Professional Documents
Culture Documents
Chapter 4 Ver. 2
Uploaded by
Ruel Mateo0 ratings0% found this document useful (0 votes)
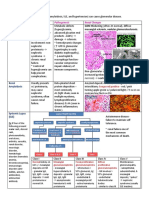
6 views2 pagesThis document summarizes hemodynamic disorders including edema, congestion, shock, hemorrhage, and thromboembolism. It discusses the pathophysiology of increased hydrostatic pressure, reduced plasma osmotic pressure, sodium retention, inflammation, and lymphatic obstruction which can cause edema. Thrombosis and embolism are described along with primary and secondary hypercoagulable states. Consequences of venous thrombosis, arterial thrombosis, and disseminated intravascular coagulation are outlined. The document also covers types of shock including cardiogenic, hypovolemic, and septic shock.
Original Description:
Original Title
Chapter 4 ver. 2.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes hemodynamic disorders including edema, congestion, shock, hemorrhage, and thromboembolism. It discusses the pathophysiology of increased hydrostatic pressure, reduced plasma osmotic pressure, sodium retention, inflammation, and lymphatic obstruction which can cause edema. Thrombosis and embolism are described along with primary and secondary hypercoagulable states. Consequences of venous thrombosis, arterial thrombosis, and disseminated intravascular coagulation are outlined. The document also covers types of shock including cardiogenic, hypovolemic, and septic shock.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views2 pagesChapter 4 Ver. 2
Uploaded by
Ruel MateoThis document summarizes hemodynamic disorders including edema, congestion, shock, hemorrhage, and thromboembolism. It discusses the pathophysiology of increased hydrostatic pressure, reduced plasma osmotic pressure, sodium retention, inflammation, and lymphatic obstruction which can cause edema. Thrombosis and embolism are described along with primary and secondary hypercoagulable states. Consequences of venous thrombosis, arterial thrombosis, and disseminated intravascular coagulation are outlined. The document also covers types of shock including cardiogenic, hypovolemic, and septic shock.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
CHAPTER 4: HEMODYNAMIC DISORDERS, * Ecchymoses
THROMBOEMBOLIC DISEASE AND SHOCK HEMODYNAMIC * hemothorax,hemopericardium, hemoperitoneum, or
DISORDERS hemarthrosis
-Edema
-Congestion HEMOSTASIS AND THROMBOSIS
-Shock * Antithrombotic Properties
EDEMA * Antiplatelet effects
Pathophysiologic Categories of Edema * Anticoagulant effects
- INCREASED HYDROSTATIC PRESSURE * Fibrinolytic effects
* Impaired venous return
* Congestive heart failure
* Constrictive pericarditis * Prothrombotic Properties
* Ascites (liver cirrhosis) * Platelet effects
* Venous obstruction or compression * Procoagulant effects
* Thrombosis * Antifibrinolytic effects
* External pressure (e.g., mass)
* Lower extremity inactivity with prolonged dependency PLATELET ADHESION AND AGGREGATION
* Arteriolar dilation PLATELETS THROMBOSIS
* Heat THROMBOSIS
* Neurohumoral dysregulation * Endothelial injury
- REDUCED PLASMA OSMOTIC PRESSURE * Alterations in Normal Blood Flow
(HYPOPROTEINEMIA) * Stasis and Turbulence
* Protein-losing glomerulopathies (nephrotic syndrome) * Promote endothelial activation
* Liver cirrhosis (ascites) * Disrupt laminar flow and bring platelets into contact with
* Malnutrition the endothelium[26]
* Protein-losing gastroenteropathy EDEMA * Prevent washout and dilution of activated clotting factors
