Professional Documents
Culture Documents
Journal Pone 0280199 PDF
Uploaded by
Michel BetyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal Pone 0280199 PDF
Uploaded by
Michel BetyCopyright:
Available Formats
PLOS ONE
RESEARCH ARTICLE
Middle ear effusion, ventilation tubes and
neurological development in childhood
Jonathan Thorsen ID1☯, Tine Marie Pedersen1,2☯, Anna-Rosa Cecilie Mora-Jensen1,2,
Elı́n Bjarnadóttir1,2, Søren Christensen Bager1,2, Hans Bisgaard1†, Jakob Stokholm ID1,2*
1 COPSAC, Copenhagen Prospective Studies on Asthma in Childhood, Herlev and Gentofte Hospital,
University of Copenhagen, Copenhagen, Denmark, 2 Department of Pediatrics, Naestved Hospital,
Naestved, Denmark
☯ These authors contributed equally to this work.
a1111111111 † Deceased.
a1111111111 * stokholm@copsac.com
a1111111111
a1111111111
a1111111111 Abstract
Background
OPEN ACCESS Otitis media with middle ear effusion (MEE) can be treated with ventilation tubes (VT) inser-
Citation: Thorsen J, Pedersen TM, Mora-Jensen A- tion, and it has been speculated that prolonged MEE in childhood can affect neurological
RC, Bjarnadóttir E, Bager SC, Bisgaard H, et al. development, which in turn may be important for later academic achievements.
(2023) Middle ear effusion, ventilation tubes and
neurological development in childhood. PLoS ONE
18(1): e0280199. https://doi.org/10.1371/journal. Objective
pone.0280199
To investigate the association between middle ear effusion (MEE), treatment with ventilation
Editor: Rafael da Costa Monsanto, Universidade tubes (VT) and childhood neurological development.
Federal de Sao Paulo/Escola Paulista de Medicina
(Unifesp/epm), BRAZIL
Received: September 14, 2022
Study design
Accepted: December 22, 2022
We examined 663 children from the Copenhagen Prospective Studies on Asthma in Child-
hood 2010 (COPSAC2010) unselected mother-child cohort study. Children were followed by
Published: January 13, 2023
study pediatricians with regular visits from pregnancy until 3 years of age. MEE was diag-
Peer Review History: PLOS recognizes the nosed using tympanometry at age 1, 2 and 3 years. Information regarding VT from age 0–3
benefits of transparency in the peer review
process; therefore, we enable the publication of
years was obtained from national registries. We assessed age at achievement of gross
all of the content of peer review and author motor milestones from birth, language scores at 1 and 2 years, cognitive score at 2.5 years
responses alongside final, published articles. The and general development score at age 3 years using standardized quantitative tests.
editorial history of this article is available here:
https://doi.org/10.1371/journal.pone.0280199
Results
Copyright: © 2023 Thorsen et al. This is an open
access article distributed under the terms of the Children with MEE had a lower 1-year word production vs. children with no disease: (median
Creative Commons Attribution License, which 2, IQR [0–6] vs. 4, IQR [1–7]; p = 0.017), and a lower 1-year word comprehension (median
permits unrestricted use, distribution, and
36; IQR [21–63] vs. 47, IQR [27–84]; p = 0.03). Children with VT had a lower 2-5-year cogni-
reproduction in any medium, provided the original
author and source are credited. tive score vs. children with no disease; estimate -2.34; 95% CI [-4.56;-0.12]; p = 0.039. No
differences were found between children with vs. without middle ear disease regarding age
Data Availability Statement: Individual-level
personally identifiable clinical data from the at achievement of gross motor milestones, word production at 2 years or the general devel-
children participating in the cohort cannot be made opmental score at 3 years.
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 1 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
freely available, to protect the privacy of the Conclusion
participants and their families, in accordance with
the Danish Data Protection Act and European Our study supports the previous findings of an association between MEE and concurrent
Regulation 2016/679 of the European Parliament early language development, but not later neurological endpoints up to the age of 3. As VT
and of the Council (GDPR) that prohibit distribution can be a treatment of those with symptoms of delayed development, we cannot conclude
even in pseudo-anonymized form. However,
research collaborations are welcome, and data can
whether treatment with VT had positive or negative effects on neurodevelopment.
be made available under a joint research
collaboration by contacting the COPSAC Data
Protection Officer (DPO), Ulrik Ralkiaer, PhD
(administration@dbac.dk).
Funding: COPSAC is funded by private and public Introduction
research funds all listed on www.copsac.com. The
Neurological development including motor and language skills, and cognitive function is
Lundbeck Foundation; The Danish Ministry of
Health; Danish Council for Strategic Research and affected by genetics and environmental factors [1, 2]. Early life influences play a significant
The Capital Region Research Foundation have role in shaping neurological development [3] and may be important determinants of a child’s
provided core support for COPSAC. No subsequent academic achievements [4–7].
pharmaceutical company was involved in the Otitis media is an inflammatory process within the middle ear space, presenting as either
study. TMP has received funding from Oticon
an acute infection or as middle ear effusion (MEE); a long-lasting condition with accumulation
Foundation and GN Store Nord Foundation. The
funding agencies did not have any role in design
of fluid without symptoms of acute infection [8]. MEE is believed to impair children’s balance
and conduct of the study; collection, management, and it has been speculated that prolonged MEE in early childhood can affect motor develop-
and interpretation of the data; or preparation, ment [9, 10]. Furthermore, MEE decreases the mobility of the tympanic membrane, which can
review, or approval of the manuscript. result in a mild to moderate conductive hearing loss [11] and potentially delay language devel-
Competing interests: I have read the journal’s opment [12–14].
policy and the authors of this manuscript have the Prolonged MEE is often treated with ventilation tubes (VT) [15]. Treatment with VT has been
following competing interests: JT has received a shown to increase the short-term hearing ability, but with no apparent long-term effects [14].
speaking fee from AstraZeneca. This does not alter Thus, recent studies investigating the effect of MEE/VT on language and neurodevelop-
our adherence to PLOS ONE policies on sharing
mental outcomes have shown conflicting results [11, 16], warranting longitudinal prospective
data and materials. The authors have no other
potential conflicts of interest to disclose. studies investigating such long-term effects of MEE and VT.
The aim of this study was to investigate the associations between untreated MEE, treatment
Abbreviations: MEE, Middle Ear Effusion; VT,
with VT and children with no middle ear disease and neurological development. We used the
Ventilation Tubes; COPSAC2010, COpenhagen
Prospective Studies on Asthma in Childhood2010; neurological assessments: age at achievement of gross motor milestones, scores in language-
ASQ-3, Ages & Stages Questionnaires®, Third and cognitive tests as well as general development of the children in the Copenhagen Prospec-
Edition; PPCA, Proportional Principal Component tive Studies on Asthma in Childhood2010 (COPSAC2010) birth cohort [17, 18].
Analysis; PC, Principal Compone; PCA, Principal
Component Analysis; IQR, Interquartile range; CI,
Confidence Interval; SD, Standard deviation.
Materials and methods
Study population
COPSAC2010 is an ongoing unselected prospective mother-child cohort study of 738 pregnant
women and their children recruited in pregnancy week 24 from 2008–2010 [17]. The key
exclusion criteria for the pregnant women were chronic disease other than asthma or lack of
fluency in Danish. Seven-hundred children were enrolled in the cohort at one week of age,
excluding children with severe congenital abnormalities. For the present study, we excluded
children with a neurological diagnosis and those born <37 weeks of gestation or with birth
weight <2500g from all analyses. The children were followed in the COPSAC research clinics
with 9 planned visits during the first three years of life. The study size was based on estimated
prevalence of early asthma symptoms, as previously described [17].
Ethics
The study was conducted in accordance with the guiding principles of the Declaration of Hel-
sinki and was approved by the Local Ethics Committee (H-B-2008-093), and the Danish Data
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 2 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Protection Agency (2015-41-3696). Both parents gave written informed consent before
enrolment.
