Professional Documents
Culture Documents
Pediatric Advanced Life Support Provider Manual (PDFDrive)
Uploaded by
will0%(1)0% found this document useful (1 vote)
213 views286 pagesPALS Manual from 2012
Original Title
Pediatric Advanced Life Support Provider Manual ( PDFDrive )
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPALS Manual from 2012
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0%(1)0% found this document useful (1 vote)
213 views286 pagesPediatric Advanced Life Support Provider Manual (PDFDrive)
Uploaded by
willPALS Manual from 2012
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 286
a
=. American Neen nan
a t Heart POR Curiae i.
a CSET (a
Pediatric
Advanced Life Support
ev har
as gee
a
é
a
Ltr
Pediatric
American
Heart
Associations
Advanced Life Support
PROVIDER MANUAL
Editors
Leon Chameides, MD, Conient Consultant
Ficardo A, Samson, MD, Associete Science Editor
Stephen M. Schesnaydor, MD, Associate Science Ealtor
Mary Fran Hazinski, PN, MSN, Senior Science Editor
‘Senior Managing Editor
Jennifer Asheraft, RN, BSN
Special Contributors
Mare D. Berg, MO
efirey M, Berman, MD
Laure Goniey, BS, RAT, ACP, NPS
Allen Fi. de Gaen, MD
‘Aaron Donoghue, MD, MSCE
Melinda L. Fiedor Hamiton, MID, MSc
Monica €. Kleinman, MD
‘Mary Ann Mctiel, MA, NREMT-P
Brenda Schoolfeld, PALS Writer
Cindy Tuttle, BN, BSN
‘Salle Young, PharmD, BOPS, Pharmacotherapy Editor
© 2011 Amarcan Heart Association
ISBN 076-0-67403-527-1
Printed in the United States ot America
Fst American Heart Associaton Priving Octobor 2011
10987654321
Pediatric Subcommittee 2010-2011
Mare D. Berg, MD, Chair
Monica E. Kloinman, MD, Immediate Past Chair, 2007-2009
ina L. Atkins, MD
Kathleen Brown, MD.
‘Adam Cheng, MD
Leura Conley, BS, RAT, ROP, NPS.
‘Allan R. de Caen, MD
Aaron Donoghue, MD, MSCE
Melinda L. Fiedor Hamiton, MD. MSC
Ericka L. Fink, MD
Eugene B. Freid, MO
Cheryl K. Gooden, MD
Sharon E Mace, MD
Bradley S. Marino, MD, MPP, MSCE
Feylon Meeks, RN, BSN, MS, MSN, EMT, PhD
Jeffrey M. Perlman, MB, ChE
Lester Proctor, MD
Faiga A. Qureshi, MD
Kennith Hans Sartoretl, MD
Wendy Simon, MA
Mark A. Terry, MPA, NREMT-P
Avoxis Topjan, MD
Else W. van der Jagt, MD, MPH
Parti
Course Overview
Course Objectives
Cognitive Course Objectives
Psychomotor Course Objectives
Course Description
BLS Competency Testing
Skills Stations
PALS Core Case Discussions and
‘Simulations
PALS Core Case Testing Stations
Written Exam
Precourse Preparation
Precourse Self-Assessment
BLS Skills
ECG Rhythm identification
Basic Pharmacology
Practical Application of Knowledge
to Clinical Scenarios
Course Materials
PALS Provider Manual
PALS Student Website
Course Completion Requirements
Suggested Reading List
6862088 8m NNN A GS
aooe ee
Part 2
Systematic Approach to the
Seriously Hl or Injured Child
Overview
Rapid Intervention to Prevent
Cardiac Arrest
Learning Objectives
Preparation for the Course
PALS Systematic Approach Algorithm
Initial Impression
Evaluate-Identify-Intervene
Evaluate
Identity
Intervene
Continuous Sequence
Determine If Problem Is
Life Threatening
Primary Assessment
Airway
Breathing
Circulation
Disability
Exposure
Life-Threatening Problems
Interventions
Secondary Assessment
Focused History
Focused Physical Examination
Diagnostic Tests
Arterial Blood Gas
Venous Blood Gas
Hemoglobin Concentration
Central Venous Oxygen Saturation
Arterial Lactate
Central Venous Pressure Monitoring
Invasive Arterial Pressure Monitoring
Chest X-Ray
Electrocaraiogram
Echocardiogram
Peak Expiratory Flow Rate
‘Suggested Reading List
Part 3
Effective Resuscitation
Team Dynamics
Overview
Learning Objectives
Preparation for the Course
Roles of the Team Leader and
Team Members
Role of the Team Leader
Role of the Team Member
Elements of Effective Resuscitation
‘Team Dynamics
Closed-Loop Communication
Clear Messages
Clear Roles and Responsibilities
Knowing Limitations
Knowledge Sharing
SBRBSRRB
8
BBBBBEBBSY
Se eee 8
Constructive Intervention
Reevaluation and Summarizing
Mutual Respect
Suggested Reading List
Part 4
Recognition of Respiratory
Distress and Failure
Overview
Learning Objectives
Preparation for the Course
Fundamental Issues Associated With
Respiratory Problems
Impairment of Oxygenation and
Ventilation in Respiratory Problems
Physiology of Respiratory Disease
Identification of Respiratory
Problems by Severity
Respiratory Distress
Respiratory Failure
Identification of Respiratory
Problems by Type
Upper Airway Obstruction
Lower Airway Obstruction
Lung Tissue Disease
Disordered Contro! of Breathing
Summary: Recognition of
Respiratory Problems Flowcharts
Suggested Reading List
Part 5
Management of Respiratory
Distress and Failure
Overview
Learning Objectives
Preparation for the Course
Initial Management of Respiratory
Distress and Failure
Principles of Targeted Management
Management of Upper
Airway Obstruction
General Management of Upper
Airway Obstruction
Specific Management of Upper
Airway Obstruction by Etiology
Management of Lower Airway
Obstruction
General Management of Lower
Airway Obstruction
Specific Management of Lower
Airway Obstruction by Etiology
Management of Lung Tissue Disease
Goneral Management of Lung
Tissue Disease
Specific Management of Lung
Tissue Disease by Etiology
dered
Management of
Control of Breathing
General Management of Disordered
Control of Breathing
Specific Management of Disordered
Control of Breathing by Etiology
‘Summary: Management of
Respiratory Emergencies Flowchart
Suggested Reading List
Resources for Management of
Respiratory Emergencies
Bag-Mask Ventilation
Overview
Preparation for the Course
How to Select and Prepare the
Equipment
49
50
50
ot
52
82
55
87
87
59
61
6
61
61
61
How to Test the Device
How to Position the Child
How to Perform Bag-Mask Ventilation
How to Deliver Effective Ventilation
Endotracheal Intubation
Potential Indications
Preparation for Endotracheal
Intubation
Part 6
Recognition of Shock
Overview
Learning Objectives
Preparation for the Course
Definition of Shook
Pathophysiology of Shock
‘Components of Tissue
Oxygen Delivery
Stroke Volume
Compensatory Mechanisms
Effect on Blood Pressure
Identification of Shock by Severity
(Effect on Blood Pressure)
Compensated Shock
Hypotensive Shock
Identification of Shock by Type
Hypovolemic Shock
Distributive Shock
Cardiogenic Shock
Obstructive Shock
Recognition of Shock Flowchart
Suggested Reading List
838
70
nm
Rn
2
Part 7
Management of Shock
Overview
Learning Objectives
Preparation for the Course
Goals of Shock Management
Warning Signs
Fundamentals of Shock
Management
Optimizing Oxygen Content of
the Blood
Improving Volume and Distribution
of Cardiac Output
Reducing Oxygen Demand
Correcting Metabolic Derangements
Therapeutic End Points
General Management of Shock
Components of General
Management
Summary: initial Management
Principles
Fluid Therapy
‘sotonic Crystalloid Solutions
Colloid Solutions
Crystalloid vs Colloid
Rate and Volume of Fluid
Administration
Rapid Fluid Delivery
Frequent Reassessment During
Fluid Resuscitation
Indication for Blood Products
Complications of Rapid
Administration of Blood Products
Glucose
Glucose Monitoring
Diagnosis of Hypoglycemia
Management of Hypoglycemia
Management According to.
