Professional Documents
Culture Documents
Corynebacterium diphtheriae: Pathogen Causing Diphtheria
Uploaded by
Xing Yu0 ratings0% found this document useful (0 votes)
9 views20 pagesOriginal Title
Untitled
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views20 pagesCorynebacterium diphtheriae: Pathogen Causing Diphtheria
Uploaded by
Xing YuCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 20
Corynebacterium diphteriae
3 RD YEAR PHARMACY, SEMESTER 2, 2021
DR. HENG KANIKA,PHARMD
Learning objectives
At the end of this session students should be able to:
➢ Describe morphology of Corynebacterium diphteriae
➢ Describe epidemiology of Corynebacterium diphteriae
➢ Explain the pathogenesis of Corynebacterium diphteriae
➢ Cite the clinical signs and symptoms given by Corynebacterium diphteriae
➢ Describe the diagnostic methods to identify bacteria
➢ Describe Prevention and treatment of Diphteria
Content
◦ Introduction
◦ Epidemiology
◦ Pathogenesis
◦ Clinical signs and Symptoms
◦ Diagnosis
◦ Treatment and Prevention
Introduction
Pathogenic bacterium that causes diphtheria. It is also known as the Klebs-
Löffler bacillus, because it was discovered in 1884 by
German bacteriologists Edwin Klebs (1834–1912) and cultivated by Friedrich
Löffler (1852–1915).
Four subspecies are recognized:
Corynebacterium diphteriae mitis,
Corynebacterium diphteriae intermedius,
Corynebacterium diphteriae gravis,
Corynebacterium diphteriae belfanti
Introduction
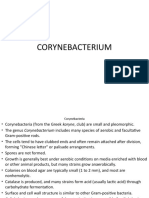
• Gram-positive pleomorphic rods
•Thick peptidoglycane cell wall
• Club shaped due to the presence of metachromatic (volutin) granules at one or
both ends.
• Chinese letter or cuneiform arrangement
•Non motile
• Aerobic bacteria
• Non spore forming Stained Corynebacterium cells. The "barred"
appearance is due to the presence of
polyphosphate inclusions called metachromatic
granules. Note also the characteristic "Chinese-
letter" arrangement of cells.
Introduction
Fastidious organisms; grows best at 37 °C on blood or serum-containing media
such as Loeffler’s medium, tellurite medium, etc
The major virulence factor is the diphtheria toxin, an A-B exotoxin; inhibits
protein synthesis
Etiologic agent of diphtheria: respiratory and cutaneous forms
Epidemiology
Worldwide distribution maintained in asymptomatic carriers and infected
patients
Humans are the only known reservoir, with carriage in oropharynx or on skin
surface
Spread person to person by exposure to respiratory droplets or skin contact
Disease observed in unvaccinated or partially immune children or adults
traveling to countries with endemic disease
Diphtheria is very uncommon in the United States and other countries with
active vaccination programs
Epidemiology
Risk factors for the spread of diphtheria include:
• Overcrowded areas
• Poor hygiene
• Lack of immunisation
Pathogenesis
Diphtherial infections are mainly because of the toxin.
The virulence of Diphtheria bacilli is due to capacity to
◦ Establish infection and grow rapidly
◦ Quickly elaborate an exotoxin
Diphtheria toxin is an exotoxin secreted by C. diphtheria. Diphtheria
toxin is a single polypeptide chain of 535 amino acids consisting of
two subunits linked by disulfide bridges, known as an A-B toxin.
Pathogenesis
There are at least four main steps involved in intoxication of a single eukaryotic
cell by diphtheria toxin:
(1) the binding of the toxin to surface receptor of its target cell;
(2) grouping of charged receptors into layered pits and internalization of the
toxin by receptor-mediated endocytosis; followed by acidification of the
endocytic vesicle by a membrane-associated, ATP-driven proton pump,
(3) Insertion of the transmembrane domain (B-subunit) into the membrane and
smoothed the delivery of catalytic domain (A-subunit) to the cytosol,
(4) the ADP-ribosylation of elongation factor 2 (EF-2), which results in the
permanent inhibition of protein synthesis. A single molecule of the catalytic
domain delivered to the cytosol is enough to be deadly for the cell.
