscopy is needed to establish the diagnosis, and endoscopic therapy may control
hemorrhage and reduce rebleeding. If endoscopy is available, cleansing of the stomach
will likely be needed. Placement of a naso or orogastric tube will be needed to perform
gastric lavage and remove clots. If endoscopy is not quickly available, consider transfer
to a facility with endoscopic capabilities.
Intravenous vasopressin or octreotide therapy may be considered when uncontrolled
variceal bleeding is suspected and endoscopy is not available. Terlipressin is the agent of
choice(dose 2mg 6th hourly) as it is almost equal to sclerotherapy, Octreotide can be
used. Maintenance infusions of 25 to 50 µg/hr continued for 48 to 72 hours may be
effective in stopping acute variceal bleeding as well as early rebleeding from varices.
c. Severe Lower Gastrointestinal Hemorrhage
Frequent causes of lower GI hemorrhage are diverticular disease, carcinoma of the
colon, inflammatory bowel disease, colonic polyps, and vascular ectasia. Evaluation
should include a thorough history and physical examination with special attention to a
history of diverticular disease, inflammatory bowel disease, previous abdominal aortic
aneurysm repair (may suggest life-threatening aortic-enteric fistula), or the presence of
a coagulation disorder. Physical examination must include inspection and a careful
rectal examination to identify hemorrhoids or rectal carcinoma. On occasion, upper GI
hemorrhage may mimic lower GI hemorrhage when associated with rapid bowel transit
of blood.
Gastric aspiration or upper GI endoscopy should be performed to eliminate an upper GI
source of hemorrhage.. Lower GI endoscopy is important for diagnosis, therapy,
anticipating rebleeding, and planning other diagnostic interventions or surgery. If
endoscopy is unavailable, transfer of the patient or direct surgical intervention will be
dictated by the patient’s condition. Angiography with embolization therapy may be
considered for unstable patients or those who are poor surgical risks. Causes of lower GI
bleeding in pediatric patients are shown in Table.
For Pediatric Patients
Causes of lower gastrointestinal bleeding in pediatric patients
1 month to 1 year Meckel’s diverticulum
1 to 2 years Intussusception
2 to 12 years Polyps, child abuse, inflammatory bowel
disease
Intensive Care Manual Controlled Copy Quality Department 118
d. Continuing Care
If the hemorrhage is controlled initially, continuing vigilance is required to detect
rebleeding. Careful monitoring of physiologic variables, laboratory parameters, and
external signs of blood loss are required in an environment where adequate, trained
staff and blood bank resources are immediately available.
B. PULMONARY EMBOLISM
a. Diagnosis
The patient’s history and clinical findings are unreliable for diagnosis of a pulmonary
embolus (PE). Risk factors for pulmonary embolism are shown in table and often
contribute to a high index of suspicion for PE.
Risk factors for pulmonary embolism
Heart failure Surgery
Advanced age Immobility, paralysis
Trauma Previous pulmonary embolism or deep
Obesity venous thrombosis
Estrogens, pregnancy Hypercoagulable disorders
Malignancy
For Pediatric Patients
PE does occur in critically ill children, but is diagnosed much less commonly
than in adults. PE may go unrecognized in critically ill patients. PE is most
commonly recognized in obese adolescents immobilized for long periods.
The classically described combination of dyspnea, pleuritic chest pain, and hemoptysis
occurs in a minority of patients with PE. Routine blood studies are nondiagnostic. Chest
radiographs frequently are unremarkable but may show nonspecific findings of
atelectasis, pleural effusion, and infiltrates. The ECG usually shows nonspecific ST-T
wave changes, and a pattern of acute cor- pulmonale is present infrequently. Sinus
tachycardia and premature atrial contractions are the most frequently encountered
arrhythmias. The most significant information provided by the ECG is often the exclusion
of other potential sources of chest pain, such as acute ischemia or pericarditis.
Hypoxemia, a nonspecific finding in cardiopulmonary disease, is commonly present, but
a normal PaO2 value or normal alveolar-arterial oxygen tension difference does not rule
out PE. Signs and symptoms of PE are shown in table.
Intensive Care Manual Controlled Copy Quality Department 119
Clinical manifestations of pulmonary embolism
Cough
Dyspnea
Tachypnea Hemoptysis
Tachycardia Fever (usually low-grade)
Chest pain
The following are key points to the approach to pulmonary embolism in the emergency
department:
1. We should consider PE in any patient with unexplained dyspnea, tachypnea, or chest
pain.
2. All patients suspected of PE must be risk stratified, ideally by using a clinical decision
rule.
3. If the D-dimer is negative, PE may be excluded in the low- and moderate-risk groups.
5. CT angiogram is the imaging study of choice for the patients.
6. V/Q scans should be used only when CT isnot available or the patient has a
contraindication to CT scans or intravenouscontrast.
7. Bedside echocardiography or hemodynamicstatus of the patient and CT angiogram
areused diagnostically for suspected massivePE. If PE is confirmed, hypotensive
patientsshould be given thrombolysis. For hypotensive patients with high clinical
suspicion of PE,thrombolytics can be considered.
8. Unfractionated heparin and low molecular weight heparin are both treatment options
for patients with confirmed pulmonary embolism.
Intensive Care Manual Controlled Copy Quality Department 120
9. A positive lower extremity study (e.g., compression ultrasound, contrast fogram,
impedance plethysmography, or radionuclide venogram) indicates the need for
treatment, since the treatment for deep venous thrombosis is the same as that for PE.
b. Therapy
Treatment usually can be limited to anticoagulation. Low-molecular-weight heparins
(dalteparin, enoxaparin, nadroparin, tinzaparin) can also be used to effectively treat PE
and offer the benefit of convenient dosing. In patients with suspected PE and no
contraindications to anticoagulation, baseline activated partial thromboplastin time
(APTT), prothrombin time (PT), and complete blood count should be obtained and
heparin therapy initiated while diagnostic tests are being obtained. Contraindications to
heparin therapy include recent major trauma with hemorrhage, recent central nervous
system (CNS) hemorrhage or infarction, active GI bleed, and clinically significant
heparin-induced thrombocytopaenia. The APPT should be monitored when using
unfractionated heparin to heparin to achieve a value 1.5 to 2.0 times the mean normal
value. Heparin therapy can be discontinued after 5 to 6 days if the INR with warfarin has
been therapeutic for 2 days. Oral warfarin therapy is started on day 1 and adjusted to
achieve and INR 2.0 to 3.0. Oral anticoagulation should continue for at least 3 months.
A massive pulmonary embolus to be treated with thrombolysis if the patient is in shock
or not in shock. The use of thrombolytic agents in the treatment of PE should be highly
individualized, and clinicians should have some latitude in using these agents. In general,
patients with hemodynamic instability who are at low risk to bleed are the best
candidates for thrombolytic therapy. Tissue plasminogen activator (t-PA) is preferred at
a dose of 100 mg infused over a 2-hour period, but none of the thrombolytics has been
shown to improve mortality in this extreme situation. Surgical embolectomy or
extraction or fragmentation of the embolus by transvenous catheters if thrombolysis is
contraindicated and it requires specialized expertise not commonly available, and is
associated with mortality is high.
An inferior vena cava filter should be considered to prevent further emboli when
there is a strong contraindication to anticoagulation
emboli recur during anticoagulation
bleeding occurs during anticoagulation
c. Clinical Issues
For the patient with manifestations consistent with hypoxemia (e.g., Tachycardia,
hypotension, anxiety, agitation), always consider performing an arterial blood gas
measurement to validate the oxyhemoglobin saturation measurement.
C. AORTIC DISSECTION
a. Clinical Presentation
Intensive Care Manual Controlled Copy Quality Department 121
Aortic dissection typically occurs after trauma or in hypertensive patients in their fifth
and sixth decades of life, but can occur in young adults with Marfan’s or Ehlers-Danlos
syndrome. Symptoms are often severe and usually include unrelenting chest pain,
frequently associated with back or epigastric pain. A patient with moderate to severe
hypertension, severe chest pain, and an enlarged mediastinum on chest radiograph has
an aortic dissection until proven otherwise. Involvement of major branches of the aorta
can lead to coma, hemiplegia, extremity ischemia, spinal cord infarction, or paraplegia.
Aortic dissection is frequently misdiagnosed as acute myocardial infarction, PE, stroke,
esophagitis, pancreatitis, peptic ulcer disease, biliary colic, and ureteral colic.
New-onset limb ischemia or aortic valve insufficiency may also suggest aortic dissection.
Physical examination should therefore include careful auscultation for a new murmur of
aortic insufficiency, assessment for asymmetric blood pressure or pulses in upper
extremities, and careful palpation of pulses in all extremities for significant asymmetry.
The diagnostic standard is angiography, if available. Computed tomography scanning
with rapid-sequence contrast and transesophageal echocardiography may also be used
for diagnosis.
b. Management
Control of blood pressure and heart rate is critical. As immediate surgical consultation is
obtained or plans are initiated for transfer, treatment with parenteral antihypertensive
agents should be initiated. Intravenous sodium nitroprusside or intravenous labetalol is
the treatment of choice. Intravenous esmolol is an alternative. If sodium nitroprusside is
necessary to lower blood pressure, concomitant β-blockade is required to reduce the
rate of rise (dp/dt), or shear force, of the blood pressure, and intra-arterial pressure
monitoring is usually necessary. The clinical goals are to relieve pain and to lower the
systolic pressure to 100 to 120 mm Hg, but to maintain a mean arterial pressure of 60 to
70 mm Hg. Medical management is always a temporizing measure until complete
diagnostic studies and surgical evaluation have been finalized.
iv. Temperature-related illness
a. Heat Stroke
Heat stroke is the most common cause of life-threatening hyperthermia. In addition to
environmental heat and humidity, predisposing factors include cardiovascular disease,
strenuous exertion, obesity, skin or sweat gland abnormalities, and drugs (e.g., alcohol,
anticholinergics, sympathomimetics, β-adrenergic blockers) that limit the patient’s
ability to dissipate body heat. The patient’s core temperature is usually > 40˚C (>104˚F).
