Professional Documents
Culture Documents
Obstetric Hemorrhage Checklist
Uploaded by
Herwinda GeraldineOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obstetric Hemorrhage Checklist
Uploaded by
Herwinda GeraldineCopyright:
Available Formats
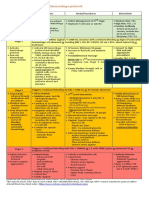
Obstetric Hemorrhage Protocol Checklist
Stage 0: All Births – Prevention & Recognition of OB Hemorrhage
Prophylactic Oxytocin, Quantitative Cumulative Evaluation of Blood Loss & Close Monitoring
Perform ongoing risk assessment at the start of the second stage of labor, at transfer to postpartum
care, and any time the patient’s condition changes
If new risk factors develop, increase risk level and convert to type and screen or type and crossmatch (see above)
Active management of third stage
Oxytocin IV infusion or 10 units IM; do not give oxytocin as IV push
Ongoing quantitative cumulative evaluation of blood loss
Using formal methods, such as graduated containers, visual comparisons and weight of blood-soaked materials (1gm = 1mL)
Ongoing evaluation of vital signs
ADDITIONAL DELIVERY & ONGOING POSTPARTUM RISK FACTORS
Low Medium High
ROUTINE INCREASED SURVEILLANCE
CARE POSTPARTUM CARE TEAM ASSESSES RESPONSE READINESS
Cesarean birth during this admission Active bleeding soaking > 1 pad per
nd
– especially if urgent/emergent/2 stage hour or passing a ≥ 6 cm clot
Operative vaginal delivery Retained placenta
rd th
Genital tract trauma including 3 & 4 Non-lower transverse uterine
degree lacerations incision for cesarean birth
Quantitative Cumulative Blood Loss Quantitative Cumulative Blood Loss
500-1000 mL with a vaginal delivery ≥ 1000 mL or treated for
hemorrhage
Received general anesthesia
Uterine rupture
Triggers to Proceed to STAGE 1:
CBL ≥ 500mL vaginal / ≥ 1000 mL cesarean with continued bleeding or Signs of concealed hemorrhage: VS abnormal or trending
(HR ≥ 110, BP ≤ 85/45, O2 sat < 95%, shock index 0.9) or Confusion
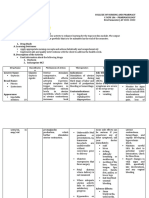
STAGE 1: Activate Hemorrhage Protocol
Clinical Trigger: CBL ≥ 500 mL vaginal / ≥ 1000 mL cesarean with continued bleeding or Signs of concealed
hemorrhage: VS abnormal or trending (HR ≥ 110, BP ≤ 85/45, O2 sat < 95%, shock index 0.9) or Confusion
MOBILIZE ACT THINK
Primary nurse, Physician or Primary nurse or designee: Consider
Midwife: Establish IV access if not present, at least 18 gauge potential
etiology:
Activate OB Increase IV oxytocin rate per hospital treatment guidelines
Hemorrhage Protocol • Uterine atony
Increase fluids
and Checklist • Trauma/laceration
Apply vigorous fundal/bi-manual massage
Primary nurse: • Retained placenta
Notify obstetrician or midwife • Amniotic fluid
MOVE ON to 2nd level uterotonic if no response (see Stage 2 meds below) embolism
(in-house and attending)
• Uterine inversion
Notify charge nurse Vital Signs, including O2 sat & level of consciousness (LOC) q5 minutes
• Coagulopathy
Notify anesthesiologist Record quantitative cumulative blood loss q5-15 minutes
• Placenta accreta
Secondary nurse: Administer oxygen to maintain O2 sat at > 95%
Convert to high risk
Assist primary nurse Empty bladder: straight catheter or place Foley with urometer and take appropriate
as needed or assign precautions. Consider
Convert to high risk: Type and Crossmatch for 2 units PRBCs STAT
staff member(s) to type and cross 2 units
(where clinically appropriate if not already done)
help PRBCs where clinically
Keep patient warm
appropriate if not
Physician or midwife: already done.