Type of Shock
Management of Hypovolemic Shock
‘Management of Distributive Shock
‘Management of Septic Shock
Management of Anaphylactic Shock
Management of Neurogenic Shock
Management of Cardiogenic Shock
‘Management of Obstructive Shock
Management of Shock Flowchart
Suggested Reading List
Resources for Management of
Circulatory Emergencies 109
Intraosseous Access 109
Sites for 10 Access 109
Contraindications 109
Procedure (Proximal Tibia) 109
After IO Insertion
Color-Coded Length-Based
Resuscitation Tape
Part 8
Recognition and Management
of Bradycardia
Overview
Learning Objectives
Preparation for the Course
Definitions
Recognition of Bradycardia
Signs and Symptoms of Bradycardia
ECG Characteristics of Bradycardia
Types of Bradyarrhythmias
Management: Pediatric Bradycardia ‘Summary of Emergency
With a Pulse and Poor Perfusion Interventions 499
Algorithm 117 Pediatric Tachycardia With a Pulse
Identify and Treat Underlying and Adequate Perfusion Algorithm 134
Cause (Box 1) 118 Initial Management (Box 1) 135
Reassess (Bax?) in Evaluate QRS Duration (Box 2) 135
i Adequate Respiration and
Perfusion (Box 4a) 118 et con of ari § 195
ip apscycatei rel CespRCAY Treat Cause of SVT (Boxes 7 and 8) 135
‘Compromise Persist: Perform Wide QRS, Possible VT vs SVT
CPR (Box 3) 118 (Boxes 9, 10, and 17) 135
Reassess Rhythm (Box 4) 119 Pharmacologic Conversion vs
‘Administer Medications (Box 5) 119 Eleven! ee a ° iad
Pediatric Tachycardia With a Pulse
Consider Cardiac Pacing (60x 5) 118 snd Poor Perfusion Algorithm ‘se
Treat Underlying Causes (Box 5) 120 Initial Management (Box 1) 4138
Pulseless Arrest (Box 6) 170) Evaluate QRS Duration (Box 2) 138
Suagested Reacing List 10 Treat Cause of ST (Box 6) 138
Treatment of SVT (Boxes 7 and 8) 198
Part 9 Wide QRS, Possible VT (Box9) 139
Recognition and Management Suggested Reading List 139
of Tachycardia 121
Overview 4
‘ Part 10
Learning Objecti 121
4 SERNOE Recognition and Management
Preparation for the Course 121 Of Cardiac Arrest ia
Tachyarrhythmias ‘21 Otervion 14
Recognition of Tachyarrhythmias 121 earring Objectives 1
Sinsand Symptoms 1 Preparation for the Course 142
Effect on Cardiac Outout 121 Definition of Cardiac Arrest 142
Classification of Tachycardia and Pathiaya te carcasa’nireat: sao
Tachyarthythmias 122 ihepih
Management of Tachyarrhythmias 126 Hypoxia om ne aes ve
ie 142,
Initial Management Questions 126 Sudden Cardiac Arrest
Fh ; Causes of Cardiac Arrest 149
Initial Management Priorities 126
; Recognition of Cardiopulmonary
Emergency interventions 126 oe tae
Recognition of Cardiac Arrest
Arrest Rhythms
Management of Cardiac Arrest
High-Quality CPR
Monitoring for CPR Quality
Pediatric Advanced Life Support in
Cardiac Arrest
Pediatric Cardiac Arrest Algorithm
Pediatric Cardiac Arrest: Special
Circumsiances
Social and Ethical Issues in
Resuscitation
Family Presence During
Resuscitation
Terminating Resuscitative Efforts
“Do Not Attempt Resuscitation” or
“Allow Natural Death” Orders
Predictors of Outcome After
Cardiac Arrest
Factors That Influence Outcome
Postresuscitation Management
Suggested Reading List
Part 11
Postresuscitation Management 171
Overview 471
Learning Objectives
Preparation for the Course
Postresuscitation Management
Primary Goals
Systematic Approach
Respiratory System
Management Priorities
General Recommendations
Cardiovascular System
Management Prioritios
General Recommendations
PALS Postresuscitation Treatment
of Shock
‘Administration of Maintenance Fluids
Neurologic System
‘Management Priorities
General Recommendations
Renal System
Management Priorities
General Recommendations
Gastrointestinal System
Management Priorities
General Recommendations
Hematologic System
‘Management Priorities
General Recommendations
Postresuscitation Transport
Coordination With Receiving Facility
Advance Preparation for Transport
Infectious Disease Considerations
Immediate Preparation Before
Transport
Communication Between Referring
and Receiving Healthcare Providers
Communication Among Facilities
and With Other Healthcare Providers
Communication With the Family
Posttransport Documentation and
Follow-up
Mode of Transport and Transport
Team Composition
Transport Triage
Suggested Reading List
Part 12 Terbutaline 21 |
Pharmacology 199 Vasopressin 202
Overview 199 |
Preparation for the Course 198 aul
Pharmacology pees : a
‘Silonosine noo BLS Competency Testing 238
‘Alburnin nen ats Skis Testing Sheets ao
easel = inal fie Child BLS With “|
" a ;cuer itl
Alprostadil (Prostegiendin E; (PGE) 203 AED Skills Testing Sheet 234 |
‘Amiodarone: a0 7- and 2-Rescuer Child BLS |
Atropine 205 With AED Skills Testing Criteria |
Calcium Chioride 207 and Descriotars x
ipassineannacons Ba Jeg 2-Rescuer Infant BLS Skiis
Dextrose’ (Giana) m0. 1- and 2-Rescuer Infant BLS Skill
Diphenhydramine 210 Testing Criteria and Descriptors. 237
Dobutamine 211 Skills Station Competency
Depitnie 212 Checklists 230
Epinephrine a Management of Respiratory
' Emergencies Skills Station
Etomidate 215 Competency Checkiist 239
Furosemide 216 Rhythm Disturbances/Electrical
Hydrocortisone 27 Therapy Skills Station
Competency Checkiist 240
Inamrinone (Amrinone) 210
‘ ; Vascular Access Skills Station
Ipratropium Bromide ae Competency Checklist 240
Ddecaine 2m: Rhythm Recognition Review 2a
Magnesium Sulfate aan Learning Station Competency
Methylprednisolone 222 Checklists 246
Milrinone 220 Respiratory Learning Station
iiSnene a Competency Checkists 216
Shock Learning Station
Niregyoain 8 Competency Checklists 250
Nitroprusside : ;
prussi , Cardiac Learning Station
(Sealant Nireprassiag 28 Competency Checklists 254
Norepinephrine 227 PALS Systematic Approach
Oxygen 228 = Summary 258
Procainamide 229 Index 261
Sodium Bicarbonate 230
Course Overview
Course Objectives
‘The Pediatric Advanced Life Support (PALS) Provider
Course is designed for healthcare providers who initiate
‘and direct basic through advanced life support. Course
‘concepts are designed to be used throughout the stabil
zation and transport phases for both in-hospital and out-
‘of-hospital pediatric emergencies. n this course you wil
‘enhance your skils in the evaiuation and management of
an infant or child with respiratory compromise, circulatory
compromise, or cardiac arrest.
During the course you will actively participate in a series of
simulated core cases. These simulations are designed to
reinioxce Important concepts, including
* Identification and treatment of problems that place the
child at risk for cardiac arest
+ Application of a systematic approach to pediatric
assessment
** Use of the “evaluate-identiy-intervene” sequence
** Use of PALS algorithms and flowcharts
‘+ Demonstration of effective resuscitation team dynamics
Cognitive Course Objectives
Upon successful completion ofthis course, you should be
able 10 do the following, independently, when presented
with a scenario of aeriticaly il or injured pedietic patent:
+ Describe the timaly recognition and interventions,
required to prevent respiratory and cardiac arrest in any
pediatric patient
* Describe the systematic approach to pediatric assess~
ment by using the intial impression, primary and sec-
ondary assessments, and diagnostic tests
* Describe priorities and specific interventions for
infants and children with respiratory and/or circulatory
‘emergencies
* Explain the importance of elfective team dynamics,
including individual roles and responsibilities, during a
peciatric resuscitation
* Describe the key elements of postresuscitation
management
Psychomotor Course Objectives
Upon successful completion of this course, you should be
‘able to do the following, independently, when presented
with a scenario of a criticaly il or injured pediatric patient:
+ Perform effective, high-quality cardiopulmonary resus-
citation (CPR) when appropriate
« Perform effective respiratory management within your
scope of practice
+ Select and apply appropriate cardiorespiratory
‘monitoring
* Select and admi
ister the appropriate medications and
electrical therapies when presented with an arshythmia
scenario
rapid vascular access to administer fluid and
‘+ Demonstrate affective commurication and team dynam-
cs both as a team member and as a team leader
Pa) The goal of the PALS Provider Course is to improve the quality of care provided to
ee aie seriously il or injured children, resulting in improved outcomes
Course Description
‘To help you achieve these objectives the PALS Provider
Course includes
+ Basic life support (BLS) competency testing
Skils stations.
*+ Core case discussions and simulations
+ Core case testing stations
* Auritten exam
BLS Competency Testing
You must pass 2 BLS tests to receive an American Heart
‘Association (AHA) PALS Provider course completion card
Se ee
Pass 1- and 2-Rescuer Child BLS With AED Skills Test
+ Pass 1- and 2-Rescuer Infant BLS Skills Test
‘The PALS Provider Course does not include detalied
instruction on how to perform basic CPR or how to use an
automated external defibilator (AED). You must know this
in advance. Consider taking a BLS for Healthcare Providers
Course if necessary. Before taking the PALS Course, review
the student BLS practice sheets and BLS skills testing
sheets in the Appendix. Also see Table 1: Summary of Key
BLS Components for Adults, Chiléren, and Infants and the
Padiatric Cardiac Arrest Algorithm in Part 10: “Recognition
and Management of Cardiac Arrest.”
Skills Stations
The course includes the foliowing skils stations:
‘+ Management of Respiratory Emergencies
‘+ Rhythm Disturbances/Electrical Therapy
* Vascular Accoss
During the skills stations you will have an opportunity to
practice specific skils and thon demonstrate competency.
Below is a brief description of each station. During the
course you will use the skills stations competency chack-
lists while practicing the skills. Your instructor wil evaluate
your skills based on the criteria specified in these check-
lists. See the Appendix for the sills station chockiste,
which list detailed steps for performing each skil.
Management of Respir
Skills Station
tory Emergencies
In the Management of Respiratory Emergencies Skils
Station you will need to demonstrate your understanding of
oxygen (0,) delivery systems and airway adjuncts. You will
have an opportunity to practice and demonstrate compe-
tency in airway management skils. including
* Insertion of an oropharyngeal airway (OPA)
+ Effective bag-mask ventilation
‘+ OPA and endotracheal (ET) tube suctioning
‘+ Confirmation of advancad airway device placement by
‘hysical examination and an exhaled carbon dioxice
(CO,) detector device
* Securing tho ET tube
{itis within your scope of practice, you may be asked io
demonstrate advanced airway skills, including corect inser
tion of an ET tube.
Rhythm Disturbances/Electrical Therapy
Skills Station
In the Rhythm Disturbances/Electrical Therapy Skills Station
you will have an opportunity to practice and demonstrate
‘competency in rhythm identfication and operation of a car-
iac monitor and manual defibrillator. Skills include
* Correct placement of electrocardiographic (ECG) leads
* Correct paddle/electrode pad selection and placement!
positioning
* Identification of rhythms that require defibrillation
* Identification of rhythme that roquire synchronized
cardioversion
* Operation of a cardiac monitor
* Sale performance of manual defibrillation and synchro:
rized cardioversion
Vascular Access Skills Station
In the Vascular Access Skils Station you will have an
‘opportunity to practice and demonstrate competency in
intreosseous (IO) access and other related skills. In this
skills station you will
* Insert an IO needle
+ Summarize how to confirm that the needle has entered
the marrow cavity
+ Summariza/demonstrate the method of giving an intra-
venous ('V)A0 bolus
+ Use a color-coded length-based resuscitation tape to
calculate correct drug doses
PALS Core Case Discussions and
Simulations
In the learning statiors you wil actively participate in a vari-
‘ety of learning activities, including
+ Core case discussions using a systematic approach for
evaluation and decision making
+ Cote case simulations
{n the learning stations you will apply your knowledge and
practice essential skits both individually and as part of a
team, This course emphasizes effective team skills as a
vital part of the resuscitative effort. You will receive train:
ing in effective team behavior and have the opportunity to
practice as a team member and a team leader.