Additional clinical manifestations in heat stroke include major CNS dysfunction
(Confusion, seizures, comma), tachypnea, and tachycardia. Hypotension is common, and
sweating may be absent or present.
Intensive Care Manual Controlled Copy Quality Department 122
Treatment of heat stroke is directed toward replacement of intravascular volume,
immediate reduction of the core body temperature, and reversal or prevention of
complications. Resuscitation measures should be instituted as outlined below.
Protect the airway
Supply oxygen
Administer intravenous fluids; the type and amount depend on assessment
of electrolytes, volume status, and vital signs. Hypo- or hyperkalemia,
hypernatremia, hypocalcemia, and hypophosphatemia may occur.
Cool the patient immediately (monitor with a rectal or esophageal thermistor
capable of recording high temperatures).
Evaporative cooling by misting the unclothed patient with tepid (not cold) water and
circulating air with a fan is easy to institute in most environments. An ice water bath is
another option for cooling, but this method may induce shivering and vasoconstriction,
thus generating more body heat and slowing its dissipation. Alternatively, application of
ice packs or ice water soaks to the maxillae and groin can be used. Antipyretics are
ineffective.
b. Hypothermia
Hypothermia is usually due to exposure or immersion and is defined as < 35˚ C (<95˚F)
core temperature. Predisposing factors include extremes of age, trauma,
erythrodermas, and drugs such as alcohol, barbiturates, phenothiazines, and
benzodiazepines. Clinical manifestations vary with the decrease in core temperature.
Neurologic changes range from impaired judgement to coma. Muscle tone is increased,
and shivering may be present at core temperatures from 30˚ to 32˚ (86˚ to 89.6˚F).
Cardiorespiratory findings include arrhythmias (including ventricular fibrillation),
hypotension, and hypoventilation. Osborn or J waves may be seen on the ECG.
Resuscitation measures should be instituted as follows and should be continued until
rewarming occurs.
Protect the airway
Institute cardiopulmonary resuscitation for a prolonged time in case of
cardiac arrest and warm up more than 95˚F.
Remove wet clothes and apply blankets
Avoid excessive patient manipulation or stimulation that may precipitate
arrhythmias. Special care is needed when inserting central venous catheters
in the chest so that the wire or catheter does not enter the heart.
Administer warm, intravenous fluids (D5 normal saline). The patient is often
hypovolemic because of a cold diuresis.
Insert rectal or esophageal temperature probe capable of recording low
temperatures.
Intensive Care Manual Controlled Copy Quality Department 123
Initiate rewarming.
Coagulopathy, bleeding, arrthmias are most common.
The choice of a rewarming technique depends on the patient’s temperature and
response to simple measures. Passive external rewarming blankets or insulting material,
as well as active external rewarming with heating blankets, is useful in mild hypothermia
(32˚ to 35˚C[89.6 to 95˚F]) and as an adjunct in more severe hypothermia. Active
rewarming should be considered for patients with a core temperature < 32˚ (<89.6˚F)
and/or life-threatening hemodynamic instability. Active, external rewarming with warm
water immersion, heat lamps, convective heaters to increase room temperature, or
forced air blankets or warming devices may be considered in moderate hypothermia
(30˚ to32˚ [86˚to 89.6˚F]) when advanced facilities are unavailable. Active core
rewarming is preferred in severe hypothermia (<28˚ C [82.4˚F]), loss of cardiac activity,
or failure to elevate temperature by 1˚ to 2˚ C (1.8˚ to3.6˚F) per hour with other
methods. Intubation and inhalation of heated, humidified oxygen is effective and is
readily available. Irrigation of the stomach and /or bladder with warm isotonic fluids is
only marginally effective and may distract from more effective therapy. Consultation
should be considered to institute peritoneal lavage, pleural lavage, warming via a
hemodialysis machine or cardiopulmonary bypass in the most unstable patients. The
intramuscular and subcutaneous routes of medication administration should be
avoided, as absorption is erratic.
With extreme hypothermia, the blood pressure and pulse may be very difficult to
record. ECG monitoring and careful attention for other signs of life (e.g., movement,
respirations) may demonstrate a stable physiology in such a patient with a profound
reduction in oxygen consumption. Vasoactive drugs should be used cautiously because
of their arrhythmogenic potential. If cardiopulmonary resuscitation is required, recall:
Defibrillation may be ineffective until core temperature is above 28˚ to 30˚ C
(82.4˚ to 86˚F).
Adrenergic drugs, likewise, may be ineffective below 30˚C(86˚F).
Full resuscitative efforts should generally be continued until the core
temperature is > 30˚ to 32˚C (86˚ to 90˚F).
The decision to terminate resuscitation is individualized on the basis of the
circumstances causing the hypothermia and other factors.
11. CRITICAL CARE IN PREGNANCY
i. Introduction
The pregnant woman can present for critical care support in two major ways. First, some
disease states are unique to pregnancy, such as eclampsia and the hemolysis-elevated liver
enzymes-low platelet count (HELLP) syndrome, and require significant immediate therapy.
Intensive Care Manual Controlled Copy Quality Department 124
Second, other critical illness not unique to pregnancy, such as thromboembolic disease,
cardiac disease, and trauma, can be precipitated or aggravated by pregnancy and may have
different manifestations during pregnancy or require alterations in planned treatment.
ii. Physiologic alterations (core)
a. Cardiovascular
Blood volume increases in each trimester during pregnancy. Cardiac output increase
30% to 50% during normal pregnancy, with most of the increase occurring during the
first trimester. Cardiac output increases as a result of increased stroke volume during
the first and second trimesters and by an increase in heart rate during the third
trimester. A significant decrease (25% to 30%) in cardiac output may occur in the third
trimester if the patient is placed in the supine position, owing to compression of the
aorta and inferior vena cava by the gravid uterus, increasing afterload and restricting
venous return to the heart. Filling pressures (central venous and pulmonary artery
pressures) typically do not change during pregnancy. Despite increases in cardiac
output, blood pressure (BP) decreases during a normal pregnancy (BP is lowest during
the second trimester) as a result of diminished systemic vascular resistance (SVR)
secondary to the vasodilating effects of progesterone. Peak reduction in BP occurs at 24
weeks; systolic pressures are reduced by 5 to 10mm Hg and diastolic pressures by 10 to
15 mm Hg. It is abnormal for blood pressure during pregnancy to exceed nonpregnant
values.
b. Pulmonary
Pulmonary changes in pregnancy include an increase in tidal volume of approximately
40% and a decrease in functional residual capacity (FRC) by 25%. The reduction in FRC
predisposes the patient to atelectasis if critical illness develops. The combination of
decreased FRC and increased oxygen consumption during pregnancy diminishes the
oxygen reserves of the mother and subsequently increases the hypoxic risk to the fetus
in response to maternal hypoventilation or apnea. Oxygen requirements increase by
approximately 30 to 40 mL/min in pregnancy and are met by an increase in minute
ventilation, primarily as a result of increased tidal volume. The increase in minute
ventilation results in a mild compensated respiratory alkalosis with a decline in the
PaCO2to ~30 torr (4.0 kPa). The pH does not change secondary to renal compensation
that results in a decrease in the serum bicarbonate concentration.
c. Gastrointestinal
Hormonal and anatomic changes in pregnancy affect the gastrointestinal tract. A
reduction in lower esophageal sphincter pressure and a resulting increase in
gastroesophageal reflux contribute to an increased risk for aspiration, starting at the
Intensive Care Manual Controlled Copy Quality Department 125
end of the first trimester. Alterations in gastric motor function may cause nausea,
vomiting, and dyspepsia.
d. Hematologic
The 40% to 60% increase in plasma volume that occurs by the third trimester is
associated with an increase in red cell mass of only 25% at term. The disproportionate
rise in plasma volume results in dilutional anemia; hemoglobin concentration is ~11 g/dL
(110g/L) at 24 weeks. The white blood cell count climbs to 10,000 cells/min3 at term,
with a slight reduction in platelet count. Concentrations of all clotting factors except XI,
XIII, and antithrombin III increase in pregnancy. Fibrinogen levels may be as high as 600
mg/dL (6.0g/L) at term; levels <150 mg/dL(<1.5g/L) are considered abnormal. Although
coagulation tests and bleeding times do not change, these compositional changes result
in a hypercoagulable state that, in association with venous stasis and vein wall trauma,
elevates the risk for thromboembolism.
iii. Hypertensive disorders (Core)
a. Diagnosis
1. Preeclampsia (Pregnancy-Induced Hypertension)
The diagnosis of preeclampsia is defined by the development of hypertension with
proteinuria, with or without edema, after 20 weeks of gestation.
Preeclampsia is classified as severe if at least one of the following signs is present:
Resting BP >160mm Hg systolic or 110 mm Hg diastolic at any time, or 140
mm Hg systolic or 90 mm Hg diastolic associated with any of the
complications listed below.
