Professional Documents
Culture Documents
Prevalencia
Uploaded by
ANA MILENA FERRUCHO AGUILAROriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prevalencia
Uploaded by
ANA MILENA FERRUCHO AGUILARCopyright:
Available Formats
Ophthalmic Epidemiology
ISSN: 0928-6586 (Print) 1744-5086 (Online) Journal homepage: http://www.tandfonline.com/loi/iope20
Pterygium: prevalence, demography and risk
factors
Seang-Mei Saw & Donald Tan
To cite this article: Seang-Mei Saw & Donald Tan (1999) Pterygium: prevalence, demography and
risk factors, Ophthalmic Epidemiology, 6:3, 219-228, DOI: 10.1076/opep.6.3.219.1504
To link to this article: https://doi.org/10.1076/opep.6.3.219.1504
Published online: 08 Jul 2009.
Submit your article to this journal
Article views: 225
Citing articles: 76 View citing articles
Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=iope20
Review article
Ophthalmic Epidemiology Pterygium: prevalence, demography and
0928-6586/99/US$ 15.00
risk factors
Ophthalmic Epidemiology
– 1999, Vol. 6, No. 3, Seang-Mei Saw1
pp. 219-228
© Æolus Press 1999 Donald Tan2
Accepted 11 September 1998 1
Department of Community, Occupational & Family Medicine,
National University of Singapore, and
2
Singapore National Eye Centre, Singapore
Abstract Pterygium is not just a degenerative disease, but may be Correspondence and
a proliferative disorder of the ocular surface. The etiology of pterygia reprint requests to:
has intrigued researchers for centuries. Several surveys have consis- Dr. Seang-Mei Saw
tently shown that countries nearer the equator have higher rates of Dept. Community, Occupational
and Family Medicine
pterygia. A possible reason for this geographic variation is that (ultra-
Faculty of Medicine, MD3
violet) UV B light may be a risk factor for the development of pterygia.
National Univ. of Singapore
UV B radiation may induce cellular changes in the medial limbus of 16 Medical Drive
the cornea. Several case-control and cross-sectional studies have attempt- Singapore 117597
ed to accurately quantify UV light exposure and document its relation- Tel.: +65 874 4976
ship with pterygia. Genetic attributes and other lifestyle behaviors may Fax: +65 779 1489
also contribute to the development of pterygia. However, further re- E-mail: cofsawsm@nus.edu.sg
search efforts are needed to enable us to better understand the relative
contribution of the different risk factors and how each risk factor may
be linked to pterygium formation. In addition, the underlying mecha-
nism of the effects of UV radiation needs to be further evaluated. By
readdressing these unresolved issues in a newly proposed epidemiolog-
ical study, new measures might be taken to reduce incidences and
improve clinical managements of diseases, in addition to preventing
UV exposure by eliminating other contributory factors. Meanwhile,
preventive measures such as protection of the eyes by the wearing of
sunglasses with UV B protective lenses and brimmed hats outdoors are
recommended.
Key words Pterygium; ultraviolet radiation; risk factors; epidemi-
ology
Introduction Pterygium management dates back to the time that
Susruta recorded the removal of a pterygium lesion in 1000 BC.1 Even
in ancient times, the recurrent nature of pterygium after surgical re-
moval was noted. Rosenthal remarked that pterygium lesions have been
“incised, removed, split, transplanted, excised, cauterized, grafted, in-
verted, galvanized, heated, dissected, rotated, coagulated, repositioned,
and irradiated.” Also, he adds that it has been “analyzed statistically,
geographically, etiologically, microscopically, and chemically, yet it
Epidemiology of pterygium 219
3212.p65 219 7/6/99, 8:51 PM
grows onward, primarily and secondarily. We look with interest to its
future”.2 Pterygium is one of the most common eye conditions and
pterygium surgery is widely practised. In 1965, Cameron in his book
‘Pterygium throughout the world’ reviewed the geographic distribution,
risk factors and management of pterygium.3 However, little is known
about the prevalence of pterygium based on population-based surveys
and the relative importance of the different risk factors that contribute
to the onset and recurrence of pterygium. The objective of this review
is to provide an update of the prevalence, demography and pathogen-
esis of pterygia and how the observed risk factors may relate to the
etiology of the disease. Important issues that will be addressed are: 1)
Pterygium is not just a degenerative but a proliferative disease; 2) The
underlying mechanism for the fact that ultraviolet radiation leads to
pterygium formation; 3) The role of genetic and other environmental
factors in pterygium pathogenesis; 4) Directions for the conduct of
further epidemiologic studies that may causally link potential risk fac-
tors to the development of pterygium.
The histology and pathogenesis of pterygium A ptery-
gium (the Greek word pterygos means ‘wing’) has been described clas-
sically as a degenerative or inflammatory process. A pterygium may be
derived from a pingueleculum which is a yellowish growth on the
corneal limbus.1,4 There are several theories on the occurrence of ptery-
gium, which include chronic infection and thrombosis of the conjunc-
tival veins resulting in the development of pterygia.5,6 However, these
theories do not provide a good explanation for the wing-like shape and
location of pterygia. Electron microscopic findings by Cameron showed
that pterygium may be due to invasion of the cornea by subconjunctival
fibroblasts.3,7 There may be a pterygium angiogenesis factor that at-
tracts blood vessels onto the cornea.4 Vessel ingrowth and the develop-
ment of pterygium may occur as a result of this factor. An immunolog-
ic mechanism may also contribute to the development of pterygium as
there is infiltration of small lymphocytes and plasma cells into the
pterygium.8 Type I hypersensitivity may also contribute to the develop-
ment of pterygium.8
More recent findings suggest that pterygia may be a proliferative
disorder rather than a degenerative process.5,6 There is new evidence to
support the claim that pterygium is a proliferative ocular condition.
