Professional Documents
Culture Documents
Communicable Disease
Uploaded by
Vince0 ratings0% found this document useful (0 votes)
31 views5 pagesOriginal Title
communicable disease.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
31 views5 pagesCommunicable Disease
Uploaded by
VinceCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
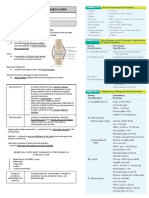
COMMUNICABLE DISEASES
COMMUNICABLE DISEASE o Warm baths – causes bronchodilation
Infectious – “Prolonged” contact/exposure DIPHTHERIA
Contagious – “Easily” Transmitted Incubation Period (IP): 1-5 days
Epidemiology – Study of disease condition occurrence CA: Corynebacterium Diphtheriae
(geographical area) MOT: Direct contact, Soiled article (Fomite)
Sporadic – Rare, Few cases, Isolated Pathognomonic Sign – Pseudomembranes
Ex. Leprosy, Lime’s Disease, Elephantiasis Types of Diphtheria
Endemic – Constant, Common Nasal – white membranes on nasal septum
Ex. Coughs, Cold, Flu Nasopharyngeal – Bull’s neck; Dangerous (closure of
Epidemic – Outbreak - Sudden inflation in cases, airway)
more than 50% of previous case Cutaneous – yellow spots in Skin
Ex. Dengue during rainy season Medical Management:
Pandemic – Worldwide: several countries o Penicillin
Ex. Covid-19, Tuberculosis, HIV o Diphtheria Antitoxins: Modified bacteria ->
Chain of Infection (SHARE ME) stimulates immune response
Susceptible Host - Human o Ice collar -> decrease pain on neck area
Agent – Causative agent (bacteria, virus, spore, o Oxygen inhalation
fungi, protozoa) o Bedrest
Reservoir – Home of agent o WOF: Closure of airway ->Bedside Tracheostomy
Exit Nursing Management:
Mode of Transmission – weakest link -> o Absolute bedrest for 2 weeks
Handwashing, PPE o Avoid Valsalva maneuver -> may cause rupture of
Entry pseudomembranes
PERTUSSIS (Whooping Cough) o Soft Diet
- Bronchoconstriction -> mucus secretions
o Vit. C -> enhance tissue repair
Incubation Period (IP): 7-14 days
Causative Agent: Bordetella Pertussis
MEASLES (Rubeola/Morbilli/Tigdas)
MOT: Droplet and Direct Contact
Measles – Rubeola
Sign and Symptoms:
German Measles – Rubella
1. Catarrhal Stage: Not full blown
Incubation Period (IP): 2 weeks
Most contagious stage
CA: Rubeola Virus
Stage of increase communicability
MOT: Airborne (>3ft) and Droplet (<3ft)
Flu-like symptoms (Cough, colds, body malaise)
Pathognomonic Sign – Koplik’s Spots: Inflammatory
2. Paroxysmal Stage:
lesions in buccal mucosa
Hallmark: Paroxysms of cough
Sign and Symptoms:
3. Convalescent Stage: (Recovery stage)
1. Pre-eruptive (Catarrhal symptoms)
Recovery and healing
- Cough, Coryza (Rhinitis), Conjunctivitis ->
Medical Management:
Photophobia (Use dark-colored glasses/large brim
o Oxygen Therapy
hats/sunvisors)
o Fluid and Electrolyte Replacement
2. Eruptive
o Erythromycin and Ampicillin (Finish duration -> to Maculopapular rash, Intermittent fever
prevent drug resistance) 3. Convalescent Stage: (Recovery stage)
o Bedrest (Hastens recovery) - Symptoms will subside
o Gammaglobulins – enhances/activates immune Medical Management:
system -> Increase immune response. o Anti-viral: IsoPRINOsine
Nursing Management: o Antibiotics: Penicillin ->with complication
o Isolate the patient o Oxygen
Isolation – Communicable Disease o IV Fluids
Reverse Isolation - Immunocompromised Nursing Management:
o Medical Asepsis o Isolation
o Suction Machine o Quiet room/dim lights (reduce stimuli)
o Sunshine – enhances metabolism o TSB (Tepid Sponge Bath) -> Dec Fever
o Fresh air – enhances oxygenation o Bed Bath
