Professional Documents
Culture Documents
Estrés, Trauma y Trastornos Relacionados
Uploaded by
AlexRázuriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Estrés, Trauma y Trastornos Relacionados
Uploaded by
AlexRázuriCopyright:
Available Formats
Psychiatry Review Course The Osler Institute ©2021
Stress , Trauma & Related Lecture outlines
Disorders. ❑ Definition of Trauma
Grief ❑ Response to Trauma
❑ Risk Factors for PTSD/ASD
❑ Adjustment Disorder
Presented and updated by: Simon Ovanessian, MD ❑ Reactive attachment Disorder
Assistant professor of Psychiatry ❑ Disinhibited Social engagement Disorder
Associate Director: Walden Behavioral care, Rockville CT ❑ PTSD
❑ Acute stress Disorder/ PTSD
❑ Treatment and Prognosis
❑ Grief Work and management
❑ Case Vignette / Q& A
Trauma & Stress related Disorders Response to Trauma
Disorders in which exposure to a traumatic or stressful event is listed
explicitly as a diagnostic criteria ❑ After traumatic experience, mind & body are in shock.
❑ Reactive Attachment disorder (RAD) ❑ As one makes sense of the trauma process emotions, can come out of
❑ Disinhibited Social engagement Disorder
it , as in non complicated bereavement.
❑ With post-traumatic stress disorder (PTSD), it is believed that patients
❑ Acute stress Disorder remain in psychological shock.
❑ PTSD ❑ Memory of what happened and the feelings about it are disconnected.
❑ Adjustment Disorder ❑ In order to move on, it’s important, may be, to face and feel memories
❑ Other specified trauma and Stressor-related Disorders. and emotions, (in the right time)
❑ The brain’s normal recovery process is somehow disrupted in
⚫ The first two share the absence of adequate caregiving during complicated grief and if continues can lead to Depression or PTSD.
childhood, RAD is internalizing disorder with depressive symptom
❑ The response vary. Anxiety and fear in the form of anhedonia
and the latter is marked disinhibition with externalizing behavior. Dysphoric symptoms , in some after a catastrophic event, may
Depersonalization Experience of being an outside observer of or develop externalizing angry or aggressive symptoms or dissociative
detached from oneself (e.g., feeling as if "this is not happening to me" symptoms in others
or one were in a dream). ❑ Mutations in a gene known as NLGN1 may be associated with more
severe response
Derealization Experience of unreality, distance, or distortion (e.g.,
"things are not real").
Risk factors / Etiology Adjustment Disorder (AD)
❑ Trauma in the past or repeated trauma
❑ Younger age, woman > men, women experienced high levels of war-
❑ Is "situational" or "reactive" and does not imply a major
zone stress compared to men - 39.9 percent versus 23.5 percent
underlying brain disease.
❑ Presence of identified psychosocial & environmental problem
❑ It is diagnosed up to 50% in psychiatric consultation setting,
❑ Previous psychiatric history or suicidal attempt
and 5-20% in outpatients
❑ Shorter length of previous treatment
❑ Acute: Duration of Symptoms is less than 6 months
❑ The stressors in AD, different than in PTSD may be less traumatic or
relatively minor, like loss of a girlfriend/boyfriend, or moving. ❑ Chronic: More than 6 months, when the stress is chronic and
continuous will still be additional 6 month period diagnosis.
❑ Genetics: Panic and generalized anxiety disorders and PTSD share
60% of the same genetic variance. Alcohol, nicotine, drug ❑ The condition is different from anxiety disorder, which lacks the
dependence share greater than 40% genetic similarities presence of a stressor, or PSTD and acute stress disorder, which
Approximately 30% of the variance in PTSD is caused from genetics usually are associated with a more intense stressor
alone. For twin pairs exposed to combat in Vietnam, a monozygotic
(identical) twin with PTSD was associated with an increased risk of the
co-twin's having PTSD compared to twins that were dizygotic .
❑ African American Veterans has 2.5 time more risk ,Hispanic 3 times to
suffer from PTSD
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 1
Psychiatry Review Course The Osler Institute ©2021
Adjustment Disorder Diagnosis Treatment
A-The development of emotional and behavioral symptoms in ❑ Psychotherapy: The most trusted treatment plan for an
response to an identifiable stress(s), occurring within 3
months of the onset of the stress and improvement of adjustment disorder as the patient begins to come to terms
symptoms within 6 months after the stressor or stressors are with how the external stressor affects them. Behavioral
removed. therapy and CBT
B- These symptoms are significant enough to cause marked ❑ Self-help & Support groups: To hear others going
distress in excess of what would be expected from exposure
through similar circumstances can help depressed individual
C- Significant impairment in social and occupational
functioning come to terms with their own suffering.
