Professional Documents
Culture Documents
Ajayan 2013
Uploaded by
Dung TranOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajayan 2013
Uploaded by
Dung TranCopyright:
Available Formats
RESEARCH BRIEF
Clinical Spectrum and Predictive Risk Factors of Major Infections in
Hospitalized Children with Nephrotic Syndrome
PAYYADAKKATH AJAYAN, SRIRAM KRISHNAMURTHY, NIRANJAN BISWAL AND *JHARNA MANDAL
From Department of Pediatrics and *Microbiology, Jawaharlal Institute of Postgraduate Medical Education and Research
(JIPMER), Pondicherry, India.
Correspondence to: This observational study was conducted with the primary objective of studying the incidence
Dr Sriram Krishnamurthy, of major infections in nephrotic syndrome (NS), while the secondary objectives were to
Assistant Professor, evaluate the risk factors for and the etiological spectrum of major infections. Eighty six
Department of Pediatrics, JIPMER, children up to 13 years of age fulfilling the International Study of Kidney Disease in Children
Pondicherry 605006, India. (ISKDC) criteria for NS, who required 101 hospital admissions were recruited from November
drsriramk@yahoo.com. 2010 to July 2012. Major infections were defined as those that are disseminated, affecting
Received: October 15, 2012; deep organs, requiring hospitalization or potentially life-threatening. The incidence of major
Initial review: November 26, 2012; infections was 36.6%. Among the major infections, peritonitis and pneumonia together
Accepted: January 04, 2013. accounted for 72.9%, while urinary tract infections and cellulitis accounted for 16.2%. On
logistic regression, severe ascites and more severe clinical types of NS independently
predicted major infections, while serum cholesterol >400 mg/dL was the sole predictor of
peritonitis.
Keywords: India, Nephrotic syndrome, major infections, peritonitis.
C
hildren with nephrotic syndrome (NS) are SPSS version16, using Student t-test, Chi square test or
exposed to multiple infectious complications Fisher exact test. Logistic regression was used to analyse
resulting in significant mortality and predictors of major infections and peritonitis.
morbidity [1,2]. There is paucity of literature
regarding the clinical spectrum of major infections in Major infections were defined as disseminated,
childhood NS from developing countries in recent years. affecting deep organs, requiring hospitalization (e.g.
Knowledge of these parameters has therapeutic and cellulitis, disseminated varicella) or potentially life-
preventive relevance [2]. We, therefore, conducted the threatening [8]. Specific major infections were defined
present study. as follows:
METHODS (1) Peritonitis: Abdominal pain, tenderness, distension,
diarrhea, or vomiting, with ascitic fluid >100
This prospective study was conducted from November leukocytes/mm3 and minimum 50% neutrophils and/
2010 to July 2012 at a tertiary hospital, and was approved or positive culture [3,9,10].
by the Institutional ethics committee. The primary
objective was to study the incidence of major infections (2) Pneumonia: fast breathing and chest indrawing with
in NS, while secondary objectives were to evaluate (a) chest X-ray confirmation [1].
the risk factors for major infections and (b) their (3) Urinary tract infection (UTI): Bacterial colony count
etiological spectrum. Children below 13 years of age, of >105 organisms/mL in a clean-catch midstream
fulfilling ISKDC diagnostic criteria for NS [3-5] were urine sample with fever (>38.5ºC), dysuria or
included if hospitalization was required for: major increased urination frequency [1].
infections, severe anasarca, shock, seizures, thrombosis,
unconsciousness, respiratory distress, tetany, or for renal (4) Cellulitis: Erythema, warmth, swelling, fever and
biopsy. local tenderness in any body part.
The incidence of major infections in NS was (5) Meningitis: Fever and one of the following: neck
estimated as 35% [2,6,7]. Assuming 10% variation with rigidity, altered sensorium, seizures, with
95% confidence, sample size for estimating incidence of confirmation by cerebrospinal fluid cytology,
major infections was 88. Results were analyzed with biochemistry and culture.