- LYMPHATIC OBSTRUCTION by fresh flowing blood and the inflow of clotting factor
* Inflammatory inhibitors
* Neoplastic * Hypercoagulability
* Postsurgical HYPERCOAGULABLE STATES
* Postirradiation PRIMARY (GENETIC)
- SODIUM RETENTION * Common
* Excessive salt intake with renal insufficiency * Factor V mutation (G1691A mutation; factor V Leiden)
* Increased tubular reabsorption of sodium * Prothrombin mutation (G20210A variant)
* Renal hypoperfusion * 5,10-Methylenetetrahydrofolate reductase (homozygous
* Increased renin-angiotensin-aldosterone secretion C677T mutation)
- INFLAMMATION * Increased levels of factors VIII, IX, XI, or fibrinogen
* Acute inflammation * Rare
* Chronic inflammation * Antithrombin III deficiency
* Angiogenesis * Protein C deficiency
* Protein S deficiency
* Very Rare
EDEMA * Fibrinolysis defects
* Increased hydrostatic pressure * Homozygous homocystinuria (deficiency of cystathione β-
* Congestive heart failure synthetase)
* Deep venous thrombosis SECONDARY (ACQUIRED)
* Reduced Plasma Osmotic Pressure * High Risk for Thrombosis
* Nephrotic syndrome * Prolonged bedrest or immobilization
* Sodium and Water Retention * Myocardial infarction
* Lymphatic Obstruction * Atrial fibrillation
* Tissue injury (surgery, fracture, burn)
Morphologically: * Cancer
* clearing and separation of the extracellular matrix and * Prosthetic cardiac valves
subtle cell swelling * Disseminated intravascular coagulation
* Subcutaneous edema * Heparin-induced thrombocytopenia
* Dependent Edema * Antiphospholipid antibody syndrome
* Pitting Edema * Lower Risk for Thrombosis
* Periorbital Edema * Cardiomyopathy
* Pulmonary Edema * Nephrotic syndrome
* Brain Edema * Hyperestrogenic states (pregnancy and postpartum)
* Oral contraceptive use
* Sickle cell anemia
HYPEREMIA AND CONGESTION * Smoking
Hyperemia
* Active process; arteriolar dilation leads to increase blood Fate of the Thrombus
flow * Propagation
Congestion * Embolization
* passive process resulting from reduced outflow of blood * Dissolution
from a tissue * Organization and recanalization
HEMORRHAGE
* extravasation of blood into the extravascular space Clinical Consequences
* Hypovolemic shock * Venous Thrombosis (Phlebothrombosis)
COMPLICATIONS: * Arterial and Cardiac Thrombosis
* Hematoma * Atherosclerosis
* Petechiae
* Purpura
DISSEMINATED INTRAVASCULAR COAGULATION (DIC) Kidney Infarct
EMBOLISM Factors That Influence Development of an Infarct
* detached intravascular solid, liquid, or gaseous mass that is * the nature of the vascular supply
carried by the blood to a site distant from its point of origin * the rate at which an occlusion develops
* dislodged thrombus * vulnerability to hypoxia
* the oxygen content of the blood
PULMONARY EMBOLISM
* Sudden death, right heart failure (cor pulmonale), or SHOCK
cardiovascular collapse * final common pathway for several potentially lethal clinical
* Embolic obstruction of medium-sized arteries with events, including severe hemorrhage, extensive trauma or
subsequent vascular rupture burns, large myocardial infarction, massive pulmonary
* Embolic obstruction of small end-arteriolar pulmonary embolism, and microbial sepsis
branches * systemic hypotension due either to reduced cardiac output
* Multiple emboli or to reduced effective circulating blood volume
CONSEQUENCES OF SHOCK
SYSTEMIC THROMBOEMBOLISM * impaired tissue perfusion and cellular hypoxia
* emboli in the arterial circulation * prolonged shock eventually leads to irreversible tissue
* intracardiac mural thrombi injury that often proves fatal.