D- It does not meet the criteria for any other diagnosis. It can ❑ Anxiety medication: for a short time, antidepressant to
be diagnosed in the presence of other mental disorder only if treat co morbid conditions,
not related to stress. (OCD, ADHD)
❑ Address Substance: abuse co-morbidity
E- The symptoms do not represent Bereavement
F- Once stress (or its consequences) has terminated the
symptoms disappears,
The Definition of Trauma in
Acute Stress Disorder
PTSD/ASD
❑ The same criteria for trauma as in PTSD. ( e.g. directly
❑ Exposure to actual threatened death, serious injury, or experiencing or witnessing the event, or learning that
sexual violence in one or more of the following ways:
it occurred to close relative or friend, etc.)
❑ Directly experiencing traumatic event(s)
❑ Witnessing in person, the events as it occurred to others ❑ Symptoms typically begin immediately after the trauma,
❑ Learning that traumatic event(s)occurred to a close family but persist for at least 3 days and up to a month
member or close friend in cases of death the event must ❑ Presence of 9 or more of 5 categories of 14 symptoms
have been violent or accidental
(Intrusion symptoms, Negative mood , Dissociative
❑ Experiencing repeated or extreme exposure to aversive
details of the traumatic event, e.g. first responders Symptoms. Arousal Symptoms, Avoidance symptoms).
collecting human remains. Intrusion Symptoms Include:
❑ It dose not apply to exposure through electronic media, TV
, unless this exposure is work related ❑ Recurrent, involuntary and intrusive distressing
memories of the events. In children repetitive play in
which the theme and aspects of events are expressed.
Acute stress Disorder
Acute Stress Disorder ❑ Negative mood: Persistent inability to experience positive
mood (happiness, satisfaction or loving feelings)
❑ Recurrent distressing dreams in which the content are
❑ Dissociative Symptoms: Altered sense of reality, (being in a
related to the event. In children there may be
daze or time slowing)
frightening dream without recognizing the content.
❑ Inability to remember important trauma event. (typically due
❑ Dissociative reaction (i.e. flash backs), the individual to dissociative amnesia & not due to TBI or drugs)
feels or acts as if the traumatic events were recurring, it ❑ Avoidance Symptoms: Avoid distressing memories, thoughts
may be continuous with the most extreme being or reminders (people, places, objects , situations)
complete loss of the surrounding or reenactment in
❑ Arousal Symptoms:
play in children. Dissociation during trauma (time
o Sleep disturbances,
distortion, depersonalization/derealization, out of body,
watching a movie, not feeling pain) o Irritability
o Hypervigilance
❑ Intense or prolonged psychological distress or marked
physiological reaction to in response to internal or o Problems with concentration
external cues that symbolize or resemble the event o Exaggerated Startle response
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 2
Psychiatry Review Course The Osler Institute ©2021
Acute Stress Disorder/PTSD Co-Morbidity
❑ PTSD has the same categories of symptoms with the
exception of Dissociative Symptoms but all are included not
❑ Major Depressive Disorder
only 9 of 14 as in Acute Stress Disorder. ❑ Substance Related Disorders
❑ The disturbance causes clinically significant distress or
impairment in social, occupational or other important areas ❑ Panic Disorder
of functioning. ❑ Agoraphobia
❑ The disturbance is not attributable to the effect of
substances or other medical condition (TBI) ❑ Obsessive Compulsive Disorder
❑ Acute Stress Disorder occurring weekly predicts PTSD.
❑ Generalized Anxiety Disorder
❑ PTSD can occur without ASD
❑ One month cut off arbitrary, 3-6 months is better ❑ Social Phobia
❑ During high stress, the hippocampus, which is associated ❑ Specific Phobia
with placing memories in the correct context of space and
time and memory recall, is suppressed. This suppression ❑ Bipolar Disorder
may be the cause of the flashbacks that can occur people
with PTSD. ❑ Sleep Disorder
PTSD/ Symptoms
PTSD ❑ The amygdalo centric model of PTSD proposes that the amygdala is very
much aroused and insufficiently controlled by the medial prefrontal
cortex and the hippocampus, in particular during extinction
❑ Exposure to actual or threatened death, serious injury
❑ This is consistent with an interpretation of PTSD as a syndrome of
or sexual violation. Duration of symptoms is >1 month. deficient extinction ability
(ASD if it is between 3 days -month) ❑ Exposure to trauma and definition of trauma is the same as in ASD.
❑ PTSD has two specifiers. ❑ In children, age 6 and under, experiencing repeated and extreme exposure
is not included in the diagnostic symptoms of Traumatic Event definition.