Pterygia often recur after surgical excision and the treatment modalities
such as wide excision, antimitotic chemotherapy and irradiation mimic
the treatment for neoplasms. Histologic findings reveal that pterygia
may invade locally and sometimes show mild dysplasia or even carci-
noma-in-situ. Recent findings of p53 in the epithelium of pterygium
specimens is further evidence that pterygium is a growth disorder rather
than a degenerative process.9 p53 is a tumor suppressor gene that acts
as a transcription factor that activates or represses the expression of
growth controlling genes. This gene has been shown to be abnormally
expressed in a wide variety of human cancers.
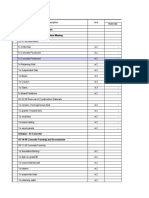
Prevalence and demography Several surveys of pterygium
eyes have been conducted in various countries (Table I). However,
220 S.M. Saw & D. Tan
3212.p65 220 7/6/99, 8:51 PM
table 1. Summary of the prevalence
Country Study Population Sample size Age Prevalence of pterygium in selected studies.
ref. no.) based ? (years) (%)
Solomon Verlee Yes 512 1 to 89 0.3
Islands (13)
South Africa Hill et al. Yes 1,519 all ages 0.5
(Transkei) (6)
Denmark Norn Yes 810 all ages 0.7
(Copenhagen) (14)
Australia Moran et al. Yes 64,314 all age 3.4 in
(12) Aborigines groups Aborigines
40,799 1.1 in
non- non-
Aborigines Aborigines
Greenland Norn et al. Yes 659 all ages 8.6
(14)
Australia Kerkenezov No 287 10 and 9.6
(New South (20) (clinic above
Wales) patients)
Jordan Norn et al. No, soldiers 127 10 and above 12
(14) and hospital
patients
most surveys are hospital or clinic-based rather than population-based
studies. Therefore, patients with asymptomatic pterygium or those who
seek advice from primary health care physicians and from practice
based ophthalmologists may not be included in such surveys. In hospi-
tal surveys, the total number of pterygium surgeries is often reported
but not pterygium cases seen at the clinic, which leads to a significant
underestimation of pterygium prevalence rates in the hospital. The age
structure of different populations may vary and age-standardized prev-
alence rates are preferred when comparing rates in different countries.
On the other hand, pterygium is an easily recognized condition and
diagnostic procedures are fairly standard across international bound-
aries.
Cameron noted that pterygium rates were higher in countries that
were hot, dusty and dry and especially in countries between 37 degrees
north and south of the Equator.3 A relative ‘pterygium belt’ may exist
where the UV radiation intensity is strongest. Most of the studies re-
viewed were a mixture of institutional surveys, community surveys and
surgical audits. The reason for this interesting geographic variation
could be that sunlight exposure may be associated with the develop-
ment of pterygium. Ringland Anderson first noticed that the prevalence
of pterygium operations was highest in the northern parts of Australia.10
A survey of pterygium operations from the main hospital in each State
in the United States of America was performed by Dimitry in 1937.11
The rate calculated was pterygium operations as a percentage of all eye
surgery. This figure varies with the pattern of operations in each hos-
Epidemiology of pterygium 221
3212.p65 221 7/6/99, 8:51 PM
pital but general comparisons of rates show that cities in the South,
including Los Angeles and New Orleans, have higher percentages (11-
13% compared to the overall average of 2.9%). We must be cautious
in the interpretation of this data as individual measurements of sunlight
exposure were not conducted.
Population-based surveys have been conducted in several countries.
In Australia, ophthalmologists examined 64,314 Aborigines, which
covers 50% of the aboriginal population, and the prevalence rate was
3.4%. In 40,799 non-aboriginal volunteers, the rate was 1.1%.12 Popu-
lation-based surveys of the islands in the Pacific Ocean show preva-
lence rates ranging from 29% in the Samoa Islands to 6.75% in the
Cocos Islands and 0.3% in the Solomon Islands.13 In South Africa, only
seven of 1519 people (0.5%) surveyed in Transkei had a pterygium
lesion.6 Only 1% of 189 Japanese in Kyoto had a pterygium in the eye
(latitude 35 degrees North).14 Examinations by Norn using a similar
apparatus showed that the prevalence of pterygium was 12% in Jordan,
9% in Greenland and 1% in Copenhagen.15,16 There have been few
population-based surveys conducted to identify the prevalence rates of
pterygia. The surveys have used different instruments to examine the
patients for pterygia and are often limited by sample size.6,15,16 Thus, it
is difficult to compare the rates of pterygia in different countries.
Other surveys have been conducted in hospitals, physician practices
and among selected occupational groups. The age-adjusted prevalence
rates for 110 male sawmill workers in Thailand was 27% compared to
2% for 164 white male sawmill workers in British Columbia.17 Hospi-
tal-based surveys show prevalence rates that vary from 31% in Lima,
Peru to 4% in the ophthalmologic department of a hospital in Kigali,
Rwanda.18,19 The prevalence of pterygia was 12.3% in several physician
practices in Brisbane, and was 9.6% in the far northern coast of New
South Wales.3,20 The heterogeneity of the study populations limit the
comparability of prevalence rates across studies. The prevalence rates
from these surveys are biased as the study population is not represen-
tative of the population as a whole. Selected population groups may
have certain characteristics leading to higher or lower rates of pterygia
than in the general population.
The prevalence of pterygium increases with age.6,12,16,21 No sex pre-
ponderance has been noted except in the non-aboriginal population of
Australia where the prevalence for women was 0.65% compared to
1.5% in men.3 There is a possibility that different sunlight exposure and
occupation patterns in males and females in certain countries may
contribute to differences in pterygium rates.
The most striking feature of the distribution of pterygium is the high-
er rates found in countries nearer the equator. However, there are still
gaps in our knowledge of the distribution of pterygium in certain parts
of the world. Population-based surveys that are a random sample of the
general population with high participation rates are needed to quantify
pterygium age-adjusted prevalence rates in countries at different lati-
tudes. It is also important that experienced ophthalmologists conduct
the clinical examinations and that uniform criteria are maintained for
diagnosis and grading.