INDIAN PEDIATRICS 779 VOLUME 50__AUGUST 15, 2013
AJAYAN, et al. MAJOR INFECTIONS IN NEPHROTIC SYNDROME
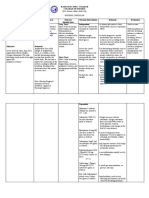
Severe ascites was defined as tense ascites or ascites TABLE I CLINICAL AND BIOCHEMICAL PROFILE OF STUDY
with dyspnea. Generalized edema (including scrotal SUBJECTS (AMONG 101 HOSPITAL ADMISSIONS * )
edema, vulval edema or severe ascites) was considered as Characteristics Value
severe anasarca. Frequently relapsing (FRNS), steroid
dependent (SDNS), steroid resistant (SRNS) or Age (y) 6.8 ± 3.5
infrequently relapsing NS (IFRNS) were considered as Duration of nephrotic syndrome (y)# 1.9 ± 1.7
‘more severe clinical types of NS’. Duration of edema before presentation (wks) 2.8 ± 2.4
Sex (male) 53 (52.5)
NS was investigated and managed as per Indian
Pneumococcal vaccine received 6 (5.9)
Pediatric Nephrology Group guidelines [3]. Blood and
Major infections, n(%) 37 (36.6)
urine cultures; and peritoneal, pleural or cerebrospinal
Spontaneous bacterial peritonitis 14 (37.8)
fluid analysis and culture were done when clinically
Pneumonia 13 (35.1)
indicated.
Urinary tract infection 3 (8.1)
RESULTS Cellulitis 3 (8.1)
86 children with NS, requiring 101 hospitalizations, were Osteomyelitis 1 (2.7)
recruited. Peritonitis and pneumonia accounted for 27 out Disseminated varicella 1 (2.7)
of the 37 children with major infections (72.9%) (Table Herpes zoster 1 (2.7)
I). Urine cultures were sent in 10 cases (3 had UTI); Meningitis 1 (2.7)
while ascitic tap was performed in 20 (14 had peritonitis). Clinical type of nephrotic syndrome
The infectious agents included E.coli (2 cases) and 1st episode 45 (44.6)
Klebsiella (1 case) in UTI, Pneumococcal peritonitis (1 IFRNS 21 (20.8)
case), Methicillin Resistant Staphylococcus aureus FRNS 9 (8.9)
(MRSA) in cellulitis and osteomyelitis (1 each), and SDNS 7 (6.9)
Pseudomonas in cellulitis (1 case). One child with SRNS SRNS 19 (18.8)
(having chronic glomerulonephritis) died of pneumonia. Severe ascites 62 (61.4)
Children aged >4 years constituted 78.6% of peritonitis, Scrotal edema (among 53 males) 20 (37.7)
while duration of NS >2 years constituted 64.3% of Vulval edema (among 48 females) 16 (33.3)
peritonitis. The mean age of children with peritonitis was Past history of major infections # 18 (17.8)
7.9 ± 3.3 years, whereas mean age of children with
Immunosuppressants received
pneumonia was 6.4 ± 3.1 years.
Prednisolone only 84 (83.3)
Web Table I depicts predictors of peritonitis on Levamisole with prednisolone 6 (5.9)
univariate analysis. On logistic regression, Cyclophosphamide with prednisolone 3 (2.9)
hypercholesterolemia >400 mg/dL independently Cyclosporine with prednisolone 8 (7.9)
predicted peritonitis (OR = 6.89 (1.30 – 36.43), P =
Histopathology (among 12 renal biopsies)
0.023).
Focal segmental glomerulosclerosis 3 (25)
Predictors for major infections on logistic regression Mesangioproliferative glomerulonephritis 4 (33.3)
were ‘more severe clinical types of NS’ when compared Minimal change disease 2 (16.7)
to first episode of NS, i.e. IFRNS [OR 9.94 (2.56 -38. C3 nephropathy 1 (8.3)
67), P< 0.01], FRNS [OR 28.19 (3.73- 212.28) , P< IgA nephropathy 1 (8.3)
0.01], SDNS [OR 25.84 (2.89-231.1), P< 0.01], SRNS Chronic glomerulonephritis 1 (8.3)
[OR 4.9 (2.56 -38. 67), P=0.033]; and severe ascites [OR Death 1 (0.9)
0.15(0.05-0.49), P< 0.01]. Serum albumin (g/dL) 2.1 ± 0.6
DISCUSSION Serum cholesterol (mg/dL) 419.8 ± 128.1
Blood urea (mg/dL) 35.2 ± 28.1
In our study, major infections constituted 36.6% of the
Serum creatinine (mg/dL) 0.7 ± 0.6
subjects. Other studies reported incidence ranging from
Spot urine protein: creatinine ratio 2.89 ± 0.3
32% to 38% [2,7]. The commonest major infection was
GFR (mL/m2/min)(Schwartz formula) 112.2 ± 75.9
peritonitis (13.8% incidence), as compared to 1.4% to
16% in other studies [1,2,7,11,12]. Ascitic fluid culture * Indications for hospitalization included severe anasarca – 55 cases
was positive in only 1 patient. Eleven of the 14 cases with (including 11 with scrotal edema), major infections- 37 (one case of
pneumonia presented with shock), renal biopsy- 6, tetany -2 and
peritonitis were initially seen by general practitioners
seizures- 1 case. #These included peritonitis in 9, UTI in 6, pneumonia
who prescribed antibiotics. These were ineffective but in 2 and cellulitis in 1 case, All values in no. (%) and mean ± SD.