COMMUNICABLE DISEASES
o Increase OFI o Use mitten in children
o MMR, Anti-measles vaccine
GERMAN MEASLES (RUBELLA/3 DAY)
Incubation Period (IP): 14-21 days FILARIASIS (Elephantiasis)
CA: Rubella Virus Incubation Period (IP): up to 82 days
MOT: Airborne, Droplet, Transplacental -> congenital CA: Wuchereria bancrofti
heart defects MOT: Mosquito Bite: Aedes Poecillus
Pathognomonic Sign – Forscheimer’s spots: pink rash Pathognomonic Sign – Elephantiasis
on soft palate (Diff of swallowing) Sign and Symptoms:
Sign and Symptoms: - Elephantiasis
1. Prodromal Stage: - Headache
- Low grade fever, Mild coryza, Lymphadenopathy - Chills and fever
2. Eruptive - s/Sx of inflammation: Rubor(Redness), Calor(heat),
Forscheimers, Testicular pain, polyarthralgia Tumor(Swelling), Dolor(pain) in arms, legs and
3. Convalescent Stage: (Recovery stage) scrotum
Medical Management: Diagnostics
o Symptomatic - Circulating filarial Antigen: Finger prick
Nursing Management: Medical Management:
o Isolation o DOC: Hetrazan
o Quiet room/dim lights (reduce stimuli) o Surgery for scrotal enlargement
o Mild liquid diet (nourishing diet) o Decreased Fortified salt
o Good ventilation Nursing Management:
o MMR o Sleep under mosquito nets
o Immune serum globulin: (+) exposure o Use mosquito repellants (OFF Lotion)
CHICKENPOX (Varicella) DENGUE
- Fluid-filled pus vesicles Dengue Fever
Incubation Period (IP): 14-21 days - A.K.A Breakbone fever, Dandy Fever, Infectious
CA: Herpesvirus varicellae Thrombocytopenic Purpura
MOT: Direct and Fomites (Highly communicable) Dengue Hemorrhagic Fever
Sign and Symptoms: - Bleeding and Hypovolemic shock
- Rash -> unexposed part: trunk area Dengue Shock Syndrome
- Macule -> Papule -> vesicle (fluid-filled) -> pustule - Most lethal –> profound shock
(pus-filled) -> Crust Incubation Period (IP): 3-14days (2 weeks)
- Celestial maps -> scabs -> Crust CA: Flaviviruses/Arboviruses
Medical Management: Reservoir: Mosquitoes (Aedes Aegypti), Humans
o Anti-viral: ZOverax/Acyclovir MOT: Blood Meal/Mosquito Bite
o Antihistamines Pathognomonic Sign – Herman’s Sign (Skin appears
o Calamine Lotion purple, Fragile capillaries)
o No to Salicylates ( CP + Aspirin = Reye’s Syndrome)
-> Dec blood sugar level, Inc blood acidity and Diagnostic Procedure:
ammonia o Rumpel Leed test/ Tourniquet test
o Antipyretics Criteria:
Salicylates (ASA) - 6 months or older
Antiplatelet - Fever for 3 days or more
Antipyretic - No signs of hemorrhagic fever
Analgesic - Presumptive screening test
Anti-inflammatory effect - BP cuff -> pressure midway D/S (applied to
Side effect: Bleeding elbow for about 5mins)
Nursing Management: - Count petechiae in antecubital fossa
o Respiratory Isolation until all vesicles have crusted (>10/square inch)
o Disinfect linens under sunlight/boiling o Platelet count (Decreased) - confirmatory
o Cut fingernails o Dengue Spot test – detection of IgG and IgM
antibodies to dengue virus
COMMUNICABLE DISEASES
o Dengue Ns1 -detection of dengue antigen - Cercum ova precipitin test - confirmatory
o Dengue Duo – Dengue Spot test + Dengue Ns1 Medical Management:
o Praziquantel for 6 months
Sign and Symptoms:
Dengue fever: Nursing Management:
- Sudden onset of fever (39-40 C), chills and o Reduce snail density
convulsions - expose to sunlight
- Frontal headache, ocular pain, myalgia, arthralgia - remove weeds
- Malaise and anorexia, Headache - Proper irrigation
- Rash: Maculopapular rash - Prevent bathing on snail infested areas