1- With dissociative symptoms: A- Must have one or more of the intrusive symptoms. (Children,
Depersonalization: feeling of detachment as though dreaming from own mind may have trauma specific reenactment in play)
and body B- Negative alteration of mood and cognition of evens associated
with the trauma as evident by 2 or more of negative symptoms or
De realization: Persistent or recurrent experiences of unreality of the inability to remember important aspects of the event, persistent or
surrounding experienced as unreal , dream like, distant or distorted exaggerated negative belief
1. Distorted cognition about the causes
2- With delayed exposure: if the full diagnostic symptoms do not develop until
6 months after the trauma. 2. Markedly diminished interest in significant activities
3. Feeling if detachment or estrangement
❑ The 3 brain areas with changed function are the prefrontal cortex, amygdala,
4. Alteration in the arousal and reactivity with traumatic events
and hippocampus. The amygdala is strongly involved in forming emotional
memories, especially fear-related memories. Neuroimaging studies in humans
have revealed aspects of PTSD morphology and function
PTSD/Symptoms PTSD/Symptoms
C- Persistent avoidance of stimuli associated with the ▪ D- Marked alterations in arousal and reactivity associated with the
traumatic event(s), beginning or worsening after the traumatic
traumatic event(s), beginning after the traumatic event(s) event(s) occurred, as evidence by two (or more) of the following:
occurred, as evidenced by one or both of the following: ▪ 1. Irritable behavior and angry outbursts (with little or no
provocation) typically expressed as verbal or physical aggression
⚫1. Avoidance of or efforts to avoid distressing memories, toward people or objects.
thoughts, or feelings about or closely associated with the ▪ 2. Reckless or self-destructive behavior.
traumatic event(s). ▪ 3. Hypervigilance.
⚫2. Avoidance of or efforts to avoid external reminders ▪ 4. Exaggerated startle response.
(people, places, conversations, activities, objects, situations) ▪ 5. Problems with concentration.
that arouse distressing memories, thoughts, or feelings about ▪ 6. Sleep disturbance (e.g., difficulty falling or staying asleep or
restless sleep).
or closely associated with the traumatic event(s). ▪ E- Duration of the disturbance (Criteria B, C, D, and F) is more
than 1 month.
▪ F- The disturbance causes clinically significant distress or
impairment in social, occupational, or other important areas of
functioning
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 3
Psychiatry Review Course The Osler Institute ©2021
PTSD/SYMPTOMS Rapid Eye movement Sleep
❑ Clingy or labile attachments (relationships) Behavior Disorder
❑ Dissociative symptoms in PTSD (are in ASD criteria)
❑ Primitive and immature defenses including splitting, denial,
devaluation/idealization, regression ❑ Repeated episodes of arousal during sleep with vocalization
❑ Unclear if psychosis (hallucinations) can be (conceptually) a post traumatic and /or complex motor behavior
syndrome. Low levels of dopamine can contribute ❑ Upon awakening during this dream the individual is
anhedonia, apathy, impaired attention, and motor deficits. Increased levels of completely awake and not confused or disoriented.
dopamine can cause psychosis, agitation, and restlessness
❑ More frequent during the later portion of the sleep
❑ Brain catecholamine levels are high, and corticotropin-releasing factor (CRF)
concentrations are high, suggesting an abnormality in the hypothalamic- ❑ During REM sleep, 90 minutes after sleep onset.
pituitary-adrenal (HPA) axis.
❑ History suggestive of either
❑ The maintenance of fear has been shown to include the HPA axis, the locus
coeruleus-noradrenergic systems, and the connections between the limbic 1. REM Sleep without atonia on polysomnographic recording
system and frontal cortex. 2. History suggestive of REM Sleep behavior disorder or
❑ Because cortisol is normally important in restoring homeostasis after the Synucleinopathy (i.e. Parkinsonism, multiple system atrophy)
stress response, it is thought that trauma survivors with low cortisol
experience a poorly contained - that is, longer and more distressing -
response, setting the stage for PTSD
Treatment Treatment
❑ Eye Movement Desensitization & Reprocessing ❑ CBT
(EMDR): The goal is to process distressing memories, ❑ Support Group
reducing their long lasting effects and allowing the ❑ Psychodynamic psychotherapy: Focuses on numerous factors
that may influence or cause a person's symptoms, such as
person to develop more adaptive coping mechanisms. early childhood experiences, current relationships and the
This is done in an eight-phase approach that includes things people do to protect themselves from upsetting
thoughts and feelings.
having the person recall distressing images while
❑ The synthetic cannabinoid nabilone is sometimes used off-
receiving one of several types of bilateral sensory input, label for nightmares in PTSD. Although some short-term
including side to side eye movements (developed by benefit was shown, adverse effects are common and it has
Francine Shapiro, PhD). not been adequately studied to determine efficacy
❑ Cultural Factors: Comprehensive evaluation of and treatment
❑ Virtual Exposure Therapy: is considered to be a should include assessment of these factors
behavioral treatment for PTSD. It targets behaviors ❑ NIMH-funded trial in New York City compared interpersonal
that people engage in (most often the avoidance). psychotherapy, prolonged exposure therapy and relaxation
therapy - were all equally effective
Medication Stages of Grief (Loss)
.
