Professional Documents
Culture Documents
Anemia Outline
Uploaded by
kaylakmills_101358680 ratings0% found this document useful (0 votes)
51 views3 pagesAnemia is defined as a low number of circulating red blood cells (RBCs) or low levels of hemoglobin (Hgb). It results from decreased RBC production, increased RBC destruction, or blood loss. Common causes include iron, vitamin B12 or folate deficiencies, blood loss, bone marrow failure, and chronic diseases like chronic kidney disease (CKD). Symptoms are usually mild but can include fatigue, dyspnea, and palpitations. Diagnosis involves a complete blood count and identifying the underlying cause. Treatment depends on the cause but may include oral or intravenous iron, B12, folate supplements, erythropoiesis-stimulating agents, or blood transfusions.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAnemia is defined as a low number of circulating red blood cells (RBCs) or low levels of hemoglobin (Hgb). It results from decreased RBC production, increased RBC destruction, or blood loss. Common causes include iron, vitamin B12 or folate deficiencies, blood loss, bone marrow failure, and chronic diseases like chronic kidney disease (CKD). Symptoms are usually mild but can include fatigue, dyspnea, and palpitations. Diagnosis involves a complete blood count and identifying the underlying cause. Treatment depends on the cause but may include oral or intravenous iron, B12, folate supplements, erythropoiesis-stimulating agents, or blood transfusions.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
51 views3 pagesAnemia Outline
Uploaded by
kaylakmills_10135868Anemia is defined as a low number of circulating red blood cells (RBCs) or low levels of hemoglobin (Hgb). It results from decreased RBC production, increased RBC destruction, or blood loss. Common causes include iron, vitamin B12 or folate deficiencies, blood loss, bone marrow failure, and chronic diseases like chronic kidney disease (CKD). Symptoms are usually mild but can include fatigue, dyspnea, and palpitations. Diagnosis involves a complete blood count and identifying the underlying cause. Treatment depends on the cause but may include oral or intravenous iron, B12, folate supplements, erythropoiesis-stimulating agents, or blood transfusions.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
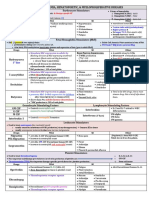
Anemia
Definition Erythropoiesis (RBC Synthesis) Symptoms Compensatory Mechanisms
↓ number of circulating RBCs Starts in bone marrow w: Asymptomatic mostly ↑ cardiac output
Low Hgb, HCT, RBC measured on o Folate, Vit. B12, Iron Fatigue** – hallmark ↑ coronary flow
CBC: o Cytokines Dyspnea Altered blood viscosity
o EPO Hyperdynamic Changes in O₂ consumption &
EPO release o Bounding pulses extraction
o Due to hypoxia (not RBC level) o Palpitations
o growth /differentiation of RBCs o Roaring in ears
-Normoblasts: slightly mature RBCs
-Reticulocytesmature RBCs Symptoms due to:
4 days to mature o Hypoxia
RBC circulate for 120 days o Hypovolemia (bleeds)
-Surrogate Markers
Pathophysiology Evaluation Evaluation
↓ RBC production Hgb < 11g/dL 1. Kinetic Approach
Hgb > 2 below baseline Focuses on underlying mechanism of anemia
o Nutrition deficiencies –B12, Fe CBC w/ indicies Primary featurereticulocyte count
o BM failure - (chemo, radiation) Blood smear morphology o Corrected against degree of anemia
o Tumor into marrow Evaluate possible causes o Normal RI = 1.0-2.0
o Endocrine deficiency –EPO synth. Reticulocyte count & MCV Low RI = ↓RBC production