- Abdominal pain and tenderness: hepatic
Dengue Hemorrhagic fever: RABIES
- Result of 2nd dengue infection - A.K.A Lyssa/Hydrophobia
- Hemorrhagic manifestation Incubation Period (IP): 2 weeks
Epistaxis Ecchymosis CA: Rhabdovirus/Rhabdoviridae-> rhabdo(bullet) –>
Hematemesis Hematochezia (fresh) Melena (dry BBB (Blood-Brain Barrier)
blood) Herman sign Sign and Symptoms:
Prodromal/Invasion
WHO DHF Grading Scale: - Salivation, Irritability, pain on bite site
Grade I: No shock, (+) tourniquet test Excitement/Neurological
Grade II: GI + Spontaneous bleeding - Excitation and Apprehension
Grade III: Shock - Nuchal Rigidity, Twitching
Grade IV: Profound Shock, Unmeasurable BP - Aerophobia/Hydrophobia
Complications: Terminal/Paralytic
- Dengue Encephalopathy -> CNS -> ALOC - Repiratory depression, Paralysis
Medical Management: Medical Management:
o Analgesics except aspirin o Tetanus Toxoid
o Blood transfusion o Anti-rabies serum/vaccine
o Oxygen Therapy Nursing Management:
o Sedatives (Anxiety and Apprehension) o Isolation
Nursing Management: o Darken the room
o Recognize Defervescence period (fever has o No water on site
subsided) -> Critical period -> rapid deterioration o IVF: wrapped securely include IV tubing
(24-48 hours) o Vaccination of all dogs
o Placed in mosquito free environment o Confine dog for 10-14 days
o Monitor V/S, Prevent Bleeding o Cut the head of the dog -> place it on ice container
o Soft & Bland diet (EDCF) > negri bodies(fluorescent test)
Tawa-tawa: Promotes cell production and prevent
platelet destruction PULMONARY TUBERCULOSIS (PTB)
CA: Mycobacterium tuberculosis
SCHISTOSOMIASIS MOT: Airborne, Droplet, Indirect (Fomites)
- A.K.A Bilharziasis/Snail Fever Pathognomonic sign: Hemoptysis
Incubation Period (IP): 14-82 days Manifestations:
CA: Schistosoma Japonicum (Phil) Asymptomatic Initially
MOT: Ingestion of infected H20, Skin pores
Vector: Oncomelania quadrasi Classifications:
Pathognomonic Sign – Swimmer’s Itch, Class I – No exposure, No infection
Jaundice Class II – Exposure, No infection
Sign and Symptoms: Class III – Infection, No disease
- Swimmer’s itch - (+) PPD but no clinical evidence of active TB
- Bloody mucoid stool Class IV – Disease, not clinically active
- Liver problems -> Jaundice/Icteric Class V – Suspected, Diagnosis pending
Diagnostics
COMMUNICABLE DISEASES
Diagnostics: C Post-Transfusion
o Sputum Exam – 3 consecutive (+) result D Delta Agent
o Chest X-ray – nodules, cavities E Enteric
o Purified Protein Derivative (PPD) – Tuberculin
F Hypothetical
Test/Mantoux Test (Exposure only)
G No Human Illness
Medical Management: Multi-Drug Therapy
o Rifampicin Onset:
o Isoniazid o Acute – Hepatitis A and E
o Pyrazinamide o Chronic – Hepatitis B and C
o Ethambutol Stages:
o Streptomycin Pre-Icteric Stage
Take on an empty stomach Fatigue Nausea, Vomiting, Anorexia
No longer contagious after 2-3 weeks of MDT and 2 Icteric Stage
(-) sputum result Jaundice, Dark urine, Acholic stool (Lack of bile)
Nursing Management: Post-Icteric Stage
o Adequate rest
o Proper nutrition – Increase CHON, Vitamin C SEXUALLY TRANSMITTED DISEASE
SYPHYLIS
o Religious intake of medications
C.A. – Treponema Pallidum
o Semi-fowler’s Position
MOT – Intimate contact
o Primary prevention
Sources of infection:
o BCG, Public education about MOT, environmental
– Discharges, Semen, Surface lesions
sanitation
Manifestations:
Prevention of Spread
Primary Syphilis: Chancres - painless raised lesions
o N95 mask worn by HCP
Secondary Syphilis: Condylomata lata – pink or