* Left ventricular wall infarcts
* left atrial dilation and fibrillation Three general categories
* aortic aneurysms, Cardiogenic shock
* thrombi on ulcerated atherosclerotic plaques, or * results from low cardiac output due to myocardial pump
fragmentation of a valvular vegetation failure
Hypovolemic shock
* results from low cardiac output due to the loss of blood or
plasma volume
Septic shock
SYSTEMIC THROMBOEMBOLISM * results from vasodilation and peripheral pooling of blood
* Major sites for arteriolar embolization:
* Lower extremities CARDIOGENIC SHOCK
* the brain * Myocardial infarction
* with the intestines, kidneys, spleen, and upper extremities * Ventricular rupture
* Arrhythmia
FAT AND MARROW EMBOLISM AIR EMBOLISM * Cardiac tamponade
* decompression sickness * Pulmonary embolism
* occurs when individuals experience sudden decreases in
atmospheric pressure HYPOVOLEMIC SHOCK
* the bends * Fluid loss (e.g., hemorrhage,
* Chokes * Vomiting
* caisson disease * diarrhea
* burns
AMNIOTIC FLUID EMBOLISM * trauma
* sudden severe dyspnea,
* cyanosis, and shock SEPTIC SHOCK
* neurologic impairment ranging from headache to seizures * Overwhelming microbial infections (bacterial and fungal)
and coma * Superantigens (toxic shock syndrome)
* infusion of amniotic fluid or fetal tissue into the maternal
circulation via a tear in the placental membranes or rupture PATHOGENESIS OF SEPTIC SHOCK
of uterine veins * severe hemodynamic and hemostatic derangements
* systemic vasodilation and pooling of blood in the periphery
Infarction leads to tissue hypoperfusion
* an area of ischemic necrosis caused by occlusion of either * accompanied by widespread endothelial cell activation and
the arterial supply or the venous drainage injury, often leading to a hypercoagulablestate
Pulmonary infarction -ischemic necrosis of the extremities SEPTIC SHOCK
(gangrene) * Inflammatory mediators
* local vasospasm, hemorrhage into an atheromatous plaque, * Endothelial cell activation and injury
or extrinsic vessel compression * Metabolic abnormalities
* include torsion of a vessel traumatic rupture, or vascular * Immune suppression
compromise by edema or by entrapment in a hernia sac * Organ dysfunction
Morphology of Infarct STAGES OF SHOCK
Red infarct * Initial nonprogressive phase
* venous occlusions ( ovary) * Progressive stage
* in loose tissues (lung) * Irreversible stage
* blood can collect in the infarcted zone
* in tissues with dual circulations (lung and small intestine) Clinical Consequences of Shock
* in tissues previously congested by sluggish venous outflow Hypovolemic and Cardiogenic shock
* when flow is re-established to a site of previous arterial * hypotension; a weak, rapid pulse; tachypnea; and cool,
occlusion and necrosis (following angioplasty of an arterial clammy, cyanotic skin
obstruction) Septic shock
* the skin may initially be warm and flushed because of
White infarct peripheral vasodilation
* occur with arterial occlusions in solid organs with end-
arterial circulation
* heart, spleen, and kidney
You might also like
- PE, Tamponade, Constrictive PericarditisDocument1 pagePE, Tamponade, Constrictive PericarditisKaylee HvezdaNo ratings yet