222 S.M. Saw & D. Tan
3212.p65 222 7/6/99, 8:51 PM
Risk factors
ultraviolet radiation The major environmental risk factor for
the development of pterygium is exposure to UV light.21 Age-related
cataract, age-related macular degeneration, climatic droplet kerato-
pathy and eyelid malignancies are also postulated to be related to UV
light.22-24 Other sunlight-related conditions such as basal cell carcino-
ma, polymorphous light eruption and xeroderma pigmentosum are of-
ten associated with pterygium.21 When UV radiation is divided into UV
A (400 to 320 nm), B (320 to 290 nm), and C (290 to 100 nm) accord-
ing to the wavelength, UV A causes sun tanning, UV B causes sunburn
and skin cancer, and UV C does not reach the earth’s surface.25 The
depletion of the ozone layer in recent decades may result in increased
ultraviolet radiation and a subsequent increase in sunlight-related con-
ditions such as pterygium.26
UV light absorbed by the cornea and conjunctiva promotes cellular
damage and hence subsequent proliferation. Experiments in mice showed
that UV radiation results in degeneration of Bowman’s membrane and
epithelial hyperplasia.27 One theory proposed by Coroneo et al. is that
UV light enters from the temporal side and is focused on the nasal side
resulting in the formation of a nasal pterygium.28,29 Albedo, or reflected
solar radiation, is responsible for most of the light rays that strike the
corneal surface and is the major factor that determines focal UV B
exposure (295 to 320 nm) of the eye.
There are several theories about the mechanism whereby UV radia-
tion may result in pterygia formation. There may be a modification of
the ocular immune system which may contribute to pterygium forma-
tion. UV radiation at the medial limbus may cause a depletion of Langer-
hans cells which may result in the conjunctival cells not recognizing
the junction between the cornea and conjunctiva, leading to a growth
of conjunctival epithelium into the corneal zone.5,30 Recent evidence
indicates that pterygium is a proliferative disease and that maximum
mitosis may occur when the cornea is exposed to UV radiation. There
is evidence that the extracellular matrix of pterygia is not normal and
UV radiation may alter the synthesis of protein, resulting in degener-
ation of the limbal region. In summary, UV light may have an actinic
effect on the mitosis of cells resulting in pterygium formation.
The amount of UV light that reaches the surface of the cornea is
affected by local and external factors. Local factors such as corneal
curvature, anterior chamber depth, length of eye lashes, and ocular
prominence may determine the fall of light on the nasal portions of the
eye. The exposure to albedo UV light also varies with external factors
such as latitude, ambient conditions, reflective terrain, time of day spent
outdoors, prescription eyewear, and protective equipment such as hats.28
The reflectance of the terrain is an important determinant of UV B
radiation with the greatest reflectance from fresh snow, followed by
sand and concrete pavements.31 The average transmission for UV B
light to the cornea as measured using a radiometer32 was highest for
soft contact lenses, followed by glass spectacle lenses, hard contact
lenses and plastic spectacle lenses.
The evidence from epidemiologic studies for UV radiation as a cause
Epidemiology of pterygium 223
3212.p65 223 7/6/99, 8:51 PM
for the onset of pterygia is not conclusive. Most epidemiologic studies
do not directly measure the exposure to UV radiation in each individual
and deductions are made from selected population groups. The studies
are also limited by sample size, lack of a clear delineation of the tem-
poral relationship between UV light exposure and pterygium formation,
and the fact that potential confounders are often not examined. Several
preliminary studies have been conducted that suggest that UV light
may play a role in the pathogenesis of pterygia.
There are several observations that support the hypothesis that UV
light promotes pterygia formation. In a study by Jensen, the results
showed that pterygium usually occurs first in the dominant eye which
is held open when facing the sun.33 The non-dominant eye remains
closed and the intensity of the incident albedo radiation decreases.
Pterygium rates increase with age which may be related to the cumu-
lative effects of ultraviolet radiation.22 Another observation is that se-
lected occupations with higher exposure to UV light have higher rates
of pterygium. Occupational studies have shown that welders and saw-
mill workers have a higher prevalence of pterygium.17,34,35 A study of
217 male welders in Copenhagen showed that 57% of welders had
pingueculae and 5% had pterygium. The prevalence increased with a
higher welding exposure.35 Pterygium was also associated with certain
outdoor occupations such as stockmen, station hands, and laborers in
the Aboriginal population.36 However, other possible confounding fac-
tors were not adjusted for and direct measures of UV exposure were
not made. The exposure to UV light for different members of the same
profession may not be uniform.
For example, a higher prevalence of pterygium was noted in coun-
tries at a higher latitude and with fewer hours of sunlight per day.3 In
350 Aborigines in Australia, the odds ratio for pterygium for those
exposed to more than 9.5 hours of sunshine per day was 1.9.37 A pos-
itive correlation was also found for latitude and pterygium. A case-
control study by Darrell showed a higher frequency of pterygium in
veterans living in the South of the United States compared to the North,
in those with outdoor occupations, and in rural areas.38 Deductions may
be made from ecologic studies in which the prevalence of pterygium in
64,314 Aborigines in Australia was 3.4% compared to 1.1% in 40,799
non-Aborigines.12 Male and female aborigines in Australia spend more
time outdoors compared to their non-aboriginal counterparts. Selection
bias may have occurred as the non-aboriginal population was self-re-
ferred.