Middle ear effusion and ventilation tubes
MEE was assessed using tympanometry performed by the research doctors in the COPSAC
unit at scheduled visits at age one, two and three years. Tympanometry was performed using
an Interacoustics MT10 hand-held impedance audiometer (Interacoustics, Middelfart, Den-
mark) with a tone of 226Hz and intensity of 85 dB SPL. A type B tympanogram (flat curve)
was interpreted as MEE [19, 20], while type A or C tympanograms were considered not MEE.
Information regarding VT insertions was obtained from two Danish registries, The Danish
National Hospital Register [21], which contains all hospital records on VT insertions (ICD-10
diagnosis: KDCA20), and The Danish National Health Service Register (procedure code:
3009) [22], which contains information on VT insertions performed in private Ear-Nose-
Throat surgeon clinics. All procedures are linked with a personal identification number of the
child, leaving no missing observations [23]. For the outcome analyses, we defined a compound
MEE/VT variable at each yearly timepoint as either a) Ventilation tube insertion before that
date, b) Middle ear effusion (type B curve) at visit or at previous visit(s), c) No VT/MEE (type
A/C curve) at visit, d) Missing data (no tympanometry measurement) at visit, in prioritized
order.
Neurological developmental assessment
Milestones. The parents received a registration form at the 1-week clinical visit, with thor-
ough instructions, based on The Denver Development Index [24] and World Health Organiza-
tion milestones registration [25]. Dates of achievement of 13 predefined milestones were
registered by the parents. Only the gross motor milestones: sit alone, stand with help, crawl,
stand alone, walk with help and walk alone were used to analyze the association with MEE and
VT because the achievement of these could be delayed by poor balance [10, 26].
Language development. Language development was assessed with the Danish version of
The MacArthur Bates Communicative Developmental Inventory [27]. Bilingual children were
excluded from this assessment, since they may follow different temporal language acquisition
patterns [28]. The assessment was performed by a web-based questionnaire filled out by
parents around the child’s 1-year (Words and gesticulation) and 2-year birthday (Words and
sentences). From the 1-year questionnaire, we used the scores regarding word production and
word comprehension. From the 2-year questionnaire, we used the word production score for
the analyses.
Cognitive development. Cognitive development was assessed at 2.5 years of age, using
the cognitive part of the third edition of the Bayley Scales of Infant and Toddler Development
[29]. During the examinations, the examiner presented a series of test materials to the child
and observed the child’s responses and behavior. Based on its objective performance, the child
was given a composite score, which was standardized by use of a normalization material of age
corrected means of 100 and a standard deviation of 15 (range 50–150). Examinations were per-
formed by 10 trained examiners and inter-examiner consistency in performance was validated
by inspection of video recordings [18].
General neurological development. The parent-completed Ages & Stages Question-
naires1, Third Edition (ASQ-3) consists of 5 categories; fine motor, gross motor, personal-
social, communication and problem solving skills. Parents completed the questionnaire prior
to the 3 years visit, where the responses were subsequently verified. Children received a score
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 3 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
for each category of the ASQ-3 and we combined the 5 areas statistically and used the com-
bined score as a general development score at the age of 3.
Covariates. Information regarding maternal age at birth, smoking during pregnancy,
maternal asthma, delivery method, gestational age, birth weight, sex and older siblings in the
household was obtained by personal interview at the 1 week visit in the COPSAC clinic. Dura-
tion of exclusive breastfeeding and age at beginning of daycare were obtained longitudinally
from clinical interviews during the first year of life. Household income, maternal age and level
of education were obtained from interviews when the children were 2 years of age and com-
bined as a composite measure of the child’s social circumstances defined as the z-scored first
component of a PCA (explaining 55% of the variance).
Statistics
Differences in the baseline characteristics between children with MEE, VT and with no middle
ear disease were determined by Chi-square test, t-test, or Wilcoxon rank-sum test. All variables
were tested for normal distribution and models were verified by visual inspection of residual
plots. Trajectories were calculated as multinomial logistic regression comparing only MEE vs
no disease as predictors and expressed as odds ratios (ORs). For the outcome analyses, we split
the children into three groups: children with untreated MEE, children who had received VT,
and children with no middle ear disease. The language data for the 1-year test were log-trans-
formed after adding a pseudocount of 1 for the linear models to derive sex-adjusted p-values.
Results were presented as medians with interquartile range (IQR) on the original scale. No
transformation of the data was needed for the 2-year language data or the cognitive test. Gen-
eral linear models were used to analyze the association between untreated MEE, treatment
with VT compared to children with no disease and their language- and cognitive development.
As sex is a known determinant of neurodevelopment [30–32], also in our cohort [18], all asso-
ciations were adjusted for sex.
Age of milestone achievement was analyzed using a probabilistic principal component anal-
ysis (PPCA). This model included the full dataset with missing values, assuming that the miss-
ing values were missing at random. Missing data were otherwise treated as missing
observations. The 5 areas of the ASQ-3 were combined in a PCA model, which was used to
extract underlying principal components (PCs) that described the systematic part of the varia-
tion across the ASQ-3 score variables in fewer uncorrelated variables. Associations between
MEE and VT at age 1 year and all the study outcomes were analyzed in a combined PCA
model.
A significance level of 0.05 was used in all analyses. All estimates were reported with 95%
confidence intervals (CI). The data processing and analysis was conducted using R [33] version
3.6.1 with the packages pcaMethods [34] and nnet [35] and visualized using the packages
ggplot2 [36] and ggforce [37].
Results
Baseline characteristics
A total of 700 children were included in the COPSAC2010 cohort at birth and information on
VT insertions was available for all 700 children. We excluded 37 children from the study
because of neurological diagnosis, low gestational age, or low birth weight (S1 Fig), leaving 663
children. In these 663 children, tympanometry was successfully performed on 537 children at
1 year, 563 at 2 years, and 578 at 3 years (S1 Fig), showing that 51% (n = 276/537) had MEE at
1 year, 37% (n = 210/563) at 2 years and 26% (n = 155/578) at 3 years (S2 Fig). 5% (n = 36/663)
of the children had VT inserted before age 1 year, 26% (n = 173/663) before 2 years and 29%
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 4 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
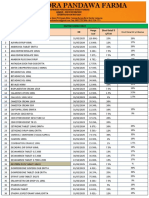
Table 1. Baseline characteristics of the COPSAC2010 cohort. Children with middle ear effusion (MEE), ventilation tubes (VT) or children without middle ear disease
before the age of 3. 30 children with missing assessments at 3 years were excluded from the table.
No middle ear disease � 3 y Middle ear effusion � 3 y P-value Ventilation tubes � 3 y P-value
N = 129 n = 312 n = 192
Pregnancy and birth
Maternal age at birth, mean (SD) 31.59 (3.95) 32.50 (4.31) 0.040 32.44 (4.54) 0.087
Delivery, Cesarean section, n (%) 26 (20.2) 61 (19.6) 0.99 39 (20.3) 1.00
Length in cm at birth, mean (SD) 52.34 (2.12) 52.08 (2.24) 0.26 52.22 (1.99) 0.62
Birth weight in kg, mean (SD) 3.63 (0.46) 3.59 (0.49) 0.34 3.60 (0.47) 0.55
Head circumference in cm at birth, mean (SD) 35.22 (1.29) 35.05 (1.75) 0.30 35.17 (1.56) 0.75
Sex, boys, n (%) 55 (42.6) 164 (52.6) 0.073 107 (55.7) 0.029
Ethnicity, caucasian, n (%) 120 (93.0) 300 (96.2) 0.25 187 (97.4) 0.11
Season of birth, n (%) <0.001 0.21
• Winter 32 (24.8) 114 (36.5) 50 (26.0)
• Spring 27 (20.9) 91 (29.2) 51 (26.6)
• Summer 43 (33.3) 45 (14.4) 44 (22.9)
• Autumn 27 (20.9) 62 (19.9) 47 (24.5)
Exposures
Smoking during pregnancy, n (%) 9 (7.0) 24 (7.7) 0.95 14 (7.3) 1.00
Older siblings, n (%) 62 (48.1) 178 (57.1) 0.11 129 (67.2) 0.001
Duration of exclusive breastfeeding in days, median (IQR)a 122 (58, 151) 122 (55.75, 149) 0.76 122 (56.50, 151) 0.99
a
Age at start in daycare in months, median (IQR) 10.4 (9.7, 11.9) 10.3 (9.1, 11.8) 0.25 10.1 (9.1, 11.3) 0.023
Social circumstances PCA scoreb, mean (SD) -0.04 (0.98) 0.08 (0.99) 0.26 -0.09 (0.97) 0.64
a b
Wilcoxon test. PCA component consist of household income, maternal age, and maternal educational level at the age of 2; Higher values of the score indicate higher
values for all input variables.
https://doi.org/10.1371/journal.pone.0280199.t001
(n = 192/663) before 3 years (S3 Fig). Table 1 shows the baseline characteristics for children,
who had either MEE or were treated with VT compared to children with no middle ear disease
before the age of 3. We found more boys with VT compared to girls. Season of birth was asso-
ciated with the risk of MEE, but not VT insertion. Having older siblings and the age at daycare
start were associated with treatment with VT, but not with MEE.
