Professional Documents
Culture Documents
Hematology SBIM Part 1
Uploaded by
Gousay Alkhazmari0 ratings0% found this document useful (0 votes)
9 views7 pagesHematology SBIM Part 1
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHematology SBIM Part 1
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views7 pagesHematology SBIM Part 1
Uploaded by
Gousay AlkhazmariHematology SBIM Part 1
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
Hematology SBIM Part 1 High Yield Facts
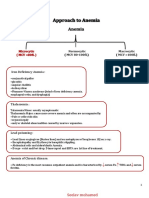
Normocytic • Inflammatory Anemia
Anemia o Reduction in EPO Activity
o Clue Ferritin High
o Transferrin Receptors Low Or Normal
o Decreased reticulocyte count
Microcytic Anemia • Iron Deficiency Anemia Most Common Cause Always Rule out first
o RBCs becomes heterogeneous in size and shape ↑ RDW
o Result in 2nd Thrombocytosis less than a million
o Consider Cancer in Elderly with +Ve FOBT
o Changes in Order
▪ Labs > Hgb > Morphologies
o Tx Oral iron, IV for those who can’t absorb Oral Iron (celiac)
▪ Hgb Concentration will rise by 2 gm\dl in 1-2 weeks
after therapy
o A Serum ferritin level >100 ng/mL rules out iron deficiency.
• Lead Poisoning Sideroblastic RBC
• Thalassemia
o Alpha Thalassemia 4 Alpha Chains
▪ Silent Carrier,1 Deletion
▪ Trait, 2 Deletion, Mild microcytic anemia Normal
hemoglobin electrophoresis Clue Normal RDW
▪ Hb H, 3 Deletion Tx Frequent Transfusion
o Beta Thalassemia 2 Beta Chains
▪ Trait 1 Deletion Normal RDW, Elevated hemoglobin
A2 in electrophoresis.
▪ Major 2 Deletion TX Frequent Transfusion,
Macrocytic • Megablastic Anemia MCV >115 a trilineage Disorder
Anemia o B12
▪ Seen in Alcoholic and IF Deficiency (Pernicious
Anemia) and Metformin users
▪ Confirmed with MVA and Homocysteine Elevated
▪ Copper Deficiency is a mimicker
o B9
▪ Only Homocysteine Elevated
o Fanconi anemia may cause Aplastic Anemia
▪ Primary
• DNA repair defect causing bone marrow
failure macrocytosis may be seen on CBC
• short stature, cafe-au-lai t spots with
thumb/radial defects.
▪ Secondary to
• AG, Heavy Metal Poisoning, Valproic Acid
Hemolytic Anemia • Congenital hemolytic anemias
o Sickle Cell Disease Low MCV
▪ AR Disorder
▪ Most Common organism for osteomyelitis S.Aurues
but they could have Salmonella .
▪ The Could Develop AVN of the Hip
▪ Aplastic Anemia with B19 Infection Rash and
Pancytopenia
▪ In VOC hydration is a must with good pain control
Alkhazmari Legacy Notes 1
Hematology SBIM Part 1 High Yield Facts
▪ Hydroxyurea Increase Hgb Fetal
• Indication More than two pain crises each
year or for those with ACS
• Response is assessed by ↑ MCV
• Decrease Mortality
▪ Exchange transfusion is indicated for patients with
an acute stroke, fat embolism, or ACS.
• ACS is usually characterized by pulmonary
infiltrates, fever, chest pain, tachypnea, and
hypoxemia
o G6PD X-linked
▪ Drug Induced and fava beans
▪ Normal Enzyme Level in Crisis
o Spherocytes
▪ Hereditary DAT +Ve
▪ Acquired DAT -Ve
• Alcoholism
• Hemolytic Transfusion reaction
o Sideroblastic
▪ Acquired B6 or Cooper Deficiency, INH or Alcohol
usage.
