Professional Documents
Culture Documents
Strategies To Reduce Under 5 Preventable Death in Selangor
Uploaded by
Joshua Taylor Thomas0 ratings0% found this document useful (0 votes)
6 views15 pagesThe document outlines strategies to reduce preventable deaths in children under 5 years old in Selangor, Malaysia. It provides checklists and guidelines for classifying and managing common childhood illnesses like cough, difficult breathing, diarrhea, and fever based on danger signs present. For severe or life-threatening classifications, the guidelines recommend immediate referral to the hospital after initial resuscitation at the clinic. For mild or moderate illnesses, guidelines provide home management instructions and advise on follow-up care. The overall goal is to ensure rapid and appropriate medical response to reduce mortality from preventable causes in young children.
Original Description:
Original Title
Untitled
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document outlines strategies to reduce preventable deaths in children under 5 years old in Selangor, Malaysia. It provides checklists and guidelines for classifying and managing common childhood illnesses like cough, difficult breathing, diarrhea, and fever based on danger signs present. For severe or life-threatening classifications, the guidelines recommend immediate referral to the hospital after initial resuscitation at the clinic. For mild or moderate illnesses, guidelines provide home management instructions and advise on follow-up care. The overall goal is to ensure rapid and appropriate medical response to reduce mortality from preventable causes in young children.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views15 pagesStrategies To Reduce Under 5 Preventable Death in Selangor
Uploaded by
Joshua Taylor ThomasThe document outlines strategies to reduce preventable deaths in children under 5 years old in Selangor, Malaysia. It provides checklists and guidelines for classifying and managing common childhood illnesses like cough, difficult breathing, diarrhea, and fever based on danger signs present. For severe or life-threatening classifications, the guidelines recommend immediate referral to the hospital after initial resuscitation at the clinic. For mild or moderate illnesses, guidelines provide home management instructions and advise on follow-up care. The overall goal is to ensure rapid and appropriate medical response to reduce mortality from preventable causes in young children.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 15
STRATEGIES
TO REDUCE UNDER 5 PREVENTABLE DEATH
IN SELANGOR
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
CHECKLIST APPROACH TO UNWELL CHILDREN UNDER FIVE YEARS LAMPIRAN 1
TABLE 1: THE SICK CHILD AGE 2 MONTHS UP TO 5 YEARS
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 2: THE SICK YOUNG INFANT AGE UP TO 2 MONTH
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
LAMPIRAN 2
APPROACH TO UNWELL CHILDREN UNDER FIVE YEARS
TABLE 1: GENERAL DANGER SIGNS
ASK LOOK AND FEEL
- Not able to drink or breastfeed - Drowsy or unconscious
- Vomit everything or greenish vomitus - Convulsion
- Convulsions during this illness
TABLE 2 : APPROACH TO COUGH OR DIFFICULT BREATHING
Signs Classification Management
Presence of: Severe Initial resuscitation
chest indrawing or disease - Secure airways
acute stridor or - Suction if necessary
fast breathing or - Support breathing
cyanosis - Give oxygen via High flow mask
SPO2 < 95% - Restore circulation (IV Drips)
Reduce air entry - Capillary blood sugar
Silent chest (Aim > 3mmol/L)
If DXT <3mmol/L give 2-3mls/kg
D10% as rapid bolus. Repeat DXT
after 30 minutes
Refer urgently to hospital after
stabilization
(Refer transport checklist)
Wheeze wheeze Treat wheeze with nebulised salbutamol
Look for any red flags (0.5ml salbutamol solution + 3.5ml
of respiratory normal saline with oxygen flow 5-8L)
distress Assess response after 15 minutes
Can give up to 3 times. If > 3 times to
refer hospital
No sign of severe Cough or Manage accordingly
disease cold Advise mother when to return
immediately
Follow up in 5 days if not improving
If coughing more than 14 days, or
recurrent wheezing refer for assessment
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 3: APPROACH TO DIARRHOEA
Signs Classification Management
Two or more of the following Severe Start IV lines / intraosseous if possible
signs dehydration Initial fluid for resuscitation of shock:
Drowsy or 20mls/kg 0.9% NS or Hartmann Solution
unconscious as rapid IV bolus. Review patient after
Sunken eyes bolus.
