Professional Documents
Culture Documents
Clinical Examination and Non
Uploaded by
Miguel SalesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Examination and Non
Uploaded by
Miguel SalesCopyright:
Available Formats
MR BARIS ATA OZDEMIR (Orcid ID : 0000-0002-0982-4482)
Article type : Research Article
Accepted Article
Title: Diabetic Medicine
Created by: Maria Hale
Accepted: 26.03.2018
Email proofs to: drbaozdemir@gmail.com
Copyright: Diabetes UK
Article no.: DME-2017-00837
Article type: Research Article
Short title/Authors running head: Screening teats for peripheral artery disease in diabetes-related foot
ulceration V. Vriens et al.
Research: Treatment
Clinical examination and non-invasive screening tests in
the diagnosis of peripheral artery disease in people with
diabetes-related foot ulceration
B. Vriens1, F. D’Abate2, B. A. Ozdemir2, C. Fenner2, W. Maynard2, J. Budge2,
D. Carradice3 and R. J. Hinchliffe4
1
Vascular Department, Colchester General Hospital, Colchester Hospital University NHS Foundation Trust,
Colchester, 2St. George’s Vascular Institute, St. George’s Hospital, St. George’s University NHS Foundation
Trust, London, 3Academic Vascular Surgical Unit, Hull York Medical School, Hull and 4Bristol Centre for
Surgical Research, University of Bristol, Bristol, UK
Correspondence to: Baris A. Ozdemir. E-mail: drbaozdemir@gmail.com
This article has been accepted for publication and undergone full peer review but has not
been through the copyediting, typesetting, pagination and proofreading process, which may
lead to differences between this version and the Version of Record. Please cite this article as
doi: 10.1111/dme.13634
This article is protected by copyright. All rights reserved.
What’s new?
We evaluated the utility of clinical examination and non-invasive bedside tests in
Accepted Article
screening for peripheral artery disease in people with diabetes. This study is unique in
both the wide variety of tests investigated and that all participants had ulceration.
Screening tests must reliably exclude the disease, as it is associated with both failure
to heal and major amputation. We demonstrate that only toe–brachial index and tibial
waveform analysis would be considered suitable for screening to exclude peripheral
artery disease. Simple bedside clinical examinations such as pulse assessment are
unreliable in excluding peripheral artery disease in this cohort.
Abstract
Aim Peripheral artery disease is common in people with diabetes-related foot ulceration and
is a risk factor for amputation. The best method for the detection or exclusion of peripheral
artery disease is unknown. This study investigated the utility of clinical examination and non-
invasive bedside tests in screening for peripheral artery disease in diabetes-related foot
ulceration.
Methods Some 60 people presenting with new-onset ulceration participated. Accuracy of
pulses, ankle pressure, toe pressure, toe–brachial index (TBI), ankle–brachial pressure index
(ABPI), pole test at ankle, transcutaneous oxygen pressure and distal tibial waveform on
ultrasound were examined. The gold standard diagnostic test used was > 50% stenosis in any
artery or monophasic flow distal to calcification in any ipsilateral vessel on duplex
ultrasound.
This article is protected by copyright. All rights reserved.
Results The negative and positive likelihood ratios of pedal pulse assessment (0.75, 1.38) and
the other clinical assessment tools were poor. The negative and positive likelihood ratios of
Accepted Article
ABPI (0.53, 1.69), transcutaneous oxygen pressure (1.10, 0.81) and ankle pressure (0.67,
2.25) were unsatisfactory. The lowest negative likelihood ratios were for tibial waveform
assessment (0.15) and TBI (0.24). The highest positive likelihood ratios were for toe pressure
(17.55) and pole test at the ankle (10.29) but the negative likelihood ratios were poor at 0.56
and 0.74.
Conclusions Pulse assessment and ABPI have limited utility in the detection of peripheral
artery disease in people with diabetes foot ulceration. TBI and distal tibial waveforms are
useful for selecting those needing diagnostic testing.
<H1>Introduction
Diabetes mellitus affects large numbers of people globally. Worldwide there has been a
dramatic increase in the prevalence, resulting in an inevitable rise in diabetes-related
complications and costs [1,2]. It is estimated that foot ulceration associated with diabetes and
diabetes cost the National Health Service (NHS) £1 billion annually in England [3]. As
diabetes becomes more prevalent, these costs are likely to increase. Diabetes mellitus is an
important factor implicated in the development of both peripheral artery disease and foot
ulceration. In the general population with diabetes, the prevalence of peripheral artery disease
is 10–26%; in people with associated foot ulceration this increases to > 50% [4–6]. It is
imperative to identify peripheral artery disease, which is associated with both delayed healing
and amputation, so that appropriate interventions can be offered [7].
This article is protected by copyright. All rights reserved.
National guidelines recommend that all individuals with diabetes-related foot ulceration are
managed by a multidisciplinary foot care team. In England and Wales, 31.0% of sites do not
Accepted Article
have a multidisciplinary team and of those that do, only 61.5% include a vascular surgeon
[8]. Focused clinical examination of the feet, particularly palpation of foot pulses, remains
fundamental to assessment [9,10]. Nevertheless, palpation of foot pulses, especially in the
presence of peripheral neuropathy, can be unreliable in screening for the presence of
peripheral artery disease in people with diabetes [11]. A range of non-invasive bedside
screening tests are available as an adjunct to clinical examination, including ankle–brachial
pressure index (ABPI), toe–brachial index (TBI) and transcutaneous pressure of oxygen
(TcPO2) [9].
Non-invasive screening tests for the detection of peripheral artery disease among individuals
with diabetes are considered important to estimate the risk of amputation, ulceration, wound
healing and the presence of cardiovascular disease, yet there are no consensus
recommendations to support one modality over another [12,13]. Surprisingly, to date, the
number of studies assessing the utility of peripheral artery disease screening tests in people
with established ulceration has been limited in both number and scope [9]. Most studies have
either excluded or not separately reported the efficacy of peripheral artery disease screening
tools in people with ulceration. Those studies that did detail assessment of people with
ulceration have investigated only a narrow range of tools. This is unfortunate as the
identification of peripheral artery disease is more influential on diabetes management in the
cohort with ulceration than those with intact feet.
This is the first study to investigate the efficacy of both clinical assessment and a wide battery
of peripheral artery disease screening tools in individuals with diabetes-related foot
ulceration.
This article is protected by copyright. All rights reserved.