• Acquired hemolytic anemias
o Drug Induced Quinine, Penicillin, α-Methyldopa
o Autoimmune Hemolytic Anemia
▪ Warm autoimmune hemolytic anemia IgG
• CLL, NHL and SLE
• Tx Glucocorticoids+/- splenectomy > IVIG >
Rituximab
▪ Cold agglutinin disease IgM
• Seen in Mycoplasma infection and Plasma
Disorder
• Cold avoidance or rituximab for persistent
symptoms
• Glucocorticoids or splenectomy are usually
ineffective.
Neutropenia • Less than 1000
• Acute HIV, CMV, EBV
• B12, Copper and Zinc Deficiency
• Cytotoxic chemotherapies
• NSAIDs, carbamazepine, phenytoin, propylthiouracil,
cephalosporins, trimethoprim-sulfamethoxazole and Ganciclovir
• SLE, RA (Felty Syndrome)
• Tx
o Remove the offending drug.
o Granulocyte colony-stimulating factor if neutropenia is
complicated by infection
Eosinophilia • Eosinophil counts greater than 1500/μL
• Connective tissue diseases, like EGPA and RA
• Helminths aka parasites
• Idiopathic, Hyper eosinophilic syndrome
Alkhazmari Legacy Notes 2
Hematology SBIM Part 1 High Yield Facts
• Neoplasms Hodgkin lymphoma and CML
• Allergies asthma and drug-induced eosinophilia, DRESS and
Addison’s disease, for some reason.
Bleeding Disorders • Mixing Study
o NOT Corrected Antibodies against coagulation factors
o Corrected Deficiency coagulation factors
• Prolonged Bleeding time a Platelet Disorder
o Acquired
▪ Scurvy
▪ Uremia
▪ MDS
Hemophilia • X-linked
von Willebrand • Type 1 (AD) Quantitative, Type 2 Qualitative, Type 3 (AR)Sever
Disease Quantitative like Hemophilia.
• Most Common Inherited Disorder
• Mucocutaneous Bleeding
• Prolonged BT and a normal or prolonged a PTT
• Secondary hemostatic dysfunction can occur due Low Factor 8
• Heyde's syndrome (AS) acquired von Willebrand Disease
• Treatment
o Mild, OCP or Tranexamic Acid to Control bleeding
o Moderate or Before Simple procedure, DDAVP
o Sever, Factor 8 Concentrate
Thrombocytopenia • Important Values for Platelet transfusion
o Bleeding or planned surgery 50,000/μL
o No other risk factors for bleeding 10,000-20,000/μL
o Platelet transfusion for intracranial bleeding 100,000/μL
• Immune thrombocytopenia
o Idiopathic immune thrombocytopenia
o Drug-induced ITP Commonly Antibiotics
o Disease-associated immune thrombocytopenia HIV, HBV,
Thyroid Disease and malignancy
▪ Indication for treatment
• Evident Bleeding
• Plt. Count less than 30 K
▪ Treatment
• Glucocorticoids
• IVIG
• Last Resort Splenectomy or rituximab
• Consumptive Thrombocytopenia
o TTP a Hematological Emergency DON’T WAIT Treat with
plasma exchange.
▪ Thrombocytopenia and Hemolytic anemia (Clue)
▪ Plus, Fever, Mental State changes and AKI
▪ ADAMST13 Deficiency resulting large multimers of
vWF in their plasma
▪ Can be Acquired with Quinine, Clopidogrel,
Cyclosporine or Chemotherapeutic agent.
Alkhazmari Legacy Notes 3
Hematology SBIM Part 1 High Yield Facts
▪ Lab Shows Elevated LDH and Bilirubin with
fragmented RBC.