Not able to drink or (pulse volume, CRT, HR, BP)
drink poorly Put on maintenance fluid 0.45% NS ( 5-
Skin pinch goes back 7mls/kg/ Hr ) until reach hospital
very slowly Refer immediately (Refer transport
Signs of shock checklist)
- Tachycardia
- Weak peripheral
pulses
- Delayed CRT > 2s
- Cold peripheries
- Depressed
mental state
- With/without
hypotension
Two or more of the following Moderate Start IV maintenance fluid 0.45% NS
signs dehydration (4mls/kg/hr)
Restless or irritable Give fluids/ ORS / breastfeed if able to
Sunken eyes tolerate (no vomiting)
Drinks eagerly, Refer immediately (Refer transport
thirsty checklist)
Skin pinch goes back
slowly
Mild / No signs of Mild/ No Give fluid and food to treat diarrhoea at
dehydration dehydration home
Extra fluid after each loose stool
( < 2Yrs : 50 -100mls ORS
>2 Yrs : 100- 200mls ORS)
Advise mother when to return
immediately ( Use mother’s card)
Give frequent, small sips of fluids
If child vomit, wait for 10 minutes
Do not give anti-diarrhoea medication
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 4: APPROACH TO FEVER ( BY HISTORY / TEMPERATURE > 38°C)
Signs Classification Management
Presence of : Severe For haemodynamically stable patient :
Stiff neck Febrile Give one dose of Paracetamol in clinic for
Changes of behavior / irritable Disease high fever (38°C or above) 15mg/kg/ dose
Petechiae /purpuric rash IV access
Signs of respiratory distress FBC if available
- chest indrawing Refer immediately (Refer transport checklist)
- acute stridor For haemodynamically unstable patient :
- fast breathing Initial resuscitation
- cyanosis - Secure airways
- SPO2 < 95% - Suction if necessary
- Reduce air entry - Support breathing
- Silent chest - Give oxygen via High flow mask
Acute abdomen - Restore circulation (IV Drips)
Warning signs for Dengue Fever - Capillary blood sugar
- Persistent vomiting / (Aim > 3mmol/L)
diarrhea If DXT <3mmol/L give 2-3mls/kg D10% as
- Intense abdominal pain rapid bolus. Repeat DXT after 30
/tenderness minutes
- Mucosal bleed Any signs of respiratory distress ( Refer table
- Lethargy / restlessness cough/ difficult breathing)
- Clinical fluid accumulation Any signs of diarrhoea (Refer table
- Liver enlargement > 2cm diarrhoea)
- Laboratory : increase in If patient convulsing/fitting:
HCT with concurrent rapid -To give PR Diazepam
decrease in platelet count 0.2- 0.5 mg/kg (Max 10mg)
Signs of shock -Give oxygen
- Tachycardia -Monitor for respiratory depression
- Weak peripheral pulses -Put left lateral position
- Delayed CRT > 2s If signs of shock:
- Cold peripheries - Initial fluid for resuscitation of shock:
- Depressed mental 20mls/kg 0.9% NS or Hartmann Solution as
state rapid IV bolus. Review patient after bolus.
- With/without (pulse volume, CRT, HR, BP)
hypotension - Put on maintenance fluid ( 5-7mls/Kg/ Hr )
until reach hospital
- Refer immediately (Refer transport
checklist)
No signs of danger signs Febrile Establish diagnosis/source of infection
Illness FBC if available and manage accordingly
Syrup Paracetamol (15mg/kg/dose every
6hourly)
Syrup Antibiotic if indicated
Advise mother when to return
Immediately (Refer mother card)
Follow-up in 2-3 days if fever persists.