PALS Core Case Testing Stations
At the end of the course you will participate as a team
leader in 2 core case testing stations to validate your
achiavement of the course objectives. You will be per-
mitted to use the PALS pocket reference card and the
2010 Handbook of Emergency Cardiovascular Care tor
Healthcare Providers, These SmUlated clinical scenarios will
test the following:
* Ability to evaluate and identity specttic medical prob-
lems covered in the course
+ Recognition and management of respiratory and shook
emergencies
+ Interpretation of core arthythmias and management
using appropriate medications and electrical therapy
* Performance as an effective team leader
‘A major emphasis of this evaluation will be your ability to
direct the integration of BLS and PALS skils by your team
members according to their scope of practice. Review
Part 2: “Effective Resuscitation Team Dynamics” before
‘the course.
Written Exam
‘The writen exam evaluates your mastery of the cognitive
objectives. The written exam is closed-book; no resources
or aids are perritted. You must score 84% or higher on the
written oxam.
Precourse Preparation
“To successtully pass the PALS Provider Course, you must
prepare before the course. Do the following:
+ Takeo the Precourse Self-Assessment
+ Make sure you are proficiant in BLS skils.
+ Practice identifying and interpreting core ECG rhythms,
+ Study basic pharmacology and know when to use
which drug.
+ Practice applying your knowledge to ctnical scenarios.
Precourse Self-Assessment
Se neil:
6 eae
Se see
eee
Serer meee
ear
BLS Skills
‘Strong BLS skills are the foundation of advanced life sup-
port. Everyone involved in the care of pediatric patients
‘must be able to perform high-quality CPR, Without high-
quality CPR, PALS interventions will fail. For this reason,
each student must pass the 1- and 2-Rescuer Child BLS
With AED and 1- and 2-Rescuer Infant BLS Skill Tests in
the PALS Provider Course. Make sure that you are proficient
in BLS skils before attending the course.
‘See the section "BLS Competency Testing” in the Appendix:
{or testing requirements and resources.
ECG Rhythm Identification
‘You must be able to identify and interpret the following core
‘hytbms during case simulations and core case tests:
= Normal sinus rhythm
Sinus bradycardia
Sinus tachycardia
Supraventricular tachycardia
* Ventricular tachycarcia
* Ventricular fioitation
+ Asystole
‘The ECG rhythm identifcation section of the Precourse
‘Self-Assessment will help you evaluate your ability to
identify these core rhythms and other common pediatric
arrhythmias. if you have difficulty with pediatric rhythm
identiication, improve your knowledoe by studying the sec-
tion “Rhythm Recognition Review” in the Appendix. The
AHA also offers self-directed online courses on rhythm ree-
cognition. These courses can be found at OnlineAHA.org.
Basic Pharmacology
‘You must know basic information about drugs used in
the PALS algorithms and flowcharts. Basic pharmacology
information includes the indications, contraindication, and
methods of administration. You will need to know when to
use which drug based on the clinical situation.
‘Tho pharmacology section of the Precourse Self-
Assessment will help you evaluate and enhance your
knowledge of mecications used in the course. If you
have difficulty with this section of the Precourse Self-
Assessment, improve your knowledge by studying
the PALS Provider Manual and the 2010 Handbook of
Emergency Cardiovascular Care for Healthcare Providers.
Practical Application of Knowledge to
Clinical Scenarios
‘The practical application section of the Precourse Self
Assessment wil help you evaluate your ability to apply your
kaowledge when presented with 2 clinical scenaro, You wil
need to make decisions based on
+ Tho PALS Systematic Approach Aigorthm and the
evaluate-identify-niervene sequence
+ identication of core rhythers
+ Knowledge of core medications
+ Knowledge of PALS flowcharts and algorithms
Be sure that you understand the PALS Systematic
PALS Student Website, and 2010 Handbook of Emergency
Cardiovascular Care for Healtncare Providers.
Course Materials
Tho PALS Provider Course matotials consist of the PALS
Provider Manual and supplementary material on the PALS.
Student Webstte
PALS Provider Manual
The PALS Provider Manual contains material that you will
use before, during, and after the course. It contains impor-
tant information that you need 10 know to effectively par=
ticipate in the course, so please read and study the manual
before the course. This important material includes con-
cepts of pediatric evaluation and the recognition and man-
‘agement of respiratory, shock, and carciac emergencies.
‘Some students may already know much of this information;
others may need extensive study before the course.
‘Approach Algorithm and the evaluate-identity-intervene
sequence, Review the core rhythms and medications. Be
familar with the PALS algorithms and flowcharts so that
you can apply them to clinical scenarios. Note that the
PALS Course Goes not teach the details of each algorithm.
Sources of information are the PALS Provider Manua,
The manual is organzed into the following parts:
fea Gok eee ee
Course Overviow What you need to know before the course, how to prepare for the course,
and what to expect during the course
The PALS systematic approach, intial impression, evaluate-identity-inter-
vene sequence, including the primary assessment, secondary assessment,
and diagnostic tests
‘Systematic Approach to the
Seriously Ill or Injured Child
Effective Resuscitation Team
Dynamics
Recognition of Respiratory
Distress and Failure
Roles of team leader and team members; how to effectively communicate
as a team leader or team member
Basic concepts of respiratory cistross and failure; how to identity respica-
tory problems according to type and severity
Management of Respiratory Intervention options for respiratory problems and emergencies
Distress and Failure
Recognition of Shock Basic concepts of shock; shock identification according to type and
severity
Management of Shock
Recognition and Management of
Bradycardia
Intervention options for shock according to etiology
Clinical and ECG characteristics of bradyarthythmias; medical and electri-
cal therapies
Recognition and Management of
Tachycardia
Clinical and ECG characteristics of tachyarihythmias; medical and electr-
cal thorapios |
‘Signs of cardiac arrest and terminal cardiac rhythms; resuscitation and
electrical therapy
Recognition and Management of
Cardiac Arrest
Postresuscitation Management —_| Postresuscitation evaluation and management; postresuecitation traneport
Pharmacology
Appendix
Details about common medications used in pediatric emergencias
Checklists for BLS competency testing, skit stations competencies, and
core case simulations; a brief rhythm recognition review
Throughout the PALS Provider Manual you will find specitic information in the following types of boxes:
‘Type of Box
Coe td
Cee
Remember to take this manual with you to the course.
PALS Student Website
mation about basic PALS concepts,
Eg
rg
‘The Precourse Self-Assessment isa vital part of your preparation for the course. Feedback from this assessment will help
yu identfy gaps in your knowledge so that you can target specific material to study.
eed
eee
eta a
Pe led
the Course
+ Pharmacology
Course Completion Requirements
To successfully complote the PALS Provider Course and
obtain your course completion card, you must do the
folowing:
* Actively participate in, practice, and complete all skills
stations and learning statons
+ Pass the 1- and 2-Rescuer Child BLS With AED and
1 and 2-Reaouer Infant BLS Skills Tests
+ Pass a virtton exam with a minimum score of 84%
+ Pass 2 PALS core caso tests as a team leador
Suggested Reading List
Donoghue A, Nishisaki A, ution R, Hales A, Boulet J
Relitilty end validity of a scoring instrument for clinical
performance during Podiatric Advanced Life Support simu-
lation seenaros. Resuscitation. 2010;81:331-896,
‘Basic information that every PALS provider should know
Important core concepts that are key to caring for critically ill or injured children,
‘An important evaluation or an immediate lifesaving intervention
‘Advanced information that you can use to increase your knowledge but that is not
required for successful course participation
@ Go to the PALS Student Website to access the Precourse Self-Assessment, Here you will also find additional infor-
‘The URL for the PALS Student Website is
www.heart.orgiecestudent
‘To enter the webstte, you will need the access code found at the bottom of page it in
the front of your PALS Provider Manual.
‘The Precourse Self-Assessment has 3 parts:
+ ECG rhythm identiication
* Practical application
Complete these assessments before the course to identify gaps in and improve your
knowledge. Print out your certificate of completion and take it with you to the course.
Hunt EA, Vera K, Diener-West M, Haggerty JA, Nelson
KL, Shatfner DH, Pronovost Pu. Delays and errors in car
diopulmonary resuscitation and defibrillation by pediat-
ric residents during simulated cardiopuimenary arrests.
Resuscitation. 2009;80:819-625.
Niles D, Sutton RM, Donoghue A, Kalsi MS, Roberts K,
Boyle L, Nishisaki A, Arbogast KB, Helfaer M, Nadkami V.
“Rolling Refreshers”: a novel approach to maintain CPR psy-
chomotor skill competence. Resuscitation. 2009:80:909-912,
Roy KM, Miler MP, Schmit K, Sagy M, Pediatric residents
‘experience a significant dectine in their response capabii-
ties to simulated life-threatening events as their training
frequency in cardiopulmonary resuscitation decreases
[pupisned online ahead of print October 1, 2010]. Peotatr
Crit Care Med. doi 10.1097/PCC.0b0198318113a0d
Sutton RM, Niles D, Meaney PA. Aplenc R. French 8.
Abella BS, Lengetti EL, Berg RA, Helfaer MA, Nadkarn)
\V. "Booster" training: evaluation of instructor-led bedside
cardiopulmonary resuscitation skill training end automated
corrective feedback to improve cardiopulmonary resuscita-
tion compliance of Pediatric Basic Life Support providers
‘during simulated cardiac arrest (oublished online ahead
Of print July 8, 2010), Pediatr Crit Care Med. doi10.1097/
PCC.0b013e818 1691271
Systematic Approach to the
Seriously Ill or Injured Child
Overview
‘The PALS provider should use a systematic approach when
Caring fora seriously i or injured child, The purpose of this
crganized approac isto enable you to quickly recognize
signs of respiratory distress, respiratory failure, and shock
and inmediatoly provide lifesaving intorventions. If not
appropriately treated, children with respiratory failure and
shock can quickly develop cardiopuimonayy failure and
even cardiac arest (Figure 1).
Rapid Intervention to Prevent
Cardiac Arrest
In infants and children, most cardiac arrests result from pro-
gressive respiratory failure, shock, or both. Less commonly,
Pediatric cardiac arrests can occur without warning (ie, with
‘sudden collapse) secondary to an arrhythmia (ventricutar
fibrilation (VF or ventricular tachycardia [VT).