Accurate measurements of UV light exposure are needed to reduce
misclassification of exposure in epidemiologic studies. Often, ambient
light levels of sunlight are used as surrogates of personal ocular expo-
sure. However, only crude estimates of UV light exposure are some-
times obtained. Global UV light exposure measurements may lead to
serious errors that may distort exposure-disease relationships. More
precise estimates of ultraviolet light exposure were made in the follow-
ing studies. A study of 135 cases and 687 age-matched controls of
watermen who worked on Chesapeake Bay found a strong association
between ocular exposure to a wide band of UV radiation and ptery-
gium.21,23 The odds ratio of pterygium in those with doubling of cumu-
224 S.M. Saw & D. Tan
3212.p65 224 7/6/99, 8:51 PM
lative blue light exposure is 1.85 (1.43 to 2.38). The odds ratio for
average annual exposure to UV-B light in the upper quartile was 3.06
(1.77-5.31) compared to the lowest quartile and a dose-response rela-
tionship was seen. A combination of interview data that combined work
and leisure time histories, history of spectacle and eyeglass wear as
well as laboratory and field measurements were made by interviewers
masked to the status of the cornea. Ocular exposure was quantified by
UV- sensitive film badges placed near the eye.39 After exposure of the
film badge to UV light, the spectrophotometer was used to measure
absorbance. A slit-lamp examination of the cornea was made to diag-
nose pterygia. In a hospital in Brisbane, in an interview study using a
standard questionnaire from the watermen study, 278 cases and a sim-
ilar number of age, sex and race matched controls were compared.40,41
The odds ratio was 44.3 for pterygium for patients living at latitude less
than 30 degrees and 14.1 for spending more than 50% of the time
outdoors in the first five years of life. However, selection bias may
have occurred as hospital controls may have different living patterns
compared to the general population.
The above studies have consistently shown a strong association of
UV light and pterygium formation. UV radiation levels may increase as
the ozone layer is gradually depleted. Despite the fact that there is a
biologically plausible model for the action of UV light, most of the
studies do not establish a well-defined temporal relationship and the
latency period, nor explore effects of the duration of UV light expo-
sure, peak exposure or cumulative exposure. To establish causality,
future studies should include a well-defined temporal sequence of events
and document the nature of the dose-response relationship. A pre-tested
and reliable questionnaire that measures ultraviolet light exposure and
other potential confounders is essential in analytic studies of the causes
of pterygia. Future cohort studies of a representative population with a
wide range of ocular exposures to UV light may provide us with valu-
able data on the incidence of pterygia in those with greater ocular
exposures to UV light compared to those with less ocular exposure. A
well-designed cohort study ideally should have a sufficient length of
follow-up to accrue a good number of new cases of pterygia and there
should be intensive efforts to decrease the number of participants who
are lost to follow-up (migrated, uncontactable, refused to participate).
A large number of subjects lost to follow-up will decrease the sample
size and introduce bias if the participants lost to follow- up have a
different exposure-disease relationship.
If the incidence of pterygium is low in the population, a case-control
design may be more efficient and the odds ratio may be used to esti-
mate the relative risk. However, a case-control study is often limited by
selection and information biases. Measures must be taken to limit the
problem of biases in such studies. Based on our present knowledge
from epidemiologic studies, we would still advise the protection of the
eyes from excessive sunlight exposure by the use of eyewear or protec-
tive clothing.
genetic factors Hereditary factors may play an important role in
the pathogenesis of pterygia. The p53 oncogene may be a possible
Epidemiology of pterygium 225
3212.p65 225 7/6/99, 8:51 PM
marker for the pterygium gene. Although case reports have described
clusters of family members with pterygium,42-44 the importance of he-
reditary factors in pterygium onset is still unknown. An interesting
study that was conducted to examine familial risk factors is a hospital-
based case-control study of 100 pterygium cases and 100 controls in
Australia. The odds ratio for a family history of pterygium was 4.7545
However, no eye examination of family members was conducted.
Another clue that genetics may play a role is that pterygium is associ-
ated with several syndromes such as the multiple pterygium syndrome
(autosomal dominant or recessive). 46 Nevertherless, there is little evi-
dence from twin studies, migration studies or segregation analysis stud-
ies on the exact nature of genetic inheritance. Familial clusters of the
disease may also arise as a result of a common environment or occu-
pation. Further research is needed to evaluate the nature of any genetic
transmission or interaction of genetic and environmental factors.
dry eyes It is possible that abnormalities in the tear film may cause
drying and predisposition to new growth. Thus, proliferation of cells
leading to the formation of pterygia may occur. The evidence for dry
eyes as a causative agent for pterygia is, however, limited to a few
studies. Aborigines with pterygium were found to have a disruption of
the marginal tear strip compared to aborigines without pterygium.47 A
hospital case-control study in Johannesburg did not show any correla-
tion between dry eyes in the Bantu and pterygium.48 However, only 43
cases and 23 controls were evaluated. When the tear film break-up time
(BUT) was studied in 56 eyes of patients with pterygium and compared
with 50 normal eyes in India, there was a significantly reduced BUT in
cases with pterygium.49 Biedner et al. found that in 60 patients with
unilateral pterygia that were examined, there was no Schirmer test
evidence for dryness.50 However, in this study, there were no compar-
isons with a control group.
other environmental risk factors The attributable risk of pte-
rygium for UV light exposure is not known. Are there other factors that
may contribute independently or interact with UV light exposure? Oth-
er observations have suggested that low humidity or microtrauma from
particulate material such as smoke or sand may play a role.21,48 The role
of genetics is not well explored. Researchers have raised the question
of whether dietary deficiencies may contribute to the formation of ptery-
gium.51 In a small case-control study by Taylor, alcohol intake, previ-
ous ocular trauma and severity of trachoma were not related to ptery-
gium.52 Other studies have raised the possibility of HPV infection
contributing to the development of pterygium.53 At present, there is no
proven evidence from epidemiologic studies on other possible genetic
or environmental risk factors for pterygium.
