Professional Documents
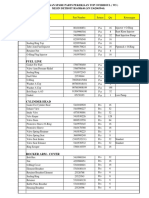
Culture Documents
A Pilot Study of Surgical Training Using A Virtual Robotic Surgery Simulator
Uploaded by
Eham AroraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Pilot Study of Surgical Training Using A Virtual Robotic Surgery Simulator
Uploaded by
Eham AroraCopyright:
Available Formats
SCIENTIFIC PAPER
A Pilot Study of Surgical Training Using a Virtual
Robotic Surgery Simulator
Ana I. Tergas, MD, MPH, Sangini B. Sheth, MD, MPH, Isabel C. Green, MD,
Robert L. Giuntoli II, MD, Abigail D. Winder, MD, Amanda N. Fader, MD
ABSTRACT tual reality simulator. Benefits unique to the simulator
platform include autonomy of use, computerized perfor-
Background and Objectives: Our objectives were to mance feedback, and ease of setup. These features may
compare the utility of learning a suturing task on the facilitate more efficient and sophisticated simulation train-
virtual reality da Vinci Skills Simulator versus the da Vinci ing above that of the conventional dry laboratory plat-
Surgical System dry laboratory platform and to assess user form, without loss of efficacy.
satisfaction among novice robotic surgeons.
Key Words: Robotic surgery, Surgical education, Surgical
Methods: Medical trainees were enrolled prospectively; simulator training, Robotics, Computer simulation, Surgi-
one group trained on the virtual reality simulator, and the cal procedures, Minimally invasive/education, Gyneco-
other group trained on the da Vinci dry laboratory plat- logic surgery.
form. Trainees received pretesting and post-testing on the
dry laboratory platform. Participants then completed an
anonymous online user experience and satisfaction sur-
vey.
Results: We enrolled 20 participants. Mean pretest com- INTRODUCTION
pletion times did not significantly differ between the 2 Recent advancements in surgical technology, including
groups. Training with either platform was associated with the introduction of robotic-assisted laparoscopic surgery,
a similar decrease in mean time to completion (simulator afford gynecologists the ability to treat an increasing num-
platform group, 64.9 seconds [P ⫽ .04]; dry laboratory ber of patients with minimally invasive surgical approaches.
platform group, 63.9 seconds [P ⬍ .01]). Most participants Robotic-assisted laparoscopic surgery has emerged as an
(58%) preferred the virtual reality platform. The majority essential minimally invasive technology with several pur-
found the training “definitely useful” in improving robotic ported advantages over conventional laparoscopic sur-
surgical skills (mean, 4.6) and would attend future training gery.1– 4 Published reports suggest that robotic surgery may
sessions (mean, 4.5). allow more surgeons to perform complex gynecologic pro-
Conclusion: Training on the virtual reality robotic simu- cedures and may lead to improved patient outcomes com-
lator or the dry laboratory robotic surgery platform re- pared with conventional laparoscopy or laparotomy.5– 8
sulted in significant improvements in time to completion Adoption of this surgical approach is rising rapidly, with
and economy of motion for novice robotic surgeons. Al- almost 50% of US robotic procedures performed by gyne-
though there was a perception that both simulators im- cologists.9,10 Given the relative merits of robotic surgery and
proved performance, there was a preference for the vir- its widespread adoption, it is paramount that gynecology
residency and fellowship programs offer comprehensive
training in this modality for their trainees.11
Department of Gynecology and Obstetrics, Johns Hopkins Medical Institutions,
Baltimore, MD, USA (Drs. Tergas, Sheth, Green, Giuntoli, Winder, Fader). In a recent survey of US obstetrics and gynecology resi-
Department of Obstetrics and Gynecology, Section of Gynecologic Oncology, dency program directors, most believed the use of robotic
Greater Baltimore Medical Center, Baltimore, MD, USA (Drs. Tergas, Sheth, Winder, surgery would increase and play a more integral role in
Fader).
gynecologic surgery.12 However, the question of how to
Accepted for an oral poster presentation at the 38th Annual Society for Gynecologic best introduce new surgical technology in the operating
Surgeons Scientific Meeting; Baltimore, MD, April 14, 2012.
room and safely instruct novice surgeons is challenging.
Address correspondence to: Amanda N. Fader, MD, Department of Gynecology
and Obstetrics, Johns Hopkins, Hospital, 600 N. Wolfe St, Phipps 287, Baltimore,
Other issues, including the recent limitation of US resident
MD 21287, Telephone: 410 955 8240, Fax: 443 849 2946, E-mail: afader1@jhmi.edu work hours and decreased hysterectomy rates, compound
DOI: 10.4293/108680813X13654754535872 this problem.13,14 Surgical training involves the develop-
© 2013 by JSLS, Journal of the Society of Laparoendoscopic Surgeons. Published by ment of technical skills that are traditionally acquired
the Society of Laparoendoscopic Surgeons, Inc. through a Halstedian apprenticeship model in the oper-
JSLS (2013)17:219 –226 219
A Pilot Study of Surgical Training Using a Virtual Robotic Surgery Simulator, Tergas AI et al.