Proteinuria > 5g/24 hr or 3+/4+ on urine dipstick
Oliguria <30 cc/hr for 3 consecutive hours
Systemic symptoms, including pulmonary edema, right upper quadrant pain,
impaired liver function, headache, visual changes, or thrombocytopaenia.
2. Eclampsia
Eclampsia is defined as preeclampsia with seizures. In some cases, pregnancy-
induced hypertension may present initially as eclampsia. Although seizures are the
most dramatic manifestation of preeclampsia, other Intracranial catastrophes such
as hemorrhage or stroke are more likely to cause death. Eclampsia usually occurs
after 20 weeks of gestation or within 48 hours after delivery but should be
considered in the differential diagnosis of seizures up to 14 days after delivery.
Eclampsia occurring > 48 hours postpartum is more likely to be misdiagnosed.
Intensive Care Manual Controlled Copy Quality Department 126
b. Management
1. General Guidelines
Patients with eclampsia or severe preeclampsia require hospital admission.
Administration of magnesium sulfate, control of blood pressure, and maternal/ fetal
monitoring should be initiated. Consultation with an obstetrician should be sought.
Issues such as ICU admission, management, and delivery of the fetus should be
discussed with an obstetrician or critical care physician as soon as possible.
Preventing maternal injury, ensuring maternal and fetal oxygenation, and initiating
seizure prophylaxis are important aspects of therapy. The therapy of choice is
delivery, but the maturity of the fetus must be considered. In most cases of severe
preeclampsia occurring after 32 weeks of gestation, the baby should be delivered.
Consultation with a maternal-fetal medicine specialist is recommended.
2. Seizure Prophylaxis
Magnesium sulfate (20% solution) is used in preeclampsia in an attempt to avoid
progression to eclampsia. This drug does not jeopardize the fetus and can be given
intramuscularly or intravenously. Magnesium sulfate therapy is usually initiated
when the diagnostic BP is > 100 mm Hg and signs of impending seizure, such as
visual blurring, scotomata, or hyperreflexia, or signs of severe preeclampsia are
present. Although magnesium sulfate is used prophylactically in the U.S. in patients
with preeclampsia, other physicians may use magnesium sulfate only for treatment
of eclamptic seizures. Clinical studies are under way to better define the appropriate
use of magnesium sulfate.
Administration of magnesium sulfate by the intravenous route is preferred because
serum levels are more stable and there is less material discomfort. A loading dose of
4 to 6 g in 200 to 250 cc normal saline over 10 to 15 minutes is followed by an
intravenous infusion of 1 to 2 g/hr. Magnesium levels are checked 2 to 4 hours late
and should be 2.0 to 3.5 mmol/L (4 to 7 mEq/L). Maternal respiratory rate, deep
tendon reflexes, level of consciousness, and urine output are monitored regularly.
Since magnesium is excreted renally, the infusion rate should be decreased if urine
output drops. The maintenance infusion should be decreased or withheld on the
basis of the serum creatinine level. Normal pregnant women have a creatinine level
of 0.5 to 0.9 mg/dL (40 to 80 μmol/L). The antidote for magnesium toxicity is 1 g
calcium chloride (10 mL of 10% solution) given intravenously over several minutes.
Manifestation of Serum Magnesium levels in the blood
Hyporeflexia>4 mEq/L
1st° AV Block>5 mEq/L
Complete Heart Block>10 mEq/L
Cardiac Arrest >13 mEq/L
Intensive Care Manual Controlled Copy Quality Department 127
3. Blood Pressure Control
The goal of therapy is to lower the systemic BP to a point at which maternal status is
stabilized. Although it is not necessary to lower BP to normal levels, diastolic BP
should be reduced to 90 to 100 mm Hg. In patients with extremely elevated BP, the
mean arterial pressure should be lowered gradually in increments of 10% to 15% at
one time. Antihypertensive therapy that results in precipitous drops in BP could
further comprise an already stressed fetus by shunting blood away from the
placental circulation. Drugs that are generally used are hydralazine (2.5 to 5 mg
administered as a slow intravenous push every 15 to 20 minutes for three doses)
and labetalol (20 mg intravenously initially, and titrated every 10 to 15 minutes). If
the initial 20-mg dose of labetalol is not effective, 40 mg should be given. If the 40-
mg dose does not lower the BP to the desired level, it should be followed by an 80-
mg dose. Diuretics should usually be avoided because most preeclamptic patients
have constricted plasma volume. Calcium-channel blockers have been used
extensively in preeclampsia; nifedipine (10 to 20 mg orally every 4 to 6 hours) is the
most commonly employed agent. Use of calcium-channel blockers, especially
nifedipine, is being reevaluated because of reported myocardial ischemia and
sudden death in the acute treatment of hypertension. The angiotensin-converting
enzyme (ACE) inhibitors are contraindicated in pregnancy because of associated
fetal and neonatal complications. Nitroprusside has also been used, despite reports
of cyanide toxicity in animal models. Nitroglycerin is less effective in preeclampsia
because of its primary venodilator effect.
4. Supportive Measures
Cardiogenic and noncardiogenic pulmonary edema can occur during severe
preeclampsia. Treatment includes supplemental oxygen to maintain maternal
PaO2>70(>9.3kPa) with oxygen saturations (SpO2) > 94% to prevent fetal hypoxia
and progressive acidosis. If necessary, tracheal intubation and mechanical
ventilation are instituted. Intubation should be approached cautiously in the
pregnant woman because of the increased risk of aspiration, reduced FRC,
pharyngeal edema, and increased hypoxic risk to the fetus. Usually, smaller
endotracheal tubes (6.0 or 6.5mm) are necessary. With cardiogenic pulmonary
edema, fluid restriction and diuretics are often the initial primary treatment. Since
preeclamptic and eclamptic patients are frequently depleted intravascularly,
invasive hemodynamic monitoring may be required to optimize management. This is
an especially important measure in patients who have altered pulmonary capillary
permeability.
Oliguria occurs frequently in severe preeclampsia and eclampsia. Intravenous fluid
challenges should be instituted cautiously. The empiric use of diuretics in the
absence of invasive hemodynamic monitoring to assess intravascular volume is
discouraged. Patients who do not respond to fluid challenges need further
assessment. Noninvasive techniques such as echocardiography can be used to assess
Intensive Care Manual Controlled Copy Quality Department 128
the cardiac output, central venous pressure, and ejection fraction. Repeated fluid
boluses will usually be tolerated by preeclamptic patients with a good ejection
fraction and cardiac output. Most preeclamptic women with oliguria will respond to
1 to 2 liters of crystalloid without the need for invasive monitoring. Failure of the
patient to respond to repeated fluid challenges, or the presence of cardiac failure,
should prompt consideration of intravascular hemodynamic monitoring. Vasodilator
therapy may be beneficial if intravascular volume is adequate.
5. Monitoring
For all patients, BP level should be monitored regularly. When magnesium sulfate is
used, monitoring consists of checking reflexes, respiratory rate, and periodic
magnesium levels. Invasive hemodynamic monitoring of preeclamptic patients is
infrequently required. Central venous pressure measurements are not reliable in this
patient population.
iv. HELLP syndrome (Core)
The HELLP syndrome identifies a severe, life-threatening condition in pregnancy. The
mnemonic “HELLP” stands for
Hemolysis – hemolytic microangiopathic anemia with an abnormal
peripheral smear, a total bilirubin > 1.2 mg/dL (21 μmol/L), or
serum lactate dehydrogenase (LDH) level > 600 U/L;
Elevated Liver enzymes - Aspartate aminotransferase (AST)>70U/L,
or LDH > 600 U/L; and
Low Platelet count - < 150,000/mm3
Variations of the syndrome do not necessarily include all manifestations. The HELLP
syndrome can present with a variety of nonspecific clinical signs and symptoms, including
epigastric or right upper quadrant pain, gum or nose bleeds, petechiae, malaise, nausea,
and vomiting. Most patients with HELLP syndrome present at a gestational age of 27 to 36
weeks. Postpartum presentations also occur, usually within 1 to 2 days after delivery.
Preeclampsia often precedes the HELLP syndrome, but one third of patients with HELLP
syndrome have no hypertension.
The HELLP syndrome is part of the fibrinolysis or hemolysis portion of the preeclamptic
syndrome. Thrombocytopaenia, DIC, intracerebral hemorrhage, liver rupture, renal failure,
and HELLP are the different manifestations. HELLP syndrome can sometimes be confused
with an acute fatty liver of pregnancy, thrombotic thrombocytopenic purpura, and the adult
hemolytic uremic syndrome. Laboratory tests that are helpful in differentiating these
conditions are listed in Table. HELLP syndrome is almost always an indication for urgent
delivery because of increased fetal and maternal morbidity and mortality. If possible,
management of the HELLP syndrome should occur in a tertiary care facility. Treatment
includes supportive care, intravenous magnesium sulfate, and antihypertensive therapy for
Intensive Care Manual Controlled Copy Quality Department 129
diastolic BP > 10 mm Hg. Plasmapheresis has also been performed when symptomatic
thrombocytopaenia continues after aggressive platelet replacement, but this option is
rarely used. Patients complaining of persistent, severe, or worsening epigastric or right
upper quadrant pain should be carefully examined for spontaneous rupture of the liver.
Computed tomography or MRI can be useful to diagnose intrahepatic bleeding.