o Face mask worn by patient
grayish white lesions
o Isolation Latent syphilis: Asymptomatic
o Handwashing Late syphilis: Gumma – deep, single, painless
o Proper disposal of secretions asymmetrical lesion
Medical Management:
DENGUE AND MALARIA o Penicillin
DENGUE MALARIA o Tetracycline
Flavivirus Plasmodium Nursing Management:
(Chikungunya and ovale, Vivax,
Causative Agent o Stress importance of continuing treatment
Onyongyong virus) Malarae,
Falciparum o Partners should be tested
Aedis Aegypti Aedis Poecilus o Universal precaution
D – ay biting N – ight biting o Keep lesion dry
L – ow flying H – igh flying
Vector GENITAL HERPES
S - tagnant F - lowing
U - rban R – ural C.A. – Herpes simplex virus
Problem Low Platelet Low RBC MOT – intimate contact
Bleeding Bleeding Manifestations:
Manifestations tendencies tendencies and o Genital sores
Anemia
o Painful sores
Symptomatic Symptomatic
Platelet Transfusion of o Fever
Transfusion RBC o Muscular pain
Management - Fresh frozen - Packed RBC o Burning sensation on urination
plasma
Medical Management: Acyclovir
- Platelet
Nursing Management: Personal hygiene
GONORRHEA
HEPATITIS
C.A. – Neisseria gonorrheae
TYPES AKA MOT
A Infectious Hepa MOT – intimate contact
Manifestations:
B Serum Hepa
Female
COMMUNICABLE DISEASES
- Burning and frequent urination o Liver, Spleen, Kidney, Brain, Peritoneum,
- Yellow vaginal discharge Testis/ovary, Spinal cord
Males Manifestations:
- Dysuria with pus - diarrhea, abdominal pain, fever, cough, urticaria,
- Rectal infection for homosexuals hepatosplenomegaly, pulmonary abnormalities
- prostatitis Medical Management
Medical Management - Praziquantel
o Ceftriaxone Nursing Management
o Penicillin - avoid eating raw or undercooked freshwater crabs
o Infants born to mother with gonorrhea – give 1% and crayfish from endemic waters
silver nitrate
Nursing Management TAENIA SAGINATA
o All info about patient is confidential Reservoir – cattle
o Isolation MOT – fecal-oral
o Sex education Manifestations:
o Contact Tracing o Asymptomatic
CHLAMYDIA o weight loss, dizziness, abdominal pain
C.A. – Chlamydia trichomatis o Diarrhea
MOT – vaginal and rectal intercourse o Chronic indigestion
Manifestations: Medical Management
o Cervicitis - Praziquantel
o Dyspareunia - Niclosamide
o Dysuria Nursing Management
o Pyuria - avoid eating raw or undercooked cattle
o Scrotal swelling HOOKWORM
o Tenesmus Reservoir – mammales (dogs, cats)
Medical Management MOT – fecal-oral
o Doxycycline x 7 days Manifestations:
o Ground itch
o Azithromycin x 1 dose
o Epigastric pains
Nursing Management
o Universal precaution o Indigestion
o Suggest both partners submit to HIV testing o nausea
TRICHOMONIASIS o Vomiting
C.A. – Trichomonas vaginalis o constipation
MOT – STD o diarrhea
Manifestations: Medical Management
o Cervicitis - Albendazole
o Vaginitis - Iron, folic acid, Vit B12 – for anemia
o Urethritis Nursing Management
o Dyspareunia - sanitation
o Dysuria
Medical Management: Metronidazole
Nursing Management
o Universal precaution
o Practicing safe sex
PARASITISMS
PARAGONIMIASIS
C.A. – Lung fluke – Paragonimus westermani
Reservoir - seafoods
MOT – fecal-oral
o Eggs may circulate to following sites:
You might also like
- CLINICAL Assigmnent 1 PDFDocument12 pagesCLINICAL Assigmnent 1 PDFChelly ClarkeNo ratings yet
- Mental Health Nursing Case Study - CompleteDocument12 pagesMental Health Nursing Case Study - Completeapi-546486919No ratings yet
- Nursing CS CroupDocument1 pageNursing CS Croupreuben kadarajaNo ratings yet