ating room, as well as the development of cognitive and Training Platforms
clinical skills.15 Fewer mentoring opportunities and de-
The da Vinci Skills Simulator is a VR simulation system
creased surgical volumes have led to the use of online
developed as a collaborative effort by Mimic Technologies
tutorials, models, and surgical skills laboratories to repli-
cate surgical situations. However, most of these methods and Intuitive Surgical. The da Vinci Skills Simulator uses
are limited in their ability to simulate live surgery, partic- MdVT and contains a variety of exercises designed for
ularly for robotic procedures. In the past decade, high- users to improve their proficiency with the da Vinci sur-
tech surgical simulators have been developed that have geon console controls. These exercises are organized by
revolutionized the approach to surgical education and the following skill categories: EndoWrist manipulation,
may help overcome many of these challenges. For in- camera and clutching, fourth-arm integration, system set-
stance, the da Vinci Surgical System (dVSS) (Intuitive Sur- tings, needle control and driving, and energy and dissec-
gical, Sunnyvale, CA, USA) can be used in conjunction tion. The simulator, which is packed in a portable case, or
with training models to create a dry laboratory platform “backpack,” measures 57.2 cm ⫻ 60.3 cm and attaches
that allows trainees to practice various robotic skills be- directly on the back of the dVSS Si or Si-e surgeon console
fore operating on patients. (Intuitive Surgical) so that the console can be used for VR
training without the need for the patient-side cart or in-
Perhaps the most exciting development in simulation sci-
struments (Figure 1). No additional system components
ence is the advent of computer or virtual reality (VR)
are required.
surgical simulators. The most sophisticated of the avail-
able robotic surgical simulators is the da Vinci Skills Sim-
ulator (Intuitive Surgical), which uses Mimic VR training
software (MdVT) (Mimic Technologies, Seattle, WA, USA).
Hung et al.16 recently demonstrated the face, content, and
construct validity of this novel VR simulator. The da Vinci
Skills Simulator contains ⬎35 training exercises including
modules that test basic skills such as camera and clutch
control, as well as more advanced tasks such as energy
control, needle driving, and suturing. The modules were
designed to be applicable for surgeons of any subspe-
cialty; however, the needle-driving and suturing exercises
are particularly relevant to gynecologists, who perform
these tasks routinely in gynecologic surgery. Therefore
the study objectives were to compare the utility of learn-
ing a specific suturing task on the da Vinci Skills Simulator
versus training on the dVSS dry laboratory platform
among novice robotic surgeons and to determine the
attitudes of gynecologic trainees regarding the different
training platforms.
METHODS
Participants
This was a single-institution, institutional review board–
approved prospective pilot study performed at Greater
Baltimore Medical Center and Johns Hopkins Hospital
(Baltimore, MD, USA). Medical students and gynecology
trainees (postgraduate years 1– 6) who had participated in
⬍10 robotic-assisted surgeries were enrolled. Participants
were assigned to train on either the da Vinci Skills Simu- Figure 1. da Vinci Skills Simulator shown attached to da Vinci
lator with MdVT or the dVSS dry laboratory platform. Surgical Si console.17
220 JSLS (2013)17:219 –226
The dVSS dry laboratory platform involves the use of all ratory model using a delayed absorbable, barbed suture
the components of the dVSS, which include the surgical on the dVSS dry laboratory platform (Figure 3). Three
console, the patient-side cart, EndoWrist instruments, and targets were placed along each side of the incision, each
the vision cart. All of the components are set up as they approximately 1 cm apart. The testing model was distinct
would be for live surgery, with a training model in place from the training exercises for both groups, and no par-
of a live patient. Various training models are available, ticipants were given the opportunity to practice on the
such as The Chamberlain Group’s Robotic Oval Hex Pod testing model. Suturing was selected as the testing task
model and Robotic Sea Spikes model (The Chamberlain because it is a complex but integral skill required in many
Group, Great Barrington, MA, USA). A demonstration of gynecologic procedures. Performance on the pretests and
the dVSS dry laboratory training platform setup is shown post-tests was monitored and recorded by 2 members of
in Figure 2. the research team watching the participants (A.I.T. and
A.N.F.). Metrics measured included time to complete the
Pretest and Post-Test task, number of instrument movements and instrument
collisions, number of instances when instruments were
Before and after completion of the training session, both
out of view, and number of missed targets. Participants
groups completed the same pretests and post-tests, con-
were timed from when they picked up the needle with the
sisting of suturing an incision in a vaginal cuff dry labo-
needle driver to when they passed through the last
target and pulled the suture for a tight closure. A
“missed target” was defined as passing the tip of the
needle through an area that was not demarcated on the
vaginal cuff model.
Training Sessions
The MdVT cohort trained on the VR simulator for 60
minutes using a needle-driving exercise known as “suture
sponge level 1.” This is an exercise in which the partici-
Figure 3. Vaginal cuff model used for pretests and post-tests
Figure 2. dVSS dry laboratory training platform setup. (inferior incision).
JSLS (2013)17:219 –226 221
A Pilot Study of Surgical Training Using a Virtual Robotic Surgery Simulator, Tergas AI et al.
pant sits at the robotic console and drives the needle backpack and powering the console and simulator on and
through entrance and exit targets on a virtual sponge off.
(Figure 4) using both hands. The exercise required the
participant to drive the needle at many different angles Survey
and with the left and right hands. After completion of the
exercise, the participant was given a detailed performance Finally, the participants completed an online anonymous
report, an example of which is shown in Figure 5. Mea- survey via the SurveyMonkey Web site. The survey as-
sured metrics included time to complete exercise, econ- sessed perceived clinical utility of the simulator platforms
omy of motion, instrument collisions, excessive instru- and queried participants regarding their overall experi-
ment force, instruments out of view, master workspace ence with the training sessions and satisfaction with the
range, drops, missed targets, critical errors, and overall training modalities. For the purposes of assessing sat-
score. These metrics were used to provide feedback to the isfaction with the MdVT, the dVSS group was allowed to
participants. spend time using the VR simulator after completion of
the post-test.