Laboratory differentiation of acute fatty liver and HELLP syndrome
Test Acute Fatty liver HELLP
Fibrinogen Normal or
Glucose Normal
Ammonia Normal
v. Peripartum cardiomyopathy (Supplemental)
a. Clinical Manifestations
Peripartum cardiomyopathy is defined as congestive heart failure occurring during the
last month of pregnancy or in the first 5 months postpartum. Clinical indicators include
severe progressive dyspnea, progressive orthopnea, paroxysmal nocturnal dyspnea, or
syncope with exertion. Signs include general or chamber-specific cardiomegaly seen on
a chest radiograph, evidence of pulmonary hypertension, murmur, prominent jugular
vein distension, cyanosis, clubbing, or arrhythmia. Heart failure without identifiable
cause in a patient between the last month of pregnancy and 5 months postpartum
suggests peripartum cardiomyopathy. The course tends to be more severe in older
patients of higher parity with later onset of symptoms after delivery.
b. Management
Initial evaluation of the patient with possible peripartum cardiomyopathy includes a
chest radiograph, electrocardiogram (ECG), and echocardiogram. Therapy includes bed
rest, sodium restriction, diuretics, and possibly vasodilators. Patients who present with
fulminant pulmonary edema and cardiac decompensation often require invasive
hemodynamic monitoring for careful fluid management, intravenous inotropic support,
and afterload reduction. Useful drugs include digoxin as an inotropic agent and ACE
inhibitors for afterload reduction (ACE inhibitors are contraindicated prior to delivery). If
symptoms develop in the antepartum period, consultation between the obstetrician,
critical care physician, and anesthesiologist can guide decisions regarding early delivery.
Anticoagulation should be considered in the pregnant woman with peripartum
Intensive Care Manual Controlled Copy Quality Department 130
cardiomyopathy, enlarged cardiac chambers, and an ejection fraction < 35%, since the
increase in both systemic and pulmonary emboli is significant. Postpartum, cardiac
function returns to normal in approximately 50% of patients. The 50% of patients who
continue to have symptoms have a mean survival time of < 5 years.
vi. Thromboembolic disease
Thromboembolic disease is a significant factor in material deaths. The incidence of
thromboembolic disease in pregnancy and the immediate postpartum period is five times
the incidence in the nonpregnant woman. A higher risk occurs with increased parity,
cesarean section, operative vaginal delivery, previous deep venous thrombosis, and
increased age.
Although manifestations of pulmonary embolism in pregnant women are similar to those in
nonpregnant women, the physiologic changes of pregnancy complicate evaluation. Lower-
extremity edema, leg pain, and dyspnea are common findings in pregnancy and create a
diagnostic dilemma for the clinician. If a chest radiograph is obtained to rule out other
pulmonary problems, such as pneumonia, the fetus must be shielded. Doppler scanning of
the lower extremities can be unreliable because of venous stasis and pooling. Ventilation/
perfusion (V/Q) scanning is reliable in a pregnant woman, but angiography is often
necessary when (V/Q) scanning results are indeterminate. A spiral CT Angiogram can be
useful, especially with centrally located emboli. Heparin therapy should be initiated when
the diagnosis of pulmonary embolism is suspected and should be continued if the diagnosis
is confirmed.
The treatment of pulmonary embolism in the pregnant patient parallels that in the non-
pregnant patient, except that coumadin is relatively contraindicated in pregnancy and
absolutely contraindicated during the first trimester, when the risk of teratogenicity is
greatest. Instead, unfractionated heparin can be administered intravenously by weight-
adjusted dose regimen to achieve an activated partial thromboplastin time (aPTT) of 1.5 to
2.5 times control. After at least 5 days of intravenous heparin, treatment can be converted
to subcutaneous administration, starting at 5000 IU of unfractionated heparin every 12
hours and aiming for the same aPTT goal measured 6 hours after administration. Indwelling
Teflon catheters (peripherally inserted central catheters) can be used during pregnancy to
facilitate heparin administration. Low molecular weight heparins (LMWH) are safe for the
fetus and can be used for the treatment of acute Xa levels must be monitored weekly.
Patients receiving heparin are at risk for heparin-induced thrombocytopaenia (the risk is
lower with LMWH) and osteoporosis. After delivery, warfarin can be substituted, for 3 to 6
months of total therapy.
Intrapartum management requires that heparin be discontinued at least 4 to 6 hours before
delivery and be resumed 6 to 24 hours after delivery. The risks with intrapartum use of
heparin include a significantly increased likelihood of hemorrhage with cesarean delivery,
and bleeding and hematomas if a regional anesthetic is used or an episiotomy or operative
vaginal delivery is performed.
Intensive Care Manual Controlled Copy Quality Department 131
vii. Severe Asthma
Asthma is the most common pulmonary condition in pregnancy. Among asthmatic patients,
50% have no change in symptoms, 30% improve, and 20% worsen. Treatment of asthma
usually does not require modification during pregnancy. Supplemental oxygen should be
administered if oxygenation is in question or a low pulse oximeters measurement is
obtained. In severe asthmatic attacks, management with inhaled β-agonists and systemic
steroids is preferred. Parenteral corticosteroids can be safely administered.
viii. Septic pelvic thrombophlebitis
Septic pelvic thrombophlebitis, characterized by infected clot(s) in the pelvic veins, occurs in
the peripartum period. Physical findings are nonspecific. Failure of fever to respond to
empiric antibiotics in a postpartum patient should prompt consideration of this condition.
Evidence of systemic septic emboli (e.g., sepsis, metastatic abscesses, septic pulmonary
emboli) may be present. Ultrasonography or computed tomography (CT) studies are not
diagnostic but can occasionally show evidence of a clot. Patients are typically treated on the
basis of clinical suspicion as a diagnosis of exclusion. Heparin, as outlined above, is used in
addition to antibiotics for management. A reduction in fever usually occurs within 24 hours.
Anticoagulation therapy is continued for 3 to 6 months postpartum.
ix. Trauma in pregnancy
Treatment priorities for the pregnant patient with traumatic injury are the same as those
for nonpregnant patients. These are, however, unique changes that should be taken into
account during clinical assessment. The gravid uterus complicates the initial abdominal
assessment of the pregnant patient. The height of the uterus is roughly at the symphysis
pubis at 12 weeks and the umbilicus at 20 weeks; then the height increases by 1 cm /wk
thereafter up to 36 to 40 weeks, when the uterus encompasses almost the entire abdomen.
Late in pregnancy, a widened symphysis pubis and widened sacroiliac joints are possible. All
pregnant patients with major traumatic injuries should be admitted to a facility with surgical
obstetric capabilities. When evaluating mental status, be aware that neurologic symptoms
of eclampsia may mimic head injury. Venocaval compression can contribute to hypotension
by restricting the return of blood to the heart. Whenever possible, the patient is placed in
the left lateral decubitus position, or, at a minimum, the right hip is raised by 4 to 8 cm to
displace the uterus off the inferior vena cava. If any question of spinal injury exists, spinal
alignment is maintained and the patient is “log-rolled.”
The pregnant patient can lose up to 35% of blood volume before significant tachycardia,
hypotension, and other signs of hypovolaemia are seen. Therefore, the fetus may actually
be in a state of hypoperfusion while the mother’s condition seems stable. An assessment of
the fetal heart rate is an essential part of the initial survey. This assessment can be
accomplished easily with a fetoscope or a Doppler fetoscope. A conventional stethoscope
can be used to auscultate the fetal heart rate in the third trimester. If available,
ultrasonography is very effective for documenting fetal cardiac activity and function.
Normal fetal heart rates are 120 to 150 beats/min. Late or persistent decelerations of the
Intensive Care Manual Controlled Copy Quality Department 132
fetal heart rate are an ominous sign. If the fetus cannot be examined adequately at the
facility, the patient should be stabilized and transported as soon as possible. A minimum of
4 hours of fetal monitoring is necessary after trauma.
Secondary assessment should evaluate uterine irritability (spasms of the uterus), fetal heart
rate, and fetal movement, and a pelvic examination should be performed, if necessary. If
there is any question of blood from the vagina, a qualified, experienced person should do a
speculum examination or, preferably, a contraindicated if placenta previa is a possibility.
Definitive care of the pregnant trauma patient includes adequate hemodynamic and
respiratory resuscitation, stabilization of the mother, continued fetal monitoring, and
radiographic studies as necessary, in addition to obstetric, critical care, and surgical
consultation. If the mother is Rh-negative, Rho (D) immune globulin (Rhogam ™) should be
given within 72 hours of injury, even when trauma is minimal. An assessment of the amount
of fetal red blood cells in the maternal circulation by means of a Kleihauer Betke stain is
advised. Obstetrical consultation for appropriate dosings if Rho (D)immune globulin is
recommended.