Conclusion Pterygium is one of the most obvious eye disorders
and the removal of pterygium one of the most commonly performed
operations in Asia. However, the nature and etiology of pterygia has
eluded many researchers for decades. New evidence has shown that
pterygium is a proliferative rather than just a degenerative disease. UV
226 S.M. Saw & D. Tan
3212.p65 226 7/6/99, 8:51 PM
radiation could be a major risk factor for pterygia and UV radiation
may have an actinic effect on cell mitosis resulting in pterygia forma-
tion. It is unlikely that there is a sole risk factor for pterygia and the
other possible contributing factors include age, hereditary factors, and
dry eyes. There may also be interaction between the different factors.
We would like to suggest directions for future epidemiologic research.
Population-based studies with adequate sample size would be useful in
defining the prevalence of pterygium in different countries. Future stud-
ies on the incidence of pterygium in a well-defined cohort would pro-
vide a clearer picture of the events surrounding disease onset.
Several studies over the past few decades suggest that UV radiation
may be associated with pterygium.12,21,23,29 Accurate exposure estima-
tions of ocular UV light exposure combining interview and field data
are essential to decrease the misclassification bias. Further studies would
determine whether any factors are causally related to pterygium as well
as the attributable risk of each factor. Several previous studies have
quantified sunlight exposure, which is a rather crude estimate of ultra-
violet light; thus, future studies should include accurate measures of
ultraviolet light exposure. Cohort and case-control studies with accu-
rate estimates of the various risk factors for pterygia would shed further
light on the causes of pterygia. Present evidence from case-control
studies suggests that UV B light is the predominant risk factor for
pterygium formation. Most light that reaches the eye is reflected solar
radiation (albedo). Conventional sunglasses may not protect the eye
from UV light as reflected light, which may strike the eye from the
side. Protection of the eyes by wearing wrap-around sunglasses with
UV B-absorbing lenses and brimmed hats outdoors has thus been rec-
ommended.41
References pathogenesis of pterygium. Am J 15 Norn MS. Spheroid degeneration,
1 Jaros PA, DeLuise VP. Pingueculae Ophthalmol 1984;98:225-8. pinguecula, and pterygium among
and pterygia. Surv Opthalmol 1988; 9 Tan D, Lim ASM, Goh HS, Smith DR. Arabs in the Red Sea territory, Jordan
33:41-9. The p53 tumour suppressor gene is Acta Ophthalmol 1982;60:949-54.
2 Rosenthal JW. Chronology of abnormally expressed in conjunctivae 16 Norn MS. Prevalence of pinguecula
pterygium therapy. Am J Ophthalmol of pterygium patients. Am J in Greenland and in Copenhagen and
1953;36:1601. Ophthalmol 1997;3:404-5. its relation to pterygium and spheroid
3 Cameron ME. Pterygium throughout 10 Anderson JR. A pterygium map. Acta degeneration. Acta Ophthalmol 1979;
the world. Springfield, Ill: Charles C Ophthalmol 1954;3:1631-42. 57:96-105.
Thomas, 1965. 11 Dimitry TJ. Dust factor in production 17 Detels R, Dhir SP: Pterygium. A
4 Wong WW. A hypothesis on the of pterygium. Am J Ophthalmol 1937; geographical study. Arch Ophthalmol
pathogenesis of pterygium. Ann 20:40. 1967;78:485-91.
Ophthlamol 1978;:10:303-8. 12 Moran DJ, Hollows FC. Pterygium 18 Rojas JR, Malaga H. Pterygium in
5 Kwok SL, Coroneo MT. A model for and ultraviolet radiation : A positive Lima, Peru. Ann Ophthalmol 1986;
pterygium formation. Cornea 1994; correlation. Br J Ophthalmol 1984;68: 18:147-9.
13:219-24. 343-6. 19 Forsius H, Maertens K, Fellman J.
6 Hill JC, Maske R. Pathogenesis of 13 Verlee DL. Ophthalmic survey in the Changes of the eye caused by the
pterygium. Eye 1989;3:218-26. Solomon Islands. Am J Ophthalmol climate in Rwanda, Africa. Ophthalm
7 Cameron ME. Histology of pterygium 1968;66:304. Epidemiol 1995;2:107-13.
: an electron microscopic study. Br J 14 Norn MS. Spheroid degeneration, 20 Kerkenezov N. A pterygium survey
Ophthalmol 1983;67:604-8. keratopathy, pinguecula, and of the far northcoast of New South
8 Pinkerton OD, Hokama Y, Shigemura pterygium in Japan (Kyoto). Acta Wales. Trans Ophthalmol Soc
LA. Immunologic basis for the Ophthalmol 1984;62:54-60. Australia 1956;16:110-9.
Epidemiology of pterygium 227
3212.p65 227 7/6/99, 8:51 PM
21 Coroneo MT. Pterygium as an early Ophthalmol Vis Sci 1986;27 7 :781-90. conjunctiva. J Med Genetics 1990;27 7:
indicator of ultraviolet insolation: a 32 Rosenthal FS, Bakalian AE, Taylor 392-4.
hypothesis. Br J Ophthalmol 1993;77: HR. The effect of prescription 43 McKeown CM, Harris R. An
734-9. eyewear on ocular exposure to autosomal dominant multiple
22 Taylor H, West S, Munoz B, ultraviolet radiation. Am J Publ Health pterygium syndrome. J Med Genetics
Rosenthal F, Bressler S, Bressler N. 1986;76:1216-20. 1988;25:96-103.
The long-term effects of visible light 33 Jensen OL : Pterygium, the dominant 44 Jang JD. An investigation of
on the eye. Arch Ophthalmol 1992; eye and the habit of closing one eye in aetiology and heredity of pterygium.
110:99-104. sunlight. Acta Ophthalmol 1982;60: Report of 11 cases in a family Acta
23 Taylor H, West S, Rosenthal F, Munoz 568-74. Ophthalmol 1987;65:413-6.
B, Newland HS, Emmett EA: Corneal 34 Karai I, Horiguchi S: Pterygium in 45 Booth F. Heredity in one hundred
changes associated with chronic UV welders. Br J Ophthalmol 1984;68: patients admitted for excision of
irradiation. Arch Ophthalmol 1989; 347-9. pterygia Aust NZ J Ophthalmol 1985;
107:1481-4. 35 Norn M, Franck C. Long-term changes 13:59-61.