Bimanual massage
Once stabilized:
Careful inspection with good exposure: Rule out retained products Postpartum
of conception, laceration, hematoma management with
Surgeon (if intra-op) increased surveillance
and response readiness
Inspect for uncontrolled bleeding at all levels, esp. broad
assessment.
ligament, posterior uterus, and retained placenta
Triggers to Proceed to STAGE 2:
Continued bleeding w/ CBL < 1500 mL or VS remain abnormal
STAGE 2: Mobilize Team and Blood Bank Support
Clinical Trigger: Continued bleeding or Vital Sign instability, and < 1500 mL cumulative blood loss
MOBILIZE ACT THINK
Perform duties by ESTABLISH TEAM LEADERSHIP AND ASSIGN ROLES Sequentially advance through procedures and
assigned role: Administer 2nd level uterotonic medication: other interventions based on etiology:
Activate OB Rapid Methylergonovine 0.2 mg IM per protocol (if not hypertensive) Vaginal birth
Response Team: If hypertensive or Methylergonovine dose ineffective: carboprost 250 mcg IM
Can repeat carboprost up to 3 times every 20 If trauma (vaginal, cervical or uterine):
PHONE min (note: 75% respond to first dose) • Visualize and
#: Only If hypertensive and asthmatic: Misoprostol 800 mcg SL repair If retained
Continue IV oxytocin and provide additional IV crystalloid solution placenta:
Administer tranexamic acid (TXA) 1 gram IV over 10 minutes – may give a second dose of 1 gm if bleeding • D&C
If not included in OB RRT:
continues after 30 minutes or if bleeding stops and then restarts within 24 hours of completing the first If uterine atony or lower uterine segment
Call obstetrician or dose bleeding:
midwife to Team leader: • Intrauterine balloon
bedside Do not delay other interventions while waiting for response to medications (see right column - THINK) Intra-op C-section:
Call Anesthesiologist Order labs STAT (CBC/Plts, Chem 12 panel, Coag Panel II, ABG) • Uterine suture
Notify Perinatologist Bimanual uterine massage
Vaginal Delivery: Complete evaluation of vaginal wall, cervix, placenta, uterine cavity (if not already done) • Intrauterine balloon
or 2nd OB
Intra-op cesarean: Inspect for uncontrolled bleeding at all levels, esp. broad ligament, posterior uterus, • Uterine artery
Notify and retained placenta (if not already done) ligation If uterine
nursing Move to OR or location where higher level of care can be adequately provided inversion:
supervisor Order 2 units PRBCs and bring to the bedside - consider use of Emergency Release products (un-crossmatched) • Anesthesia and uterine relaxation drugs
Notify blood bank of Transfuse PRBCs based on clinical signs and response, do not wait for lab results; KEEP AHEAD for manual reduction
hemorrhage; order W/ VOLUME & BLOOD PRODUCTS If amniotic fluid embolism:
products as directed Primary nurse (or designee): • Maximally aggressive respiratory,
Bring hemorrhage Establish 2nd large bore IV, at least 18 gauge vasopressor and blood product
cart to the Assess and announce Vital Signs and quantitative cumulative blood loss q5-15 minutes support
patient’s location Set up blood administration set and blood warmer for transfusion
Administer meds, blood products and draw labs, as ordered If vital signs derangement inconsistent with
Initiate OB Keep patient warm measured blood loss consider concealed
hemorrhage record Second nurse: hemorrhage: lower uterine genital tract
scribing Obtain hemorrhage cart if not already in the room hematoma with extension; uterine rupture,
Assign single person Obtain portable light broad ligament laceration; or other source of
to communicate Place Foley with urometer (if not already done) internal bleeding; move to laparotomy.
with blood bank Obtain blood products from the blood bank (or send designee) Consider activating MTP if there is continued
Assign a family Assist with move to OR or higher level of care (if indicated) bleeding.
support Blood Bank: Once stabilized: Postpartum management with
person/medical social Prepare to activate massive transfusion protocol if needed increased surveillance and response readiness
worker per procedure assessment.