12. MICROBIOLOGY PROTOCOLS
1. Policy
a. The diagnosis of infection in critically ill patients is both important and difficult
b. Sepsis is the most common cause of death in critically ill patients. It shall be aggressively
sought and promptly treated with surgical drainage (where indicated) and appropriate
antibiotics.
c. Simple preventive measures are the most important factors in the containment of
hospital associated infections and development of bacterial resistance
i. Compulsory hand washing or alcohol hand rub by all staff before and after contact
with a patient
ii. Attention to aseptic technique for invasive procedures
iii. Attention to invasive procedure protocols outlined in the procedures section
iv. Avoidance of over-prescription of antibiotics and rational usage.
d. Investigation shall only be ordered on specific indications and when necessary
e. Please refer to antimicrobial guidelines for antimicrobial usage especially prophylactic
and empirical usage and for combination therapy
f. De escalate antimicrobials, as soon as possible
2. Definitions
a. Systemic Inflammatory Response Syndrome (SIRS)
i. Describes the inflammatory process that occurs in response to a variety of clinical
insults resulting in a clinical picture suggestive of “sepsis”
ii. The syndrome includes at least 2 of the following:
a. Temperature more than 38º C(Degrees C) or less than 36 Degrees C
Intensive Care Manual Controlled Copy Quality Department 133
b. Heart rate more than 90 beats per minute
c. Respiratory rate more than 20 breathes per minute, or PaCO2 less than 32
mmHg.
d. White cell count more than 12,000/cubic mm, or less than 4,000/cubic mm, or
more than 10% immature (banded) Neutrophills
iii. SIRS is non-specific and may be due to non-infectious causes:
a. Trauma
b. Haemorrhagic shock
c. Post-operatively after major surgery
d. Pancreatitis
e. Burns
f. Blood transfusion
g. Drug reactions
h. Intracranial pathology especially intraventricular blood and Thalamic Pathology
b. Sepsis: the presence of SIRS secondary to infection
c. Septic shock: decreased vital organ perfusion / function secondary to sepsis
d. Nosocomial infection is defined as infection that occurs during hospitalization that was
neither present, nor incubating on admission.
e. Colonization is defined as the presence of microorganisms that do not elicit an
inflammatory response.
3. Microbiological Investigation.
a. Routine, performed only on the clinical suspicion of sepsis
i. New pyrexia
ii. Raised TLC or marked decrease in TLC
iii. Thrombocytopenia
iv. Deteriorating gaseous exchange or pH
v. Cardiovascular instability
a. Hypotension / relative hypovolaemia
b. Increased or new inotrope requirement
vi. Oliguria or increased Creatinine
GUIDELINES FOR MICROBIOLOGY INVESTIGATIONS
a. All samples shall be collected in sterile containers
b. Never send samples for microbiology investigations in formalin
c. If delay in delivery of samples for culture and sensitivity is Unavoidable, collect or
inoculate the sample in transport media.
d. Wherever possible collect the sample before the start of antibiotics
e. The following information is necessary for microbiological investigations mention
antimicrobial therapy given, presently or in recent past.
Mention provisional diagnosis
f. The label shall indicate the identification of the specimen e.g. Name
Identification (UHID No. ), Date and Time of collection and nature of specimen
Intensive Care Manual Controlled Copy Quality Department 134
g. Containers for the samples shall be STERILE and shall not contain anything other
than the specimen asked for unless advised by the Microbiology services.
h. All samples shall be collected aseptically
i. Please not that Microbiology lab is accepts specimens round the clock
b. Screening
i. Urine (routine / microscopy and culture)
ii. Tracheal aspirate (gram stain and culture)
iii. Blood culture x sets
iv. Gram Stain and culture of appropriate drainage fluid, for example, wound aspirate,
pleural fluid etc.,
c. Other investigations, as appropriate to clinical conditions
i. Fungal cultures
ii. CSF culture and routine / microscopy
iii. Pleural tap for routine / microscopy and culture –aerobic, AFB, Fungal as
appropriate, ADA
iv. Sinus X-rays
v. Bronchoscopy specimens (BAL): gram’s staining, fungal smear/ KOH mount/ Z.N.
staining / Modified Z.N. staining, Silver Methanmine (PCP), aerobic culture, AFB
culture, Fungal culture, Anaerobic, as appropriate
d. Interpretation of results
i. Urine
a. UTI in a catheterized patient is defined as:
1. More than 105 bacteria/ml on positive culture of organisms, plus
2. More than 500 WBC/HPF.
b. Bacteria and white cells are a normal finding in the urine in a catheterized
patient
c. Treatment with antibiotics shall not result in clearance of colonization and is only
indicated if it is thought that the patient is systemically unwell from this source.
e. Blood cultures
i. May be contaminated by skin organisms: care shall be taken with technique:
a. Clean the skin with an alcohol or betadine swab
b. Clean the top of culture medium bottle with an alcohol swab
COLLECTION PROCEDURE
Collection is by venipuncture o peripheral veins only.
Observe universal precautions. Wear gloves before procedure
Blood is NOT to be taken from indwelling vascular catheter / cannula, until
and unless so specified.
Cleanse and disinfect top of appropriate culture bottles with alcohol swabs
after flipping off the cap.
Apply tourniquet, select vein, and palpate site, release tourniquet.
Intensive Care Manual Controlled Copy Quality Department 135
Cleanse and disinfect site with iodine / povidone – iodine (ask for any
previous history of sensitivity to Iodine / Betadine) if not possible than with
70% isopropyl alcohol and leave for 30 seconds (secs)
With circular movement, starting from center to periphery, swab an area of
diameter 5-6 cm. (I using both iodine and alcohol, allow iodine to dry (60
secs) then scrub with 70% isopropyl alcohol and leave it for 30 secs).
Apply tourniquet
Withdraw blood from previously selected vein site
Do not repalpate venipuncture site.
Change needle if second venipuncture is required.
Do not change needle prior to inoculation into culture bottles.
Inoculate Blood Culture Bottles with appropriate volume of blood as given on
the bottle label.
Clean site with 70% alcohol to remove iodine
Allow to completely dry before injecting
c. Use a sterile needle an aseptic technique during vein puncture
d. Inject blood immediately into bottle with same needle: do not touch needle
ii. Blood cultures are best taken by venipuncture, next best alternative is to take
sample from the arterial line.
iii. Skin organisms grown from a single bottle are usually considered a contaminant but
shall be interpreted in the context of the patient.
4. Investigation of pneumonia
a. Community acquired pneumonia
i. Usual organisms: Streptococcus pneumonia, H. influenza
ii. Less commonly
a. Bacterial: legionella sp., Gram-negative bacilli, Staph aureus
b. Viral: Influenza A, B, Para influenza, Adenovirus, RSV
c. Others Mycoplasma pneumoniae,
Chlamydia psittaci (birds)
Coxiella burnetti (sheep or cattle)
Mycobacteria (TB and NTM or MOTT), Chlamydia Pneumoniae
iii. Investigation
a. Haematology – High (more than 15000/mm3) or Low (less than 3000/mm3) WCC
– coagulopathy
b. Biochemistry – note Renal function and LFTs
c. CXR
d. ABGs
e. Microbiology: * prior to antibiotic treatment where possible
1. Blood cultures x 2 sets
Intensive Care Manual Controlled Copy Quality Department 136
2. Endotrachel aspirate
i. KOH Mounts and urgent gram stain
ii. Legionella culture**
iii. Respiratory viral Ag**
NB: if not intubated, then collect a nasopharyngeal aspirate for respiratory viruses**
3. Serology – Legionella**, Mycoplasma, Respiratory viruses**
4. Urine- L pneumoniae – 1 Ag
5. Pleural fluid – KOH Mount, gram staining, AFB staining, Aerobic, Fungal and
AFB C/S
b. Community acquired pneumonia – Immunosuppressed Host
i. Possible organisms
a. As above plus
1. Bacterial: Nocardia
2. Viral: CMV, HSV, Varicella Zoster
3. Fungal: Candida, Cryptococcus, Aspergillus
4. Protozoal : Pneumocystis carinii
ii. Investigations: * As per above, plus
a. Sputum or tracheal aspirate for
1. Fungal stain and culture
2. Silver methanamine stain/ DFAT for Pneumocystis. HIV patients only, all
others require BAL.
iii. Treatment prior to microbiological diagnosis: refer to antibiotic / antimicrobial
guidelines
c. Nosocomial pneumonia in ICU
i. Principles
a. Accurate diagnosis and appropriate treatment are important but difficult,
b. Incidence: 20% of all ICU patients 70% of patients with ARDS, major cause of death
in patients with ARDS
c. Clinically indistinguishable from pulmonary fibrosis, alveolar hemorrhage, atelectasis
and other causes of lung infiltrates
d. Clinical diagnosis, including use of tracheal aspirate, has poor sensitivity and
specificity
e. Appropriate antibiotics do improve outcome, empiric broad – spectrum antibiotics
are potentially harmful.
ii. Consider nosocomial pneumonia when
a. New and persistent CXR changes
b. Tachycardia, tachypnoea
c. Fever or hypothermia – temperature more than 37.5 or less than 35.5 degrees C
d. Leucocytosis or leucopenia – WCC: more than 11 or less than 4 X 109/l
e. Purulent sputum
f. Deterioration in lung function
iii. Confirmation of pulmonary infection:
Intensive Care Manual Controlled Copy Quality Department 137
a. Tracheal aspirate with quantitative culture is the most practical method of
diagnosing nosocomial pneumonia. Quantitative culture
b. Sensitivity and specificity may be comparable to bronchoalveolar lavage and
protected brush specimens in many situations.
c. Preliminary results to direct therapy may be obtained on gram stain
d. Consideration shall be given to obtaining pulmonary samples by bronchoalveolar
lavage (or open lung biopsy) for patients with
1. Persistent signs of pneumonia
2. Inadequate response to antibiotics
3. Inability to obtain adequate tracheal aspirates, or
4. To exclude non-infectious causes of respiratory failure (for example, interstitial
fibrosis or alveolar hemorrhage).
e. Maximum value that can be elicited out of BAL for diagnosis of Nosocomial
pneumonia can be only if the patient has been antibiotic free for more than 48
hours. Refer to BAL in procedure section
f. Septic screen including blood cultures shall be performed.