INDIAN PEDIATRICS 780 VOLUME 50__AUGUST 15, 2013
AJAYAN, et al. MAJOR INFECTIONS IN NEPHROTIC SYNDROME
probably contributed to low ascitic fluid culture positivity act as guarantor of the paper.
[2]. Pneumonia was the second commonest infection in Funding: None; Competing interests: None stated.
the subjects (12.9%), as compared to 3.9% to14% in REFERENCES
Indian studies [1,2]. UTI was relatively uncommon in
our subjects. In consonance with our observations, 1. Alwadhi RK, Mathew JL, Rath B. Clinical profile of
Srivastava, et al. [7] reported no episodes of UTI in their children with nephrotic syndrome not on glucocorticoid
therapy, but presenting with infection. J Paediatr Child
study. In other studies, UTI incidence ranged from 13.7%
Health. 2004;40:28–32.
to 46% [1]. These variations probably reflect 2. Gulati S, Kher V, Gupta A, Arora P, Rai PK, Sharma
geographical or socioeconomic heterogeneity of patient RK. Spectrum of infections in Indian children with
populations. nephrotic syndrome. Pediatr Nephrol. 1995;9:431-4.
3. Indian Pediatric Nephrology Group, Indian Academy of
Peritonitis in NS has been usually described to occur
Pediatrics, Bagga A, Ali U, Banerjee S, Kanitkar M,
within initial few years after diagnosis and in younger Phadke KD, et al. Management of steroid sensitive
children [6,13,14]. Our results; however, indicate that nephrotic syndrome: revised guidelines. Indian Pediatr.
irrespective of age or increasing duration of disease 2008;45:203-14.
(probably related to multiple relapses) [1,2,7,13,14], 4. Early identification of frequent relapsers among children
major infections prevail in NS. Immunosuppressive with minimal change nephrotic syndrome. A report of the
agents did not predict major infections, as in some studies International Study of Kidney Disease in Children. J
[2,6], suggesting that the origin of infections in NS is far Pediatr. 1982;101:514-18.
more complex and multifactorial. 5. Kher KK. Urinalysis. In: Kher KK, Makker SP ed.
Clinical Pediatric Nephrology 1st edn. New York:
Hypercholesterolemia >400 mg/dL was a risk factor McGraw-Hill, 1992. p. 186-8.
for peritonitis. Hypercholesterolemia may have a direct 6. Senguttuvan P, Ravanan K, Prabhu N, Tamilarasi V.
pathophysiological role as hypercholesterolemic serum Infections encountered in childhood nephrotics in a
inhibits lymphocyte proliferation in response to antigen pediatric renal unit. Indian J Nephrol. 2004;14:85-8.
7. Srivastava RN, Mooudgil A, Khurana O. Serious
stimulation [15] Secondly, hypercholesterolemia is an
infections and mortality in nephrotic syndrome. Indian
indirect consequence of hypoalbuminemia which has Pediatr. 1987;24:1077-80.
been mentioned as a predictor of peritonitis in NS [2,13]. 8. Irastorza GR, Olivares N, Arruza IR, Berriotxoa AM,
The merits of our study include prospective design, Egurbide MV, Aguirre C. Predictors of major infections
in systemic lupus erythematosus. Arthritis Res Ther.
and a large sample size. Our study also has limitations.
2009;11:R109.