- Fundamentals of Nursing ReviewerDocument9 pagesFundamentals of Nursing Reviewerchie9268No ratings yet
- Literature Review On Secondhand SmokeDocument6 pagesLiterature Review On Secondhand Smokeapi-519859495No ratings yet
- Finals Reviewer and Activities NCM 116 LecDocument24 pagesFinals Reviewer and Activities NCM 116 LecMary CruzNo ratings yet
- Module 3 Nursing Skills Procedure On GI, Endo-Metab Concept (A)Document18 pagesModule 3 Nursing Skills Procedure On GI, Endo-Metab Concept (A)Nashebah A. BatuganNo ratings yet
- Understanding Eye Anatomy and Common Eye DisordersDocument174 pagesUnderstanding Eye Anatomy and Common Eye DisordersroseNo ratings yet
- AUBF Synovial FluidDocument6 pagesAUBF Synovial FluidRichelyn Grace B. VenusNo ratings yet
- MS LecDocument15 pagesMS LecAngel YN Patricio FlorentinoNo ratings yet
- Fluids and Renal DisorderDocument139 pagesFluids and Renal DisorderLhara MañoNo ratings yet
- Dams - DVT (New)Document48 pagesDams - DVT (New)Msd KishorNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- Relevance of Laboratory On Teaching of Int - ScienceDocument83 pagesRelevance of Laboratory On Teaching of Int - ScienceAdemolaNo ratings yet
- Pediatrics Lecture on Malnutrition Criteria and InterventionsDocument8 pagesPediatrics Lecture on Malnutrition Criteria and InterventionskrishNo ratings yet
- Medical-Surgical Nursing ArthritisDocument8 pagesMedical-Surgical Nursing ArthritisNoelyn BaluyanNo ratings yet
- Metabolic DisturbancesDocument34 pagesMetabolic DisturbancesKyle DapulagNo ratings yet
- Health Assessment Inspection and Palpation FindingsDocument7 pagesHealth Assessment Inspection and Palpation FindingsJa DimasNo ratings yet
- Pediatric Nursing CA Sir Archie Alviz 04-09-2022Document3 pagesPediatric Nursing CA Sir Archie Alviz 04-09-2022Jonah MaasinNo ratings yet
- PEDIA Handouts 2010Document17 pagesPEDIA Handouts 2010Jannine Marie EmpasisNo ratings yet
- Ortho Supplemental NotesDocument6 pagesOrtho Supplemental Notestanya merdeNo ratings yet
- PEDIA Review TransesDocument12 pagesPEDIA Review TransesJennie KimNo ratings yet
- Medical Concept Mapping Type 2 DiabetesDocument1 pageMedical Concept Mapping Type 2 DiabetesRENEROSE TORRESNo ratings yet
- Notes I III Life Threatening ConditionsDocument5 pagesNotes I III Life Threatening ConditionsFaye MontenegroNo ratings yet
- Endocrine Focus PointsDocument10 pagesEndocrine Focus PointsHayden ShulerNo ratings yet
- Common Ent EmergenciesDocument65 pagesCommon Ent EmergenciesferaNo ratings yet
- Types of Arthritis: SOLOMON SALLFORSDocument3 pagesTypes of Arthritis: SOLOMON SALLFORSSolomon Seth SallforsNo ratings yet
- Important Points To Diagnose Scenarios of OphthalmologyDocument57 pagesImportant Points To Diagnose Scenarios of OphthalmologyHadra NuviNo ratings yet
- AsthmaDocument35 pagesAsthmakarthikeyan rajeevNo ratings yet
- MS Eent (Nle)Document3 pagesMS Eent (Nle)Maginalyn CangasNo ratings yet
- UPump Pediatric NursingDocument21 pagesUPump Pediatric NursingJan Leslie VergaraNo ratings yet
- Set Ea505092Document3 pagesSet Ea505092davidvpnNo ratings yet
- Week 11 - Vision Hearing Communication - 20171106Document33 pagesWeek 11 - Vision Hearing Communication - 20171106hkdawnwongNo ratings yet
- Requirement in PathophysiologyDocument38 pagesRequirement in PathophysiologyckathreenahNo ratings yet
- 312 MidDocument60 pages312 MidVALERIANO TRISHANo ratings yet
- Chapter 10: Muscle Tissue: VoluntaryDocument13 pagesChapter 10: Muscle Tissue: VoluntaryClyde BaltazarNo ratings yet