▪ Normal PT, aPTT, D-dimer, and fibrinogen levels
o DIC
▪ Thrombocytopenia and schistocytes
▪ Abnormal PT, aPTT, D-dimer, and fibrinogen levels
o HELLP
▪ Hemolysis, Elevated liver enzymes, and a Low
platelet count
▪ Occurs in association with pre-eclampsia or
eclampsia
▪ Treatment Delivery
o HUS
▪ Escherichia coli O157:H7 or Shigella infections
▪ Generally, within 6 days after diarrhea onset
Heparin-Induced • Type 1 Direct Destruction
Thrombocytopenia • Type 2 Antibodies mediated Thrombosis and Thrombocytopenia
and Thrombosis o Platelet decrease of >50% in a patient taking heparin
o or a thromboembolic event 5 to 10 days after starting
heparin
o Tx Stop Heparin and start argatroban, fondaparinux or
bivalirudin to treat Thrombosis
Thrombophilia • Acquired Thrombophilia
o Antiphospholipid antibody syndrome
▪ Lupus anticoagulants prolong PTT Confirmation
Russel viper venom associated with thrombosis
▪ Anticardiolipin antibody
▪ Diagnosed with Abs Positive in 2 occasions 12 weeks
apart.
▪ Recurrent Miscarriage at least 3 before 10th week or
one death after 34th weeks
▪ Tx Long term OAC
• Inherited Thrombophilia
o Factor V Leiden mutation Homozygous mutation is an
indication for prolonged OAC
o Antithrombin III can be lost in Nephrotic Syndrome
▪ They become heparin Resistant
Transfusion • An Acute hemolytic transfusion reaction
Medicine o ABO incompatibility
o Positive DAT
o Hypotension and Tachycardia
• A Delayed hemolytic transfusion reaction High Yield
o Delayed emergence of an alloantibody 2 to 10 days after
transfusion
o Extravascular hemolysis elevated serum bilirubin and LDH
levels new alloantibody
• A Febrile nonhemolytic transfusion reaction
o Donor leukocyte or alloantibodies directed against donor
leukocytes
o Tx Antipyretics
• Transfusion-related acute lung injury
Alkhazmari Legacy Notes 4
Hematology SBIM Part 1 High Yield Facts
o ARDS (hypoxemia and noncardiogenic pulmonary edema)
o Leukocyte aggregation in the pulmonary capillary bed within
6 hours
• Transfusion-associated circulatory overload
o Most common therefore we give Lasix in susceptible
individuals.
o Within 6 hours of transfusion
• An allergic transfusion reaction
o Especially in IgA deficiency
▪ Recurrent Sinopulmonary Disease
▪ Associated with autoimmune disease
Tumor lysis • UA level need to be Drawn on Ice pack
Syndrome • Labs ↑K+ ↑UA ↑ PO4 ↓Ca2+
• May be the first manifestation of AML
• Management
o Allopurinol and hydration Increase UOP for Moderate UA
level
o Rasburicase for Sever UA level or aggressive tumor
Acute Myeloid • Proliferation of myeloid cells with Auer rods
Leukemia • Leukostasis syndrome leukocyte count is very high CNS sx and Lung
sx
o Leukapheresis if leukocyte count >50 K or With Symptoms
• Labs ↑↑↑ Leukocyte count, Anemia, thrombocytopenia, and
Blasts
• Definitive Diagnosis Bone marrow biopsy showing >20% Blasts.
• Pancytopenia, but bone marrow will be hypercellular with 20% or
more blasts
• favorable risk: t(8;21), inv(16), t(15;17)
o t(15;17) Can Develop DIC treatment ATRA Vit A Analogue
▪ ATRA Side Effect; Differentiation syndrome
▪ Fever, pulmonary infiltrates, hypoxemia, and,
occasionally, hyperleukocytosis.