The training session for the dVSS group was also 60
minutes and consisted of suturing around the perimeter of Statistics
geometric shapes on a dry laboratory model (Figure 6)
Performance metrics were analyzed with the Student paired
distinct from the testing model. A proctor was present at
t test, and P ⬍ .05 was considered statistically significant.
all times and provided performance-improvement feed-
Statistical analysis was performed with Stata statistical soft-
back to participants in both training cohorts.
ware, version 11.1 (StataCorp, College Town, TX, USA).
The dVSS dry laboratory platform required the presence of
a scrub technician, Intuitive Surgical representative, or an RESULTS
attending physician with knowledge of the robotic system
to set up the robotic arms in the appropriate configura- Twenty trainees participated in the study: 10 medical stu-
tion, install the appropriate instruments, white-balance dents and 10 obstetrics and gynecology residents or fel-
and calibrate the camera, oversee the training session, and lows. Table 1 shows participant characteristics. Regarding
undock the instruments and power down the system at previous surgical experience, 80% of the participants had
the completion of the training. Conversely, the MdVT no previous robotic surgery experience and 50% also had
session required the surgeon console with the attached no experience with laparoscopy.
The results of the pretests and post-tests for the 2 simulation
groups are shown in Table 2. The mean pretest completion
times were comparable between the MdVT and dVSS groups
(189.8 seconds and 235.0 seconds, respectively; P ⫽ .390).
Training on both the MdVT and the dVSS was associated
with a significant and comparable decrease in time to com-
pletion of the tasks (64.9-second decrease in time to com-
pletion for MdVT [P ⫽ .044] and 63.9-second decrease for
dVSS [P ⫽ .002]). An improvement in the number of move-
ments used to complete the task was seen in both groups
(mean of 12.1 fewer movements in the MdVT group [P ⫽
.022] and mean of 17.3 fewer movements in the dVSS group
[P ⬍ .001]). However, training on the dVSS, but not the
MdVT, was associated with a significant decrease in the
number of missed targets (0.8 fewer missed targets for MdVT
[P ⫽ .153] and 1.1 fewer missed targets for dVSS [P ⫽ .007]).
Similarly, training on the dVSS, but not the MdVT, was
associated with a significant decrease in instances of instru-
ments out of view (0.4 fewer instances for MdVT [P ⫽ .443]
Figure 4. Screen shot of da Vinci Skills Simulator “suture sponge and 0.7 fewer instances for dVSS [P ⫽ .045]). The mean
level 1” needle-driving exercise. number of instrument collisions for the pretest was less than
222 JSLS (2013)17:219 –226
Figure 5. Example of da Vinci Skills Simulator performance evaluation report.18
1 for both groups, and therefore no meaningful improve- attend future training sessions (mean, 4.5). Respondents
ment occurred as a result of the training sessions. Subjec- believed that the MdVT improved hand-eye coordination
tively, setup for the dVSS dry laboratory training sessions (95.8%), dexterity (100%), and instrument multitasking
required substantially more time and effort and the presence (87.5%) and that the VR software provided high-fidelity,
of a proctor with a high working knowledge and familiarity realistic training scenarios (87.5%). Specifically, the re-
with the robotic system than setup of the MdVT simulation spondents believed that the following aspects of the sim-
session. As described earlier, there were many more metrics ulator were realistic: instrument movement (mean, 4.1),
measured with the MdVT that could not be calculated or depth perception (mean, 3.8), and interaction of instru-
measured with the dVSS and therefore were not recorded for ments with other objects (mean, 3.7). We asked the ob-
the purpose of comparison of performance between the 2 stetrics and gynecology trainees only how important they
groups. consider training in robotic surgery; these respondents
Almost all of the participants (19 of 20) completed the believe that training in robotic surgery is “extremely”
23-item survey. On a 5-point Likert scale, most partici- important (mean, 4.6). Regarding user preference, most
pants found the training “definitely useful” in improving participants (58%) preferred the MdVT training plat-
robotic surgical skills (mean, 4.67) and would “definitely” form, with 33% preferring the dVSS training platform
JSLS (2013)17:219 –226 223
A Pilot Study of Surgical Training Using a Virtual Robotic Surgery Simulator, Tergas AI et al.
DISCUSSION
This is one of the first prospective studies in gynecology
comparing the utility of a VR robotic simulator with that of
a standard dVSS dry laboratory platform in the training of
gynecologic residents and fellows. In this pilot study,
training on either the VR da Vinci Surgical Simulator or the
dVSS dry laboratory platform resulted in significant im-
provements in technical performance for novice robotic
surgeons, including a decrease in time to completion and
number of instrument movements. Training on the dVSS
dry laboratory platform also resulted in a decrease in the
number of missed targets and instances of instruments out
of view. However, both groups had such low mean num-
bers of both metrics that this additional benefit seen in the
dVSS group is difficult to interpret and may not be “clin-
ically” significant. Our results show that training on both
simulation platforms improved economy of motion, an
important metric that may help surgeons operate more
efficiently and potentially minimize tissue handling. How-
Figure 6. Robotic Oval and Hex Pod model (The Chamberlain ever, most of the study participants preferred the MdVT
Group) used for dVSS dry laboratory platform training session.19 training platform, although both platforms were found to
be “definitely useful” for improving robotic surgical skills.
Table 1.