Due to resource constraints, detailed pathophysiological 9. Wei CC, Yu IW, Lin HW, Tsai AC. Occurrence of
investigations were not undertaken. Secondly, although infection among children with nephrotic syndrome during
the predictors for major infections and peritonitis were hospitalizations. Nephrology (Carlton). 2012;17:681-8.
analyzed, this study is not powered enough for the same. 10. Bagga A, Srivastava RN. Nephrotic syndrome. In:
Srivastava RN, Bagga A. Pediatric Nephrology. 5th ed.
Our hospital caters to patients of low socioeconomic New Delhi: Jaypee; 2005. p. 195 -234.
status, which explains poor coverage of pneumococcal 11. Gorensek MJ, Lebel MH, Nelson JD. Peritonitis in
vaccination (6%). Improving pneumococcal vaccination children with nephrotic syndrome. Pediatrics. 1988;
coverage in NS could be a potentially important strategy 81:849-56.
to decrease the incidence of major infections. In the 12. Feinstein EI, Chesney RW, Zelikovic I. Peritonitis in
presence of hypercholesterolemia >400 mg/dL, an childhood renal disease. Am J Nephrol. 1988; 8:147–65.
aggressive search for serious infections is essential along 13. Hingorani SR, Weiss NS, Watkins SL. Predictors of
with prompt and aggressive antibiotic therapy. peritonitis in children with nephrotic syndrome. Pediatr
Nephrol. 2002;17:678-82.
Contributors: PA, SK and NB: were involved in management 14. Uncu N, Bulbul M, Yildiz N. Primary peritonitis in
of the patients; PA: collected the data, reviewed the literature children with nephrotic syndrome: results of a 5-year
and drafted the manuscript; SK: conceptualized the study, multicenter study. Eur J Pediatr. 2010;169:73-6.
reviewed the literature and critically reviewed the manuscript; 15. Anderson S, Garcia DL, Brenner BM. Renal and systemic
NB: also critically reviewed the manuscript; JM: supervised the manifestations of glomerular disease. In: Brenner BM,
laboratory tests. All authors contributed to writing the paper Rector FC Jr, eds. The kidney. 4th ed. Philadelphia:
and approved the final version of the manuscript and SK: shall Saunders; 1991. p. 1831-70.
INDIAN PEDIATRICS 781 VOLUME 50__AUGUST 15, 2013
You might also like
- NECROTIZINGDocument6 pagesNECROTIZINGphuong mai leNo ratings yet
- Streptococcus suis infections in ThailandDocument6 pagesStreptococcus suis infections in ThailandAram Dumnoen-ngamNo ratings yet
- Causes and Factors of Persistent Pneumonia in ChildrenDocument4 pagesCauses and Factors of Persistent Pneumonia in ChildrenBereket temesgenNo ratings yet
- Clinical Feature and Etiology of Septic Arthritis and Osteomyelitis in ChildrenDocument5 pagesClinical Feature and Etiology of Septic Arthritis and Osteomyelitis in ChildrenIfit Bagus ApriantonoNo ratings yet
- Peds 2020029249Document17 pagesPeds 2020029249nana wardhaniNo ratings yet
- Bacterial Etiology of Pediatric Subacute Hematogenous OsteomyelitisDocument6 pagesBacterial Etiology of Pediatric Subacute Hematogenous OsteomyelitismiNo ratings yet
- Nosocomial Infections in The General Pediatric Wards of A Hospital in TurkeyDocument4 pagesNosocomial Infections in The General Pediatric Wards of A Hospital in TurkeyAmira AmouraNo ratings yet
- Prasad 2012Document5 pagesPrasad 2012Gladys OliviaNo ratings yet
- JurnalDocument5 pagesJurnalgustina mariantiNo ratings yet
- Journal Siklus Anak 5Document5 pagesJournal Siklus Anak 5dwi-148502No ratings yet
- Diagnostic Significance of Blood Eosinophilia in Returning TravelersDocument5 pagesDiagnostic Significance of Blood Eosinophilia in Returning TravelersMira Permatasari LunardiNo ratings yet
- CKD PDFDocument7 pagesCKD PDFniaNo ratings yet
- Eid18 91 PDFDocument5 pagesEid18 91 PDFAnonymous fOcbAtNo ratings yet