▪ Treatment is Dexamethasone
Acute • Extremely Aggressive
Lymphoblastic • CNS involvement
Leukemia • CNS prophylaxis (intrathecal chemotherapy with or without
radiation) Because standard chemotherapy cannot get into the CNS
and kill cancer cells
Chronic Myeloid • Confirmed by the presence of the Philadelphia chromosome
Leukemia (activated tyrosine kinase)
o Bad Prognosis
o Treatment Tyrosine kinase inhibitors: imatinib
• Elevated leukocyte count Basophils are Your Clue Almula Rule
Chronic • Asymptomatic
Lymphocytic • Diagnosis is confirmed by flow cytometry demonstrating cell surface
Leukemia antigens CD5 and CD23.
• Smudge cells
• Low serum IgG levels require replacement therapy to prevent
infection.
Alkhazmari Legacy Notes 5
Hematology SBIM Part 1 High Yield Facts
Leukemoid • Benign State
Reaction • High leukocyte alkaline phosphatase
• Response to stressors (eg, infections, medications, severe
hemorrhage)
Lymphoma • Enlarging lymphadenopathy associated with systemic symptoms
• To diagnosis lymphoma an excisional biopsy is a must then follow it
with a full body imaging with PET for Staging
o Hodgkin Lymphoma >>> Reed-Sternberg cells
▪ Aggressive lymphomas require immediate therapy
and often can be cured.
▪ Staging Spleen is not part of the staging
• Stage I one lymph node region or organ.
• Stage II Two or more lymph nodes are
affected. Above or below the diaphragm.
• Stage III Both sides of the diaphragm.
• Stage IV Every Where
▪ Treatment: ABVD followed by radiation therapy
• Most Questions are about complications
• (A)driamycin aka doxorubicin > Dilated CMP
• (B)leomycin > Lung Fibrosis
• (V)inblastine > Peripheral neuropathy
• (D)acarbazine > Sterility
▪ Radiotherapy increase Risk for secondary cancers
(breast, lung, skin) and CAD.
o Non-Hodgkin lymphoma
Plasma Cell • Multiple Myeloma
Disorder o Signs and symptoms
▪ C (hyperCalcemia)
▪ R (Renal failure)
▪ A (Anemia)
▪ B (Bone disease: lytic lesions, fractures, or
osteoporosis)
o Testing SPEP or UPEP a clue is low anion gap
o a Skeletal Survey to assesses for lytic bone lesions Do not
use bone scans.
o Even if you suspect MM but the presentation is an cute
neurological manifestation MRI Spine is your answer
• Waldenström Macroglobulinemia
o A Fake ☺ Lymphoma (Lymphadenopathy, hepatomegaly, and
splenomegaly)
o IgM Elevated (Pentamer)
o Hyperviscosity syndrome an emergency treated with
plasmapheresis.
Alkhazmari Legacy Notes 6
Hematology SBIM Part 1 High Yield Facts
Myeloproliferative • Polycythemia Vera
Neoplasms o Hemoglobin level is >16.5 g/dL in men or >16 g/dL
o Low EPO level a clue to rule out secondary causes
(hypoxemia, kidney or liver carcinoma and use of
androgens)
o The JAK2 mutation 97%
o Budd Chiari and Hepatic vein thrombosis r\o PV
o Pruritus (↑ hot water), and SPLENOMEGALY
o LOW DOSE ASA is Indicated (High Dose result in Thrombosis)
o Treatment
▪ Low Risk
• Phlebotomy Hct level to <45%.
▪ High Risk Group
• Old Above 60 yrs
• History of thrombosis
• Elevated WBC count
• Phlebotomy and Hydroxyurea
• Essential Thrombocythemia
o Platelet counts greater than 450,000/μL
o The JAK2 mutation 50%
o Hyper Viscosity Symptoms
o Treatment
▪ Low Risk
• ASA to reduces Hyper Viscosity
▪ High Risk Group
• Old Above 60 yrs
• History of thrombosis
• Elevated WBC count above 11K
• ASA and Hydroxyurea
▪ Plateletpheresis in life-threatening situations or to
reduce count rapidly
• TIA, stroke, MI, or GI bleeding
• Myelofibrosis
o Teardrop erythrocytes, and bone marrow fibrosis
o Splenomegaly and hepatomegaly result from
extramedullary hematopoiesis.
