Professional Documents
Culture Documents
Lichen Aureus
Uploaded by
HaeruddinHasyimPasingariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lichen Aureus
Uploaded by
HaeruddinHasyimPasingariCopyright:
Available Formats
22 Part 22
::
Vascular Diseases
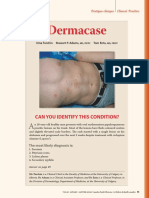
Figure 143-3 Pigmented purpuric dermatosis: Majocchi
disease. Multiple nonpalpable, nonblanching purpuric
lesions arranged in annular configurations and associated
with tiny telangiectasias. Note brownish discoloration of Figure 143-5 Lichen aureus. (Used with permission from
older lesions. Dr. Ashley Crew.)
clinically by mild scaling overlying pinpoint ery- subtype presents with more localized and persistent
thematous macules and patches with associated lesions with circumscribed macules or papules that
pruritus. Lichenification can occur from repeated are a distinctive gold, rust, or orange color (Fig. 143-5).
scratching. Histopathologically, spongiosis is pres- Histologically a dense, band-like lichenoid infiltrate
ent, in addition to the classic histopathologic fea- of inflammatory cells is seen. The lesions are gener-
tures of PPD. This subtype spreads rapidly over a ally asymptomatic but at times are intensely pruritic.
period of 15 to 30 days and will subsequently fade They are most commonly localized to one lower
without treatment over several months to years, extremity, but other body sites can be involved, and a
although recurrence is possible. segmental distribution has been reported.11,12 This dis-
order has a predilection for young adult males, with
a peak incidence in the second and third decades. It
runs a chronic course, with stable or slowly progress-
LICHEN AUREUS ing lesions.
In 1958, Martin first reported this subtype of PPD
under the term lichen purpuricus, which was later
named lichen aureus in 1960 by Calnan to emphasize ITCHING PURPURA
its vivid yellow-orange color.9,10 As opposed to pig-
mented purpuric lichenoid dermatosis of Gougerot (DISSEMINATED
and Blum, where lichenoid refers to the clinical mor-
phology of the lesions, in lichen aureus, lichen refers
PRURIGINOUS
to both its clinical and histopathologic features. This ANGIODERMATITIS)
Itching purpura, also known as disseminated prurigi-
nous angiodermatitis, presents acutely with widely
disseminated orange-brown to purpuric lesions asso-
ciated with severe pruritus.13,14 The lesions first appear
on the dorsal feet or lower extremities and then spread
upward, sometimes with involvement of the trunk.
Purpuric lesions are more apparent along the waist-
line, axilla, antecubital and popliteal fossae. Although
2592 Figure 143-4 Lichenoid dermatosis of Gougerot and Blum. this subtype of PPD has a chronic course, spontaneous
(Used with permission from Dr. April Armstrong.) remissions are possible.
Kang_CH143_p2590-2598.indd 2592 04/12/18 9:21 am
UNILATERAL LINEAR
connection between these 2 diseases, and the occur-
rence of MF in the setting of a PPD is rare, 3 different
22
CAPILLARITIS (SEGMENTAL relationships have been reported: MF mimicking pig-
mented purpura clinically, pigmented purpura evolv-
PIGMENTED PURPURA) ing into MF, and pigmented purpura that simulates
MF histologically.