- NLM ReviewerDocument32 pagesNLM ReviewerAmber BlodduweddNo ratings yet
- Part 1 LeadershipDocument5 pagesPart 1 LeadershipHoloNo ratings yet
- Nur 111 Session 17 Sas 1Document8 pagesNur 111 Session 17 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Rhu d1 Compiled December LatestDocument169 pagesRhu d1 Compiled December LatestDilausan B MolukNo ratings yet
- Hansens DiseaseDocument83 pagesHansens DiseaseSajin AlexanderNo ratings yet
- LRTIDocument13 pagesLRTIRomina Mae FajardoNo ratings yet
- Pnle Medical Surgical ReviewDocument17 pagesPnle Medical Surgical ReviewKyla Rose ToledoNo ratings yet
- Amoebiasis: An Overview of Its Causes, Symptoms, Diagnosis and TreatmentDocument8 pagesAmoebiasis: An Overview of Its Causes, Symptoms, Diagnosis and TreatmentCheska ت HortelanoNo ratings yet
- Microbiology NotesDocument13 pagesMicrobiology NotesMalekNo ratings yet
- Ate Hidj PLE TipsDocument2 pagesAte Hidj PLE TipsAmal RangirisNo ratings yet
- UE 1 Clavicle FracturesDocument46 pagesUE 1 Clavicle FracturesDavidBeatonComuladaNo ratings yet
- Communicable Disease Nursing GuideDocument14 pagesCommunicable Disease Nursing GuideFrancis Alfred EscaranNo ratings yet
- Pediatric NursingDocument6 pagesPediatric NursingViktoria Leeahna LehNo ratings yet
- Pedia S1Document22 pagesPedia S1betweenNo ratings yet
- Med Surge 4Document28 pagesMed Surge 4rave andrei MacanayaNo ratings yet
- Leprosy: Hansen'S Disease/HansenosisDocument31 pagesLeprosy: Hansen'S Disease/Hansenosislyka resurreccionNo ratings yet
- Nasopharyngeal + Oropharyngeal Swab Inconclusive Inconclusive Inconclusive For Sars-Cov-2 Needs Clinical Correlation, Follow Up & Repeat If Required.Document1 pageNasopharyngeal + Oropharyngeal Swab Inconclusive Inconclusive Inconclusive For Sars-Cov-2 Needs Clinical Correlation, Follow Up & Repeat If Required.Kartik ShuklaNo ratings yet
- Communicable Disease NursingDocument22 pagesCommunicable Disease NursingNur SanaaniNo ratings yet
- Cardiovascular Disorders: Coronary AtherosclerosisDocument6 pagesCardiovascular Disorders: Coronary AtherosclerosisHazel BandayNo ratings yet
- Nursing Care of Clients With Upper Airway or Respiratory DisordersDocument6 pagesNursing Care of Clients With Upper Airway or Respiratory DisordersLuna MarieNo ratings yet
- Perioperative Nursing ManagementDocument19 pagesPerioperative Nursing ManagementSarah SeverreNo ratings yet
- God is Our Refuge in TroubleDocument3 pagesGod is Our Refuge in TroubleMaginalyn CangasNo ratings yet
- Nursing Fundamentals Refresher Post-Test ReviewDocument3 pagesNursing Fundamentals Refresher Post-Test ReviewBRYAN PINGOLNo ratings yet
- Neurology 4 PDF-mergedDocument358 pagesNeurology 4 PDF-mergedAnuraag YadavNo ratings yet
- MSN Communicable DiseaseDocument29 pagesMSN Communicable DiseaseLuis LazaroNo ratings yet
- Communicable Diseases: InfectiousDocument4 pagesCommunicable Diseases: InfectiousRichmond Catchillar BonusNo ratings yet
- Bovine Ephemeral Fever: ImportanceDocument4 pagesBovine Ephemeral Fever: ImportanceAamir AliNo ratings yet
- Comparative Single-Dose Pharmacokinetics of Amantadine Hydrochloride and Rimantadine Hydrochloride in Elderly AdultsDocument6 pagesComparative Single-Dose Pharmacokinetics of Amantadine Hydrochloride and Rimantadine Hydrochloride in Elderly AdultsLety LagunaNo ratings yet
- Nasolacrimal Obstruction Caused by Root Abscess of The Upper Canine InacatDocument4 pagesNasolacrimal Obstruction Caused by Root Abscess of The Upper Canine InacatIngrid MachadoNo ratings yet