Trajectories of middle ear disease
The middle ear status of each child at each yearly assessment is illustrated in Fig 1. 274 children
had MEE, but no VT, at the 1-year visit. At 2 years, 102 of these (37%) still had MEE, 73 (27%)
had VT, 75 (27%) had no disease, and 24 (9%) had missing data. A total of 193 children had
MEE, but no VT, at the 2-year visit. At 3 years, 63 (33%) of these still had MEE, 14 (7%) had
VT, 95 (49%) had no disease and 21 (11%) had missing data. Compared to children with no
disease, those with MEE at 1 year had increased risk of still having MEE at 2 years (OR 2.33,
95% CI [1.50;3.61], p = 0.0002), as well as increased risk of VT at 2 years (2.81, [1.70;4.64],
p<0.0001). Similarly, those with MEE at 2 years had increased risk of MEE at 3 years (3.26
[1.9;5.32], p<0.0001) and VT at 3 years (5.97 [1.91;18.7], p = 0.002) although the latter transi-
tion was rare in both groups.
Gross motor milestones
Information on achievement of at least one gross motor milestone and information regarding
MEE and VT before the age of 1 year was available for 75% (n = 500/663) of the children. The
overall gross motor development represented by the PC1 score of the PCA model, which
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 5 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Fig 1. Yearly trajectories of early-life chronic middle ear disease. Middle ear effusion was assessed with yearly tympanometry measurements. Ventilation
tubes was defined by start date in registries and carried forward throughout the whole period. Colors correspond to the 2-year timepoint. N = 663.
https://doi.org/10.1371/journal.pone.0280199.g001
explained 63.7% of the variance in the original variables, was used to analyze the associations
(S4 Fig). Neither MEE nor VT were significantly associated with age of gross motor milestone
achievement compared to children without middle ear disease (Table 2 and S4 Fig).
Language development at 1 and 2 years
Completed language assessment at 1 year and information regarding MEE and VT before the
age of 1 year was obtained for 46% (n = 305/663) of the children (Fig 1). Children with MEE at
age 1 year had a lower word production at the concurrent language assessment compared to
children with no middle ear disease (median 2, IQR [0–6] vs. 4, IQR [1–7]), corresponding to
a reduction of 24%, 95% CI [5%;39%], p = 0.02. MEE at age 1 year was also associated with a
lower word comprehension compared with no middle ear disease (median 36; IQR [21–63] vs.
47; IQR [27–84]), corresponding to a reduction of 21%, 95% CI [2%;35%], p = 0.03. No associ-
ations were found between VT insertions and the 1-year language scores (Table 2).
Completed language assessment at 2 years and information on MEE at 1 or 2 years or VT
insertions before age 2 years was obtained for 71% (n = 472/663) of the children. No associa-
tions were found between MEE or VT and the 2-year language scores (Table 2).
Cognitive score
A completed cognitive test at 2.5 years and information regarding MEE at age 1 or 2 years and
VT before 2.5 years was obtained for 84% (n = 558/663) of the children. VT insertion was asso-
ciated with a lower composite score; adjusted estimate -2.34; 95% CI [-4.56;-0.12]; p = 0.04,
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 6 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Table 2. Associations between middle ear effusion (MEE) or treatment with ventilation tubes (VT) and neurological development. All analyses are adjusted for sex.
Gross Motor Milestones PPCA
PC1 (higher value = faster achievement) N = 500 Estimate 95% CI P-value
MEE at 1 year 253 (-0.03) [-0.37;0.30] 0.84
VT � 1 year 34 0.33 [-0.34;1.01] 0.33
No VT, no MEE � 1 year 213 reference - -
Word production at 1 year N = 305 Median words IQR P-value
MEE at 1 year 159 2 [0–6] 0.017
VT � 1 year 21 5 [1–8] 0.74
No VT, no MEE � 1 year 125 4 [1–7] Reference
Word comprehension at 1 year N = 305 Median words IQR P-value
MEE at 1 year 159 36 [21–63] 0.030
VT � 1 year 21 44 [20–76] 1.00
No VT, no MEE � 1 year 125 47 [27–84] reference
Word production at 2 years N = 472 Median words IQR P-value
MEE at 1 or 2 years 230 242 [121–356] 0.29
VT � 2 years 130 226 [87–361] 0.17
No VT, no MEE � 2 years 112 282 [155–370] reference
Cognitive test at 2.5 years (higher value = faster development) N = 558 Estimate 95% CI P-value
MEE at 1 or 2 years 258 (-0.38) [-2.43;1.66] 0.71
VT � 2.5 years 169 (-2.34) [-4.56;-0.12] 0.039
No VT, no MEE � 2.5 years 131 reference - -
ASQ-3 PCA at 3 years
PC1 (higher value = faster development) N = 414 Estimate 95% CI P-value
MEE ever (at 1, 2, or 3 years) 211 (-1.80) [-4.50;0.90] 0.19
VT � 3 years 117 (-1.55) [-4.53;1.44] 0.31
No VT, No MEE � 3 years 86 reference - -
Combined PCA of all neurological assessments
PC1 (higher value = more developed) N = 531 Estimate 95% CI P-value
MEE at 1 year 270 (-0.15) [-0.49;0.20] 0.40
VT � 1 year 35 0.42 [-0.27;1.12] 0.23
No VT, No MEE � 1 year 226 reference - -
PC2 (higher value = better language and cognition) N = 531 Estimate 95% CI P-value
MEE at 1 year 270 (-0.23) [-0.46;-0.002] 0.048
VT � 1 year 35 (-0.04) [-0.50;-0.42] 0.87
No VT, No MEE � 1 year 226 reference - -
PC = Principal Component. PPCA = Probabilistic Principal Component Analysis.
https://doi.org/10.1371/journal.pone.0280199.t002
(Table 2). However, there were no differences between children with MEE at either 1 or 2
years and children with no middle ear disease with regards to the cognitive scores at 2.5 years.
General development assessment (ASQ-3)
Completed ASQ-3 assessment at 3 years and information regarding MEE at age 1, 2 or 3 years
or VT before 3 years of age was obtained for 62% (n = 414/663) of the children (Fig 1). The
ASQ-3 PCA resulted in a PC1 score, which explained 47.5% of the variation in the data (S5
Fig). There were no differences between children with MEE at either 1, 2 or 3 years of age, VT
before the age of 3 and children with no middle ear disease with regards to the general develop-
ment of the child at age 3 years (Table 2).
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 7 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Fig 2. PCA biplot of the neurological development scores of each child and loadings of the neurological variables. Ellipses illustrate the scores (95% CI) of
children with middle ear effusion, treatment with ventilation tubes and no disease. Gross motor milestones (Sit alone, Stand with help, Stand alone, Walk with
help, Walk alone) language development at 1 and 2 years, cognitive score at 2.5 years and the ASQ-3 scores (problem solving, communication, gross motor,
fine motor) at 3 years comparing children with middle ear effusion, ventilation tubes and children without middle ear disease.
https://doi.org/10.1371/journal.pone.0280199.g002
Combined PCA of neurological endpoints
To analyze effects of middle ear disease and all later neurological endpoints, we examined
MEE at age 1 year and VT before 1 year in a combined PPCA model of all neurological mea-
sures. PC1 explained 38.1% of the variation in the neurological data and PC2 explained 18.5%
of the variation (Fig 2). MEE at 1 year was significantly associated with a lower PC2-value;
adjusted estimate -0.23; 95% CI [-0.46;-0.002]; p = 0.048; but was not associated with PC1 and
no significant associations were found for VT before 1 year of age.