Participant Characteristics Currently, there are 4 VR robotic surgical simulators avail-
Characteristics Data able in the United States: RoSS (Simulated Surgical Sys-
tems, Williamsville, NY, USA), SEP Robot (SimSurgery,
a
Mean age (SD ), yr 29 (4.8) Boston, MA, USA), da Vinci Skills Simulator (Intuitive
Gender Surgical, Sunnyvale, CA, USA), and Mimic dV-Trainer
Female 70% (Mimic Technologies, Seattle, WA, USA). VR robotic sur-
Male 30% gery simulators are an emerging technology, and the re-
search on their use as an educational tool in robotic
Level of training
surgery is limited. Schreuder et al.20 recently published a
Medical students 7
systematic review on training and learning strategies for
Junior residentsb 5 robotic-assisted laparoscopic surgery. Most the available
Senior residentsc 5 reported studies were small and comprised heteroge-
Fellowsd 3 neous study populations. Of the 13 studies of training
Mean no. of cases (SD) 1.9 (3.6) using VR robotic surgical simulators that were included in
this review, 8 had fewer than 20 participants and 6 had
a
SD ⫽ standard deviation.
b
groups that consisted of both surgical novices and ex-
First- and second-year obstetrics and gynecology residents. perts. The results of our study are consistent with this
c
Third- and fourth-year obstetrics and gynecology residents. review of the current literature, which shows that surgical
d
First-year obstetrics and gynecology fellows. skills training on VR simulators does have a significant
learning effect.20 Furthermore, our results are also consis-
tent with a study by Lerner et al.,21 which shows that
and 8% having no preference. Interestingly, when que- training on the VR Mimic dV-Trainer improved perfor-
ried regarding whether they had had any adverse ef- mance on the robot system equal to training with the
fects from the 60-minute study training sessions, 42% of robot itself with regard to improvements in completion
the participants reported mild hand and wrist soreness, times and number of instrument movements. A similar
16% reported neck or back pain, and 11% reported a equivalent improvement in technical performance was
transient headache. shown in a systematic review of conventional laparoscopy
224 JSLS (2013)17:219 –226
Table 2.
Pretest and Post-test Results for MdVT and dVSS Groups
MdVT Group dVSS Group
Metric Pretest Post-test Difference P Value Pretest Post-test Difference P Value
Time to completion, s 189.8 124.9 64.9 .044a 235.0 171 63.9 .002a
Instrument movements (no.) 43.7 31.6 12.1 .023a
54.0 36.7 17.3 ⬍.001a
Missed targets (no.) 2.3 1.5 0.8 .153 2.5 1.4 1.1 .007a
Instruments out of view (no.) 1.1 0.7 0.4 .443 1.1 0.4 0.7 .045a
Instrument collisions (no.) 0 0.1 ⫺0.1 .343 0.7 0.2 0.5 .052
a
Statistically significant.
surgical simulation training modalities.15 In this review, sim- of robotic console experience and baseline performance.
ulation training modalities generally showed results superior Moreover, use of the same pretest and post-test between
to no training at all but were not convincingly superior to the groups allowed for a direct comparison of perfor-
standard training or watching videos when assessed by op- mance after the training sessions on the respective plat-
erative performance. forms. However, this study was limited by the small num-
ber of participants, as well as the short duration and
Although this study and the current data on VR robotic
frequency of training sessions. The optimal duration and
surgery simulators do not support the notion that this
frequency of simulation training sessions are unknown.
technology is better than existing training modalities,
On the basis of the musculoskeletal complaints and tran-
there are benefits unique to the VR simulators that may
sient headaches reported by several of our participants,
not be captured in quantitative studies of technical per-
perhaps the duration of a training session should be less
formance. Most of our study participants preferred the VR
than 60 minutes to minimize strain caused by repetitive
simulator over the dVSS. Expert surgeons rated the simu-
movements.
lator highly for visual field, movement, and precision
compared with live surgery.16 VR simulators also provide
In the past decade, the rapid expansion and evolution of
detailed, objective feedback that can be stored and used
robotic surgery have posed a challenge for surgical edu-
to evaluate surgeon performance over time. The variety of
cators: what is the optimal approach to teaching robotic
exercises available provides a wide range of training tasks
surgery so that trainees achieve proficiency? Several other
and may prevent training from becoming dull and repet-
issues, such as mandated limited resident work hours and
itive. Both of these features may improve surgeon engage-
fewer procedures to be performed, contribute to this chal-
ment and motivation to use the trainer. Furthermore, in-
lenge. To address this, it is imperative that structured and
dependence from a moderator is key to facilitate use and
standardized robotic surgery training curricula are devel-
may not be necessary to improve surgeon performance.22
oped and implemented in residency and fellowship pro-
The many unique benefits of a VR surgical simulator
grams.20 Guzzo and Gonzalgo23 described a 3-phase struc-
should be weighed against its potential drawbacks, per-
tured robotic training program: the preclinical phase, the
haps the most significant of which is cost, which is ap-
beside-assistant phase, and the operative console phase.
proximately $100,000 according to the manufacturer of
VR simulators would be useful in both the preclinical
the da Vinci Skills Simulator. For some institutions, this
phase and the operative console phase. After the trainee
may be cost-prohibitive. Furthermore, in their current
has gained familiarity with the robotic system through
state of development, the VR simulators are not sophisti-
didactics and videos, VR simulators can provide a stress-
cated enough to perform specific procedural tasks, such
free environment in which they can gain familiarity and
as hysterectomy or prostatectomy or even knot-tying. If
then proficiency with the console hand controls and foot
these issues can be mitigated, then the utility of the VR
pedals. During the operative console phase, the trainee
simulators would improve substantially.
may fine-tune and build on the technical skills that they
Strengths of the study include a prospective study design have gained in the other phases of training and while
and comparison groups that were well matched in terms performing live surgery.
JSLS (2013)17:219 –226 225
A Pilot Study of Surgical Training Using a Virtual Robotic Surgery Simulator, Tergas AI et al.