‘Once cardiac arest occurs, even with optimal resuscitation
cfforts, the outcome is generally poor. In the out-of-hospital
setting only 4% to 13% of children who experience cardiac
arrest survive to hospital discharge. The outcome is better
{or children who experience carclac arrest in the hospital,
although oniy about 33% of those children survive to hos
pital discharge. For this reason itis important to learn the
concepts prasentod in the PALS Provider Course so that
Rapid, systematic intervention for seriously ill or injured infants and children is Key to
preventing progression to cardiac arrest. Such rapid intervention can save lives.
you can identity signs of respiratory feilure and shock and.
rapidly intervono to prevent progression to cardiac arrest.
Learning Objectives
‘After completing this Part you should be able to
* Discuss the evaluate-identiy-intervene sequence
‘+ Explain the purpose and components of the initial
improssion
'* Describe the ABCDE components of the primary
assessment
* Interpret the clinical findings during the primary
‘assessment
* Evaluate respiratory or circulatory problems by using
the ABCDE mode! in the primary assessment
+ Describe the components of the secondary
assessment
* List diagnostic and laboratory tests used to identify
respiratory and circulatory problems
Preparation for the Course
‘You rieed to know all of the concepts presented in this Part
to be able to identify respiratory or circulatory problems
‘and target appropriate managomont in case simulations.
‘The ongoing process of evaluate-identfy-intervene is a core
‘component of systematic evaluation and care of a seriously
i oF injured child,
Precipitating Problems
Respiratory Circulatory Sudden
Cardiac Arrest
(Arrhythmia)
Figure 1. Pathways to pediatic cardiac arest. Note that respiratory problems may progress to respiratory falure wth or witout signs of resp=
ratory distess, Pespratory failure without respiratory dstiess ozcurs when the chld falls to maintain an open alway oF adoquate respiratory afort
and is typically associated with a decreased Iavelo! consciousness. Sudden cardiac arrestin chieren is less common than in aduls and typically
resus from arhythmias such as VF or VT. Ouring sports activities, sudden cavdlac arest ean occur in children with underlying cardige problems
‘hat may oF may not have bean previously recogrized.
Se een a a oe Red
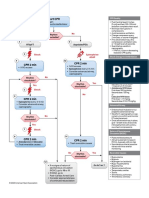
ALS Systematic Approach Algorithm
‘The PALS Systematic Approach Algorithm (Figure 2) outlines the approach to cating for a critically il or injured child.
Initial Impression
‘Activate Emergency Response
18 appropriate for setting)
Goto
Pediatric Cardiac Arrest
Algorithm
‘After ROSC, begin
Evaluate-Identity-Intorvene
‘sequence (right column)
©2011 Amaroan Heat Aosocaton
Figure 2. PA.5 systematic Approach Algor,
If at any time you identify a life-threatening problam, immediately begin appropriate
Interventions. Activate emergency response as indicated in your practice setting,
Initial Impression
The initial impression (Figure 2) is your first quick “trom the
doorway” observation. Ths inital visual and aucitory obser-
provide compressions and ventilations. Proceed
‘according to the Pediatric Cardiac Arrest Algorithm.
1» If the heart rate is 260/min, begin the evaluate-
identity-intervene sequence. Be prepared to inter-
vene according to the Pediatric Cardiac Arrest |
Algorithm if needed, |
« Ifthe child is breathing adequately, proceed with the
evaluate-identify-intervene sequence. If at any time you
identify cardiac arrest, begin CPR and proceed accord-
vation of the chilo's consciousness, breathing, and color is
accomplished within seconds of encountering the child.
ees
Consciousness | Leve! of consciousnoss ing to the Pediatric Cardiac Arrest Algorithm.
(¢9, unresponsive, iritable, alert)
[resting | wreesed wacof treating, coset | Ewaluate-Identify-Intervene
cr decreased respiratory effort, or Use the evaluate-identify-intervene sequence (Figure 3)
‘abnormal sounds heard without | when caring fora seriously il or injured child. This wil helo
auscuttation you to determine the best treatment or intervention at any
———— point. From the information gathered during your evaluation,
Soler ‘Abnormal skin Color, Such a5 yaNO- | identity the child’s problom by type and severity. Intervene
Ss pelos erring with appropriate actions. Then repeat the sequence. This
process is ongoi
‘The level of consciousness may be characterized as unre- ee
sponsive, irtable, or alert. Decreased lavel of conscious-
ness may result from inadequate O, or substrate delivery or
brain trauma/dystunction. Abnormal breathing includes use
‘of accessory muscles, extra sounds of breathing, or abnor-
‘mal breathing patterns. Pale, mottied, or bluish/gray skin
color suggests poor parfusion, poor oxygenation, or both.
A flushed appearance suggests fever or the presence of
atoxin.
Use your intial impression to determine the next best stops:
« If the child is unresponsive and not breathing or only
gesping, shout for help or activate emergency response
{as appropriate for your practice setting). Check to see
if there is a pulse.
~ If there is no pulse, start CPR, beginning with chest
‘compressions. Proceed according to the Pediatric
Cardiac Arrest Algorithm. Alter return of spontane-
us circulation (FOS), begin the evaluate-identify-
intervene sequence.
~ Ifa pulse is present, provide rescue breathing.
‘=f, despite adequate oxygenation and ventilation, the
bear rate is <60/rmin with signs of poor perfusion,
Figure 3. Evaluate-derify- intervene sequence.
Always be alert to a life-threatening problem. if at any point
you identify a life-threatening problem, immediately activate
‘emergency response (or send someone to do so) while you
begin lifesaving interventions.
oa The initial impression used in this version of the PALS Provider Course is a modification
Of the Paciatric Assessment Triangle (PAT) that was used in the 2008 PALS Provider
Course.* The PAT, lke the rapid cardiooulmonary essessment (which was taught in all
Of the PALS courses before 2006),’is part of a systerratic approach to assessing an il
© injured child. These slightly different assessment approaches use many of the same
‘common terms. The goal ofall of these approaches is to help the provider quickly rec-
‘ognize a chi at risk for deterioration and prioritize actions and interventions.
tee
‘Dieckmann RD, Brownstein OR, Gausche-HillM, eds. Pediatric Education fr Prehospta!
Professionals Insttuctor Took. Sudbury. MA: American Academy of Pedi and Jones &
BBarlet Publishers; 2000. ‘Ralston M, Hazinski MF, Zarsky AL, Schexrayder SM, Klerman ME
‘eds, Peclatic Advanced Life Support Provider Manual. Dallas, TX: American Heart Assocation;
12000. Hazinski MF, Zantsky AL, Nadkarni VM, Hickey RW, Schexnayder SM, Berg RA, eds
Pediatric Advanced Life Support Prove Manual. Dalia, TX: American Heatt Asscciaton: 2002.
SC ene Ue ae Rd
Evaluate
It no ife-threatening problem is present, evaluate the child's
condition by using the clinical assessment tools described
below.
re
pinay Cea
Primary A rapid, hands-on ABCDE approach
assessment | to evaluate respiratory, cardiac, and
neurologic function; this step includes
assessment of vital signs and pulse
oximetry
Secondary —_| A focused medical history and a
assessment | focused physical exam.
Diagnostic | Laboratory, radiographic, and other
tests ‘advanced tests that help to identify
the child's physiologic condition and
diagnosis
Note: Providers should be aware of potential environmental
dangers when providing cars. In out-of-hospital settings,
always assess the scane before you evaluate the child.
Identify
Try to identify the type and severty of the chic's problem.
vid Ee
Respiratory | * Uppor airway = Respiratory
obstruction cistress
* Lower airway * Respiratory
obstruction failure
* Lung tissu disease
* Disordered control
of breathing
Circulatory | + Hypovolemic shook
‘+ Compensated
* Distributive shook | shock
*# Cardiogenic shock | * Hypotensive
shock
*# Obstructive shock
Cardiopulmonary Failure
Cardiac Arrost
The child's ciinical condition can result rom a combination
of respiratory and circulatory problems. As a seriously il or
injured child deteriorates, one problem may lead to others.
eka Ty
ROS Ca Le * Alter each intervention
Intervene Sequence Is
erates
Note that in the initial phase of your identification you may
bbe uncertain about the type or soverty of problems.
Identifying the problem will help you determine the best
initial interventions. Recognition and management are dis
cussed in deal later in this manual,
Intervene
(On the basis of your identiication of the child's problem,
intervene with appropriate actions within your scope of
practice. PALS interventions may include
‘ Positioning the child to maintain a patent airway
‘* Activating emergency response
* Staring CPR
+ Obtaining the code cart and monitor
+ Placing the child on a cardiac monitor and pulse
oximeter
«= Administering O.
‘Supporting ventilation
* Starting medications and fluids (eg, nebulizer
treatment, IV/1O fuuid bolus)
Continuous Sequence
The sequence of evaluate-identily-intervene continues
Until the chid is stable. Use this sequence belore and atter
each intervention to lack for trencs in the child's condktion.
For example, after you give O., reevaluate the chid. is the
CChid breathing a lite easier? Ave color end mental status
improving? After you give a flid bolus to a child in hypo-
volemic shock, do heart rate and perfusion improve? Is.
‘another bolus neadec? Use the evaluate-identily.intervene
‘sequence vibenever the child's condition changes.
Determine If Problem Is Life
Threatening
‘On the basis of the initial impression and throughout care,
determine ifthe child's problem is
«Lite threatering
* Not life threatening
Life-threatening probleme include absent or agorsal res
pirations, respiratory distress, cyanosis, or decreased
level of consciousness (see the section “Lite-Threatenng
Problems" later inthis Part). If the problem is life threaten-
ing, immediately begin appropriate interventions. Activate
‘emergency response as indicated in your practice setting
It the problem ss not if threatening, continue with the sys-
tematic approach.
Remember to repeat the evaluate-identify-intervene soquence until the child is stable
+ When ihe child's concition changes or deteriorates
a ‘Sometimes a child's condition may saem stable despite the presence of a lfe-threat-
ening problem, An example is @ child who has ingested a toxin but is not yet snowing
effects, Another example is a trauma victim with internal bleeding who may initially
mainiain blood pressure by increasing heart rate and systemic vascular resistance (SVF).
eee
Retry
Ie Ou cu)
Primary Assessment
A B
E c
D
‘The primary assessment uses an ABCDE model:
+ Ainway
+ Broathing
* Circulation
+ Disability
+ Exposure
‘The primary 2esessment is a hands-on evaluation of
respiratory, cardiac, and neurologic function. This assoss-
‘ment includes evaluation of vital signs and O, saturation by
pulse oximetry.