Pathogenesis
Pathogenesis
C. diphtheriae occurs in the respiratory tract, in wounds, or on the skin of
infected persons or normal carriers. It is spread by droplets or by direct contact.
Portal of entry: respiratory tract or skin abrasions. Diphtheria bacilli colonize and
grow on mucous membranes, and start to produce toxin, which is then absorbed
into the mucous membranes, and even spread by the bloodstream.
Local toxigenic effects: elicit inflammatory response and necrosis of the facial
mucosa cells-- formation of "pseudo-membrane“ (composed of bacteria,
lymphocytes, plasma cells, fibrin, and dead cells), causing respiratory
obstruction.
Systemic toxigenic effects: necrosis in heart muscle, liver, kidneys and adrenals.
Also produces neural damage.
Clinical signs and Symptoms
Diagnosis
Sample: Swabs (preferably two) from the lesion of throat, larynx or nasal cavity; one
for direct examination and another for culture or a portion of the pseudomembrane.
Direct examination
•Smears of the throat swab should be stained with both Gram stain and methylene
blue or Albert stain.
. Culture
• Loeffler’s medium:
best morphology
Diagnosis
Blood tellurite agar: It is a selective and differential medium
for C. diphtheriae.After 48-72 hours, colonies of C. diphtheria
appear as small, grey, or black with a raised center.
Tinsdale’s Agar: After incubation for at least 48 hours, colonies
of Corynebacterium diphtheriae appear black with dark brown halos
Rapid identification methods
API Coryne strip and RapID CB Plus are commercial products available for the rapid identification
of Corynebacterium diphtheriae.
Diagnosis
Toxigenicity testing
• Elek immunodiffusion test: It is the most common in vitro assay for determining toxigenicity of C.
diphtheriae. This test is based on the double diffusion of diphtheria toxin and antitoxin in an agar
medium. A sterile, antitoxin-saturated filter paper strip is embedded in the culture medium, and C
diphtheriae isolates are streak-inoculated at a 90° angle to the filter paper. The production of
diphtheria toxin can be detected within 18 to 48 hours by the formation of a toxin-antitoxin precipitin
band in the agar.
Diagnosis
• Detection of toxin gene by polymerase chain reaction (PCR).
• In vivo test: inject the culture into antitoxin-protected and unprotected guinea pigs
subcutaneously.
Treatment
Penicillin
Erythromycin
Anti toxin from horse serum to stop the toxin made by the bacteria from damaging the
body. This treatment is very important for respiratory diphtheria infections, but it is rarely used
for diphtheria skin infections.
Prevention
Diphtheria vaccine is a bacterial toxoid, a toxin whose toxicity has been
inactivated.
The vaccine is normally given in combination with other vaccines as DTwP/DTaP
vaccine or pentavalent vaccine. For adolescents and adults the diphtheria toxoid
is frequently combined with tetanus toxoid in lower concentration (Td vaccine).