- Session 6 - Performing Abdominal ExaminationDocument33 pagesSession 6 - Performing Abdominal ExaminationOtsward OwdenNo ratings yet
- Biology Notes CHPTR 12Document14 pagesBiology Notes CHPTR 12Wan HasliraNo ratings yet
- 0 Stroke Rehabilitation by Richard Wilson and Preeti Raghavan 2019 PDFDocument295 pages0 Stroke Rehabilitation by Richard Wilson and Preeti Raghavan 2019 PDFDiana MesquitaNo ratings yet
- Physical Education H.O.P.E 1 Module 6Document17 pagesPhysical Education H.O.P.E 1 Module 6Reynaldo Jr LundagNo ratings yet
- Heart Failure Types: Right vs Left Sided and Systolic vs DiastolicDocument3 pagesHeart Failure Types: Right vs Left Sided and Systolic vs DiastolicKryffa DegayNo ratings yet
- Anesthesia For Patients With Diabetes Mellitus - UpToDateDocument31 pagesAnesthesia For Patients With Diabetes Mellitus - UpToDateEduardoNo ratings yet
- Schizophrenia Spectrum and Other Psychotic DisordersDocument8 pagesSchizophrenia Spectrum and Other Psychotic DisordersRain Simonette GuanNo ratings yet
- Choosing Wisely Canada PDFDocument152 pagesChoosing Wisely Canada PDFaayceeNo ratings yet
- Viruses Bacteria Protists and FungiDocument63 pagesViruses Bacteria Protists and Fungim umair zahirNo ratings yet
- CASE STUDY (Gastro)Document3 pagesCASE STUDY (Gastro)Jake Yvan DizonNo ratings yet
- 19mbm003 Aiswarya Lakshmi Thakka Ravunni Y - 12798 - Assignsubmission - File - Mip-19mbm003, Aiswarya Lakshmi Thakka Ravunniy-SignedDocument21 pages19mbm003 Aiswarya Lakshmi Thakka Ravunni Y - 12798 - Assignsubmission - File - Mip-19mbm003, Aiswarya Lakshmi Thakka Ravunniy-SignedVadivelNo ratings yet
- SAPOTA: Nature's Superfruit with 16 Health BenefitsDocument1 pageSAPOTA: Nature's Superfruit with 16 Health Benefitsprof renanNo ratings yet
- N O Judul Penulis Tahu N Abstrak 1Document8 pagesN O Judul Penulis Tahu N Abstrak 1riskyameliaNo ratings yet
- JC BdiDocument36 pagesJC BdiArisa KudidthalertNo ratings yet
- Time TableDocument28 pagesTime TablePetWise Animal ClinicNo ratings yet
- Medical Surgical Questions LiverDocument17 pagesMedical Surgical Questions LiverHasan A AsFourNo ratings yet
- Passed Like A ShadowDocument15 pagesPassed Like A ShadowTimoNo ratings yet
- A Neuro-Heuristic Approach For Recognition of Lung Diseases From X-RayDocument15 pagesA Neuro-Heuristic Approach For Recognition of Lung Diseases From X-RaySarah NixonNo ratings yet
- Form C AuthorizationRequestForm PDFDocument4 pagesForm C AuthorizationRequestForm PDFKalaimani SNo ratings yet
- FERENAL, CLS Dummy ChartDocument4 pagesFERENAL, CLS Dummy ChartChristine Lorraine FerenalNo ratings yet
- Oscillococcinum for InfluenzaDocument5 pagesOscillococcinum for InfluenzaDeepak KumarNo ratings yet
- Leg Length Discrepancy (LLD) : H Fcmaf PM Ambcare AMB P AGE OFDocument1 pageLeg Length Discrepancy (LLD) : H Fcmaf PM Ambcare AMB P AGE OFanuragNo ratings yet
- ABIS HSE L4 F 01 Risk Assessment FormDocument61 pagesABIS HSE L4 F 01 Risk Assessment FormOvais FarooqNo ratings yet
- SCORE Project Form Internal Medicine DepartmentDocument7 pagesSCORE Project Form Internal Medicine DepartmentGeorge CobuzNo ratings yet
- Grade Level: Grade 4 Subject: Health Quarter Content Standards Performance Standards Most Essential Learning Competencies Duration K To 12 CG CodeDocument3 pagesGrade Level: Grade 4 Subject: Health Quarter Content Standards Performance Standards Most Essential Learning Competencies Duration K To 12 CG CodeHamizha Zhamyrra Santillana-MamaNo ratings yet