In 1990, a transient PPD in a segmental distribution In a study of T-cell clonality and markers, T-cell
on the lower trunk of a middle-aged woman was monoclonality of PPD was most likely to predict pro-
reported. Later, Riordan and colleagues reported PPDs gression to MF, whereas the absence of certain T-cell
in 4 young men with linear and pseudodermatomal markers was a less reliable predictor.30 It is impor-
patterns, which they termed unilateral linear capillaritis.15 tant to note that both MF and PPD can display clon-
Both “segmental pigmented purpura” and “qua- ality. Histologic clues of MF are subtle and include
drantic capillaropathy” are considered subtypes of greater lymphoid atypia in the intraepidermal lym-
unilateral linear capillaritis.16,17 This PPD is clinically phocytes compared to dermal lymphocytes, large
Chapter 143 :: Pigmented Purpuric Dermatoses
distinguished by its linear or segmental distribution. It intraepidermal groups of lymphocytes anywhere in
tends to have a favorable prognosis, with spontaneous the epidermis, or many lymphocytes in the spinous
resolution occurring more commonly than in the other layer.30,31 Santucci and colleagues suggested that to
subtypes of PPDs. distinguish early MF from its inflammatory mimick-
ers the most important feature is lymphocytes with
extremely convoluted, medium to large nuclei, that
are single or clustered in the epidermis and in small
GRANULOMATOUS sheets in the dermis.32 Ackerman compared the his-
tologic features of lichenoid purpuric eruptions
PIGMENTED PURPURA with plaque stage MF and noted many similarities,
concluding that it may be impossible to differentiate
The first report of the granulomatous variant of PPDs these two on a histologic basis alone.33
was in 1996 by Saito and Matsuoka and since then The differentiation between PPD and MF can be
more than 17 cases have been reported.18-20 It is most difficult and requires the integration of clinical, histo-
common in middle age and has been reported more logic and immunophenotypic information.30,33 PPDs
commonly in patients of Asian descent.1,20 Clinically, with large areas of confluence, reticular arrange-
the lesions appear similar to other PPDs with purpuric ments, a superimposed violaceous hue, or pruritus
and brown macules developing most commonly on that has been present or relapsing for several years are
the lower extremities and dorsal feet. This subtype is suspicious for MF. There is a predominance in adult
distinguished by its histopathologic findings. In addi- males.21,34 For selected patients, long-term followup is
tion to the classic histopathologic features of a PPD, needed to monitor for evolution into MF, even though
a granulomatous infiltrate is present. The granuloma- the overall incidence of MF occurring in association
tous infiltrate is most commonly located in the pap- with PPD is rare.
illary dermis, but may be in the mid to deep dermis
separate from a more superficially located lichenoid
infiltrate. Systemic granulomatous disorders and
infectious processes (mycobacterial and deep fungal) ETIOLOGY AND
must be ruled out in these patients. Hyperlipidemia is
a relatively common association with granulomatous
PATHOGENESIS
pigmented purpura with 9 of 17 reported cases show- There are 3 different views on the pathogenesis of
ing elevated cholesterol levels in a review from 2014.19 PPDs. The first is that there is a disturbance or weak-
ness of cutaneous blood vessels, leading to capillary
fragility and erythrocyte extravasation. This pro-
PIGMENTED PURPURIC posed mechanism, however, does not account for the
inflammatory infiltrate that is also seen in these erup-
DERMATOSIS/MYCOSIS tions. The second theory is that PPDs develop from a
humoral immune response. This theory is supported
FUNGOIDES OVERLAP by direct immunofluorescence studies showing vas-
cular deposition of C3, C1q, immunoglobulin M, or
In 1988, Barnhill and Braverman reported the first immunoglobulin A.35,36 The final theory is that PPDs