- Week 7. Renal Pathology Continued.Document9 pagesWeek 7. Renal Pathology Continued.Amber LeJeuneNo ratings yet
- Endocrinology Notes for Medical StudentsFrom EverandEndocrinology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (1)
- CH3 Patho D&R AgamDocument30 pagesCH3 Patho D&R AgamS Balagopal SivaprakasamNo ratings yet
- Lecture On Hemodynamic and Thromboembolic DisordersDocument77 pagesLecture On Hemodynamic and Thromboembolic DisordersCharmaine Torio PastorNo ratings yet
- Pathophysiology of StrokeDocument2 pagesPathophysiology of StrokeJoy Rachelle Fermin100% (2)
- Week 10 - Hypertension, Atherosclerosis, ArrhythmiaDocument14 pagesWeek 10 - Hypertension, Atherosclerosis, Arrhythmiashivani patel100% (1)
- Materi 12 IMELS - Trombosis Emboli Paru, Iskemik Tungkai Akut - KritisDocument64 pagesMateri 12 IMELS - Trombosis Emboli Paru, Iskemik Tungkai Akut - KritismaharyadyNo ratings yet
- Thrombosis - NewDocument108 pagesThrombosis - NewheruNo ratings yet
- CardiomyopathyDocument89 pagesCardiomyopathyahmad aminNo ratings yet
- Haemodynamic DisordersDocument74 pagesHaemodynamic Disordersakoeljames8543No ratings yet
- Gangguan Hemodinamik, Trombosis Dan Syok: Fk-Uncen JayapuraDocument67 pagesGangguan Hemodinamik, Trombosis Dan Syok: Fk-Uncen Jayapuramarsal25No ratings yet
- Hemo Dynamic Disorders Thrombo Embolism and ShockDocument29 pagesHemo Dynamic Disorders Thrombo Embolism and ShockMai ÜüNo ratings yet
- Cva IschemicDocument53 pagesCva IschemicJuliatikaNo ratings yet
- Platelet Disorders:: Marshell Tendean, MD Department of Internal Medicine UKRIDA Jakarta 2016Document27 pagesPlatelet Disorders:: Marshell Tendean, MD Department of Internal Medicine UKRIDA Jakarta 2016charlesy TNo ratings yet
- 4 Circulation Disorders PDFDocument69 pages4 Circulation Disorders PDFSetiawan SukmadjaNo ratings yet
- Therapy 2019Document100 pagesTherapy 2019mndpkasaudhanNo ratings yet
- Learning Objectives in Cardiovascular DiseaseDocument13 pagesLearning Objectives in Cardiovascular DiseaseZul Azim AnuarNo ratings yet
- Oedema, Hemorrhages and ThrombosisDocument72 pagesOedema, Hemorrhages and ThrombosisTheBoss 20No ratings yet
- Hemodinamik Dan Penyakit Thrombosis (MU) HEMODINAMIK DAN PENYAKIT THROMBOSISDocument59 pagesHemodinamik Dan Penyakit Thrombosis (MU) HEMODINAMIK DAN PENYAKIT THROMBOSISflowerpearlyNo ratings yet
- Hemodynamic Disorders, Thromboembolic Disease and ShockDocument3 pagesHemodynamic Disorders, Thromboembolic Disease and ShockRuel MateoNo ratings yet
- Stroke 1Document69 pagesStroke 1Berk HalilbeyoğluNo ratings yet
- PediatricDocument8 pagesPediatricGuillana Mae CastellonNo ratings yet
- Bleeding Disorders of Primary HemostasisDocument18 pagesBleeding Disorders of Primary Hemostasisمصطفي خندقاويNo ratings yet
- HemodialysisDocument17 pagesHemodialysissayedmohammad mirlohiNo ratings yet
- Thrombosis: Pgi Ricky G. JalecoDocument34 pagesThrombosis: Pgi Ricky G. JalecoRicky JalecoNo ratings yet
- Disseminated Intravascular Coagulation (Dic)Document14 pagesDisseminated Intravascular Coagulation (Dic)Maria Rowena O. SalvoNo ratings yet
- Disseminated Intravascular CoagulationDocument7 pagesDisseminated Intravascular CoagulationSunaina AdhikariNo ratings yet