o Chronic DZ – renal, liver, High RI = ↑ or normal RBC
infection
Blood loss – most common** Additional Cues or Tests 2. Morphologic Approach size of RBC
Iron deficiency Microcytic: <80 - Fe deficiency
o Trauma, Ulcers, NSAIDs
o TIBC- reflects Fe storage seen in hepatocellular carcinoma or renal cell carcinoma
RBC destruction
o TSAT- bound Fe in serum Normocytic: MCV 80-100 - Blood loss
o Hemolysis o Ferritin- Fe storage protein also hemolysis, BM failure, chronic inflam, renal insufficiency
o Drug-Induced Hemorrhage: + stool guaiac key follow up test: reticulocyte count
Hemolysis: + coombs test, ↑LDH Macrocytic: MCV >100 - B12/folate deficiency
also abnormal RBC maturation
or indirect bilirubin
Classifications: CKD: GFR <60 for >3 months, ↓EPO
Based on MCV – size of RBC Vitamin B12:
level Abnormal DNA metabolism: Releases large, immature RBCs
o Microcytic: ↓ than normal
o Normocytic Often Drug Induced: MTX, 6-MP
o Macrocytic: than normal Treatment:
o Cyanocobalamin 1000mcg IM/SQ weekly X 4-6 weeks
Based on Hgb content o Cyanocobalamin PO daily X 1 month
o Hypochromic – ↓normal Maintenance: Cyanocobalamin IM/SQ monthly or PO QD
o Normochromic Folic Acid:
Poor intake or drug induced: 5-FU, 6-MP, MTX
o Hyperchromic – normal
Txt: Folic Acid 1 mg PO daily X 4 months
Iron Deficiency anemia
Causes Fe Storage and Requirements Lab Results
Blood loss: Stored as Ferritin in:
o Menstruation, GI bleed, Trauma o Liver, Spleen, Marrow
↓ absorption: Absorbed as Ferrous (Fe 2+) in:
o Gastrectomy, Inflammation, Poor diet o Duodenum, Upper Jejunum
↑ requirement: Pregnancy Nutritional requirements:
Impaired utilization: Heredity o Adult M /Post-menopause Fem – 8 mg
o Pre-menopausal women – 18 mg
Iron Treatments
PO Supplementation IV Supplementation
Recommended: 200 mg elemental Fe daily Indications: Iron Wk 1: Test dose 25 mg Anaphylactic type rxn
Tx for 3-6 months to replete stores Intolerance to PO Dextran (slow IV push); 1 hr -uneventful test dose
Dosed based on tolerability Malabsorption later 75 mg over 5 min DOES NOT ensure rxn
Sig blood loss Week2-10: 100 mg will not occur w.
over 5 min QW therapeutic dose
Counseling Points: CKD
Ferric IV infusion:125 mg Hypersensitivity rxn
AEs: dark stools, N/V/D/C Chemo pt on ESAsGluconat over 1 hr Avoid rapid admin
Give with Vit C to ↑ absorption e Repeat dose QW x 8wk Dilute in 100 ml NS
Take 1 hr before meals trial showed Hgb (Ferrlecit)
o milk & tea ↓ absorption increase is greater in Iron Diff doses for CKD & Anaphylactic type rxn
IV iron than PO iron Sucrose
Take 2 hr before or 4 hr after antacid chemo-assoc anemia Dilute doses
(Venofer)
Anemia of Chronic Kidney Disease
Caused by:
Chemotherapy
Infections (e.g. HIV)
Inflammatory disease
CKD
Treatments
PRBCs ESAs
About Preferred for immediate correction Takes weeks to elicit Hgb response
o Rapid ↑ in Hgb & Hct Was popular in early 2000s for cancer
o 1 unit PRBC (300 mL) ↑Hgb 1g/dL Allows for 16% reduction in transfusions
Neutropenic pts may need CMV (-) PRBCs o Mostly just improves QOL
Used when Hgb > 10g/dL (or >7-8 via AABB) Dosed differently for CKD or chemo related anemia
May enhance OS High risks, minimal benefit
Survival Retrospective study of 56 unresectable esophageal cancer pts N/A
on
RT w/ cisplatin & 5-FU
5 yr OS 65% compared to 21% in placebo
Risks Transfusion rxn (type & test for cross reactivity first) ↑ mortality & tumor progression
CHF Thromboembolism (strong link)
Bacterial contamination/viral infect. (rare) HTN & seizures
Fe overload (w/ numerous transfusions) Pure red cell aplasia
VTE **REMS PROGRAM due to multitude of risks!