cases of pigmented purpura-like eruptions progressing develop as a result of a cellular immune response.37,38
to mycosis fungoides.21 Furthermore, the first patient This theory suggests that the inflammatory infiltrate,
diagnosed with lichen aureus in the United States consisting of lymphocytes, macrophages, and Langer-
was later diagnosed with mycosis fungoides (MF; hans cells, leads to vascular fragility and subsequent
see Chap. 119). Some evidence supports the idea that extravasation of erythrocytes. Aiba and Tagami used
lichenoid variants of PPD may be precursors of MF, immunohistologic studies in 8 cases of Schamberg dis-
with similar histologic findings and clonal popula- ease to demonstrate that the dermal infiltrate was pre- 2593
tions of lymphocytes.22-29 Although there is no clear dominantly composed of helper-inducer T-cells and
Kang_CH143_p2590-2598.indd 2593 04/12/18 9:21 am
You might also like
- Gracella Irwana - G - Pert 04 - Sia - 1Document35 pagesGracella Irwana - G - Pert 04 - Sia - 1Gracella IrwanaNo ratings yet
- Book Reading Poltak Daniel Veron Panjaitan - Fitzpatrick's Chapter 143Document9 pagesBook Reading Poltak Daniel Veron Panjaitan - Fitzpatrick's Chapter 143Poltak PanjaitanNo ratings yet
- Jurnal Pigmented Purpuric DermatosesDocument6 pagesJurnal Pigmented Purpuric DermatosesBianca CaterinalisendraNo ratings yet
- V26i2 BielsaDocument6 pagesV26i2 BielsaAmanbosNo ratings yet
- Vesiculobullous Disorders: Chapter 52:: Pemphigus:: Aimee S. Payne & John R. StanleyDocument17 pagesVesiculobullous Disorders: Chapter 52:: Pemphigus:: Aimee S. Payne & John R. StanleyrizkyNo ratings yet
- Prurigo Simplex or Itchy Red BumpsDocument7 pagesPrurigo Simplex or Itchy Red BumpsS FznsNo ratings yet
- Dermatologicmanifestations of Internalcancer: Bruce H. Thiers, M.DDocument19 pagesDermatologicmanifestations of Internalcancer: Bruce H. Thiers, M.DWilianto LimNo ratings yet
- Gonzalez Delgado2020Document2 pagesGonzalez Delgado2020reda rashwanNo ratings yet
- Poroma: A Review of Eccrine, Apocrine, and Malignant FormsDocument9 pagesPoroma: A Review of Eccrine, Apocrine, and Malignant FormsDaham ThuljayaNo ratings yet
- LSKDocument4 pagesLSKAinia TaufiqaNo ratings yet
- HEMAREPORT1Document6 pagesHEMAREPORT1Sarah Grace KamlaniNo ratings yet
- HAPP-PICO Tissue Pathology Journal ResearchDocument4 pagesHAPP-PICO Tissue Pathology Journal ResearchArlynn MartinezNo ratings yet
- Novo 6 - Mal de Pott HidradeniteDocument3 pagesNovo 6 - Mal de Pott HidradeniteJosé Paulo Ribeiro JúniorNo ratings yet
- Non Hemo TropicDocument9 pagesNon Hemo TropicMichael GresonNo ratings yet
- 575 1273 0 Immunofluorescence in Dermatology-MutasimDocument22 pages575 1273 0 Immunofluorescence in Dermatology-MutasimLeandro QuitoNo ratings yet
- Target and Targetoid Lesions in Dermatology.Document5 pagesTarget and Targetoid Lesions in Dermatology.KuldeepSinghBanaNo ratings yet
- (Serbian Journal of Dermatology and Venereology) Dermoscopy Case of The Month PDFDocument5 pages(Serbian Journal of Dermatology and Venereology) Dermoscopy Case of The Month PDFArya NugrahaNo ratings yet
- Dermacase. Pityriasis Rosea.Document3 pagesDermacase. Pityriasis Rosea.Brenda Ruth PanjaitanNo ratings yet
- Parakeratosis Pustulosa: A Diagnostic Conundrum: Review ArticleDocument4 pagesParakeratosis Pustulosa: A Diagnostic Conundrum: Review ArticleRandy Al-fatihNo ratings yet
- Prurigo Nodularis of HydeDocument12 pagesPrurigo Nodularis of HydeAugusto MonjardimNo ratings yet
- 6 Vascular DisordersDocument3 pages6 Vascular DisordersJoj VergaraNo ratings yet
- Mud I Gonda 2013Document3 pagesMud I Gonda 2013Febyan AbotNo ratings yet
- Deep Mycotic InfectionDocument5 pagesDeep Mycotic InfectionjalalfaizNo ratings yet
- Lichen Planus/lupus Erythematosus Overlap With Hypothyroidism: A Case ReportDocument3 pagesLichen Planus/lupus Erythematosus Overlap With Hypothyroidism: A Case ReportcuribepNo ratings yet