- Hemodynamic Disorders: By: Dr. SL RasonableDocument59 pagesHemodynamic Disorders: By: Dr. SL RasonableJenneth Marquez JoloNo ratings yet
- Name: Pardillo, Melody Jane B. Section: Bmls 10-3CDocument8 pagesName: Pardillo, Melody Jane B. Section: Bmls 10-3CJohnpaul FedericoNo ratings yet
- Perdarahan: DR - Suhaemi, SPPD, FinasimDocument27 pagesPerdarahan: DR - Suhaemi, SPPD, Finasimwie_wie_wieNo ratings yet
- ShockDocument1 pageShockWong Liang TungNo ratings yet
- Class 17Document46 pagesClass 17Nishani SatiyaseelanNo ratings yet
- Cardiovascular PathologyDocument182 pagesCardiovascular PathologyPavan chowdaryNo ratings yet
- Asuhan Keperawatan Pada Klien Stroke HemorraghicDocument126 pagesAsuhan Keperawatan Pada Klien Stroke HemorraghicHerna PattakitaNo ratings yet
- Hemodynamic Disorders Thromboembolic Disease and ShockDocument13 pagesHemodynamic Disorders Thromboembolic Disease and ShockAbu HuraraNo ratings yet
- Hemostasis Coaching NotesDocument45 pagesHemostasis Coaching NotesBen SabladaNo ratings yet
- Cardiovascular Pathology 2024Document132 pagesCardiovascular Pathology 2024Chen HouyuNo ratings yet
- ApendexDocument75 pagesApendexFuad Aman AbjNo ratings yet
- Path 3Document26 pagesPath 3رؤى مصطفىNo ratings yet
- PolychyemiaDocument38 pagesPolychyemiaRashmita DahalNo ratings yet
- Hemodynamic Disorders, Thrombosis and ShockDocument40 pagesHemodynamic Disorders, Thrombosis and ShockAndi Tri NugrahaNo ratings yet
- Heart Failure and CardiomyopathiesDocument26 pagesHeart Failure and Cardiomyopathieslionel andreaNo ratings yet
- Patho MicroDocument17 pagesPatho Microjyothsna yarraNo ratings yet
- Kuliah Patologi Gangguan Sirkulasi 11092017Document72 pagesKuliah Patologi Gangguan Sirkulasi 11092017Oman SetiyantoNo ratings yet
- Bleeding Disorders: (Hemorragic Diathesis)Document25 pagesBleeding Disorders: (Hemorragic Diathesis)nurina_abdrahimNo ratings yet
- Topic: Hemodynamic Dysfunction Fluid DistributionDocument44 pagesTopic: Hemodynamic Dysfunction Fluid DistributionSaleha ZainNo ratings yet
- Hemodynamics and GeneticsDocument14 pagesHemodynamics and GeneticsLeanna DaneNo ratings yet
- Heart Failure Idi SidoarjoDocument111 pagesHeart Failure Idi SidoarjoIka Kusuma WardhaniNo ratings yet
- Cheat Sheet #92 - Disseminated Intravascular CoaguationDocument3 pagesCheat Sheet #92 - Disseminated Intravascular CoaguationAsssNo ratings yet
- Cardio Day 3 TemplateDocument24 pagesCardio Day 3 TemplateMikeNo ratings yet
- Disseminated Intravascular Coagulation: Dr. Rudy Afriant, Sppd-KhomDocument22 pagesDisseminated Intravascular Coagulation: Dr. Rudy Afriant, Sppd-Khomsonnya morisaNo ratings yet
- Anemia DifferentialDocument1 pageAnemia Differentialkep1313No ratings yet
- Hematologi Css UploadDocument40 pagesHematologi Css UploadtutuptekoNo ratings yet
- CardiomyopathiesDocument13 pagesCardiomyopathiesNinna Isabel VictorioNo ratings yet
- Disseminated Intravascular CoagulationDocument3 pagesDisseminated Intravascular CoagulationArlan Abragan100% (1)
- Blood Transfusion JottingsDocument49 pagesBlood Transfusion JottingsAishat AwodeleNo ratings yet
- Patofisiologi StrokeDocument14 pagesPatofisiologi Strokenatalia alexandraNo ratings yet