<H1>Participants and methods
Ethical approval for the study was granted by the NHS Health Research Authority (NRES)
Accepted Article
Committee London – City Road and Hampstead (Reference 12/LO/1579) and the research
was performed according to the Declaration of Helsinki (2008).
<H2>Study design and participants
People with diabetes presenting to either a multidisciplinary diabetes foot clinic or emergency
department with foot ulceration of < 2 months duration were recruited into this prospective,
single-centre observational study at a large teaching hospital.
All individuals with diabetes, regardless of type, presenting with primary lower limb
ulceration were potentially eligible. Exclusion criteria were: aged < 18 years, previous
revascularization, non-diabetes related ulceration, lacking capacity to consent to inclusion in
the study and pregnant. Informed, written consent was obtained from all those willing to
participate in the study.
All study assessments were undertaken during routine clinical visits. Patient management
followed routine local protocols which are themselves compliant with national guidance [14].
<H2>Clinical and radiological assessors
Participants were assessed clinically, and the screening were tests performed by a single post-
completion of training vascular surgical fellow, experienced in the management of diabetes-
related ulceration and familiar with the screening tools. Additional training was provided to
the screener by the vascular laboratory for toe pressure and TcPO2 assessment to ensure
compliance with the manufacturer’s recommendation.
This article is protected by copyright. All rights reserved.
Patients and their medical records were consulted for demographic data.
Clinical examination included documentation of characteristics of the lower limbs, namely
Accepted Article
hair loss, muscle atrophy, dependent rubor, cool skin, blue or purple skin, capillary refill time
and venous filling time. A capillary refill time of > 2 s and a venous filling time of > 15 s
were classified as screen positive for peripheral artery disease. Other clinical examination
criteria were recorded as present or absent based on the assessor’s subjective judgement.
The presence of peripheral neuropathy was determined using a 10-G monofilament applied to
the tips of the first, third and fifth toes, and the dorsum of both halluces for 2 s [15]. Absence
of sensation in any one of these areas was classified as neuropathy. Peripheral pulses
(femoral, popliteal, dorsalis pedis and posterior tibial) were palpated bilaterally. Absent pedal
pulses were classified as indicating peripheral arterial disease.
The ulcer was examined, and the severity was staged using the Site, Ischemia, Neuropathy,
Bacterial infection, Area, Depth (SINBAD) classification [15,16]. The Society of Vascular
Surgery Wound Infection Ischaemia (SVS WIfI) score was used to classify the clinical status
of the foot [17].
<H2>Screening tests
Screening tests were performed after a 20-min rest period at room temperature (18–20 °C)
room. Participants were placed in a 30° reclined position on a clinical examination couch. A
duplex ultrasound scan was performed by a single experienced and accredited vascular
sonographer. The investigator and sonographer were blinded to each other’s findings.
This article is protected by copyright. All rights reserved.
<H2>Ankle pressure and ankle–brachial pressure index
Ankle and brachial pressures were measured using a manual inflatable cuff and a handheld
Accepted Article
continuous-wave Doppler probe (Huntleigh Dopplex MD2, Huntleigh, UK). Ankle pressure
of < 70 mmHg was considered abnormal. A resting ABPI was performed using the brachial
pressure on the right arm and the pressure values at the level of the posterior tibial artery and
dorsalis pedis artery. The highest calculated ABPI value was used in the analysis with a value
< 0.9 or > 1.3 classified as abnormal.
<H2>Toe pressures, toe–brachial pressure index and TcPO2
Toe pressures were measured using a laser Doppler probe and toe pressure cuff (Periflux
5000 with PF 5010 laser Doppler perfusion monitor unit and PF 5050 pressure unit with PF
5051 pressure accessory kit, Perimed AB, Datavägen, Sweden) on the largest available toe.
Three separate readings were obtained over a 5-min interval and the mean of the values was
used. Toe pressure of < 50 mmHg was considered abnormal. A TBI of ≤ 0.75 was considered
abnormal.
TcPO2 measurements were taken from the dorsum of the foot using (Periflux 5000 with PF
5010 laser Doppler perfusion monitor unit and PF 5020 temperature unit, Perimed AB). The
skin was cleaned with normal saline, an adhesive ring applied and the manufacturer’s
recommended contact liquid introduced. The probe was then attached and left in place for
15 min while the trace was recorded. TcPO2 < 60 mmHg was considered abnormal [18].
This article is protected by copyright. All rights reserved.
<H2>Pole test
The pole test was performed using a handheld Doppler probe (Huntleigh Dopplex MD2,).
Accepted Article
With the patient supine, the leg was elevated passively at the hip while continuing to listen
for the Doppler signal. The height (in cm) at which the Doppler signal was lost was recorded.
To confirm that flow was lost, the leg was lowered and considered positive if the flow to the
vessel returned. The test was repeated on both the dorsalis pedis and posterior tibial arteries
bilaterally. The highest of the two measurements was used for analysis. If there was no loss
of flow or the patient was unable to elevate the leg, this was recorded [19,20].
<H2>Waveform analysis
Waveforms recorded at the level of the distal tibial arteries were included in the analysis to
verify whether Doppler waveforms at this level could be discriminatory in identifying
peripheral artery disease. Recordings were made at the level of the medial malleolus, the
dorsalis pedis and in the mid-calf for the peroneal artery. It is important to note that this part
of the analysis was not blinded, i.e. the vascular sonographer performing the reference scan
also performed the tibial waveform analysis.
<H2>Gold standard test
A duplex ultrasound scan was performed by an accredited vascular scientist using a GE Logic
E9 ultrasound scanner (GE, Green Bay, WI, USA). The abdominal, femoral and lower limb
arteries (femoral, popliteal and tibial) supplying the ulcerated limb were studied. A C5-
1 MHz curvilinear array was used to assess the abdominal vessels, whereas a linear 3–9 MHz
transducer was used for the lower limb arteries. All arteries were examined by using a
This article is protected by copyright. All rights reserved.
combination of B-mode imaging, colour Doppler and spectral Doppler ultrasound in
transverse and longitudinal planes. Peak systolic velocity (PSV) was measured throughout the
Accepted Article
iliac, femoral, popliteal and tibial arteries and recorded for further analysis only in the distal
tibial arteries. PSV was measured at the point in the vessel where the highest velocity was
detected. The PSV ratio between a stenosed region and the proximal PSV was used to grade
stenosis and was classified as abnormal when the PSV ratio was > 2, which represents a
stenosis of > 50%.