- Clinicopathological Profile and Outcome of Infection-Related Glomerulonephritis (Irgn) :a Single Center ExperienceDocument7 pagesClinicopathological Profile and Outcome of Infection-Related Glomerulonephritis (Irgn) :a Single Center ExperienceIJAR JOURNALNo ratings yet
- (10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenDocument6 pages(10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenFatima RamirezNo ratings yet
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocument4 pagesClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaNo ratings yet
- AygunDocument5 pagesAygunotheasNo ratings yet
- Radiological Features of AIDS-related Pneumocystis Jiroveci InfectionDocument3 pagesRadiological Features of AIDS-related Pneumocystis Jiroveci InfectionJavi MontañoNo ratings yet
- Clinical Microbiology and InfectionDocument9 pagesClinical Microbiology and InfectionAguilarKrystell'No ratings yet
- Scrub Typhus Meningitis in ChildrenDocument6 pagesScrub Typhus Meningitis in Childrenandrian dwiNo ratings yet
- RequestedDocument9 pagesRequestedGaurav MauryaNo ratings yet
- Update On Endocarditis-Associated GlomerulonephritisDocument9 pagesUpdate On Endocarditis-Associated GlomerulonephritisWenny A. YuliantiNo ratings yet
- Extraintestinal Focal Infections in Adults With Nontyphoid Salmonella 2006Document10 pagesExtraintestinal Focal Infections in Adults With Nontyphoid Salmonella 2006Carlos Antonio Arrieta NieblesNo ratings yet
- 2017 Kdigo CKD MBD GL UpdateDocument8 pages2017 Kdigo CKD MBD GL UpdateJorge Luis Corral VillalbaNo ratings yet
- Commonly Occurring Bacteria in Diabetic Foot Infections and Their Sensitivity To Various AntibioticsDocument5 pagesCommonly Occurring Bacteria in Diabetic Foot Infections and Their Sensitivity To Various Antibioticsdoctor wajiha100% (1)
- Epidemiology and Clinical Manifestations of Mucormycosis CMIDocument9 pagesEpidemiology and Clinical Manifestations of Mucormycosis CMIDINESH VENKATESANNo ratings yet
- Wound Infection Secondary To Snakebite: ResearchDocument5 pagesWound Infection Secondary To Snakebite: ResearchPuti Alifa RizqiaNo ratings yet
- TrombositopeniaDocument2 pagesTrombositopeniaSoraya RezekiNo ratings yet
- Profile of Acute Epididymo-Orchitis Patients in Arifin Achmad Regional General Hospital Riau Province, IndonesiaDocument5 pagesProfile of Acute Epididymo-Orchitis Patients in Arifin Achmad Regional General Hospital Riau Province, IndonesiaKuran AtikaNo ratings yet
- 21, Malaria Vs Dengue 2020Document4 pages21, Malaria Vs Dengue 2020Raquel FernandezNo ratings yet
- Jog 9999 0Document7 pagesJog 9999 0Rocio Ayaque AguirreNo ratings yet
- Clinical Features and Aetiology of Septic Arthritis in Northern Israel 2005Document5 pagesClinical Features and Aetiology of Septic Arthritis in Northern Israel 2005HoussemSoltanaNo ratings yet
- 10 1016@j Jaad 2019 05 096Document8 pages10 1016@j Jaad 2019 05 096JohnNo ratings yet
- 3 Septicshock SIRS PDFDocument11 pages3 Septicshock SIRS PDFRhobbigfirly UnggulNo ratings yet
- Characteristics of Bacteremia Between Community-Acquired and NosocomialDocument7 pagesCharacteristics of Bacteremia Between Community-Acquired and NosocomialKarla MéndezNo ratings yet
- 100220080112Document8 pages100220080112Nabil MrhiliNo ratings yet
- 1 s2.0 S1198743X14632079 MainDocument9 pages1 s2.0 S1198743X14632079 MainAizaz HassanNo ratings yet
- Art 19644Document5 pagesArt 19644Francisca BallesterosNo ratings yet
- ICU Infection Sources in Sepsis PatientsDocument5 pagesICU Infection Sources in Sepsis PatientsEndah Novianti SoenarsinNo ratings yet