Refer hospital when no response to
treatment or worsening condition
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
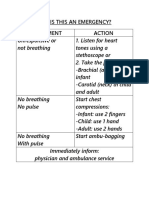
TABLE 5 : MANAGEMENT OF SICK INFANT UP TO 2 MONTHS OLD
Signs Classification Management
Presence of any sign or Initial resuscitation
symptom below: Severe - Secure airways
Not feeding well disease - Suction if necessary
● Greenish vomitus - Support breathing
● Convulsions or abnormal - Give oxygen via High flow mask /
movement headbox oxygen if available (10-
● Fast breathing 15L/min)
Apnoea - Restore circulation (IV Drips)
● Severe chest indrawing. - Capillary blood sugar
● Fever (37.5°C or above) or (Aim > 3mmol/L)
Low body temperature If DXT <3mmol/L give 2-3mls/kg
(below 35.5°C) D10% as rapid bolus. Repeat DXT
● Movement only when after 30 minutes
stimulated or No movement - Maintain optimal temperature (36.5-
at all 37°C)
Refer urgently to hospital after
stabilization
(Refer Lampiran 3, Table 1,2,3)
● Redness of umbilical Bacterial Refer hospital for further management
stump or draining pus infection
●Generalised skin pustules
●No sign of very severe Not severe Advise mother to give home care for
disease or local bacterial disease or young infant
infection local
infection
TABLE 6: APPROACH TO FAILURE TO THRIVE
Signs Classification Management
Presence of signs of Severe Refer hospital urgently
kwashiokor / marasmus ailure To
-Visible severe wasting Thrive
- Oedema of both feet
Identify causes
<-3SD weight-to-age Kurang Refer MO/ FMS
Berat Badan Refer PSP /dietician
Teruk Refer paediatric clinic if indicated
-2SD to -3SD weight – to- Kurang Berat Identify causes
age Badan Refer MO/ FMS
Sederhana Refer PSP /dietician
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 7 : APPROACH TO ANEMIA CHILD
Signs Classification Management
Pallor with signs and symptoms of Symptomatic Anemia Refer hospital for
failure further management
- Shortness of breath Give oxygen
- Reduce effort tolerance IV access
- Fainting episodes
- Tachycardia
- Tachypnoea
Pallor with hepatosplenomegaly
Pallor without signs and symptoms Asymptomatic Anemia Investigate causes of
of failure anemia at KK level
If nutritional cause to
refer PSP/ dietician
Refer paediatric clinic
for treatment
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 8 : Normal Value for Age
TABLE 8 : Normal Value for Age
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
LAMPIRAN 3
TABLE 1 :CHECKLIST FOR REFERRAL AND TRANSPORTATION TO HOSPITAL (PAEDIATRIC CASE)
Name: RN: Date:
No Staff Yes Remarks
Responsible
1. Contact / inform specialist in charge of the Medical
ward / KK when referral is made Officer/MA/SN
2. Contact referral centre and inform the medical Medical Name of
officer or specialist on call before the child is Officer/ MA specialist:
transported Ward:
3. Contact and inform parents before referral. If Medical
necessary obtain consent and get specimen of Officer/
mother’s blood ( for < 6 months baby) if the MA/SN
mother is unable to accompany the child
4. Write referral letter with adequate details and Medical
history of the child Officer*
Document in referral letter:
. history and examination findings
. treatment given
. progress of patient before transfer
. date, time and person contacted
5. Arrange transport and inform accepting MA/SN
hospital regarding time of departure
6. Review and stabilise patient before transport Medical BP: RR:
Officer/MA PR: SPO2:
7. Ensure availability and functioning of: MA/SN
.Transport bag
. Pulse oxymeter/ BP set (NIBP monitor)
.Infusion pump / IV drip with chamber
.Oxygen tank
.Portable suction unit
8. Give proper instructions to staffs Medical What
accompanying the child Officer/MA instructions?
9. Intubated child Medical ETT size:
-Ensure correct ETT position and reinforce Officer/MA/SN Anchored at:
anchoring before transfer
-Use a manometer while ambubagging
10. During transport Medical
-Regular assessment and vital signs monitoring Officer
every 15 minutes (record in observation chart) /MA/SN
-Suction prn
-Ensure correct position of ETT if intubated
*May not be applicable for Health clinics
*For Health clinics- Ill child must be attended by MO for facilities with staying in MO on call
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 2: OBSERVATION CHART
DATE TIME HEART RATE RESPIRATORY OXYGEN REMARKS
RATE SATURATION
BEFORE TRANSPORTATION
DURING TRANSPORTATION
TABLE 3: MEDICATION GIVEN DURING TRANSPORTATION
DATE TIME DRUG DOSAGE ROUTE REMARK
LEFT HOSPITAL / PREMISE @:
ARRIVED AT DESTINATION @:
NAME OF DOCTOR / MEDICAL ASISTANT / STAFF NURSE:
RECEIVED BY:
DR:
SISTER/ STAFFNURSE:
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
LAMPIRAN 4
FETAL KICK CHART (FKC)
Apa itu Fetal Kick Chart?