Flow velocity waveforms were also recorded. Triphasic or biphasic waveforms with a fast
systolic rise time and no flow at end-diastole were considered normal lower limb resting
waveforms. Monophasic (damped) waveforms were considered abnormal and indicative of
proximal arterial obstructive disease. At the site of a stenosis the flow waveform has
abnormally high velocities throughout the cardiac cycle with a ragged outline due to the
presence of turbulent flow. Distal to a stenosis the waveform is damped with a prolonged
systolic rise time and forward flow throughout the cardiac cycle.
Peripheral artery disease was defined as > 50% stenosis in any named lower limb artery or
monophasic flow beneath a calcified segment [14,21,22].
<H2>Statistical analysis
Statistical analysis was performed using R 3.1.1 (R Core Team, R Foundation for Statistical
Computing, Vienna, Austria).
The negative likelihood ratio (NLR) was the primary outcome of interest. The positive
likelihood ratio (PLR), sensitivity, specificity, positive and negative predictive values are also
reported. The NLR is the probability of a negative test in an individual with the disease
This article is protected by copyright. All rights reserved.
divided by the probability of a negative testing in an individual without the disease
(1 − sensitivity/specificity). The PLR is the probability of a positive test in an individual with
Accepted Article
the disease divided by the probability of positive test in an individual without the disease
(sensitivity/1 − specificity).
The likelihood ratios detail the extent to which the outcome of a test alters the pretest
probability of disease. Interpretation is influenced by context but, in general, a NLR < 0.1
suggests that a test can reliably exclude disease and PLR > 10 can reliably confirm the
presence of a disease [23].
<H1>Results
Some 60 participants with diabetes-related foot ulceration were included in the study (Table
1). The ulcer characteristics of the study participants are detailed in Tables 2 and 3. A total of
20 (33%) participants had peripheral artery disease on diagnostic ultrasound.
The NLR and PLR of pedal pulse assessment (0.75, 1.38) and the other physical examination
findings were poor (Table 4). Similarly, the NLR and PLR of ABPI (0.53, 1.69), TcPO2 (1.1,
0.81) and ankle pressure (0.67, 2.25) as screening tools to identify peripheral artery disease
were unsatisfactory. The lowest NLR was for tibial waveform assessment (0.15) and TBI
(0.24). The highest PLR were for toe pressure (17.55) and pole test at the ankle (10.29), but
the NLR values were again poor at 0.56 and 0.74, respectively (Table 4).
This article is protected by copyright. All rights reserved.
<H1>Discussion
The identification of peripheral artery disease is crucial to the management of diabetes-
Accepted Article
related foot ulceration because it risk stratifies people that are at greater risk of failure to heal,
amputation and, perhaps more importantly, those who may potentially benefit from
revascularization [7]. The most important characteristic of a screening tool in people with
established ulceration is therefore the ability to exclude peripheral artery disease. Any screen-
positive patient will need to undergo one or more reference investigations to confirm or
exclude peripheral artery disease and detail the anatomy of the lower limb arterial tree. The
consequences of a false negative are potentially more severe than the consequences of a false
positive, as the initial diagnostic tests utilized by most units are non-invasive and unlikely to
lead to harm. To this end a NLR < 0.1 provides convincing screening evidence that the
disease is absent [23]. In our study, no test achieved this cut-off but the toe brachial pressure
index and tibial waveform analysis, which almost reached this threshold, could be considered
as screening tools, with caveats. In our study population, where prevalence was lower than
the reported literature, TBI would have led to false negatives in two (10.5%) and tibial
waveform analysis in three (7.0%) of those with peripheral artery disease. We therefore
recommend that patients classified as screen-negative with these tests are monitored closely.
A degree of clinician judgement is required but in practice those with severe ulceration, ulcer
deterioration or failure to progress, should still undergo formal diagnostic imaging. We
certainly recommend that clinicians without access to these tools request formal imaging to
exclude peripheral artery disease. Unfortunately, the commonly used clinical assessments
including pulse assessment and screening tests such as ankle pressure and ABPI are not very
useful for disease exclusion in people with established ulceration.
This article is protected by copyright. All rights reserved.
This analysis is consistent with previous research that has demonstrated that the utility of
pulse assessment, ankle pressure and ABPI to identify peripheral artery disease in those with
Accepted Article
neuropathy (85% of our cohort) is low. It is anticipated that the utility of these tests
diminishes further in individuals with ulceration. This is expected because oedema,
calcification and arteriovenous shunting all increase with progression of diabetes and unduly
influence the outcome of these screening tests [24]. Previous studies assessing the utility of
ABPI in intact feet have demonstrated NLR values of < 0.1 to 0.5 [26,27]. Although Aboyans
et al. [27] reported a NLR of < 0.1 in a cohort with 94% ulceration, most other studies that
explicitly include some individuals with ulcers report NLR values ranging from 0.3 to 0.7
[21,27–29]. Williams et al. [25] reported that the NLR for TBI was < 0.1 for people with
intact feet and neuropathy. Predictably, in our cohort with ulceration, TBI performed less
well with a NLR of 0.24. Nevertheless, TBI probably represents the most useful screening
tool for peripheral artery disease in the community foot clinic where access to diagnostic tests
may be limited. Unfortunately, due to previous minor amputations or digital ulcers not all can
undergo this investigation.
Waveform analysis was the best screening tool to exclude peripheral artery disease in our
study and Normahani and colleagues [30] demonstrate that it is possible to train podiatrists to
perform a focused duplex ultrasound scan of the tibial vessels at the ankle. The costs of
training and the availability of ultrasound machines may be limitations. Medical devices are
available that can record the ankle pulse waveform but their utility in individuals with
established ulceration remains to be assessed [31]. We did not have access to this technology
at the time of the study. An alternative is to refer all those with ulceration for a limited tibial
waveform scan by a vascular sonographer. Only those who screen positive should then
proceed to full duplex ultrasound
This article is protected by copyright. All rights reserved.
<H2>Strengths and limitations
This study focused on the identification of peripheral artery disease as the primary outcome
Accepted Article
of interest. Despite its importance, not all those with peripheral artery disease require
revascularization to heal their ulcer. An additional consideration is whether perfusion is
adequate to heal the ulcer with best medical and wound care, i.e. is revascularization
required? This is a more complex and different question and would require a different study
design to reach a conclusion. Screening tools that exclude peripheral artery disease can help
to identify individuals that are unlikely to benefit from more time-consuming and costly
diagnostic investigations that sometimes expose the patient to nephrotoxic agents or
radiation.