o Death transformation to acute leukemia, or portal
hypertension complications
Alkhazmari Legacy Notes 7
You might also like
- HematologyDocument20 pagesHematologyJunaid SabirNo ratings yet
- Hemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamDocument56 pagesHemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamMarcelliaNo ratings yet
- AnemiaDocument55 pagesAnemiaapi-2682649650% (2)
- Approach To AnemiaDocument4 pagesApproach To AnemiapNo ratings yet
- Haematology: MAP 6.1 AnaemiaDocument12 pagesHaematology: MAP 6.1 AnaemiaGrecia BocuNo ratings yet
- Nursing Clients With Hematologic DisordersDocument4 pagesNursing Clients With Hematologic DisordersLuna MarieNo ratings yet
- Hematologic Disorders - CumulativeDocument28 pagesHematologic Disorders - CumulativeThesmith Fam100% (1)
- Haemolytic Anaemia: DR Nurul Fahmiza Tumiran P109273Document55 pagesHaemolytic Anaemia: DR Nurul Fahmiza Tumiran P109273Nurul FahmizaNo ratings yet
- Anemia: Prof. Dr. Djoni Djunaedi, DR., SP - PD., KptiDocument48 pagesAnemia: Prof. Dr. Djoni Djunaedi, DR., SP - PD., KptiHarmas Novryan FarezaNo ratings yet
- Hematology Lecture - AnemiaDocument10 pagesHematology Lecture - AnemiaKimberly EspaldonNo ratings yet
- Hematologi ModulDocument67 pagesHematologi ModulSyifa Mahmud Syukran Akbar100% (1)
- Super Simplified Pathology Hematology - Dr. Priyanka SachdevDocument500 pagesSuper Simplified Pathology Hematology - Dr. Priyanka SachdevMohd SaquibNo ratings yet
- Hemoglobin Opa ThiesDocument11 pagesHemoglobin Opa ThiesprasasthiNo ratings yet
- Hemolytic AnemiasDocument59 pagesHemolytic AnemiasRajesh darlingNo ratings yet
- Blok 5 Antianaemic DrugsDocument26 pagesBlok 5 Antianaemic DrugsPutri HusnanNo ratings yet
- ANEMIADocument34 pagesANEMIAAkashNo ratings yet
- Interpreting The CBC - When To ReferDocument44 pagesInterpreting The CBC - When To ReferKannan KannanNo ratings yet
- Chapters 33 and 33: Hematological System Iron Deficiency Anemia Etiology (Cause)Document14 pagesChapters 33 and 33: Hematological System Iron Deficiency Anemia Etiology (Cause)Celena LorenaNo ratings yet
- Hematological Disorders Hematological Disorders: Renzn405Document23 pagesHematological Disorders Hematological Disorders: Renzn405Jhodie PabalanNo ratings yet
- Child With Hematologic DisordersDocument5 pagesChild With Hematologic Disordersjadengg.pandak014No ratings yet
- AnaemiaDocument25 pagesAnaemiaIshali NuwanjiniNo ratings yet
- Hematology Final ExamDocument20 pagesHematology Final ExamAlon GoldfainerNo ratings yet
- Thalassemia 170303193104Document23 pagesThalassemia 170303193104interna MANADONo ratings yet
- Spleen Outline For FacultyDocument9 pagesSpleen Outline For Facultygaulep3164valNo ratings yet
- Hemolytic Anemia-Pediatric MasterDocument62 pagesHemolytic Anemia-Pediatric MasterPedia 2020No ratings yet
- Hemolytic AnemiaDocument1 pageHemolytic AnemiaVirgile KenmoueNo ratings yet