Discussion
Primary findings
In an unselected prospective birth cohort, we assessed MEE and VT longitudinally in the first
three years of life in 663 children. While most untreated MEE remitted spontaneously, a signif-
icantly increased risk of persistence or VT insertion in the following year was found both for
the 1- and 2-year timepoint. We found slightly lower language scores at age 1-year among chil-
dren with concurrent MEE compared to children without middle ear disease, but no differ-
ences in the 2-year language scores and no associations between VT and language scores.
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 8 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Children who received VT had a reduced cognitive score at 2.5 years, but without associations
among children who had MEE. No differences were found between children with MEE or VT
and those without disease for gross motor milestone achievement or for the general develop-
ment ASQ-3 score at 3 years of age.
Strengths and limitations
The children in the COPSAC2010 cohort have been followed prospectively since birth with sev-
eral neurological assessments to evaluate the development of the children. We have both early
and late measures of the motor development. We have evaluated the language development
both at age 1 and 2 years and as part of the ASQ-3 at 3 years. Furthermore, we evaluated the
cognitive development of the children by the objective cognitive test in the research clinic.
This provides a unique collection of standardized neurological developmental tests performed
prospectively in a large cohort of children.
Not all children completed all tests (S1 Fig), which could limit the statistical power. Missing
information on specific milestones was handled by the PPCA model. A single missing mile-
stone would otherwise have excluded the child in a traditional PCA model.
MEE was diagnosed by the tympanometry measurement, which is an objective, well recog-
nized test and easy to perform. The limitation is the nature of an annual spot measurement in
the COPSAC clinic, as children may have had periods of MEE between the examinations.
However, most children are affected by MEE over longer periods of time, making the yearly
measurements an acceptable measure of MEE burden. Season of birth was associated with
MEE but not with VT. This could be due to the study design with annual measurements, since
children were assessed in the same season around their birthday every year (Table 1).
The Danish registries strengthen the study as they contain information regarding all VT
procedures and contacts with the health care system linked to a personal identification num-
ber. Therefore, we have information regarding VT procedures on all 700 children in the
cohort. The registries do not contain information on the VT indication (middle ear effusion,
recurrent acute otitis media or other reason), or for how long the VT was in place, which may
limit our interpretation.
The study is limited by its observational design. Since treatment with ventilation tubes was
performed by indication, we cannot know if any observed differences between groups are due
to disease history, treatment, or both. Similarly, we cannot observe the counterfactual non-
treatment outcomes in the children who were treated with VTs. Only a randomized trial can
evaluate the efficacy of VT insertion with respect to later developmental endpoints.
Interpretation
We found that approximately half of 1-year old children, reducing to one quarter of 3-year-old
children, have MEE as assessed by tympanometry. Furthermore, the risk of subsequent MEE
was increased in those children who previously had MEE.
In our study, MEE but not VT was associated with language scores at 1 but not 2 years. This
could indicate that the VT insertion is beneficial for the short-term hearing ability; however, at
2 years of age, we found no difference between the children with MEE or VT and children
without disease regarding their language development. The Australian Raine cohort study
(n = 1344) found only a very slightly reduced rate of vocabulary growth at 10 years in children
who had bilateral OM at 6 years [38]. These observations are supported by previous literature
describing MEE to cause a mild hearing impairment, which often resolves spontaneously [14].
We found an increased rate of VT in children with siblings, and a non-significant trend
towards the same for MEE. This could be due to increased risk of infections in children with
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 9 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
siblings [39], or due to an effect on the airway microbiota [40], which may in turn influence
infection susceptibility [41].
We found that the cognitive test at the age of 2.5 years was associated with VT but not
MEE. This could indicate that treatment with VT did not have beneficial effects on the cogni-
tive development of the children or simply indicate confounding by indication; the children
treated with VT were those, who had the most symptoms of delayed development, which is
consistent with current guidelines [15].
We observed no associations between early middle ear disease and neither the gross motor
milestones nor the general development measured by ASQ-3 [42]. The combined PCA analysis
of all recorded neurological measures showed that MEE at 1 year was significantly association
with PC2 (mainly driven by lower language and cognitive scores) (Fig 2). No association was
found for VT in the combined PCA analysis, which could be because only few children were
treated with VT before 1 year of age. The result of this combined neurological PCA supports
the individual endpoint analyses.
The literature shows conflicting results regarding the beneficial effects of treatment with
VT on neurodevelopmental outcomes [11, 16, 43–45]. In the American study by Paradise
et al., children with MEE were randomized to treatment either promptly with VT or after 9
months if MEE persisted, and they were followed until the age of 9–11 years with developmen-
tal evaluations. They found no difference between children in the two groups regarding cogni-
tive, language, speech, or psychosocial development [46, 47]. In the Australian Raine cohort,
recurrent OM at 3 years was associated with behavior at 10 years of age [48]. Developmental
outcomes may vary between countries. It is known that Danish children generally score lower
in early language tests, probably caused by the nature of the Danish sound structure [49].
Other factors potentially accounting for discrepancies between studies could be cultural differ-
ences such as age of daycare attendance [49].
Our study supports the previous findings of an effect of MEE on concurrent early language
development. Except for the 1-year language scores, the children with VT had lower estimates
compared to children with MEE or children without middle ear disease. We cannot conclude
whether treatment with VT had any beneficial neurological effects, but we demonstrated no
long-term differences between treated and untreated children.
In our cohort 29% of the children received VT before the age of 3 [50], which is a very high
prevalence for a treatment with no solid evidence of long-term beneficial effects. Well-
designed randomized controlled trials to gauge the efficacy of VTs for improving neurological
development are warranted.
Conclusion
MEE and VT insertion were very common in this cohort of 663 unselected Danish children.
MEE displayed a high degree of recurrence and risk of subsequent VT insertion. Children with
MEE at 1 year had slightly lower language scores at 1-year of age, but they were not affected in
any other neurological endpoints to age 3 years. We did not find any major differences in the
neurological development between children treated with VT and children without middle ear
disease. In summary, children with middle ear disease in the first three years of life did not
have materially delayed neurologic development by age 3.
Supporting information
S1 Fig. Flowchart and participation in each study assessment and outcome analysis.
(TIF)
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 10 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
S2 Fig. Prevalence of middle ear effusion measured by tympanometry at 1, 2 and 3 years of
age in the COPSAC2010 cohort.
(TIF)
S3 Fig. Kaplan-Meier curve illustrating time to first ventilation tube insertion in the COP-
SAC2010 cohort.
(TIF)
S4 Fig. PPCA biplot of the gross motor milestone scores of each child and loadings of the
neurological variables. Ellipses illustrate the scores (95% CI) of children with middle ear effu-
sion, treatment with ventilation tubes and no disease in the first year of life. The figure shows
that there is no difference between children with middle ear effusion, ventilation tubes and no
disease in the age of achieving the gross motor milestones. High PC1 scores can be interpreted
as lower age at achievement of alle the gross motor milestones, especially Stand with help,
Stand alone, Walk with help, Walk alone.
(TIF)
S5 Fig. PCA biplot of the ASQ-3 scores of each child and loadings of the neurological vari-
ables. Ellipses illustrate the scores (95% CI) of children with middle ear effusion, treatment
with ventilation tubes and children with no disease. The ASQ-3 consists of 5 categories; fine
motor development, gross motor development, personal-social skills, communication and
problem solving. When the scores are analyzed together as one measure of the child’s develop-
ment it results in a PC1 score, which explains 47.5% of the variation. Higher values on PC1
equates to higher scores in all categories, especially Fine motor and Problem solving, which
can be interpreted as children with high PC1 scores are further in their development than
those with low PC1 scores.