We chose a definition of abnormal ABPI of < 0.9 or > 1.3. Most studies assessing the utility
of ABPI as a screening test for peripheral artery disease use a value of < 0.9. Our definition
of abnormal ABPI was chosen because we restricted our study to those with established
ulceration where robust exclusion is more important than specificity.
To our knowledge this is the first study to test such a wide variety of peripheral artery disease
screening tools in individuals with ulceration. Other screening tools are available that were
not included in this study such as pulse oximetry.
The clinical assessment of our participants was performed by a post-completion of training
vascular fellow. The applicability of this assessment to non-specialist nurse or podiatrists is
unknown. We anticipate that the ability of pulse assessment to exclude peripheral artery
disease would be even worse if undertaken by non-specialists.
The size of the study was limited to 60 participants due to the time-consuming nature of
performing such a wide battery of tests for each participant. Future studies or registries,
This article is protected by copyright. All rights reserved.
validating the findings of this study, should focus on TBI and tibial waveform analysis alone
to facilitate the inclusion of a larger number of patients. A larger study could also help to
Accepted Article
address the question of whether a combination of ulcer characteristics and these two tests
could be used to more reliably exclude peripheral artery disease in people with diabetes-
related foot ulceration.
<H1>Conclusions
TBI and tibial waveform analysis at the ankle are viable screening tools to exclude peripheral
artery disease in people with foot ulceration where the equipment and training for their
utilization exists or can be set up. However, even these tools can miss patients with peripheral
artery disease so patients with severe ulceration, failure to progress or deterioration should
undergo diagnostic vascular imaging. Traditionally used clinical assessment and alternative
screening tools perform poorly in excluding peripheral artery disease in people with
established diabetes-related foot ulceration. In the absence of appropriate TBI or tibial
waveform analysis all individuals with diabetes-related foot ulceration should undergo
diagnostic vascular imaging unless there is a very rapid response to best medical and wound
care.
Funding sources
None.
This article is protected by copyright. All rights reserved.
Competing interests
None declared.
Accepted Article
References
1 Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ et al.; Global
Burden of Metabolic Risk Factors of Chronic Disease Xollaborating Group (Blood
Glucose). National, regional, and global trends in fasting plasma glucose and diabetes
prevalence since 1980: systematic analysis of health examination surveys and
epidemiological studies with 370 country years and 2.7 million participants. Lancet
2011; 378: 31–40
2 Van Houtum WH, Lavery LA, Harkless LB. The costs of diabetes related lower
extremity amputations in the Netherlands. Diabetic Med 1995; 12: 777–781.
3 Diabetes UK. Improving footcare for people with diabetes and saving money: an
economic study in England. Available at https://diabetes-resources-production.s3-eu-
west-1.amazonaws.com/diabetes-
storage/migration/pdf/Improving%2520footcare%2520economic%2520study%2520%28Janu
ary%25202017%29.pdf Last accessed 9 February 2018.
4 Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in
the United States: results from the national health and nutrition examination survey.
Circulation 2004; 110: 738–743.
5 Jude EB, Oyibo SO, Chalmers N, Boulton AJM. Peripheral arterial disease in diabetic
and nondiabetic patients a comparison of severity and outcome. Diabetis Care 2001;
24: 1433–1437.
This article is protected by copyright. All rights reserved.
6 Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K et al. High
prevalence of ischaemia, infection and serious comorbidity in patients with diabetic
Accepted Article
foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007;
50: 18–25.
7 Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D et al.
Prediction of outcome in individuals with diabetic foot ulcers: focus on the
differences between individuals with and without peripheral arterial disease. The
EURODIALE Study. Diabetologia 2008; 51: 747–755.
8 NHS Digital. National Diabetes Inpatient Audit 2015. Available at
https://digital.nhs.uk/media/28531/National-Diabetes-Inpatient-Audit-NaDIA-2015-
annual-report-Supporting-data/Any/nati-diab-inp-audi-15-sup-dat Last accessed 9
February 2018.
9 Brownrigg JRW, Schaper NC, Hinchliffe RJ. Diagnosis and assessment of peripheral
arterial disease in the diabetic foot. Diabet Med 2015; 32: 738–747.
10 Hinchliffe RJ, Brownrigg JRW, Apelqvist J, Boyko EJ, Fitridge R, Mills JL et al.
IWGDF guidance on the diagnosis, prognosis and management of peripheral artery
disease in patients with foot ulcers in diabetes. Diabetes Metab Res Rev 2016;
32(Suppl. 1): 37–44.
11 Williams DT, Harding KG, Price P. An evaluation of the efficacy of methods used in
screening for lower-limb arterial disease in diabetes. Diabetes Care 2005; 28: 2206–
2210.
12 Brownrigg JRW, Hinchliffe RJ, Apelqvist J, Boyko EJ, Fitridge R, Mills JL et al.;
International Working Group on the Diabetic Foot. Performance of prognostic
markers in the prediction of wound healing or amputation among patients with foot
This article is protected by copyright. All rights reserved.
ulcers in diabetes: a systematic review. Diabetes Metab Res Rev 2016; 32(Suppl. 1):
128–135.
Accepted Article
13 Brownrigg JRW, Hinchliffe RJ, Apelqvist J, Boyko EJ, Fitridge R, Mills JL et al.;
International Working Group on the Diabetic Foot. Effectiveness of bedside
investigations to diagnose peripheral artery disease among people with diabetes
mellitus: a systematic review. Diabetes Metab Res Rev 2016; 32(Suppl. 1): 119–127.
14 National Institute for Health and Clinical Excellence. Diabetic Foot Problems.
Inpatient Management of Diabetic Foot Problems. Clinical guideline 119. Available
at
https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0041804/pdf/PubMedHealth_PMH
0041804.pdf Last accessed 17 October 2017.
15 Rayman G, Vas PR, Baker N, Taylor CG Jr, Gooday C, Alder AI et al. The Ipswich
Touch Test: a simple and novel method to identify inpatients with diabetes at risk of
foot ulceration. Diabetes Care 2011; 34: 1517–1518.
16 Ince P, Abbas ZG, Lutale JK, Basit A, Ali SM, Chohan F et al. Use of the SINBAD
classification system and score in comparing outcome of foot ulcer management on
three continents. Diabetes Care 2008; 31: 964–967.
17 Mills JL, Conte MS, Armstrong DG, Pomposelli FB, Schanzer A, Sidawy AN et al.;
Society for Vascular Surgery Lower Extremity Guidelines Committee. The Society
for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk
stratification based on wound, ischemia and foot infection (WIfI). J Vasc Surg 2014;
59: 220–234.