- Pyoderma Gangrenosum - A Guide To Diagnosis and Management: Authors: Christina GeorgeDocument5 pagesPyoderma Gangrenosum - A Guide To Diagnosis and Management: Authors: Christina GeorgeTasyaIndrianiRcisNo ratings yet
- PatogenezDocument10 pagesPatogenezlloplNo ratings yet
- Drug Induced Drug PathologyDocument13 pagesDrug Induced Drug PathologyBagus Putra KurniawanNo ratings yet
- Seminars in Diagnostic Pathology: Bullous, Pseudobullous, & Pustular DermatosesDocument11 pagesSeminars in Diagnostic Pathology: Bullous, Pseudobullous, & Pustular DermatosesCynthia OktariszaNo ratings yet
- Mikimos,+09 +lisi 56 60Document5 pagesMikimos,+09 +lisi 56 60MaylafaizaNo ratings yet
- Pityriasis RoseaDocument7 pagesPityriasis RoseaHaeruddinHasyimPasingariNo ratings yet
- Pulmonary Tuberculosis: o Also Called PPD - ID (Purified Protein Derivative)Document9 pagesPulmonary Tuberculosis: o Also Called PPD - ID (Purified Protein Derivative)LoramaematuteNo ratings yet
- Oral Lesions in Patients With Pemphigus Vulgaris and Bullous PemphigoidDocument6 pagesOral Lesions in Patients With Pemphigus Vulgaris and Bullous PemphigoidmkoaaoNo ratings yet
- Autoimmune Bullous DiseaseDocument10 pagesAutoimmune Bullous DiseaseSiti Habibah ZeinNo ratings yet
- Case ReportDocument6 pagesCase ReportSalma KarimahNo ratings yet
- Seminars in Diagnostic Pathology: Mark R. WickDocument11 pagesSeminars in Diagnostic Pathology: Mark R. WickAbdillah AkbarNo ratings yet
- Bullous Pemphigoid Guide To Diagnosis and Treatment - Prescriber - 2010 - BowerDocument4 pagesBullous Pemphigoid Guide To Diagnosis and Treatment - Prescriber - 2010 - BowerVinh ThếNo ratings yet
- Sarkar, 2016Document7 pagesSarkar, 2016vtolentinoscribdNo ratings yet
- Lichen Striatus On AdultDocument4 pagesLichen Striatus On Adultmustafa566512345No ratings yet
- Parry Romberg SyndromeDocument7 pagesParry Romberg SyndromeAlexcr199415No ratings yet
- Perioral DermatitisDocument6 pagesPerioral DermatitisYeni OktaviaNo ratings yet
- Medicina 57 01004Document12 pagesMedicina 57 01004Ilham MahardikaNo ratings yet
- Seminars in Diagnostic Pathology: Mark R. WickDocument12 pagesSeminars in Diagnostic Pathology: Mark R. WickNancy ManriqueNo ratings yet
- Pyoderma Gangrenosum: A Review: Cutaneous PathologyDocument11 pagesPyoderma Gangrenosum: A Review: Cutaneous PathologyBela RomanNo ratings yet
- Chapter 34:: Granuloma Annulare:: Julie S. Prendiville: Cutaneous FindingsDocument8 pagesChapter 34:: Granuloma Annulare:: Julie S. Prendiville: Cutaneous FindingsLidia MdNo ratings yet
- Perioral Dermatitis: Acta Dermatovenerologica Croatica: ADC / Hrvatsko Dermatolosko Drustvo February 2008Document6 pagesPerioral Dermatitis: Acta Dermatovenerologica Croatica: ADC / Hrvatsko Dermatolosko Drustvo February 2008Firdani MutiaraNo ratings yet
- Braun Falco 2012Document7 pagesBraun Falco 2012Alexandra OpreaNo ratings yet
- Psoriasis Inversa: A Separate Identity or A Variant of Psoriasis Vulgaris?Document6 pagesPsoriasis Inversa: A Separate Identity or A Variant of Psoriasis Vulgaris?PrimeraNo ratings yet
- 41 Yugandar EtalDocument4 pages41 Yugandar EtaleditorijmrhsNo ratings yet
- Leprosy PPT ManyaDocument25 pagesLeprosy PPT Manyakhushi.gupta2122No ratings yet
- Yellow and Orange in Cutaneous Lesions: Clinical and Dermoscopic DataDocument9 pagesYellow and Orange in Cutaneous Lesions: Clinical and Dermoscopic DataAFA.BLSNo ratings yet
- Herpetiform Pemphigus: Courtesy, Ronald P Rapini, MDDocument1 pageHerpetiform Pemphigus: Courtesy, Ronald P Rapini, MDCristian QuitoNo ratings yet
- Cutaneous TuberculosisDocument10 pagesCutaneous TuberculosisjalalfaizNo ratings yet
- CANINE-Pemphigus Complex-Pathogenesis and Clinical PresentationDocument5 pagesCANINE-Pemphigus Complex-Pathogenesis and Clinical Presentationtaner_soysuren100% (4)
- Practice: Palmoplantar PustulosisDocument1 pagePractice: Palmoplantar Pustulosisdewa gede eka yuditiraNo ratings yet
- Veruka VulgarisDocument31 pagesVeruka VulgarisfenskaNo ratings yet
- Terminologia MédicaDocument4 pagesTerminologia MédicaGuadalupeNo ratings yet