Airway
When you assess the ainay, you determine if it is patent
(open). To assess upper airway patency:
* Look for movement of the chest or abdomen
* Listen for air movement and breath sounds
Decide if the upper airway is clear, maintainable, or not
‘maintainable as described in the following table:
pe
Clear Airway is open and unobstructed for
normal breathing
Maintainable | Airway |s obstructed but can be main-
tained by simple measures (eg, head
tilt-chin It)
Not Airway is obstructed and cannot be
maintainable | maintained without advanced interven-
tions (eg, intubation)
‘The following signs suggest that the upper airway is
obstructed:
+ Increased inspiratory effort with retractions
‘+ Abnormal inspiratory sounds (snoring or high-pitched
stridor)
+ Episodes where no airway or breath sounds are pres-
‘ent despite respiratory effort (le, complete upper airway
obstruction)
If the upper airway ie obstructed, determine if you can open
land maintain the airway with simple measures or if you
need advanced interventions.
‘Simple measures to open and maintain a patent upper air-
way may include one or more of the following:
+ Allow the child to assume a position of comfort or posi-
ton the child to improve airway patency.
+ Use nead tit-chin lft or jaw thrust to open the airway.
~ Use the head tit-chin lft maneuver to open the a
‘way unless you suspect cervical spine injury. Avoid
overextending the head/neck in infants because ths
may ecclude the airway.
~ Hf you suspect cervical spine injury (eg, the chi has
head or neck injury), open the away by using a jaw
‘thrust without neck extension. If this maneuver does.
not open the airway, use a head tit-chin lift or jaw
‘trust with neck extension because opening the ai.
\way is a prio. During CPR stabilize the head and
neck manually rather than with immobikzation devicos.
I at any time you identity a life-threatening problem, immediately begin appropriate
interventions. Activate emergency response as indicated in your practice setting
— Note that the jaw thrust may be used in children
without trauma as vrell,
‘Avoid overextending the head/neck in infants because
this may occlude the airway. Suction the nose and
‘oropharynx.
Perform foreign-bedy airway obstruction (FBAO) relief
techniques if you suspect that the child has aspirated
a foreign body, has complete airway obstruction ($
tunable to make any sound), and is stil responsive,
Repeat the folowing es needed:
~ <1 year of age: Give 5 back slaps and 5 chest
thrusts
= 21 year of aga: Give abdominal thrusts
Use airway adjuncts (eg, nasopharyngeal airway [NPA]
or oropharyngeal airway [OPA)) to keep the tongue
{rom falling back and obstructing the airway.
Advanced Interventions
Advanced interventions to maintain airway patency may
include one or more of the following:
‘+ Encotracheal intubation or placement of a laryngeal
mask airway
‘+ Application of continuous positive airway pressure
(CPAP) or noninvasive ventilation
‘+ Removal ofa foreion body: this intervention may
requite drect laryngoscopy (ie, visualizing the larynx
with a laryngoscope)
* Cricothyrotomy (a needle puncture or surgical opening
through the skin and criecthyroid membrane and into’
the trachea below the vocal cords)
Breathing
Assessment of breathing includes evaluation of
* Respiratory rate
* Respiratory effort
* Chest expansion and air movement
Cred
DOO CAC
Cee ie
el
‘An airway adjunct will help to maintain an open airway, but you may stil need to use a
head tit-chin lift. Don't rely only on an adjunct alone, Assees the pati
Acconsistent respiratory rate of less than 10 or more than 60 breaths/min in a child of
any age is abnormal and suggests the presence of a potentially serious problem.
SS ee RGR ae Ee eked
* Lung and airway sounds
‘+ 0, saturation by pulee oximetry
Normal Respiratory Rate
Normal spontaneous breathing is accomplished with mini
‘mal work, resulting in quiot breathing with unlabored inspi-
ration and passive expiration. The normal respiratory rate
Inversely related to age (see Tabie 1); it is rapid in the neo-
ate and decreases as the chiki gets older.
Table 4. Normal Respiratory Rates by Age
oS Breaths/min
[event et yoo) 01080
Toddler (1 to 3 years) 24 to 40
Preschooler (4 to 5 years) 221034
School age (6 to 12 years) 180.90
| Adolescent (13 to 18 years) 121016
Respiratory rate is often best evaluated before your hands-
on assessment bacause anxiaty and agitation commonly
alter the baseline rata. Ifthe child has any condition that
causes an increase in metabolic demand (eg, excitement,
anxiety, exercise, pain, or fever), itis appropriate for the
respiratory rate to be higher than normal.
Determine the respiratory rate by counting the number of
times the chest rises in 30 seconds and multiplying by 2.
Be aware that normal sleeping intents may have irregular
(periodic) breathing with pauses lasting up to 10 or even
16 seconds. If you count the number of times the chest
rises for <30 seconds, you may estimate the respiratory
rate inaccurately. Count the respiratory rate several timas
‘as you assess and reassess the child to detect changes.
Alternatively, the respiratory rate may be displayed continu-
‘ously on a monitor.
A decrease in respiratory rate from 2 rapid to a more
“normal” rate may indicate overall improvement if itis
associated with an improved level of consciousness and
reduced signe of air hunger and work of breathing. A
decreasing or irregular respiratory rate in a chid with a
deteriorating level of consciousness, however, often indi
cates a worsening of the child's clinical condition.
Abnormal Respiratory Rate
‘Abnormal respiratory rates are classified as
+ Techypnea
+ Bradypnea
+ Apnea
Tachypnea
Tachypnea is a breathing rate that is more rapi than nor-
‘mal for age. It is often the first sign of respiratory distress in
Infants. Tachypnea also can be a physiologic (appropriate)
response to stress.
Tachypnea with respiratory distress is, by definition, associ
ated with other signs of increased respiratory effort. “Quiet
tachypnea” is the term used if tachypnea is present without
signs of increased respratory effort (e, without respiratory
distress). This often results from an attempt to maintain
near-normal blood pH by increasing the amount of air mov-
ing in and out of the lungs (ventilation) this decreases GO.
leve's in the blood and increases biood pH.
Quiet tachypnea commonly results from nonpulmonary
problems, including
* High fever
» Pan
‘+ Mild metabolic acidosis associated with dehydration or
diabetic ketoacidosis (DKA)
‘+ Sopsis (without pnaumonia)
* Congestive heart failure (early)
* Severe anemia
* Some cyanotic congenital heart defects (eg. transposi-
tion of the great arteries)
eee
See aa cd
Rega eel
Signals Impending Arrest
a7
resent:
eee ae
apnea
Bradypnea cr an irregular respiratory rate in an acutely il infant or chile is an ominous,
clinical sign and often signals impending arrest. |
‘Apnea is classified into 3 types, depending on whether inspiratory muscle activity
* In central apnea there is no respiratory effort because of an abnormality or sup
pression of the brain or spinal cord,
® In obstructive apnea there is inspiratory eftort without airflow (ie, airflow is partially
‘or completely blocked).
‘= In mtxed apnea there are poriods of obstructive apnea and periods of contral
for age, Frequontly the breathing is both slow and iregu-
lar, Possible causas are respiratory muscle fatigue. central
‘nervous system injury or infection, hypothermia, or medica-
tions that depress respiratory drive. |
Apnea
‘Apnea is the cessation of breathing for 20 seconds or ces-
sation for less than 20 seconds i accompanied by brady-
cardia, cyanosis, or pallor.
Bradypnea
Bradypnea is a breathing rate that is slower than normal
‘Agonal gasps are common in adults after sudden cerdiac
arrest and may be confused with normal breathing. Agonal
‘gasps will not produce effective oxygenation and ventilation.
Respiratory Effort
Increased respiratory effort results from conditions that
increase resistance to airflow (eg, asthma or bronchiclitis)
cr that cause the lungs to be stiffer and difficult to inflate
(e9, pnoumoria, pulmonary edema, or pleural effusion)
Nonpulmonary conditions that result in severe metabolic
acidosis (€g, DKA, sabcylate ingestion, indorn errors of
metabolism) can also cause increased respiratory rate
and effort. Signs of increased respiratory effort retlect the
child's attempt to improve oxygenation, ventilation, or both,
Use the presence or absence of these signs to assess the
severity of the condition and the urgency for intervention.
Signs of increased respiratory effort include
‘= Nasal flaring
‘+ Retractions
‘+ Head bobbing or seesaw respirations
thor signs of increased respiratory effort are prolonged
inspiratory or expiratory times, open-mouth breathing,
‘gasping, and use of accessory muscles. Grunting Is a serl-
‘ous sign and may indicate respiratory distress or respiratory
failure, (See “Grunting” later inthis Part.)
‘Systematic Approach to the Seriously Ill or Injured Child
Nasal Flaring (continued)
‘Nasal faring is dation of the nostri with each inhalation, Pe cc
‘The nostris open more widely to maximize airflow. Nasal Cre aed
flaring is most commonly observed in infants and younger
chilcron and is usually a sign of respiratory distress.
Severe (may | Supraciavicular | Retraction in the
include the ‘neck, ust above the
Retractions same retrac- collarbone
Retractions ere inward movements of the chest wallortis- | tlorsasseen [sr atermal | Retraction in the
sues, neck, oF sternum ding inspiration. Chest retractions | With mil chest, just above
are a sign that the child is trying to move air tothe turgs | tomoder- the breastbone
by using the chest muscies, but air movement is impaired ate breathing
by increased airway resistance or stif lungs. Retractions aiticury) Sternat Retraction of the
‘may occur in several areas of tho chest. The severity of the ctor foward
the spine
retractions generally corresponds with the severity of the
child's breathing difficuty.
Head Bobbing or Seesaw Respirations
“The following table describes the location of retractions Head bobbing and seesaw respirations often indicate that
‘commonly associated with each level of breathing difficulty: the child has increased risk for deterioration
+ Heed bobbing is caused by tho uso of neck muscles
Ca eee
pete (rete to assist breathing. The child lits he chin and extencs
the neck during inspiration and allows the chin to fal
‘Subcostal Ratraction of the forward during expiration. Head bobbing is most tre= |
abdomen. just quently seen in infants and can be @ sign of respiratory
Delow the rib cage falure |
+ Seesaw respirations are present when the chest |
Substernal_ | Retraction of the retracts and the abdomen expands during inspiration.
abdomen at the During expiration the movement reverses: the chest
bottom of the ‘expands and the abdomen moves inward. Soesaw
respirations usvally indicate upper airway obstruction,
Pression: They also may be observed in severe lower airway
intercostal | Retraction betweon obstruction, lung tissue disease, and disordered control
the rbe | Of breathing, Seesaw respirations are characteristic
al J Of infants and children with neuromuscular weakness.