18 Norgen L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR on behalf
of the TASC II Working Group. Inter-society consensus for the management of
peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg 2007; 33: S1–S70.
This article is protected by copyright. All rights reserved.
19 Paraskevas N, Ayari R, Malikov S, Mollo M, Branchereau P, Hut F et al. ‘Pole test’
measurements in critical leg ischaemia. Eur J Vasc Endovasc Surg 2006; 31: 253–
Accepted Article
257.
20 Pâhlsson H, Wahlberg E, Olofsson P, Swedenborg J.The toe pole test for evaluation
of arterial insufficiency in diabetic patients. Eur J Vasc Endovasc Surg 1999; 18:
133–137
21 Clairotte C, Retout S, Potier L, Roussel R, Escoubet B. Automated ankle–brachial
pressure index measurement by clinical staff for peripheral arterial disease diagnosis
in nondiabetic and diabetic patients. Diabetes Care 2009; 32: 1231–1236.
22 Zhang H, Li XY, Si YJ, Lu XL, Luo XS, Liu ZY. Manifestation of lower extremity
atherosclerosis in patients with high ankle–brachial index. Br J Diabetes Vasc Dis
2009; 9:160–164.
23 Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature III. How
to use an article about a diagnostic test. B. What are the results and will they help me
in caring for my patients? JAMA 1994; 271: 703–707.
24 Ozdemir BA, Brownrigg JR, Jones KG, Thompson MM, Hinchliffe RJ. Systematic
review of screening investigations for peripheral arterial disease in patients with
diabetes mellitus. Surg Technol Int 2013; 23: 51–58.
25 Williams DT, Harding KG, Price P. An evaluation of the efficacy of methods used in
screening for lower-limb arterial disease in diabetes. Diabetes Care 2005; 28: 2206–
2210.
26 Lewis JEA, Owens DR. The pulse volume recorder as a measure of peripheral
vascular status in people with diabetes mellitus. Diabetes Tech Ther 2010; 12: 75–82.
This article is protected by copyright. All rights reserved.
27 Aboyans V, Ho E, Denenberg JO, Ho LA, Natarajan L, Criqui MH. The association
between elevated ankle systolic pressures and peripheral occlusive arterial disease in
Accepted Article
diabetic and nondiabetic subjects. J Vasc Surg 2008; 48: 1197–1203.
28 Premalatha G, Ravikumar R, Sanjay R, Deepa R, Mohan V. Comparison of colour
Duplex ultrasound and ankle–brachial pressure index measurements in peripheral
vascular disease in type 2 diabetic patients with foot infections. J Assoc Physicians
India 2002; 50: 1240–1244.
29 Vogelberg KH, Stork W. Measurement of pulse reappearance time in diagnosis of
peripheral vascular disease in diabetes. Diabetes Care 1988; 11: 345–350.
30 Normahani P, Powezka K, Aslam M, Standfield N, Jaffer U. Podiatry ankle duplex
scan: readily learned and accurate in diabetes. Angiology 2018; 69: 220–227.
31 Lewis JEA, Williams P, Davies JH. Non-invasive assessment of peripheral arterial
disease: automated ankle brachial index measurement and pulse volume analysis
compared to duplex scan. SAGE Open Med 2016; 4: 2050312116659088.
This article is protected by copyright. All rights reserved.
Table 1 Demographics of study participants
Age, years* 66 (29–92)
Male 45 (75)
Accepted Article
Inpatient 15 (25)
Duration of diabetes, years* 2 (0.04–62)
HbA1c, mmol/mol* 65 (36–106)
HbA1c, %* 8.1 (5.4–16.2)
Diabetes:
Type 1 7 (12)
Type 2: Diet/oral hypoglycaemic only 23 (28)
Type 2: Requiring insulin 30 (50)
Smoking:
Never or stopped > 10 years 44 (73)
Stopped < 10 years ago 9 (15)
Abstinence < 1 year or < 1 pack/day 3 (5)
> 1 pack/day 4 (7)
Hypertension 44 (73)
Hyperlipidaemia†
Absent 10 (17)
Diet controlled 7 (12)
Diet and drug therapy 43 (72)
Previous transient ischaemic attack or stroke 4 (7)
Cardiac disease 16 (27)
Chronic kidney disease 23 (38)
Pulmonary disease 6 (10)
Values are given as number of participants (%), except *median (range).
†Hyperlipidaemia is defined as a previous documentation of (general practitioner or secondary care) or current
cholesterol of > 5.2 mmol/l.
This article is protected by copyright. All rights reserved.
Table 2 SINBAD ulcer classification of study participants.
No.
SINBAD
participants
Accepted Article
Site 20 (33)
Ischaemia 35 (58)
Neuropathy 51 (85)
Infection 19 (32)
Area 25 (58)
Depth 13 (22)
Total score:
0 3 (5)
1 7 (12)
2 22 (37)
3 8 (13)
4 7 (12)
5 10 (17)
6 3 (5)
Values are number of participants (%) scoring for each criterion.
Score 1 for each of the following: Site, ulcer midfoot/hindfoot; ischemia, evidence of ischemia (neither pulse
palpable with signs of reduced tissue perfusion, with or without gangrene); neuropathy, defined as being present
based on routine examination using 10-G nylon monofilaments; infection (using clinical signs of infection of
either soft tissue or bone proposed by the Infectious Diseases Society of America and the International Working
Group on the Diabetic Foot); area > 1 cm2; depth reaching to tendon, periosteum, joint capsule or bone. For
more details see Ryman et al. [15] and Ince et al. [16].
This article is protected by copyright. All rights reserved.
Table 3 SVS WIfI ulcer classification of study participants. Values are number of participants (percentage).
Accepted Article
SVS WIfI score No.
Wound
0 (No ulcer) 0
1 (Small shallow ulcer) 44 (73)
2 (Deeper ulcer) 8 (13)
3 (Extensive deep ulcer) 8 (13)
Ischaemia
0 (none) 62 (37)
1 (mild) 23 (14)
2 (moderate) 12 (7)
3 (severe) 3 (2)
Infection
0 (no infection) 36 (60)
1 (local but superficial infection) 10 (17)
2 (local infection with erythema > 2cm or involvement of deeper structures) 8 (13)
3 (local infection with systemic inflammatory response) 6 (10)
SVS WIfI, Society of Vascular Surgery Wound Infection Ischaemia.