Fetal Kick Chart adalah carta pergerakan bayi untuk merekod bilangan dan corak pergerakan bayi
dalam kandungan. Carta ini sangat penting untuk memantau pergerakan bayi dalam kandungan dari
28 minggu hingga bersalin. Carta ini adalah satu cara yang mudah yang boleh anda lakukan dirumah
atau tempat kerja bagi memantau corak pergerakan bayi anda.
Mengapakah anda harus menggunakan carta pergerakan bayi?
1. Untuk pengesanan awal masalah dengan kandungan anda melalui perubahan pada
pergerakan bayi.
2. Untuk mengambil tindakan segera jika ada perubahan pergerakan bayi.
Bagaimana anda menggunakan carta pergerakan bayi?
1. Tulis tarikh dan masa yang anda memulakan kiraan pergerakan
2. Anda dinasihatkan bermula pada pukul 9 pagi. Bagi ibu yang bertugas malam , mula mengira
pergerakan dari 7 malam.
3. Kira dan tanda (√) setiap gerakan bayi.
4. Rekod waktu pergerakan yang ke 10 dalam carta FKC.
5. Lakukan yang sama pada hari keesokan dan menggunakan baris dan tarikh yang baru
Anda seharusnya mencapai 10 gerakan bayi dalam tempoh 12 jam.
Ciri-ciri pergerakan bayi
1. Tendangan bayi / berpusing / gerakan bayi menggeliat
*Pergerakan bayi yang banyak pada suatu masa hanya dikira sebagai satu.
Bilakah anda perlu berjumpa doktor segera?
1. Tidak cukup 10 tendangan dalam masa 12 jam
2. Corak dan tempoh pergerakan bayi luar biasa pada hari tersebut
i) Cukup 10 kali tendangan dalam masa 12 jam tetapi lemah dari kebiasaan.
ii) Pergerakan yang terlampau aktif dari hari biasa( contohnya setiap hari cukup 10 kali
tendangan pada pukul 7 malam tetapi pada hari tersebut cukup 10 kali tendangan
pada pukul 12 tengahari).
iii) Pergerakan bayi lewat dari kebiasaan (contohnya, setiap hari cukup 10 kali
tendangan pada pukul 7 malam tetapi pada hari tersebut pada pukul 7malam masih
tidak mencukupi)
*Pergerakan bayi yang berkurangan mungkin bermakna bayi anda memerlukan perhatian segera.
Apa yang mungkin akan dilakukan di hospital?
Untuk mengesahkan status kesihatan bayi anda melalui :
1. Cardiotocographic (CTG) – memantau degupan jantung bayi
2. Ultrasound Abdomen (jika perlu)
3. Anda mungkin akan dimasukkan ke wad untuk tindakan lanjut
Unit Kesihatan Keluarga JKN Selangor 2017
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
TABLE 1: FEEDING RECOMMENDATION DURING SICKNESS AND HEALTH LAMPIRAN 5
(Source: Integrated Management of Childhood Illness)
Unit Kesihatan Keluarga JKN Selangor 2017 12
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
Table 1: WARNING SIGNS IN CHILDREN LAMPIRAN 6
(Source: Integrated Management of Childhood Illness)
Unit Kesihatan Keluarga JKN Selangor 2017 13
“STRATEGIES TO REDUCE UNDER 5 PREVENTABLE DEATH” PERINGKAT NEGERI SELANGOR
Unit Kesihatan Keluarga JKN Selangor 2017
You might also like
- Immunisation HandbookDocument546 pagesImmunisation HandbookPritam Dugar100% (1)
- Wisdom Chi KungDocument0 pagesWisdom Chi KungDevlinPyxNo ratings yet
- Quiz RespiratoryDocument123 pagesQuiz RespiratoryMedShare100% (23)
- 109 Upper Extremity Questions and AnswersDocument8 pages109 Upper Extremity Questions and AnswersChioma BenedetteNo ratings yet
- ATI NotesDocument16 pagesATI NotesMei Sarte100% (1)
- TEST - Cancer-ParasiteDocument41 pagesTEST - Cancer-ParasiteRazvan Andrei ValcuNo ratings yet
- Algorithm - Managing A COPD Exacerbation in Primary CareDocument1 pageAlgorithm - Managing A COPD Exacerbation in Primary Caremufidah mawaddahNo ratings yet