Sickle Cell Anemia
Etiology/Epidemiology Fetal Hgb (HbF) Complications
Inherited, autosomal recessive Hgb 2 alpha & 2 gamma Hgb subunits Hemolysis
disorder o Adult Hgb = 2 alpha & 2 beta o Sickle cell life span 10-20 days
o DNA substitution mutation at o <2% of adult Hgb is this form o Shorter life span than normal RBC bc of
beta-globin gene Inhibits polymerization that results in hemolysis anemia
o TA substitution results in more sickle shape o ↓NO vasoconstriction
negative charge polymerized, o >20% HbF milder disease ↑adhesion/coag initiation
sickle-shaped RBCs o If we can induce this, it could be Obstructed blood flow to
Sickled RBCs are rigid & cause occlusions in beneficial! spleen ↑risk of infection
microvasculature Vaso-occlusion
o Poor oxygenation o Pain
o Excrutiating pain o Stroke
2.5 mill American carriers o Acute chest syndrome
70,000 w/ disease Similar to ARDS
Survival advantage in malaria areas Causes cough/dyspnea
o Priapism
o Splenic sequestration
o Osteonecrosis
o Renal insufficiency
o Anemia
o Infection w/ encapsulated organisms
Management
Prevention/Txt of crisis Pain Mgmt (cornerstone) Infection Prevention
Hydroxyurea:↑HgF synth & ↓ neutrophils Usually requires opioids (often IV) PCV13 & PPSV23
Indicated if: Hydration w/ D5W ½ NS w/ 20 mEq KCl for Meningococcal vaccine
o 3+ pain crisises/yr severe crisis PCN prophylaxis (erythromycin for PCN allergy)
o acute chest syndrome
o severe anemia Txt:
Monitoring Common Organisms: S. pneumo, H. flu, S.
o CBC w/ indicies q 2-4 wks aureus, E. coli, EGNR
o Reticulocyte count, HgF, CMP q 3-6 mo. Ceftriaxone
AEs: Vancomycin only if meningitis suspected
o Neutropenia, thrombocytopenia
o Hyperpigmentation & drying of skin/nails
o Teratogenicity (preg. Cat D)
Hydroxyurea requires dose titration**
SUMMARY:
Anemias have various etiologies
Treatment depends on the morphology of the anemia
Folic acid, Vitamin B12, and iron supplementation is needed for their respective deficient anemias
ESAs are limited in use due to high risks and minimal benefit
Sickle cell anemia is an inherited disorder that requires lifelong management of its complications
Hydroxyurea is the drug of choice to manage sickle cell crisis and it requires dose titration
You might also like
- Agents For Anemia, Hematopoietic, & Myeloproliferative DiseasesDocument2 pagesAgents For Anemia, Hematopoietic, & Myeloproliferative Diseaseskaylakmills_10135868No ratings yet
- Fludrocortisone: Steroid Side EffectsDocument3 pagesFludrocortisone: Steroid Side Effectskaylakmills_10135868No ratings yet
- Bacterial Infectious Diseases Empiric TherapyDocument17 pagesBacterial Infectious Diseases Empiric Therapykaylakmills_10135868No ratings yet
- Learner: Lord Mvoula: Test Name Completion Date Score Timespent ResultDocument3 pagesLearner: Lord Mvoula: Test Name Completion Date Score Timespent ResultLord M.No ratings yet
- Pharmacology SummaryDocument16 pagesPharmacology Summaryshenric16No ratings yet
- Vancomycin Protocol RQHRDocument15 pagesVancomycin Protocol RQHRl1o2stNo ratings yet
- EMS Final Exam JulyDocument267 pagesEMS Final Exam Julyraja bouguerraNo ratings yet
- Pharmacology Quick HitsDocument6 pagesPharmacology Quick HitsHuma Hameed DogarNo ratings yet