Ischaemia grading is according to ankle-brachial pressure index, ankle systolic pressure or TcPO2. For
more details see Mills et al. [17].
This article is protected by copyright. All rights reserved.
ccepted Articl
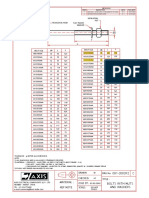
Table 4 Diagnostic utility of physical examination of and screening tests to identify peripheral artery disease compared to Duplex ultrasound scan
Positive predictive Negative predictive Positive likelihood Negative likelihood
Sensitivity Specificity value value ratio ratio
Either pedal pulse 0.55 (0.33–0.77) 0.60 (0.45–0.75) 0.41 (0.22–0.59) 0.73 (0.58–0.88) 1.38 (0.79–2.38) 0.75 (0.43–1.30)
Hair loss 0.8 (0.62–0.98) 0.44 (0.28–0.59) 0.42 (0.26–0.58) 0.81 (0.64–0.98) 1.42 (1.00–2.02) 0.46 (0.18–1.18)
Atrophy 0.5 (0.28–0.72) 0.87 (0.77–0.98) 0.67 (0.43–0.91) 0.77 (0.65–0.90) 3.9 (1.54–9.87) 0.57 (0.36–0.90)
Dependent rubor 0 1 Not discriminatory* 0.66 (0.54–0.78) Not discriminatory* 1
Cool skin 0.3 (0.10–0.50) 0.90 (0.80–0.99) 0.6 (0.30–0.90) 0.71 (0.59–0.84) 2.93 (0.93–9.19) 0.78 (0.57–1.06)
Blue/purple skin 0 0.92 (0.84–1.01) 0 0.64 (0.51–0.76) 0 1.09 (0.99–1.19)
Capillary refill 0.42 (0.20–0.64) 0.63 (0.48–0.78) 0.36 (0.16–0.56) 0.69 (0.53–0.84) 1.14 (0.58–2.24) 0.92 (0.58–1.44)
Venous filling 0 1 Not discriminatory† 0.65 (0.51–0.79) Not discriminatory† 1
Ankle pressure 0.47 (0.25–0.70) 0.79 (0.66–0.92) 0.53 (0.29–0.77) 0.75 (0.62–0.88) 2.25 (1.03–4.90) 0.67 (0.42–1.05)
Toe pressure 0.45 (0.23–0.67) 0.97 (0.92–1.00) 0.90 (0.71–1.00) 0.78 (0.66–0.89) 17.55 (2.39–128.96) 0.56 (0.38–0.84)
Toe brachial pressure index 0.89 (0.76–1.00) 0.45 (0.29–0.61) 0.45 (0.29–061) 0.89 (0.76–1.00) 1.62 (1.17–2.2) 0.24 (0.06–0.91)
Ankle brachial pressure index 0.68 (0.48–0.89) 0.59 (0.44–0.75) 0.46 (0.28–0.65) 0.79 (0.63–0.94) 1.69 (1.03–2.77) 0.53 (0.26–1.08)
Pole test at ankle 0.28 (0.07–0.48) 0.97 (0.92–1.00) 0.83 (0.54–1.00) 0.73 (0.61–0.86) 10.29 (1.29–81.60) 0.74 (0.55–0.99)
TcPO2 0.28 (0.07–0.48) 0.66 (0.51–0.81) 0.28 (0.07–0.48) 0.66 (0.51–0.81) 0.81 (0.34–1.93) 1.10 (0.76–1.58)
Waveform analysis 0.85 (0.69–1.00) 1‡ 1‡ 0.93 (0.85–1.00) Diagnoses PAD‡ 0.15 (0.05–0.43)
Values in parentheses are 95% CI.
*Not discriminatory because dependent rubor was not elicited in any patient.
† Not discriminatory because impairment of venous filling was not elicited in any patient.
‡ The gold standard definition of peripheral arterial disease (PAD) used included monophasic (damped) waveforms in any vessel, therefore the specificity and positive
predictive value ratios are 1 and, positive likelihood is effectively infinite and diagnoses PAD.
This article is protected by copyright. All rights reserved.
You might also like
- Diabetes and Peripheral Vascular Disease: Diagnosis and ManagementFrom EverandDiabetes and Peripheral Vascular Disease: Diagnosis and ManagementNo ratings yet
- Guidelines of The International Writing Group On The Diabetic Foot On DiagnosisDocument12 pagesGuidelines of The International Writing Group On The Diabetic Foot On DiagnosisHan's OfficialNo ratings yet
- Jurnal 2Document8 pagesJurnal 2radiyNo ratings yet
- PeripheralDocument7 pagesPeripheralerdynNo ratings yet
- AnemiaDocument10 pagesAnemiaRamesh VaradharajanNo ratings yet
- Reviewed - IJHSS - Format-Risk of Lower Extremity Peripheral Artery Disease and Presence of Symptoms of Intermittent Claudication Among Diabetic Patients Cross Sectional StudyDocument10 pagesReviewed - IJHSS - Format-Risk of Lower Extremity Peripheral Artery Disease and Presence of Symptoms of Intermittent Claudication Among Diabetic Patients Cross Sectional Studyiaset123No ratings yet
- ASNJ-Volume 9-Issue 24.0 - Page 170-181 PDFDocument12 pagesASNJ-Volume 9-Issue 24.0 - Page 170-181 PDFMayasumita Wijayana05No ratings yet
- Detection, Evaluation, and Management of Preoperative Anaemia in The Elective Orthopaedic Surgical Patient: NATA GuidelinesDocument10 pagesDetection, Evaluation, and Management of Preoperative Anaemia in The Elective Orthopaedic Surgical Patient: NATA GuidelinesDiego Martin RabasedasNo ratings yet
- Ijmrhs Vol 4 Issue 2Document219 pagesIjmrhs Vol 4 Issue 2editorijmrhsNo ratings yet
- Perfusion Assessment and Treatment in the Diabetic PatientDocument10 pagesPerfusion Assessment and Treatment in the Diabetic PatientArthur TeixeiraNo ratings yet
- Diabetes and Ulceration of The Foot 2011Document2 pagesDiabetes and Ulceration of The Foot 2011alex1973maNo ratings yet
- 2017 - Bansal - Corelation of HbA1c Levels and Duration of Diabetes With PADDocument4 pages2017 - Bansal - Corelation of HbA1c Levels and Duration of Diabetes With PADbuat nugas28No ratings yet
- Prospective Study of Routine Heparin Avoidance Hemodialysis in A Tertiary Acute Care Inpatient PracticeDocument10 pagesProspective Study of Routine Heparin Avoidance Hemodialysis in A Tertiary Acute Care Inpatient PracticeAdi SuciptoNo ratings yet
- Case Report Peripheral Arterial Disease Vaskular 2015Document8 pagesCase Report Peripheral Arterial Disease Vaskular 2015NovrizaL SaifulNo ratings yet