- The 13 Remedies of DR John Henry Clarke: SULPHUR (Brimstone Flowers of Sulphur.)Document20 pagesThe 13 Remedies of DR John Henry Clarke: SULPHUR (Brimstone Flowers of Sulphur.)Anonymous eKt1FCDNo ratings yet
- ASCIA Guidelines Acute Management Anaphylaxis 2017 Updated PDFDocument8 pagesASCIA Guidelines Acute Management Anaphylaxis 2017 Updated PDFAyu WahyuniNo ratings yet
- Study Guide For Med Surg 1Document15 pagesStudy Guide For Med Surg 1desireemaenugentNo ratings yet
- Pedia ReviewerDocument27 pagesPedia ReviewerEvangeline GoNo ratings yet
- ASCIA Guidelines Acute Management Anaphylaxis 2019Document8 pagesASCIA Guidelines Acute Management Anaphylaxis 2019Asadulla KhanNo ratings yet
- Peripheral Neuropathy HandoutDocument16 pagesPeripheral Neuropathy HandoutTatiana IonascuNo ratings yet
- Case Pres CellulitisDocument97 pagesCase Pres CellulitischelybabyjynxNo ratings yet
- DR Mwanzas Pediatric Protocols 2017Document143 pagesDR Mwanzas Pediatric Protocols 2017Mwambazi MathewsNo ratings yet
- Integrated Prevention and Management of Selected Acute and Chronic Illness (IPMSACI) - Job AidDocument9 pagesIntegrated Prevention and Management of Selected Acute and Chronic Illness (IPMSACI) - Job AidCOMDIS-HSDNo ratings yet
- Management of Medical Complications in Severe Acute Malnutrition (SAM)Document4 pagesManagement of Medical Complications in Severe Acute Malnutrition (SAM)Archana SinghNo ratings yet
- Current Guidelines in Management of DiarrhoeaDocument40 pagesCurrent Guidelines in Management of Diarrhoeaokwadha simionNo ratings yet
- Emergency Pediatric AidsDocument29 pagesEmergency Pediatric AidsRana SalemNo ratings yet
- Flowchart 1 Immediate Management of An AsphyxiatednewbornDocument3 pagesFlowchart 1 Immediate Management of An Asphyxiatednewborndessy pratiwiNo ratings yet
- Flowchart 1 Immediate Management of An Asphyxiated NewbornDocument3 pagesFlowchart 1 Immediate Management of An Asphyxiated Newborndessy pratiwiNo ratings yet
- ASCIA HP Guidelines Acute Management Anaphylaxis 2020Document8 pagesASCIA HP Guidelines Acute Management Anaphylaxis 2020Munshi KamrulNo ratings yet
- Acute Management of Anaphylaxis: Adrenaline (Epinephrine) Is The First Line Treatment For AnaphylaxisDocument8 pagesAcute Management of Anaphylaxis: Adrenaline (Epinephrine) Is The First Line Treatment For AnaphylaxissigmapomalNo ratings yet
- NCLEX LABS +few PointersDocument5 pagesNCLEX LABS +few PointersSNo ratings yet
- Kondisi Yang Mengancam Nyawa Dan Memerlukan Intervensi Yang Agresif SecepatnyaDocument3 pagesKondisi Yang Mengancam Nyawa Dan Memerlukan Intervensi Yang Agresif SecepatnyaAbu QaireenNo ratings yet
- CPG Acute Infectious Diarrhea Pocket Guide v2Document21 pagesCPG Acute Infectious Diarrhea Pocket Guide v2Moonyeen Jann Casera BalicNo ratings yet
- DISEASES CASE MANAGEMENT PROTOCOL Final Draft DTD August 2014-VaidDocument34 pagesDISEASES CASE MANAGEMENT PROTOCOL Final Draft DTD August 2014-VaidferasNo ratings yet
- Approach To Acute Diarrhoea: Dr. Pankaj Kumar Singhal Govt. Medical College, KotaDocument43 pagesApproach To Acute Diarrhoea: Dr. Pankaj Kumar Singhal Govt. Medical College, KotaVandanaNo ratings yet
- Clinical Presentation and Case ManagementDocument34 pagesClinical Presentation and Case ManagementPatrick MukosoNo ratings yet
- 01 - Management of Critically Ill ChildrenDocument42 pages01 - Management of Critically Ill ChildrenMin MinTheinNo ratings yet
- Do'S and Don'Ts For DoctorsDocument4 pagesDo'S and Don'Ts For DoctorsTalha ENo ratings yet