5. Vascular catheter sepsis
a. Refer to the invasive procedure section
b. Suspect line sepsis when
i. Evidence of systemic infection
a. New, unexplained fever
b. Unexplained increase or decrease in WCC
c. Deterioration in organ function
d. Positive blood culture by venipuncture with likely organisms (Coagulase negative
Staph, Candida)
ii. Evidence of local infection – inflammation or pus at the insertion site
iii. The following patients are more susceptible to line infections:
a. Prolonged vascular access (more than 7-10 days). The incidence of line infection
increases exponentially after 4 days.
b. Endovascular infection (SBE, prosthetic graft infection)
c. Cutaneous infection
d. Burns
e. Severe intra-abdominal infection (Pancreatitis) or deep seated infections
(empyema / abscess)
iv. In case of line sepsis with antibiotic impregnated lines (incidence of line sepsis is
around 1%), the most likely organisms include Candida sp.
c. Protocol
i. Take blood cultures from two different peripheral venous sites.
ii. Positive bottles shall be carefully labeled as to the site of sampling
a. Organisms commonly implicated in line sepsis are hose that normally colonize
the skin : Staph. Sp., C. albicans, but in the ICU settings low pathogenicity
potential gram negative organisms (Chryseobacterium, Burkholderia,
Stenotrophomonas etc) and other gram-negative bacilli can also be involved.
Intensive Care Manual Controlled Copy Quality Department 138
iii. On suspicion of line sepsis the line shall be removed
iv. The tip of the catheter shall be sent for culture. To avoid contamination of the
catheter tip with skin organisms the skin shall be cleaned thoroughly with alcohol,
allowing at least one-minute drying time, before removing the catheter.
v. Catheter related bloodstream infection is defined as infection where the same
organism is grown from the blood and from the catheter tip.
d. Treatment
i. Removal of the infected line shall usually clear the bacteraemia and result in a fall in
temperature and resolution of septic signs
ii. Antibiotics are only indicated if signs of sepsis continue after the catheter has been
removed, or the patient is a high risk patient (for example, prosthetic implants)
iii. If this occurs, more blood cultures shall be taken prior to starting antibiotics
iv. Refer to antibiotics guidelines
e. Further venous access
i. In ICU, as central access is usually required for inotropes or TPN, removal of a line
usually involves reinsertion of another
ii. if possible wait 24 hours before reinsertion
iii. Whenever possible insert a new line at a different site
iv. Guide wire exchanges are not performed unless
a. Mechanical problems in a new catheter (leaks/kink and less than 4 days old)
b. Difficult or limited central access (for example, burns) Mechanical problems in a
new catheter (leaks/kink and less than 4 days old)
c. Difficult or limited central access (for example, burns) Mechanical problems in a
new catheter (leaks/kink and less than 4 days old)
d. Difficult or limited central access (for example, burns) Mechanical problems in a
new catheter (leaks/kink and less than 4 days old)
e. Difficult or limited central access (for example, burns)
6. Bacterial Meningitis
a. Antibiotics are as per the requirement, which is case dependent. Refer to antimicrobial
guidelines
7. Fungal infections
a. General principles
i. The incidence of systemic fungal infections in Intensive Care patients has increased
in recent years.
ii. This is due to increased numbers of immunosuppressed patients admitted to ICU,
the use of broad-spectrum antibiotics and prolonged use of intravascular catheters.
iii. Fungaemia is generally used as an indication to commence antifungal therapy.
Whilst Candidaemia is associated with significant mortality, systemic infections can
occur even when blood cultures are negative.
b. Risk factors for Candidaemia and disseminated Candidiasis
Intensive Care Manual Controlled Copy Quality Department 139
i. Neutropenia
ii. Long term CVC use
iii. Candida colonization
iv. Broad spectrum antibiotics
v. Haemodialysis
vi. Immunosuppressants.
c. Antifungal prophylaxis
i. Systemic prophylaxis is not recommended for general ICU patients
ii. Solid organ transplant patients do not require prophylaxis
iii. Fluconazole prophylaxis is effective and tolerated in bone marrow transplant and
neutropenic cancer patients.
d. Indications for antifungal therapy
i. Candiduria in a high-risk defined patients (debilitating diseases, Uncontrolled
Diabetes, prolonged broad spectrum antimicrobial therapy with deteriorating
clinical status.
ii. Single positive blood culture in a high-risk patient
iii. Isolation of Candida from any sterile body site (except urine)
iv. Positive microscopy for yeast from a sterile specimen.
v. Histological evidence of yeast or Mycelia forms in tissue from high-risk patients.
vi. Fungal susceptibility testing for yeasts shall be asked for in all such cases as soon as
the results of positive fungal growth are available
f. Specific antifungal therapy
8. Protocol for patients with narcotizing soft tissue infections
a. General principles
i. This is a generic group of patients with life threatening infections involving
combinations of Mucocutaneous, facial and myofascial planes.
ii. These infections represent a medical emergency patients may present with severe
septic shock and rapidly developing multiple organ failure.
iii. In rapidly progressive infections, local signs of inflammation may underestimate the
degree of underlying tissue necrosis.
iv. These infections are usually due to one or more of the following organisms.
a. Anaerobes (Clostridium sp, Bacteroides)
b. Gram positives (Group A Streptococcus, Staphylococcus aureus)
c. Gram negative (Enteric organisms, Pseudomonas aeruginosa)
b. Management protocol
i. The hallmarks of management involve a detailed multidisciplinary approach
coordinated by the duty Intensive Care consultant and involving the following.
Intensive Care Manual Controlled Copy Quality Department 140
ii. Prompt and effective resuscitation, restoration of vital organ perfusion and control
of metabolic emergencies.
iii. Send appropriate specimens for Microbiology, before starting antimicrobials.
iv. Hit and hit hard in critical situations.
v. Prompt identification antibiotics / antimicrobials as required.
vi. De escalate as soon as possible.
vii. For usage of Restricted antimicrobials, Sr. Consultant, Microbiology / Infection
Control Team shall be notified as soon as possible.
1. Indications for hyperbaric oxygen on Microbiological grounds is – Progressive bacterial
(Clostridial )gas gangrene..
* Only where high index of suspicion or outbreak;
** Ask Microbiology if facility available at that moment.
13. APPENDIX
Collection of Microbiology specimens
Urine culture
i. The Timing of Collection
Best samples are obtained before the administration of antimicrobial therapy. If already on
antimicrobials, preferably at least 72 hrs, gap shall be there between the last dose
administered and the sample collected.
Day’s first voided samples are preferred. If it is not possible, then the patient is asked to
hold back voiding urine for as long as possible i.e., the total time between the last void and
the sample has to be maximized. Intake of large volumes of fluids shall be avoided before
the sample is obtained.
ii. Methods of collection
i. MSU (Mid Stream Urine)
Adequate periurethral washing before sampling yields a fairly good sample.
Washing with any good soap solution and water or even copious amounts of water
alone can be used.
The hands of the collector shall also be washed. The patient is instructed to sit on the
toilet seat.
ii. Methods of Collection
1. MSU (Mid-Stream Urine)
- Adequate periurethral washing before sampling yields a fairly good sample.
Intensive Care Manual Controlled Copy Quality Department 141
- Washing with any good soap solution and water or even copious amounts of water
alone can be used.
- The hands of the collector shall also be washed. The patient is instructed to sit on
the toilet seat.
Female patients
- The female patient shall sit with her knees widely separated. The labia are
separated, urethral meatus is cleansed at least 4-5 times with recommended soda
soaked gauze sponge or with plenty of water only if soap is unavailable.
- A front to back stroke (downward) is a must, discarding the gauze after each stroke.
- The urethral meatus is then rinsed with gauze sponges moistened with water in the
same manner as with soap.
- Keeping the labia separated, the patient shall void about 15-30 ml (initial void) into
the toilet seat and without any stopping of the urinary stream, the specimen (about
15-20 ml) is collected in a sterile container.
- The rest is again voided into the toilet.
Male patients
- In males, the foreskin or the prepuce has to be retracted in the uncircumcised
patient.
- The urethral meatus is adequately washed with soap and then water or with plenty
of water only I soap is not available.
- Urine sample is then taken as above.
2. Sample from Catheter (Chronic Indwelling Urethral Catheter)
Sample form such catheters usually do not reflect bladder pathogen.
The catheter tubing shall be clamped away from the sampling area, which shall be as
near to the urethral meatus as is possible (to collect freshly voided sample). The soft
rubber connecter between catheter and collecting tubing can also be utilized for this
purpose.
The site of sampling shall be prepared as for I/V line, with povidone-iodine and then
70% alcohol. The urine is collected by aspiration from the prepared site with a sterile
needle No. 26/28 and syringes, then the sample is quickly transferred to a sterile
container.
Sample shall NEVER be collected from the collection bag or by disconnecting catheter
from drainage bag or from the urine pot.
3. Heal Conduit / Urostomy Specimen
Strict aseptic precautions are required for collection of sample.
Intensive Care Manual Controlled Copy Quality Department 142
The opening shall be cleansed and specimen collected through a double lumen catheter
inserted beyond the fascial level.
Alternatively a fresh urostomy bag is used to collect sample after cleansing the opening.