24 Young RW. The family of sunlight- in the outer part of the eye in welders. 46 Thompson EM, Donnai D, Baraitse
related eye diseases. Optom Vis Sci Acta Ophthalmol 1991;69:382-6. M, Hall CM, Pembrey ME, Fixsen J.
1994;71:125-44. 36 Taylor HR. Climatic droplet Multiple pterygium syndrome:
25 Taylor HR, West SK, Rosenthal FS, keratopathy and pterygium Aust J evolution of the phenotype. J Med
Munoz B, Newland HS, Abbey H, Ophthalmol 1981;9:199-206. Genetics 1987;24:733-49.
Emmett EA. Effect of ultraviolet 37 Taylor HR. The prevalence and causes 47 Taylor HR. Studies on the tear film in
radiation on cataract formation. New of anterior segment disease in climatic droplet keratopathy. Arch
Engl J Med 1988;319:1429-33. Australian Aborigines in North- Ophthalmol 1980;98:86-8.
26 Ozone depletion quickens. [Editorial.] western Australia. Aust J Ophthalmol 48 Goldberg L, David R. Pterygium and
Lancet 1991;337:1132-3. 1980;8:289-301. its relationship to the dry eye in the
27 Lippincott SW, Blum HF. Neoplasms 38 Darrell RW, Bachrach CA. Pterygium Bantu. Br J Ophthalmol 1976;60:721-
and other lesions of the eye induced among veterans. Arch Ophthalmol 31.
by ultraviolet radiation in Strain A 1963;70:158. 49 Rajiv, Mithal S, Sood AK. Pterygium
mice. J Natl Cancer Inst 1943;3:545- 39 Rosenthal FS, Phoon C, Bakalian AE, and dry eye – a clinical correlation.
54. Taylor HR. The ocular dose of Ind J Ophthalmol 1991;39:15-6.
28 Coroneo MT. Albedo concentration in ultraviolet radiation to outdoor 50 Biedner B, Biger Y, Roghkoff L, et
the anterior eye : a phenomenon that workers. Invest Ophthalmol Vis Sci al, Pterygium and basic tear secretion.
locates some solar diseases. Ophthalm 1988;29:649-56. Ann Ophthalmol 1979;11:1235.
Surg 1990;20:60-6. 40 Mackenzie FD, Hirst LW, Battistutta 51 Beard HH, Dimitry TJ. Some
29 Archila EA, Arenas MC. D, Green A. Risk analysis in the observations upon the chemical
Etiopathology of pinguecula and development of pterygia. nature of pterygium. Am J
pterygium. Cornea 1995;14:543-4. Ophthlamology 1992;99:1056-61. Ophthalmol 1954;28:306.
30 Chandler JW, Cummings M, Gillette 41 Taylor HR, West SK, Rosenthal FS, et 52 Taylor HR. Aetiology of climatic
TE. Presence of Langerhans cells in al. Effect of ultraviolet radiation on droplet keratopathy and pterygium Br
central corneas of normal human cataract formation. New Engl J Med J Ophthalmol 1980;64:154-63.
infants. Invest Ophthalmol Vis Sci 1988;319:1429-33. 53 Varinli S, Varinli I, Erkisi K, Doran
1985;26:113-6. 42 Hecht F, Shoptaugh MG : Winglets of F. Human papillomavirus in
31 Sliney D. Physical factors in the eye. Dominant transmission of pterygium. Cent Afr J Med 1994;40:
cataractogenesis : ambient ultraviolet early adult pterygium of the 24-6.
radiation and temperature. Invest
228 S.M. Saw & D. Tan
3212.p65 228 7/6/99, 8:51 PM
You might also like
- Psych 1xx3 Quiz AnswersDocument55 pagesPsych 1xx3 Quiz Answerscutinhawayne100% (4)
- FacebookH Cking 1 3 (SFILEDocument10 pagesFacebookH Cking 1 3 (SFILEFitra AkbarNo ratings yet
- Pterygium 2022Document16 pagesPterygium 2022Jose A BolivarNo ratings yet
- Incidences of Pterygium by Physical Examination Using A Slit Lamp and To Find Its Association To Exposure To UV-B Rays in Outdoor Workers in A Tertiary Care HospitalDocument2 pagesIncidences of Pterygium by Physical Examination Using A Slit Lamp and To Find Its Association To Exposure To UV-B Rays in Outdoor Workers in A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Etiology of Proptosis in Children Sindhu 1998Document3 pagesEtiology of Proptosis in Children Sindhu 1998Putri Wulan SukmawatiNo ratings yet
- Clinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesDocument7 pagesClinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesRiza Haida WardhaniNo ratings yet
- Viral involvement in pterygium pathogenesisDocument5 pagesViral involvement in pterygium pathogenesisNhaNa HikmAtulNo ratings yet
- Orbital CellulitisDocument20 pagesOrbital CellulitissarahNo ratings yet
- Orbital Cellulitis 2018Document20 pagesOrbital Cellulitis 2018María Alejandra Rojas MontenegroNo ratings yet
- Comparison of Recurrence of Pterygium Following Excision by Bare Sclera Technique With and Without Mitomycin CDocument80 pagesComparison of Recurrence of Pterygium Following Excision by Bare Sclera Technique With and Without Mitomycin CShoaib AbbasNo ratings yet
- DIAGNOSIS AND MANAGEMENT OF ENDOGENOUS ENDOPHTHALMITISDocument24 pagesDIAGNOSIS AND MANAGEMENT OF ENDOGENOUS ENDOPHTHALMITISBenk Setsuna F. SeieiNo ratings yet
- Candidate Genes of High Myopia NT Fix YetDocument18 pagesCandidate Genes of High Myopia NT Fix YetFitria RizkyNo ratings yet