CONCLUSION 9. Intuitive Surgical. Annual report 2009. Available at: https://
materials.proxyvote.com/Approved/46120E/20100222/AR_53320/
In our study the VR simulator was shown to be a valuable HTML2/default.htm. Accessed December 5, 2011.
learning tool that trainees preferred over the dry labora-
10. Intuitive Surgical. Annual report 2010. Available at: http://
tory platform with similar efficacy. Additional benefits investor.intuitivesurgical.com/phoenix.zhtml?c⫽122359&p⫽
unique to the VR platform include autonomy of use, irol-reportsAnnual. Accessed December 5, 2011.
computerized performance feedback, and ease of setup.
These features may facilitate more efficient and sophisti- 11. Lee JY, Mucksavage P, Sundaram CP, McDougall EM. Best
cated simulation training above that of the conventional practices for robotic surgery training and credentialing. J Urol.
2011;185:1191–1197.
dry laboratory simulators, with no loss of efficacy. Pro-
spective validation studies of surgical curricula that incor- 12. Gobern JM, Novak CM, Lockrow EG. Survey of robotic
porate VR robotic surgical simulators are warranted. surgery training in obstetrics and gynecology residency. J Minim
Invasive Gynecol. 2011;18:755–760.
References: 13. Lepine LA, Hillis SD, Marchbanks PA, et al. Hysterectomy
1. Ballantyne GH, Moll F. The da Vinci telerobotic surgical surveillance—United States, 1980 –1993. MMWR CDC Surveill
system: the virtual operative field and telepresence surgery. Surg Summ. 1997;46:1–15.
Clin North Am. 2003;83:1293–1304, vii. 14. Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hys-
2. Shafer A, Boggess JF. Robotic-assisted endometrial cancer terectomy surveillance in the United States, 2000 –2004. Am J
staging and radical hysterectomy with the da Vinci surgical Obstet Gynecol. 2008;198:34.e1–34.e7.
system. Gynecol Oncol. 2008;111(Suppl):S18 –S23. 15. Sutherland LM, Middleton PF, Anthony A, et al. Surgical
3. van der Schatte Olivier RH, Van’t Hullenaar CD, Ruurda JP, simulation: a systematic review. Ann Surg. 2006;243:291–300.
Broeders IA. Ergonomics, user comfort, and performance in 16. Hung AJ, Zehnder P, Patil MB, et al. Face, content and
standard and robot-assisted laparoscopic surgery. Surg Endosc. construct validity of a novel robotic surgery simulator. J Urol.
2009;23:1365–1371. 2011;186:1019 –1024.
4. Ramirez PT, Adams S, Boggess JG, et al. Robotic-assisted 17. da Vinci Surgical Simulator brochure. Available at: http://
surgery in gynecologic oncology: a Society of Gynecologic On- www.intuitivesurgical.com/products/skills_simulator/. Ac-
cology consensus statement. Gynecol Oncol. 2012;124:180 –184. cessed December 18, 2011.
5. Gaia G, Holloway RW, Santoro L, Ahmad S, Di Silverio E, 18. Mimic Technologies. Available at: http://www.mimic.ws/
Spinillo A. Robotic-assisted hysterectomy for endometrial cancer products/performance-evaluation.php. Accessed December 18,
compared with traditional laparoscopic and laparotomy approach- 2011.
es: a systematic review. Obstet Gynecol. 2010;116:1422–1431.
19. The Chamberlin Group. Available at: http://www.thecgroup.
6. Reza M, Maeso S, Blasco JA, Andradas E. Meta-analysis of com/product/reproductive-urological/robotic-3/robotic-oval-hex-
observational studies on the safety and effectiveness of robotic pod. Accessed December 18, 2011.
gynaecological surgery. Br J Surg. 2010;97:1772–1783.
20. Schreuder H, Wolswijk R, Zweemer R ,Schijven M, Verheijen
7. Lim PC, Kang E, Park do H. A comparative detail analysis of R. Training and learning robotic surgery, time for a more struc-
the learning curve and surgical outcome for robotic hysterec- tured approach. BJOG. 2012;119:137–149.
tomy with lymphadenectomy versus laparoscopic hysterectomy
with lymphadenectomy in treatment of endometrial cancer: a 21. Lerner MA, Ayalew M, Peine WJ, Sundaram CP. Does train-
case-matched controlled study of the first one hundred twenty ing on a virtual reality robotic simulator improve performance on
two patients. Gynecol Oncol. 2011;120:413– 418. the Da Vinci surgical system? J Endourol. 2010;24:467– 472.
8. Weinberg L, Rao S, Escobar PF. Robotic surgery in gynecol- 22. Boyle E, O’Keeffe DA, Naughton PA, Hill AD, McDonnel CO,
ogy: an updated review. Obstet Gynecol Int. 2011;2011:852061. Moneley D. The importance of expert feedback during endovascu-
lar simulator training. J Vasc Surg. 2011;54:240 –248.e1.
23. Guzzo TJ, Gonzalgo ML. Robotic surgical training of the
urologic oncologist. Urol Oncol. 2009;27:214 –217.