- Leprosy ClinicalkeyDocument14 pagesLeprosy ClinicalkeyeugeniaNo ratings yet
- Spine TBDocument4 pagesSpine TBWorthless BoysNo ratings yet
- Venkatraman K PDFDocument3 pagesVenkatraman K PDFRana Zara AthayaNo ratings yet
- Chapter 26:: Seborrheic Dermatitis:: Dae Hun Suh: Clinical FeaturesDocument10 pagesChapter 26:: Seborrheic Dermatitis:: Dae Hun Suh: Clinical FeaturesmyztNo ratings yet
- Familial Mediterranean FeverFrom EverandFamilial Mediterranean FeverMarco GattornoNo ratings yet
- Pityriasis RoseaDocument7 pagesPityriasis RoseaHaeruddinHasyimPasingariNo ratings yet
- Ulcer DiabeticsDocument3 pagesUlcer DiabeticsHaeruddinHasyimPasingariNo ratings yet
- Heroin CannabisDocument3 pagesHeroin CannabisHaeruddinHasyimPasingariNo ratings yet
- Hepatoerythropoietic Porphyria: DiagnosisDocument3 pagesHepatoerythropoietic Porphyria: DiagnosisHaeruddinHasyimPasingariNo ratings yet
- Pipe Freezing StudyDocument8 pagesPipe Freezing StudymirekwaznyNo ratings yet
- A Method For Prediction of Gas/Gas Ejector PerformanceDocument6 pagesA Method For Prediction of Gas/Gas Ejector PerformancedhavaleshNo ratings yet
- Half Yearly Examination, 2017-18: MathematicsDocument7 pagesHalf Yearly Examination, 2017-18: MathematicsSusanket DuttaNo ratings yet
- Unit 20: TroubleshootingDocument12 pagesUnit 20: TroubleshootingDongjin LeeNo ratings yet
- Chapter 9Document28 pagesChapter 9Aniket BatraNo ratings yet
- Cornish BoilerDocument3 pagesCornish BoilerDeepak KV ReddyNo ratings yet
- Sistemas de Mando CST Cat (Ing)Document12 pagesSistemas de Mando CST Cat (Ing)Carlos Alfredo LauraNo ratings yet
- QF Jacket (Drafting & Cutting) - GAR620Document15 pagesQF Jacket (Drafting & Cutting) - GAR620abdulraheem18822No ratings yet
- Present Perfect Simp ContDocument14 pagesPresent Perfect Simp ContLauGalindo100% (1)
- 3.0 Series and Parallel DC CircuitsDocument29 pages3.0 Series and Parallel DC CircuitsJinky Loyce RaymundoNo ratings yet
- Kursus Jabatan Kejuruteraan Mekanikal Sesi Jun 2014Document12 pagesKursus Jabatan Kejuruteraan Mekanikal Sesi Jun 2014ihsanyusoffNo ratings yet
- The Teacher Research Movement: A Decade Later: Cite This PaperDocument13 pagesThe Teacher Research Movement: A Decade Later: Cite This PaperAlexandre NecromanteionNo ratings yet
- Nascsa - Sponsor Solicitation List: January 06, 2021Document35 pagesNascsa - Sponsor Solicitation List: January 06, 2021Prasoon SimsonNo ratings yet
- Gandhi and The Non-Cooperation MovementDocument6 pagesGandhi and The Non-Cooperation MovementAliya KhanNo ratings yet
- SRS For Travel AgencyDocument5 pagesSRS For Travel AgencyHardik SawalsaNo ratings yet
- Bearing 1Document27 pagesBearing 1desalegn hailemichaelNo ratings yet
- IoT Security Checklist Web 10 17 r1Document39 pagesIoT Security Checklist Web 10 17 r1SubinNo ratings yet
- QAI Golden Pass Fact SheetDocument2 pagesQAI Golden Pass Fact SheetQatar-America InstituteNo ratings yet
- Icc Esr-2302 Kb3 ConcreteDocument11 pagesIcc Esr-2302 Kb3 ConcretexpertsteelNo ratings yet
- Elasticsearch, Logstash, and Kibana - CERTDocument35 pagesElasticsearch, Logstash, and Kibana - CERTManuel VegaNo ratings yet
- Collins Ks3 Science Homework Book 3Document5 pagesCollins Ks3 Science Homework Book 3g3pz0n5h100% (1)
- GST RATE LIST - pdf-3Document6 pagesGST RATE LIST - pdf-3Niteesh KumarNo ratings yet
- 3DS 2017 GEO GEMS Brochure A4 WEBDocument4 pages3DS 2017 GEO GEMS Brochure A4 WEBlazarpaladinNo ratings yet
- Free ConvectionDocument4 pagesFree ConvectionLuthfy AditiarNo ratings yet
- Panera Bread Case StudyDocument28 pagesPanera Bread Case Studyapi-459978037No ratings yet
- The Other Twelve Part 1Document5 pagesThe Other Twelve Part 1vv380100% (2)
- Royal British College Dancesport TeamDocument10 pagesRoyal British College Dancesport TeamAnna rose CabatinganNo ratings yet
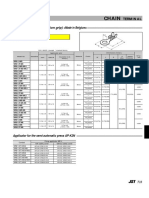
- Chain: SRB Series (With Insulation Grip)Document1 pageChain: SRB Series (With Insulation Grip)shankarNo ratings yet
- FIGMADocument22 pagesFIGMACessNo ratings yet