- Viral involvement in pterygium pathogenesisDocument14 pagesViral involvement in pterygium pathogenesisZahara FonnaNo ratings yet
- Liu 2013Document7 pagesLiu 2013YolandaNo ratings yet
- Bilateral Blindness Due To Pterygium - A Case ReportDocument3 pagesBilateral Blindness Due To Pterygium - A Case ReportDavid Al HavizNo ratings yet
- Pterigium 2Document12 pagesPterigium 2adnanalikhan72No ratings yet
- Viral Involvement in Pterygium PathogenesisDocument5 pagesViral Involvement in Pterygium PathogenesisChristianWicaksonoNo ratings yet
- Clinical Profile of Ptosis in A Tertiary Care CentreDocument5 pagesClinical Profile of Ptosis in A Tertiary Care CentreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Fungal Keratitis in Developing CountriesDocument11 pagesFungal Keratitis in Developing CountriesChikita Rizqi HanifatiNo ratings yet
- 6 SaDocument9 pages6 SaRizqi AmaliaNo ratings yet
- Experimental Eye ResearchDocument10 pagesExperimental Eye ResearchApriansyah Arfandy AzisNo ratings yet
- Ocular ToxocariasisDocument2 pagesOcular ToxocariasisEnderson UsecheNo ratings yet
- Mol S Poveda - Et - Al 2019 Pediatric - DermatologyDocument2 pagesMol S Poveda - Et - Al 2019 Pediatric - DermatologyMaria TebiesNo ratings yet
- Clinical Features and Treatment of Ocular Toxoplasmosis: AbstractDocument8 pagesClinical Features and Treatment of Ocular Toxoplasmosis: AbstractInne Budi Kusuma WardhaniNo ratings yet
- Candidate Genes of High Myopia Done1Document21 pagesCandidate Genes of High Myopia Done1Fitria RizkyNo ratings yet
- December 2017 Ophthalmic PearlsDocument2 pagesDecember 2017 Ophthalmic PearlsMEDIWAY CLINICNo ratings yet
- 1 PBDocument11 pages1 PBMega RebbekaNo ratings yet
- Acute Epiglottitis: Trends, Diagnosis and Management: Claude AbdallahDocument3 pagesAcute Epiglottitis: Trends, Diagnosis and Management: Claude AbdallahNadhilaNo ratings yet
- PterigiumDocument6 pagesPterigiumNdha SolidarityNo ratings yet
- Bilateral Congenital Toxoplasmosis Complicated by Choroidal Neo-Vessels A Case ReportDocument3 pagesBilateral Congenital Toxoplasmosis Complicated by Choroidal Neo-Vessels A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- MK in pediDocument7 pagesMK in pedifikerteadelleNo ratings yet
- The Genetics of Cataract: NEW DevelopmentsDocument2 pagesThe Genetics of Cataract: NEW DevelopmentsVidini Kusuma AjiNo ratings yet
- Anophthalmia and MicrophthalmiaDocument8 pagesAnophthalmia and MicrophthalmiaLjubomirErdoglijaNo ratings yet
- Epidemiology of Keratoconus Symposium: KeratoconusDocument2 pagesEpidemiology of Keratoconus Symposium: KeratoconusdechastraNo ratings yet
- Systemic Disorders Associated With Peripheral Corneal UlcerationDocument4 pagesSystemic Disorders Associated With Peripheral Corneal UlcerationYoga KharismaNo ratings yet
- Infectious Endophthalmitis After: CataractDocument6 pagesInfectious Endophthalmitis After: CataractSurendar KesavanNo ratings yet
- Patophysiology of Endometriosis PDFDocument9 pagesPatophysiology of Endometriosis PDFHanna LibrianaNo ratings yet
- Prevention Ulcus CornealDocument7 pagesPrevention Ulcus Cornealalifah syarafinaNo ratings yet
- Bacterial Brain AbscessDocument16 pagesBacterial Brain AbscessYunike DindaNo ratings yet
- Zhou 2016Document13 pagesZhou 2016alif bagusNo ratings yet
- 12.management of PterygiumDocument3 pages12.management of PterygiumDiamond DustNo ratings yet
- Pilocytic Astrocytoma: Pathology, Molecular Mechanisms and MarkersDocument15 pagesPilocytic Astrocytoma: Pathology, Molecular Mechanisms and MarkersDomNo ratings yet
- Histopathological Parameters in Pterygia and Significant Clinical CorrelationsDocument9 pagesHistopathological Parameters in Pterygia and Significant Clinical CorrelationsSepti AyaNo ratings yet
- 1 s2.0 S0738081X14002375 MainDocument13 pages1 s2.0 S0738081X14002375 Mainmarisa araujoNo ratings yet
- NigerJOphthalmol26289-4304105 115721Document10 pagesNigerJOphthalmol26289-4304105 115721Alfina nurNo ratings yet
- An Update On Acute Postinfectious Glomerulonephritis WorldwideDocument12 pagesAn Update On Acute Postinfectious Glomerulonephritis WorldwideGabyRamónNo ratings yet
- Prevention, Diagnosis, and Management of Acute Postoperative Bacterial EndophthalmitisDocument16 pagesPrevention, Diagnosis, and Management of Acute Postoperative Bacterial EndophthalmitisNiñoTanNo ratings yet
- Prevalence of Eyelid Diseases Among Adults in Hong Kong: Shiu Ting Mak, Sze Wai Jeremy John Kwok, Hunter KL YuenDocument4 pagesPrevalence of Eyelid Diseases Among Adults in Hong Kong: Shiu Ting Mak, Sze Wai Jeremy John Kwok, Hunter KL YuenAndrewNo ratings yet