❑ Antidepressants: Evidence provides support for a small or ❑ By Elisabeth Kubler Ross (1969)
modest improvement with sertraline, fluoxetine, paroxetine,
❑ People grieve differently . Some in 5 stages some even
and venlafaxine. Thus, these four medications are
considered to be first-line medications for PTSD. expands the stages to 7 stages
▪ They may help to treat the depressive aspects or anxiety. 1. Denial and Isolation: It is a defense mechanism that
❑ Prazosin (Minipress, generic), a drug that was developed to buffers the immediate shock.
treat high blood pressure, has been found to be useful in
managing sleep-related problems caused by trauma. It works 2. Anger: Reality and its pain re-emerge, not ready for
by blocking certain alpha-1receptors in the brain, which intense emotion is deflected, redirected and
might lead to better, deeper sleep
▪ In addition to preventing nightmares and insomnia, it can help expressed instead as anger.
improve symptoms, such as flashbacks, and irritability or 3. Bargaining: This is a weaker line of defense
anger.
▪ Treatment of hyperarousal and associated anxiety and 4. Depression
Psychotic Symptoms 5. Acceptance
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 4
Psychiatry Review Course The Osler Institute ©2021
Bereavement & Grief in DSM V Diagnosis
❑ The criteria of Depression with Bereavement is similar to Major Depressive
Disorder.
DSM V is changing to diagnosis of Major Depressive
❑ No Bereavement exclusion in DSM V
Disorder if it fulfills the criteria in two weeks.
❑ Bereavement can last 1- 2 years
DSM IV required not to make diagnosis of Depressive
❑ Bereavement can precipitate major depressive episode – Disorder within 2 months of the loss, unless
❑ Major depression in bereavement worsens clinical course – -It causes marked functional impairment
❑ Depressive symptoms with bereavement respond to same interventions as
-If includes certain conditional features
no bereavement associated depression
1. Suicide
Major Depression Grief 2. Morbid preoccupation with worthlessness
Expression of mood is despair and Loss or emptiness 3. Psychotic symptoms
hopelessness 4. Psychomotor retardation
Time course: Steady and waxing Surges and retreats The uncomplicated bereavement does not include the
Content of thoughts; unreleased of Memories and thoughts of departed conditional features of suicide, morbid preoccupation with
own misery worthlessness, psychotic symptoms, and psychomotor
Death wishes; Wishes of own death Life is still worth of living, but I think of retardation, is of shorter duration.
suicidal plans death
Uncomplicated Bereavement in
DSM V How to interview
❑ When a person grieves a loss with anxiety, depression ❑Empathy
and preoccupation with guilt. ❑Facilitation
❑ DSM V allows the diagnosis of uncomplicated
Bereavement. The following symptoms will help you ❑Validation
decide if, in addition to being bereaved, the patient is
suffering from Major Depressive Disorder ❑Support
❑Guilt feelings (other than about actions that might have ❑Explanation
prevented the death)
❑Slowed down Psychomotor activity ❑Summation
❑Death wishes (other than wishing to have died with the loved
one) ❑Silence, listen
❑Severe preoccupation with worthlessness
❑Engage
❑Severely persistent impairment in functioning for a long time
❑Hallucinations (other than seeing or hearing the dead) ❑Body Language
Case Vignette
Case Vignette
A 38 years old female had lost her father in a car accident 3
Q2-Which of the following doesn’t constitute as stressor or trauma by
weeks ago. She experiences waves of sad moods, especially definition in DSM V for PTSD or Acute Stress Disorder.
when she walks by the office where her father worked. For the
A)- Witnessing in an individual die in a tragic accident
last 2 weeks she has also felt guilty and has very low energy.
She did seek out support from a fireman she knew and who B)- Learning about your father’s death
came to the accident scene. She says it is very stressful for C)- Repeatedly exposure to human remains in a disaster area soon after it
happens
her. She experiences intrusive thoughts and flash backs that
interfere with her daily routine. In addition, she sleeps poorly, D)- Exposure to train accident in your town the night before on TV
has lost weight. –Q1-Which of the following symptoms E)- Previously (last month) being attacked by robbers at work place who
necessitate the need to start treatment for major Depressive threatened to killing her
Disorder in future? Q3-If she is diagnosed with PTSD 6 months later, what specifier in DSM V
would be used.