226 JSLS (2013)17:219 –226
You might also like
- The SAGES Manual of Robotic SurgeryFrom EverandThe SAGES Manual of Robotic SurgeryAnkit D. PatelNo ratings yet
- Comprehensive Healthcare Simulation: Surgery and Surgical SubspecialtiesFrom EverandComprehensive Healthcare Simulation: Surgery and Surgical SubspecialtiesDimitrios StefanidisNo ratings yet
- Virtual SurgeryDocument20 pagesVirtual SurgeryMidhun MadhavanNo ratings yet
- Virtual Surgery 07012013125131 Virtual SurgeryDocument20 pagesVirtual Surgery 07012013125131 Virtual Surgeryjosemonj77No ratings yet
- Residency Training in Robotic Surgery The Role of SimulationDocument7 pagesResidency Training in Robotic Surgery The Role of SimulationGabrielly RobledilhoNo ratings yet
- Bjs 9711Document15 pagesBjs 9711Bintang MuslimahNo ratings yet
- Technical Seminar PPTDocument15 pagesTechnical Seminar PPTshashidharsykNo ratings yet
- Seminar Report On Virtual SurgeryDocument17 pagesSeminar Report On Virtual SurgeryAfrah RamsheedNo ratings yet
- Virtual SurgeryDocument22 pagesVirtual SurgeryMounika Surapaneni100% (1)
- Walliczek Dworschak2016Document10 pagesWalliczek Dworschak2016Eham AroraNo ratings yet
- Emergence of Three-Dimensional Video Microsurgery For Male InfertilityDocument2 pagesEmergence of Three-Dimensional Video Microsurgery For Male InfertilityZaliyaNo ratings yet
- Virtual Surgery ReportDocument6 pagesVirtual Surgery ReportNaveen Krishnan75% (4)
- The Use of Surgical Simulators To Reduce ErrorsDocument14 pagesThe Use of Surgical Simulators To Reduce ErrorsVasenkoMishaNo ratings yet
- Robotics in General Surgery: James Wall, MD, Venita Chandra, MD and Thomas Krummel, MDDocument18 pagesRobotics in General Surgery: James Wall, MD, Venita Chandra, MD and Thomas Krummel, MDRizwan AhmedNo ratings yet
- Jara 2020Document8 pagesJara 2020Ágoston János CsigiNo ratings yet
- CH 3Document21 pagesCH 3Mohamed AhmedNo ratings yet
- Simulation Improves Patient SafetyDocument5 pagesSimulation Improves Patient SafetyZeptalanNo ratings yet
- 10.1007/s00464 017 5634 6 PDFDocument11 pages10.1007/s00464 017 5634 6 PDFAnonymous wVUGfwWSYNo ratings yet
- Robotic-Assisted Surgery For Low Rectal Dissection: From Better Views To Better OutcomeDocument6 pagesRobotic-Assisted Surgery For Low Rectal Dissection: From Better Views To Better OutcomeMarwa MedNo ratings yet
- Vs ReportDocument20 pagesVs ReportSagar PawadiNo ratings yet
- Preliminary Design and Evaluation of A Remote Tele Mentoring System For Minimally Invasive SurgeryDocument12 pagesPreliminary Design and Evaluation of A Remote Tele Mentoring System For Minimally Invasive Surgeryjackie tesilloNo ratings yet
- Collaborative Robotics Toolkit CRTK Open Software Framework For Surgical Robotics Research-2Document8 pagesCollaborative Robotics Toolkit CRTK Open Software Framework For Surgical Robotics Research-2Varun KumarNo ratings yet
- 1 s2.0 S1931720414000749 MainDocument6 pages1 s2.0 S1931720414000749 MainFarzadNo ratings yet
- Adaptive Architecture Supports Context-Aware Collaborative Surgical SimulatorsDocument2 pagesAdaptive Architecture Supports Context-Aware Collaborative Surgical SimulatorsJhofran ArleyNo ratings yet
- Me326 Individual ProjectDocument5 pagesMe326 Individual Projectapi-582462159No ratings yet
- Latest Trends in Minimally Invasive SurgeryDocument4 pagesLatest Trends in Minimally Invasive SurgeryMc_Lopez_1761No ratings yet
- A Development of Assistant Surgical Robot System Based On Surgical Operation by Wire and Hands On Throttle and Stick 2016Document19 pagesA Development of Assistant Surgical Robot System Based On Surgical Operation by Wire and Hands On Throttle and Stick 2016Andualem TadesseNo ratings yet
- Trainpdt EVT0905 Featured Inno 01 Us PiDocument3 pagesTrainpdt EVT0905 Featured Inno 01 Us PiSandeep KumarNo ratings yet
- Virtual Reality Simulation To Enhance Laparoscopic Salpingectomy SkillsDocument7 pagesVirtual Reality Simulation To Enhance Laparoscopic Salpingectomy SkillsHanna 123No ratings yet
- Augmented Reality To Improve Surgical Simulation Lessons Learned Towards The Design of A Hybrid Laparoscopic Simulator For CholecystectomyDocument14 pagesAugmented Reality To Improve Surgical Simulation Lessons Learned Towards The Design of A Hybrid Laparoscopic Simulator For CholecystectomyJohn DoeNo ratings yet
- VR simulation for CPR trainingDocument17 pagesVR simulation for CPR trainingomamah.almousaNo ratings yet
- Augmented-Reality-Based-Visual-Haptic-Modeling-For 2021 Virtual-Reality - inDocument13 pagesAugmented-Reality-Based-Visual-Haptic-Modeling-For 2021 Virtual-Reality - inapi-688059491No ratings yet