CDC is recommended that children receive 5 doses of DTaP, usually at the
following ages:
◦ 2 months
◦ 4 months
◦ 6 months
◦ 15–18 months
◦ 4–6 years
References
◦ P.Murray-Medical Microbiology ,7th edition,2012
◦ Diphteria - CDC Fact Sheet (Detailed)
◦ www.osmosis.org/learn/Corynebacterium diphtheria
◦ https://www.who.int/immunization/diseases/diphtheria/en/
You might also like
- Organism ID & Types of ShockDocument5 pagesOrganism ID & Types of ShockAdrian BrillantesNo ratings yet
- AUBF - Chapter 1Document7 pagesAUBF - Chapter 1Kristin SoquilloNo ratings yet
- Gram Positive Bacilli: Corynebacterium Diphtheriae and Bacillus anthracisDocument28 pagesGram Positive Bacilli: Corynebacterium Diphtheriae and Bacillus anthracisMustafa SaßerNo ratings yet
- Corynebacterium DiphtheriaeDocument27 pagesCorynebacterium DiphtheriaeBarkavi 9620No ratings yet
- Cory Ne BacteriumDocument25 pagesCory Ne BacteriumjmalavanuNo ratings yet
- Non Spore Forming G+ Bacilli I - Seni-1Document20 pagesNon Spore Forming G+ Bacilli I - Seni-1alicerugaibula123No ratings yet
- Diphteria, ListeriaDocument20 pagesDiphteria, ListeriaLore LorenaNo ratings yet
- DIPTHERIADocument3 pagesDIPTHERIARed Angela DinsonNo ratings yet
- Cory Ne BacteriumDocument25 pagesCory Ne BacteriumSona SandiNo ratings yet
- MICROBIOLOGY Pathogenic Gram-Positive Bacilli (Corynebacterium)Document7 pagesMICROBIOLOGY Pathogenic Gram-Positive Bacilli (Corynebacterium)Ravindra SinghNo ratings yet
- Corynebacterium Diphtheriae: A Paradigm of The Toxigenic Infectious DiseasesDocument20 pagesCorynebacterium Diphtheriae: A Paradigm of The Toxigenic Infectious DiseasesRahma FatmawatiNo ratings yet
- CorynebacteriumDocument20 pagesCorynebacteriumMohammed JaferNo ratings yet
- Case Study: Pathogenic Bacteriology 2009Document16 pagesCase Study: Pathogenic Bacteriology 2009Porombita PorumbelNo ratings yet
- Aerobes Chapter 12Document6 pagesAerobes Chapter 12Kristine BoholstNo ratings yet
- Clinical Manifestations of DiphtheriaDocument7 pagesClinical Manifestations of DiphtheriaRuturaj JadejaNo ratings yet
- CORYNEBACTERIUMDocument22 pagesCORYNEBACTERIUMHamidreza RahmaniNo ratings yet
- Corynebacterium DiphtheriaDocument39 pagesCorynebacterium DiphtheriaSubhada GosaviNo ratings yet
- (24a) Respiratory Infecitons and MeningitisDocument48 pages(24a) Respiratory Infecitons and MeningitisFarrah BenoitNo ratings yet
- DiphteriaDocument24 pagesDiphteriasalmaNo ratings yet
- GRAM POSITIVE RODSCroyneDocument22 pagesGRAM POSITIVE RODSCroynejoseadreannes.pinedaNo ratings yet
- Corynebacterium Diphtheria: Zainab A. AldhaherDocument41 pagesCorynebacterium Diphtheria: Zainab A. Aldhaherمروه عماد عيسىNo ratings yet
- K10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Document42 pagesK10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Juanto Tio VocNo ratings yet
- Mikrobiologi Parasitologi Respiration: AN IMO 2019Document64 pagesMikrobiologi Parasitologi Respiration: AN IMO 2019Sleeping BeautyNo ratings yet
- NeisseriaDocument32 pagesNeisseriaKeshant SamarooNo ratings yet
- ChlamydiaDocument22 pagesChlamydiadelia rahmaNo ratings yet
- B.Sc. DEGREE (CBCS) EXAMINATION NOW 2020Document5 pagesB.Sc. DEGREE (CBCS) EXAMINATION NOW 2020Jíīhìn JøHhnNo ratings yet
- CHAPTER IV Pathogenic Gram Negative CocciDocument23 pagesCHAPTER IV Pathogenic Gram Negative Cocciyosef awokeNo ratings yet
- Parvobacteria: Dr. Shehab Ahmed LafiDocument61 pagesParvobacteria: Dr. Shehab Ahmed Lafiقدامه زين العابدين حسان عثمانNo ratings yet