- Risk 3Document9 pagesRisk 3Rabiyatul AliuNo ratings yet
- Acute Appendicitis in Patients With End-Stage Renal Disease: Original ArticleDocument7 pagesAcute Appendicitis in Patients With End-Stage Renal Disease: Original ArticleUkh ChyNo ratings yet
- J CPM 2019 02 010Document13 pagesJ CPM 2019 02 010Mohamed GoudaNo ratings yet
- Diabetic Foot Risk Factors in Type 2 Diabetes Patients: A Cross-Sectional Case Control StudyDocument5 pagesDiabetic Foot Risk Factors in Type 2 Diabetes Patients: A Cross-Sectional Case Control Studychintya claraNo ratings yet
- Diabetic Foot Thesis TopicsDocument8 pagesDiabetic Foot Thesis Topicsmonicabogdaneverett100% (2)
- Identificar PAD en Pacientes Con Pie DiabeticoDocument12 pagesIdentificar PAD en Pacientes Con Pie DiabeticoSamuel GarciaNo ratings yet
- Chest: High Prevalence of Undiagnosed Airfl Ow Limitation in Patients With Cardiovascular DiseaseDocument8 pagesChest: High Prevalence of Undiagnosed Airfl Ow Limitation in Patients With Cardiovascular DiseaseRoberto Enrique Valdebenito RuizNo ratings yet
- Ankle 2020 Article 389Document6 pagesAnkle 2020 Article 389Hening yumiNo ratings yet
- Patients With Gout Adhere To Curative Treatment If Informed Appropriately: Proof-Of-Concept Observational StudyDocument5 pagesPatients With Gout Adhere To Curative Treatment If Informed Appropriately: Proof-Of-Concept Observational Studytika_876267153No ratings yet
- Arthroplasty TodayDocument4 pagesArthroplasty TodayCristina SavaNo ratings yet
- Ima 1Document9 pagesIma 1larasatiwibawaniNo ratings yet
- Journal of Clinical & Translational EndocrinologyDocument5 pagesJournal of Clinical & Translational EndocrinologyRicky BooyNo ratings yet
- 1 s2.0 S0168822714003106 MainDocument9 pages1 s2.0 S0168822714003106 Maindawit simionNo ratings yet
- Early TIPS Versus Endoscopic Therapy For Secondary Prophylaxis After Management of Acute Esophageal Variceal Bleeding in Cirrhotic Patients: A Meta-Analysis of Randomized Controlled TrialsDocument26 pagesEarly TIPS Versus Endoscopic Therapy For Secondary Prophylaxis After Management of Acute Esophageal Variceal Bleeding in Cirrhotic Patients: A Meta-Analysis of Randomized Controlled Trialsray liNo ratings yet
- Synopsis 142Document8 pagesSynopsis 142AneesUrRahmanNo ratings yet
- Sex-Related Relationships Between Uric Acid AnDocument8 pagesSex-Related Relationships Between Uric Acid Annguyenthanhluan2801No ratings yet
- Analysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerDocument10 pagesAnalysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerNurul Fitrawati RidwanNo ratings yet
- Korelasi Antara Gambaran Spektral Doppler Arteri Tibialis Posterior Dan Arteri Dorsalis Pedis Dengan Skor PEDIS Pada Penderita Ulkus Kaki DiabetikDocument9 pagesKorelasi Antara Gambaran Spektral Doppler Arteri Tibialis Posterior Dan Arteri Dorsalis Pedis Dengan Skor PEDIS Pada Penderita Ulkus Kaki DiabetikJOHANES BERECHMANS PRANOTO RUMARATUNo ratings yet
- Ulkus2Document11 pagesUlkus2Stefanie SuwitaNo ratings yet
- Scopus Q4Document7 pagesScopus Q4nur alifNo ratings yet
- NIH Public Access: Author ManuscriptDocument16 pagesNIH Public Access: Author Manuscriptgonzalo_acosta_6No ratings yet
- Safe Cholecystectomy Multi-Society Practice Guideline and State of The Art Consensus ConferenceDocument52 pagesSafe Cholecystectomy Multi-Society Practice Guideline and State of The Art Consensus ConferenceChristopher NaherNo ratings yet
- Diabetic Foot Ulcer : Risk Factors Stratification in Patients. A Study of 150 PatientsDocument6 pagesDiabetic Foot Ulcer : Risk Factors Stratification in Patients. A Study of 150 PatientsAnanda WulandariNo ratings yet
- Ijms 20 03805 v2Document21 pagesIjms 20 03805 v2badria bawazirNo ratings yet
- AbiDocument11 pagesAbiMiftahul JannahNo ratings yet
- Jurnal KadekDocument6 pagesJurnal KadekNikadek Ayu Dwi LestariNo ratings yet
- CKD Patients LVM Periodontal StatusDocument12 pagesCKD Patients LVM Periodontal Statusyuna pratiwiNo ratings yet
- Circulation 2012 Vieira S145 50Document7 pagesCirculation 2012 Vieira S145 50pasebanjatiNo ratings yet
- Foot Ulcers in The Diabetic Patient, Prevention and TreatmentDocument12 pagesFoot Ulcers in The Diabetic Patient, Prevention and TreatmentAndriawan BramNo ratings yet
- Stroke 3Document11 pagesStroke 3Amalia Zulfa AmandaNo ratings yet
- 05 - N031 - 38796 ThesisDocument22 pages05 - N031 - 38796 ThesisdrtareksNo ratings yet
- Grip Et Al-2018-British Journal of SurgeryDocument9 pagesGrip Et Al-2018-British Journal of SurgeryIrma SihotangNo ratings yet
- CLTI Guidelines ESVS SVS WFVSDocument142 pagesCLTI Guidelines ESVS SVS WFVSAhmed Elmallah100% (1)
- 1 s2.0 S1051227616301789 MainDocument7 pages1 s2.0 S1051227616301789 MainResearch OfficeNo ratings yet
- Frank 2019Document15 pagesFrank 2019Oliver ArteagaNo ratings yet
- Evaluate of The Physical Performance of Patients Undergoing HemodialysisDocument9 pagesEvaluate of The Physical Performance of Patients Undergoing HemodialysisAhmed AlkhaqaniNo ratings yet