A)- Persistent & marked functional impairment with sad mood A)- With anxiety symptoms
and morbid preoccupation > 2 weeks. B)- With chronic onset
B)- Presence of sad mood and guilt in waves > 10 days C)- With Delayed Exposure
C)- Anxiety & flash backs and memories > 2 weeks. D)- With dissociative symptoms
D)- Presence of poor appetite and wishes to be with the E)- With Grief
deceased for a week
E)- Persistence of intrusive memories for more than two weeks.
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 5
Psychiatry Review Course The Osler Institute ©2021
Vignette Answer 1 Vignette Answers
A)-Symptoms of marked functional impairment and morbid Answer 2 D)- Espouser by TV to a plain crash. According to
preoccupation persisting for 2 weeks. DSM V, exposure through electronic media, television, movies
❑ The presence of sad mood, guilt, anxiety or flashbacks and memories are is not considered enough of a to cause PTSD or Acute Stress
all non-specific symptoms of depression and are part of what is called in Disorder, unless it is work related
DSM V as uncomplicated bereavement. Dominant affect is feelings of
emptiness and loss. Capacity for positive emotional experiences and self- Answer 3 C)- with delayed expression
esteem preserved. Fleeting thoughts of joining deceased may occur.
❑ Dysphoria in Grief tends to occur in waves and tends to be connected with
thoughts and reminders of the loss.
The ICD-10 Clinical Descriptions and Diagnostic Guidelines (3, p. 150) state that “normal
bereavement reactions, appropriate to the culture of the individual concerned and not
usually exceeding 6 months in duration” should not be coded in the chapter on mental
disorders, but in chapter XXI (“Factors influencing health status & contacts with health
services”).
-------------------------------------------------------------------------------------------------------------------------------------------------------
Reference: American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). ------------------------------------------------------------------------------------------------------------------------------------------------------
Arlington, VA: American Psychiatric Publishing. pp. 271–280. ISBN 978-0-89042-555-8.
Reference: American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Arlington, VA: American Psychiatric Publishing. pp. 271–280. ISBN 978-0-89042-555-8.
Question 1 Question 2
A 68 years old man, with no previous history of mental Which of the following sleep disorder was found to
illness, who lost his wife due to terminal illness is angry be common in Veterans with PTSD and violence?
at the doctor who diagnosed her illness. His emotion is
best explained as: A)- Narcolepsy
A)- Reaction to inner feeling of insecurity B)- Sleep epilepsy
B)- As part of anxiety and fear of his own demise C)- Less percentage of REM episodes
C)- Is one of the stages of bereavement & loss D)- REM Behavior Disorder
D)- The anger is a manifestation of late onset Bipolar disorder.
E)- Longer total time of deep sleep with
E)- It is a brief psychotic disorder due to shock.
nightmares
Answer 1 Answer 2
C)- Is one of the stages of bereavement & loss D)- REM Behavior Disorder
Normal bereavement is exclusion criteria in DSM V for This is a parasomnia characterized by the actual enactment of
diagnosis of Adjustment Disorder dream sequences during REM sleep. In addition, PTSD sleep
pattern is characterized by
❑ Higher percentage of REM sleep, more REM density, with
greater likelihood of periodic limb movement in sleep.
❑ Shortened duration of total sleep with increased awakening
time
--------------------------------------------------------------------------------------
Reference : Kübler-Ross, Elisabeth; Kessler, David (June 5, 2007). "On Grief ❑ Lower rate of co-morbid depression tends to have more
and Grieving: Finding the Meaning of Grief Through the Five Stages of Loss". PTSD sleep disturbances
Scribner. Retrieved November 27, 2016 – via Amazon.