(continued) Tis inefficient form of ventlation can cuiekly lead to
fatigue.
a etvactions accompanied by stridor or an inspiratory snoring sound suggest upper
ih airway obstruction. Retractions accompanied by expratory weezing suggest marked
ans ower airway obstruction (asthma or bronchiolitis), causing obstruction during both
Renee USE Reus
RPO cu ala
Peer ego
inspiration and expiration, Retractions accompanied by grunting or labored respira-
tions suggest lung tissue disease. Severe retractions also may be accompanied by
head bobbing or seesaw respirations,
The cause of seesaw breathing in mest children with neuromuscular disease is weak~
ness of the abdominal and chest wall muscles. Seesaw breathing Is caused by stiong
contraction of the diaphragm that dominates the weaker abdominal and chest wall
muscles. The result is retraction of the chest and expansion of the abdomen during
inspiration.
oe td
Eee
eee)
Chest Expansion and Air Movement
Evaluate magnitude of chest wall expansion and air move~
ment to assess adequacy of the chile’s tidal volume. Tidal
volume is the volume of air inspired with each breath,
Normal tidal volume is approximately 5 to 7 mL/kg of body
weight and remains fairy constant throughout Ife, Tidal
volume is difficult to measure unless a child is mechanically
ventilated, so your clinical assessment is very important,
Chest Wall Expansion
Chest expansion (chest rige) during inspiration should be
symmetric. Expansion may be subtle during spontane
‘ous quiet breathing, especially when clothing covers the
chest. But chest expansion should be readily visible when
the chest is uncovered. In normal infants the abdomen
‘may move moro than the chest. Decreased or asymmetric
cchest expansion may result from inadequate effort, ainway
obstruction, atelectasis, pneumothorax, hemothorax, pleu-
ral effusion, mucous plug, or foreign-body aspiration,
Air Movement
‘Auscuttation for air movement is critical. Listen for the
intensity of breath sounds and quality of air movement,
Particularly in the cistal lung fields. To evaluate distal ar
entry, Isten below both axillao. Because these areas are
farthest from the larger conducting airways, upper airway
Sounds are less likely to be transmitted. Typical inspiratory
‘sounds can be heard distally as soft, quiet noises ocour-
ring simultaneously with observed inspiratory effort. Normal
‘expiratory breath sounds are often short and quiets.
‘Sometimes you may not hear normal expiratory
breath sounds.
You should also auscuitate for lung and airway sounds
ver the anterior and posterior chest. Because the chest is
small and the chest wall is thin in infants or children, breath
‘sounds are readily transmittad from one side of the chest to
tne other, Breath sounds also may be transmitted from the
upper airway.
Decreased chest excursion or decreased air movement
observed during auscultation often accompanies poor
+ Stow respiratory rate
*+ Small tical volume (ie, shallow breathing, high airway resistance, stft lungs)
+ Extremely rapid respiratory rate i tidal volumes are very small)
Minute ventilation is the volume of air that moves into or out of the lungs each minute,
{tis the product of the number of breaths per minute (respiratory rate) and the volume
of each breath (ida! volume)
Minute Ventilation = Respiratory Rate x Tidal Volume
Low minute ventilation (hypoventilation) may result from
respiratory effort. In tho child with apparently normel or
increased respiratory effort, diminished distal air entry
‘Suggests airflow obstruction or lung tissue disease. If the
child's work of breathing and coughing suggest lower al-
way obstruction but no wheezes are heard, the amount and
rate of airflow may bo insufficient to cause wheezing,
Distal ir entry may be dificult to hear in the obese child.
As a result, it may be difficult to identify significant airway
abnormalities in this population
Lung and Airway Sounds
During the primary assessment, listen for lung and airway
sounds. Abnormal sounds include stridor, grunting, gur-
gling, wheezing, and crackles.
Stridor
Strider is a coarse, usually higher-pitched breathing sound
typically heard on inspiration. It also may be heard during
both inspiration and expiration. Stridor is a sign of upper
airway (extrathoracic) obstruction and may indicate that the
obstruction is critical and requires immediate intervention.
‘Thote ave many causes of stridor, such @s FBAO and infec
tion (eg, croup). Congenital airway abnormalities (eg, laryn-
omaiacia) and acquired airway abnormalities (2g, tumor
Cr cySt) also can cause stridor. Upper airway edema (eg,
allergic reaction or swelling after a medical procedure) is
‘another cause ofthis abnormal breathing sound.
Grunting
Granting is typically a short, low-pitched sound heard
uring expiration. Sometimes it can be misinterpreted as
a soft ory, Grunting occurs as the child exhales against a
partialy closed glottis. Although grunting may accompany
the response to pain or fever, infants and children often
grunt to help keep the small aways and alveolar sacs in
the lungs open. This is an attempt to optimize oxygenation
and ventilation,
Grunting is often a sign of lung tissue disease resuting
from smal airway collapse, alveolar collapse, or both.
Grunting may indicate progression of respiratory distress to
uel eon ni na Rem a Rel]
Grunting is typically a sign of severe respiratory distress or failure from jung tissue
disease. Identity and treat the cause as quickly as possible. Be prepared to quickly
intervene If the chila's condition worsens.
respiratory failure. Pulmonary conditions that cause grunt
ing include pneumonia, pulmonary contusion, and acute
respiratory distress syndrome (ARDS). It may he caused by
‘cardiac conditions. such as congestive heart faiure, that
result in pulmonary edema. Grunting may be a sign of pain
resulting from abdominal pathology (eg, bowel obstruction,
porforated viscus, appendicitis, or peritonitis).
Gurgling
Gurgling is a bubbing sound heard during inspiration or
‘expiration. It results from upper airway obstruction due to
airway secretions, vomit, or blood.
Wheezing
Wheezing is a high-pitched or low-pitched whistling or sigh:
ing sound heard most often during expration. itis heard
less frequently during inspiration. This sound typically ind-
cates lower (intrathoracic) airway obstruction, especially of
the emaller aways. Common causes of wheezing aro bron:
chioitis and asthma. Isolated inspiratory wheezing suggasts
‘a foreign body or other cause of partial obstruction of the
trachea or upper airway.
Crackles
Grackies, also known as rales, are sharp, crackling inspira-
tory sounds. The sound of dry crackles can be described
as the sound made when you rub several hairs together
close to your ear. Crackles may be described as moist or
dry. Moist crackles indicate accumulation of alveolar fluid,
‘They are typically associated with lung tissue disease
(eg, pneumonia and pulmonary edema) or interstitial lang
ured
OME Ty
disease. Dry crackles are more often heard with alelectasis
(smal airway collapse) and interstitial lung disease. Noto
that you may not hear crackles despite the presence of
pulmonary edema,
Oxygen Saturation by Pulse Oximetry
Pulse oximetry is a tool to monitor the percentage of the
child's hemogiobin that is saturated with O, (Spo). The
pulse oximeter consists of a probe Inked to a monitor.
The probe is attached to the child's finger, toe, or earlobe.
The unit displays the calculated percentage of oxygenated
hemoglobin. Most units make an audiole sound for each
pulse beat and display the heart rate. Some models display
the quality of the pulse signal as a waveform or with bars.
Pulse oximetry can indicate low ©, saturation (hypoxemia)
before it causes cyanosis or bradycardia. Providers can
use pulse oximetry to monitor trends in O, saturation in
response to treatment. If avaiable, contiruously monitor
pulse oximetry fora child in respiratory distress or faire
during stabiization, transport, and postresuscitation care.
Caution in Interpreting Pulse Oximetry Readings
Be careful to interpret pulse oximetry readings in conjunc-
tion with your cinical assessment and other signs, such as
respiratory rate, respiratory effort, and level of conscious-
ness. A child may be In respiratory distress yet maintain
normal O, Saturation by increasing respiratory rate and
effort, especially if supplementary ©, is administered. H the
heart rate displayed by the pulse oximeter is not the same
as the heart rate determined by ECG monitoring, the O,
‘The O, saturation is the percent of {otal hemogiobin that is saturated with O,.
“This saturation dove not indicate the amount of O, delivered to the tissues. O, delivery
is the product of artarial O, content (oxygen bound to hemoglobin plus dissolved 0.)
and cardiac output.
{tis also Important to note that O; saturation does not provide information about effec-
tiveness of ventilation (CO, elimination).
‘An O, saturation (Spo,) 284% while @ child is breathing room air usually indicates that |
‘oxygenation is adequate. Consider administration of supplementary O» if the Op satu-
ration is below this value in a ori
ly ill or injured child. An Spo; of <90% in a child
receiving 100% O, is usually an indication for additional intervention.
‘saturation reading is not reliable. When the pulse oximeter
dows not detect a consistent pulse or there is an irregular
‘or poor waveform, the child may have poor distal pertusion
‘and the pulse oximeter reading may not be accuraie—check
the child and intervene as needed. The pulse oximeter may
rot be accurate if the child develops severe shock and
‘won't be accurate during cardiac arrest. As noted above,
pulse oximetry only indicates O; saturation and does not
indicate O, delivery. For example, if the child is profoundly
anemic (hemoglobin is very low), the saturation may be
100%, but ©, content in the blood and O, delivery may be
low.
The pulse oximeter does not accurately recognize met-
hemoglobin or cartvoxynemogiobin (hemoglobin bound
to carbon monoxide). If carboxyhemoglobin (from carbon
‘monoxide poisoning) is prosont, the pulco oximeter will
reflect a falsely high O, saturation. if methemoglobin con-
centrations are above 5%. the puise oximeter will read
approximately 85% regardless of the degree of methemo-
globinemia, If you suspect etther of these conditions, obtain
2 blood gas with O, saturation measurement by using a
co-oximeter.
Circulation
c
Circulation is assessed by the evaluation of
* Heart rate and rhythm
* Pulses (both peripheral anc central)
* Capitary rel time
* Skin color and temperature
+ Blood pressure
Unne output and level of consciousness also reflect
adequacy of circulation. See the Fundamental Fact box
“Assessment of Urine Output” at the end of this section,
For more information on assessing level of consciousness,
‘see the section “Disability” later in this Par.