4. Clean Initial Void Urine.
For diagnosing urethritis, after proper cleansing, as described above for MSU sample,
the early stream (5-10 ) ml and late stream samples from single voiding are taken into
consideration for culture. Both the samples shall be sent as separate urine cultures
indicating clearly the initial and the late stream sample on the request form/ requisition
slip and label on the container.
5. Segmented Urine Sample.
For the diagnosis of prostates, sequential specimens are collected along with prostatic
massage.
The initial 5-10 ml of voided urine, then MSU sample, followed by prostatic massage and
collection of expressed out prostatic secretion and finally post prostatic massage urine
(2-3 ml of post massage voided urine) form the samples for culture. All the samples shall
be sent as separate culture indicating clearly the initial / MSU / prostatic massage / post
prostatic massage urine on the accompanying request form/ requisition slip and label on
the container.
6. Suprapubic Aspiration
After appropriate and proper preparation of the part and with total aseptic technique,
at least 1.0 ml of urine shall be aspirated for culture of aerobes and anaerobes. Larger
volumes are required for Mycobacteria and Fungi.
The sample can be sent either in the appropriate BacTAlert and / or Anaerobic
(Pediatric) bottle and quickly sent to Microbiology Laboratory in a sterile container
especially if gram staining or other microscopy is required.
Suprapubic aspiration is recommended in
a. Diagnosis of bacteriuria in infants and small children.
b. For evaluating repeatedly doubtful counts or low count clean voided MSU.
c. When anaerobic organisms are suspected to be the causative agents.
Contraindicated in Coagulopathies
7. Sample for Mycobacteria
Intensive Care Manual Controlled Copy Quality Department 143
First voided whole early morning sample shall be collected in a sterile container
obtained from the Department of Microbiology and submitted on three consecutive
days with a separate request for each day. Both AFB staining as well as AFB culture shall
be asked for.
8. Sample for Anaerobic Bacterial Culture
Suprapubic aspiration is the recommended method.
A prior intimation and interaction with the Microbiology laboratory is necessary for such
culture.
At least 1.0 ml of urine shall be aspirated, optimally 5.0 ml to 10.0 ml. The urine shall be
sent immediately to the laboratory in the syringe in which it was aspirated. Any residual
air shall be expelled out form the syringe and preferably a rubber stopper is to be
applied. Alternatively the sample can be sent in an appropriate BacTAlert Culture Bottle.
9. Samples in Pediatric and Neonatal Age Group
Following samples are usually provided.
Invasive procedure
- Supra pubic aspirate (Recommended with strict aseptic precautions)
- In and out catheterization
Non-Invasive Methods
- Supra pubic tapping
The area is cleaned as for MSU about an hour after feed.
Baby is tapped just above the pubis with two fingers.
1 tap / second is given for 1 minute (60 taps / min)
This is followed by rest for 1 minute and the cycle repeated
MSU (if possible) as above
10. External Collection Devices.
Often used in neonates and males with urinary incontinence
Due to their proximity to skin and urethra the urine collected may be unreliable for
determining bladder bacteriuria.
Repeated growth of the same uropathogens may help in such cases if initially the
bag has been aseptically applied.
URINE SPECIMENS UNSUITABLE FOR MICROBIOLOGICAL PROCESSING
- Specimens obtained from urinals / bedpans
Intensive Care Manual Controlled Copy Quality Department 144
- Specimens mixed with stool
- Midstream Urine sample for Anaerobic Culture
- Urine collected from catheter bags directly
- Diluted specimens
- Specimens collected in leaking / broken containers
- Specimens contaminated by foreign materials like dyes, oily chemicals etc.
- Specimen left at room temperature without any preservation for more than 2 hours.
- Frozen samples.
Samples not to be encouraged
Tips of Foley’s catheters, until and unless justified
Blood culture
Blood culture bottles
Different Culture Bottles (Bactec / BacTAlert) are available for different types of organisms i.e.
For Aerobic : BACTEC PLUS + Aerobic / F
or
BacT/ ALERT FN
For Fungal : Myco / F Lytic / Mycosis
For AFB / Mycobacteria : Myco / F Lytic
Collection procedure : follow as given above
Sputum
Well and deep coughed out sputum sample is required. The sample shall be coughed out
directly into the sterile container and shall not be mixed with saliva.
Postural drainage or help from physiotherapists or respiratory consultants may be required to
stimulate coughed out sputum in cases where spontaneous output is lacking.
Supervised (under a respiratory consultant) aerosol – induced sputum may also be given in such
cases where it is not contraindicated.
It shall be immediately transported to Microbiology Department
Urethral Swab
After taking proper universal precautions, a swab is inserted 2 cm inside the urethra and
rotated gently before withdrawing back. Separate swabs are required for gram’s staining and
for culture for Gonococci. If other organisms are also being suspected it is advisable to send as
many swabs. Special media (Stuart’) is required for transportation of these swabs in case of
delay. This is available from department of Microbiology on demand.
Intensive Care Manual Controlled Copy Quality Department 145
It shall be immediately transported to Microbiology Department.
Elisa and Serological tests
About 5-10 ml of aseptically out blood collected in sterile red capped plain vacutainer tube or
equivalent plain tube without any additives is required for ELISA tests.
Fasting samples are generally not required until and unless specified so.
Samples for the following tests are drawn by Microbiology Laboratory Technical Staff after
receipt of requisition slip in the Microbiology Lab.
- Cryoglobulins
- Cold Agglutinins
All samples especially for Complement component shall be sent as quickly as they are drawn
out.
63. Annexure A&B Insuline infusion scales.
Intensive Care Manual Controlled Copy Quality Department 146
You might also like
- Icu GuidebookDocument43 pagesIcu Guidebookdrimran570100% (5)
- Critical Care - ICU Skills ChecklistDocument2 pagesCritical Care - ICU Skills ChecklistRandi Brown0% (1)
- Medical Assistant Study GuideDocument116 pagesMedical Assistant Study GuideErns Jean-baptiste100% (11)
- Post Anesthesia Care UnitDocument19 pagesPost Anesthesia Care UnitRizqidio LarisoNo ratings yet
- ICU Procedures ManualDocument64 pagesICU Procedures Manualenumula kumar100% (1)
- ICU Checklist - TEN FASTHUGSSS v3.0Document35 pagesICU Checklist - TEN FASTHUGSSS v3.0gxjjsjejdu100% (3)
- ICU/CCU Only Competencies and Johns Hopkins MHA ICU ProjectDocument107 pagesICU/CCU Only Competencies and Johns Hopkins MHA ICU Projecthery100% (2)
- CriticalCare - ICU Skills ChecklistDocument8 pagesCriticalCare - ICU Skills Checklistyash Inficare100% (2)
- PACU Monitoring Sheet - RR Record - SCT-CONDocument4 pagesPACU Monitoring Sheet - RR Record - SCT-CONFitz JaminitNo ratings yet
- PICU HandbookDocument113 pagesPICU HandbookCarkos Moreno100% (2)
- CCRN-PCCN Review RenalDocument11 pagesCCRN-PCCN Review RenalGiovanni MictilNo ratings yet
- Acute Critical Care Nursing HandoutDocument17 pagesAcute Critical Care Nursing HandoutJulie May100% (6)
- Nursing Practice Skills: Adult Intensive Care Unit PatientsDocument10 pagesNursing Practice Skills: Adult Intensive Care Unit PatientsMona Doria67% (3)
- Icu Nurse Crash CourseDocument3 pagesIcu Nurse Crash CourseSERA B.100% (2)
- Transferring, Logrolling and PositioningDocument89 pagesTransferring, Logrolling and PositioningJay Vincent MedranoNo ratings yet
- Board Review Geriatrics: Manage Depression with Increased Sertraline DoseDocument95 pagesBoard Review Geriatrics: Manage Depression with Increased Sertraline DoseCharis Paroginog100% (2)
- IcuDocument8 pagesIcuBikul Nayar100% (1)
- ICU ProtocolsDocument35 pagesICU ProtocolsJohn Reynolds100% (6)
- Icu Protocols-1Document38 pagesIcu Protocols-1M.IMRAN ANJUM100% (1)
- Icu NotesDocument47 pagesIcu NotesChryst Louise SaavedraNo ratings yet
- Critical Care Nursing Course MapDocument1 pageCritical Care Nursing Course MapMelissa David0% (1)
- Code Blue MedsDocument35 pagesCode Blue Medssbjon984924100% (1)