- Pharmacology Exam4 ReviewDocument8 pagesPharmacology Exam4 ReviewNatalia BortellNo ratings yet
- Required Formulas Look ThruDocument6 pagesRequired Formulas Look Thrukaylakmills_10135868No ratings yet
- Pharma FinalADocument33 pagesPharma FinalAvaegmundigNo ratings yet
- Cholinergics and Cholinergic BlockersDocument5 pagesCholinergics and Cholinergic Blockersapi-3739910100% (3)
- Basic Practice of Anesthesiology FinalDocument70 pagesBasic Practice of Anesthesiology FinalAfiqah So JasmiNo ratings yet
- Know Common Disease ManagementDocument14 pagesKnow Common Disease Managementcdx25No ratings yet
- Cancer Drugs Drugs Indication Adverse Effects Interaction and ContraindicationDocument5 pagesCancer Drugs Drugs Indication Adverse Effects Interaction and ContraindicationOndari gisemba OSINDENo ratings yet
- Introduction of Neonatal Disease-Bi GuangliangDocument43 pagesIntroduction of Neonatal Disease-Bi GuangliangsinghNo ratings yet
- PHARM ATI ReviewDocument76 pagesPHARM ATI Reviewth233100% (1)
- Drug Interactions of Antianginal Drugs..Document40 pagesDrug Interactions of Antianginal Drugs..Kamal SikandarNo ratings yet
- Induction Agents MOA Onset, Duration Special Uses / Notes PropofolDocument3 pagesInduction Agents MOA Onset, Duration Special Uses / Notes PropofolpaveethrahNo ratings yet
- Anticoagulants DrugsDocument6 pagesAnticoagulants DrugsHusam Al-OdatNo ratings yet
- Calcium 1000mg or 1.5 G + Vit D (Enhances Absorption) 400-600 IU/ DayDocument1 pageCalcium 1000mg or 1.5 G + Vit D (Enhances Absorption) 400-600 IU/ DayRie PangilinanNo ratings yet
- Vancomycin ReviewDocument26 pagesVancomycin Reviewkhangsiean89No ratings yet
- Critical Care Drugs 2Document23 pagesCritical Care Drugs 2Asri Ernadi100% (1)
- Pre Exam Answers I FoundDocument73 pagesPre Exam Answers I FoundDuy LuuNo ratings yet
- Drugs and AntidotesDocument1 pageDrugs and AntidoteskiranbhandarkarNo ratings yet
- ACE InhibitorDocument19 pagesACE InhibitorApurba Sarker ApuNo ratings yet
- Antimicrobials AntibioticsDocument2 pagesAntimicrobials AntibioticsJULIE ANNE TAN100% (1)
- Goljan ErrataDocument9 pagesGoljan Erratajwmeadow2401No ratings yet
- Neurodegenerative DiseasesDocument32 pagesNeurodegenerative DiseasesApurba Sarker Apu100% (1)
- Acute GlomerulonephritisDocument21 pagesAcute Glomerulonephritisbrinda johnNo ratings yet
- Pharmacology - Chapter 29Document5 pagesPharmacology - Chapter 29Ashley-Michelle LewisNo ratings yet
- Cholinergic DrugsDocument15 pagesCholinergic DrugsChris Girgis100% (1)
- Summary of Antidiabetic Drugs PDFDocument3 pagesSummary of Antidiabetic Drugs PDFZinc YuloNo ratings yet
- Impactednurse Nurses Reference PackDocument2 pagesImpactednurse Nurses Reference PackRaenell CurryNo ratings yet
- Bleeding DisordersDocument24 pagesBleeding Disorderskholoud220No ratings yet
- Hypertension Drugs Cheat Sheet: by ViaDocument3 pagesHypertension Drugs Cheat Sheet: by ViaGulzaib KhokharNo ratings yet
- Management of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFDocument4 pagesManagement of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFveerrajuNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- PharmacologyDocument3 pagesPharmacologyMohd Afiq AizuddinNo ratings yet