(TIF)
Acknowledgments
We express our deepest gratitude to the children and families of the COPSAC2010 cohort study
for all their support and commitment. We acknowledge and appreciate the unique efforts of
the COPSAC research team.
Governance
We are aware of and comply with recognized codes of good research practice, including the
Danish Code of Conduct for Research Integrity. We comply with national and international
rules on the safety and rights of patients and healthy subjects, including Good Clinical Practice
(GCP) as defined in the EU’s Directive on Good Clinical Practice, the International Confer-
ence on Harmonisation’s (ICH) good clinical practice guidelines and the Helsinki Declaration.
We follow national and international rules on the processing of personal data, including the
Danish Act on Processing of Personal Data and the practice of the Danish Data Inspectorate.
Author Contributions
Conceptualization: Jonathan Thorsen, Tine Marie Pedersen, Hans Bisgaard, Jakob Stokholm.
Data curation: Jonathan Thorsen, Tine Marie Pedersen, Anna-Rosa Cecilie Mora-Jensen, Elı́n
Bjarnadóttir.
Formal analysis: Jonathan Thorsen, Tine Marie Pedersen, Jakob Stokholm.
Funding acquisition: Tine Marie Pedersen, Hans Bisgaard, Jakob Stokholm.
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 11 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
Investigation: Jonathan Thorsen, Tine Marie Pedersen, Anna-Rosa Cecilie Mora-Jensen, Elı́n
Bjarnadóttir, Søren Christensen Bager, Hans Bisgaard, Jakob Stokholm.
Methodology: Tine Marie Pedersen, Elı́n Bjarnadóttir, Hans Bisgaard, Jakob Stokholm.
Project administration: Jonathan Thorsen, Tine Marie Pedersen, Hans Bisgaard, Jakob
Stokholm.
Supervision: Hans Bisgaard, Jakob Stokholm.
Validation: Jonathan Thorsen, Jakob Stokholm.
Visualization: Jonathan Thorsen.
Writing – original draft: Jonathan Thorsen, Tine Marie Pedersen, Jakob Stokholm.
Writing – review & editing: Jonathan Thorsen, Tine Marie Pedersen, Anna-Rosa Cecilie
Mora-Jensen, Elı́n Bjarnadóttir, Søren Christensen Bager, Hans Bisgaard, Jakob Stokholm.
References
1. Hackman DA, Farah MJ. Socioeconomic status and the developing brain. Trends Cogn Sci. 2009; 13:
65–73. https://doi.org/10.1016/j.tics.2008.11.003 PMID: 19135405
2. Jansen AG, Mous SE, White T, Posthuma D, Polderman TJC. What Twin Studies Tell Us About the
Heritability of Brain Development, Morphology, and Function: A Review. Neuropsychol Rev. 2015; 25:
27–46. https://doi.org/10.1007/s11065-015-9278-9 PMID: 25672928
3. Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, Garner AS, et al. The Lifelong Effects of
Early Childhood Adversity and Toxic Stress. Pediatrics. 2012; 129: e232–e246. https://doi.org/10.1542/
peds.2011-2663 PMID: 22201156
4. Monk C, Georgieff MK, Osterholm EA. Research Review: Maternal prenatal distress and poor nutrition–
mutually influencing risk factors affecting infant neurocognitive development. Journal of Child Psychol-
ogy and Psychiatry. 2013; 54: 115–130. https://doi.org/10.1111/jcpp.12000 PMID: 23039359
5. Hertzman C, Siddiqi A, Hertzman E, Irwin LG, Vaghri Z, Houweling TAJ, et al. Bucking the inequality
gradient through early child development. BMJ. 2010; 340: c468. https://doi.org/10.1136/bmj.c468
PMID: 20147358
6. Taanila A, Murray GK, Jokelainen J, Isohanni M, Rantakallio P. Infant developmental milestones: a 31-
year follow-up. Dev Med Child Neurol. 2005; 47: 581–586. PMID: 16138663
7. Nyaradi A, Li J, Hickling S, Foster J, Oddy WH. The role of nutrition in children’s neurocognitive develop-
ment, from pregnancy through childhood. Front Hum Neurosci. 2013; 7: 97. https://doi.org/10.3389/
fnhum.2013.00097 PMID: 23532379
8. Rovers MM, Schilder AGM, Zielhuis GA, Rosenfeld RM. Otitis media. Lancet. 2004; 363: 465–473.
https://doi.org/10.1016/S0140-6736(04)15495-0 PMID: 14962529
9. Gawron W, Pośpiech L, Orendorz-Fraczkowska K. An evaluation of postural stability and the effects of
middle-ear drainage on vestibulo-spinal reflexes of children with chronic otitis media with effusion. Int J
Pediatr Otorhinolaryngol. 2004; 68: 1175–1179. https://doi.org/10.1016/j.ijporl.2004.03.017 PMID:
15302148
10. Cohen H, Friedman EM, Lai D, Pellicer M, Duncan N, Sulek M. Balance in children with otitis media with
effusion. Int J Pediatr Otorhinolaryngol. 1997; 42: 107–115. https://doi.org/10.1016/s0165-5876(97)
00113-4 PMID: 9692620
11. Roberts J, Hunter L, Gravel J, Rosenfeld R, Berman S, Haggard M, et al. Otitis media, hearing loss, and
language learning: controversies and current research. J Dev Behav Pediatr. 2004; 25: 110–122.
https://doi.org/10.1097/00004703-200404000-00007 PMID: 15083134
12. Klausen O, Møller P, Holmefjord A, Reisaeter S, Asbjørnsen A. Lasting effects of otitis media with effu-
sion on language skills and listening performance. Acta Otolaryngol Suppl. 2000; 543: 73–76. https://
doi.org/10.1080/000164800454026 PMID: 10908983
13. Rovers MM, Straatman H, Ingels K, Wilt G-J van der, Broek P van den, Zielhuis GA. The Effect of Venti-
lation Tubes on Language Development in Infants With Otitis Media With Effusion: A Randomized Trial.
Pediatrics. 2000; 106: e42–e42. https://doi.org/10.1542/peds.106.3.e42 PMID: 10969126
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 12 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
14. Browning GG, Rovers MM, Williamson I, Lous J, Burton MJ. Grommets (ventilation tubes) for hearing
loss associated with otitis media with effusion in children. Cochrane Database of Systematic Reviews.
2010 [cited 24 May 2022]. https://doi.org/10.1002/14651858.CD001801.pub3 PMID: 20927726
15. Rosenfeld RM, Tunkel DE, Schwartz SR, Anne S, Bishop CE, Chelius DC, et al. Clinical Practice Guide-
line: Tympanostomy Tubes in Children (Update). Otolaryngol Head Neck Surg. 2022; 166: S1–S55.
https://doi.org/10.1177/01945998211065662 PMID: 35138954
16. Zumach A, Gerrits E, Chenault M, Anteunis L. Long-term effects of early-life otitis media on language
development. J Speech Lang Hear Res. 2010; 53: 34–43. https://doi.org/10.1044/1092-4388(2009/08-
0250) PMID: 19635942
17. Bisgaard H, Vissing NH, Carson CG, Bischoff AL, Følsgaard NV, Kreiner-Møller E, et al. Deep pheno-
typing of the unselected COPSAC2010 birth cohort study. Clin Exp Allergy. 2013; 43: 1384–1394.
https://doi.org/10.1111/cea.12213 PMID: 24118234
18. Bjarnadóttir E, Stokholm J, Chawes B, Thorsen J, Mora-Jensen A-RC, Deleuran M, et al. Determinants
of Neurodevelopment in Early Childhood—Results from the Copenhagen Prospective Studies on
Asthma in Childhood (COPSAC2010) Mother-Child Cohort. Acta Paediatr. 2019. https://doi.org/10.