Y}Ovanessian (8/23/2021) Trauma and Stressor Related Disorders page 6
You might also like
- Manual Emdr Parts Work Treating Complex TraumaDocument73 pagesManual Emdr Parts Work Treating Complex Traumacora4eva5699100% (1)
- Dissociative DisorderDocument44 pagesDissociative DisorderKiaraMaeRhiasNo ratings yet
- Understanding PTSDDocument22 pagesUnderstanding PTSDLucy FoskettNo ratings yet
- PTSD Diagnosis & AssessmentDocument2 pagesPTSD Diagnosis & AssessmentAlesha Rose100% (6)
- PTSD PaperDocument7 pagesPTSD PaperBeccaShanksNo ratings yet
- PTSD TreatmentDocument2 pagesPTSD TreatmentAlesha Rose100% (1)
- DSM Diagnosis of Conduct DisorderDocument12 pagesDSM Diagnosis of Conduct DisorderponchossNo ratings yet
- PTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDocument28 pagesPTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDardo Arreche100% (2)
- Psychotherapy in PTSDDocument14 pagesPsychotherapy in PTSDraquka06100% (2)
- PTSD Research PaperDocument11 pagesPTSD Research Paperapi-548851649No ratings yet
- Trauma and Stressor-Related DisordersDocument58 pagesTrauma and Stressor-Related DisordersHamid Colangcag AmborNo ratings yet
- Ask and RecieveDocument60 pagesAsk and RecieveScribdnera100% (1)
- Post Traumatic Stress Disorder PowerpointDocument18 pagesPost Traumatic Stress Disorder Powerpointapi-505733770100% (3)
- Pat Ogden Sensorimotor Therapy PDFDocument16 pagesPat Ogden Sensorimotor Therapy PDFEmili Giralt GuarroNo ratings yet
- Amistoso - DMDDDocument25 pagesAmistoso - DMDDAndréAmistosoNo ratings yet
- Behavioral Problems EncounteredDocument35 pagesBehavioral Problems EncounteredNamoAmitofou100% (1)
- Practice Essentials: Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)Document20 pagesPractice Essentials: Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)Anonymous 2ernTkNo ratings yet
- Post-Traumatic Stress Disorder (PTSD) PDFDocument13 pagesPost-Traumatic Stress Disorder (PTSD) PDFSheza SiddiquiNo ratings yet
- 2018.02.08 Trauma and Stressor Related DisordersDocument38 pages2018.02.08 Trauma and Stressor Related DisordersErin RyanNo ratings yet
- The Uk College of Hypnosis Hypnotherapy PDFDocument23 pagesThe Uk College of Hypnosis Hypnotherapy PDFblu6660% (1)
- The Evolution of Morality - Todd K. Shackelford y Ranald D. HansenDocument327 pagesThe Evolution of Morality - Todd K. Shackelford y Ranald D. HansenSam De León100% (1)
- The Art of EMDR Therapy in PTSD and Trauma: A Practical HandbookFrom EverandThe Art of EMDR Therapy in PTSD and Trauma: A Practical HandbookNo ratings yet
- Emotion Perception in MusicDocument5 pagesEmotion Perception in Musicnefeli123No ratings yet
- Prescribing Antipsychotics in Geriatric Patients:: First of 3 PartsDocument8 pagesPrescribing Antipsychotics in Geriatric Patients:: First of 3 PartsAlexRázuri100% (1)
- PTSD Takes Over The BrainDocument3 pagesPTSD Takes Over The Brainapi-548851649No ratings yet
- Trauma - and Stressor-Related DisordersDocument39 pagesTrauma - and Stressor-Related Disordersraneemghandour28No ratings yet
- Psych AdjustmentDocument2 pagesPsych Adjustmentapi-3704562No ratings yet
- Post-Traumatic Stress Disorder and Acute Stress DisorderDocument3 pagesPost-Traumatic Stress Disorder and Acute Stress Disorderag.carismaaNo ratings yet
- Ies RDocument2 pagesIes RJohn PrestonNo ratings yet
- Adjustment DisordersDocument2 pagesAdjustment DisordersIsabel CastilloNo ratings yet
- PTSDDocument4 pagesPTSDAzim Arif HashmiNo ratings yet
- Stress and Related DsDocument49 pagesStress and Related DsRibhav GuptaNo ratings yet
- Depression in Children and Young People: Symposium: PsychiatryDocument8 pagesDepression in Children and Young People: Symposium: Psychiatry126 - Askandarnur riskisa PahleviNo ratings yet
- PTSD EssayDocument7 pagesPTSD Essayaqsa rehmanNo ratings yet
- Abnormal Psychology (Chapter 5)Document3 pagesAbnormal Psychology (Chapter 5)Mavy QueenNo ratings yet
- DepressionDocument2 pagesDepressionIQRA ZAINABNo ratings yet
- Leaflet JiwaDocument3 pagesLeaflet JiwabilaNo ratings yet
- PTSDDocument3 pagesPTSDdaryaNo ratings yet