Re-Evaluate Bleeding and Vital Signs
Triggers to Proceed to STAGE 3:
Continued bleeding with CBL > 1500mL or > 2 units PRBCs given or abnormal VS or suspicion of DIC
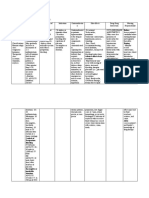
STAGE 3: Initiate Massive Transfusion Protocol & Surgical Approaches
Clinical Trigger: Continued bleeding with CBL > 1500mL or > 2 units PRBCs given or abnormal VS or suspicion of DIC
MOBILIZE ACT THINK
Perform duties by assigned Reidentify team leadership and micro brief Interventions based on etiology not yet completed
role: with additional team members Prevent hypothermia, acidemia
Activate Massive Team leader:
Transfusion Protocol Order Massive Transfusion Pack Conservative or Definitive Surgery:
(PRBCs + FFP + 1 pheresis pack Plts—see note in right • Uterine sutures
PHONE #: • Uterine artery ligation
column)
Ensure additional team experts Move to OR if not already there • Hysterectomy
available� Repeat CBC/Plts, Coag Panel II STAT and Chem 12 panel For Resuscitation:
Examples: q30- 60 min Aggressively Transfuse
Advanced Gyn surgeon Repeat ABGs
(e.g., Gyn Oncologist) Consider cell saver if preplanned or immediately Based on Vital Signs, Blood Loss
Second anesthesiologist available; notify transfusionist After the first 2 units of PRBCs use
Main OR staff Anesthesiologist (as indicated):
Adult intensivist Ongoing monitoring of VS and communication to team Near equal FFP and PRBC for
Supervisor, CNS, Arterial blood gases massive hemorrhage:
or manager Consider central hemodynamic monitoring 1 PRBC to 1 FFP
Reassign staff as needed CVP or PA line
If considering selective Arterial line 1 platelet apheresis pack per 4-6
embolization, call-in Vasopressor support units PRBCs
Interventional Radiology Intubation
team and second Calcium replacement If above measures unproductive:
Electrolyte monitoring
Interventional Radiology (IR) for selective
anesthesiologist
embolization as appropriate if patient stable
Blood Bank: Ensure large bore IV for transfusion
for transport and team immediately
Prepare to issue Primary nurse:
available -
additional blood Announce cumulative quantitative blood loss q5-10 minutes
products as needed in Apply upper body warming blanket
physician who is able to immediately call for
and move to surgery should be in house.
accordance with MTP – Use fluid warmer and/or rapid infuser for fluid &
stay ahead blood product administration Unresponsive Coagulopathy:
If patient at risk for Apply sequential compression stockings to lower • Role of rFactor VIIa is very
multiorgan failure or extremities controversial. After 8-10 units PRBCs
residual coagulopathy Circulate in OR and coagulation factor replacement
– contact ICU Second nurse and/or anesthesiologist: with ongoing hemorrhage, may
regarding transfer. Continue to administer meds, blood products and draw consider risk/benefit of rFactor VIIa in
Continue family support labs as ordered consultation with hematologist or
Third Nurse: trauma surgeon
Recorder Once Stabilized: Modified postpartum
management with increased surveillance;
consider ICU
Postpartum
If patient is:
Status post hemorrhage and at risk for multi-organ failure:
Admit to ICU or location for advanced care and continue MTP
Stable for transition to postpartum care after experiencing hemorrhage:
Perform risk assessment on transfer to postpartum care considering all prenatal, delivery and immediate postpartum factors
Provide increased surveillance and ensure adequate response readiness is in
place Stable for admission to postpartum post-delivery:
Perform risk assessment on transfer to postpartum care considering all prenatal, delivery and immediate postpartum factors
Provide routine care or increased surveillance and ensure adequate response readiness is in place based on risk assessment
BLOOD PRODUCTS
Packed Red Blood Cells (PRBC) Best first-line product for blood loss
Approx. 35-40 min. for crossmatch—once sample is in the lab and
1 unit = 200 mL volume
assuming no antibodies present
If antibody positive, may take hours to days for crossmatch. In some
cases, such as autoantibody crossmatch compatible may not be
possible. Use “least incompatible” in urgent situations.
Fresh Frozen Plasma (FFP) Highly desired if > 2 units PRBCs given, or for prolonged PT, PTT
Approx. 35-45 minutes to thaw for release
1 unit = 180 mL volume
Platelets (Plts) Priority for women with Platelets < 50,000
Local variation in time to release (may need to come from regional
Single-donor apheresis unit (= 6 units of platelet concentrates) provides
blood bank)
40-50,000 transient increase in platelets
Cryoprecipitate (Cryo) Priority for women with Fibrinogen levels < 80
Approx. 35-45 minutes to thaw for release
10-unit pack (or 1 adult dose) raises Fibrinogen 80-100 mg/dL
Best for DIC with low fibrinogen and where volume replacement is not
needed.
Caution: 10 units come from 10 different donors, so infection risk is
proportionate.