1111/apa.14753 PMID: 30748036
19. Jerger J. Clinical Experience With Impedance Audiometry. Archives of Otolaryngology. 1970; 92: 311–
324. https://doi.org/10.1001/archotol.1970.04310040005002 PMID: 5455571
20. Lous J, Ryborg CT, Damsgaard JJ, Munck AP. Tympanometry in general practice: use, problems and
solutions. Family Practice. 2012; 29: 726–732. https://doi.org/10.1093/fampra/cms045 PMID:
22850248
21. Andersen TF, Madsen M, Jørgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Regis-
ter. A valuable source of data for modern health sciences. Dan Med Bull. 1999; 46: 263–268. PMID:
10421985
22. Andersen JS, Olivarius NDF, Krasnik A. The Danish National Health Service Register. Scand J Public
Health. 2011; 39: 34–37. https://doi.org/10.1177/1403494810394718 PMID: 21775348
23. Pedersen CB, Gøtzsche H, Møller JO, Mortensen PB. The Danish Civil Registration System. A cohort
of eight million persons. Dan Med Bull. 2006; 53: 441–449. PMID: 17150149
24. Frankenburg W, Dodds J. The Denver developmental assessment (Denver II). Denver: University of
Colorado Medical School; 1990.
25. Wijnhoven TM, de Onis M, Onyango AW, Wang T, Bjoerneboe G-EA, Bhandari N, et al. Assessment of
gross motor development in the WHO Multicentre Growth Reference Study. Food Nutr Bull. 2004; 25:
S37–45. https://doi.org/10.1177/15648265040251S105 PMID: 15069918
26. Casselbrant ML, Furman JM, Rubenstein E, Mandel EM. Effect of otitis media on the vestibular system
in children. Ann Otol Rhinol Laryngol. 1995; 104: 620–624. https://doi.org/10.1177/
000348949510400806 PMID: 7639471
27. Bleses D, Vach W, Slott M, Wehberg S, Thomsen P, Madsen TO, et al. The Danish Communicative
Developmental Inventories: validity and main developmental trends. J Child Lang. 2008; 35: 651–669.
https://doi.org/10.1017/S0305000907008574 PMID: 18588718
28. Højen A, Bleses D, Jensen P, Dale PS. Patterns of educational achievement among groups of immi-
grant children in Denmark emerge already in preschool second-language and preliteracy skills. Applied
Psycholinguistics. 2019; 40: 853–875. https://doi.org/10.1017/S0142716418000814
29. Bayley, N. Bayley Scales of Infant and Toddler Development (Third edition),Administration Manual.
Harcourt Assessment. San Antonio, TX; 2006.
30. Zhang Y, Xu M, Zhang J, Zeng L, Wang Y, Zheng QY. Risk factors for chronic and recurrent otitis
media-a meta-analysis. PLoS ONE. 2014; 9: e86397. https://doi.org/10.1371/journal.pone.0086397
PMID: 24466073
31. Keyhani S, Kleinman LC, Rothschild M, Bernstein JM, Anderson R, Simon M, et al. Clinical characteris-
tics of New York City children who received tympanostomy tubes in 2002. Pediatrics. 2008; 121: e24–
33. https://doi.org/10.1542/peds.2007-0623 PMID: 18166541
32. Koutra K, Chatzi L, Roumeliotaki T, Vassilaki M, Giannakopoulou E, Batsos C, et al. Socio-demographic
determinants of infant neurodevelopment at 18 months of age: Mother-Child Cohort (Rhea Study) in
Crete, Greece. Infant Behav Dev. 2012; 35: 48–59. https://doi.org/10.1016/j.infbeh.2011.09.005 PMID:
22018719
33. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical
Computing, Vienna, Austria. 2018. Available: https://www.R-project.org/.
34. Stacklies W, Redestig H, Scholz M, Walther D, Selbig J. pcaMethods—a bioconductor package provid-
ing PCA methods for incomplete data. Bioinformatics. 2007; 23: 1164–1167. https://doi.org/10.1093/
bioinformatics/btm069 PMID: 17344241
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 13 / 14
PLOS ONE Middle ear effusion, ventilation tubes and neurological development in childhood
35. Venables WN, Ripley BD. Modern Applied Statistics with S. Fourth. New York: Springer; 2002. Avail-
able: http://www.stats.ox.ac.uk/pub/MASS4
36. Wickham H. ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag New York; 2016. Available:
https://ggplot2.tidyverse.org
37. Pedersen TL. ggforce: Accelerating “ggplot2.” 2019. Available: https://CRAN.R-project.org/package=
ggforce
38. Brennan -Jones Christopher G., Whitehouse AJO, Calder SD, Costa CD, Eikelboom RH, Swanepoel
DW, et al. Does Otitis Media Affect Later Language Ability? A Prospective Birth Cohort Study. Journal
of Speech, Language, and Hearing Research. 2020; 63: 2441–2452. https://doi.org/10.1044/2020_
JSLHR-19-00005 PMID: 32539591
39. Vissing NH, Chawes BL, Rasmussen MA, Bisgaard H. Epidemiology and Risk Factors of Infection in
Early Childhood. Pediatrics. 2018; 141. https://doi.org/10.1542/peds.2017-0933 PMID: 29794229
40. Christensen ED, Hjelmsø MH, Thorsen J, Shah S, Redgwell T, Poulsen CE, et al. The developing air-
way and gut microbiota in early life is influenced by age of older siblings. Microbiome. 2022; 10: 106.
https://doi.org/10.1186/s40168-022-01305-z PMID: 35831879
41. Christensen ED, Thorsen J, Stokholm J, Pedersen TM, Brix S, Krogfelt KA, et al. Early life bacterial air-
way colonization, local immune mediator response and risk of otitis media. J Med Microbiol. 2020; 69:
1124–1131. https://doi.org/10.1099/jmm.0.001227 PMID: 32597749
42. Casselbrant ML, Villardo RJM, Mandel EM. Balance and otitis media with effusion. Int J Audiol. 2008;
47: 584–589. https://doi.org/10.1080/14992020802331230 PMID: 18821228
43. Simpson SA, Thomas CL, van der Linden MK, Macmillan H, van der Wouden JC, Butler C. Identification
of children in the first four years of life for early treatment for otitis media with effusion. Cochrane Data-
base Syst Rev. 2007; CD004163. https://doi.org/10.1002/14651858.CD004163.pub2 PMID: 17253499
44. Paradise JL, Dollaghan CA, Campbell TF, Feldman HM, Bernard BS, Colborn DK, et al. Otitis media
and tympanostomy tube insertion during the first three years of life: developmental outcomes at the age
of four years. Pediatrics. 2003; 112: 265–277. https://doi.org/10.1542/peds.112.2.265 PMID: 12897272
45. Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Effect of early
or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at
the age of three years. N Engl J Med. 2001; 344: 1179–1187. https://doi.org/10.1056/
NEJM200104193441601 PMID: 11309632
46. Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Rockette HE, Pitcairn DL, et al. Tympanost-
omy tubes and developmental outcomes at 9 to 11 years of age. N Engl J Med. 2007; 356: 248–261.
https://doi.org/10.1056/NEJMoa062980 PMID: 17229952
47. Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Early versus
delayed insertion of tympanostomy tubes for persistent otitis media: developmental outcomes at the
age of three years in relation to prerandomization illness patterns and hearing levels. Pediatr Infect Dis
J. 2003; 22: 309–314. https://doi.org/10.1097/01.inf.0000059764.77704.55 PMID: 12690269
48. Da Costa C, Eikelboom R h., Jacques A, Swanepoel D w., Whitehouse A j. o., Jamieson S e., et al.
Does otitis media in early childhood affect later behavioural development? Results from the Western
Australian Pregnancy Cohort (Raine) Study. Clinical Otolaryngology. 2018; 43: 1036–1042. https://doi.
org/10.1111/coa.13094 PMID: 29495111
49. Bleses D, Vach W, Slott M, Wehberg S, Thomsen P, Madsen TO, et al. Early vocabulary development
in Danish and other languages: a CDI-based comparison. J Child Lang. 2008; 35: 619–650. https://doi.
org/10.1017/S0305000908008714 PMID: 18588717
50. Pedersen TM, Mora-Jensen A-RC, Waage J, Bisgaard H, Stokholm J. Incidence and Determinants of
Ventilation Tubes in Denmark. PLoS ONE. 2016; 11: e0165657. https://doi.org/10.1371/journal.pone.