- Weaning From Mechanical Ventilation Using SBT PDFDocument29 pagesWeaning From Mechanical Ventilation Using SBT PDFEdgar Bravo Santibañez100% (1)
- Necrotizing Otitis 2022Document20 pagesNecrotizing Otitis 2022asmashNo ratings yet
- Cardiac PacingDocument4 pagesCardiac PacingmrygnvllNo ratings yet
- Critical CareDocument5 pagesCritical CareYousef Khalifa0% (1)
- Neuro ICU Midlevel Orientation ChecklistDocument15 pagesNeuro ICU Midlevel Orientation ChecklistShilpa PhilipNo ratings yet
- Perioperative Care For CABG PatientsDocument32 pagesPerioperative Care For CABG PatientsAya EyadNo ratings yet
- Hospital ICU Organization and TypesDocument82 pagesHospital ICU Organization and TypesPaul Shan GoNo ratings yet
- Recent Modes of Ventilation 103Document103 pagesRecent Modes of Ventilation 103medico_bhalla100% (2)
- The Intensive Care Unit MaualDocument356 pagesThe Intensive Care Unit MaualMariefel Villanueva AlejagaNo ratings yet
- Patient A KARDEX 1Document2 pagesPatient A KARDEX 1Franz Patrick Legria, CPAC - SNNo ratings yet
- Intensive Care Unit NursingDocument10 pagesIntensive Care Unit NursingCute Clothing Store0% (1)
- RN Critical Care Competency ChecklistDocument19 pagesRN Critical Care Competency ChecklistMary ElizabethNo ratings yet
- Hemodynamics For The Bedside Nurse 1CEUDocument7 pagesHemodynamics For The Bedside Nurse 1CEURN333100% (1)
- Antrim ED Handbook 2019Document238 pagesAntrim ED Handbook 2019Chris Jardine LiNo ratings yet
- ICU Procedure HandoutsDocument26 pagesICU Procedure HandoutsDadi Veen100% (2)
- Pre Op SyllabusDocument50 pagesPre Op Syllabusmunira.2707No ratings yet
- PEDIATRIC ASSESSMENT OVERVIEWDocument2 pagesPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- Assessment of An ICU PatientDocument71 pagesAssessment of An ICU PatientTito Tesfaye100% (1)
- Code Blue Presentation: CPR and Emergency ResponseDocument22 pagesCode Blue Presentation: CPR and Emergency ResponseNurhayatiNo ratings yet
- Alfred Hosp ICU-orientation-manualDocument85 pagesAlfred Hosp ICU-orientation-manualdragon66No ratings yet
- ECMO Journal ClubDocument15 pagesECMO Journal Clubjoe kayongoNo ratings yet
- Hemodynamic Management Pocket Card PDFDocument8 pagesHemodynamic Management Pocket Card PDFjenn1722No ratings yet
- Perioperative - Semester SummaryDocument67 pagesPerioperative - Semester SummaryPatricia Eleanor FranksNo ratings yet
- Medical Intensive Care UnitDocument120 pagesMedical Intensive Care Unithaaronminalang100% (6)
- Assessing Patients Preoperatively (A2 B2 C2 D2 E2 F2 G2Document40 pagesAssessing Patients Preoperatively (A2 B2 C2 D2 E2 F2 G2marina_shawkyNo ratings yet
- Intravenous Anesthetic AgentsDocument23 pagesIntravenous Anesthetic Agentsdrhiwaomer100% (7)
- Managing Cardiac Patients in the ICUDocument26 pagesManaging Cardiac Patients in the ICUvamshidh100% (2)
- Cath Lab Cardiac Cath LabDocument3 pagesCath Lab Cardiac Cath LabMaria Edel100% (2)
- PACU Discharge CriteriaDocument1 pagePACU Discharge CriteriaTarquin Tomada100% (2)
- Interpret Blood Gas Analysis & Acid-Base ImbalancesDocument3 pagesInterpret Blood Gas Analysis & Acid-Base ImbalancesChameera Bandara100% (2)
- Basic Mechanical Ventilation 2014Document62 pagesBasic Mechanical Ventilation 2014dragon66No ratings yet
- Anesthesia ManualDocument21 pagesAnesthesia ManualDocFrankNo ratings yet
- Float Pool - Orientation - RN Critical Care Competency ChecklistDocument19 pagesFloat Pool - Orientation - RN Critical Care Competency Checklistpurwadis100% (2)
- CCRN Exam Review Course: Save The Date & Request The TimeDocument1 pageCCRN Exam Review Course: Save The Date & Request The TimeHelen Hughes0% (1)
- 50 Shades of Practice QuestionsDocument11 pages50 Shades of Practice QuestionsAmie Ray100% (1)
- Emergency Care Algorithms 2023Document88 pagesEmergency Care Algorithms 2023Ali Aborges Jr.No ratings yet
- CCRN Cert Review Neuro IDocument16 pagesCCRN Cert Review Neuro IGiovanni MictilNo ratings yet
- Disaster Management Manual - ControlledDocument44 pagesDisaster Management Manual - ControlledanithaNo ratings yet
- Cop-5-Policy On Uniform Use of CPRDocument23 pagesCop-5-Policy On Uniform Use of CPRanithaNo ratings yet
- Cop-3-Policy On Ambulance ServicesDocument9 pagesCop-3-Policy On Ambulance ServicesanithaNo ratings yet
- NABH 5th Edition - COP - Emergency ServicesDocument14 pagesNABH 5th Edition - COP - Emergency ServicesanithaNo ratings yet
- Cop-5 Do Not Resuscitate-DnrDocument3 pagesCop-5 Do Not Resuscitate-DnranithaNo ratings yet
- NABH 5th Edition - COP - Emergency ServicesDocument14 pagesNABH 5th Edition - COP - Emergency ServicesanithaNo ratings yet
- Effective Governance The Roles and Responsibilities of Board MembersDocument5 pagesEffective Governance The Roles and Responsibilities of Board MembersanithaNo ratings yet
- Training schedule-AQCA-2022Document1 pageTraining schedule-AQCA-2022anithaNo ratings yet
- Joint Preservation Hip & Ankle ArthroscopiesDocument1 pageJoint Preservation Hip & Ankle ArthroscopiesanithaNo ratings yet
- Patient Engagement and Safety - PSNetDocument5 pagesPatient Engagement and Safety - PSNetanithaNo ratings yet
- Culture of Safety - PSNetDocument4 pagesCulture of Safety - PSNetanithaNo ratings yet
- Aha Guidelinedriven Management of Hypertension An Evidencebased UpdateDocument56 pagesAha Guidelinedriven Management of Hypertension An Evidencebased UpdateNanda Gopal Reddy AnamNo ratings yet
- Pi Is 0828282 X 19315508Document16 pagesPi Is 0828282 X 19315508Mitch TobinNo ratings yet
- Postural HypotensionDocument3 pagesPostural HypotensionSimran JosanNo ratings yet
- Management of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiDocument9 pagesManagement of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiSatya AsatyaNo ratings yet
- PharmacologyDocument236 pagesPharmacologyyalahopa100% (2)
- Updates On The Diagnosis and Treatment of Peripheral Autonomic NeuropathiesDocument16 pagesUpdates On The Diagnosis and Treatment of Peripheral Autonomic Neuropathiesdeepam kapoorNo ratings yet
- Mobility and ImmobilityDocument37 pagesMobility and ImmobilityAndrea Huecas Tria100% (2)
- Is This Patient HypovolemicDocument8 pagesIs This Patient HypovolemicNicholasNo ratings yet
- Viva in Oral Surgery For Dental Students - Jaypee Brothers (2012) PDFDocument147 pagesViva in Oral Surgery For Dental Students - Jaypee Brothers (2012) PDFIsak Isak Isak0% (1)
- Management of Orthostatic Hypotension.12-1Document24 pagesManagement of Orthostatic Hypotension.12-1Cristina GhizdavetNo ratings yet
- Amedex 2023 - PagenoDocument1,943 pagesAmedex 2023 - PagenosajihanNo ratings yet
- Doctor's Order Levodopa +carbidopa 250mg/25mg 1 Tab BIDDocument25 pagesDoctor's Order Levodopa +carbidopa 250mg/25mg 1 Tab BIDspain michaelisNo ratings yet
- ECG ProjectDocument58 pagesECG Projectد. سعد قاسم الاجهزة الطبيةNo ratings yet
- CHARTING SYSTEMS GUIDEDocument4 pagesCHARTING SYSTEMS GUIDELydia D. GalinganNo ratings yet
- Cardiovascular Autonomic Dysfunction in Parkinson's DiseaseDocument7 pagesCardiovascular Autonomic Dysfunction in Parkinson's DiseaseCocosul Cocosului CocosaruluiNo ratings yet
- Tool5 Multifactorial Falls Risk AssessmentDocument7 pagesTool5 Multifactorial Falls Risk AssessmentHenry Philip Sabado PrestoNo ratings yet
- Clinmed 21 3 E275Document8 pagesClinmed 21 3 E275Carlos CoronaNo ratings yet
- Syncope ShockDocument39 pagesSyncope ShockBunga Erlita RosaliaNo ratings yet
- Makalah Bahasa Inggris I1Document22 pagesMakalah Bahasa Inggris I1faridaNo ratings yet
- Orthostatic Hypotension Medical StudentsDocument21 pagesOrthostatic Hypotension Medical StudentsRobMarvinNo ratings yet
- Managing Fall Risk in an 84-Year-Old Asian MaleDocument4 pagesManaging Fall Risk in an 84-Year-Old Asian Malesavvy_as_98-1No ratings yet
- Geriatric Rle Prelim ReviewerDocument15 pagesGeriatric Rle Prelim ReviewerVivien IgnacioNo ratings yet
- History Taking For A Patient With SyncopeDocument4 pagesHistory Taking For A Patient With SyncopehabbouraNo ratings yet
- Effect of Exercise and Posture On Blood PressureDocument19 pagesEffect of Exercise and Posture On Blood PressureSreedeep TejaNo ratings yet
- An Essay On A House On FireDocument8 pagesAn Essay On A House On Fireezksennx100% (2)
- Ancient Acupuncture Diagnostic SkillsDocument28 pagesAncient Acupuncture Diagnostic Skillskckejaman100% (1)
- Download Clinical Neurology 10Th Edition Roger P Simon full chapterDocument67 pagesDownload Clinical Neurology 10Th Edition Roger P Simon full chapterdoug.wiggins940100% (6)