This table was adapted from the Improving Health Care Response to Obstetric Hemorrhage: A California Quality Improvement Toolkit, funded by the California Department of
Public Health, 2015; supported by Title V funds.
You might also like
- Obstetric Haemorrhage: EsmoeDocument40 pagesObstetric Haemorrhage: EsmoePoonam RanaNo ratings yet
- Haemorrhage ProtocolDocument1 pageHaemorrhage ProtocolHerwinda GeraldineNo ratings yet
- Eclampsia PPHDocument43 pagesEclampsia PPHizafamirna743No ratings yet
- Drug Study For OxytocinDocument2 pagesDrug Study For OxytocinAngelica CorpuzNo ratings yet
- 240 243Document5 pages240 243Rika WulandariNo ratings yet
- OxytocinDocument1 pageOxytocinIvanne Hisoler100% (7)
- Emergency Peripartum Hysterectomy As Life Saving Surgery For Postpartum Haemorrhage in Women With Single Kidney - A CaseReportDocument5 pagesEmergency Peripartum Hysterectomy As Life Saving Surgery For Postpartum Haemorrhage in Women With Single Kidney - A CaseReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Now, Try Some Big Leap.: Keep GoingDocument10 pagesNow, Try Some Big Leap.: Keep GoingCameron De GuzmanNo ratings yet
- NCP Alterations in Normal LaborDocument9 pagesNCP Alterations in Normal LaborCameron De GuzmanNo ratings yet
- Generic/ Brand Name Classification Mechanism of Action Indication Side Effects Nursing ImplicationsDocument14 pagesGeneric/ Brand Name Classification Mechanism of Action Indication Side Effects Nursing ImplicationsbokanegNo ratings yet
- Third Stage of Labor: by Feyisa T. (Obstetrician and Gynecologist)Document51 pagesThird Stage of Labor: by Feyisa T. (Obstetrician and Gynecologist)Haleluya LeulsegedNo ratings yet
- Obstetric HaemorrhageDocument34 pagesObstetric HaemorrhageKosie Soyama NambaNo ratings yet
- Inversion, Retained Placenta, AfeDocument95 pagesInversion, Retained Placenta, Afesushma sharmaNo ratings yet
- HemorrhageProtocol TableChart v1.4Document1 pageHemorrhageProtocol TableChart v1.4manleyj5305No ratings yet
- Post-Partum Hemorrhage (PPH) : 6/25/22 1 Fentahun ADocument30 pagesPost-Partum Hemorrhage (PPH) : 6/25/22 1 Fentahun ADani AsmareNo ratings yet
- GLM0021 Postpartum Haemorrhage PDFDocument15 pagesGLM0021 Postpartum Haemorrhage PDFRubiahSheBiachNo ratings yet
- Drug StudyDocument15 pagesDrug Studyjustine franchesca abonNo ratings yet
- Generic NameDocument3 pagesGeneric NameSittie Nashieva A. UsmanNo ratings yet
- NCP Example Pre EclampsiaDocument6 pagesNCP Example Pre EclampsiaChristian Joseph OpianaNo ratings yet
- Uerm Board Review - ObDocument15 pagesUerm Board Review - ObCamilla FernandezNo ratings yet
- Revised NCPDocument6 pagesRevised NCPTiffany AdriasNo ratings yet
- PPH ReportDocument22 pagesPPH ReportJose Bernel100% (1)
- Seminar 11 APH and PPHDocument61 pagesSeminar 11 APH and PPHIshak IzharNo ratings yet
- Stages of LabourDocument43 pagesStages of LabourhaisureshNo ratings yet
- Drug StudyDocument10 pagesDrug StudyFrancis BelotindosNo ratings yet
- OxytocinDocument2 pagesOxytocinshefawNo ratings yet
- WNHS Og AntepartumHaemorrhageDocument17 pagesWNHS Og AntepartumHaemorrhagelydia amaliaNo ratings yet
- Transes MidtermDocument16 pagesTranses MidtermDexter NicolasNo ratings yet
- Post Partum Hemorrhage (PPH) : Nasheel Kaur Gill Supervisor: DR KosillaDocument40 pagesPost Partum Hemorrhage (PPH) : Nasheel Kaur Gill Supervisor: DR KosillaHaziq MarsNo ratings yet