0165657 PMID: 27875554
PLOS ONE | https://doi.org/10.1371/journal.pone.0280199 January 13, 2023 14 / 14
You might also like
- Adenoids and Diseased Tonsils Their Effect on General IntelligenceFrom EverandAdenoids and Diseased Tonsils Their Effect on General IntelligenceNo ratings yet
- Early Signs of Autism in Toddlers - A Follow Up StudyDocument10 pagesEarly Signs of Autism in Toddlers - A Follow Up StudyLu MoreiraNo ratings yet
- Early Life Predictors of IntelligenceDocument15 pagesEarly Life Predictors of IntelligenceRobert WardNo ratings yet
- PhilippDocument15 pagesPhilippLATERA TAGESUNo ratings yet
- Journal Reading2 PDFDocument9 pagesJournal Reading2 PDFanggoroNo ratings yet
- Chronic Effects of Pediatric Ear Infections On Postural StabilityDocument6 pagesChronic Effects of Pediatric Ear Infections On Postural StabilityFajar SutrisnaNo ratings yet
- Youth Perspective On Pulmonary Tuberculosis Parent's CareDocument7 pagesYouth Perspective On Pulmonary Tuberculosis Parent's CareIJPHSNo ratings yet
- Indoor and Outdoor SmokingDocument6 pagesIndoor and Outdoor SmokingyuliaevitasariNo ratings yet
- Journal Reading CP Dan PneumoniaDocument14 pagesJournal Reading CP Dan PneumoniaNisaNo ratings yet
- 1 s2.0 S0165587617300812 MainDocument8 pages1 s2.0 S0165587617300812 MainFrancisca GarcíaNo ratings yet
- Andersson 2018Document7 pagesAndersson 2018FernandaPïlapañaNo ratings yet
- Medicina IpossiaDocument13 pagesMedicina IpossiaAlbeNo ratings yet
- Ni Hms 804361Document11 pagesNi Hms 804361Makhda Nurfatmala LubisNo ratings yet
- Reference Values For Respiratory Events in Overnight Polygraphy FromDocument5 pagesReference Values For Respiratory Events in Overnight Polygraphy FromJhonatan Mata ANo ratings yet
- Communication Development in Children Who Receive The Cochlear Implant Younger Than 12 Months Risks Versus BenefitsDocument9 pagesCommunication Development in Children Who Receive The Cochlear Implant Younger Than 12 Months Risks Versus BenefitsChris SakeNo ratings yet
- JR Ortho 1Document7 pagesJR Ortho 1Putri HandayaniNo ratings yet
- Deformidad Craneal y Desarrollo MotorDocument9 pagesDeformidad Craneal y Desarrollo MotordianareinaNo ratings yet
- (2021) Correlates of Inadequate Sleep Health Among Primary School ChildrenDocument12 pages(2021) Correlates of Inadequate Sleep Health Among Primary School ChildrenFabian Opazo DelgadoNo ratings yet
- Nej M 200104193441601Document9 pagesNej M 200104193441601Tri Rahma Yani YawatiNo ratings yet
- Caries - Oral Health - Quality Life of 3a.lima2019Document24 pagesCaries - Oral Health - Quality Life of 3a.lima2019Haydee Concepcion Romero CuicaNo ratings yet
- Wa0002Document4 pagesWa0002ninaNo ratings yet
- Carolina Marpaung - Maurits K. A. Van Selms - Frank LobbezooDocument8 pagesCarolina Marpaung - Maurits K. A. Van Selms - Frank LobbezooMarco Saavedra BurgosNo ratings yet
- Pone 0269706Document13 pagesPone 0269706Meidita Annisa PurmanNo ratings yet
- Kulkarni2018 PDFDocument7 pagesKulkarni2018 PDFtooba uroojNo ratings yet
- Pone 0272262Document12 pagesPone 0272262Marco Saavedra BurgosNo ratings yet
- Level of Exposure To Childhood Tuberculosis in Household Contacts With Adult Pulmonary TuberculosisDocument6 pagesLevel of Exposure To Childhood Tuberculosis in Household Contacts With Adult Pulmonary Tuberculosisdapajiangu asniNo ratings yet
- Pzab 177Document10 pagesPzab 177LORENZO GABRIEL BANAYONo ratings yet
- The Impact of Cosleeping Less Than 6 Months On Childrens Anxiety Oral Habits and Malocclusion in A Spanish Sample Between 2 and 5 Years Old A Cross Sectional StudyDocument6 pagesThe Impact of Cosleeping Less Than 6 Months On Childrens Anxiety Oral Habits and Malocclusion in A Spanish Sample Between 2 and 5 Years Old A Cross Sectional StudyRifqiyanti IsmiNo ratings yet
- Association Between Endocrine Diseases and Serous Otitis Media in ChildrenDocument4 pagesAssociation Between Endocrine Diseases and Serous Otitis Media in Childrengaluh muftiNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- The Effects of Orofacial Myofunctional Therapy On Children With OSAHS's Craniomaxillofacial Growth: A Systematic ReviewDocument15 pagesThe Effects of Orofacial Myofunctional Therapy On Children With OSAHS's Craniomaxillofacial Growth: A Systematic Reviewpj.krzeszewskaNo ratings yet
- Ferhm Effectiveness of Adenotonsillectomy Vs Watchful Waiting in Young ChildrenDocument17 pagesFerhm Effectiveness of Adenotonsillectomy Vs Watchful Waiting in Young Childrendanielesantos.202019No ratings yet
- Parental Education and Inequalities in Child MortaDocument13 pagesParental Education and Inequalities in Child MortaCláudia SilvaNo ratings yet
- Association Between Endocrine Diseases and Serous Otitis Media in ChildrenDocument4 pagesAssociation Between Endocrine Diseases and Serous Otitis Media in Childrengaluh muftiNo ratings yet
- Risk Factors of Hearing Loss in Children Under 10 Years of Age - A Clinical Study in A Tertiary Care CentreDocument6 pagesRisk Factors of Hearing Loss in Children Under 10 Years of Age - A Clinical Study in A Tertiary Care CentreIJAR JOURNALNo ratings yet
- Neurodevelopmental Outcomes of Preterm Infants: A Recent Literature ReviewDocument6 pagesNeurodevelopmental Outcomes of Preterm Infants: A Recent Literature ReviewJyotirmayeeNo ratings yet
- Accepted Manuscript: Seminars in Fetal and Neonatal MedicineDocument47 pagesAccepted Manuscript: Seminars in Fetal and Neonatal MedicineGiiszs AlvarezNo ratings yet
- Prevalence of Sleep Bruxism and Associated Factors in Tanta Preschool ChildrenDocument8 pagesPrevalence of Sleep Bruxism and Associated Factors in Tanta Preschool ChildrenChristiana TomescuNo ratings yet
- Neuro J 1Document11 pagesNeuro J 1Anonymous CtjSRA4No ratings yet
- 2012 Parner Etal AnnalsofEpidemiologDocument8 pages2012 Parner Etal AnnalsofEpidemiologV_FreemanNo ratings yet
- Profile of Detection and Intervention in Children With Congenital Deafness in Audiology Clinic Dr. Soetomo HospitalDocument1 pageProfile of Detection and Intervention in Children With Congenital Deafness in Audiology Clinic Dr. Soetomo Hospitalelman jokoNo ratings yet
- Effect of Infant Prematurity On Auditory Brainstem Response at Preschool AgeDocument8 pagesEffect of Infant Prematurity On Auditory Brainstem Response at Preschool AgeHanum AmeliaNo ratings yet
- PREMM: Preterm Early Massage by The Mother: Protocol of A Randomised Controlled Trial of Massage Therapy in Very Preterm InfantsDocument12 pagesPREMM: Preterm Early Massage by The Mother: Protocol of A Randomised Controlled Trial of Massage Therapy in Very Preterm InfantsLeisa A PNo ratings yet
- Lodha 2014Document12 pagesLodha 2014madhuNo ratings yet
- Neurodevelopmental Aspects and Cortical AuditoryMaturation in Children With Cochlear ImplantsDocument10 pagesNeurodevelopmental Aspects and Cortical AuditoryMaturation in Children With Cochlear ImplantsneculavNo ratings yet