- Atm 08 23 1626Document12 pagesAtm 08 23 1626Susana MalleaNo ratings yet
- Gadjradj2017 - Criterio Cirurgia ColunaDocument23 pagesGadjradj2017 - Criterio Cirurgia ColunaDr Aléssio NovaisNo ratings yet
- Diastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseaseDocument6 pagesDiastolic Function Is A Strong Predictor of Mortality in Patients With Chronic Kidney DiseasehanifahrafaNo ratings yet
- Risk factors for diabetic foot in IndonesiaDocument4 pagesRisk factors for diabetic foot in IndonesiaFernando SilalahiNo ratings yet
- Diabetic Foot Care Education LackingDocument5 pagesDiabetic Foot Care Education LackingSarah EddiahNo ratings yet
- Clinical Outcome of Donors PDFDocument7 pagesClinical Outcome of Donors PDFEngidaNo ratings yet
- The Significance of Neutrophil-Lymphocyte Ratio, Platelet-Lymphocyte Ratio and Lymphocyte Monocyte Ratio Predicting AmputationDocument23 pagesThe Significance of Neutrophil-Lymphocyte Ratio, Platelet-Lymphocyte Ratio and Lymphocyte Monocyte Ratio Predicting AmputationjeovanniNo ratings yet
- Synoptic Reporting of EchocardiographyDocument11 pagesSynoptic Reporting of Echocardiography林昌恩No ratings yet
- The Changes of Trends in The Diagnosis and Treatment of Diabetic Foot Ulcer Over A 10-Year Period: Single Center StudyDocument11 pagesThe Changes of Trends in The Diagnosis and Treatment of Diabetic Foot Ulcer Over A 10-Year Period: Single Center StudyAnonymous UTUWFODCEYNo ratings yet
- 828 FullDocument7 pages828 FullMayra LoeraNo ratings yet
- Dhi-Ehs-Hsm-028 Work Over Water Rev0Document5 pagesDhi-Ehs-Hsm-028 Work Over Water Rev0Phạm Đình NghĩaNo ratings yet
- JBNBNBNBNBNBDocument4 pagesJBNBNBNBNBNBmaheshNo ratings yet
- 18th Century Political Formation. CL 7Document22 pages18th Century Political Formation. CL 7Gamer AditKills100% (1)
- Bangladesh Premier League 2024 Schedule, Live Scores and ResultsDocument5 pagesBangladesh Premier League 2024 Schedule, Live Scores and Resultsmoslahuddin2022No ratings yet
- Combined SGMA 591Document46 pagesCombined SGMA 591Steve BallerNo ratings yet
- Davall Stock Gears Worm Wheel Gear Sets 17pages PDFDocument17 pagesDavall Stock Gears Worm Wheel Gear Sets 17pages PDFharish ahireNo ratings yet
- EN - Ultrasonic Sensor Spec SheetDocument1 pageEN - Ultrasonic Sensor Spec Sheettito_matrixNo ratings yet
- IVECO NEF SeriesDocument36 pagesIVECO NEF SeriesOlivier ORMANNo ratings yet
- Agni Free PDF - 2 For Sbi Clerk Mains 2024Document18 pagesAgni Free PDF - 2 For Sbi Clerk Mains 2024supriyo248650No ratings yet
- 452-Chapter 15 PDFDocument14 pages452-Chapter 15 PDFYoan Barriga BerriosNo ratings yet
- WheelHorse Power Take Off Manual 8-3411Document4 pagesWheelHorse Power Take Off Manual 8-3411Kevins Small Engine and Tractor ServiceNo ratings yet
- Live Sound 101: Choosing Speakers and Setting Up a Sound SystemDocument14 pagesLive Sound 101: Choosing Speakers and Setting Up a Sound Systemohundper100% (1)
- Carpenter Company MarketingDocument14 pagesCarpenter Company Marketingsladex17No ratings yet
- Fin4010 Assignment 3Document3 pagesFin4010 Assignment 3Grace AtteNo ratings yet
- Comments PRAG FinalDocument13 pagesComments PRAG FinalcristiancaluianNo ratings yet
- BTP Presentation - Sem 8Document24 pagesBTP Presentation - Sem 8Nihal MohammedNo ratings yet
- C Programming JNTU PDFDocument171 pagesC Programming JNTU PDFfakeNo ratings yet
- Compound Sentences FANBOYS WorksheetDocument7 pagesCompound Sentences FANBOYS WorksheetVerenice SuarezNo ratings yet
- Material: Ref Note: Rev # Description Appv. Rev DateDocument1 pageMaterial: Ref Note: Rev # Description Appv. Rev DateNimish TaterhNo ratings yet
- Cash Flow Statement and Balance Sheet of A Solar Power Plant in APDocument35 pagesCash Flow Statement and Balance Sheet of A Solar Power Plant in APSriharsha Vavilala100% (1)
- The Difficult Patient' As Perceived by Family Physicians: Dov Steinmetz and Hava TabenkinDocument6 pagesThe Difficult Patient' As Perceived by Family Physicians: Dov Steinmetz and Hava TabenkinRomulo Vincent PerezNo ratings yet
- Nasrullah March23Document11 pagesNasrullah March23Angellin JoiceNo ratings yet
- SolidWorks Motion Tutorial 2010Document31 pagesSolidWorks Motion Tutorial 2010Hector Adan Lopez GarciaNo ratings yet
- Document - University Admission SystemDocument100 pagesDocument - University Admission SystemNaresh SharmaNo ratings yet
- Index NumbersDocument23 pagesIndex NumbersemmaNo ratings yet
- Microprocessor 8086 Memory and ArchitectureDocument13 pagesMicroprocessor 8086 Memory and ArchitecturehrrameshhrNo ratings yet
- Safety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingDocument8 pagesSafety Data Sheet: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingFerry Dela RochaNo ratings yet
- Questionnaire For ThesisDocument5 pagesQuestionnaire For ThesisRamiz HassanNo ratings yet
- Nevada Reports 1882-1883 (17 Nev.) PDFDocument334 pagesNevada Reports 1882-1883 (17 Nev.) PDFthadzigsNo ratings yet
- EIE Resume FormatDocument1 pageEIE Resume FormatRakesh MandalNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)