- Tuberculous Spondylitis: Risk Factors and Clinical/paraclinical Aspects in The South West of IranDocument6 pagesTuberculous Spondylitis: Risk Factors and Clinical/paraclinical Aspects in The South West of IrantheresiaaquilaNo ratings yet
- Adam 2018Document7 pagesAdam 2018yuastikapsNo ratings yet
- International Journal of Infectious DiseasesDocument8 pagesInternational Journal of Infectious DiseasesDara AlfiaNo ratings yet
- Surveillance of Extrapulmonary Nontuberculous Mycobacteria InfectionsDocument4 pagesSurveillance of Extrapulmonary Nontuberculous Mycobacteria Infectionsluck2livNo ratings yet
- Viruses and Bacteria in Sputum Samples of Children With CAPDocument8 pagesViruses and Bacteria in Sputum Samples of Children With CAPZieNo ratings yet
- MOJ Vol7 Issue2 27Document2 pagesMOJ Vol7 Issue2 27Michael Steven Sanchez PinedaNo ratings yet
- Espondilodiscitis Infecciosa Por Patógenos Poco ComunesDocument5 pagesEspondilodiscitis Infecciosa Por Patógenos Poco ComunesOthoniel RamirezNo ratings yet
- Peritoneal Dialysis-Related Peritonitis Caused by Pseudomonas Species: Insight From A Post-Millennial Case SeriesDocument9 pagesPeritoneal Dialysis-Related Peritonitis Caused by Pseudomonas Species: Insight From A Post-Millennial Case SeriesDesi HutapeaNo ratings yet
- Bacterial and Fungal Coinfections in Covid 19 Patients Hospitalized During The New York City Pandemic SurgeDocument5 pagesBacterial and Fungal Coinfections in Covid 19 Patients Hospitalized During The New York City Pandemic SurgeReynaldo CarvajalNo ratings yet
- Candidiasis in PICUDocument6 pagesCandidiasis in PICUMeirinda HidayantiNo ratings yet
- Thwaites 2004Document11 pagesThwaites 2004Navisa HaifaNo ratings yet
- Actualización en Sepsis y Choque Septico 2023Document23 pagesActualización en Sepsis y Choque Septico 2023Alberto De La VegaNo ratings yet
- Tuberculous Pericarditis Optimal Diagnosis and ManagementDocument8 pagesTuberculous Pericarditis Optimal Diagnosis and ManagementLink BuiNo ratings yet
- Associated Clinical Factors For Serious Infections in Patients With Systemic Lupus ErythematosusDocument8 pagesAssociated Clinical Factors For Serious Infections in Patients With Systemic Lupus ErythematosusadeliaputriNo ratings yet
- 149 FullDocument10 pages149 Fullসোমনাথ মহাপাত্রNo ratings yet
- Pathomorphological Peculiarities of Tuberculous Meningoencephalitis Associated With HIV InfectionDocument6 pagesPathomorphological Peculiarities of Tuberculous Meningoencephalitis Associated With HIV InfectionBesseMarwah AgusHusainNo ratings yet
- 10MJMS26012019 Oa7Document8 pages10MJMS26012019 Oa7senkonenNo ratings yet
- Resistencia de Uropatógenos en Infecciones de Tracto Urinario en Leon NicaraguaDocument4 pagesResistencia de Uropatógenos en Infecciones de Tracto Urinario en Leon NicaraguaMiguel AnguianoNo ratings yet
- Full TextDocument34 pagesFull TextkanNo ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Diagnostics to Pathogenomics of Sexually Transmitted InfectionsFrom EverandDiagnostics to Pathogenomics of Sexually Transmitted InfectionsSunit Kumar SinghNo ratings yet
- Journal of Infection and Public HealthDocument5 pagesJournal of Infection and Public HealthDung TranNo ratings yet
- Daily Corticosteroids Reduce Infection-Associated 2011 63Document7 pagesDaily Corticosteroids Reduce Infection-Associated 2011 63Mutiara RizkyNo ratings yet
- Immunology of Idiopathic Nephrotic Syndrome: ReviewDocument12 pagesImmunology of Idiopathic Nephrotic Syndrome: ReviewDung TranNo ratings yet
- Spontaneous Bacterial Peritonitis Organism-Specific Therapy - Specific Organisms and Therapeutic RegimensDocument2 pagesSpontaneous Bacterial Peritonitis Organism-Specific Therapy - Specific Organisms and Therapeutic RegimensDung TranNo ratings yet