- MCQ For Training To Step-1, Intermediate and Final Control in 2014 - 2015 YearsDocument11 pagesMCQ For Training To Step-1, Intermediate and Final Control in 2014 - 2015 YearsAbhishekAbhiNo ratings yet
- Pharmacology Test 1Document39 pagesPharmacology Test 1Niki BolinNo ratings yet
- Lippincott Questions CH 2Document15 pagesLippincott Questions CH 2rajuNo ratings yet
- OB ATI Study Guide: Initial Prenatal VisitDocument26 pagesOB ATI Study Guide: Initial Prenatal Visitxoxo318No ratings yet
- Antihyperlipidemic Drugs: Key Terms Chapter ObjectivesDocument9 pagesAntihyperlipidemic Drugs: Key Terms Chapter ObjectivesSasa AbassNo ratings yet
- Patho Physio 51 To 100qDocument67 pagesPatho Physio 51 To 100qRaquel BencosmeNo ratings yet
- Nephrotic and NephriticDocument27 pagesNephrotic and Nephritictam meiNo ratings yet
- Pathology Checklist DR Preeti SharmaDocument5 pagesPathology Checklist DR Preeti SharmaAvi Khanna100% (1)
- AnxietyDocument5 pagesAnxietyJohn HolmesNo ratings yet
- Anthrax TeachingDocument78 pagesAnthrax Teachingtummalapalli venkateswara raoNo ratings yet
- Prefix, Suffix of DrugsDocument6 pagesPrefix, Suffix of DrugsBriel Jake CabusasNo ratings yet
- Pharma CollectionDocument40 pagesPharma CollectionMuhd Nico DariyantoNo ratings yet
- Usmle World Step 1 Pharmacology: Question ListDocument73 pagesUsmle World Step 1 Pharmacology: Question ListAnonymous 4txA8N8etNo ratings yet
- Drug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsDocument57 pagesDrug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsManisha ShakyaNo ratings yet
- Hypertension ExamDocument11 pagesHypertension Exambobtaguba100% (1)
- AntibioticsDocument54 pagesAntibioticsYvan MercedNo ratings yet
- Antibiotics 9Document11 pagesAntibiotics 9Beth Morales100% (1)
- Types of Anaemia and How To Remember Them: With Sophie BroughtonDocument28 pagesTypes of Anaemia and How To Remember Them: With Sophie BroughtonurtikikeNo ratings yet
- AnaemiaDocument7 pagesAnaemiaYousef El3alameyNo ratings yet
- NCM107 ObstetricsDocument9 pagesNCM107 ObstetricsKM PanganibanNo ratings yet
- RBC DisordersDocument70 pagesRBC DisordersNdor Baribolo100% (1)
- Cardio: Cyp SubstratesDocument4 pagesCardio: Cyp Substrateskaylakmills_10135868No ratings yet
- Gerd 2x Per Week Pud : Gastric Eating Bad or Duodenal Ulcer Eating HelpsDocument3 pagesGerd 2x Per Week Pud : Gastric Eating Bad or Duodenal Ulcer Eating Helpskaylakmills_10135868No ratings yet
- Required Formulas Look ThruDocument6 pagesRequired Formulas Look Thrukaylakmills_10135868No ratings yet
- New Dyslipidemia 2021 Naplex QuickDocument2 pagesNew Dyslipidemia 2021 Naplex Quickkaylakmills_1013586883% (6)
- HIV Drugs Class and DDIDocument5 pagesHIV Drugs Class and DDIkaylakmills_101358680% (1)
- Cephalosporin Generations and CoverageDocument3 pagesCephalosporin Generations and Coveragekaylakmills_10135868No ratings yet
- Julius Klaproth: His Life and Works With Special Emphasis On Japan Hartmut Walravens, BerlinDocument15 pagesJulius Klaproth: His Life and Works With Special Emphasis On Japan Hartmut Walravens, BerlinSarbu Ana100% (1)
- David CarpenterDocument2 pagesDavid CarpenterbobblobNo ratings yet
- Book Blast 23 June 2023Document2 pagesBook Blast 23 June 2023ionaNo ratings yet
- RA 8371 Key PointsDocument6 pagesRA 8371 Key PointsKristine DiamanteNo ratings yet