- Antepartum HaemorrhageDocument19 pagesAntepartum HaemorrhageKvy OngNo ratings yet
- OXYTOCIN-drug StudyDocument4 pagesOXYTOCIN-drug StudyCarissa Mae Tapec EstradaNo ratings yet
- Post-Partum Hemorrhage: DR - R Av Eendra MV DNB-FM 3 Year Resident de Pt. of Obg, Ci Hs RDocument30 pagesPost-Partum Hemorrhage: DR - R Av Eendra MV DNB-FM 3 Year Resident de Pt. of Obg, Ci Hs RRaveendra M.vNo ratings yet
- Drug Study (Oxytocin & HNBB)Document6 pagesDrug Study (Oxytocin & HNBB)NE TdrNo ratings yet
- 11 Drug StudyDocument13 pages11 Drug Studykwon nanaNo ratings yet
- OXYTOCINDocument3 pagesOXYTOCINJaye Aprile Adrianne KuizonNo ratings yet
- OBII - 14 Postpartum HemorrhageDocument8 pagesOBII - 14 Postpartum HemorrhageFelina CabadingNo ratings yet
- POSTPARTUM-HEMORRHAGE LecDocument13 pagesPOSTPARTUM-HEMORRHAGE LecMay MayNo ratings yet
- Post Partum HemorhageDocument7 pagesPost Partum HemorhageLithiya JoseNo ratings yet
- Complications of 3 Stage of Labour: Supervisor - Sas Dr. Mon Mon Khine Presenter - Hs Chan Bawm HszwekoooDocument48 pagesComplications of 3 Stage of Labour: Supervisor - Sas Dr. Mon Mon Khine Presenter - Hs Chan Bawm HszwekooozkoNo ratings yet
- Post Partum HemorrahgeDocument41 pagesPost Partum HemorrahgegibreilNo ratings yet
- Gyna ResearchDocument17 pagesGyna ResearchAya AnwerNo ratings yet
- Postpartum Hemorrhage (PPH) : Prakash Thakulla InternDocument38 pagesPostpartum Hemorrhage (PPH) : Prakash Thakulla InternPrakash ThakullaNo ratings yet
- Common Side Effects of Oxytocin Include:: CNS: Maternal: COMADocument3 pagesCommon Side Effects of Oxytocin Include:: CNS: Maternal: COMAann camposNo ratings yet
- Case:: Bleeding Without PainDocument3 pagesCase:: Bleeding Without PainDarwin QuirimitNo ratings yet
- Case Study 29-APHDocument31 pagesCase Study 29-APHZarul Naim Mohd TamiziNo ratings yet
- RetainedDocument2 pagesRetainedSeptian TheaNo ratings yet
- DR Drug Study: 401 2nd SemDocument2 pagesDR Drug Study: 401 2nd SemHazel Grace AhitoNo ratings yet
- MOH Pocket Manual in Obstetrics and GynaecologyDocument194 pagesMOH Pocket Manual in Obstetrics and GynaecologyBea SamonteNo ratings yet
- Obstructed Labour and The Partogram: EsmoeDocument89 pagesObstructed Labour and The Partogram: EsmoeLana LocoNo ratings yet
- Maternal Ncps FinalDocument33 pagesMaternal Ncps FinalCarey Jamille YadanNo ratings yet
- Drug Name Classificatio N Mechanism of Action Therapeutics Effects Nursing ConsiderationsDocument7 pagesDrug Name Classificatio N Mechanism of Action Therapeutics Effects Nursing ConsiderationsHaleNo ratings yet
- PHINMA Education Network College of Health SciencesDocument2 pagesPHINMA Education Network College of Health SciencesJozarine ChelseaNo ratings yet
- Postpartum HaemorrhageDocument26 pagesPostpartum HaemorrhagePriyanka ViswanathNo ratings yet
- Postpatum Obstetric EmergenciesDocument46 pagesPostpatum Obstetric EmergenciesSooryaNo ratings yet
- Pregnancy Trauma NotesDocument8 pagesPregnancy Trauma NotesHisham FahadNo ratings yet
- Oxytocin Induction or Stimulation of Labor BeforeDocument4 pagesOxytocin Induction or Stimulation of Labor BeforeIrene Grace BalcuevaNo ratings yet
- 36 PPHDocument12 pages36 PPHRisqi YuliNo ratings yet
- Hemorrhage Scenario (Helen) - JinangDocument3 pagesHemorrhage Scenario (Helen) - JinangKian Bryne Peña JinangNo ratings yet