- BelgicaDocument43 pagesBelgicaAlvaro Bejarano MartinNo ratings yet
- Paulsson2019 Article TheImpactOfPrematureBirthOnDenDocument7 pagesPaulsson2019 Article TheImpactOfPrematureBirthOnDenBanyu علي تقويم BiruNo ratings yet
- Breastfeeding and Risk of Febrile Seizures in Infants The - 2019 - Brain and deDocument9 pagesBreastfeeding and Risk of Febrile Seizures in Infants The - 2019 - Brain and deSunita ChayalNo ratings yet
- 23 OSAS Kids PDFDocument10 pages23 OSAS Kids PDFyafetNo ratings yet
- Effects of Rapid Palatal Expansion On The Upper Airway SpaceDocument11 pagesEffects of Rapid Palatal Expansion On The Upper Airway SpacevenancioNo ratings yet
- Hearing Status of Children Under Five Years Old in Jatinangor DistrictDocument5 pagesHearing Status of Children Under Five Years Old in Jatinangor DistricterickNo ratings yet
- Paediatric Epilepsy Research Annual Report 2011Document16 pagesPaediatric Epilepsy Research Annual Report 2011meenakshi.r.agrawalNo ratings yet
- Hearing Thresholds in Young Children With Otitis Media With Effusion With and Without Cleft PalateDocument8 pagesHearing Thresholds in Young Children With Otitis Media With Effusion With and Without Cleft PalatePutra WaspadaNo ratings yet
- Prevalence of Malocclusion in Children With Sleep Disordered BreathingDocument4 pagesPrevalence of Malocclusion in Children With Sleep Disordered BreathingMu'taz ArmanNo ratings yet
- Association Between Endocrine Diseases and Serous Otitis Media in ChildrenDocument4 pagesAssociation Between Endocrine Diseases and Serous Otitis Media in Childrencharles indraNo ratings yet
- Bassler 2018 Ensayo CohorteDocument10 pagesBassler 2018 Ensayo Cohortewisdom loverNo ratings yet
- Scherer Et Al. - Mental Health Support For Children and Adolescents With Hearing LossDocument11 pagesScherer Et Al. - Mental Health Support For Children and Adolescents With Hearing LossPablo VasquezNo ratings yet
- Articulo NeurocienciasDocument37 pagesArticulo NeurocienciasSaul PsiqNo ratings yet
- ORTODONCIAchildren 10 00176Document11 pagesORTODONCIAchildren 10 00176EstreLLA ValenciaNo ratings yet
- Music Therapy For Preterm Infants and Their Parents: A Cluster-Randomized Controlled Trial ProtocolDocument24 pagesMusic Therapy For Preterm Infants and Their Parents: A Cluster-Randomized Controlled Trial ProtocolDaniele PendezaNo ratings yet
- EULAR Recommendations For The Management of Rheumatoid Arthritis With Synthetic and Biological Disease-Modifying Antirheumatic Drugs: 2019 UpdateDocument15 pagesEULAR Recommendations For The Management of Rheumatoid Arthritis With Synthetic and Biological Disease-Modifying Antirheumatic Drugs: 2019 UpdateZeeshan AhmadNo ratings yet
- Jurnal 02 PDFDocument10 pagesJurnal 02 PDFMichel BetyNo ratings yet
- Journal Pone 0280199 PDFDocument10 pagesJournal Pone 0280199 PDFMichel BetyNo ratings yet
- LSIT 2017Document2 pagesLSIT 2017Michel BetyNo ratings yet
- 1473 The Bohemian ThrustDocument8 pages1473 The Bohemian ThrustRichard TonsingNo ratings yet
- Handwashing Poster A4Document1 pageHandwashing Poster A4kaduwd100% (2)
- All in One...Document261 pagesAll in One...Dr. Mahmoud Tawfik ElSorady100% (1)
- Updated PPT Surgical Hand WashingDocument13 pagesUpdated PPT Surgical Hand WashingInsatiable CleeNo ratings yet
- LA Times - 1708Document32 pagesLA Times - 1708JESUS YOBALNo ratings yet
- Listing of Medical Institutions For General InquiriesDocument2 pagesListing of Medical Institutions For General InquiriesSania M. ChoudhryNo ratings yet
- Nonextraction Treatment With Begg TechniqueDocument14 pagesNonextraction Treatment With Begg TechniqueSyed Mohammad Osama AhsanNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- Full Download Test Bank For Paramedic Care Principles and Practice Volume 1 5th Edition Bryan e Bledsoe PDF Full ChapterDocument36 pagesFull Download Test Bank For Paramedic Care Principles and Practice Volume 1 5th Edition Bryan e Bledsoe PDF Full Chapterkentcarsonfxivk96% (23)
- Central Directory Individuals BasicDocument3,755 pagesCentral Directory Individuals BasicNaveenJainNo ratings yet
- Alps-Our Recent Projects and List of Clients - 2022Document2 pagesAlps-Our Recent Projects and List of Clients - 2022Alps EngineeringNo ratings yet
- About The Applicant: Applicant Name: Post Applied ForDocument3 pagesAbout The Applicant: Applicant Name: Post Applied ForBilal Khan MarwatNo ratings yet
- Continuation of Knerr's Repertory-Working Methods, Merits & QuestionsDocument10 pagesContinuation of Knerr's Repertory-Working Methods, Merits & QuestionsDrNaveen Singh Rajpurohit KaduNo ratings yet
- STEM12 Group2 PETA1Document21 pagesSTEM12 Group2 PETA1Shaine Louisse B. EmNo ratings yet
- Dentists in Kansas CityDocument3 pagesDentists in Kansas CityHamza Naeem KhanNo ratings yet
- Sample NGO OrganogramDocument2 pagesSample NGO OrganogramOjonimi AdegbeNo ratings yet
- Industrial Pharmacy 2 2021 Solution For 2 Marks Most Important QuestionsDocument20 pagesIndustrial Pharmacy 2 2021 Solution For 2 Marks Most Important QuestionsTushar PrajapatiNo ratings yet
- Brazil Anvisa RDC 37 2015 Labeling Rubber Latex enDocument1 pageBrazil Anvisa RDC 37 2015 Labeling Rubber Latex enElaine NascimentoNo ratings yet
- Suture BootiesDocument1 pageSuture Bootiespatrickkalmeida6565No ratings yet
- Reading ListDocument1 pageReading ListShaikh TahiraNo ratings yet
- Checklist For The VS Measurement (TPR and BP) A. Temperature A.1. Axillary Temperature (Digital Thermometer) Done Needs PracticeDocument3 pagesChecklist For The VS Measurement (TPR and BP) A. Temperature A.1. Axillary Temperature (Digital Thermometer) Done Needs PracticeCyrillNo ratings yet
- Daftar Harga JuliDocument3 pagesDaftar Harga JuliRomandaniNo ratings yet
- Assignment Unit ConversionDocument1 pageAssignment Unit ConversionDanisha JohansyahNo ratings yet
- Catheterization: NCM 107 LabDocument4 pagesCatheterization: NCM 107 LabCatherine PradoNo ratings yet
- RMA HP Footprint 02.02.2021 NamibiaDocument14 pagesRMA HP Footprint 02.02.2021 NamibiaPerera KusalNo ratings yet
- PMH 2017PublicSectorCompensationDisclosureReport Aug27 2018Document43 pagesPMH 2017PublicSectorCompensationDisclosureReport Aug27 2018Vikranth DNo ratings yet
- Dentist FormDocument2 pagesDentist FormkianmiguelNo ratings yet
- Specimen Handling, I. Procedure For Receipt of Specimen and RequestDocument6 pagesSpecimen Handling, I. Procedure For Receipt of Specimen and RequestGretchel PontilarNo ratings yet
- Utkal University: Public Health Surveillance & ResearchDocument6 pagesUtkal University: Public Health Surveillance & Researchsmruti ranjanNo ratings yet
- E.O. No-02-2022 BadacDocument4 pagesE.O. No-02-2022 BadacAnnie IgnacioNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)