Heart Rate and Rhythm
‘To determine heart rate, check the pulse rata, listen to the
heart, or view a monitor display of the electrocardiogram
(ECG) or pulse oximeter wavelorm. The heart rate should
‘be appropriate for the child’s age, level of activity, and clini-
cal condition (Table 2). Note that there is a wide range for
normal heart rates. For example, a child who is sleeping
‘or is athletic may have a heart rate lower than the normal
range for age.
‘Table 2. Normal Heart Rates (por Minute) by Age |
Awake Sr)
es Go ior Rate
Nowborn to | 8510205 | 140 | ato 160
months
months te2 | 1000190 | 130 | 75t0 160
years
2yearsto10 | Bto140 | 89 | 60t0.90
years |
>iyears | 6010100 | 75 | S0t090
Modifed tron Gilette PC, Garson A J, Craword F Ross B, Ziegler
V, Bucklos D. Dysthythmias. I: Adams FH, Emmanouiides GC,
Fimenschneider TA, eds. Moss’ Hear Dissese in arts, Crilcren, ana
Adolosconts 4th ed, Batimore, MD: Willams & Wiking; 1980:026-020,
‘The heart rhythm is typically regular with only small flic-
tuations in rate. When checking the heart rate, assess
for abnormalities in the monitored ECG. Cardiac rhythm
disturbances (arrhythmias) result from abnormalities in, or
incults to, the cardiac conduction system or heart tissue,
Arrhythmias also can result from shock ar hypoxia. In the
advanced life support setting, an arthythmia in a child can,
be broadly classified according to the observed heart rate
or effect on perfusion:
Coun Ceo
Slow Bradycardia
Fast Tachycardia
Absent Cardiac arrest
Bradycardia is a heart rate slower than normal for a child's
‘age. Slight bradycardia may be normal in athletic children,
uta very siow rate in a child with other symptoms is @
worrisome sign and may indicate that cardiac arrest is
imminent. Hypoxia is the most common cause of brady-
cardia in chilcren. Ifa child with bradycardia has signs of
oor partusion (decreasad responsiveness, weak peripheral
ulses, cool mottled skin), immediately support ventitation
with a bag end mask and administer supplementary O.. If
the chi with bradycercia is alert and has no signs of poor
perfusion, consider other causes of a siow heart rate, such
as heart biock or drug overdose.
Tachycardia is a resting heart rate that is faster than the
normal range for a child's age. Sinus tachycardia is a com-
‘mon, nonspecific response to a variaty of conditions. Itis
often appropriate when the child is seriously ill oF injured. To.
determine if the tachycardia is a sinus tachycardia or rep-
resents a cardiac rhythm disturbance, evaluate the child's,
history, clinical condition, and ECG.
Systematic Approach to the Seriously Ill or Injured Child
Consider the following when evaluating the heart rate and rhythm in any seriously il or
injured chité:
eae
eu cca cy
es ‘+ The child's typical heart rate and baseline rhythm
*+ The child's level of activity and clinical condition (including baseline cardiac
function)
Children with congenital heart disease may have conduction abnormalities. Consider
the child's baseline ECG when interpreting heart rate and rhythm. Chicren with poor
cardiac function are more likely to be symptomatic from arrhythmias than are children
with good cardiac function,
In healthy children the heart rate may fluctuate with the respiratory cycle, increas-
ing with inspiration and siowing down with expiration. This condition is called sinus
arrhythmia. Note if the child hs an irregular rhythm that is not related to breathing. An
iregular rhythm may indicate an underlying rhythm cisturbance, such as premature
ventricular or atrial contractions or an atrioventricular (AV) block
Fundamental Fact
Relationship of
eae Rca
Cy
For more information, see Part 8: “Recognition and
Management of Bradycardia,” Part 9: “Recognition and
Management of Tachycardia,” and Part 10: "Recognition,
‘and Management of Cardiac Arrest.”
Evaluation of pulses is critica to the assessment of sys-
temic perfusion in an ill or injured child. Palpate both cen-
tral and peripheral pulses. Central pulses are ordinarily
stronger than peripheral pulses because they are present
in vessels of larger size that are located closer to the heart.
Exeggeration of the difference in quality between central
land peripheral pulses occurs when peripheral vasocon-
striction is associated with shook. The following pulses ere
easily palpable in healthy infants and children (unless the
Child is Cbese or the ambient temperature is Cold)
Central Pulses
+ Femoral
* Brachial (in infants)
* Carotid (in older children)
+ Axillary
© Racial
* Dorsalis pedis
+ Posterior tibia)
heat
‘Weak central pulses are worrisome and indicate the need
for very rapid intervention to prevent cardiac arrest.
beat-to-beat fluctuation in pulse volume may occur in
children with arrhythmias (eg, premature atrial or ventricular
Contractions}. Fluctuation in pulse volume with the respira-
tory cycle (pulsus paradoxus) can occur in children with
severe asthma and pericardial tamponade. In an intubated
child receiving positive-pressure ventilatory support, a
reduction in pulse volume with each positive-pressure
breath may indicate hypovolemia.
Capillary Refill Time
Capillary refil ime is the time it takes for blood to return to
tissue blanched by pressure. Capillary refll time increases
as skin perfusion decreases. A prolonged capillary refi imo
may indicate low cardiac output. Normal capillary refill time:
Is <2 seconds,
Iti best to evaluate capillary refil in a neutral thermal envi-
ronment (ie, oom temperature). To evaluate capillery refill
time, lft the extremity slightly above the level of the heart
‘press on the skin, and rapa release the pressure. Note
how many seconds it takes for the area to return to its
baseline color,
{As cardiac output decreases in shock. systemic perfusion decreases incrementally.
The decrease in perfusion starts in the extremities with a Gecrease in intensity of
Deo ag aed
reed
pulses and then an absence of peripheral puises. As cardiac output and perfusion
decrease further, thore is eventual weakening of central pulses.
A cold environment can cause vasoconstriction and a discrepancy between peripheral
‘and central pulses. However, if cardiac output remains adequate, central pulses should
remain sirorg,
‘Common causes of sluggish, delayed, or prolonged capi
lary refill (a refil time >2 seconds) are dehydration, shock,
‘and hypothermia. Note that shock can be present despite
‘@ normal (or even brisk) capilary retil time. Children with
warm” septic shock (see Part 6: “Recognition of Shock"),
may have excellent (le, <2 seconds} capillary refill time
despite the presence of shock.
Skin Color and Temperature
‘Monitor changes in skin color, tomporature, and capillary
rofl time to assess a child's perfusion and response to
therapy. Normal skin color and temperature sould be con-
sistent over the trunk and extremities. The mucous mem-
branes, nail beds, palms of the hands, and soles of the feet
‘should be pink. When perfusion deteriorates and O; delivery
to the tiesues becomes inadequate, the hands and feet are
typicelly affected first. They may become cool, pale, dusky,
oF mottied, It perfusion becomes worse, the skin over the
trunk and extremities may undergo similar changes.
Carefully moniter for the following skin findings, which may
indicate inadequate O; dalivery to the tissues:
+ Pator
+ Motting
+ Cyanosis
Pallor, or paleness, Is a lack of normal cotor jn the skin or
mucous membrane. Pallor may be caused by
'* Decreased blood supply to the skin (cold, stress,
shock, especially hypovolemic end cardiogenic)
‘+ A decteased number of red blood cells (anemia)
++ Decreased skin pigmentation
Pallor must be interpreted within the context of other
signs and symptoms. It is not necessarily abnormal and
ccan result from lack of exposure to sunlight or inherited
palenass. Palloris often difficult to detect in a child with
dark skin, Thick skin and variation in the vascularity of
subcutaneous t'ssue also can make detection of pallor dif-
ficut, Family members often can toll you if a child's color
is abnormal, Central pallor (e, pale color of the lips and
mucous membranes) strongly suggests anemia or poor per-
fusion. Pallor of the mucous membranes (the lips, ining of
the mouth, tongue, lining of the eyes) an¢ pale palms and
soles are more likely to be clinically significant.
(Mottling is an irregular or patchy discoloration of the skin,
‘Areas may appear as an uneven combination of pink, bluish
gray, or pale skin tones. Mottling may occur due to variax
tions in distribution of skin melanin and may be normal.
Serious conditions, such as hypoxomia, hypovolemia, or
shock, may cause intense vasoconstriction from an irregular
supply of oxygenated biood to the skin, leacing to mottiing.
Cyanosis is a blue discoloration of the skin end mucous
membranes. Blood saturated with O, is bright red, whereas
unoxygenated blood is dark bluich-rod. The location of
‘cyanosis is important.
Acrocyanosis is a bluish discoloration of the hands and
feet. It is a common norma’ finding during the newborn
period,
Peripheral cyanosis (ie, bluish discoloration of the hands
‘and feat seen beyond the newborn period) can be caused
bby diminished O, delivery to the tissues. It may be seen
in conditions such as shock, congestive heart failure, or
peripheral vascular disease, or conditions causing
venous stacis,
Central cyanos's is a blue color of the lips and other
‘mucous membranes. Cyanosis is not apparent unti at
least § g/dL of hemoglobin are desaturated (not bound to
©,). The O; saturation at which a child will appear cyanotic
depends on the child's hemoglobin concentration. For ex-
‘ample, in a child with a hemoglobin concentration of 16 g/dl.
‘cyanosis will appear at an O; saturation of approximately
70% (le, 30% of the hemoglobin, oF 4.8 g/dL, is desatu-
rated). If the hemoglobin concentration is low (eg, 8 g/l),
a very low arterial O, saturation (eg, <40%) is required to
produce cyanosis, Thus, cyanosis may be apparent with a
eg tas Consider the temperature of the child's surroundings (ie, ambient temperature) when
evaluating skin color and temperature. If the ambiont temperature is cool, poriphoral
vasoconstriction may produce mottling or pallor with cool skin and delayed capitary
refil, particularly in the extremities, These changes develop despite normal cardiovas-
cular function
eeu ay
acu ie
To assess skin temperature, use the back of your hand. The back of the hand is more
sensitive to temperature changos than the palm, which has thicker skin. Slide the back
of your hand up the extremity to datermine if there is point where the skin changes
from cool to warm. Monitor this ine of demarcation between warm and coal skin over
time to determine the child's response to therapy. The line should move distally as the
child improves.