- My Co BacteriaDocument20 pagesMy Co BacteriaAnzo SimonNo ratings yet
- Pathogenic Gram Negative CocciiDocument31 pagesPathogenic Gram Negative Cocciitemesgensemahegn55No ratings yet
- Microbiology Lab Guide Brawijaya University ENT DiseasesDocument32 pagesMicrobiology Lab Guide Brawijaya University ENT DiseasesfhfebriiNo ratings yet
- Cory Ne BacteriumDocument28 pagesCory Ne BacteriumDayana PrasanthNo ratings yet
- All 45 BugsDocument26 pagesAll 45 Bugsroboat96No ratings yet
- Diphtheria - AMBOSSDocument8 pagesDiphtheria - AMBOSSSadikNo ratings yet
- Diptheria Nursing ManagementDocument14 pagesDiptheria Nursing ManagementMey MeyNo ratings yet
- Crypto Cocco SisDocument32 pagesCrypto Cocco SisLincy JohnyNo ratings yet
- Diphtheria Disease Caused By CorynebacteriumDocument12 pagesDiphtheria Disease Caused By CorynebacteriumNununNo ratings yet
- Infectious DiseasesDocument22 pagesInfectious DiseasesAbiNo ratings yet
- ReckitsiaDocument17 pagesReckitsiaAlhassn NasserNo ratings yet
- 8 Corynebacterium DiphtheriaeDocument5 pages8 Corynebacterium DiphtheriaeRami Moneem Oda SolaibiNo ratings yet
- I. Corynebacterium: Non-Spore Forming Gram Positive BacilliDocument6 pagesI. Corynebacterium: Non-Spore Forming Gram Positive BacilliTob MoradosNo ratings yet
- Tuberculosis: Therapeutics IIDocument54 pagesTuberculosis: Therapeutics IIdstu20No ratings yet
- DiphtheriaDocument25 pagesDiphtheriaRohan TejaNo ratings yet
- Lecture7 Medical Mycology - YeastsDocument32 pagesLecture7 Medical Mycology - YeastsKarthick AnbuNo ratings yet
- Non Spore Forming, Nonbranching Catalase Positive BacilliDocument5 pagesNon Spore Forming, Nonbranching Catalase Positive BacilliFaithNo ratings yet
- Respiratory and Nosocomial InfectionsDocument70 pagesRespiratory and Nosocomial InfectionsCezar Alexander GuevaraNo ratings yet
- Gram Positive Rod of Medical Imortance IIDocument36 pagesGram Positive Rod of Medical Imortance IIJoeyNo ratings yet
- Aerobic Non-Spore Forming Gram-Positive BacilliDocument31 pagesAerobic Non-Spore Forming Gram-Positive BacilliCagar Irwin TaufanNo ratings yet
- CorynebacteriumDocument43 pagesCorynebacteriumIsak Isak Isak0% (1)
- Diphtheria Presentation[1]Document12 pagesDiphtheria Presentation[1]Rwapembe StephenNo ratings yet
- Candidiasis CryptococcosisDocument44 pagesCandidiasis CryptococcosisthaeonlooreNo ratings yet
- Dm-Lecture 4-11-23Document28 pagesDm-Lecture 4-11-23s.zainabtanweerNo ratings yet
- Corynebacterium Diphtheriae Pathogenic BacteriaDocument3 pagesCorynebacterium Diphtheriae Pathogenic BacteriaknedhNo ratings yet
- DipDocument12 pagesDipmentira11No ratings yet
- Cryptococcosis: Dr.C.Meenakshisundaram.Document16 pagesCryptococcosis: Dr.C.Meenakshisundaram.Meenakshisundaram CNo ratings yet
- Corynebacteria diphtheriae_JawetzDocument5 pagesCorynebacteria diphtheriae_JawetzHUỲNH QUỐC KHÁNHNo ratings yet
- 5 CorynebacteriumDocument41 pages5 Corynebacterium01. Akhmad Gilang R - XII MIPA 4No ratings yet
- CALDERON Bacteriology Worksheet With AnswersDocument3 pagesCALDERON Bacteriology Worksheet With AnswersJames Belgira TamayoNo ratings yet
- BACTE Aerobic Non Spore FormersDocument4 pagesBACTE Aerobic Non Spore FormersVera June RañesesNo ratings yet
- Diphteria, Leprae, Tetanus, Typhoid, Leptospirosis, MeningitisDocument57 pagesDiphteria, Leprae, Tetanus, Typhoid, Leptospirosis, MeningitisNur OctavianiNo ratings yet
- Protist PacketDocument3 pagesProtist Packetcrying catNo ratings yet