- Emergency Triage Assessment and Treatment: National Neonatology ForumDocument6 pagesEmergency Triage Assessment and Treatment: National Neonatology ForumSatya Prakash TiwariNo ratings yet
- ASCIA Guidelines ADVANCED Acute Management Anaphylaxis Dec2016Document7 pagesASCIA Guidelines ADVANCED Acute Management Anaphylaxis Dec2016SPV DoctorNo ratings yet
- Medical EmergenciesDocument9 pagesMedical EmergenciesThe KittyNo ratings yet
- PHC EmergencyDocument42 pagesPHC Emergencyمحمداحمد محمدنور ابايزيدNo ratings yet
- Triage Emergency Signs and Normal VSDocument4 pagesTriage Emergency Signs and Normal VSbonziebuddyNo ratings yet
- Pediatric Life SupportDocument33 pagesPediatric Life SupportAndre montolaluNo ratings yet
- Stabilization CentreDocument64 pagesStabilization CentreShafaat HussainNo ratings yet
- Akp Important Guidelines 22 Guidlines Brief FinalDocument55 pagesAkp Important Guidelines 22 Guidlines Brief FinalRaheelNo ratings yet
- Ammonia Algorithm v9Document5 pagesAmmonia Algorithm v9Danielle ConcepcionNo ratings yet
- Anaphylaxis Guidance CardsDocument2 pagesAnaphylaxis Guidance CardsElein Datu SeruNo ratings yet
- ASCIA Guidelines Acute Management Anaphylaxis Dec2016Document5 pagesASCIA Guidelines Acute Management Anaphylaxis Dec2016kkkssbbNo ratings yet
- Morning Case Report: October 4th 2011Document22 pagesMorning Case Report: October 4th 2011Felicia adeline ChristianNo ratings yet
- Epilepsy Recovery Period - Second YrDocument3 pagesEpilepsy Recovery Period - Second YrBrian MaloneyNo ratings yet
- Pediatric Emergencies ?-1Document96 pagesPediatric Emergencies ?-1zahraaNo ratings yet
- Aclspediatric BradycardiaDocument2 pagesAclspediatric BradycardiasalamredNo ratings yet
- OB - Hypertensive DisordersDocument4 pagesOB - Hypertensive DisordersJasmine Nicole RemetreNo ratings yet
- Gut FeelingsDocument70 pagesGut FeelingsAngela MagnoNo ratings yet
- Emergency GuidelinesDocument11 pagesEmergency GuidelineswinstonappsNo ratings yet
- Pedia ReportDocument4 pagesPedia ReportBeda MalecdanNo ratings yet
- Eclampsia PPHDocument43 pagesEclampsia PPHizafamirna743No ratings yet
- Guidelines and Protocols Of: Diabetes EmergenciesDocument36 pagesGuidelines and Protocols Of: Diabetes Emergenciesyassen hassanNo ratings yet
- 3.15 Febrile Child Under 5 Years Without A FocusDocument8 pages3.15 Febrile Child Under 5 Years Without A Focusiffi82No ratings yet
- Chapter 5. Diarrhoea and Severe DehydrationDocument24 pagesChapter 5. Diarrhoea and Severe DehydrationSwarnavo DasNo ratings yet
- Sepsis Flow Chart FinalDocument2 pagesSepsis Flow Chart FinalDevindraPrptNo ratings yet
- Paediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Document14 pagesPaediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Nadia SalwaniNo ratings yet
- DKA Protocol TGDocument11 pagesDKA Protocol TGabelNo ratings yet
- Nursing Care During LaborDocument19 pagesNursing Care During LaborBaniwas Marie AgnesNo ratings yet
- Intravenous Insulin Prescription and Fluid Protocol: For Diabetic Keto-Acidosis (Dka)Document4 pagesIntravenous Insulin Prescription and Fluid Protocol: For Diabetic Keto-Acidosis (Dka)sunrise755No ratings yet
- O&G Off-Tag Assesment Logbook: Traces-Pdf-248732173Document9 pagesO&G Off-Tag Assesment Logbook: Traces-Pdf-248732173niwasNo ratings yet
- Anaphylaxis Wallchart 2018Document1 pageAnaphylaxis Wallchart 2018simranNo ratings yet