- Abpsych Midterms NotesDocument8 pagesAbpsych Midterms NotesJoshua MendezNo ratings yet
- Module 5a - Stress, Health, and Coping: Selye's Concept of StressDocument2 pagesModule 5a - Stress, Health, and Coping: Selye's Concept of Stress5676758457No ratings yet
- Perinatal Depression Review 20Document5 pagesPerinatal Depression Review 20Paula SouzaNo ratings yet
- Psych 410 PTSD NotesDocument4 pagesPsych 410 PTSD Notesapi-736917344No ratings yet
- Psychiatry - Mood Life and DeathDocument2 pagesPsychiatry - Mood Life and Deathhaladaqqa1No ratings yet
- Mental Health AwarenessDocument8 pagesMental Health AwarenessOyvin SemillaNo ratings yet
- Understanding and Dealing With ViolenceDocument58 pagesUnderstanding and Dealing With ViolenceIrene Grace FernandezNo ratings yet
- BCMJ 49 Vol3 Articles Posttraumatic StressDocument6 pagesBCMJ 49 Vol3 Articles Posttraumatic StressFrancisca AldunateNo ratings yet
- PTSD AwarenessDocument2 pagesPTSD AwarenessAdyson MorrisNo ratings yet
- PTSD-reading 2Document11 pagesPTSD-reading 2Az Z IrcNo ratings yet
- 4 - StressDocument60 pages4 - StressAman Singh RaoNo ratings yet
- Megan Simpson SBCNA 2018Document7 pagesMegan Simpson SBCNA 2018Priya JadhavNo ratings yet
- P.E. Group 3 PTSDDocument17 pagesP.E. Group 3 PTSDDavid Aldrich LimNo ratings yet
- DialoguesClinNeurosci 21 417Document12 pagesDialoguesClinNeurosci 21 417VickeyNo ratings yet
- Prof - Ed Task10Document2 pagesProf - Ed Task10Xyriz Seline SecillanoNo ratings yet
- Chapter 2 Trauma and Trauma ReactionsDocument42 pagesChapter 2 Trauma and Trauma ReactionsAnton BalansagNo ratings yet
- Chapter 9Document11 pagesChapter 9nayaddouaihyNo ratings yet
- Clinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956Document14 pagesClinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956abelim01No ratings yet
- Perinatal Depression: A ReviewDocument5 pagesPerinatal Depression: A ReviewDewi NofiantiNo ratings yet
- Trauma and Related DisorderDocument127 pagesTrauma and Related DisorderMayla WahabNo ratings yet
- Psychological Therapies For Posttraumatic Stress Disorder PDFDocument5 pagesPsychological Therapies For Posttraumatic Stress Disorder PDFJessicaPudduNo ratings yet
- Acute Stress DisorderDocument13 pagesAcute Stress DisorderYaska MusaNo ratings yet
- TRAUMADocument18 pagesTRAUMAcameronjuli.patubo.sciNo ratings yet
- Trauma Concept PaperDocument7 pagesTrauma Concept Paperapi-226804663No ratings yet
- What Is Trauma?Document10 pagesWhat Is Trauma?gayle livelo100% (1)
- Jane - Narrative PresentationDocument75 pagesJane - Narrative PresentationKathy ProcykNo ratings yet
- James Morrison Chapter 6 and 7 JMDocument7 pagesJames Morrison Chapter 6 and 7 JMAmanda ParrellaNo ratings yet
- Lesión Cerebral TraumáticaDocument8 pagesLesión Cerebral TraumáticaAlexRázuriNo ratings yet
- Correspondence: Atypical Presentation of COVID-19 in Young InfantsDocument1 pageCorrespondence: Atypical Presentation of COVID-19 in Young InfantsAlexRázuriNo ratings yet
- Trastornos PsicóticosDocument5 pagesTrastornos PsicóticosAlexRázuriNo ratings yet
- BMJ inflammatorySD ChildrenDocument1 pageBMJ inflammatorySD ChildrenAlexRázuriNo ratings yet
- EEG Epilepsia y Sueño 2Document12 pagesEEG Epilepsia y Sueño 2AlexRázuriNo ratings yet
- UK - BTS - Respiratory Support of Patients On Medical WardsDocument5 pagesUK - BTS - Respiratory Support of Patients On Medical WardsAlexRázuriNo ratings yet
- UK - Rapid Guideline Critical Care in AdultsDocument13 pagesUK - Rapid Guideline Critical Care in AdultsAlexRázuriNo ratings yet
- Article Covid-19 Children ReviewDocument12 pagesArticle Covid-19 Children ReviewAlexRázuri100% (1)
- Consensus Guidelines For Managing The Airway in Children With COVID-19Document11 pagesConsensus Guidelines For Managing The Airway in Children With COVID-19AlexRázuriNo ratings yet
- Remember:: Before Caring For Patients With Confirmed or Suspected COVID-19, Healthcare Personnel (HCP) MustDocument1 pageRemember:: Before Caring For Patients With Confirmed or Suspected COVID-19, Healthcare Personnel (HCP) MustAlexRázuriNo ratings yet