- Anemia OutlineDocument3 pagesAnemia Outlinekaylakmills_10135868No ratings yet
- AnemiaDocument27 pagesAnemiaSri Ram Prasath TNo ratings yet
- HEMA 2 - Midterm Topic 1 - ADDITIONAL NOTESDocument6 pagesHEMA 2 - Midterm Topic 1 - ADDITIONAL NOTESLowenstein JenzenNo ratings yet
- Pendekatan Diagnosis AnemiaDocument7 pagesPendekatan Diagnosis AnemiaFerry GhifariNo ratings yet
- Anemia 2Document42 pagesAnemia 2AbdulKhaleq AlkadimiNo ratings yet
- PediatricDocument192 pagesPediatricbolt boltNo ratings yet
- Diseases of The Newborn Part2Document6 pagesDiseases of The Newborn Part2sarguss14100% (1)
- Macrocytic AnemiaDocument49 pagesMacrocytic AnemiaANo ratings yet
- An Approach To Anemia: Brad Lewis Director Hematology San Francisco General HospitalDocument47 pagesAn Approach To Anemia: Brad Lewis Director Hematology San Francisco General HospitalyapponNo ratings yet
- Lab ValueDocument12 pagesLab ValuefmakenlyneNo ratings yet
- TrW-Guwv 0g VwhuPGl65PBCquGkt3j5Document65 pagesTrW-Guwv 0g VwhuPGl65PBCquGkt3j5Shikhar MishraNo ratings yet
- Lecture Lesson 9. Red Blood Cell DisordersDocument7 pagesLecture Lesson 9. Red Blood Cell DisordersHANA LUNARIANo ratings yet
- Anemia 1Document92 pagesAnemia 1Bikash PatgiriNo ratings yet
- Hema FinalsDocument12 pagesHema FinalsHANA LUNARIANo ratings yet
- HematologyDocument42 pagesHematologyalvin.de.fieryNo ratings yet
- Thalassemi ADocument23 pagesThalassemi Ainterna MANADO100% (1)
- BoardReviewPart1A BenignHemePathDocument170 pagesBoardReviewPart1A BenignHemePathMaria Cristina Alarcon NietoNo ratings yet
- What Is A "SickleDocument11 pagesWhat Is A "SickleElsa FitrianiNo ratings yet
- Week 5 Pedia Blood Disorders StudentDocument39 pagesWeek 5 Pedia Blood Disorders StudentJaslir MendozaNo ratings yet
- RBC DisordersDocument70 pagesRBC DisordersNdor Baribolo100% (1)
- 1.05 Qualitative 0 Quantitative Platelet DisordersDocument9 pages1.05 Qualitative 0 Quantitative Platelet DisordersShiena ArchividoNo ratings yet
- Evaluation of The Anemic PatientDocument44 pagesEvaluation of The Anemic PatientShobana KmNo ratings yet
- Hemolytic Anemia IntrinsicDocument14 pagesHemolytic Anemia IntrinsicSophia Gail ChingNo ratings yet
- HEMATOLOGYDocument17 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- HematologyDocument5 pagesHematologyIvy Jan OcateNo ratings yet
- Amenia FinalDocument11 pagesAmenia FinalChihnita ChandanaNo ratings yet
- Types of Anaemia and How To Remember Them: With Sophie BroughtonDocument28 pagesTypes of Anaemia and How To Remember Them: With Sophie BroughtonurtikikeNo ratings yet
- Haematology-Summary My NotesDocument24 pagesHaematology-Summary My NotesToria053No ratings yet
- Anemia TutoringDocument28 pagesAnemia TutoringngNo ratings yet
- Anemia 1Document30 pagesAnemia 1Aishwarya JeeNo ratings yet
- Anemia SDocument42 pagesAnemia SCristinaGheorgheNo ratings yet
- Finals Week 10Document8 pagesFinals Week 10MARIE NELLIE MOSTRADONo ratings yet