- Icu 58 297 PDFDocument2 pagesIcu 58 297 PDFNeil GriggNo ratings yet
- 2023-PEg TRAnsfer Workflow Recognition Challenge Report - Do Multimodal Data Improve RecognitionDocument18 pages2023-PEg TRAnsfer Workflow Recognition Challenge Report - Do Multimodal Data Improve RecognitionlancerhlyNo ratings yet
- New Microsoft Office Word Document1Document46 pagesNew Microsoft Office Word Document1rajaishaNo ratings yet
- Assignment 4 SolutionDocument6 pagesAssignment 4 SolutionAya SulaqNo ratings yet
- Viglialoro 2018Document14 pagesViglialoro 2018vishalmate10No ratings yet
- REMOTE SURGERY: TELESURGERY OVER LONG DISTANCESDocument6 pagesREMOTE SURGERY: TELESURGERY OVER LONG DISTANCESramananbmeNo ratings yet
- Robotic Surgery A Current Perspective: ObjectiveDocument7 pagesRobotic Surgery A Current Perspective: ObjectiveirismgallNo ratings yet
- Robotics in Colorectal Surgery: Telemonitoring and TeleroboticsDocument10 pagesRobotics in Colorectal Surgery: Telemonitoring and TeleroboticsprivedNo ratings yet
- Surgeons Strive Hard To Break The Da Vinci CodeDocument3 pagesSurgeons Strive Hard To Break The Da Vinci CodeasdasddsaNo ratings yet
- Korzeniowski 2016Document13 pagesKorzeniowski 2016KhalilSemlaliNo ratings yet
- Survey on impact of Robotics on HealthcareDocument8 pagesSurvey on impact of Robotics on Healthcareharsh3112aNo ratings yet
- Robotic Nurse Duties in The Urology Operative Room: 11 Years of ExperienceDocument8 pagesRobotic Nurse Duties in The Urology Operative Room: 11 Years of ExperienceLaura CursaruNo ratings yet
- Computer Vision in The Surgical Operating Room: Review ArticleDocument7 pagesComputer Vision in The Surgical Operating Room: Review Articlelabril.torresmNo ratings yet
- Robo SurgeryDocument9 pagesRobo Surgeryrwong1231No ratings yet
- Coles, Meglan, John - 2010 - The Role of Haptics in Medical Training Simulators A Survey of The State-Of-The-ArtDocument18 pagesColes, Meglan, John - 2010 - The Role of Haptics in Medical Training Simulators A Survey of The State-Of-The-ArtNigel W. JohnNo ratings yet
- Robotic SurgeryDocument11 pagesRobotic SurgerySam AlatawiNo ratings yet
- Enhanced Recovery Simulation in Colorectal Surgery: Design of Virtual Online PatientsDocument9 pagesEnhanced Recovery Simulation in Colorectal Surgery: Design of Virtual Online PatientsjohanisNo ratings yet
- Anaesthesia For Robotic SurgeryDocument5 pagesAnaesthesia For Robotic Surgerysangamitraachu100% (1)
- Training in Uniportal VATS LobectomyDocument7 pagesTraining in Uniportal VATS LobectomyAlin Ionut BurlacuNo ratings yet
- RoboticSurgery An Evolution in PracticeDocument3 pagesRoboticSurgery An Evolution in PracticeJoão Lourenço0% (1)
- "Reality Is Merely An Illusion, Although A Very Persistent One." - Albert Einstein (German Born American Physicist)Document28 pages"Reality Is Merely An Illusion, Although A Very Persistent One." - Albert Einstein (German Born American Physicist)Nitin KumarNo ratings yet
- Urologic Robots and Future Directions: Dan Stoianovici, PHDDocument10 pagesUrologic Robots and Future Directions: Dan Stoianovici, PHDavinashjhamechxNo ratings yet
- Adhami2000 Chapter PlanningAndSimulationOfRoboticDocument10 pagesAdhami2000 Chapter PlanningAndSimulationOfRoboticYessica RosasNo ratings yet
- Robot Assisted Surgery1Document18 pagesRobot Assisted Surgery1Mahesh JoshiNo ratings yet
- Bhandari 2019Document7 pagesBhandari 2019Ágoston János CsigiNo ratings yet
- Review of DL in Minimally Invasive SurgeryDocument21 pagesReview of DL in Minimally Invasive SurgeryJoel JacobNo ratings yet
- Indoor Navigation Strategies for Aerial Autonomous SystemsFrom EverandIndoor Navigation Strategies for Aerial Autonomous SystemsRating: 5 out of 5 stars5/5 (2)
- Bariatric Robotic Surgery: A Comprehensive GuideFrom EverandBariatric Robotic Surgery: A Comprehensive GuideCarlos Eduardo DomeneNo ratings yet
- Hernia-To-Neck Ratio Is Associated With Emergent Ventral Hernia Repair - PubMedDocument1 pageHernia-To-Neck Ratio Is Associated With Emergent Ventral Hernia Repair - PubMedEham AroraNo ratings yet
- Al-Mansour2021 Validation of A Simple Technique of Volumetric Analysis of Complex Hernias Without 3D ReconstructionDocument7 pagesAl-Mansour2021 Validation of A Simple Technique of Volumetric Analysis of Complex Hernias Without 3D ReconstructionEham AroraNo ratings yet
- Fafaj2021 Tanaka Score ReliabilityDocument6 pagesFafaj2021 Tanaka Score ReliabilityEham AroraNo ratings yet
- Mommers2017 Impact of Hernia Volume On Pulmonary Complications in Complex Hernia RepairsDocument6 pagesMommers2017 Impact of Hernia Volume On Pulmonary Complications in Complex Hernia RepairsEham AroraNo ratings yet