- Free Time Is For The Untouched: Ricardo Rodriguez Novel Chapter 9/21/15Document3 pagesFree Time Is For The Untouched: Ricardo Rodriguez Novel Chapter 9/21/15api-299832803No ratings yet
- India Patent Form 13Document2 pagesIndia Patent Form 13adityakochharNo ratings yet
- Capstone PDFDocument6 pagesCapstone PDFapi-351689838No ratings yet
- Law of Evidence - InterimDocument6 pagesLaw of Evidence - InterimshanikaNo ratings yet
- Atoms vs. Ions Worksheet: CationsDocument5 pagesAtoms vs. Ions Worksheet: CationsR NovNo ratings yet
- HRD Multiple Choice QuestionDocument29 pagesHRD Multiple Choice QuestionHayat TarrarNo ratings yet
- Application - For - Adjunct Faculty - COEPDocument7 pagesApplication - For - Adjunct Faculty - COEPSwapnilMahajanNo ratings yet
- Creation of The PNPDocument1 pageCreation of The PNPKyla MatulacNo ratings yet
- Sem Osteoporosis (Edit)Document31 pagesSem Osteoporosis (Edit)Rhomizal MazaliNo ratings yet
- Bservation of A Commonplace Phenomenon,: Theory of Vortex SoundDocument19 pagesBservation of A Commonplace Phenomenon,: Theory of Vortex SoundQianZHNo ratings yet
- 6 Maqaamaat Deen Thalatha PDFDocument10 pages6 Maqaamaat Deen Thalatha PDFIsma'eel BakareNo ratings yet
- Biography of 16th Karmapa and 3d Jamgon KongtrulDocument16 pagesBiography of 16th Karmapa and 3d Jamgon KongtrulSergey SergeyNo ratings yet
- Totalitarianism Reading QuesitonsDocument2 pagesTotalitarianism Reading Quesitonsapi-264099960No ratings yet
- Thoth (Djhuty) Analysis and Etymology - by - Alexis BianchiniDocument9 pagesThoth (Djhuty) Analysis and Etymology - by - Alexis BianchiniAlexis BianchiniNo ratings yet
- Zhang Age Estimation Using Pulpenamel Volume Ratio of ImpactedDocument9 pagesZhang Age Estimation Using Pulpenamel Volume Ratio of ImpactedMeris JugadorNo ratings yet
- Davidich 2013Document13 pagesDavidich 2013mahima pahawaNo ratings yet
- Lauren Gantz On - The Palm Wine Drinkard - E3W Review of BooksDocument2 pagesLauren Gantz On - The Palm Wine Drinkard - E3W Review of BooksjayasriniNo ratings yet
- Costa and Andreaus - 2020 - Social Impact and Performance Measurement SystemsDocument25 pagesCosta and Andreaus - 2020 - Social Impact and Performance Measurement SystemsMaryam AhmedNo ratings yet
- Corporate Finance North South University ReportDocument44 pagesCorporate Finance North South University ReportTahsin UddinNo ratings yet
- USH 1.05 HonorsDocument7 pagesUSH 1.05 HonorsAubrey HovanNo ratings yet
- Literacher ReviewDocument5 pagesLiteracher ReviewEsha PandyaNo ratings yet
- Coulmas 2009Document13 pagesCoulmas 2009Katie Bernstein0% (1)
- ORAL-COMMUNICATION11 - Q1 - Module 1 - 08082020Document27 pagesORAL-COMMUNICATION11 - Q1 - Module 1 - 08082020Lily CruzNo ratings yet
- Book Review Assignment Book: The Da Vinci Code Group Members: Sadia Jabeen World LiteratureDocument5 pagesBook Review Assignment Book: The Da Vinci Code Group Members: Sadia Jabeen World LiteratureZone MusicNo ratings yet
- Why Parents Should Avoid Telling Their Children Fairy Tales SlidesDocument21 pagesWhy Parents Should Avoid Telling Their Children Fairy Tales SlidesGebriellaNo ratings yet
- Exercise 1.3: Predicate and QuantifiersDocument17 pagesExercise 1.3: Predicate and QuantifiersBaby balochNo ratings yet