- Artigo 2 - MestradoDocument6 pagesArtigo 2 - MestradoThiago RodriguesNo ratings yet
- Trop Med 140515Document10 pagesTrop Med 140515Arfa AlyaNo ratings yet
- Immunopathology in Ocular Toxoplasmosis: Facts and Clues: Justus G Garweg /, Ermanno CandolfiDocument10 pagesImmunopathology in Ocular Toxoplasmosis: Facts and Clues: Justus G Garweg /, Ermanno CandolfiJuan Andrés Castaño CisfNo ratings yet
- Cataracts Pathophysiology and Managements: Abdulrahman Zaid AlshamraniDocument4 pagesCataracts Pathophysiology and Managements: Abdulrahman Zaid AlshamraniOcha24 TupamahuNo ratings yet
- Jurnal Otitis EksternaDocument4 pagesJurnal Otitis EksternaZóélkårnåín PhåntómhívéNo ratings yet
- 1 s2.0 S003962571630090X MainDocument14 pages1 s2.0 S003962571630090X MainBenjamin NgNo ratings yet
- Reti No Blast OmaDocument11 pagesReti No Blast OmaNiluh Ita PasyantiNo ratings yet
- Papiloma TerbalikDocument6 pagesPapiloma TerbalikLasman RadjaNo ratings yet
- Review 01-06 PDFDocument6 pagesReview 01-06 PDFEditor IjprtNo ratings yet
- Clinical: Peripheral Ossifying Fibroma: A Case ReportDocument4 pagesClinical: Peripheral Ossifying Fibroma: A Case Reportsagarjangam123No ratings yet
- Isrn Urology2012-707329 PDFDocument6 pagesIsrn Urology2012-707329 PDFNaomiRimaClaudyaNo ratings yet
- Review Article: Phimosis in ChildrenDocument7 pagesReview Article: Phimosis in ChildrenmerlinNo ratings yet
- Astrocytoma 10.1007/s00401-015-1410-7Document14 pagesAstrocytoma 10.1007/s00401-015-1410-7Rikizu HobbiesNo ratings yet
- DTS-00750 Mast Maintenance ManualDocument12 pagesDTS-00750 Mast Maintenance Manualsertecs polNo ratings yet
- Science MELCsDocument42 pagesScience MELCsRanjell Allain TorresNo ratings yet
- CS6711 Security Lab ManualDocument84 pagesCS6711 Security Lab ManualGanesh KumarNo ratings yet
- Teaching Vocabulary Through TPR Method ToDocument41 pagesTeaching Vocabulary Through TPR Method ToAan Safwandi100% (3)
- 4) April 2023 Current AffairsDocument24 pages4) April 2023 Current AffairsPicturesque vibrant shadesNo ratings yet
- Covid 19 PDFDocument117 pagesCovid 19 PDFvicky anandNo ratings yet
- Internship Report Zannatul Ferdousi Alam YameemDocument51 pagesInternship Report Zannatul Ferdousi Alam YameemZannatul Ferdousi Alam YameemNo ratings yet
- Basketball 2011: Johnson CountyDocument25 pagesBasketball 2011: Johnson CountyctrnewsNo ratings yet
- Twingo 3 & Clio 4Document10 pagesTwingo 3 & Clio 4Alexandre Le GrandNo ratings yet
- CARP Law NotesDocument5 pagesCARP Law NotesJustisia KaunlaranNo ratings yet
- Bài tập tiếng Anh 12 (Reading)Document7 pagesBài tập tiếng Anh 12 (Reading)Minh AnhNo ratings yet
- Basic Facts in EventDocument1 pageBasic Facts in EventAllan AgpaloNo ratings yet
- Cubic Spline Tutorial v3Document6 pagesCubic Spline Tutorial v3Praveen SrivastavaNo ratings yet
- Unit Rates and Cost Per ItemDocument213 pagesUnit Rates and Cost Per ItemDesiree Vera GrauelNo ratings yet
- Grab E-Receipt for 15,000 RP Ride on March 30Document1 pageGrab E-Receipt for 15,000 RP Ride on March 30WellyNo ratings yet
- Medication Calculation Examination Study Guide: IV CalculationsDocument2 pagesMedication Calculation Examination Study Guide: IV Calculationswaqas_xsNo ratings yet
- Analects of A.T. Still-Nature Quotes-UnboundedDocument8 pagesAnalects of A.T. Still-Nature Quotes-UnboundedBruno OliveiraNo ratings yet
- CS310 Sample PaperDocument10 pagesCS310 Sample PaperMohsanNo ratings yet
- Sato Printer Api Reference DocumentDocument34 pagesSato Printer Api Reference Documentsupersteel.krwNo ratings yet
- Surge arrester protects electrical equipmentDocument25 pagesSurge arrester protects electrical equipmentSyed Ahsan Ali Sherazi100% (3)
- ZiffyHealth Pitch DeckDocument32 pagesZiffyHealth Pitch DeckSanjay Kumar100% (1)
- Board Question Paper: March 2018: Geography and EconomicsDocument2 pagesBoard Question Paper: March 2018: Geography and EconomicsVishvajit PatilNo ratings yet
- Intermediate Accounting 2 - CL NCL Lecture NotesDocument2 pagesIntermediate Accounting 2 - CL NCL Lecture NotesRacheel SollezaNo ratings yet
- Crashing Pert Networks: A Simulation ApproachDocument15 pagesCrashing Pert Networks: A Simulation ApproachRavindra BharathiNo ratings yet
- Classification of AnimalsDocument6 pagesClassification of Animalsapi-282695651No ratings yet
- GMS175CSDocument4 pagesGMS175CScorsini999No ratings yet
- From Memphis To KingstonDocument19 pagesFrom Memphis To KingstonCarlos QuirogaNo ratings yet
- Safety Data Sheet: 1. Identification of The Substance/preparation and of The Company/undertakingDocument4 pagesSafety Data Sheet: 1. Identification of The Substance/preparation and of The Company/undertakingBalasubramanian AnanthNo ratings yet