- Hassan2022 Novel Machine Learning Approach For The Prediction of Hernia Recurrence, Surgical Complication, and 30-Day Readmission After Abdominal Wall ReconstructionDocument10 pagesHassan2022 Novel Machine Learning Approach For The Prediction of Hernia Recurrence, Surgical Complication, and 30-Day Readmission After Abdominal Wall ReconstructionEham AroraNo ratings yet
- Objective Assessment of Technical Surgical SkillsDocument17 pagesObjective Assessment of Technical Surgical SkillsEham AroraNo ratings yet
- The Effect of Different Training Exercises On The Performance Outcome On The Da Vinci Skills SimulatorDocument9 pagesThe Effect of Different Training Exercises On The Performance Outcome On The Da Vinci Skills SimulatorEham AroraNo ratings yet
- Walliczek Dworschak2016Document10 pagesWalliczek Dworschak2016Eham AroraNo ratings yet
- Objective Structured Assessment of Technical Skill (OSATS) For Surgical ResidentsDocument6 pagesObjective Structured Assessment of Technical Skill (OSATS) For Surgical ResidentsEham AroraNo ratings yet
- User Guide For Speedlink: Hearing Instrument Programming InterfaceDocument26 pagesUser Guide For Speedlink: Hearing Instrument Programming InterfaceMarcio Lobo SelvagemNo ratings yet
- 16V2000 Detroit W5Document2 pages16V2000 Detroit W5Rendy Chavez LesmanaNo ratings yet
- DS3 QueuesDocument38 pagesDS3 QueuesHabib ur rehmanNo ratings yet
- Project Managemen 2 PDFDocument14 pagesProject Managemen 2 PDFMisha RanaNo ratings yet
- Journal of Energy StorageDocument14 pagesJournal of Energy StorageLuis Antonio CNo ratings yet
- SET UP EQMOD SOFTWARE FOR ASTROPHOTOGRAPHYDocument5 pagesSET UP EQMOD SOFTWARE FOR ASTROPHOTOGRAPHYMechtatel HrenovNo ratings yet
- RSP Robinson R44 Quick Start Guide BETA1.1Document14 pagesRSP Robinson R44 Quick Start Guide BETA1.1CristianoVelosodeQueirozNo ratings yet
- Memorandum: From: TJC and Associates, Inc. Date: March, 2014 Subject: Seismic Anchorage Submittals ChecklistDocument2 pagesMemorandum: From: TJC and Associates, Inc. Date: March, 2014 Subject: Seismic Anchorage Submittals ChecklistponjoveNo ratings yet
- Induction Cooker Circuit DesignDocument39 pagesInduction Cooker Circuit DesignMr. Pushparaj Ghodke74% (31)
- Colas Rail Brochure CORPORATE v4 0Document28 pagesColas Rail Brochure CORPORATE v4 0mostafa shoshaNo ratings yet
- All Motor, &electrical Equipment in StorDocument8 pagesAll Motor, &electrical Equipment in StorMd. Saddam HossainNo ratings yet
- SRX SFP 10ge Dac 1MDocument7 pagesSRX SFP 10ge Dac 1MAssem SamirNo ratings yet
- 6 - StringsDocument19 pages6 - Stringsaljazi mNo ratings yet
- SG110CXPV Grid-Connected Inverter User ManualDocument101 pagesSG110CXPV Grid-Connected Inverter User ManualAizat AlongNo ratings yet
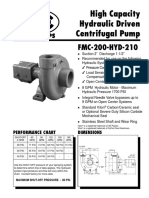
- FMC 200 Hyd 210Document2 pagesFMC 200 Hyd 210Ruben SaccoNo ratings yet
- CCIE SPv4 Topology DiagramsDocument17 pagesCCIE SPv4 Topology DiagramsTilak RoyNo ratings yet
- Lecture - Week - 3 - Software MetricsDocument29 pagesLecture - Week - 3 - Software MetricsManlNo ratings yet
- Mrs J's Resource Creations ©Document7 pagesMrs J's Resource Creations ©syddysNo ratings yet
- Service Bulletin: Fuel Injection PumpDocument15 pagesService Bulletin: Fuel Injection PumpKrunoslavNo ratings yet
- + - OSDI2020-FIRM - An Intelligent Fine-Grained Resource Management Framework For SLO-Oriented MicroservicesDocument22 pages+ - OSDI2020-FIRM - An Intelligent Fine-Grained Resource Management Framework For SLO-Oriented MicroservicesBENKEMCHI OussamaNo ratings yet
- 9Document36 pages9vscolegit shoppeNo ratings yet
- Networks Pre Connection Attacks PDFDocument15 pagesNetworks Pre Connection Attacks PDFaniket kasturiNo ratings yet
- Luanshya Technical College SCADA Scan IntervalDocument5 pagesLuanshya Technical College SCADA Scan IntervalAlfred K ChilufyaNo ratings yet
- Prediction of Stock Price Based On Hidden Markov Model and Nearest Neighbour AlgorithmDocument31 pagesPrediction of Stock Price Based On Hidden Markov Model and Nearest Neighbour AlgorithmFirman AkbarNo ratings yet
- Data Mining 1-3Document29 pagesData Mining 1-3Singer JerowNo ratings yet
- MTB 500i W R TXM Technical ManualDocument26 pagesMTB 500i W R TXM Technical ManualSaranyoo CHOOTIMASNo ratings yet
- Ryobi 18 Volt Impact Wrench Model Number P261 Repair SheetDocument4 pagesRyobi 18 Volt Impact Wrench Model Number P261 Repair SheetRicardo Ran Pos100% (1)
- CMT1Document10 pagesCMT1Dongneu Nguyen100% (1)
- Lesson Plan in Random VariableDocument10 pagesLesson Plan in Random VariableJeson N. RondinaNo ratings yet
- Control Valves PDFDocument21 pagesControl Valves PDFRiyadh DaoudiNo ratings yet