- Uptodate - Covid Guidelines LinksDocument10 pagesUptodate - Covid Guidelines LinksAlexRázuriNo ratings yet
- Article Origin Transmission Characterist COVID PDFDocument8 pagesArticle Origin Transmission Characterist COVID PDFAlexRázuriNo ratings yet
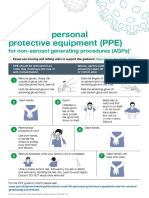
- Taking Off Personal Protective Equipment (Ppe) : For Non-Aerosol Generating Procedures (Agps)Document1 pageTaking Off Personal Protective Equipment (Ppe) : For Non-Aerosol Generating Procedures (Agps)AlexRázuriNo ratings yet
- T2 Poster Recommended PPE For Primary Outpatient Community and Social Care by SettingDocument1 pageT2 Poster Recommended PPE For Primary Outpatient Community and Social Care by SettingAlexRázuriNo ratings yet
- Uptodate - Coronavirus Epi, PreventionDocument55 pagesUptodate - Coronavirus Epi, PreventionAlexRázuriNo ratings yet
- Article Epidemio Therapeutics Vaccines Covid PDFDocument12 pagesArticle Epidemio Therapeutics Vaccines Covid PDFAlexRázuriNo ratings yet
- Epidemiology and Clinical Characteristics of COVID-19: MedicineDocument4 pagesEpidemiology and Clinical Characteristics of COVID-19: MedicineAlexRázuriNo ratings yet
- 1er ArticuloDocument7 pages1er ArticuloAlexRázuriNo ratings yet
- Betty Neuman Systems TheoryDocument6 pagesBetty Neuman Systems TheoryJenny SorianoNo ratings yet
- The Evaluation of Minecraft SampsonDocument7 pagesThe Evaluation of Minecraft Sampsonapi-279981311No ratings yet
- Barrett D 1992 Through A Glass Darkly Images of The Dead in DreamsDocument12 pagesBarrett D 1992 Through A Glass Darkly Images of The Dead in DreamsJuan ArizaNo ratings yet
- Grade 1 RHGP Module 2023Document59 pagesGrade 1 RHGP Module 2023JEANNo ratings yet
- Homework Marriage SolDocument4 pagesHomework Marriage Soltranthanhhoa2468No ratings yet
- Financial and Non-Financial Incentives - Explained!: by DR - Khalid RashidDocument47 pagesFinancial and Non-Financial Incentives - Explained!: by DR - Khalid RashidAshrafAliNo ratings yet
- Introduction To The Course: Midterm/Final GradeDocument9 pagesIntroduction To The Course: Midterm/Final GradeRanniel EstrellaNo ratings yet
- Action Research Presentation Berf 4.0Document21 pagesAction Research Presentation Berf 4.0Ricardo Evalla Jueves Jr.No ratings yet
- Adult DisordersDocument2 pagesAdult DisordersKai PesquiraNo ratings yet
- Writing Assignment Week TwoDocument3 pagesWriting Assignment Week TwoyesihavenNo ratings yet
- Introduction To Cross Culture and Human Resource ManagementDocument9 pagesIntroduction To Cross Culture and Human Resource ManagementRachel CoutinhoNo ratings yet
- Leadership Questions PDFDocument10 pagesLeadership Questions PDFdeanNo ratings yet
- Chapter 1 To 5Document72 pagesChapter 1 To 5Genesis AngeloNo ratings yet
- Lesson 10 - What - S Your PersonalityDocument21 pagesLesson 10 - What - S Your PersonalityLOVELY DELA CERNA50% (2)
- Teacher Stress Final Pre-Publication DraftDocument18 pagesTeacher Stress Final Pre-Publication DraftRegine CuntapayNo ratings yet
- Socio-Political Realities in Relation To Contemporary World.Document3 pagesSocio-Political Realities in Relation To Contemporary World.emmanuel.egoniaNo ratings yet
- FULLRESEARCHWORKONSTRESS EmmaDocument81 pagesFULLRESEARCHWORKONSTRESS EmmaCarmina BesarioNo ratings yet
- Robert Mager CRIDocument7 pagesRobert Mager CRInelieltuodeshvank50% (2)
- Lesh&harel BigfootDocument33 pagesLesh&harel BigfootAyşe YolcuNo ratings yet
- Group2 Lesson4 ReportDocument15 pagesGroup2 Lesson4 ReportJann Marie CalledoNo ratings yet
- NURS FPX 6105 Assessment 1 Learning Theories and DiversityDocument6 pagesNURS FPX 6105 Assessment 1 Learning Theories and Diversityzadem5266No ratings yet
- Organizational Behavior 4th Edition Hitt Test BankDocument19 pagesOrganizational Behavior 4th Edition Hitt Test BankSaraSmithdgyj100% (40)
- Alex A. Courtney-Guy-Data Blitz PresentationDocument10 pagesAlex A. Courtney-Guy-Data Blitz PresentationEvie EmeryNo ratings yet
- Practical Nursing Clinical Syllabus-2014-15Document110 pagesPractical Nursing Clinical Syllabus-2014-15jedisay1No ratings yet