Se ee CR Tey
milder degree of hypoxemia in a child with cyanotic con-
genital neart cisease and polycythemia (increased amount
cf hemoglobin and red blood cel’) but may not be appar-
ent despite significant hypoxemia i the child is anemic.
The causes of central cyanosis include
+ Low ambient ©, tension (eg, high attitude)
* Alveolar hypoventiiation (eg, traumatic brain injury, drug
overdose)
* Diffusion defect (eg, pneumonia)
* Ventilation/perfusion imbalance (eg, asthma, bronchiol-
itis, ARDS)
* Intracardiac shunt (eg, cyanotic congenital heart
disease)
Cyanosis may be more obvious in the mucous membranes
and nail beds than in the skin, particulatly if the skin is
dark. It also can be seen on the soies of the fest, tip of the
nose, and earlobes. As noted above, children with aitferent
hemoglobin levels will be cyanotic at different levels of O;
‘saturation; cyanosis is more readily detected at higher O:
saturations if the hemoglobin level is high. The development
of central cyanosis typically indicates the need for emer-
gency intervention, such as Q, administration and ventiia-
tory support
Blood Pressure
Accurate blood pressure measurement requires a prop-
erly sized cul. The cuff bladder should cover about 40%
of the mid-upper arm circumference. The blood prossure
cuff should extend at least 50% to 75% of the length of
the upper arm (from the axilla to the antecubital fossa)
For more details see The Fourth Report on the Diagncsis,
Evaluation, and Treatment of High Blood Pressure in
Children and Adolescents, 2008 (full reference in the
Suggested Reading List at the end of this Part),
Normal Blood Pressures
‘Table 3 lists normal blood pressures by age. This table
‘summarizes the range from the 33rd to 67th percentile
in the first year of tie and from the 5th to 95th percentile
for systolic and diastolic blood pressure according to age
‘and gender and assuming the 50th percentile for height
Teas Red
for children 21 year of ago. Like heart rate, there is a wide
range of values within the normal range.
‘Table 3. Normal Blood Pressures in Children by Age
See moet ar
ee poor’
a) )
Neonate | 601076 | 601074 | 31t045 | 3010.44
(day)
Neonate | 671063 | 681064 | 971059 | 351059
(4 days)
Infant 731091 | 741094 | 961056 | 37 1085
(1 month)
Infant Tato 100 | 8110 103 | 4064 | 451065
(@ months)
Infant 820 102 | 8710 105 | 461066 | 48 1068
(6 months) |
Infant 6810 104 | 6710 108 | 2210 60 | 201058
(1 yea)
Child 710 105 | 70t0 106 | 2710 65 | 251069
(2years) fo |
chia (7 | 7910113 | 7910118 | s9t0 77 | 381078
years)
‘Adolescent | 9310 127 | 05t0 131 | 471085 | 45 1085
(15 years)
‘Blood proseurerangos for nacnate and infat 1 to 6 montha) are
from Gemeli i, Mancanaro R, Marri C, De Luca F Longtudinal
study of blood pressure durng the 1st your off, Eur J Pec
1990:1493318-320.
Blood presaue ranges for infant (1 year child, and adolescent are
from National High Blood Pressure Education Program Vioking Group
(on High Blood Pressure in Children and Adolescents. The Fourth
‘Report on the Diagnosis, Evaluation, and Treatment of High Blood
Pressure #1 Children and Adolescents, Bethesda, MD: National Heat,
Lung. and Blood Institute: 2005. NH publication 05-5267,
Hypotension
Hypotension is defined by the thresholds of systolic blood
pressure in Table 4
Table 4. Definition of Hypotension by Systolic Blood
Pressure and Age
Beers)
ae au)
Term neonates <60
(0 to 28 days)
Infants (1 to 12 months) <70 |
Children 1 to 10 years ‘<70 + (age in years = 2)
{6th blood prossure
percentile)
Children >10 years <90
Note that these blood pressure thresholds approximate just
above the 5th percentile systolic blood pressures for age,
so they will overlap with normal blood pressure values for
‘5% of healthy children, An observed decrease in systolic
blood pressure of 10 mm Hg from baseline should prompt
serial evaluations for additional signs of shock. In addition,
remember that these threshold values were established
in normal, resting children. Children with injury and stress
typically have increased blood pressure. A blood pressure
in the low-normal range may be abnormal in a seriously
ilchid,
Er ue lia lad
ecco
Coens
et ae es
ened
Assessment of Urine
Ort
‘When hypotension develops in a child with shock, physiologic compensatory
mechanisms (eg, tachycardia and vasoconstriction) have failed. Hypotension with
hemorrhage is thought to be consistent with an acute joss of 20% to 25% of circulat
1g blood volume. Hypotension may be a sign of septic shock, where there is inappro-
priate vasodilation rather than loss of intravascular volume.
The development of bradycarcia in a child with tachycardia and hypotension is an
‘ominous sign, Management of airway and breathing and aggressive fluid resuscitation
are needed to prevent cardiac arrest.
Urine output 's an indirect indication of Kidney perfusion. Children with shock typically
have decreased urine output.
Measure urine output in all critically ill or injured children with an indwelling catheter.
Initial urine output is not a reliable indicator of the child's clinical condition because
uch of the urine may have been produced before the onset of symptoms. An
increase in urine output is a good indicator of positive response to therapy.
Disability
D
‘The disability assessmont is a quick evaluation of neuro-
logie function. Rapid assessment can use one of several
tools to evaluate responsiveness and level of conscious:
ress. Perform this evaluation at the end of the primary
assessment, Repeat it during the secondary assessment 10
moritor for changes in the chilc’s neurologic status,
Clinical signs of brain perfusion are important indicators
of circulatory function in the ill or injured pediatric patient,
‘These signs incide level of consciousness, muscle tone,
‘and pupil responses. Signs of inadequate O, delivery to the
brain correlate with the severity and duration of cerebral
hypoxia,
‘Sudden and severe cerebral hypoxia may present with the
folowing neurologic signs:
* Docreasod level of consciousness
* Loss of muscular tone
* Generalized seizures
* Pupi dilation
SU a er enn ea ee thea ed
‘You may observe other neurologic signs when cerebral
hypoxia develops gradually. These signs can be subtle and
are best detected with repeated measurements over time:
‘+ Decreased level of consciousness with confusion
* Ietapaity
* Letnaray
* Agitation aternating with letharay
‘Standard evaluations incluce
+ AVPU (Alert, Responsive to Voice, Responsive to Pain,
Urresponsive) Pediatrie Response Seale
* Glasgow Coma Scale (GCS)
* Pupil response to light
AVPU Pediatric Response Scale
To rapidly evaluate cerabral cortex function, use the AVPU.
Pediatric Response Scale. This scale is a system for rating
a child's level of consciousness, an indicator of cerebral
cortex function. The scale consists of 4 ratings:
Auer
The child is awake, active, and
‘appropriately responsive to parents
‘and external stimuli, “Appropriate
responea" is assossod in terms of the
anticipated response based on the
chid's age and the setting or situation.
The child responds only to voice (eg,
tho child’s name or speaking
Voice
foul)
‘The child responds only to a paintul
‘stimulus, such as pinching the nail
bod,
Paintui
‘The child does not respond to any
Unresponsive
pene | stimulus.
Causes of decreased level of consciousness in children
include
+ Poor cerebral perfusion
+ Traumatic brain injury
* Encephalitis, meningitis
+ Hypoglycemia
+ Drugs
+ Hypoxemia
+ Hypercarbia
| an if or injured child has decreased responsiveness, immediately assess oxygen-
ation, ventilation, and perfusion.
Glasgow Coma Scale Overview
The GCS is the most widely used method of evaluating
2 child's level of consciousness and neurologic status,
‘Tho chic's best eye opening (6), verbal (V), and motor (My
responses are individually scored (Tebe §). The individual
scores are then added together to produce the GCS score,
For example: A child who has spontaneous eye opening
(E = 4) is fully oriented (V = 5), and is able to follow com-
‘mands (M = 6) is assigned a GCS score of 15, the highest
possible score. A child with no oye opening (E = 1), no
verbal response (V = 1), and no motor response (M = 1) to
4 painful stimulus is assigned a GCS score of 3, the lowest
possible score,
‘Severity of head injury is categorized into 3 levels based on
GCS score alter intial resuscitation:
+ Mild head injury: GCS score 13 to 15
+ Moderate head injury: GCS score 9 to 12
+ Severe head injury: GCS score 3 to 8
Glasgow Coma Scale Scoring
‘The GOS has been moditied for preverbal or nonverbal
‘children (Table 5}. Scores for eye opening are essentially the
‘same as for the standard GCS. The best motor response
‘score (of a possible 6 requires that a child fotow com-
‘mands, so this section was adapted to accommodate the
preverbal or nonverbal child. The verbal score wes also
adapted to assess age-appropriate responses.
‘Important: When using the GCS cr its pediatric modifioa-
tion, record the individual components of the score. if the
Patient is intubated, unconscious, or preverbal, the most
important part of this scale is motor response, Providers
should carefully evaluate this component.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Psychological Anatomy and Psychotherapy Psyc 101Document4 pagesPsychological Anatomy and Psychotherapy Psyc 101willNo ratings yet
- Adult Basic Life Support Algorithm For Healthcare ProvidersDocument1 pageAdult Basic Life Support Algorithm For Healthcare ProvidersKavya ShreeNo ratings yet
- Adult Cardiac Arrest Algorithm: VF/PVT Asystole/PEADocument1 pageAdult Cardiac Arrest Algorithm: VF/PVT Asystole/PEARamos SiahaanNo ratings yet
- Psyc 101 Quiz Gross Human SociologyDocument3 pagesPsyc 101 Quiz Gross Human SociologywillNo ratings yet
- Psyc 102 Quiz Human SociologyDocument3 pagesPsyc 102 Quiz Human SociologywillNo ratings yet
- Midterm 2015 PDFDocument12 pagesMidterm 2015 PDFwillNo ratings yet
- Astronomy NotesDocument11 pagesAstronomy NoteswillNo ratings yet
- Vegetation and Soil CanadaDocument2 pagesVegetation and Soil CanadawillNo ratings yet
- 生命是美麗的 - jok2945 ppt - 0Document25 pages生命是美麗的 - jok2945 ppt - 0willNo ratings yet