- Pediatric Advanced Life Support: Jan Bazner-Chandler CPNP, CNS, MSN, RNDocument65 pagesPediatric Advanced Life Support: Jan Bazner-Chandler CPNP, CNS, MSN, RNد. محمد فريد الغنامNo ratings yet
- Clinical Pathway Peds Sepsis 2012Document3 pagesClinical Pathway Peds Sepsis 2012Kim MedairosNo ratings yet
- Case ReportDocument27 pagesCase ReportRuni ArumndariNo ratings yet
- Pre EclampsiaDocument3 pagesPre EclampsiaStar SingsonNo ratings yet
- ASV - Treatment Protocol.Document5 pagesASV - Treatment Protocol.Kayalvizhi ThirumalNo ratings yet
- Severe Sepsisand Septic Shock GuidelinesDocument17 pagesSevere Sepsisand Septic Shock GuidelinesdrquamrulNo ratings yet
- Individualised Perioperative Open-Lung Approach Versus Standard Protective Ventilation in Abdominal Surgery (IPROVE) - A Randomised Controlled TrialDocument11 pagesIndividualised Perioperative Open-Lung Approach Versus Standard Protective Ventilation in Abdominal Surgery (IPROVE) - A Randomised Controlled TrialVic HNNo ratings yet
- Text Book Reading: Hipoxic Ischaemic EncephalopatyDocument23 pagesText Book Reading: Hipoxic Ischaemic EncephalopatyPanduRespatiNo ratings yet
- CasestudyvaccinesDocument5 pagesCasestudyvaccinesapi-323720899No ratings yet
- FEARS Database-FDA Database of glp1 Disproportionate Adverse EventsDocument20 pagesFEARS Database-FDA Database of glp1 Disproportionate Adverse EventsW Antonio Rivera MartínezNo ratings yet
- MSC Yoga - Semester 2 Hatha Yoga Pradipika - Answers To 10 Marks QuestionsDocument32 pagesMSC Yoga - Semester 2 Hatha Yoga Pradipika - Answers To 10 Marks QuestionsHenrickNo ratings yet
- DiphtheriaDocument1 pageDiphtheriaapi-275493729No ratings yet
- Chronic Renal Failure Due To EhrlichiosiDocument4 pagesChronic Renal Failure Due To EhrlichiosiUNICORN TIMENo ratings yet
- MediPrime Claim FormDocument8 pagesMediPrime Claim Formrahul0105100% (1)
- Steroids PowerPointDocument33 pagesSteroids PowerPointLeeYates340% (1)
- AfflictionsDocument12 pagesAfflictionsshiraaazNo ratings yet
- Health Guard Customer Information Sheet: Bajaj Allianz General Insurance Company LimitedDocument3 pagesHealth Guard Customer Information Sheet: Bajaj Allianz General Insurance Company LimitedKumud GandhiNo ratings yet
- FLM-porto Systemic AnastomosisDocument10 pagesFLM-porto Systemic AnastomosisYusuf Bin ZaidiNo ratings yet
- Thyroid DiseaseDocument30 pagesThyroid Diseasemy Lord JesusNo ratings yet
- Physical Medicine and Therapy. Means of PT. Therapeutic Exercise. Electrotherapy. Balneology and Climate MedicineDocument64 pagesPhysical Medicine and Therapy. Means of PT. Therapeutic Exercise. Electrotherapy. Balneology and Climate MedicineEcaterina GorganNo ratings yet
- Problems in Nutrition and EliminationDocument4 pagesProblems in Nutrition and EliminationBianca BautistaNo ratings yet
- What Is Kidney (Renal) Failure?: Female Urinary TractDocument6 pagesWhat Is Kidney (Renal) Failure?: Female Urinary TractthenameisvijayNo ratings yet
- NCMB316 Lec MidtermDocument28 pagesNCMB316 Lec Midterm2 - GUEVARRA, KYLE JOSHUA M.No ratings yet
- Daun PDFDocument5 pagesDaun PDFDaniel OktavianusNo ratings yet
- Glycogen Storage DiseaseDocument7 pagesGlycogen Storage DiseaseJuliana CorreaNo ratings yet
- CLT ScriptDocument3 pagesCLT ScriptMarioNo ratings yet
- Masumeen (As) - XKP - Duas From TIBB AL a-IMMA - Islamic Medical WisdomDocument124 pagesMasumeen (As) - XKP - Duas From TIBB AL a-IMMA - Islamic Medical WisdomAkbar Ali KhanNo ratings yet
- BoilsDocument48 pagesBoilsPű JäNo ratings yet