- Journal of Infection and Public HealthDocument5 pagesJournal of Infection and Public HealthDung TranNo ratings yet
- ZH 800906003455Document8 pagesZH 800906003455Dung TranNo ratings yet
- Pippard 1978Document4 pagesPippard 1978Dung TranNo ratings yet
- BR J Haematol - 2021 - Shah - Guidelines For The Monitoring and Management of Iron Overload in Patients WithDocument15 pagesBR J Haematol - 2021 - Shah - Guidelines For The Monitoring and Management of Iron Overload in Patients WithDung TranNo ratings yet
- Clubfoot ThesisDocument7 pagesClubfoot ThesisCollegePaperGhostWriterAkron100% (2)
- NCP #2Document2 pagesNCP #2Faith CalimlimNo ratings yet
- Aki To CKDDocument22 pagesAki To CKDSrinivas PingaliNo ratings yet
- Ste Conchem q4m5 Ffhnas Annex PDFDocument31 pagesSte Conchem q4m5 Ffhnas Annex PDFJesus GombaNo ratings yet
- Nursing care plan for post-op cataract surgeryDocument2 pagesNursing care plan for post-op cataract surgeryFranz goNo ratings yet
- Drugs and Therapeutics in DentistryDocument51 pagesDrugs and Therapeutics in DentistryEdwina JacklinNo ratings yet
- The Gram-Positive Bacilli of Medical Importance: Group 5Document148 pagesThe Gram-Positive Bacilli of Medical Importance: Group 5Tolentino, Ma. LykaNo ratings yet
- TyphusDocument21 pagesTyphusJ J MEDIANo ratings yet
- Abcde ApproachDocument3 pagesAbcde ApproachHala BahaaNo ratings yet
- Antibiotic Time-Out ChecklistDocument2 pagesAntibiotic Time-Out ChecklistNawwal Naeem100% (1)
- P2 Funda LecDocument8 pagesP2 Funda LecAira Mae R. AndradaNo ratings yet
- Ra 9262Document43 pagesRa 9262Kim ZeNo ratings yet
- Full Download Test Bank For Pathophysiology A Clinical Approach Second Edition Carie A Braun PDF Full ChapterDocument18 pagesFull Download Test Bank For Pathophysiology A Clinical Approach Second Edition Carie A Braun PDF Full Chapterpicheywitlingaip34100% (18)
- Isosorbide DinitrateDocument1 pageIsosorbide Dinitrate202110439No ratings yet
- وتين ٥Document26 pagesوتين ٥Mohammad AlrefaiNo ratings yet
- DKA Texas Children 19Document9 pagesDKA Texas Children 19Eduardo RuizNo ratings yet
- Caroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesDocument15 pagesCaroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesFarid RakhmanNo ratings yet
- Severe Anxiety Case StudyDocument2 pagesSevere Anxiety Case StudyCamille SindayNo ratings yet
- Mental Status Assessment FormDocument3 pagesMental Status Assessment FormJohn Paolo OrioNo ratings yet
- UntitledDocument264 pagesUntitledFed Espiritu Santo GNo ratings yet
- Daren G. Linatoc, RN, RM, LPT, Man, MaedDocument7 pagesDaren G. Linatoc, RN, RM, LPT, Man, MaedMike Faustino SolangonNo ratings yet
- 2020 Moreira Relationship Between Adverse Childhood Experiences and Psychopathy 1-S2.0-S1359178920301567-MainDocument14 pages2020 Moreira Relationship Between Adverse Childhood Experiences and Psychopathy 1-S2.0-S1359178920301567-MainjbNo ratings yet
- ANAPHYLAXIS CAREDocument6 pagesANAPHYLAXIS CAREKirstin del CarmenNo ratings yet
- ThyrotoxicosisDocument16 pagesThyrotoxicosisFiorella Peña MoraNo ratings yet
- DD DemensiaDocument25 pagesDD DemensiaPutri HarahapNo ratings yet
- Case Analysis - Pregnant With AsthmaDocument1 pageCase Analysis - Pregnant With AsthmaJanine mae MacaraigNo ratings yet
- Sleep Study ThesisDocument5 pagesSleep Study Thesisamandasanchezalbuquerque100% (2)
- BurnsDocument8 pagesBurnsNursiaNo ratings yet
- German Measles Lesson PlanDocument17 pagesGerman Measles Lesson PlanKhushboo SinghNo ratings yet
- MCQ On Disorder of RBCS: Group (4) PresentsDocument6 pagesMCQ On Disorder of RBCS: Group (4) PresentsIrekton GGNo ratings yet