- Endo Perio RelationsDocument28 pagesEndo Perio RelationsMunish BatraNo ratings yet
- Haemagglutination, This: Treponema Pallidum Hemagglutination Assay (TPHA) Is A Treponemal TestDocument3 pagesHaemagglutination, This: Treponema Pallidum Hemagglutination Assay (TPHA) Is A Treponemal TestPrativa RajbhandariNo ratings yet
- Urn Uvci 01 Ro M4q6dre9p31zg8ekv5zv705oygk8w2bDocument2 pagesUrn Uvci 01 Ro M4q6dre9p31zg8ekv5zv705oygk8w2bReni FerencziNo ratings yet
- Health Number Code GrabovoiDocument12 pagesHealth Number Code Grabovoimysticsoul100% (2)
- Sample Exam With AnswersDocument4 pagesSample Exam With Answerslimenghan.evaNo ratings yet
- Antimicrobial Screen - Dub DiolDocument4 pagesAntimicrobial Screen - Dub DiolNgân BảoNo ratings yet
- Name: Zata Haura Al'adani School: Daarut Tauhid Boarding School Putri Bandung (DTBS Putri)Document4 pagesName: Zata Haura Al'adani School: Daarut Tauhid Boarding School Putri Bandung (DTBS Putri)compare motoNo ratings yet
- PubmedDocument5 pagesPubmedapi-521437627No ratings yet
- Hannoun 2013Document10 pagesHannoun 2013bilou hertNo ratings yet
- List of Different Phobias2Document3 pagesList of Different Phobias2Deborah ChristineNo ratings yet
- Communicable Diseases EpidemiologyDocument44 pagesCommunicable Diseases EpidemiologyIrum QureshiNo ratings yet
- Chemistry Project Final 1Document12 pagesChemistry Project Final 1mokey420opNo ratings yet
- Hand Hygiene IdaDocument7 pagesHand Hygiene IdaOem Boed ColectionNo ratings yet
- MRSADocument6 pagesMRSAKimberly Clarisse VegaNo ratings yet
- National Immunization Schedule (NIS) : For Infants, Children and Pregnant WomenDocument13 pagesNational Immunization Schedule (NIS) : For Infants, Children and Pregnant WomenPrabir Kumar Chatterjee100% (1)
- Tropical: MedicineDocument27 pagesTropical: MedicineDwi Esthi PutriNo ratings yet
- Checklist For CLABSIDocument1 pageChecklist For CLABSIRicardo Balau100% (1)
- UrinDocument2 pagesUrinaniaNo ratings yet
- Ayurvedic Herb Giloy Benefits Immunity LiverDocument1 pageAyurvedic Herb Giloy Benefits Immunity LiverGorav Bhalla0% (1)
- CephalexinDocument4 pagesCephalexinCHIEF DOCTOR MUTHUNo ratings yet
- Long Essay On World Health Day in EnglishDocument2 pagesLong Essay On World Health Day in EnglishHii Ing ChungNo ratings yet
- The Plague Free Summary by Albert CamusDocument15 pagesThe Plague Free Summary by Albert CamusNoriees Noriees100% (1)
- Nursing Care Plan Related Learning Experience: Lorma Colleges Con TemplateDocument2 pagesNursing Care Plan Related Learning Experience: Lorma Colleges Con TemplateKrizzia Mae ColladoNo ratings yet
- CLINICAL PLACEMENT PERMIT CHECKLIST Brock UniversityDocument2 pagesCLINICAL PLACEMENT PERMIT CHECKLIST Brock UniversityroldinpgNo ratings yet
- Ch1 Kitabcd Class 8 MSBHSE Science NotesDocument8 pagesCh1 Kitabcd Class 8 MSBHSE Science NotesONE CLICK COMPUTERNo ratings yet
- The Association Between Migrant Worker, Schools, and Shopping Malls Factors in Thailand's Metropolitan Provinces and The Newest Covid-19 EpidemicDocument6 pagesThe Association Between Migrant Worker, Schools, and Shopping Malls Factors in Thailand's Metropolitan Provinces and The Newest Covid-19 EpidemicInternational Journal of Innovative Science and Research Technology100% (1)












































![Diphtheria Presentation[1]](https://imgv2-1-f.scribdassets.com/img/document/724997802/149x198/a793dc3a96/1713636751?v=1)